Abstract
The advances in mobile technologies and applications are driving the transformation in health services delivery globally. Mobile phone penetration is increasing exponentially in low-and middle-income countries, hence using mobile phones for healthcare services could reach more people in resource-limited settings than the traditional forms of healthcare provision. The review presents recent literature on facilitators and barriers of implementing mHealth for disease screening and treatment support in low-and middle-income countries. We searched for relevant literature from the following electronic databases: MEDLINE; CINAHL with full text via EBSCOhost; Science Direct; PubMed; Google Scholar and Web of Science using the keywords for relevant studies. We searched for published studies from 2015 to August 2020 with no language limitations. A total of 721 articles identified, 125 articles met the inclusion criteria and were included in the qualitative synthesis. The review demonstrates relevant facilitators for the implementation of mHealth, which includes knowledge, attitudes, and perceptions of stakeholders on the use of mHealth and the performance of mHealth for disease diagnosis in low and-middle-income countries. Barriers and challenges hindering the implementation of mHealth applications were also identified. We proposed a framework for improving the implementation of mHealth for disease screening and treatment support in low-and middle-income countries.
Keywords: Mobile health applications, Disease screening, Disease diagnosis, Treatment support and low-and middle-income countries
Mobile health applications; Disease screening; Disease diagnosis; Treatment support and low-and middle-income countries.
1. Introduction
The advances in mobile technologies and applications are driving the transformation in health services delivery globally. Mobile health (mHealth) is defined as the use of voice calls, short message service (SMS), wireless transmission of data, and mobile phone applications to support healthcare provision [1]. Other forms of technologies being employed to support healthcare delivery are telehealth, telemedicine, telecare, virtual health, digital health, and others. Telehealth is defined as the use of medical information that could be exchanged from one point to another via electronic communication to promote the health conditions of patients [2]. It also includes a wide range of technologies and services to give patient care and enhance the healthcare delivery system entirely. Telemedicine is also defined as the provision of remote clinical services to patients without an in-person visit through the use of electronic communication (computers, video, phone calls, messaging) in both audio and virtual means [3]. Telecare refers to the provision of healthcare at-a-distance via the use of technology to support vulnerable people [4]. Telecare provides a 24-hour connection between individuals in their homes and trained Carelink call-handlers at a 24-hour monitoring center [4]. Digital health could also be referred to as the use of wearable devices, mobile health, health information technology, telehealth, telemedicine to improve healthcare access, reduce costs and inefficiencies, and increase quality care for patients [5]. Virtual health involves clinical care and professional partnership via telehealth, telemedicine, and collaboration at-a-distance to link physicians, patients, care teams, and other healthcare professionals to give clinical services, assist patient self-management and co-ordinate care [6].
Mobile health technologies have been recognized as a cheaper and easier approach to provide high-quality healthcare services to patients in low-and middle-income countries (LMICs) with its fragile health systems, high prevalence of tropical diseases, high rate of infectious diseases, high mortality rate, and many others [7]. Although mHealth activities are mostly predominant in high-income countries (HICs) for transforming healthcare [7], there is a rise in the integration of mobile health into the existing eHealth services in LMICs [8]. Mobile phone penetration and its acceptability are increasing exponentially in low-and middle-income countries [9], hence using mobile phones for healthcare services could reach more people in resource-limited settings than the traditional forms of disease control. The conventional way of using cell phone text message components for communication has now shifted, and it's being used to support healthcare provision [10].
Mobile health technology has been identified as a means to help achieve universal health coverage, particularly in resource-limited settings of HICs [11, 12]. Prior studies have shown that mobile health applications have been extensively used in transforming healthcare services in HICs in terms of screening and diagnoses of infectious and non-infectious diseases such as COVID-19, HIV/AIDS, Tuberculosis, cancer, hypertension, and many others [13, 14, 15]. Other studies conducted in some HICs focused on mobile health applications to support treatment and management of patients' conditions in terms of medication adherence, appointment reminders, disease surveillance, tracking of emergencies, and others [11, 16, 17, 18]. Recent studies have demonstrated that mobile devices have improved regular communication and monitoring between healthcare workers and their patients in HICs [19, 20, 21]. These have led to an increase in the quality of healthcare provision and a reduction in the cost of accessing healthcare services in HICs, especially in this era of COVID-19 pandemic [16, 18]. Hence, this review seeks to present an overview of recent literature on the use of mHealth, facilitators, and barriers of implementing mHealth for disease screening and treatment support in LMICs.
1.1. Aim
The purpose of this study is to review recent literature that highlights the use of mHealth applications, facilitators, and barriers and challenges of implementing mHealth for disease screening and treatment support in LMICs.
2. Materials and methods
2.1. Design
A narrative review approach was employed to allow a comprehensive analysis of published literature from electronic-based journal articles, grey literature, and books. In situations where data aggregation is difficult due to the several different studies that are being examined, a narrative review method is considered to be effective.
2.2. Literature search strategy
For this narrative review, we searched published studies from 2015 to August 2020 with no language limitations. A thorough electronic search was conducted to identify relevant literature from the following databases: MEDLINE and CINAHL with full-text via EBSCOhost; Science Direct; PubMed; Google Scholar and Web of Science. The search terms used were: ‘‘mobile health applications’’, ‘‘disease screening’’, ‘‘disease diagnosis’’, ‘‘treatment support’’ and ‘‘low-and middle-income countries’’. These keywords were used to include published articles on knowledge, attitudes, and perceptions of users of mHealth, the accuracy of disease diagnosis with mHealth, screening of diseases with mHealth, treatment support of patients’ conditions using mHealth, and others. The searches yielded 721 articles. Two hundred and six duplicates were removed, and 312 articles were also excluded. Seventy-eight articles did not meet the eligibility criteria. Leaving 125 articles for review. For the included studies, 40 articles were quantitative, 35 qualitative articles, 4 mixed method articles, 40 review articles, and 6 grey literature articles.
3. Overview
3.1. Use of mHealth for pandemic management in HICs
Recently, during the outbreaks of Ebola and Severe Acute Respiratory Syndrome (SARS), mHealth applications exhibited its potential in screening, detecting, and monitoring such global epidemics [14, 22, 23]. Mobile health technologies and applications have been utilized in this current COVID-19 pandemic and other infectious diseases in most HICs as compared to LMICs [24, 25, 26]. Currently, a study in Canada has revealed that mHealth applications have been utilized for screening, diagnosis, and monitoring of COVID-19 cases [14]. In some HICs, mHealth applications are being used for contact tracing of COVID-19 cases to support the global fight against this outbreak [24, 27, 28]. Other studies in China have identified mHealth as a tool for screening and treatment of COVID-19 patients to help reduce the risk of transmission to other patients and healthcare professionals [28, 29]. Researches showed that mHealth applications have the potential to enhance the early detection of this highly infectious COVID-19 disease compared to the traditional form of disease diagnosis and treatment [30, 31].
