Abstract
Background/Objective:
Mobility limitation is commonly the first sign of impaired physical function and predisposes older adults to disability. Moreover, recent epidemiological studies have classified neuromuscular strength as the best explanator of mobility limitation. However, existing cutoffs have not been adequately analyzed regarding accuracy. Therefore, our aims were to define and compare the accuracy of different cutoff points of handgrip strength for the identification of mobility limitation.
Methods:
Cross-sectional study with 5,783 participants from the SABE (Saúde, Bem-Estar e Envelhecimento [Health, Wellbeing and Aging]) and ELSA (English Longitudinal Study of Ageing) cohorts aged 60 years or older. Handgrip strength was measured using a dynamometer. Walking speed <0.8m/s was considered mobility limitation. Receiver operating characteristic curves and probabilities of presenting mobility limitation were calculated.
Results:
Handgrip strength <32 kg for men and <21 kg for women demonstrated good diagnostic accuracy for mobility limitation, with 49.1% sensitivity and 79.8% specificity for men and 58.6% sensitivity and 72.9% specificity for women. The fully adjusted models had an area under the curve of 0.82 for men and 0.83 for women, with odds of presenting mobility limitation of 1.88 [95% CI: 1.50 – 2.37] for men and 1.89 [CI95 %: 1.57 – 2.27] for women.
Conclusions:
The results of this study support the accuracy of handgrip strength as a clinical marker of mobility limitation. Furthermore, manual dynamometry is easily incorporated into clinical practice, has a good cost-benefit, besides being a simple, valid, reliable and effective method for use in both the scientific community and outpatient practice.
Keywords: Accuracy analysis, Grip strength, Gait speed, Mobility limitation, Older adults
1. Introduction
Handgrip strength is one of the key components in the evaluation of frailty and sarcopenia and is strongly associated with diverse negative outcomes in older adults (Dodds et al., 2014; Cruz-Jentoft et al., 2019). Among such outcomes, the Foundation for the National Institutes of Health Sarcopenia Project reports that a mobility limitation is commonly the first sign of impaired physical functioning and predisposes older adults to functional disability, falls (Cruz-Jentoft et al., 2010; Cruz-Jentoft et al., 2019), hospitalizations (Kim & Choi, 2013), institutionalization and premature death (Alexandre, Duarte, Santos, Wong & Lebrão, 2014).
The European Working Group on Sarcopenia in Older People (EWGSOP, 2018) recommends concentrating the diagnosis of sarcopenia on low muscle strength as its fundamental characteristic, suggesting handgrip cutoffs of < 27 kg for men and < 16 kg for women (Cruz-Jentoft et al., 2019). Researchers have also suggested an association between low muscle strength and reductions in both muscle mass and quality and that a poor physical performance attributed to the mobility limitation is an indicator of the severity of sarcopenia adults (Dodds et al., 2014; Cruz-Jentoft et al., 2019).
However, consensus has not been achieved about the best cutoff point for handgrip strength to identify mobility limitation (Cawthon et al., 2020; McLean et al., 2014; Studenski et al., 2014; Manini, 2013). Lauretani and collaborators (2003) were the first researchers to present a cutoff for handgrip strength as an explanator of mobility limitation (< 30 kg for men and < 20 kg for women). Different cutoffs were subsequently proposed, such as < 37 kg for men and < 21 kg for women (Sallinen et al., 2010); < 32.45 kg for men and < 18.95 kg for women (Dong et al., 2016); < 25.8 kg for men and < 17.4 kg for women (Vasconcelos et al., 2016); and < 39 kg for men and < 22 kg for women (Duchowny, Peterson & Clarke, 2017). Moreover, Aley and collaborators (2014) proposed cutoffs of < 26 kg for men and < 16 kg for women as a better indicator of weakness associated with mobility limitation and cutoffs of < 32 kg for men and < 20 kg for women as a better indicator of intermediate weakness associated with mobility limitation.
Cawthon et al. (2020) describe handgrip strength as the best discriminator for limited mobility, highlighting the need for further studies involving the development of a risk model capable of explaining this outcome considering age, sex and comorbidities, since existing cutoffs do not explain mobility limitation and do not present good accuracy analyses. Therefore, the aims of the present study were to establish a cutoff for handgrip strength that enables identifying mobility limitation in older adults and compare it to the accuracy properties attributed to cutoffs of < 26, < 27, < 30, < 32, < 33, < 37 and < 39 kg for men and < 16, < 17, < 19, < 20, < 21 and < 22 kg for women found in the literature.
2. Methods
2.1. Study population
The data were extracted from the Saúde, Bem-Estar e Envelhecimento (SABE [Health, Wellbeing and Aging]) Study, which is a longitudinal study with a probabilistic, representative sample of individuals aged 60 years or older residing in urban areas of the city of São Paulo, Brazil (Palloni & Peláez, 2003; Silva, 2003; Lebrão & Duarte, 2008), and the English Longitudinal Study of Ageing (ELSA), which is a longitudinal study with a representative sample of adults aged 50 years or older residing in England. Detailed descriptions of both studies can be found elsewhere (Leeds UK, 2008; Marmot et al., 2011; Steptoe, Breeze, Banks & Nazroo, 2013).
We used data from the third wave of the SABE study (2010) involving 1,344 individuals and the sixth wave of the ELSA (2012) involving 7,107 individuals. All participants were aged 60 years or older. Three hundred SABE participants were excluded due to missing data on mobility, handgrip strength or other covariables, resulting in a final sample of 1,044 individuals. A total of 2,368 individuals were excluded from the ELSA study for the same reasons, resulting in a final sample of 4,739 individuals. Thus, the total analytical sample in the present study comprised of 5,783 individuals.
