Abstract
Face shield are the unmistakable plastic gatekeepers secures eyes and face, simpler to wear and a group of specialists state face shields may supplant masks as an increasingly agreeable and progressively successful obstacle to COVID-19. Face shields are useful in stopping respiratory droplets from speading from the wearer to others. The droplets, which come into contact with the shield, are quickly spread over a large area, both transversely and vertically, over the shield, but with a shrinking concentration of droplets, as opposed to face masks, which appear to slide under the nose of the wearer or, worse, collapse entirely off the shield. Hence, a face- shield can be considered as personal protective equipment (PPE), which is a first line of resistance, utilized by the clinicians and forefront health workers for protection against the infectious body fluid and aerosols. Face-shields are mainly fabricated using polycarbonate material, because of their excellent optical transparency in UVA-visible-IR spectrum and mechanical properties. The goal of this article is to provide researchers working in the same area, as well as health and industrial staff, with a detailed analysis of the usage of face shields against bioaerosols and the need for personal security. The reviews main focus on the background of the face shield, provide assistance in the selection, its design and structure, applications, advantages and disadvantages. Lastly, people's view about the usage of face shield as it becomes an essential part of human beings like an accomplice during this current pandemic situation.
Keywords: Aerosols, Virus, Face shield, PPE
Graphical abstract
1. Introduction
Respiratory infections in human beings are the major reason of the massive international pandemics and hyperendemics encountered by people [1]. Viable (alive) bioaerosols are ubiquitous airborne biological particles generated in the course of action incorporating the biological agents which creates a sufficient amount of energy to disintegrate the small particles from the larger substance, such as air, water, wind or physiological motion[2]. These bio-aerosols are predominantly liable for microbiological activities are infectious or pathogenic responsible for causing disease. People are suffered by various airborne biological matters affecting their health by causing respiratory related diseases like asthma and emphysema. These respiratory sensitization makes breathing difficult for the them. A well-known occurrence was the epidemic of meningococcal meningitis in sub-Saharan Africa, which was associated with dust storms during dry seasons. Other outbreaks related to dust incidents, including Mycoplasma pneumonia and tuberculosis [3]. Another incidence was an increase in human respiratory disorders in the Caribbean, which may have been caused by residue of heavy metals, micro - organisms bioaerosols, and chemicals carried by dust clouds through the Atlantic Ocean [4]. Thus, protection barriers are required from these airborne particles. Prevention from these bioaerosols infections and control measures include self-hygiene and personal protective equipment. The personal protective equipment(PPEs) having standard precautions consists of gloves, mask, gown or coverall, face shield, head cover, rubber boots apparels to safeguard the health care workers or any other persons of catching infection [5].
2. Utilities of face shield over surgical (Face) mask
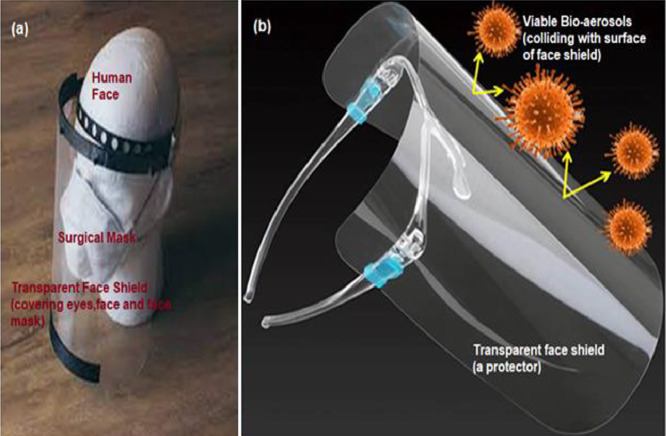
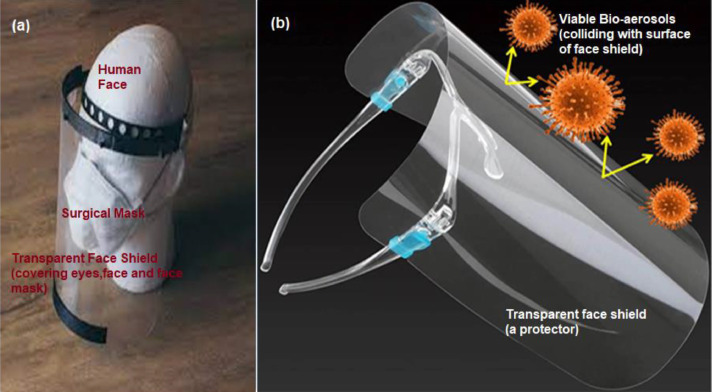
Highly contagious new coronavirus (COVID-19) disease continues to spread across the globe, with specialists more than once underlining the importance of changing our way of life in order to remain safe [6], [7], [8], [9]. Covid-19 can be transmitted from infected people to healthy people by three variant routes: coming in direct contact with infected people, indirect contact (like touching things of infected people) and most affectively by airborne transmission [10,11]. Up till now, there is no cure, diagnostics and therapeutics treatment known, henceforth they present an massive danger of a disastrous global pandemic [12], [13], [14]. The confinement and regulations of this disease has been a major issue, given the enormous protocols put forward by various regulatory authorities, such as the WHO. Standard guidelines and protocols provided by the WHO, the Centers for Disease Control, the International Labor Organization and the European Agency for Safety and Health to Prevent Infections between Healthcare Workers and Non-Health Workers Safety measures include cleaning facilities, proper and adequate hand-washing, hygiene and ethics, national travel recommendations, emphasis on staying at home to control the contamination and compliance with the rules of procedure, case notification and management, and proper use of face masks [15], [16], [17]. For the protection of people “Prevention is always marked superior than cure” to fight against infectious, transmittable and communicable disease. Thus, as per the current scenario, to combat this unprecedented and promptly transmitting COVID-19 pandemic, only way is to follow precautionary measures well in advanced [18]. While researchers and clinical specialists are working day and night to build an antibody to fight infection, there is no complete solution to the infection from now on. This is the reason for practicing social distancing, wearing face covers or masks while venturing outside and washing hands regularly ranks at the head of prudent steps. Sanitization is a considered as the best preventive adapted measure to constrain the spread of SARS-CoV2 [19].Disease Control and Prevention (CDC), the Occupational Safety and Health Administration (OSHA), World Health Organization (WHO) as well as Indian bodies including Ministry of Health and Family Welfare (MoHFW), among others, have recommended the use of PPEs (like surgical mask, safety goggles, face shields, masks and medical clothings) to patients and healthcare providers [20]. Personal protective equipment (PPE) are devices utilized by numerous specialists e.g., clinical, dental, veterinary for protection of the facial area and related