Abstract
Introduction:
Fractures of the upper cervical spine are often but not always amenable to either internal fixation or conservative management using a rigid cervical collar. For all other fractures in this area, management with a halo-vest orthosis is indicated, but it also has limitations. Here, we present an operative alternative to the halo-vest orthosis that provides more secure stability and less complications.
Methods:
Three patients presented to our hospital with atypical fractures of C1 and C2 and were given the choice of either a halo-vest orthosis or secure internal fixation without fusion and accepted the latter. Internal fixation without fusion from occiput to the subaxial spine was performed for all three and then removed-6 months later -after radiologic confirmation of healing.
Results:
All three patients underwent the procedure successfully and achieved and maintained acceptable alignment. Range of motion was preserved, and no intermediate-term issues were observed.
Conclusion:
Spanning internal fixation provides a safe and effective technique in the management of complex upper cervical spine injuries without the drawbacks of using a halo-vest orthosis.
Keywords: Cervical spine, spine fractures, internal fixation
INTRODUCTION
Fractures of the upper cervical spine account for over 45%–50% of all cervical spine trauma.[1,2] Most of these injuries are treated conservatively using a halo-vest orthosis, but the trend toward operative fixation is growing internationally.[3] The rationale behind that global trend is the high complication rates and the questionable efficacy of halo-vest treatment.[4,5,6] Furthermore, the surgeon is occasionally faced with a complex fracture of the Atlas or Axis that neither fusion nor halo-vest immobilization is a good option. The ideal solution would provide better stabilization and less complications-than a halo-vest and would not eliminate motion from the adjacent segments. In this study, we present three cases of upper cervical spine injury where internal fixation was executed as a temporary stabilization measure, achieving the goals mentioned above.
METHODS
Three patients presented to our institution with fractures of C1 or C2 which would normally be managed with a halo-vest orthosis. The benefits and risks of halo-vest immobilization were explained to all patients. All patients were offered surgical treatment as an alternative, and all three accepted surgical treatment and preferred it to halo-vest immobilization.
Surgical technique
The patients were taken to the operating room where general anesthesia was administered. Mayfield frame immobilization was performed in the supine position and the patient was then rolled carefully into the prone position using the Jackson frame. A routine posterior cervical approach from the occiput to C4 followed, limiting the sub-periosteal dissection of the injured vertebrae. Specifically, the insertions of the rectus capitis and the longissimus muscles to C1 and C2 were preserved. Routine subperiosteal dissection of the occiput and subaxial spine allowed for instrumentation occipital plates and lateral mass screws bilaterally. A rod was then placed on each side and fixed to the plates/screws from the occiput to C3/C4 spanning the soft-tissue envelope over C1/C2. Closure was then done in layers, and a rigid cervical collar was applied for further external stabilization. The patient was mobilized the next day and discharged shortly thereafter. The cervical collar was removed at 12 weeks and a computerized tomography (CT) was performed at 6 months. Once healing of the fractures was established, a second operation was done to remove the implants and physical therapy was started 6 weeks following the second operation to regain range of motion and strengthen the cervical musculature.
RESULTS
All patients underwent the procedure successfully without complication. Radiological fusion was obtained in all three, and all had the implants removed 6 months postoperative [Figures 1-3]. A focused physical therapy program-6 weeks after implant removal was mandated with two objectives: Regain cervical motion first, and then strengthen the weak cervical paraspinal musculature. Details of each patient's clinical course are presented in Table.
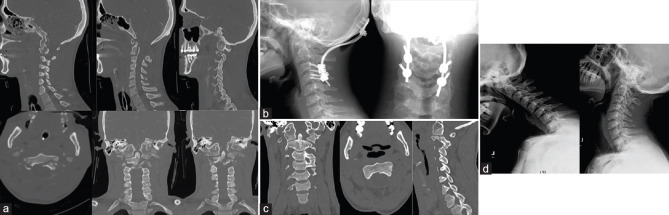
Figure 1.