Studies in the US and China have found that mHealth applications are being deployed currently to assist preliminary screening and early identification of possible COVID-19 infected persons [25, 32]. Again, a survey in the US illustrated that mHealth applications have been integrated into the healthcare delivery system to screen health workers of symptoms of COVID-19 to support the global fight against this pandemic [26]. Research has shown that in Switzerland, mHealth applications assisted medical professionals to screen COVID-19 cases for early detection and isolation of infected persons to slow the transmission and reduce the rate of infection [33]. In Singapore, an mHealth app was used as an essential tool by public health officials to screen and track down individuals exposed to COVID-19 infected patients to help break the infection chain [34].
3.2. Use of mHealth applications in healthcare in LMICs
The advent of mHealth interventions has a significant transformative effect on healthcare delivery, particularly in treatment support, diagnostic purposes, health monitoring, data accuracy, and many others [1, 35, 36, 37]. The integration of mobile health technology into the current clinical services is providing new different channels of quality healthcare delivery [37]. This new technology can engage the health system, health workers, and patients in promoting quality healthcare services [37]. The following are some of the significant benefits of mHealth in LMICs: mHealth for screening infectious diseases, non-infectious diseases, disease surveillance, medication and treatment compliance, appointment reminders, communication between health providers and patients, and maternal and child health [38, 39, 40, 41, 42, 43].
3.2.1. mHealth for screening infectious diseases
Mobile health technologies and applications have been recognized as an avenue that could support the screening of infectious diseases such as COVID-19, Ebola, Severe Acute Respiratory Syndrome (SARS), HIV, and others [44, 45, 46]. In Brazil, a study revealed that healthcare authorities have encouraged the use of digital health such as mHealth for remote screening and detection of COVID-19 suspected cases [38]. A similar study in India has demonstrated that mHealth solutions are being used by frontline health workers to screen potential COVID-19 cases to support early identification [47]. Recently, during the Zika virus outbreak in Brazil, mHealth applications were deployed as tools for diagnosing and screening potential cases to help control the rapid spread of the virus [48].
The recent Ebola and Zika virus epidemics in West Africa and Southern America have illustrated the utility of mHealth applications for promoting early screening and testing of infected patients [48, 49]. In sub-Saharan Africa, during the Ebola outbreak mHealth technologies and applications helped frontline health workers in screening and diagnosing potential cases [22, 23]. Sutcliffe et al. reported that mHealth interventions could improve the early infant diagnosis of HIV infections in Zambia [45]. In addition, a study in South Africa found that mHealth interventions have improved HIV testing rates among vulnerable populations in rural communities [50]. Furthermore, a similar study conducted in Malaysia showed that mHealth applications supported the diagnosis or detection of tuberculosis (TB) diseases in real-time [51]. In Southern America and some of parts of Asia, mHealth applications have been utilized to screen infectious diseases a lot more as compared to sub-Saharan Africa due to their higher advancement in technology.
3.2.2. mHealth for screening non-infectious diseases
Mobile health applications are been utilized to could support the screening of non-infectious diseases like hypertension, diabetes, cancer, and several others [52, 53]. Studies in LMICs suggested that mHealth applications supported the screening of cancer conditions in rural communities [52, 54, 55]. Other studies in LMICs illustrated that mHealth applications were useful in screening cardiovascular disease conditions among the people living in remote areas [53, 56]. Similar studies conducted in Latin America and India indicated that mHealth applications were deployed to help diagnose cardiometabolic conditions and non-communicable diseases [57, 58]. In Brazil, mHealth applications have been used for supporting the diagnosis of chest pain among patients [59]. Moreover, a survey in Nigeria found that frontline health workers used mHealth applications for diagnosing diseases as well as making differential diagnoses of diseases on patients' conditions [44]. The higher advancement of technology in India has made the use of mHealth applications for the screening of non-infectious diseases more prevalent as compared to other countries like Nepal, Tanzania, Nigeria, and Brazil.
3.2.3. mHealth for disease surveillance
In LMICs, surveillance of infectious and non-infectious disease outbreaks is fragile due to logistical, financial, and infrastructural constraints [60]. However, the advent of mHealth interventions has decreased the costs associated with disease surveillance to a larger extent and have given a more effective way to perform surveillance in such countries [60]. For instance, in the current COVID-19 global pandemic, mHealth applications have been deployed for surveillance activities to help control the transmission rate [61]. Watkins et al. suggested that mHealth interventions have the potential to provide lifesaving information to the most remote and resource-limited settings in LMICs [62]. It is essential to note that early access to disease reports by health workers could lead to rapid and timely identification as well as control of disease outbreaks [62]. In LMICs, mHealth interventions have widely been used to promote surveillance initiatives for both infectious and non-infectious diseases [63].
A study in India demonstrated that mHealth applications were utilized for contact tracing procedures which are a globally adopted surveillance system [47]. A similar study has revealed that countries such as Ghana, Czech Republic, Columbia, Iceland, Hungary, and others have deployed mHealth applications for robust surveillance of COVID-19 cases to help control this pandemic [64]. Research indicated that in Zambia, mHealth used by health workers have the potential to enhance surveillance activities and improve outreach services in hard-to-reach communities [60]. Studies have shown that disease surveillance has been strengthened with the introduction of mHealth designed for data collection, data analysis, and responding timely to emergency outbreaks [65, 66]. Again, studies in Kenya and India found that mHealth technologies were deployed for disease surveillance purposes to promote healthcare delivery [66, 67]. The available evidence presented shows that mHealth applications have improved disease surveillance across these several countries.
3.2.4. mHealth for medication and treatment compliance
Poor treatment and medication compliance could lead to an increase in mortality rates, high multi-drug resistance, and several others [60, 68]. Research has demonstrated that one of the effective ways to overcome non-compliance to treatment and medication procedures is the use of mHealth applications [60]. There are several cases where mHealth applications in medication and treatment compliance have enhanced adherence in most LMICs. In LMICs, mHealth interventions promoted adherence to cardiovascular disease medications and treatment procedures [40]. Also, a study in Asia illustrated that text message reminders from healthcare professionals improved medication adherence in bipolar 1 disorder patients [69]. Studies in Mexico, Argentina, India, Vietnam, Kenya, and South Africa demonstrated that mHealth reminders supported healthcare workers in ensuring that HIV infected patients complied with antiretroviral adherence [70, 71, 72, 73, 74].