mucous films (nose, eyes, mouth) from sprinkles, showers, and splash of body liquids during assessment, medical procedure and post therapy care. The surgical mask and face shield is a first line of defense against the transmission of diseases via physical contact from aerosols and body fluids in the operating theatres and hospital wards for the frontline health workers and clinicians also a mean of eased of restrictions on extreme social distancing. Generally, Face shields are not being used on their own, but in conjunction with other protective equipment and are therefore classified as adjunctive personal protective equipment [Fig.1(a)] [21], [22], [23]. Since ages, the presence of virus/bacteria contained in the droplets emanating from the nose and mouth while coughing or sneezing are the root cause of disease transmission. Keeping the guidelines in mind, plenty of people are reaching out for face mask to keep themselves safe. While earlier face mask was seen as the go to protection gear against this battle with corona virus, more and more people are opting to wear face shield. Just as face masks as protection gear commonly worn in public to against the battle of corona virus similarly, the face shields are clear plastic shields that cover the face are starting to be worn outside of medical settings and for good reason [24,25]. As indicated by the researchers' in vitro experiments, face masks provide sufficient filtration of virus-sized aerosol particles, but face shields may provide a better choice than face masks. As face shields offer a transparent plastic barrier to the user's face. For greater protection, the shield should stretch to the ears or below the chin and there should be no exposed space between the front and the headpiece of the shield. The face masks give several benefits over the face mask. Face Masks are often worn improperly exposing the nose and eyes to provide quick inhalation and virus intake [26,27]. Also, face masks also do not adjust comfortably and wearers are more vulnerable to touching their mouths, raising the chances of infection or viral entrance. Face masks have a small lifespan and a little reprocessing capacity, while face shields can be reused for an infinite time and can be washed daily with soap and water or household cleaning disinfectants. They are easy to wear, protect viral entry portals, and reduce the risk for auto-inoculation by stopping the wearer from touching his skin. People with face masks nearly often have to remove them in order to interact with those around them; this isn't really required with face shields. The use of a face shield is often a reminder that a good space remains between them, but it also allows facial gestures and motions of the mouth to be noticeable for speech understanding.
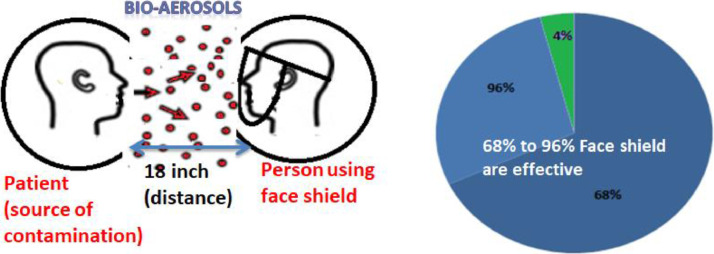
Wearing masks, which act as a barrier to contain infectious agents from exhaled air or being inhaled, has been shown to drastically minimize disease transmission in certain countries. According to recent study, a surgical mask will effectively inhibit the spread of infectious agents by symptomatic persons. The removal of surgical masks can prevent aerosols inhalation, matters from entering the lungs, which may help to reduce the risk factors are being impacted, as well as proper hand hygiene as one methods of sterilization [28]. The improper use and disposal of masks, on the other hand, pose a high risk of secondary transmission and also jeopardize the protection effect when persistent pathogens gather over surgical masks. Analysis reveals that the commercial face masks have no capacity to destroy the contained bacteria. Approximately about 90% bacterial or viral infection persists over the surface of surgical mask proliferative even after 8 h of time period. [29], [30], [31]. Huang et.al in his study reveal that surgical face masks has a very little capability to destroy the contaminated virus. This constitutes a danger to community when surgical masks are inappropriately used or discarded [32].Whereas, at a distance of just 18 inches from a coughing individual, face shields have been shown to reduce immediate viral exposure by 96%, according to a study using influenza virus [33] and a review of studies of coronavirus transmission found that the use of eye protection was associated with 78% less infection than with no eye protection, with the researchers noting that "Eye protection are naturally under considered and can be effective in communal settings." by Chu, Lancet [34]. Most relevantly, face shields significantly reduce levels of exposure to the influenza virus, other vapor, or droplet spread of respiratory infection. Face shields were shown to reduce direct viral exposure by 96 percent when worn by a person who is healthy, within 18 inches of cough in a simulation study. Face shield creates a protective shield or impact roughly equal to ~ 80 percent even after half an hour of exposure and also prevents the entrance of small particle aerosols to 68 percent which are not considered to be an influential cause of SARS-CoV-2 infection. Maintaining the social gap, its shielding efficiency increased to 92%. Thus, through analyzing the simulation analysis, the effectiveness levels of the face shield range differ from 68% to 96% [35]. Face shields use inexpensive material such as plastic sheets, polycarbonate sheets, etc. for manufacturing and production lines can be recycled very easily. Apple, Nike, GM, and John Deere are only a few face shield suppliers. This shield may also be made from items used in art or office supplies shops. In fact, for the initiated face shield, a transparent plastic sheet that covers the whole face instead of only the mouth just protects our eyes (Fig.1 (b)). The figures clearly show how these viable bio-aerosols interact with surface of face shield and representing the danger of direct inhale of aerosols by eye nose and mouth, if not wearing face shield. Besides, virus stability and expensive diagnostics still remain as challenges to overcome this pandemic situation. The features of face shield can be used as an effective tool for managing personal point of care and personalized health management [36]
Fig. 1.