(a) Patient 1 radiologic presentation: plain roentgenograms and CT. (b) Patient 1 postoperative images. (c) Patient 1 final flexion extension films after removal of implants
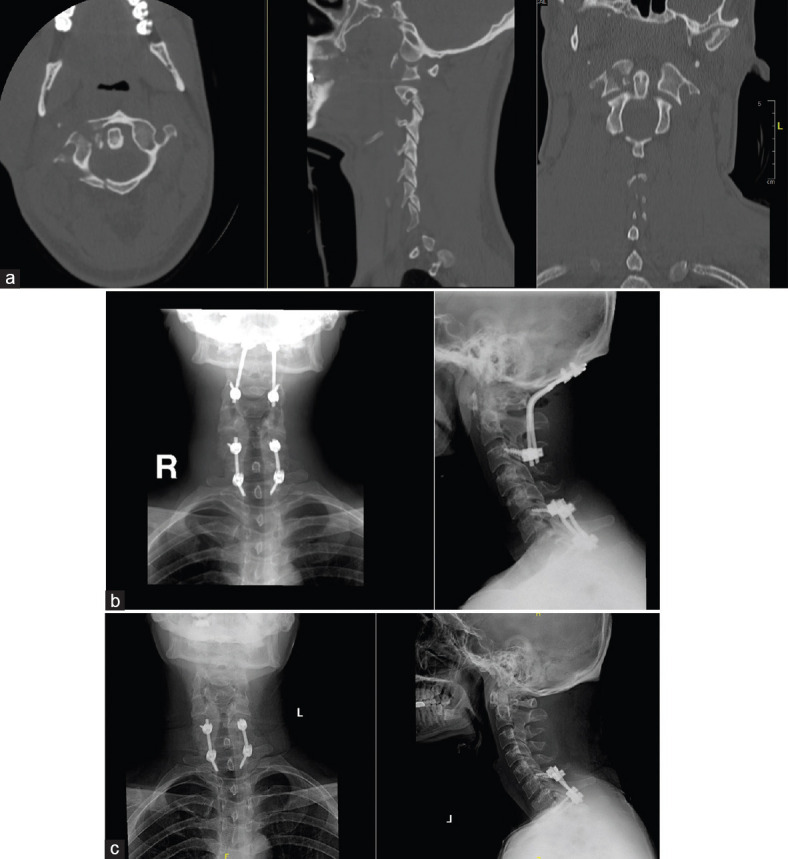
Figure 3.
(a) Patient 3 radiologic presentation: CT. (b) Patient 3 postoperative images. (c) Patient 3 CT showing complete healing of the C2 fracture. (d) Patient 3 flexion-extension radiographs following removal of implants
Table.
Clinical course of the patients in the study
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Age (years) | 53 | 31 | 28 |
| Traumatic event | Motor vehicle collision | Motor vehicle collision | Motor vehicle collision |
| Physical examination | Severe neck pain, neurologically intact | Severe neck pain, neurologically intact | Multiple injuries including brain contusion, facial bone fracture but neurologically intact |
| Imaging | C2 body fracture with anterior displacement, extending to pars interarticularis bilaterally | C1 vertebra anterior and posterior arch fracture with avulsion of transverse ligament tubercle | C2 body fracture extending to pars interarticularis bilaterally + congenital fusion of atlantooccipital joint |
| Postoperative course | Uneventful, discharged day 3 postoperative | Uneventful, discharge was delayed until day 15 due to concurrent femur fracture slowing mobilization | Long hospital stay due to brain injury, but cervical spine injury was managed in a similar matter to the other two cases once the patient regained full mental capacity 17 days after admission and medical stabilization |
| CT evaluation at 6 months | Fracture fully united | Fractures fully united | Fractures fully united |
| Last follow-up | At 2 years, mild limitation in neck rotation but no loss of flexion/extension and no functional deficit | At 18 months, full range of motion regained except for mild loss of rotation possibly due to concurrent C7 fracture treated with a fusion | At 12 months, limitation was only in flexion-extension, but that could be due to congenital atlanto-occipital fusion |
| Figures | Figure 1a-c | Figure 2a-c | Figure 3a-d |
CT - Computed tomography
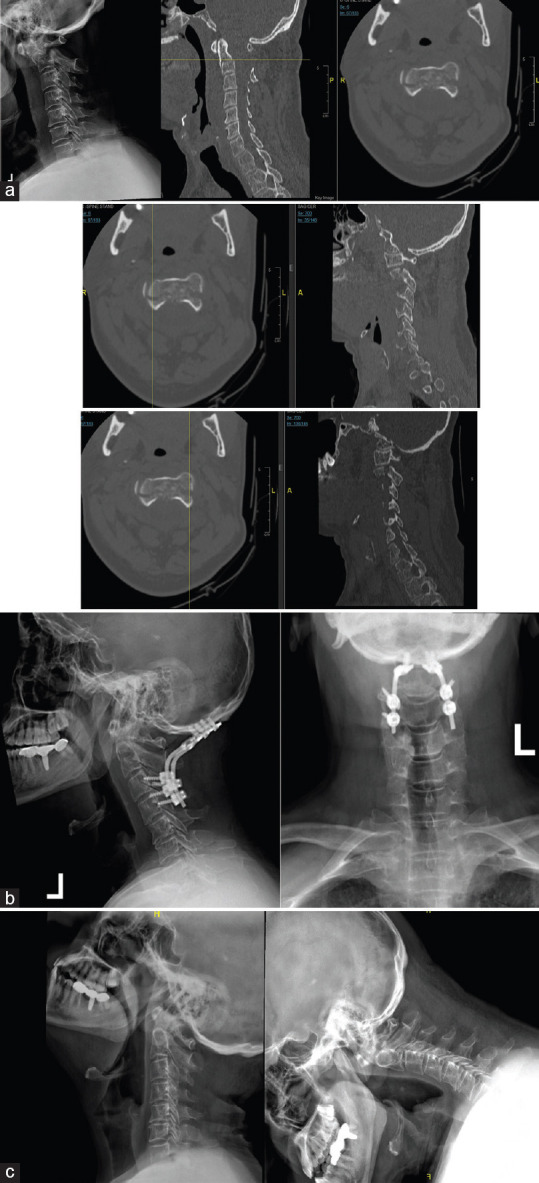
Figure 2.
(a) Patient 2 radiologic presentation: CT. (b) Patient 2 postoperative images. (c) Patient 2 final images after removal of implants
DISCUSSION