A similar study in Pakistan showed that mHealth applications encouraged stroke patients to adhere to medication procedures [75]. Researches have shown that in sub-Saharan Africa, medication adherence, and compliance with antiretroviral therapy (ART) improved significantly by introducing mHealth interventions [76, 77]. Moreover, in Thailand, mHealth applications deployed by health professionals assisted tuberculosis patients to observe treatment and medication adherence [78]. Similar studies have also demonstrated that mHealth interventions had increased compliance to the treatment procedure of tuberculosis (TB) in Southern Africa [77, 79]. In addition, a survey in Nigeria revealed that mHealth interventions helped hypertensive patients adhere to medication procedures [80]. The results of the studies presented from these countries show that mHealth applications have equally enhanced medication and treatment compliance.
3.2.5. mHealth for appointment reminders
Studies have found that mHealth applications were used to encourage appointment adherence among patients [77, 79, 81]. In LMICs, mHealth applications such as SMS were sent to HIV-positive pregnant women to remind them of their appointment in promoting quality healthcare provision [41]. A study conducted in Nigeria demonstrated that text message reminders were sent to women to attend postpartum care after delivery to enhance PNC visits [82]. Researches found that in Southern Africa, mHealth interventions were utilized to decrease missed clinic appointments [79, 83]. In Palestinian, mHealth solutions promoted adherence to clinic appointments particularly for non-communicable disease patients [84].
Moreover, in Mozambique, a study illustrated that mHealth applications helped HIV/TB patients to avoid missing their medical appointments to promote quality healthcare delivery [77]. Also, cancer patients were interested in receiving appointment reminders via mHealth applications to help them adhere to their clinical appointments in South Africa [81]. In Guatemala, patients were willing to use cellular phones for their clinic appointment reminders to promote adherence to ART treatment [85]. Another study in India found that mHealth reminders supported cardiovascular disease patients to adhere to their clinical appointments [86]. Again, in Argentina, patients suffering from Chagas disease received appointment reminders via mHealth applications from healthcare workers [87]. Furthermore, a survey conducted in Kenya indicated that mHealth applications such as SMS and phone calls improved the uptake of HIV tests by increasing appointment attendance among patients [88]. The findings from these countries suggest that mHealth applications have improved appointment reminders of patients.
3.2.6. mHealth for communication between healthcare providers and patients
Recent studies have revealed that the use of mHealth applications has improved significantly the relationship between healthcare providers and their patients [33, 77]. For instance, studies conducted in LMICs illustrated that mHealth interventions could enhance patient-health provider communication aimed at improving self-management of diabetes [42, 63]. Research has shown that mHealth has the potential to strengthen postnatal care in several rural communities in LMICs [89]. Again, in LMICs, regular communication via mHealth between health professionals and their patients has improved the quality of treatment support given to patients and increased patient-clinician relationships [37]. A study in India suggested that mHealth applications were used for communication with tuberculosis patients during care and treatment procedures [90].
In South Africa, mHealth applications assisted in coordinating care, speed-up patients referrals, encouraged medication, and clinic appointment adherence via communication [62]. Moreover, in Saudi Arabia, mHealth communication helped patients to constantly engage their healthcare providers remotely in managing their mental health conditions [91]. A survey conducted in Nigeria illustrated that mHealth applications could provide cost-effective solutions to communication barriers between patients and their healthcare providers in rural clinics [92]. Furthermore, in Malawi, mHealth could help improve the availability of scientific and medical research to physicians, enhancing communication between physicians and their patients, and encouraging networking among physicians [93]. The findings from these countries demonstrate that mHealth applications promoted communication between healthcare providers and their patients.
3.2.7. mHealth for maternal and child health
The consistent provision of quality maternal and child health services is a significant challenge for LMICs where most of the population dwells in rural communities [94, 95]. Low utilization of antenatal care (ANC), delivery services, and postnatal care (PNC) have been identified as major contributing factors for high maternal and child mortality rates in LMICs [94]. Mobile health applications are recognized as tools that could address some of these challenges to help improve quality health services rendered to expectant mothers and neonates [95, 96, 97]. For instance, studies conducted in some LMICs revealed that mHealth interventions are one of the practical solutions needed to improve maternal, neonatal, and child health services [8, 43]. Other studies conducted in LMICs found that mHealth applications are considered as tools that could strengthen PNC given to mothers and neonates in rural areas to promote quality healthcare [89, 96]. Research has shown that in LMICs, mHealth applications have the potential to enhance ANC and PNC services particularly targeted at changing the behavior of pregnant women and mothers in the postnatal period [98].
According to Atnafu et al., mHealth interventions on maternal and child health services have increased the number of antenatal care visits by expectant mothers and the percentage of delivery attended by healthcare workers in Ethiopia [94]. A study in Ghana demonstrated that mHealth applications improved maternal and neonatal care among the rural poor by providing them with information on postpartum depression and education on essential vaccinations and management of critical childhood diseases [60]. Studies conducted in India and Bangladesh showed that mHealth applications promoted quality maternal, neonatal, and child health services, particularly in hard-to-reach communities [99, 100]. In Nigeria revealed that mHealth applications could change the behavior of pregnant women and improve the quality of maternal and child health services provided by frontline community health workers [101]. The results from the studies across these countries identified mHealth applications as solutions that could improve maternal and child health, particularly for resource-limited settings.
3.3. Risk of mHealth applications in healthcare in LMICs
Although research available indicates the potential benefits of mHealth applications, there are some risks associated with the use of these technologies. A study conducted in LMICs revealed that some patients are non-adherent to medication procedures though they are using mHealth applications for self-management [102]. Also, patients receiving text messages only without follow-ups are unable to get the necessary medical assistance to actively manage their health conditions at home [102, 103]. Other studies further demonstrated that the use of mHealth applications alone may not be as effective in promoting patient self-management as anticipated [104, 105]. In LMICs, a study found that the use of mHealth technologies by some HIV patients indicated a higher-risk of non-adherence to antiretroviral treatment [106]. Research has demonstrated some potential risks associated with mHealth applications are the wrong amount of medications administered by patients and inaccurate interpretation of data by both patients and healthcare professionals [107].
Other risks associated with the use of mHealth interventions could be data transmission problems and wrong insertion of data by patients that may affect their health conditions when medical decisions are taken based on such data [108, 109]. Also, a study in LMICs has shown that using mHealth applications remotely could pose a risk in situations where are drug-drug interactions and patients suffering from hypoglycemia that could lead to complications [110]. A similar study conducted in LMICs has illustrated that some mHealth apps designed for the opioid conversion of dosage or detection of melanoma showed poor accuracy as they did not follow evidence-based guidelines [111]. Also, poor security of patients' data could pose a major risk for patients and healthcare professionals using mHealth apps to support healthcare delivery [110]. In addition, research has shown that mHealth apps that carry out complex tasks such as drug dosage calculations may have a greater risk potential because of programming errors [112]. Furthermore, mHealth apps that have out-of-date content or contain inaccurate content could increase the risk of causing harm to potential users [113].