(a) Face shield (as Adjunt Personal Protective Equipment)(b)Represents Tranparent (Face) Shield Protects against pathogenic microbes to enter through eyes, nose and mouth.
Here, the focus of this review is on face shields as the important means to protect both health care providers and patients from contamination and spreading of disease. Face shields address three key means of preventing coronavirus transmission: They provide a barrier to respiratory droplets (which, according to the CDC, can occur when a person coughs, sneezes, or talks), help wearers avoid touching their face and recommended especially for eye protection. In addition, unlike masks and N95 respirators, they cover the eyes as well as the mouth and nose, allow for easier communication, and are more easily cleaned (with just soap and water or household disinfectants) for reuse. They provide a better barrier to respiratory droplets in close proximity to an infectious person.
3. Face shield as safety concern and precautions: research overviews
Discussion among the researchers suggests that “Faceshields” are considered more suitable than “Face masks” for Corona virus. As it is widely accepted that a surgical mask gives more protection to other person than the individual wearing it whereas, face shield, offers the wearer an additional safety which may be more helpful in preventing transmission of virus. Some of the statements given by user's and researchers during this pandemic about the faceshield are “Face shields, can be developed and distributed rapidly and affordably, should be used as part of approaches to safe sound and substantially minimize spread in the community environment,' as stated by trio of University of Iowa physicians. According to Perencevich's research group, "Face shields offer a better option with a range of benefits above the face masks. Furthermore, they are endlessly reusable; they simply need soap and water or traditional disinfectants to be cleaned. Shields are probably easier to wear than masks, and they create a barrier to prevent individuals from touching their faces easily [37]. People always take a mask down when chatting to make it easier but that's not required with a face shield "the use of a face shield is also a reminder to maintain social distancing, but allows visibility of facial expressions and lip movements for speech perception," the writers pointed out. Large-scale experiments have not yet been performed, according to the Iowa team. But "in a simulation study, face shields were shown to reduce immediate viral exposure by 96 percent when worn by a simulated health care worker within 18 inches of a cough". Thus, Face shield has the ability to prevent coronavirus transmission more effectively [38,39]. The medical professional peoples are also suggesting about the use of “faceshield”. Dr. Robert Glatter, at New York City's Lenox Hill Hospital. Reading through the new report, he agreed that the use of face shields is the most meaningful option, particularly given the drawbacks of face masks and face shields. This is the Reading through the new study; he agreed that the use of face shields is the solution that makes the most sense, particularly in view of the limitations of face masks and face coverings. The notion of risk assessment and management needs to be added to discussions of PPE for non-healthcare workers and common man are that one can touch their face easily with an ease by using these face shield also they are non-suffocating or easy to breath
4. Approaches to face shield assembly
Face shields are simple, translucent screens that cover the face and avoid contagious droplets from penetrating the eyes, nose and mouth. These are usually worn in combination with goggles or breathers, preventing splashes and sprays from hitting the skin and preventing staff from scratching their mouths [40]. They typically consist of only two parts: a face-covering visor, usually made of plastics such as polyvinyl chloride (PVC), polycarbonate, propionate, acetate, and polyethylene terephthalate glycol (PETG), and a way of keeping the visor in place, such as a headband or brace. Polycarbonate material face shield are most popular due to its excellent impact resistance, optical quality, heat resistance. The strap may be made of molded resin, 3D-printed plastic or even elastic [41]. Polycarbonate face shields build a transparent mask or protection for people. They are clear round plastic pads, typically attached to safety glasses or a headband, allowing another person to sit in front of your face, disabling any source of pollution. As a result, plastic sheets serve as a sneeze guard that stops droplets from moving from one mouth or nose to another. Cover the eyes and other mucous membrane areas from bacterial infection [42]. As per the current scenario, vast number of individuals use face masks, but the guidelines for their use differ from office to the medical profession, and no literature or analysis is open to the public as to their appropriateness.
