Abstract
Syphilis is a sexual transmitted disease caused by Treponema pallidum and an underdiagnosed and underreported cause of acute hepatitis. In recent years, reported cases of primary and secondary syphilis have been increasing, mostly in men who have sex with men. Clinical manifestations of syphilis are diverse, earning the name of “the great imitator” which can affect virtually any organ. Nonetheless, hepatic involvement is rare, but it can occur at any stage of the disease.
We present the case of a 41-year-old immunocompetent male, that presents to us with a cholestatic hepatitis and a diffuse erythematous rash with palmo-plantar affection. The patient had no history of primary syphilis. After throughout aetiologic study, he was diagnosed with syphilitic hepatitis and treated with intramuscular Benzathine benzylpenicillin, with the disappearance of the rash and normalization of liver enzymes after 3 months. We would like to highlight that this aetiology should be considered in patients with unexplained elevation of liver enzymes (mainly cholestatic enzymes) and an epidemiologic context of unsafe sexual exposure.
Key Words: Acute Hepatitis, Secondary Syphilis, Syphilitic Hepatitis, Immunocompetent Patient, Sexually Transmitted Infection
Introduction
Syphilis is a sexually transmitted disease caused by Treponema pallidum. Over the last years, its incidence has increased, mainly in people with risky sexual behaviour (1). It has been described as “the great imitator”, because it is a venereal disease with multiorgan involvement. Hepatic involvement is uncommon, but elevation of hepatic enzymes can be found in about 10% of the infected patients, whilst not having any other feature of hepatitis. Clinically relevant syphilitic hepatitis can occur at any phase of the disease. It is estimated that 3% of secondary syphilis cases evolve as hepatitis. Fulminant hepatitis or progression to cirrhosis is rare (2–5).
Case Report
We describe the case of a 41-years-old male that presents to our Emergency Room (ER) due to epigastric pain and anorexia. He is discharged on pantoprazole and sucralfate. Two days later, he develops a non-itchy rash of the trunk and limbs and discontinues the medication. One month later, he returns to the ER due to the persistence of severe epigastric pain, nausea and maintenance of the cutaneous lesions (Figure 1). He denied fever, loss of weight, hypersudoresis, jaundice, diarrhea or adenopathies. He had no significant personal or familiar background, besides history of unprotected sexual relations with multiple males. He denied taking any medication, alcohol, drugs or tobacco consumption. He also denied consumption of protein supplementation, non-prescribed medication or tea consumption.
Figure 1.
Photograph showing non-itchy, non-vesicular, macular, erythematous lesions of the anterior trunk (a) and left trunk (b)
On physical examination, he revealed non-itchy, non-vesicular, maculo-papular, erythematous lesions of the trunk and limbs, with palmo-plantar affection and pain to deep palpation of the epigastric region. Liver was palpable 1cm below costal border, with plain, regular and unpainful palpation. No genital, anal or oral lesions were found. No jaundice or others stigmas of hepatic disease were present.
Analytically, elevation of liver enzymes was found (aspartate aminotransferase 85U/L, alanine aminotransferase 178 U/L, alkaline phosphatase (ALP) 891U/L and gamma-glutamyl transferase 1844U/L), hyperbilirubinemia (1.57mg/dL) due to increase in the direct fraction (0.84mg/dL) and increased C Reactive Protein (4.55mg/dL). Prothrombin time and serum albumin were within normal values. Complete blood cell count was normal. Abdominal echography revealed globous liver, with a small increase in its size, without any other changes. We admitted patient to our ward for etiologic study of a cholestatic hepatitis.
Virologic study revealed immunization by vaccination to HBV and immunization by contact to Cytomegalovirus. Antibodies against HAV, HCV, HEV, HIV, Toxoplasma gondii and Epstein-Barr were negative. Anti-nuclear, anti-smooth muscle, anti-mitochondrial and liver kidney microsomal antibodies were all negative. Serum plasmatic proteins electrophoresis, serum immunoglobulins, Alpha-1 antitrypsin and ceruloplasmina were within normal range. Total cholesterol was 191mg/dL and triglycerides 155mg/dL.
Magnetic resonance cholangiogram showed a slightly increased liver size (17cm in the longest axis in the longitudinal plane), with homogeneous structure, without steatosic infiltration or any other stigma of chronic hepatic disease. No intra or extra hepatic biliary ducts stenosis or dilation were found. Given severe epigastric pain, upper digestive endoscopy was requested. No changes were found in endoscopy.