3.4. mHealth patient pathway in LMICs
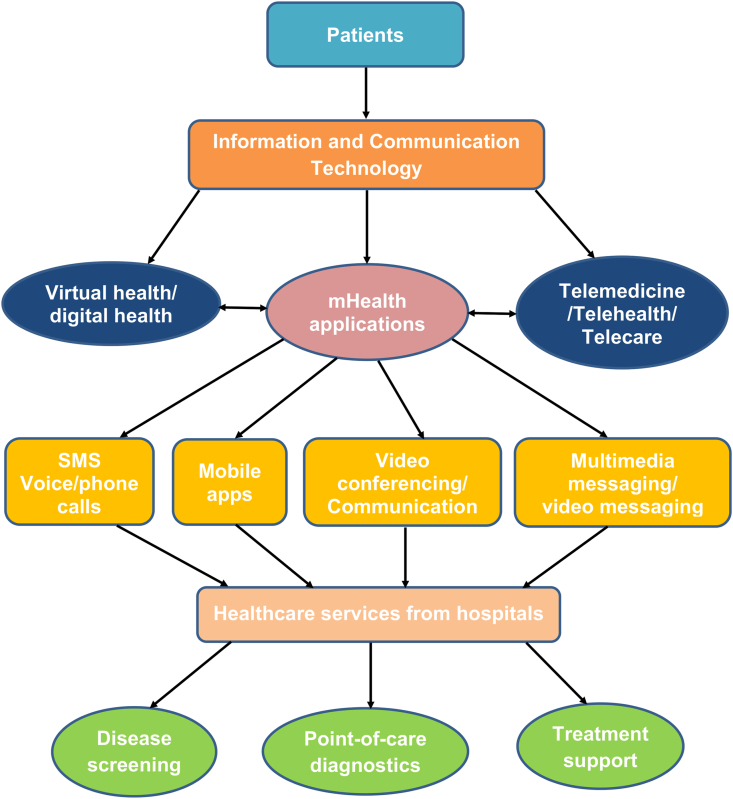
Currently, the hospital setting is becoming a dynamic environment where clinical staff, patients, and healthcare systems are constantly in motion. The daily operations of healthcare depend on a complex architecture of information, clinical staff, processes as well as physical assets [114]. In such an environment where clinical information is siloed and clinical processes occur independently, duplication and waste are unavoidable [114]. This affects quality, efficiency, patient satisfaction, cost of care, and others. Healthcare systems or hospitals are being re-engineered with knowledge and technologies in promoting quality care delivery [115]. mHealth technology is one of the key strategies needed in finding clinical solutions across the range of operations in hospitals. With the integration of mHealth applications, health facilities are creating new patient-provider interactions, sharing and capturing clinical knowledge at point-of-care, and addressing issues of cost and quality [115]. mHealth innovations are being driven by systemic gaps in healthcare delivery such as inadequate health infrastructure, insufficiently skilled health professionals, lack of specialty physicians, and others [116]. Patients are now able to use mHealth for point-of-care diagnostics, disease screening, and treatment procedures of conditions due to the uniqueness of wireless technology and the imperative desire to transform healthcare delivery [117]. Patients could access healthcare services such as diagnostics, screening, medication adherence, appointment reminders, follow-ups, and others with mHealth innovations due to the advancement of technologies. Figure 1 demonstrates a patient pathway of using mHealth for healthcare delivery.
Figure 1.
A proposed patient pathway of using mHealth for accessing healthcare services.
3.5. Facilitators for implementing mHealth applications
Facilitators of mHealth applications in LMICs are associated with financial support, sound policy decision, leadership abilities, connectivity, capacity building, and others [118]. Facilitators identified toward implementing mHealth applications for disease screening and treatment support in LMICs are knowledge, attitudes, and perceptions of stakeholders on the use of mHealth and the performance of mHealth for disease diagnosis [119, 120, 121].
3.5.1. Knowledge, attitudes, and perceptions of stakeholders on mHealth applications
Knowledge, attitudes, and perceptions of stakeholders on the use of mHealth applications to support the provision of quality healthcare are essential. In this review, healthcare stakeholders are referred to health workers, patients, health managers, health insurance companies, employers, pharmaceutical firms, non-government organizations, governments, and others involved in healthcare services [7]. A survey conducted in an LMIC revealed that health professionals believe that mHealth interventions can promote accuracy and efficiency in healthcare delivery [37]. Studies have demonstrated that health professionals and other users of mHealth generally had positive attitudes toward the use of mHealth to promote quality healthcare delivery in sub-Saharan Africa [122, 123].
A study conducted in Ghana found that some healthcare stakeholders’ knowledge on the use of mHealth interventions to support healthcare is low [124]. In Mozambique, research showed that healthcare workers and patients have considerable expertise in using mHealth interventions to support healthcare delivery [77]. Atnafu et al. reported that health extension workers exhibited good knowledge and a highly favorable attitude towards the use of mHealth interventions to promote maternal health services in Ethiopia [94]. In Nigeria, medical doctors had a very high knowledge of the use of mHealth applications to support the treatment and management of patients' conditions [125]. Studies in Saudi Arabia demonstrated that healthcare workers had poor attitudes and perceptions towards the use of mHealth for disease screening and treatment support [126, 127]. Moreover, in Iran, a study indicated that older users had negative attitudes toward the use of mHealth applications for disease screening and treatment [128].
In Ethiopia, research has found that diabetic patients showed their willingness to receive healthcare services via mHealth interventions [129]. Prior studies demonstrated that health workers perceived mHealth interventions as supportive in giving accurate diagnoses of diseases during consultations and treatment procedures in Tanzania and Senegal [119, 120]. According to Laktabai et al., both patients and health professionals are comfortable using mHealth interventions to support healthcare delivery in Kenya [121]. A study in Ghana revealed that patients are confident that their medical information's privacy would be protected with the use of mHealth applications [130]. Similar studies showed that primary healthcare workers exhibited positive perceptions concerning the relevance and benefits of introducing mHealth interventions to support healthcare delivery in Nigeria and Ghana [122, 130].