The Occupational Safety and Health Administration's (OSHA's) guideline 29 CFR 1910.133 involves the utilization of eyes and face protection when laborers are presented in eye or face dangers, for example, airborne items, liquid metal, chemicals, acids or burning fluids, compound gasses or fumes, or possibly harmful light radiation. OSHO addresses the certain standards for eyes and face protection in 1971 and set up Federal norms and public agreement guidelines also. From that point forward, OSHA has changed its eye and face protection norms on various events. “The American National Standards Institute (ANSI)’ also set up their own standards for Eye and Face Protection Devices standard firstly, in 1968 and reviewed them 5 times in 1979, 1989, 2003, 2010 and 2015. In 1989, ANSI specifically emphasized on design, materials, technologies and product performance of the devices made. In 2003, added an upgraded client choice outline with a framework for choosing equipment, for example, spectacles, goggles and face shields that satisfactorily shield from a specific risk. In 2010, concentrated on a environmental exposure, for example, scattered dust particles, sway, optical radiation, fine residue and fog, and indicates the sort of equipment expected to shield from that danger and in 2015 focus was to modify product efficiency synchronized with universal standards. Basically, in 2015 standards were made to modify the structural and efficiency of hazard-based products of 2010. While most of eye and face protection being used today is planned, tried and produced as per the ANSI Z87.1–2010 norm. It characterizes a faceshield as "a defender usually proposed to, when used in combination with spectacles, glasses or goggles, shield the user or wearer's face, or parts thereof, notwithstanding the eyes from specific perils for eyes and face, chiefly depends on faceshield type”[43]. ANSI Z87.1–2015 describes faceshield as “a defender projected to defend the face of wearer, from certain perils, as specified by the marking of faceshield used.” It can be considered as a complete device or protector with components intended to use for protection. Inspite of the fact that, from year 2010 till 2015, the definition of faceshield is completely changed comprising the standards mentioned in 2015 can be classified as “standalone devices”[44].
It is important to remember the importance of comfort, health and ease of use when choosing face shields. Faceshields should fit nicely and through the headgear, the primary way to ensure a snug fit is (suspension). Typically, headgear is adjustable in diameter and width. For circumference fit, the headband is adjusted and the topmost band should be adjusted for depth. The face shield should be centered for optimum alignment when worn properly and the suspension should lie between half an inch and one inch just above eyebrows. Meanwhile, faceshields are used in combination with other PPE, the PPE interaction must be smooth. It is best to have clear, easy-to-use faceshields that allow users to change the fit quickly. William G.Lindsley groups invented and explored the efficiency of face shield against the cough aerosol droplets and represented his results in graphical form. They studies the parameters of infection form aerosols “with and without faceshield” (Fig.2 .) and represented the deposition of aerosols faceshield on long term exposure. The graph presented in the figure clearly states that employing the face shield decrease the spread of infection among humans [45].
Fig. 2.
Schematic and graphical representation of Face shield (effectiveness) guard against bio-aerosols [Ref.No.20.].
5. Face shield design and its structure
The 3 chief essential constituents of a face shield (Fig.3 .) considering the eyes and face protection are described below:
Fig. 3.
Decoration of face shield assembly further protection from airborne viruses transmission .
5.1. Visor and its material
Visors are transparent lenses or windows are made of any of several types of materials, including polycarbonate, propionate, acetate, polyvinyl chloride polyethylene terephthalate glycol (PETG) and are accessible as removable, reusable and replaceable models.Polycarbonate is one of the most widely used for making visor due to its Optical integrity, which helps to minimize the pressure of the eye involved with wearing a face mask [46], [47], [48].Visors can be treated with specialized coatings that have anti-glare, anti-static and anti-fogging properties, protection against ultraviolet light (UV) and scratch resistance functions to extend the life of the visor [49,50].
5.2. Frame
There are a range of frame styles, including flexible and non-adjustable lenses, which encircle the circumference of the skull entirely or partly, or those with temple-shaped eyeglass bars worn as regular eyewear. Available metal clip-on frames for mounting face shields on prescription eyewear are available, and some frames allow the viewfinder to be flipped if not in operation. In order to easily change the face shield visor, the detachable frames often consist of a silicone cushion on the forehead, which gives a supporting seal on the forehead.
5.3. Suspension systems
There are a variety of face shield suspension systems on the market that deliver fully or partly circumferential attachment characteristics. Fully circumferential suspension systems with silicone headbands that are adjustable by means of a ratchet mechanism, pin-lock systems for comfort; elastic belts are used for non-adjustable systems. For suspensions with or without eyewear-like nose pads and bridge assemblies, some versions use temple-type eyeglass bars to better control face shield position and face protection [51].
Types of Face shield: The Occupational Safety and Health Administration (OSHA) advises that you wear face masks if you are in contact with certain explosives, acids, radiation, toxic vapors or airborne objects. Face shields are encouraged to be used for safety purpose if you work in any of the following sectors, such as Food Service, Hospitals, Renovation, Laboratory Technicians, Art, Manufacturing and Supermarket, or retail stores. For all these different tyoes or shapes of face shield are available. There are 6 different types of face shields (shown in Fig.4 .) are:
-
•
Headband face shield that fits around the forehead,
-
•
Food-grade plastic shield Food-grade plastic shields used by cooks, bakers, and anybody else who deals around food,
-
•
The disposable face shield is a single-use shield only;
-
•
Wide face shield wider than ususal used face shields,
-
•
Pivot face shield are adjustable, and can be pivot on the top,
-
•
Face shield with built-in goggles protects the eye and is very important for many professions, such as welders, construction workers and mechanics [52], [53], [54], [55].
Fig. 4.
Various types of face shield : (a) Head band (b) Food-grade (c) Dispodable (d) Wide Shape (e) Pivot (f) Face shield with built in glasses [Ref.No.27].
Safety Guidelines of making and usage of face shield: Facial shields should be manufactured keeping into account the welfare of frontline Heath care staff and other industrial consumers. There are some points to be highlighted:
-
•
The shield should be secure or snug on the forehead. There should be no distance between the forehead and the shield and it should be securely mounted around the head without any loopholes or gaps .
-
•
A soft sponge must be used between the head and the face shield for ease of relaxed wear.
-
•
The translucent portion of the face shield thickness should be closer to ~150 to 200 μ for quick air passage and also prevent crimping.
