INTRODUCTION
The annual colorectal cancer (CRC) incidence and mortality rate has been increasing in the past three decades for young adults, defined as patients under 50 years of age(1–3). The American Cancer Society (3) and United States Preventive Service Task Force (4) have made qualified recommendations to initiate screening at age 45 years based on modeling analyses. We hypothesized that if CRC prevalence is increasing before age 50, there may be a concomitant increase in cancer precursor lesions before and after age 50. We have analyzed colonoscopy data from 2002 to 2014 to determine the rates of finding polyp(s) > 9 mm (P9mm) which we used as a surrogate for traditional advanced adenomas. The aim of this study is to determine the trend of P9mm prevalence over this time period.
METHODS
The Clinical Outcomes Research Initiative (CORI) is a consortium of gastrointestinal practices which use a structured computerized endoscopic report (5). We identified the first colonoscopy performed for all patients aged 40 to 59 years of age in the Clinical Outcomes Research Initiative database from 2002 to 2014. Patients were included if the indication for colonoscopy was diagnostic evaluation, average risk, polyp or CRC surveillance, or family history of CRC. If patients had more than one exam during the 2002–2014 period, only the first exam was used in this analysis. Diagnostic evaluation includes all patient symptoms such as melena, hematochezia, abdominal pain, diarrhea, constipation, weight loss, and anemia. All other indications for colonoscopy such as hereditary gastrointestinal cancer syndromes and inflammatory bowel disease were excluded from our study. The primary end-point was the detection of P9mm, which is a robust surrogate for advanced neoplasia with low rates of misclassification (5). Descriptive statistics were used to report patient characteristics and prevalence of P9mm. Pearson’s chi-square test was used to test for differences between proportions of categorical variables. Cochran-Armitage test was used to test the trend of proportions over time. All analysis was performed using SAS software 9.4 (SAS Institute, Inc, Cary, NC).
RESULTS
Our study included 87,745 patients (22%) aged 40 to 49 years and 310,905 patients (78%) aged 50 to 59 years of age with complete colonoscopy and adequate bowel prep. As expected, patients under 50 years of age have higher rates of family history and diagnostic examinations while patients over 50 years of age have higher rates of polyp surveillance and average-risk screening.