All participants signed a statement of informed consent. The SABE study received approval from the Human Research Ethics Committee of the School of Public Health of the University of São Paulo. The ELSA study received approval from the National Research Ethics Service – London Multicentre Research Ethics Committee.
2.2. Mobility assessment
In both studies, mobility was assessed using the walk test of the Short Physical Performance Battery Assessing Lower Extremity Function and mobility limitation was defined as a gait speed < 0.8m/s (Cruz-Jentoft et al., 2010; Lauretani et al., 2003; Guralnik, 1997).
2.3. Muscle strength assessment
Handgrip strength was determined using a manual dynamometer (Takei Kiki Kogyio TK 1201 in the SABE study and Smedley in the ELSA study). During the trials, the participant remained seated with the elbow supported on the table and the forearm and hand turned upward. The participant was then instructed to squeeze the dynamometer as strongly as possible. Two trials were performed with the dominant upper limb and a one-minute rest interval between trials. The largest of the two values was considered in the analysis (Al Snih, Markides, Ottenbacher & Raji, 2004; Bohannon & Magasi, 2015).
2.4. Covariables
Sociodemographic, lifestyle and health characteristics associated with mobility limitation were included as covariates.
2.4.1. Sociodemographic characteristics
Age (in years), schooling years (> 13 years; 12–13 years; 0–11 years), marital status (with or without a conjugal life) and income (categorized in highest, intermediate or lowest income) (Alexandre, Scholes, Santos, Duarte & Oliveira, 2018).
2.4.2. Behavioral characteristics
In the SABE study, physical activity level was determined using the Brazilian version of the International Physical Activity Questionnaire (Guedes, Lopes & Guedes, 2005; Von Bonsdorff, Rantanen, Laukkanen, Suutama & Heikkinen, 2006). In the ELSA study, physical activity level was determined using three questions taken from a validated instrument used in the Health Survey for England. We categorized physical activity into two groups: a sedentary lifestyle (no weekly activity) or active lifestyle (light, moderate or vigorous activity at least once a week) (Von Bonsdorff et al., 2006). Regarding smoking status, the individuals were classified as smokers, former smokers or non-smokers. Alcohol intake was classified as never or rarely (up to once a week), often (two to six times a week) or daily in both studies (Alexandre et al., 2018).
2.4.3. Health conditions
The clinical conditions were self-reported doctor-diagnosed arterial hypertension, diabetes, stroke, heart disease, lung disease, joint disease, osteoporosis, cancer and falls in the previous year. Body mass index (BMI) was categorized according to the classification proposed by the World Health Organization as undernourished (< 18.5 kg/m2), ideal range (≥ 18.5 and < 25 kg/m2), overweight (≥ 25 and < 30 kg/m2) or obese (≥ 30 kg/m2) (WHO, 2000). The occurrence of polypharmacy (use of more than five medications) was recorded. Depressive symptoms were evaluated using the Geriatric Depression Scale in the SABE study (≥ 5 points considered risk of depression) and the Center for Epidemiologic Studies Depression Scale in the ELSA study (≥ 4 points considered risk of depression) (Almeida & Almeida, 1999; Yesavage & Sheikh, 1986).
2.4.4. Basic and instrumental activities of daily living
We assessed the number of self-reported difficulties performing basic activities of daily living (ADL) using the modified Katz Index (Katz, Ford, Moskowitz, Jackson & Jaffe, 1963) and difficulties performing instrumental activities of daily living (IADL) using the modified version of the Lawton Scale (Lawton & Brody, 1970).
2.5. Statistical analysis
The characteristics of the sample were expressed as means, standard deviations and proportions. Differences between (1) included participants and excluded participants (due to missing data) as well as (2) sex and mobility status were analyzed using the chi-squared (x2) test, ANOVA and Tukey’s post-hoc test. A p-value < 0.05 was considered indicative of statistical significance.
Sensitivity, specificity, log-likelihood positive (LR+), negative (LR-) and Youden Index values were calculated to determine the accuracy of handgrip strength in identifying mobility limitation. Once the best cutoffs were determined, the probability of exhibiting mobility limitation was calculated using a logistic regression model adjusted for the covariables using the stepwise forward method (p < 0.20) in the univariate analyses. The area under the receiver operating characteristic (ROC) curves of the adjusted models was analyzed and a bootstrap model was created for the confirmation of the results. Other cutoffs in the literature (< 26, < 27, < 30, < 32, < 33, < 37 and < 39 kg for men; < 16, < 17, < 19, < 20, < 21 and < 22 kg for women) were submitted to the same accuracy analyses for the purposes of comparison to the cutoffs proposed in the present study (< 32 kg for men and < 21 kg for women). The Stata 14® statistical package was used for all analyses.
3. Results
Table 1 displays the sociodemographic and behavioral characteristics of the sample stratified by sex and mobility status. Table 2 displays the health conditions, anthropometric, ADL and IADL data. Mobility limitation was more prevalent among women (37.3%) than men (28.9%). In both sexes, individuals with mobility limitation were older, had no conjugal life, were in the intermediate income and had less schooling. They also never or rarely consumed alcohol and had more health problems, lower mean handgrip strength, a higher mean BMI and greater number of difficulties performing basic and instrumental activities of daily living (p < 0.05).
Table 1.