-
•
The important aspect of the face shield is that it can be reused after careful sterilization. The face shields can be sterilized by holding them in 1% sodium hypochlorite solution for around 10 min, with sunlight exposure about half an hour. It can also be sterilized by using 2 percent Glutaraldehyde for 10 min, wash it with regular saline, dry it again. It can also be clean with water and soap.
-
•
Consumers must always avoid touching and holding the front side of the OHP/face shield and should use the correct sterilization process.
-
•
The face shield should indeed be safely disposed of only after sterilization in order to prevent infection and damage to others [56].
6. Diversities of face-shield utilization in various other fields
7.1. Medical: Face protection" in medical applications refers to a variety of instruments used in the process of an operation to protect a medical worker that may be exposed to blood or other highly contagious fluids. Examples include the usage of a CPR mask as a rescue ventilation or CPR. Use of personal protective equipment to protect the face against exposure of potentially infectious species or products is another example.
7.2.Defense: For ballistic or non-ballistic defense, a face shield can be built in military or law enforcement environments. A non-ballistic shield does not protect against projectiles shot from a ballistic face shield designed to deter or scatter explosions and debris from operators wearing bomb suits.
7.3.Construction sites: Many employees use face masks at many construction sites to protect them from debris or sparks. The use of a face mask is recommended by many instruments for cutting and working with metal. Welding equipment or metal chop saws, for instance [57].
7.4.Protection against the Arc Flash – These faceshields are used against an arc flash for defense. In the National Fire Protection Association (NFPA) 70E standard, the specifications for arc flash protection are provided.Face shields are part of this norm and must be secured on the basis of the Arc Thermal Efficiency Value (ATPV) measured in calories per square centimeter (cal/cm2) [58]. In order to pick the shield that will have the best defense, the calorie rating must be measured first.
7.5. Heat and Radiation – Face shields are required to protect from heat and radiation. These face shields prevent burns by blocking out ultraviolet (UV) and infrared (IR) radiation. They are made of specially coated polycarbonate. An example of this will be the application of a thin layer of gold film to increase reflectivity.
7.6.Welding – Shaded face shield welding protects against UV and IR radiation emitted when dealing with molten metal. The shades typically vary from Shade 2 to 14, with Shade 14 being the darkest color or shade [59].
8. Advantages and disadvantages of face shields: Face shield as an eye and face protector is compared with other personal protective equipments such as mask, goggles and safety glasses. Its advantages and disadvantages are:
8.1. Advantages: Face shields are curved plastic pieces that protect the whole face from the top of the forehead to the ear. Scientist and researchers suggest that a face shield inhibits large Coronavirus droplets from moving through mucus membranes in the eyes, nose, and mouth from blocking 96 percent of the flu virus in large droplets and 68 percent of tiny droplets. Some advantages of the use of a face shield include:
-
•
Imperensible (plastic covering)
-
•
More comfortable-protect a larger portion of the face-less facial dermal retention
-
•
Wearers are less likely to touch their faces and eyes.
-
•
Protects eyes to block the infection from entering
-
•
heat-less fogging than goggles-less claustrophobic fogging
-
•
No impact of breathing resistance as restricted in the face mask
-
•
No fit testing is needed
-
•
It can be easily disinfected
-
•
The wearer would not need to be shaved clean
-
•
Reasonably affordable
-
•
No impact of vocalization
-
•
can be worn at the same time as the other EPP face/eye
-
•
Decreased anxiety among patients
-
•
easy to scrub with soap and water
-
•
Defends against self-inoculation over a larger facial region.
-
•
Facial non-verbal contact cannot be obstructed
-
•
can improve the useful life of a protective face mask when used together.
8.2. Disadvantages: Some drawbacks of using Face shields are:
-
•
Glare-fogging
-
•
Optically defective
-
•
Certain versions do not match correctly on some of the respirators
-
•
More cumbersome than helmets and safety lenses
-
•
Peripheral suit worse than defensive facial masks (e.g. duckbill filtering facial breathers)
[60].
Certain crucial steps should be taken face shield manufacturing companies to overcome these disadvantages by using high quality transparent sheet mainly commonly made up of Polycarbonate material. Its optical quality and transparency should be verified and tested by certified labs for making high quality shields.
7. Conclusions, outlook and future aspects
If there is a risk for damage to the face from flying debris, molten metals, liquid chemicals, acids or caustic substances, toxic gasses or vapors, potentially dangerous light radiation or a combination of these, appropriate eye and face protectors must be provided. Personal protective equipment (PPE) such as gloves, masks, gowns or blankets, face shields, head caps, rubber boots are all used as barriers to infectious control and avoid contamination with viral infections. A Face shield is an impenetrable translucent layer with the wearer's whole eyes and the face protects virus contamination from being infected by hazards such as flying particles and road waste, chemical splashes in labs and warehouses, or possibly infectious materials. According to the view of people, face shields are a much better option than masks as constantly people fussing with their masks, pulling them up and down over their nose which just smears any virus all over their noses and faces. Also, they are breathable; you can see a person's face and mouth when they talk. Constructing hats with shielding attached would be simple for younger kids to wear. Polycarbonate is considered the best material used for face shields because of its optical clarity and impact resistance. Face shields are highly used in chemical applications as they have high optical transparency, inflexibility and firmness. They can also tolerate clamping and breaking over a large temperature range under normal tension, along with excellent resistance to oil and grease. They also have higher longevity over long stretches of time and do not get distorted or bent under normal temperatures. In order to make face shield more efficient and optimal security in stopping viral spread, one suggestive move can be considered here, The face shield should be extended to the bottom of the chin. The distance usually filled with a foam cushion should also protect the ears and there should be no exposed gap between the front and the headpiece of the shield. Face shields are cost-effectively manufactured and can be used as part of policies to ensure a safe and significant reduction in transmission in group settings. Both safety requirements and guidelines for their use, disposal and sterilization must be taken into account by both the manufacturer and the customer.