Annual prevalences of P9mm over time are shown for each age group in Figure 1. From 2002 to 2005, P9mm prevalence declined. In 2002, most colonoscopies were diagnostic (57%) and average-risk screening accounted for only 17%. By 2005, screening colonoscopy was established and accounted for more than 50% of colonoscopies. Since asymptomatic patients have lower P9mm prevalence than symptomatic patients, we believe that this shift in colonoscopy utilization to screening may explain the initial decline in P9mm before 2005, after which the utilization of colonoscopy was stable.
Figure 1:
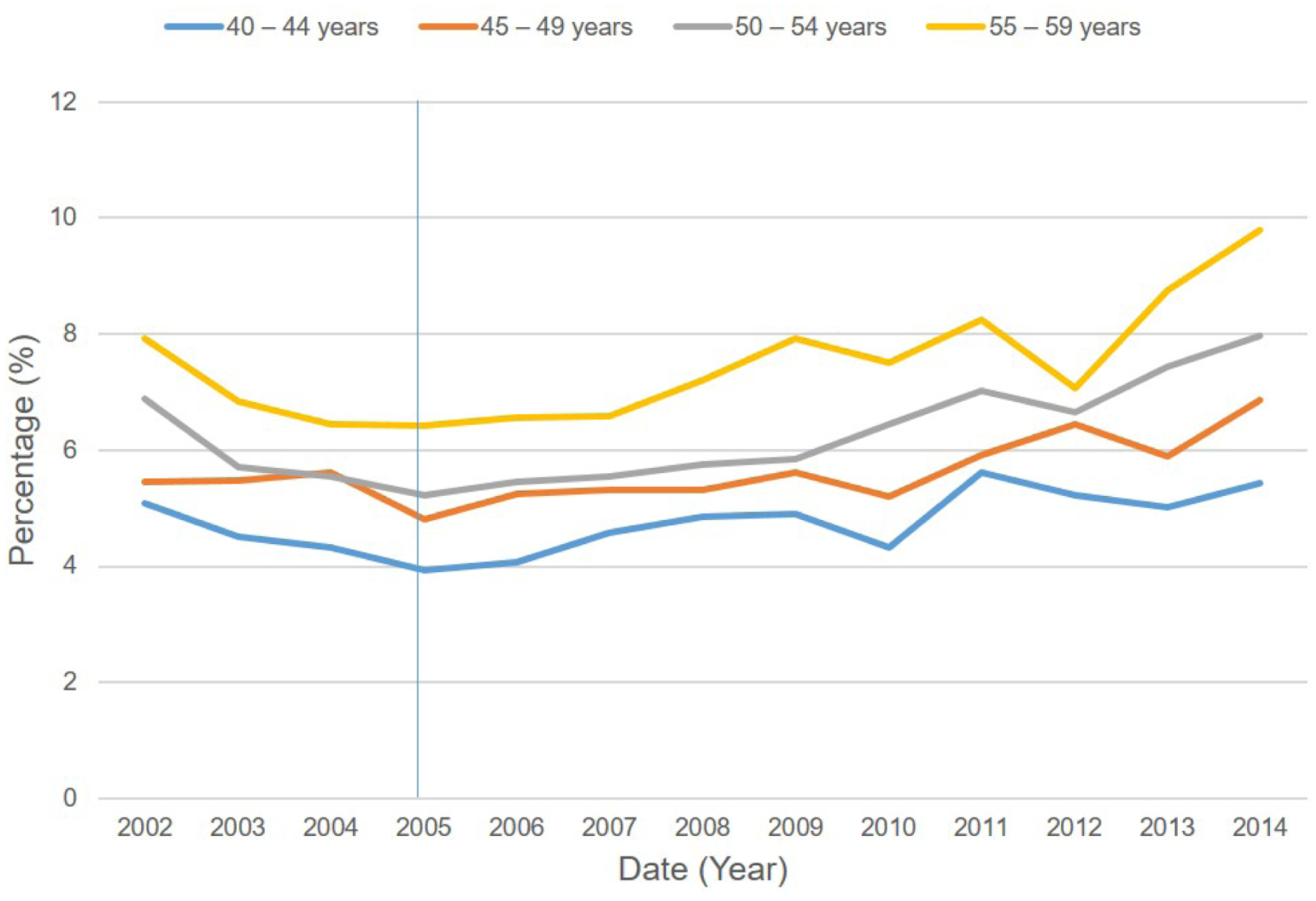
Total Rates of Polyps greater than 9mm by Age over time
There was a steady increase in P9mm prevalence in each age groups after 2005 of 39 to 54%. The prevalence of P9mm was stratified by age group, sex and procedure indication in 2005 versus 2014 (Table 1 supplement). For individuals, age 50 to 54 years and 55 to 59 years, P9mm prevalence increased significantly in each procedure indication category from 2005 to 2014. For individuals less than 50, we observed an increased prevalence of P9mm for diagnostic procedures from 2005 to 2014 in both men and women. During the entire study period, men age 40 to 49 years have similar prevalence of P9mm compared to women 10 years older. For example, in 2014 the prevalence of P9mm in men age 40 to 44 (6.32%) and women age 50–54 (6.01%) and in men age 45 to 49 (8.34) and women age 55–59 (8.31%) was not statistically different.
Procedure indications:
Screen: Screening exam as primary indication
FHX: Family history of CRC as primary indication
Surv: Surveillance after prior neoplasia as primary indication
Diag: Diagnostic exam for evaluation of symptoms.
DISCUSSION
From 2005 to 2014, we observed an increased prevalence of P9mm in men and women age 40 to 59 years receiving colonoscopy (Figure 1). This increase was observed for each procedure indication for men and women age 50 to 59 (Table 1 Supplement). The 54% rise in P9mm prevalence for the 50 to 54 year age group parallels a rise in CRC of 17% from 1999 to 2017 (7). The temporal increase in P9mm prevalence in 45 to 49 year old men and women undergoing predominantly diagnostic procedures, occurred in the distal but not proximal colon. Studies have shown that the greatest rise of CRC in patients under 50 years is in the distal colon (8). Among all patients undergoing diagnostic colonoscopy, men age 40 to 49 have a similar prevalence of P9mm compared to women 10 years older (aged 50–59 years).