In addition, studies carried out in Kenya, and Mozambique revealed that some health workers and patients felt that using mHealth interventions to support healthcare was comfortable and convenient [80, 131]. Again, a study conducted in South Africa demonstrated some health workers' interest in using mHealth interventions to support healthcare but raised concerns about privacy [81]. The findings presented from some of the studies in these countries illustrated that users of mHealth applications have considerable knowledge on the use of mHealth and are comfortable in using such technologies in practice. This may due to the high penetration rate of mobile phones in sub-Saharan Africa and the relatively higher level of awareness of such technologies used in promoting healthcare delivery. The findings further revealed that in sub-Saharan Africa, users showed a positive attitude towards the use of mHealth as compared to those from Saudi Arabia and the Philippine with poor attitudes. This may be due to less than 6% of healthcare providers and patients using mHealth applications to support healthcare in Saudi Arabia and the Philippine.
3.5.2. Performance of mHealth applications for disease diagnosis
The performance of mHealth in this review has been defined as the use of mHealth devices to give an accurate diagnosis of disease conditions in a population [131]. Research suggested that some mHealth devices offer analytical sensing abilities, which can be explored when typical tools designed for diagnostic purposes cannot be accessed quickly [132]. A survey carried out in an LMIC showed that mHealth interventions had demonstrated a significant promise to effectively diagnose neglected tropical diseases (NTDs) in resource-poor settings [133]. Studies conducted in rural settings of Ghana and Côte d’Ivoire illustrated that mHealth devices were used to diagnose Schistosoma mansoni, Schistosoma haematobium accurately, and other Intestinal Protozoa infections to assist health workers in providing quality healthcare services [134, 135]. Jaworek-Korjakowska et al. reported that mHealth applications were also utilized to accurately diagnose or detect Malignant Melanoma cases among individuals in Poland [136]. A study in Madagascar has shown that mHealth devices were deployed to accurately diagnose soil-transmitted helminth infections to promote healthcare delivery [137].
Again, in Botswana and Madagascar, studies have demonstrated that mHealth devices were also used to accurately screen cervical cancer and Human Papillomavirus-positive conditions for early treatment to be initiated [138, 139]. In India, a study revealed that mHealth applications have been deployed to accurately diagnose cardiometabolic diseases [140]. According to Coulibaly et al., mHealth interventions were incorporated into the routine practice of community-based screening activities to detect or diagnose malaria infections in Côte d’Ivoire [141]. Also, in Senegal, mHealth interventions have been used to accurately screen cardiovascular conditions in low-income backgrounds to support the provision of quality healthcare services [142]. The results from the studies across these countries revealed that mHealth applications have been utilized to accurately diagnose and screen some diseases to promote quality healthcare delivery.
3.6. Barriers and challenges relating to the implementation of mHealth applications
Despite the global increase in mHealth applications to support universal health coverage, several barriers and challenges are affecting the adoption of such interventions by healthcare stakeholders [7]. Barriers and challenges related to the implementation of mHealth across LMICs include geographical access and internet connectivity barriers, policy/regulatory barriers, funding challenges, limited healthcare workers competence, limited awareness of mHealth services, inadequate information and communication technology (ICT) infrastructure, poor architecture and standardization, and many others [143, 144, 145, 146, 147].
3.6.1. Geographical access and internet connectivity barriers
Geographical access is one of the significant barriers affecting the implementation of mHealth technologies and applications for disease screening and treatment support across resource-limited settings in LMICs [148]. Past studies have demonstrated that many LMICs populations are based in rural settings, and access to healthcare requires travelling long distances with high transportation costs and poor road networks [145, 146]. This may prevent several patients from seeking healthcare and can affect their health conditions. mHealth interventions may be one of the tools to help people in hard-to-reach communities access healthcare. Due to unreliable mobile network coverage or insufficient cellular signal, unstable internet services, and a lack of continuous power supply, they are unable to access healthcare via mHealth [144, 148, 149]. In many LMICs, bandwidth for internet connectivity is minimal, and the cost involved in internet connectivity remains expensive since the majority of people cannot afford [149]. Research has shown that rural communities in LMICs have feeble network connections used in transmitting data, which may sometimes affect the quality of images from reported cases [144]. Many patients have short battery life for their mobile phones due to lack of power supply, particularly for patients in hard-to-reach communities. Again, research revealed that in LMICs, six out of ten people do not have access to electricity, and even those who have access experience continuous blackouts [150]. To this end, implementing and accessing mHealth services pose a challenge for such patients.
3.6.2. Policy/regulatory barriers
In many LMICs, weak policy regulations are guiding mHealth developments, implementation, and accessibility as compared to the Data Protection Regulation for countries within the European Union (EU) and the Health Insurance Portability and Accessibility Act (HIPAA) in the US [151, 152, 153]. Several LMICs do not have well developed national policies, regulatory frameworks that are essential components for the establishment of standard protocols, common technical infrastructure, and interoperability systems to adopt mHealth in healthcare [154]. In LMICs, where mobile phones may be shared between family members, there are huge concerns about data breaches. Also, weak policy regulations and guidelines on patients' data security and privacy in LMICs may affect many patients' desire to access healthcare through mHealth [155]. Moreover, recent studies in LMICs have also suggested that fragile policy guidelines and regulatory frameworks may lead to compromising data integrity, especially when text messages are sent via insecure protocols, storing data on third party servers and weak log systems [152, 153]. Furthermore, research has demonstrated that in some LMICs, there is no robust legal framework needed to guide health data transfer, data storage, identify access control and medical liability that are key to implementing mHealth interventions [151].
3.6.3. Funding challenges
One of the significant barriers to mHealth intervention is the inconsistent funding of mHealth applications in many LMICs by governments. This leaves such countries to rely on development partners, multinational organizations, and non-governmental organizations (NGOs) for assistance solely [145, 154]. Designing, developing, and maintaining ICT applications infrastructure is highly expensive; the costs involved are mostly higher than the budgetary allocations dedicated to the health sectors in several LMICs [7]. Also, mHealth infrastructure financing requires systematic coordination and collaboration among several partners within the public and private sectors of the economy [154]. If this fails, implementing mHealth applications will be a significant difficulty. In LMICs, health facilities are unable to partner with other governmental agencies and the private sector to mobilize enough resources needed to support mHealth [154]. This makes the implementation of mHealth a major challenge. Research has demonstrated that individuals who use mHealth interventions in some LMICs are charged for utilizing such services [154, 155]. When the costs attached to using mHealth services are not affordable, most patients, especially those in hard-to-reach communities, will not be able to access the services [156, 157]. Hence that may affect their health conditions.
3.6.4. Limited awareness of mHealth
One of the significant barriers affecting the implementation of mHealth is the limited awareness of most stakeholders on the potential benefits of using mHealth to support healthcare delivery [145]. Some healthcare stakeholders do not know the potential benefits of incorporating mHealth in healthcare provision, especially LMICs [7]. Also, the accessibility and utilization of mHealth services may be limited if the general public or patients are not aware of the numerous benefits of mHealth [146]. Given this, there should be medium to long-term strategic plans in health sectors of LMICs to develop mHealth infrastructure to create more awareness to support healthcare delivery [7].