8. Credit author statement
The corresponding author is responsible for ensuring that the descriptions are accurate and agreed by all authors.
Declaration of Competing Interest
No conflicts of Interest.
Acknowledgments
Archana Chakravarty is thankful to University Grants Commission (UGC), New Delhi for financial support in the form of Dr. DS Kothari Post Doctoral Fellowship for preparation of this manuscript.
References
- 1.Raji V., Pal K., Zaheer T., Kalarikkal N., Thomas S., Souza F.G.D., SI A. Gold nanoparticles against respiratory diseases: oncogenic and viral pathogens review. Ther. Deliv. 2020;11:521–534. doi: 10.4155/tde-2020-0071. https://doi.org/10.4155/tde-2020-0071. [DOI] [PubMed] [Google Scholar]
- 2.Ghosh B., Lal H., Srivastava A. Review of bioaerosols in indoor environment with special reference to sampling, analysis and control mechanisms. Environ. Int. 2015;85:254–272. doi: 10.1016/j.envint.2015.09.018. doi:10.1016/j.envint.2015.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molesworth A.M., Cuevas L.E., Morse A.P., Herman J.R., Thomson M.C. Dust clouds and spread of infection. Lancet. 2002;359:1–90. doi: 10.1016/S0140-6736(02)07304-X. https://doi.org/10.1016/S0140-6736(02)07304-X. [DOI] [PubMed] [Google Scholar]
- 4.W.Griffith D. Atmospheric movement of microorganisms in clouds of desert dust and implications for human health. Clin. Microbiol. Rev. 2007;20:459–477. doi: 10.1128/CMR.00039-06. 10.1128/CMR0047-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.M.Cook T. Personal protective equipment during the COVID-19 pandemic - a narrative review. Anaesthesia. 2020;75:920–927. doi: 10.1111/anae.15071. https://doi.org/10.1111/anae.15071. [DOI] [PubMed] [Google Scholar]
- 6.Chan J.F.-W., Kok K.-.H., Zhu Z., Chu H., Wang To K.K., Yuan S., Yuen K.Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020;9:221–236. doi: 10.1080/22221751.2020.1719902. 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . 2020. Coronavirus Disease 2019 (COVID-19): Situation report, 51. World Health Organization 2020.https://apps.who.int/iris/handle/10665/331475 (accessed by March 11, 2020) [Google Scholar]
- 8.Sohrabi C., Alsafi Z., Neill N.O., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.CDC . US Department of Health and Human Services, CDC; Atlanta, GA: 2020. Coronavirus Disease 2019 (COVID-19) (2020): schools, workplaces, & Community Locations. (accessed by February,5 2021) https://www.cdc.gov/coronavirus/2019ncov/community/index.html? CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fpreparing-individuals-communities.html. [Google Scholar]
- 10.World Health Organization . World Health Organization; 2020. Modes of Transmission of Virus Causing COVID-19: Implications For IPC Precaution recommendations: Scientific Brief.https://apps.who.int/iris/handle/10665/331601 [Google Scholar]
- 11.Ong S.W.X., Tan Y.K., P.Y.Chia T.H.Lee, Ng O.T., Wong M.S.Y., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323:1610–1612. doi: 10.1001/jama.2020.3227. doi:10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.E.A. Pharo, S.M. Williams, V. Boyd , V.Sundaramoorthy, P.A. Durr, M.L. Baker, Host pathogen responses to pandemic influenza H1N1pdm09 in a human respiratory airway model viruses,12 (2020) 679.doi:10.3390/v12060679. [DOI] [PMC free article] [PubMed]
- 13.Nuzzo J.B., Mullen L., Snyder M., A.Cicero T, Inglesby V. 2020. Preparedness For a High.-Impact Respiratory Pathogen Pandemic; The Johns Hopkins Center For Health Security: Baltimore, MD, USA. (accessed by September 2019)1- 84. https://apps.who.int/gpmb/assets/thematic_papers/tr-6.pdf. [Google Scholar]
- 14.Global Preparedness Monitoring Board . World Health Organization; Geneva, Switzerland: 2019. A World at Risk: Annual Report On Global Preparedness For Health Emergencies; pp. 1–52.https://apps.who.int/gpmb/assets/annual_report/GPMB_AR_2020_EN.pdf [Google Scholar]
- 15.Alao M.A., Durodola A.O., Ibrahim O.R., Asinobi O.A. Assessment of health workers knowledge, beliefs, attitudes, and use of personal protective equipment for prevention of COVID-19 infection in low-resource settings. Adv. Pub. Health. 2020;2020:1–10. https://doi.org/10.1155/2020/4619214. [Google Scholar]
- 16.Razai M.S., Doerholt K., Ladhani S., Oakeshott P. Coronavirus disease 2019 (covid-19): a guide for UK GPs. BMJ. 2020;368:m800. doi: 10.1136/bmj.m800. doi: 10.1136/bmj.m800. [DOI] [PubMed] [Google Scholar]
- 17.Ambigapathy S., Rajahram G.S., Shamsudin U.K., Khoo E.M., Cheah W.K., Peariasamy K.M., Goh P.P., Khor S.K. How should front-line general practitioners use personal protective equipment (PPE)? Malays Fam. Phys. 2020;15:2–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7136675/ [PMC free article] [PubMed] [Google Scholar]