Modern operative management of spine fractures evolved from the management of extremity fractures. In the second half of the twentieth century, internal fixation slowly took over the conservative treatment of extremity fractures. This was mostly due to better outcomes and less complications compared with plaster cast or traction immobilization associated with direct reduction and stable fixation.[7,8] This effect made its way into spine surgery with the introduction of modern spinal implants. With certain fractures, internal fixation was not possible, and spanning external and later internal fixation methods were developed as definitive treatment or as temporary measures until the patient's condition allowed internal fixation.[9] Spanning internal fixation, however, has less complications than external fixation and provides better stability biomechanically.[10]
The halo-vest orthosis was first introduced in the 1950s for the treatment of children with poliomyelitis, cases of cervical spine trauma in addition to other conditions.[11] Although a revolutionary device when first introduced, even in their initial report the authors discussed the issues of inadequate fixation, pin site infections, and discomfort reported by the patients. At the time, modern implants were decades away from development and widespread use. Nowadays the halo-vest is still utilized in many centers across the globe, although less frequently than in previous decades. The complications associated with its use have been well described in the literature.[11,12,13,14,15,16] Particularly in the elderly, its use is associated with increased incidence of pneumonia and increased mortality.[4,17,18] More recent reports have challenged this,[3,16,19] but it remains a concern for the clinician. From a biomechanical perspective, the halo-vest orthosis confers little stability to the fractured cervical spine,[20,21] and a non-invasive halo maybe just as good.[22] Reports directly comparing internal fixation with halo-vest immobilization have been shown superior fusion rates, better alignment, less pain, and earlier return to work for both Atlas and Axis fractures.[23,24]
There have been a few similar studies in the literature recently reporting for temporary internal fixation for upper cervical spine fractures.[25,26,27] These initial reports prove that certain fractures of the Atlas and Axis are better served with internal fixation without biologic fusion. The technique we report in our series confirms that and opens the door for further larger comparative series.