3.6.5. Limited healthcare workers competence in mHealth
Studies have indicated that in LMICs, there are inadequate ICT trained health professionals to man these mHealth interventions to support universal health coverage [154, 158]. Most health professionals and other stakeholders do not have sufficient knowledge in information technology (IT) needed to deploy and effectively manage mHealth interventions to promote quality healthcare delivery [154]. Also, the general public or patients expect healthcare professionals to respond timely to any request via mHealth and should have the requisite competencies to provide such services [77]. This underpins the need for healthcare professionals to be given additional and efficient training in using and managing any mHealth interventions.
3.6.6. Inadequate information and communication technology infrastructure (ICT)
Several LMICs have a lot of existing mHealth interventions that are on small scale levels and fragmented with minimal coverage due to poor ICT infrastructure [145, 147]. ICT infrastructure in various forms is the essential requirement for mHealth interventions, but in most LMICs, the coverage and reliability of such support are a significant challenge [154]. The poor ICT infrastructure within the healthcare industry can also be attributed to the inability of most ministries of communication, finance, and technology to support and finance the deployment of ICT infrastructure to promote mHealth [147, 159]. Similarly, the poor ICT infrastructure can be ascribed to the weak deployment of a network infrastructure that is a prerequisite for any ICT strategy in any sector, including the healthcare industry [143]. Research has shown that inadequate ICT infrastructure makes the implementation of mHealth in resource-limited settings a significant challenge affecting patients' health conditions [146].
3.6.7. Poor architecture and standardization
The main goal of mHealth applications is to make them become part of the healthcare systems so that their data can be distributed across different healthcare applications and connect to electronic healthcare systems as well as national or international programs [144]. However, studies have demonstrated that the lack of interoperability of mHealth is another barrier in implementing mHealth interventions for improving the provision of quality healthcare [143, 147]. Other research has also revealed that there are no typical architecture and standardization for the many existing mHealth interventions, especially in some LMICs [158]. The absence of a typical technical architecture that enables interoperability and scale-up of mHealth interventions makes the implementation of such programs very difficult. The lack of integration of mHealth interventions with the relevant national health systems poses accessibility and utilization challenges for populations in hard-to-reach communities [147, 154]. Again, many LMICs are confronted with the problem of integrating mHealth into the existing eHealth initiatives and the overarching health and poor ICT infrastructure to ensure their operationalization [147].
4. Discussion
The review provides an overview of the literature on the benefits of mHealth applications; risks of using mHealth applications; facilitators and barriers toward implementing mHealth for disease screening and treatment support in LMICs. Our study shows numerous significant evidence on the benefits of mHealth for screening infectious diseases, non-infectious diseases, disease surveillance, medication and treatment compliance, appointment reminders, communication between health providers and patients, and maternal and child health [38, 40, 41, 42, 47, 55, 60, 63, 96, 160]. The results from the studies show that mHealth applications are used for screening infectious and non-infectious diseases most often in India than in other countries in South America and sub-Saharan Africa probably due to the higher technology advancement. The findings also demonstrate that mHealth applications improved disease surveillance, medication and treatment compliance, appointment reminders, communication, and maternal and child health across many LMICs.
The review also suggests that healthcare stakeholders have considerable knowledge on the use of mHealth applications and are comfortable in using such technologies [122, 123, 125]. This could be due to some form of education they might have received on mHealth technologies and applications. The findings further indicate that in sub-Saharan Africa users show favorable attitudes toward the use of mHealth as compared to the poor attitude across Saudi Arabia and the Philippine [122, 123, 125, 126, 127]. This is because of the higher mobile phone penetration rate and some level of awareness creation of such technologies in sub-Saharan Africa. In Saudi Arabia and Philippine, there is an extremely small percentage of health workers using mHealth applications and a low level of awareness of such technologies. Again, the review illustrates that mHealth devices provide accurate diagnostic procedures for a few disease conditions across LMICs to promote quality healthcare services [133, 136]. The review further illustrates some risks associated with the use of mHealth such as non-adherence to antiretroviral treatment, the wrong amount of medications, inaccurate data interpretation, wrong insertion of data by patients, and others across many LMICs [106, 107, 108].
Despite the rising interest in mHealth in recent times, the literature suggests that access to mHealth applications remains a challenge and requires urgent attention. The research also reveals some potential challenges and barriers that hinder the implementation of mHealth for disease screening and treatment support in LMICs. These are geographical access and internet connectivity barrier, policy/regulatory barrier, limited awareness of mHealth applications, inadequate ICT infrastructure, limited healthcare workers' competence in mHealth, funding challenges, poor architecture, and standardization in LMICs [143, 145, 146, 147, 154, 155, 158]. Besides, the literature further illustrates that these challenges and barriers do not act in isolation and hence require the attention of all relevant healthcare stakeholders to help improve the implementation of mHealth interventions.
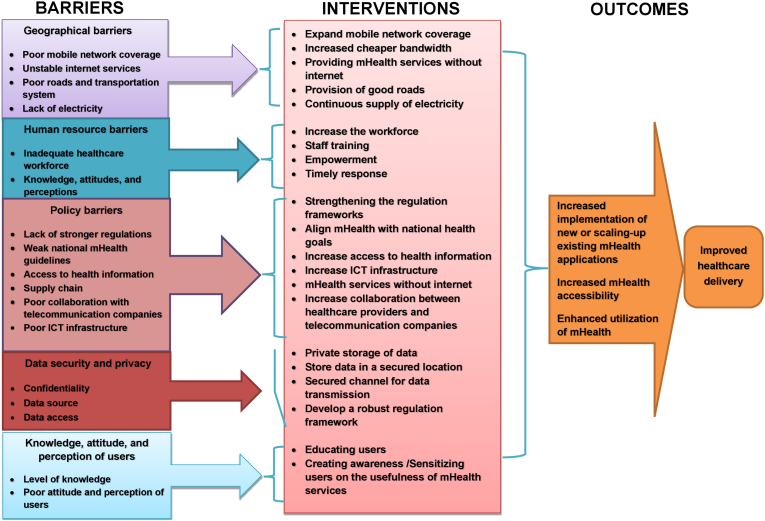
Considering the numerous challenges and barriers confronting the implementation of mHealth in LMICs, we propose a framework for improving the implementation of mHealth for disease screening and treatment support in LMICs (Figure 2). The proposed framework is basically to address the identified challenges and barriers that may arise when implementing mHealth in LMICs. This proposed framework will also improve the implementation of mHealth to help achieve universal health coverage, particularly for hard-to-reach populations. The building blocks in this framework include geographical barriers, human resource barriers, policy barriers, data security and privacy, and knowledge, attitudes, and perceptions of users [153, 154]. This framework seeks to help implement mHealth in resource-limited settings by expanding mobile network coverage, supplying stable internet services, and providing mHealth without the internet and at no cost to patients. Also, expanding electricity coverage to rural communities and continuously supplying electricity will sustain rural health workers and their patients' interest in mHealth.