- 18.Bhavanaa V., Thakora P., Sing S.B., Mehra N.K. COVID-19: pathophysiology, treatment options, nanotechnology approaches, and research agenda to combating the SARS-CoV2 pandemic. Life Sci. 2020;261 doi: 10.1016/j.lfs.2020.118336. https://doi.org/10.1016/j.lfs.2020.118336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan M.H., Yadav H. Sanitization during and after COVID 19 pandemic: a short review. Trans. Indian Natl. Acad. Eng. 2020;5:617–627. https://doi.org/10.1007/s41403-020-00177-9. [Google Scholar]
- 20.Sharma N., Hasan Z., Velayudhan A., Emil M.A., Mangal D.K., Gupta S.D. personal protective equipment: challenges and strategies to combat covid-19 in india: a narrative review. J. Health Manag. 2020;22:157–168. https://doi.org/10.1177%2F0972063420935540. [Google Scholar]
- 21.Roberge R.J. Face shields for infection control: a review. J. Occup. Environ. Hyg. 2016;13:235–242. doi: 10.1080/15459624.2015.1095302. https://dx.doi.org/10.1080%2F15459624.2015.1095302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization . 2020. Rational Use of Personal Protective Equipment (PPE) For Coronavirus Disease (COVID-19): Interim Guidance. (accessed by March,19 2020).https://apps.who.int/iris/handle/10665/331498. [Google Scholar]
- 23.World Health Organization . World Health Organization; Geneva, Switzerland: 2014. Personal Protective Equipment in the Context of Filovirus Disease Outbreak Response Rapid Advice Guideline: Summary of the Recommendations. (accessed by October 2014) 1-12. https://apps. who.int/iris/handle/10665/137410. [PubMed] [Google Scholar]
- 24.Bowles J., Hjort J., Melvin T., Werker E., Ebola E. Jobs and Economic Activity in Liberia. J. Epidemiol. Community Health. 2016;70:271–277. doi: 10.1136/jech-2015-205959. doi: 10.1136/jech-2015-205959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Offeddu V., Yung C.F., Low M.S.F., Tam C.C. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin. Infect. Dis. 2017;65:1934–1942. doi: 10.1093/cid/cix681. https://doi.org/10.1093/cid/cix681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coibion O., Gorodnichenko Y., Weber M. Labor markets during the COVID-19 crisis: a preliminary view. SSRN J. 2020 2020, Labor Markets During the COVID-19 Crisis: A Preliminary View, NBER Working Paper No. 27017 (accessed by April 2020) 1-15.https://www.nber.org/system/files/working_papers/w27017/w27017.pdf. [Google Scholar]
- 27.McKibbin W.J., Fernando R. The global macroeconomic impacts of COVID-19: seven scenarios. CAMA working paper 19/2020. SSRN J. 2020 (accessed by 2 March,2020).https://dx.doi.org/10.2139/ssrn.3547729. [Google Scholar]
- 28.Pal K., Kyzas G.Z., Kralj S., de Souza F.G. Sunlight sterilized, recyclable and super hydrophobic anti-COVID laser-induced graphene mask formulation for indelible usability. J.Mol. Struc. 2021;1233 doi: 10.1016/j.molstruc.2021.130100. doi.org/10.1016/j.molstruc.2021.130100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.H., McDevitt J.J., Hau B.J.P., Yen H.L., Li Y., Ip D.K.M., Peiris J.S.M., Seto W.H., Leung G.M., Milton D.K., Cowling B.J. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. doi.org/10.1111/irv.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eikenberry S.E., Mancuso M., Iboi E., Phan T., Eikenberry K., Kuang Y., Kostelich E., Gumel A.B. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020;5:293–308. doi: 10.1016/j.idm.2020.04.001. doi: 10.1016/j.idm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feng S., Shen C., Xia N., Song W., Fan M., Cowling B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020;8:434–436. doi: 10.1016/S2213-2600(20)30134-X. doi: 10.1016/S2213-2600(20)30167-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.L.Huang L.Ling, Su J., Song Y., Wang Z., Tang B.Z., Westerhoff P., Ye R. Self-reporting and photothermally enhanced rapid bacterial killing on a laser-induced graphene mask. ACS App. Mat. Interface. 2020;12:51864–51872. doi: 10.1021/acsnano.0c05330. doi: 10.1021/acsami.0c16596. [DOI] [PubMed] [Google Scholar]
- 33.Walker M. 2020. Universal Face Shields For COVID-19: The New and Improved Mask?https://www.medpagetoday.com/infectiousdisease/covid19/86273 [Google Scholar]
- 34.Chu D.K., Akl Elie A, Duda S., Solo K., Yaacoub S., Schünemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. doi.org/10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perencevich E.N., Diekema D.J., Edmond M.B. Moving personal protective equipment into the community face shields and containment of COVID-19. JAMA. 2020;2020323:2252–2253. doi: 10.1001/jama.2020.7477. doi:10.1001/jama.2020.7477. [DOI] [PubMed] [Google Scholar]
- 36.Mishra S., Kim E.S., Sharma P.K., Wang Z.J., Yang S.H., Kaushik A.K., Wang C., Li Y., Kim N.Y. Tailored biofunctionalized biosensor for the label-free sensing of prostate-specific antigen. ACS Appl. Bio Mater. 2021 doi: 10.1021/acsabm.0c01002. doi.org/10.1021/acsabm.0c01002. [DOI] [PubMed] [Google Scholar]
- 37.Mundell E.J. 2020. Are Face Shields Better Than Face Masks For Coronavirus?https://www.medicinenet.com/script/main/art.asp?articlekey=230978 [Google Scholar]