CONCLUSION
Temporary spanning occipitalcervical fixation is a viable alternative to either operative fusion or halo-vest immobilization for the management of upper cervical spine fractures. It provides instant, maintained rigid stability not possible with halo-vest immobilization to these fractures with the complete loss of motion associated with definitive fusion surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Passias PG, Poorman GW, Segreto FA, Jalai CM, Horn SR, Bortz CA, et al. Traumatic Fractures of the Cervical Spine: Analysis of Changes in Incidence, Cause, Concurrent Injuries, and Complications Among 488,262 Patients from 2005 to 2013. World Neurosurg. 2018;110:e427–e437. doi: 10.1016/j.wneu.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 2.Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: An evidence-based narrative review of management. Europ Spine J. 2011;20:195–204. doi: 10.1007/s00586-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DePasse JM, Palumbo MA, Ahmed AK, Adams CA, Jr, Daniels AH. Halo-vest immobilization in elderly odontoid fracture patients: Evolution in treatment modality and in-hospital outcomes. Clin Spine Surg. 2017;30:E1206–10. doi: 10.1097/BSD.0000000000000483. [DOI] [PubMed] [Google Scholar]
- 4.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60:199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 5.Shin JJ, Kim SJ, Kim TH, Shin HS, Hwang YS, Park SK. Optimal use of the halo-vest orthosis for upper cervical spine injuries. Yonsei Med J. 2010;51:648–52. doi: 10.3349/ymj.2010.51.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan L, Ou D, Huang X, Pang M, Chen XX, Yang B, et al. Surgery vs. conservative treatment for type II and III odontoid fractures in a geriatric population: A meta-analysis. Medicine. 2019;98:e10281. doi: 10.1097/MD.0000000000010281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perren SM, Russenberger M, Steinemann S, Müller ME, Allgöwer M. A dynamic compression plate. Acta Orthop Scand Suppl. 1969;125:31–41. [PubMed] [Google Scholar]
- 8.Glenn JN, Miner ME, Peltier LF. The treatment of fractures of the femur in patients with head injuries. J Trauma. 1973;13:958–61. doi: 10.1097/00005373-197311000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): The results of a prospective, standardized protocol. J Orthop Trauma. 2005;19:448–55. doi: 10.1097/01.bot.0000171881.11205.80. [DOI] [PubMed] [Google Scholar]
- 10.Wolf JC, Weil WM, Hanel DP, Trumble TE. A biomechanic comparison of an internal radiocarpal-spanning 2.4-mm locking plate and external fixation in a model of distal radius fractures. J Hand Surg Am. 2006;31:1578–86. doi: 10.1016/j.jhsa.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 11.Nickel VL, Perry J, Garrett A, Heppenstall M. The halo. A spinal skeletal traction fixation device. J Bone Joint Surg Am. 1968;50:1400–9. [PubMed] [Google Scholar]
- 12.Baum JA, Hanley EN, Jr, Pullekines J. Comparison of halo complications in adults and children. Spine. 1989;14:251–2. doi: 10.1097/00007632-198903000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Dormans JP, Criscitiello AA, Drummond DS, Davidson RS. Complications in children managed with immobilization in a halo vest. J Bone Joint Surg Am. 1995;77:1370–3. doi: 10.2106/00004623-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Glover AW, Zakaria R, May P, Barrett C. Overtightening of halo pins resulting in intracranial penetration, pneumocephalus, and epileptic seizure. Int J Spine Surg. 2013;7:e42–4. doi: 10.1016/j.ijsp.