Sociodemographic and behavioral characteristics of 5,783 older adults from the SABE and ELSA studies stratified by sex and mobility status
| Men (n = 2,510) 43.4% | Women (n = 3,273) 56.6% | |||
|---|---|---|---|---|
| Characteristics | Normal mobility (n = 1,785) 71.1% | Mobility limitation (n = 725) 28.9% | Normal mobility (n = 2,052) 62.7% | Mobility limitation (n = 1,221) 37.3% |
| Sociodemographic characteristics | ||||
| Age, years, mean (SD) | 68.8 (6.5)* § | 74.2 (8.4)* § | 68.2 (6.2)* § | 73.9 (8.1)* § |
| 60 – 69 (%) | 60.1* § | 33.1* | 63.6* § | 33.0* |
| 70 – 79 (%) | 32.3* § | 40.0* | 31.0* § | 40.6* |
| 80 or more (%) | 7.6* § | 26.9* | 5.4* § | 26.4* |
| Marital status (with conjugal life), (%) | 81.5* § | 69.0* § | 62.6* § | 44.5* § |
| Income, (%) | ||||
| Highest income, (%) | 54.5* § | 27.6* § | 47.0* § | 22.4* § |
| Intermediate income, (%) | 36.2* § | 48.8* § | 38.2* § | 48.4* § |
| Lowest income, (%) | 7.1* § | 21.8* § | 11.1* § | 24.4* § |
| Income not declared, (%) | 2.2* § | 1.8* § | 3.7* § | 4.8* § |
| Schooling (years), (%) | ||||
| > 13 years of schooling, (%) | 42.7* § | 19.7* § | 25.4* § | 13.2* § |
| 12 – 13 years of schooling, (%) | 21.7* § | 17.9* § | 26.9* § | 17.2* § |
| 0 – 11 years of schooling, (%) | 35.6* § | 62.4* § | 47.7* § | 69.6* § |
| Behavioral characteristics | ||||
| Level of physical activity (active), (%) | 91.3* | 74.5* § | 92.7* | 78.6* § |
| Weekly alcohol intake, (%) | ||||
| Never or rarely | 17.4* § | 37.9* | 31.7* § | 59.1* |
| Often | 35.3* § | 33.5* | 40.7* § | 26.9* |
| Daily | 47.3* § | 28.6* | 27.6* § | 14.0* |
| Smoking, (%) | ||||
| Non-smoker | 30.7* § | 21.8* § | 47.8 § | 47.0 § |
| Former smoker | 60.6* § | 66.2* § | 43.6 § | 42.4 § |
| Smoker | 8.7* § | 12.0* § | 8.6 § | 10.6 § |
Note: Data expressed as proportion, mean, and standard deviation.
Difference per mobility status in same sex (p < 0.05).
Difference between sexes within same mobility status (p < 0.05)
Table 2 –
Health conditions, anthropometric data, and functioning characteristics of 5,783 older adults from the SABE and ELSA studies stratified by sex and mobility status.
| Men | Women | |||
|---|---|---|---|---|
| Characteristics | Normal mobility (n = 1,785) 71.1% | Mobility limitation (n = 725) 28.9% | Normal mobility (n = 2,052) 62.7% | Mobility limitation (n = 1,221) 37.3% |
| Health conditions | ||||
| Stroke (yes), (%) | 2.9* | 9.8* § | 2.3* | 7.0* § |
| Cancer (yes), (%) | 5.9* | 10.2* § | 4.8* | 6.5* § |
| Heart disease (yes), (%) | 18.3* § | 32.6* § | 14.0* § | 27.1* § |
| Diabetes (yes), (%) | 12.0* § | 21.7* | 8.7* § | 19.3* |
| Joint disease (yes), (%) | 27.8* § | 43.2* § | 41.1* § | 58.6* § |
| Arterial hypertension (yes), (%) | 41.1* | 57.5* | 39.4* | 60.3* |
| Osteoporosis (yes), (%) | 1.7* § | 5.7* § | 13.0* § | 24.1* § |
| Lung disease (yes), (%) | 11.0* | 17.2* | 12.4* | 16.8* |
| Polypharmacy (yes), (%) | 24.4* | 51.9* | 23.3* | 51.8* |
| Fall in previous 12 months (yes), (%) | 20.8* § | 31.5* | 25.7* § | 35.4* |
| Depressive symptoms (yes), (%) | 5.2* § | 13.8* § | 10.8* § | 23.6* § |
| Anthropometric characteristics | ||||
| Handgrip strength (kg), mean (SD) | 39.0 (8.5)* § | 31.9 (9.1)* § | 23.9 (5.6)* § | 19.5 (6.2)* § |
| Body mass index (kg/m²), mean (SD) | 27.8 (4.1)* | 28.5 (4.6)* | 27.7 (5.1)* | 29.5 (6.1)* |
| Normal weight (%) | 24.0* § | 21.4* § | 31.2* § | 22.4* § |
| Undernourished (%) | 0.4* § | 0.7* § | 1.0* § | 1.6* § |
| Overweight (%) | 51.7* § | 45.9* § | 39.5* § | 33.2* § |
| Obese (%) | 23.9* § | 32.0* § | 28.3* § | 42.8* § |
| ADL and IADL | ||||
| ADL (number of affected activities), mean (SD) | 0.1 (0.4)* | 0.5 (1.0)* § | 0.1 (0.4)* | 0.6 (1.2)* § |
| IADL (number of affected activities), mean (SD) | 0.0 (0.3)* | 0.3 (0.8)* § | 0.0 (0.2)* | 0.4 (0.8)* § |
Note: Data expressed as proportion, mean, and standard deviation. ADL – basic activities of daily living; IADL – instrumental activities of daily living;
Difference per mobility status in same sex (p < 0.05).
Difference between sexes within same mobility status (p < 0.05).
The participants excluded due to missing data were younger, had a conjugal life, fewer schooling years and were in the intermediate income. Most were former smokers, consumed alcohol frequently, were overweight and had fewer health problems. These individuals had greater mean handgrip strength, were slower, reported more difficulties to perform activities of daily living, fell less often and had fewer depressive symptoms than the individuals included in the sample (p < 0.05).