Figure 2.
A proposed framework for improving the implementation of mHealth for disease screening and treatment support in LMICs.
The availability of adequately trained human resources is further required for increasing accessibility, utilization, and implementation of mHealth applications. Since health professionals are not traditionally taught to use mHealth to provide healthcare, it is essential to train these people and empower them to respond timely to patients' needs in this regard. Similarly, to implement mHealth, there is the need to develop more robust regulation frameworks, secure channels for data transmission, and secure location for data storage. In doing this in LMICs, the data protection policy established by either the US or EU could be adopted to support the development of mHealth to strengthen patients' data security, privacy, and confidentiality. The evidence available shows that adopting such policies could improve the security of patients’ data leading to an increase in the utilization of mHealth for disease screening and treatment support in LMICs. Others include building and expanding more ICT infrastructure with increased collaboration between health providers and telecommunication companies, align new and existing mHealth with national health goals, and many others. Furthermore, this framework seeks to suggest that potential mHealth users should be educated to create more awareness of the existence and usefulness of mHealth applications to help promote its implementation.
5. Conclusion
The use of mHealth applications for achieving universal health coverage, particularly for hard-to-reach populations, cannot be underestimated. The review illustrates several significant usefulness of mHealth applications to promote quality healthcare delivery in LMICs. This review identifies some risks associated with the use of mHealth applications for disease screening and treatment support in LMICs. The study also shows limited research in the literature of knowledge, attitudes, and perceptions of stakeholders on the use of mHealth for disease screening and treatment support in LMICs. In addition, the review suggests limited research in the literature on the use of mHealth for diagnostic accuracy of diseases in LMICs. Furthermore, the study demonstrates several barriers and challenges of implementing mHealth for disease screening and treatment support in LMICs. Therefore, we proposed a framework for improving the implementation of mHealth for disease screening and treatment support in LMICs. Finally, we also recommend that future research should focus on the performance of mHealth on health outcomes in LMICs.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors wish to thank the University of KwaZulu-Natal for giving us all the necessary resources in developing this review.
References
- 1.Babirye D., Shete P.B., Farr K., Nalugwa T., Ojok C., Nantale M. Feasibility of a short message service (SMS) intervention to deliver tuberculosis testing results in peri-urban and rural Uganda. J. Clin. Tuberculos. Other Mycobacter. Dis. 2019;16:100110. doi: 10.1016/j.jctube.2019.100110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tuckson R.V., Edmunds M., Hodgkins M.L. Telehealth. New Engl. J. Med. 2017;377(16):1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 3.Hollander J.E., Carr B. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 4.Lu Y., Li L., Peng H., Yang Y. An enhanced biometric-based authentication scheme for telecare medicine information systems using elliptic curve cryptosystem. J. Med. Syst. 2015;39(3):32. doi: 10.1007/s10916-015-0221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ronquillo Y., Meyers A., Korvek S.J. StatPearls Publishing; 2020. Digital Health. StatPearls [Internet] [PubMed] [Google Scholar]
- 6.Webster P. Virtual health care in the era of COVID-19. J. Lancet. 2020;395(10231):1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO . 2016. Global diffusion_of_eHealth-_Making_universal_health_coverage_achievable Report on the Third Global Survey on eHealth Geneva World Health Organization; p. 156. [Google Scholar]
- 8.Sondaal S.F.V., Browne J.L., Amoakoh-Coleman M., Borgstein A., Miltenburg A.S., Verwijs M. Assessing the effect of mHealth interventions in improving maternal and neonatal care in low-and middle-income countries: a systematic review. PloS One. 2016;11(5) doi: 10.1371/journal.pone.0154664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.GSMA The Mobile Economy. 2019;56 [Google Scholar]
- 10.Castelnuovo G., Zoppis I., Santoro E., Ceccarini M., Pietrabissa G., Manzoni G.M. Managing chronic pathologies with a stepped mHealth-based approach in clinical psychology and medicine. Front. Psychol. 2015;6:407. doi: 10.3389/fpsyg.2015.00407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Sappagh S., Ali F., Hendawi A., Jang J.-H., Kwak K.-S. A mobile health monitoring-and-treatment system based on the integration of the SSN sensor ontology and the HL7 FHIR standard. BMC Med. Inf. Decis. Making. 2019;19(1):97. doi: 10.1186/s12911-019-0806-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palmer M.J., Barnard S., Perel P., Free C. Mobile phone-based interventions for improving adherence to medication prescribed for the primary prevention of cardiovascular disease in adults. Cochrane Database Syst. Rev. 2018;6:Cd012675. doi: 10.1002/14651858.CD012675.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma A., Mentz R.J., Granger B.B., Heitner J.F., Cooper L.B., Banerjee D. Utilizing mobile technologies to improve physical activity and medication adherence in patients with heart failure and diabetes mellitus: rationale and design of the TARGET-HF-DM Trial. Am. Heart J. 2019;211:22–33. doi: 10.1016/j.ahj.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 14.Alwashmi M.F. The use of digital health in the detection and management of COVID-19. Int. J. Environ. Res. Publ. Health. 2020;17(8):2906. doi: 10.3390/ijerph17082906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schnall R., Bakken S., Rojas M., Travers J., Carballo-Dieguez A. mHealth technology as a persuasive tool for treatment, care, and management of persons living with HIV. AIDS Behav. Med. 2015;19(2):81–89. doi: 10.1007/s10461-014-0984-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiang N., Guo M., Amico K.R., Atkins L., Lester R.T. Interactive two-way mHealth interventions for improving medication adherence: an evaluation using the behaviour change wheel framework. JMIR Mhealth Uhealth. 2018;6(4):e87. doi: 10.2196/mhealth.9187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henry B.L., Quintana E., Moore D.J., Garcia J., Montoya J.L. Focus groups inform a mobile health intervention to promote adherence to a Mediterranean diet and engagement in physical activity among people living with HIV. BMC Publ. Health. 2019;19(1):101. doi: 10.1186/s12889-018-6386-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zha P., Qureshi R., Porter S., Chao Y.-Y., Pacquiao D., Chase S. Utilizing a mobile health intervention to manage hypertension in an underserved community. West. J. Nurs. Res. 2020;42(3):201–209. doi: 10.1177/0193945919847937. [DOI] [PubMed] [Google Scholar]