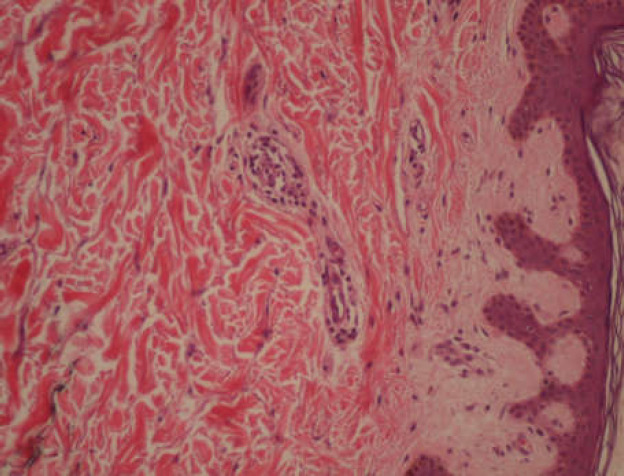
Given the sexual history of our patient and the clinical presentation, syphilis test was performed. VDRL test was reactive (64 dilutions), with positive microhemagglutination assay test (>5120 dilutions). Skin lesions were biopsied which revealed superficial perivascular infiltrate of lymphomonocytic round cells, with rare plasmocytic cells. This result was compatible with syphilitic roseola (Figure 2).
Figure 2.
Histopathological findings – superficial perivascular infiltrate of lymphomonocytic round cells (haematoxylin-eosin x200) (2)
Secondary syphilis was assumed with syphilitic hepatitis. Patient was medicated with a unique dose of intramuscular Benzathine benzylpenicillin (2.4 million units). After treatment, he presented favourable clinic and analytic evolution and was discharged and oriented to our outpatient clinic. Three weeks later, in an office visit, all skin lesions had disappeared (Figure 3). Ten weeks after treatment, liver enzymes were within normal range (Table 1). Nine months after treatment, VDRL was non-reactive and patient continued to present normal liver enzymes and negative HIV test.
Figure 3.
Photograph 3 weeks after treatment with Benzathine benzylpenicillin
Table 1.
Analytical evolution from the initial presentation till 9 months after treatment
| 13/01 | 16/01 | 23/01 | 07/02 | 05/04 | 24/10 | |
|---|---|---|---|---|---|---|
| AST (U/L) | 85 | 52 | 45 | 62 | 34 | 27 |
| ALT (U/L) | 178 | 106 | 87 | 123 | 61 | 31 |
| ALP (U/L) | 891 | 665 | 575 | 251 | 91 | 71 |
| G-GT (U/L) | 1844 | 1489 | 1319 | 577 | 79 | 27 |
| TB (mg/dL) | 1.57 | 1.26 | 1.17 | 0.87 | 1.28 | |
| PT (seconds) | 11.80 | 11.60 | 12.10 | |||
| VDRL | Reactive (64 dilutions) |
Non-reactive |
Note: aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP); gamma-glutamyl transferase (G-GT), Total Bilirubin (TB), Prothrombin time (PT).
Discussion
The etiologic agent of syphilis, Treponema pallidum, can infect any organ. Cutaneous, genital and central nervous system involvements are exhaustively described (6). However, syphilis can have atypical presentations, such as hepatitis. In recent years, most cases of syphilis have been reported in young males who have unprotected sex with males (around 67% of recently reported primary or secondary syphilis) (7–9).
In almost all cases of syphilitic hepatitis, it is common to find a disproportional increase in ALP, when compared to the increase in aminotransferases. (9). Histopathological examination is non-specific. Lymphocytic infiltrate of portal spaces with focal necrosis of peri-portal hepatocytes can be found (8–10). Pathophysiology of hepatic syphilitic lesion is unknown, but it is thought to have been caused by pericholangiolar inflammation present in these situations (4,7). Multisystemic involvement can be justified by an immune-mediated mechanism, such as the host inflammatory response to the infection. Microorganism identification in hepatic biopsy is pathognomonic, yet rarely achievable (11).
In Mullick et al. (2004), the proposed diagnostic criteria for syphilitic hepatitis are as follows: (i) abnormal liver enzyme levels indicating hepatic involvement; (ii) serological evidence for syphilis, with a positive RPR titer and a reactive FTA-Abs result or microhemagglutination assay result positive for T. pallidum (MHA-TP) in conjunction with an acute clinical presentation consistent with secondary syphilis; (iii) exclusion of alternative causes of hepatic damage, such as acute viral hepatitis, use of medication, malignancy, or opportunistic infection; and (iv) improvements in liver enzyme levels following appropriate antimicrobial therapy (7).