The balance between the sensitivity, specificity, LR+, LR- and Youden Index values indicated that the best cutoffs were < 32 kg for men (49.1% sensitivity, 79.8% specificity, LR+ of 2.43, LR- of 0.64 and Youden Index of 28.9) and < 21 kg for women (58.6% sensitivity, 72.9% specificity, LR+ of 2.16, LR- of 0.57 and Youden Index of 31.5).
Table 3 shows the diagnostic accuracy properties of the cutoffs proposed herein as well as those described in the literature and applied to the present sample. Odds ratios (OR) and their respective 95% confidence intervals (CI) were calculated to estimate the odds of a mobility limitation among men and women based on the cutoffs determined in the present study and those reported in the literature. The results of the logistic regression model adjusted for the covariates are presented in Table 4 and were confirmed by the bootstrap model. Finally, ROC curves were plotted from the adjusted model as well as the graphs of the relation between sensitivity and specificity and the probability of the cutoffs proposed in the present investigation i.e. < 32 kg for men and < 21 kg for women (Figure 1).
Table 3.
Diagnostic properties of handgrip strength cutoffs to identify mobility limitation (SABE and ELSA Studies)
| Cutoffs | Sensitivity | Specificity | LR+ | LR- | Youden | Correct Classification |
|---|---|---|---|---|---|---|
| Men | ||||||
| < 26 kg | 26.8 | 94.4 | 4.82 | 0.77 | 21.2 | 74.9 |
| < 27 kg | 29.5 | 92.9 | 4.15 | 0.76 | 22.4 | 74.6 |
| < 28 kg | 33.4 | 91.3 | 3.84 | 0.73 | 24.7 | 74.6 |
| < 29 kg | 36.4 | 89.3 | 3.40 | 0.71 | 25.7 | 74.0 |
| < 30 kg | 40.4 | 87.1 | 3.12 | 0.68 | 27.5 | 73.6 |
| < 31 kg | 44.1 | 82.5 | 2.52 | 0.68 | 26.6 | 71.4 |
| < 32 kg | 49.1 | 79.8 | 2.43 | 0.64 | 28.9 | 71.0 |
| < 33 kg | 53.2 | 76.5 | 2.26 | 0.61 | 29.7 | 69.8 |
| < 37 kg | 69.4 | 60.7 | 1.76 | 0.50 | 30.1 | 63.2 |
| < 39 kg | 76.3 | 51.9 | 1.58 | 0.46 | 28.2 | 58.9 |
| Women | ||||||
| < 16 kg | 28.6 | 93.4 | 4.34 | 0.76 | 22.0 | 69.2 |
| < 17 kg | 33.6 | 90.9 | 3.68 | 0.73 | 24.5 | 69.5 |
| < 18 kg | 38.1 | 88.3 | 3.24 | 0.70 | 26.4 | 69.5 |
| < 19 kg | 45.3 | 84.1 | 2.85 | 0.65 | 29.4 | 69.6 |
| < 20 kg | 50.2 | 80.8 | 2.61 | 0.62 | 31.0 | 68.3 |
| < 21 kg | 58.6 | 72.9 | 2.16 | 0.57 | 31.5 | 67.5 |
| < 22 kg | 63.9 | 67.3 | 1.95 | 0.54 | 31.2 | 66.0 |
Note: LR+: positive Log-likelihood; LR-: negative Log-likelihood.
Table 4.
Final model for likelihood of mobility limitation among older men and women according to different cutoffs (SABE and ELSA Studies)
| Cutoffs | OR | 95%CI | |
|---|---|---|---|
| Men | < 26 kg | 3.18 | [2.32 – 4.35] |
| < 27 kg | 2.71 | [2.02 – 3.63] | |
| < 28 kg | 2.62 | [1.99 – 3.46] | |
| < 29 kg | 2.35 | [1.80 – 3.06] | |
| < 30 kg | 2.27 | [1.76 – 2.92] | |
| < 31 kg | 1.80 | [1.42 – 2.29] | |
| < 32 kg | 1.88 | [1.50 – 2.37] | |
| < 33 kg | 1.85 | [1.47 – 2.32] | |
| < 37 kg | 1.80 | [1.44 – 2.26] | |
| < 39 kg | 1.71 | [1.36 – 2.17] | |
| Women | < 16 kg | 2.51 | [1.94 – 3.25] |
| < 17 kg | 2.24 | [1.78 – 2.83] | |
| < 18 kg | 2.11 | [1.70 – 2.62] | |
| < 19 kg | 2.07 | [1.69 – 2.53] | |
| < 20 kg | 2.02 | [1.67 – 2.45] | |
| < 21 kg | 1.89 | [1.57 – 2.27] | |
| < 22 kg | 1.78 | [1.49 – 2.13] | |
Note: OR: odds ratio; CI: confidence interval.
Figure 1.