These results suggest that along with temporal increase in incidence of early-onset CRC, cancer precursor lesions have also increased in prevalence in young individuals with and without GI symptoms in the past two decades. Some portion of the increased prevalence of polyps at colonoscopy during this time period could be due to higher quality colonoscopy. By limiting our analysis to P9mm, we hoped to minimize the impact of ascertainment bias that might otherwise occur if small polyps were also included.
These data provide support for recommendations from the American Cancer Society and the USPSTF to consider screening at age 45 years. However, our data do not fully explain the rise in early onset CRC, so there may be alternative factors, other than the adenoma-carcinoma sequence that may also underlie the increase in early-onset CRC. These data may be useful for benchmarking advanced adenoma detection in individuals age 40 to 59 years old.
Our data also indicate that patients less than 50 years who have a diagnostic colonoscopy for possible lower GI symptoms such as rectal bleeding, iron deficiency anemia or unexplained weight loss, have a risk of large polyps similar to patients undergoing average-risk screening at age 50 to 54 years (5.2 versus 5.4%). Therefore, colonoscopy should be strongly considered in such patients.
In summary, we found an increasing prevalence of P9mm in men and women age 40–59 years, undergoing colonoscopy from 2005 to 2014. By 2014, the prevalence of P9mm in 45 to 49 men and women was similar or higher than men and women age 50–59 in 2005, for whom screening is recommended. If these data are confirmed in other cohorts, average-risk screening before age 50 years could result in early onset cancer prevention by detection and removal of cancer precursor lesions.
Supplementary Material
Grant support:
This project was supported with funding from NIDDK U01DK57132. In addition, the practice network (Clinical Outcomes Research Initiative) has received support from the following entities to support the infrastructure of the practice-based network: AstraZeneca, Novartis, Bard International, Pentax USA, ProVation, Endosoft, GIVEN Imaging, and Ethicon. The commercial entities had no involvement in this research.
Financial support:
None to disclose
List of abbreviations:
- AA
Advanced adenoma
- CORI
Clinical Outcomes Research Initiative
- CRC
Colorectal cancer
- P9mm
Polyp greater than 9 mm
- USPSTF
United States Preventive Services Task Force
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest:
Benjamin Yip has no financial, professional, or personal relationships to disclose
Jennifer Holub has no financial, professional, or personal relationships to disclose
David Lieberman has no financial, professional, or personal relationships to disclose
References
- 1.Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal Cancer Incidence Patterns in the United States, 1974–2013. J Natl Cancer Inst 2017;109:27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL,. Miller KD, Jemal A Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970–2014. JAMA 2017; 318: 572–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lui RN, Tsoi KKF, Ho JMW, et al. Global Increasing Incidence of Young-Onset Colorectal Cancer Across 5 Continents: A Joinpoint Regression Analysis of 1,922,167 Cases. Cancer Epidemiol Biomarkers Prev 2019;28:1275–1282. [DOI] [PubMed] [Google Scholar]
- 4.Wolf AMD, Fontham ETH, Church TR et al. Colorectal cancer screening for average-risk adgults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin 2018; 68: 250–81 [DOI] [PubMed] [Google Scholar]
- 5. https://uspreventiveservicestaskforce.org/uspstf/public-comments-and-nominations/opportunity-for-public-comment.
- 6.Lieberman D, Moravec M, Holub J, et al. Polyp Size and Advanced Histology in Patients Undergoing Colonoscopy Screening: Implications for CT Colonography. Gastroenterology 2008;135:1100–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. https://wonder.cdc.gov/controller/datarequest/D160.
- 8.Murphy CC, Wallace K, Sandler RS, et al. Racial Disparities in Incidence of Young-Onset Colorectal Cancer and Patient Survival. Gastroenterology 2019;156:958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