In our case, the presence of exanthema and the exclusion of other causes of cholestatic hepatitis raised the suspicion of secondary syphilis. This diagnosis was confirmed by VDRL, MHA-TP and the skin biopsy result. There was no history of primary syphilis. It is important to highlight that genital syphilis lesion is most often unpainful and most of the times does not need any treatment to heal and may not be diagnosed. (10) In the end, the favourable clinical and analytical response to the administration of Benzathine benzylpenicillin confirmed the diagnosis of syphilitic hepatitis, according to Mullick’s diagnostic criteria (7).
With this case, the authors intend to highlight that syphilis (“the great imitator”) should be considered for the differential diagnosis of acute or chronic cholestatic hepatitis. This is particularly important in sexually active patients, because it is reversibly and easily treatable, although it can evolve to fulminant hepatitis (12). This high index of suspicion should include immunocompetent patients.
Funding Sources
The authors declare that there were no external financial sources for this study.
Conflict of interests
The authors declare that they have no conflict of interest.
References
- 1.Division of STD Prevention. Centers for Disease Control and Prevention. Sexually Transmitted Disease (STD) Surveillance 2017. Atlanta, Georgia: U.S. Department of Health and Human Services Centers for Disease Control and Prevention. [2018]. Available from: https://www.cdc.gov/std/stats17/2017-STD-Surveillance-Report_CDC-clearance-9.10.18.pdf.
- 2.Noto P, Del Nonno F, Licci S, Chinello P, Petrosillo N. Early syphilitic hepatitis in an immunocompetent patient: really so uncommon? Int J STD AIDS. 2008;19:65–6. doi: 10.1258/ijsa.2007.007037. [DOI] [PubMed] [Google Scholar]
- 3.Adachi E, Koibuchi T, Okame M, Sato H, Kikuchi T, Koga M, et al. Liver dysfunction in patients with early syphilis: a retrospective study. J Infect Chemother. 2013;19:180–2. doi: 10.1007/s10156-012-0440-5. [DOI] [PubMed] [Google Scholar]
- 4.Baveja S, Garg S, Rajdeo A. Syphilitic Hepatitis: An Uncommon Manifestation of a Common Disease. Indian J Dermatol. 2014;59 doi: 10.4103/0019-5154.127711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubio-Tapia A, Hujoel IA, Smyrk TC, Poterucha JJ. Emerging secondary syphilis presenting as syphilitic hepatitis. Hepatology. 2017;65:2113–5. doi: 10.1002/hep.28974. [DOI] [PubMed] [Google Scholar]
- 6.Adachi E, Koibuchi T, Okame M, Sato H, Imai K, Shimizu S, et al. Case of Secondary Syphilis Presenting with Unusual Complications: Syphilitic Proctitis, Gastritis, and Hepatitis. J Clin Microbiol. 2011;49:4394–6. doi: 10.1128/JCM.01240-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mullick CJ, Liappis AP, Benator DA, Roberts AD, Parenti DM, Simon GL. Syphilitic Hepatitis in HIV-Infected Patients: A Report of 7 Cases and Review of the Literature. Clin Infect Dis. 2004;39:e100–5. doi: 10.1086/425501. [DOI] [PubMed] [Google Scholar]
- 8.Solari PR, Jones C, Wallace MR. Hepatic Lesions with Secondary Syphilis in an HIV-Infected Patient. Case Rep Med. 2014;2014:1–5. doi: 10.1155/2014/604794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang J, Lin S, Wan B, Zhu Y. A Systematic Literature Review of Syphilitic Hepatitis in Adults. J Clin Transl Hepatol. 2018;6:1–4. doi: 10.14218/JCTH.2018.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tolia S, Kassem H, Capatina-Rata A. The Great Impostor: Transaminitis Masking the Coinfection of Syphilis and Human Immunodeficiency Virus. Case Rep Med. 2017;2017 doi: 10.1155/2017/2481961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bork JT, Macharia T, Choi J, Gilliam BL, Buchwald UK. Syphilitic Hepatitis Treated With Doxycycline in an HIV-Infected Patient and Review of the Literature. Sex Transm Dis. 2014;41:507–10. doi: 10.1097/OLQ.0000000000000143. [DOI] [PubMed] [Google Scholar]
- 12.Lo JO, Harrison RA, Hunter AJ. Syphilitic hepatitis resulting in fulminant hepatic failure requiring liver transplantation. J Infect. 2007;54:e115–7. doi: 10.1016/j.jinf.2006.07.005. [DOI] [PubMed] [Google Scholar]