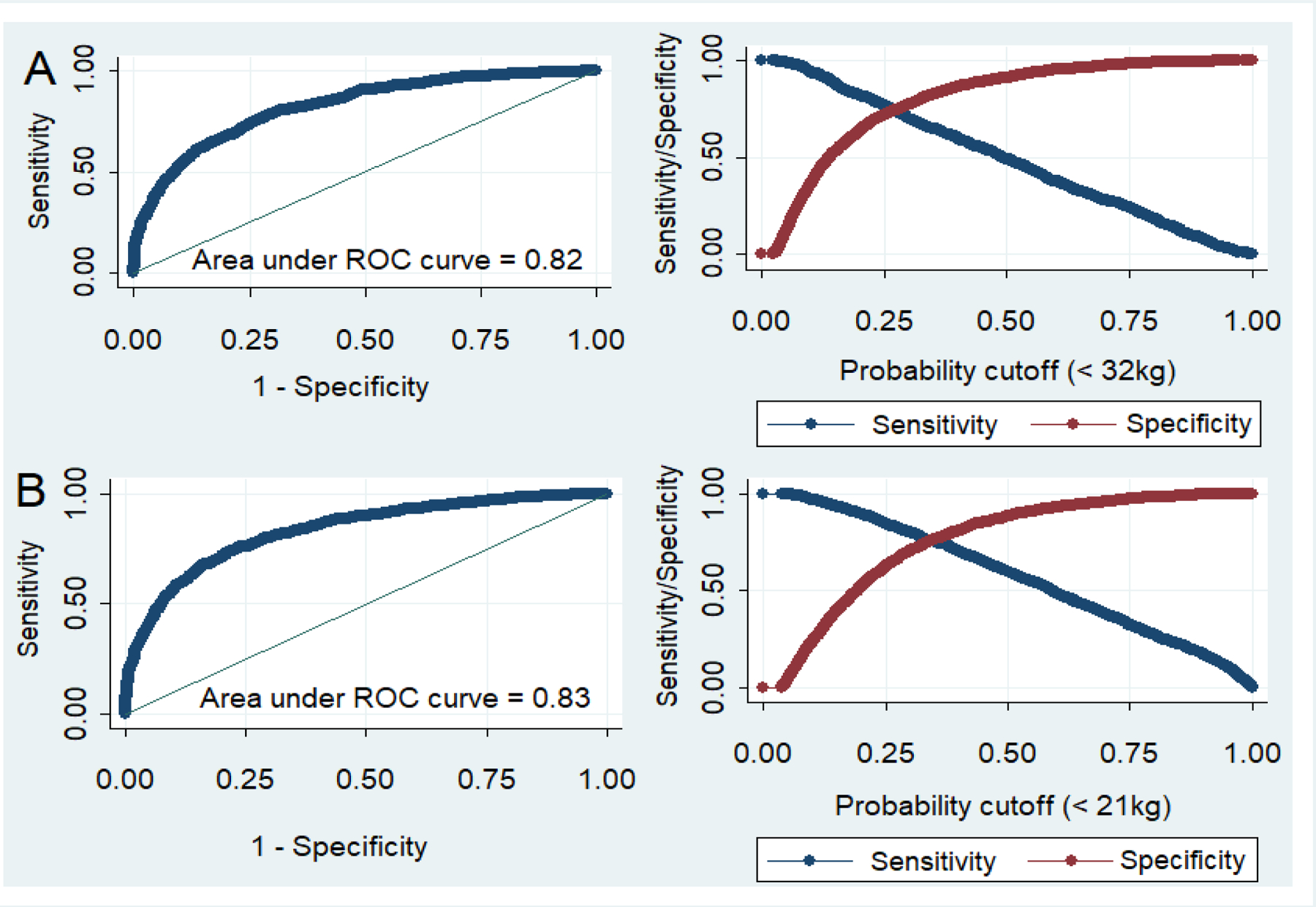
ROC curve of adjusted model for cut-offs of < 32kg for men and < 21kg for women, relation between sensitivity and specificity, and probability of grip strength to identify of mobility limitation among older men (A) and women (B).
4. Discussion
The present findings suggest that a handgrip strength < 32 kg for men and < 21 kg for women are indicators of a greater probability of a mobility limitation among older adults. The cutoff of < 32 kg for men had 49.1% sensitivity, 79.8% specificity, LR+ of 2.43, LR- of 0.64 and Youden Index of 28.9, whereas the cutoff of < 21 kg for women had 58.6% sensitivity, 72.9% specificity, LR+ of 2.16, LR- of 0.57 and a Youden Index of 31.5. In the fully adjusted model using these cutoff points, the area under the curve (AUC) was 0.82 for men and 0.83 for women, with an OR of 1.88 [95% CI: 1.50 – 2.37] and 1.89 [95%CI: 1.57 – 2.27] respectively.
The cutoff point of handgrip strength to identify mobility limitation found in the present study for men was similar to that reported by Dong et al. (2016), who analyzed 1,049 Chinese individuals 60 years of age or older (469 men) and defined mobility limitation as the slowest 20% on the four-meter walk test and/or the Timed Up and Go Test. The authors found 74.6% sensitivity, 62.7% specificity and an AUC of 0.63 for the cutoff < 32.45 kg. In the present study, despite the lower sensitivity, the cutoff < 32 kg was more specific and had a higher LR+, indicating a greater likelihood of the occurrence of mobility limitation when handgrip strength is lower than the established cutoff (McGee, 2016), as well as a higher AUC. The higher sensitivity in the study by Dong et al. (2016) may be the result of the different cutoff point adopted to define mobility limitation as well as the exclusion of individuals with stroke and cancer. In the present study these individuals were included in our analyses. Furthermore, the lower cutoff reported by Dong et al. (2016) for women (< 18.95 kg) compared to the present study (< 21 kg) may be explained by the fact that our sample was older (70.4 vs. 66.3 years) and had a greater mean strength (22.3 kg vs. 20.47 kg).
The handgrip strength cutoff to identify mobility limitation found for women in the present study was similar to that described by Sallinen et al. (2010), who analyzed 3,392 Finnish individuals 55 years of age or older (1562 women) and defined mobility limitation based on self-reported difficulty walking 500 m and/or going up and down stairs. The authors found 67% sensitivity, 73% specificity and an AUC of 0.75 for the cutoff < 21 kg. In our analysis, although this cutoff point had lower sensitivity with similar specificity, it obtained the best performance test value among the cutoffs analyzed (Youden index = 31.5) (Youden, 1950). The greater sensitivity found by Sallinen et al. (2010) for women may be the result of mobility limitation being self-reported, as mean handgrip strength values were similar (23 kg vs. 22.3 kg) despite the difference in age. The cutoff point of < 37 kg for men, which is higher than that found in the present study, may be due to a sample with a younger mean age and greater mean handgrip strength (41 kg vs. 36.9 kg).