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menon KV, Al Rawi AE, Taif S, Al Ghafri K, Mollahalli KK. Orbital roof fracture and orbital cellulitis secondary to halo pin penetration: Case report. Global Spine J. 2015;5:63–8. doi: 10.1055/s-0034-1384818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Middendorp JJ, Slooff WB, Nellestein WR, Oner FC. Incidence of and risk factors for complications associated with halo-vest immobilization: A prospective, descriptive cohort study of 239 patients. J Bone Joint Surg Am. 2009;91:71–9. doi: 10.2106/JBJS.G.01347. [DOI] [PubMed] [Google Scholar]
- 17.Horn EM, Theodore N, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK. Complications of halo fixation in the elderly. J Neurosurg Spine. 2006;5:46–9. doi: 10.3171/spi.2006.5.1.46. [DOI] [PubMed] [Google Scholar]
- 18.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: A death sentence? J Trauma. 2005;59:350–6. doi: 10.1097/01.ta.0000174671.07664.7c. [DOI] [PubMed] [Google Scholar]
- 19.Isidro S, Molinari R, Ikpeze T, Hernandez C, Mahmoudi MS, Mesfin A. Outcomes of halo immobilization for cervical spine fractures. Global Spine J. 2019;9:521–6. doi: 10.1177/2192568218808293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koch RA, Nickel VL. The halo vest: An evaluation of motion and forces across the neck. Spine (Phila Pa 1976) 1978;3:103–7. [PubMed] [Google Scholar]
- 21.Glaser JA, Myers MA, McComis GP, Simons MP, Butler VH, Rust PF. Cervical motion after adding a posterior pad to the halo vest. Am J Orthop (Belle Mead NJ) 2000;29:557–62. [PubMed] [Google Scholar]
- 22.DiPaola CP, Sawers A, Conrad BP, Horodyski M, DiPaola MJ, Del Rossi G, et al. Comparing cervical spine motion with different halo devices in a cadaveric cervical instability model. Spine. 2009;34:149–55. doi: 10.1097/BRS.0b013e3181920e7c. [DOI] [PubMed] [Google Scholar]
- 23.Kim MK, Shin JJ. Comparison of radiological and clinical outcomes after surgical reduction with fixation or halo-vest immobilization for treating unstable atlas fractures. Acta Neurochir (Wien) 2019;161:685–93. doi: 10.1007/s00701-019-03824-5. [DOI] [PubMed] [Google Scholar]
- 24.Kim SK, Shin JJ, Kim TH, Shin HS, Hwang YS, Park SK. Clinical outcomes of halo-vest immobilization and surgical fusion of odontoid fractures. J Korean Neurosurg Soc. 2011;50:17–22. doi: 10.3340/jkns.2011.50.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Theologis AA, Deviren V, Tay B. Temporary fusionless posterior occipitocervical fixation for a proximal junctional type II odontoid fracture after previous C2-pelvis fusion: Case report, description of a new surgical technique, and review of the literature. Europ Spine J. 2017;26(Suppl 1):243–8. doi: 10.1007/s00586-017-5093-8. [DOI] [PubMed] [Google Scholar]
- 26.Yuan S, Wei B, Tian Y, Yan J, Xu W, Wang L, et al. Posterior temporary C1-2 fixation for 3-part fractures of the axis (odontoid dens and Hangman fractures) Medicine (Baltimore) 2018;97:e12957. doi: 10.1097/MD.0000000000012957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo Q, Deng Y, Wang J, Wang L, Lu X, Guo X, et al. Comparison of clinical outcomes of posterior C1-C2 temporary fixation without fusion and C1-C2 fusion for fresh odontoid fractures. Neurosurgery. 2016;78:77–83. doi: 10.1227/NEU.0000000000001006. [DOI] [PubMed] [Google Scholar]