- 38.Centers for Disease Control and Prevention(CDC) 2020. Questions & Answers Regarding Respiratory Protection For Infection Control Measures for 2009 H1N1 Influenza among Health care Personnel.http://www.cdc.gov/h1n1flu/guidance/ill-hcp_qa.htm (accessed March 20, 2013) [Google Scholar]
- 39.Mundell E.J. 2020. Face-shields-a-potential-alternative-to-masks-experts-say.https://www.upi.com/Health_News/2020/04/30/Face-shields-a-potential-alternative-to-masks-experts-say/4081588260103/ (accessed April 13,2020) [Google Scholar]
- 40.International Safety Equipment Association (ISEA) 2015. Draft ISEA 119: Standard for Eye and Face Protection Against Biological Hazards.https://safetyequipment.org/userfiles/File/Background_statement.pdf [Google Scholar]
- 41.Wesemann, Pieralli S., Fretwurst T., Nold J., Nelson Katja, Schmelzeisen R., Hellwigand E., Spies B.C. 3-D printed protective equipment during COVID-19 pandemic christian. Materials (Basel) 2020;13:1997. doi: 10.3390/ma13081997. https://doi.org/10.3390/ma13081997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berger A.S. 2020. Face Shields: Are They Functional Or Just Fashionable?https://www.gideononline.com/2020/06/08/face-shields-are-they-functional-or-just-fashionable/ (accessed 8june2020) [Google Scholar]
- 43.ISO 4007 . 2018. (en), Personal protective Equipment—Eye and Face Protection. https://www.iso.org/obp/ui/#iso:std:iso:4007:en. [Google Scholar]
- 44.ANSI/ISEAZ87 . 2015. Personal Eye and Face Protection Devices.https://www.ishn.com/articles/105559-ansiisea-z87-2015 [Google Scholar]
- 45.Lindsley W.G., Noti J.D., Blachere F.M., Szalajda J.V., Beezhold D.H. J. Occup.Environ.Hyg. 2014;11:509–518. doi: 10.1080/15459624.2013.877591. doi: 10.1080/15459624.2013.877591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beckerdite K. Eye & face protection: overcome the challenges to using faceshields. Indust. Hyg. Safety. News. 2012 Available at: http://www.ishn.com/articles/94033- eye—face-protection. (accessed July 15, 2015) [Google Scholar]
- 47.Nighswonger T. 2000. Face Up to Proper protection. Environ Health Safety. Available at: http://ehstoday.com/ppe/eye-face-head/ehs_imp_33545. (accessed July 15, 2015) [Google Scholar]
- 48.Farrier S.L., Farrier J.N., Gilmour A.S.M. Eye safety in operative dentistry – a study in general dental practice. Br. Dent. J. 2006;200:218–223. doi: 10.1038/sj.bdj.4813257. [DOI] [PubMed] [Google Scholar]
- 49.Beckerdite K. Eye & face protection: overcome the challenges to using faceshields. Indust. Hyg. Safety. News. 2012 http://www.ishn.com/articles/94033-eye—face-protection. [Google Scholar]
- 50.Centers for Disease Control and Prevention (CDC):Workplace Safety & Health Topics. Eye Protection for Infection Control. http://www.cdc.gov/niosh/topics/eye/eye-infectious.html (accessed July 29,2013).
- 51.Nighswonger T. Face up to proper protection. Environ. Health Safety. 2000 http://ehstoday.com/ppe/eye-face-head/ehs_imp_33545 (accessed July 15, 2015) [Google Scholar]
- 52.Gillespie C. 2020. Is a Face Shield Better Protection Against the Coronavirus Than a Face Mask?https://www.health.com/condition/infectious-diseases/coronavirus/face-shield-coronavirus (accessed 28May2020) [Google Scholar]
- 53.Perencevich E., Diekema D., Edmond M. 2020. Moving Personal Protective Equipment Into the Community.2020.https://jamanetwork.com/journals/jama/fullarticle/2765525?guestAccessKey=6af59d69-940c-49d6-8fc3-d790577a6a48 [DOI] [PubMed] [Google Scholar]
- 54.Harvard Health Publishing . 2020. COVID-19 Basics. 2020(10 July 2020) https://www.health.harvard.edu/diseases-and-conditions/covid-19-basics] [Google Scholar]
- 55.Mertes A. 2021. A Guide to Face Shields: Here's Everything You Need to Know.https://www.qualitylogoproducts.com/blog/different-face-shields (accessed 11 Feb,2021) [Google Scholar]
- 56.Khan M.M., Parab S.R. Safety guidelines for sterility of face shields during COVID 19 pandemic. Indian J. Otolaryngol. Head Neck Surg. 2020:1–2. doi: 10.1007/s12070-020-01865-2. doi: 10.1007/s12070-020-01865-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bhatnagar A. Woodhead Publishing; 2018. Lightweight Ballistic Composites: Military and Law-Enforcement Applications; pp. 396–397. eBook ISBN: 9780081004258. [Google Scholar]
- 58.Perencevich E.N., Diekema D.J., Edmond M.B. JAMA. 2020;323:2252–2253. doi: 10.1001/jama.2020.7477. doi:10.1001/jama.2020.7477. [DOI] [PubMed] [Google Scholar]
- 59.OSHA Fact Sheet, Eye Protection against Radiant Energy During Welding and Cutting in Shipyard Employment. https://www.osha.gov/Publications/OSHAfactsheet-eyeprotection-during-welding.pdf. (accessed February 18,2020)
- 60.Bradley K., Cassandra H., Gaeta R.N., Sharpp L., Tara J. Unmasking misunderstandings strategies for better communication with patients. Nursing (Brux) 2021;51:56–59. doi: 10.1097/01.NURSE.0000724368.90257.74. doi: 10.1097/01.NURSE.0000724368.90257.74. [DOI] [PubMed] [Google Scholar]