Although the cutoff points of < 30 kg for men and < 20 kg for women described by Lauretani et al. (2003) are very close to those that we considered to be the most adequate for the identification of mobility limitation, the authors did not present sensitivity, specificity or other important components of the accuracy analysis, which impedes a more precise comparison of the results. Moreover, according to our analyses, a cutoff point of < 30 kg for men implies an 8.7% loss of sensitivity at the expense of 7.3% specificity and a reduction of the Youden index by 1.2%. Likewise, a cutoff of < 20 kg for women implies an 8.6% loss of sensitivity at the expense of 8.1% specificity and a reduction of the Youden index by 0.5%.
Alley et al. (2014) analyzed data from multiple studies linked to the Foundation for the National Institutes of Health Biomarkers Consortium Sarcopenia Project involving a sample of 9,897 men and 10,950 women, dividing handgrip strength data into categories (normal, intermediate and weak) and cross-referencing with data obtained for walking speed. The authors found that handgrip strength < 26 kg for men (23.4% sensitivity and 96.6% specificity) and < 16 kg for women (30.6% sensitivity and 87.5% specificity) best indicated a greater probability of clinically important impaired muscle strength related to mobility limitation (< 0.8 m/s). Moreover, handgrip strength < 32 kg for men (47.8% sensitivity and 87.2% specificity) and < 20 kg for women (61.8% sensitivity and 65.2% specificity) were the best indicators of intermediate weakness related to mobility limitation (Alley et al., 2014). When applied to the present sample, cutoffs of < 26 kg and < 16 kg had similar sensitivity and specificity to the values described by Alley et al. (2014), but with the lowest Youden index values for mobility limitation among all cutoffs analyzed. However, < 32 kg for men was also what we identified as the best cutoff for identifying mobility decline, whereas < 20 kg for women has implications when compared to < 21 kg, as discussed above.
Duchowny, Peterson and Clarke (2017) also sought to identify cutoff points of handgrip strength for the identification of mobility limitation (0.8 m/s) using data from 7,688 non-institutionalized Americans (3,182 men and 4,506 women) aged 65 years or older. The authors obtained a cutoff point of < 39 kg for men (75.16% and 69.34% sensitivity and 54.25% and 64.89% specificity for white and black men, respectively) and < 22 kg for women (60.48% and 90.48% sensitivity and 67.58% and 29.21% specificity for white and black women, respectively). When applied to the present sample, < 39 kg for men had high sensitivity (76.3%) but lower specificity (51.9%) and a 0.7% drop in the Youden index as well as 12.2% fewer correct classifications of cases compared to < 32 kg. For women, < 22 kg led to a 5.3% gain in sensitivity but losses of 5.6% in specificity, 0.3% on the Youden index and 1.5% in the correct classification of cases compared to < 21 kg.
Vasconcelos et al. (2015) analyzed the accuracy of handgrip strength for mobility limitation based on data from 1,374 older Brazilian adults who participated in the FIBRA study. The authors calculated sensitivity, specificity, positive predictive values and negative predictive values, proposing cutoffs of < 25.8 kg for men and < 17.4 kg for women. However, when applied to the present sample, the results were unsatisfactory and similar to those found when using the cutoffs proposed by Alley et al. (2014).
In 2018, the EWGSOP recommended low muscle strength as a fundamental characteristic for the diagnosis of sarcopenia and a poor physical performance as an indicator of the severity of this condition. The group suggests that low muscle strength is considered when handgrip strength is < 27 kg for men and < 16 kg for women. For mobility limitation, the group suggests that a poor physical performance is considered when walking speed is < 0.8m/s. However, neither the handgrip strength cutoff of < 16 kg for women, previously proposed by Alley et al. (2014), nor < 27 kg for men presented good accuracy when applied to the present sample (Cruz-Jentoft et al., 2010; Cruz-Jentoft et al.,2019).
The cutoffs for handgrip strength described in the literature and those proposed in the present study did not show high sensitivity. However, mobility is a complex phenomenon for which neuromuscular strength is not the only component. Thus, it is not possible to demand better results for diagnostic properties, as other variables exert an influence on this process. Hence, we believe that our sensitivity values, although not particularly high, are very satisfactory (César, Mambrini, Ferreira & Lima-Costa, 2015; Silva, Pedraza & Menezes, 2015).
The same may be true for the Youden Index, which did not indicate a good performance of handgrip strength as an explanator of mobility limitation in the present study. The values of this index range from 0 to 1, for which 0 indicates the same proportion of positive results for groups with and without a disease (useless test) and 1 indicates the absence of false positive and false negatives (perfect test) (Youden, 1950). Nevertheless, the Youden Index presented in our study is better than that obtained in the others performed so far.
On the other hand, even though our cutoffs did not show a good sensitivity, the specificity was satisfactory. Good specificity guarantees the test with a rare erroneous classification (false positives) (McGee, 2016). In this sense, the cutoffs presented by our study, compared to those proposed in the literature, would not classify older adults with preserved mobility as individuals with mobility limitations.
The results of the AUC analysis confirm the accuracy of our cutoffs. The fully adjusted model showed an AUC of 0.82 for men and 0.83 for women. An AUC ≥ 0.9 indicates high precision, 0.7 to 0.9 indicates moderate precision and 0.5 to 0.7 indicates low precision. Thus, a test can be considered adequate when the AUC is ≥ 0.75 (Barbosa-Silva, Menezes, Bielemann, Malmstrom & Gonzalez, 2016).
Moreover, working with higher cutoffs seems more advantageous, as they enable an early diagnosis, development of interventions that can preserve functional capacity, ensure social interactions and contribute to reducing health care costs. All these factors lend support to the present findings.
The strengths and limitations of our study should be acknowledged. The following are the main strong points: the use of data from large and representative samples; the use of mobility limitation probability models adjusted for important variables associated with the outcome which allowed the size of the associations of the cutoffs tested to be analyzed independently of confounding variables; and the comparison of our cutoffs to those described in previous studies, thereby enabling the choice of the best values. One potential limitation of the study was the use of a dynamometer and procedures other than those recommended by the Southampton Group (Roberts et al., 2011). Moreover, the exclusion of individuals for whom no data was available on handgrip strength, walking speed or other covariables could have biased the results to some degree.
5. Conclusion
A handgrip strength < 32 kg for men and < 21 kg for women showed the best probability to identify mobility limitation among older adults in Brazil and England, after comparing their accuracy properties to the cutoffs described in the literature.
Highlights.
Handgrip < 32kg was the best cutoff point to identify mobility limitation in men.
Handgrip < 21kg was the best cutoff point to identify mobility limitation in women.
Handgrip < 32kg for men has 49.1% sensitivity, 79.8% specificity and AUC of 0.82.
Handgrip < 21kg for women has 58.6% sensitivity, 72.9% specificity and AUC of 0.83.
Acknowledgments
The authors are grateful to all the staff who worked on the SABE and ELSA studies and all participants in the two studies.
Funding
The SABE study is funded by the Foundation for Research Support of the State of São Paulo (FAPESP), grant number 2009/53778-3. ELSA is funded by the National Institute on Aging USA (grant number 5R01AG017644-16) and a consortium of United Kingdom government departments coordinated by the Economic and Social Research Council (ESRC). The Brazilian National Council for Scientific and Technological Development (CNPq) (grant number 303981/2017-2) and FAPESP (grant number 18/13917-3) finances Tiago da Silva Alexandre. This study was financed in part by the CNPq through the Institutional Program of Scientific Initiation Scholarships - PIBIC (grant number 113586/2018-3).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Al Snih S, Markides KS, Ottenbacher KJ, & Raji MA (2004). Hand grip strength and incident ADL disability in elderly Mexican Americans over a seven-year period. Aging Clinical and Experimental Research, 16(6), 481–486. 10.1007/BF03327406 [DOI] [PubMed] [Google Scholar]
- Alley DE, Shardell MD, Peters KW, McLean RR, Dam TTL, Kenny AM, … & Ferrucci L (2014). Grip strength cutpoints for the identification of clinically relevant weakness. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 69(5), 559–566. 10.1093/gerona/glu011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida OP, & Almeida SA (1999). Short versions of the geriatric depression scale: a study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. International Journal of Geriatric Psychiatry, 14(10), 858–865. [DOI] [PubMed] [Google Scholar]
- Barbosa-Silva TG, Menezes AMB, Bielemann RM, Malmstrom TK, & Gonzalez MC (2016). Enhancing SARC-F: improving sarcopenia screening in the clinical practice. Journal of the American Medical Directors Association, 17(12), 1136–1141. 10.1016/j.jamda.2016.08.004 [DOI] [PubMed] [Google Scholar]
- Bohannon RW, & Magasi S (2015). Identification of dynapenia in older adults through the use of grip strength t-scores. Muscle & Nerve, 51(1), 102–105. 10.1002/mus.24264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawthon PM, Travison TG, Manini TM, Patel S, Pencina KM, Fielding RA, … & Cummings SR (2020). Establishing the link between lean mass and grip strength cut points with mobility disability and other health outcomes: proceedings of the sarcopenia definition and outcomes consortium conference. The Journals of Gerontology: Series A, 75(7), 1317–1323. 10.1093/gerona/glz081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- César CC, Mambrini JVDM, Ferreira FR, & Lima-Costa MF (2015). Capacidade funcional de idosos: análise das questões de mobilidade, atividades básicas e instrumentais da vida diária via Teoria de Resposta ao Item. Cadernos de Saúde Pública, 31, 931–945. 10.1590/0102-311X00093214 [DOI] [PubMed] [Google Scholar]
- Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, … & Topinková E (2010). Sarcopenia: European consensus on definition and diagnosis Report of the European Working Group on Sarcopenia in Older. Age and Ageing, 39(4), 412–423. 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, … & Schneider SM (2019). Sarcopenia: revised European consensus on definition and diagnosis. Age and Ageing, 48(1), 16–31. 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva Alexandre T, de Oliveira Duarte YA, Santos JF, Wong R, & Lebrão ML (2014). Prevalence and associated factors of sarcopenia among elderly in Brazil: findings from the SABE study. The Journal of Nutrition, Health & Aging, 18(3), 284–290. 10.1007/s12603-013-0413-0 [DOI] [PubMed] [Google Scholar]
- da Silva Alexandre T, Scholes S, Santos JLF, de Oliveira Duarte YA, & de Oliveira C (2018). The combination of dynapenia and abdominal obesity as a risk factor for worse trajectories of IADL disability among older adults. Clinical Nutrition, 37(6), 2045–2053. 10.1016/j.clnu.2017.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Souza Vasconcelos KS, Dias JD, de Carvalho Bastone A, Vieira RA, de Souza Andrade AC, Perracini MR, … & Dias RC (2016). Handgrip strength cutoff points to identify mobility limitation in community-dwelling older people and associated factors. The Journal of Nutriti>on, Health & Aging, 20(3), 306–315. 10.1007/s12603-015-0584-y [DOI] [PubMed] [Google Scholar]
- Dodds RM, Syddall HE, Cooper R, Benzeval M, Deary IJ, Dennison EM, … & Kirkwood TB (2014). Grip strength across the life course: normative data from twelve British studies. PloS One, 9(12), e113637. 10.1371/journal.pone.0113637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong R, Wang X, Guo Q, Wang J, Zhang W, Shen S, … & Fu L (2016). Clinical relevance of different handgrip strength indexes and mobility limitation in the elderly adults. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 71(1), 96–102. 10.1093/gerona/glv168 [DOI] [PubMed] [Google Scholar]
- Duchowny KA, Peterson MD, & Clarke PJ (2017). Cut points for clinical muscle weakness among older Americans. American Journal of Preventive Medicine, 53(1), 63–69. 10.1016/j.amepre.2016.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guedes DP, Lopes CC, & Guedes JERP (2005). Reprodutibilidade e validade do Questionário Internacional de Atividade Física em adolescentes. Revista Brasileira De Medicina do Esporte, 11(2), 151–158. 10.1590/S1517-8692200500020001 [DOI] [Google Scholar]
- Guralnik JM (1997). Assessment of physical performance and disability in older persons. Muscle & Nerve, S14–S16. [PubMed]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, & Jaffe MW (1963). Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. The Journal of the American Medical Association, 185(12), 914–919. 10.1001/jama.1963.0306012002401 [DOI] [PubMed] [Google Scholar]
- Kim TN, & Choi KM (2013). Sarcopenia: definition, epidemiology, and pathophysiology. Journal of Bone Metabolism, 20(1), 1–10. 10.11005/jbm.2013.20.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, … & Ferrucci L (2003). Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. Journal of Applied Physiology, 95(5), 1851–1860. 10.1152/japplphysiol.00246.2003 [DOI] [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1970). Assessment of older people: self-maintaining and instrumental activities of daily living. Nursing Research, 19(3), 278. [PubMed] [Google Scholar]
- Lebrão ML, & de Oliveira Duarte YA (2008). Desafios de um estudo longitudinal: o Projeto SABE. Saúde Coletiva, 5(24), 166–167. [Google Scholar]
- [dataset] Leeds UK (2008). Joint Health Surveys Unit, National Centre for Social Research and University College London Research Department of Epidemiology and Public Health. The Health Survey for England 2008. [Google Scholar]
- Manini TM (2013). Mobility decline in old age: a time to intervene. Exercise and Sport Sciences Reviews, 41(1), 2. 10.1097/JES.0b013e318279fdc5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [dataset] Marmot M, Nazroo J, Banks J, Blundell R, Erens B, Lessof C, & Huppert FA (2011). English Longitudinal Study of Ageing: Wave 0 (1998, 1999 and 2001) and Waves 1–4 (2002–2009) [computer file]. Colchester, Essex: UK Data Archive [distributor]. [Google Scholar]
- McGee S (2016). Evidence-based physical diagnosis e-book. Elsevier Health Sciences. [Google Scholar]
- McLean RR, Shardell MD, Alley DE, Cawthon PM, Fragala MS, Harris TB, … & Kritchevsky SB (2014). Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the foundation for the National Institutes of Health (FNIH) sarcopenia project. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 69(5), 576–583. 10.1093/gerona/glu012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palloni A, & Peláez M (2003). Histórico e natureza do estudo. In: Lebrão ML (Org.); Duarte YAO (Org.) SABE – Saúde, Bem-estar e Envelhecimento – O projeto SABE no Município de São Paulo: uma abordagem inicial. Brasília: Distrito Federal, cap.1, p. 15. [Google Scholar]
- Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, & Sayer AA (2011). A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age and Ageing, 40(4), 423–429. 10.1093/ageing/afr051 [DOI] [PubMed] [Google Scholar]
- Sallinen J, Stenholm S, Rantanen T, Heliövaara M, Sainio P, & Koskinen S (2010). Handgrip strength cut points to screen older persons at risk for mobility limitation. Journal of the American Geriatrics Society, 58(9), 1721–1726. 10.1111/j.15325415.2010.03035.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva NDA, Pedraza DF, & Menezes TND (2015). Desempenho funcional e sua associação com variáveis antropométricas e de composição corporal em idosos. Ciência & Saúde Coletiva, 20, 3723–3732. 10.1590/1413-812320152012.01822015 [DOI] [PubMed] [Google Scholar]
- Silva NN (2003). Aspectos Metodológicos: Processo de amostragem. In: Lebrão ML (Org.); Duarte YAO (Org.). SABE– Saúde, Bem-estar e Envelhecimento – O projeto SABE no Município de São Paulo: uma abordagem inicial. Brasília: Distrito Federal, cap. 3, p. 47. [Google Scholar]
- Steptoe A, Breeze E, Banks J, & Nazroo J (2013). Cohort profile: The English longitudinal study of ageing. International Journal of Epidemiology, 42(6), 1640–1648. 10.1093/ije/dys168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, … & Kiel DP (2014). The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 69(5), 547–558. 10.1093/gerona/glu010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Bonsdorff M, Rantanen T, Laukkanen P, Suutama T, & Heikkinen E (2006). Mobility limitations and cognitive deficits as predictors of institutionalization among community-dwelling older people. Gerontology, 52(6), 359–365. 10.1159/000094985 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2000). Obesity: preventing and managing the global epidemic. 10 Report of a WHO Consultation. WHO: Geneva. 10.1017/s0021932003245508 [DOI] [PubMed] [Google Scholar]
- Yesavage JA, & Sheikh JI (1986). 9/Geriatric depression scale (GDS) recent evidence and development of a shorter version. Clinical Gerontologist, 5(1–2), 165–173. 10.1300/J018v05n01_09 [DOI] [Google Scholar]
- Youden WJ (1950). Index for rating diagnostic tests. Cancer, 3(1), 32–35. [DOI] [PubMed] [Google Scholar]