- 19.Palmer M.J., Henschke N., Villanueva G., Maayan N., Bergman H., Glenton C. Targeted client communication via mobile devices for improving sexual and reproductive health. Cochrane Database Syst. Rev. 2020;(8) doi: 10.1002/14651858.CD013680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santo K., Redfern J. The potential of mHealth applications in improving resistant hypertension self-assessment, treatment, and control. Curr. Hypertens. Rep. 2019;21(10):81. doi: 10.1007/s11906-019-0986-z. [DOI] [PubMed] [Google Scholar]
- 21.Hardinge M., Rutter H., Velardo C., Shah S.A., Williams V., Tarassenko L. Using a mobile health application to support self-management in chronic obstructive pulmonary disease: a six-month cohort study. BMC Med. Inf. Decis. Making. 2015;15(1):46. doi: 10.1186/s12911-015-0171-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bempong N.-E., De Castañeda R.R., Schütte S., Bolon I., Keiser O., Escher G. Precision global health–the case of Ebola: a scoping review. J. Glob. Health. 2019;9(1) doi: 10.7189/jogh.09.010404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tom-Aba D., Nguku P.M., Arinze C.C., Krause G. Assessing the concepts and designs of 58 mobile apps for the management of the 2014-2015 West Africa Ebola outbreak: systematic review. JMIR Publ. Health Surv. 2018;4(4):e68–e. doi: 10.2196/publichealth.9015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kleinman R.A., Merkel C. Digital contact tracing for COVID-19. CMAJ. 2020 doi: 10.1503/cmaj.200922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rao A.S.S., Vazquez J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone-based survey in the populations when cities/towns are under quarantine. Infect. Contr. Hosp. Epidemiol. 2020:1–18. doi: 10.1017/ice.2020.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang H., Dimitrov D., Simpson L., Singh B., Plaks N., Penney S. A web-based, mobile responsive application to screen healthcare workers for COVID symptoms: descriptive study. MedRxiv. 2020 doi: 10.2196/19533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Filer J., Gheorghiu D. Test, track, and trace: how is the NHSX Covid app performing in a hospital setting? medRxiv. 2020 [Google Scholar]
- 28.Cheng W., Hao C. Case-initiated COVID-19 contact tracing using anonymous notifications. JMIR mHealth uHealth. 2020;8(6) doi: 10.2196/20369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao Y., Liu R., Zhou Q., Wang X., Huang L., Shi Q. Application of telemedicine during the coronavirus disease epidemics: a rapid review and meta-analysis. medRxiv. 2020 doi: 10.21037/atm-20-3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hong Z., Li N., Li D., Li J., Li B., Xiong W. Telemedicine during the COVID-19 pandemic: experiences from Western China. J. Med. Internet Res. 2020;22(5) doi: 10.2196/19577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu L., Gu J., Shao F., Liang X., Yue L., Cheng Q. Application and preliminary outcomes of remote diagnosis and treatment during the COVID-19 outbreak: retrospective cohort study. JMIR mHealth uHealth. 2020;8(7) doi: 10.2196/19417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yasaka T.M., Lehrich B.M., Sahyouni R. Peer-to-Peer contact tracing: development of a privacy-preserving smartphone app. JMIR mHealthuHealth. 2020;8(4) doi: 10.2196/18936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zamberg I., Manzano S., Posfay-Barbe K., Windisch O., Agoritsas T., Schiffer E. A mobile health platform to disseminate validated institutional measurements during the COVID-19 outbreak: utilization-focused evaluation study. JMIR Publ. Health Surveill. 2020;6(2) doi: 10.2196/18668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cho H., Ippolito D., Yu Y.W. Contact tracing mobile apps for COVID-19: privacy considerations and related trade-offs. arXiv. 2020 preprint arXiv:11511. [Google Scholar]
- 35.Bitsaki M., Koutras C., Koutras G., Leymann F., Steimle F., Wagner S. ChronicOnline: implementing a mHealth solution for monitoring and early alerting in chronic obstructive pulmonary disease. Health Inf. J. 2017;23(3):197–207. doi: 10.1177/1460458216641480. [DOI] [PubMed] [Google Scholar]
- 36.Kaunda-Khangamwa B.N., Steinhardt L.C., Rowe A.K., Gumbo A., Moyo D., Nsona H. The effect of mobile phone text message reminders on health workers' adherence to case management guidelines for malaria and other diseases in Malawi: lessons from qualitative data from a cluster-randomized trial. Malar. J. 2018;17(1):481. doi: 10.1186/s12936-018-2629-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adepoju I.O., Albersen B.J., De Brouwere V., van Roosmalen J., Zweekhorst M. mHealth for clinical decision-making in sub-Saharan Africa: a scoping review. JMIR Mhealth Uhealth. 2017;5(3):e38. doi: 10.2196/mhealth.7185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caetano R., Silva A.B., Guedes A.C.C.M., Paiva CCNd, Ribeiro GdR., Santos D.L. Challenges and opportunities for telehealth during the COVID-19 pandemic: ideas on spaces and initiatives in the Brazilian context. Cad. Saúde Pública. 2020;36 doi: 10.1590/0102-311x00088920. [DOI] [PubMed] [Google Scholar]
- 39.Abaza H., Marschollek M. mHealth application areas and technology combinations: a comparison of literature from high and low/middle-income countries. J. Methods Inf. Med. 2017;56(Suppl 1):e105. doi: 10.3414/ME17-05-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khonsari S., Subramanian P., Chinna K., Latif L.A., Ling L.W., Gholami O. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. Eur. J. Cardiovasc. Nurs. 2015;14(2):170–179. doi: 10.1177/1474515114521910. [DOI] [PubMed] [Google Scholar]
- 41.Kerrigan A., Kaonga N.N., Tang A.M., Jordan M.R., Hong S.Y. Content guidance for mobile phone short message service (SMS)-based antiretroviral therapy adherence and appointment reminders: a review of the literature. AIDS Care. 2019;31(5):636–646. doi: 10.1080/09540121.2018.1549723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alshahrani A., editor. Self-Management and Diabetes Mellitus mHealth, a Glance at the Present and a Glimpse into the Future. ICIMTH; 2019. [DOI] [PubMed] [Google Scholar]
- 43.Barron P., Pillay Y., Fernandes A., Sebidi J., Allen R. The Mom Connect mHealth initiative in South Africa: early impact on the supply side of MCH services. J. Publ. Health Pol. 2016;37(2):201–212. doi: 10.1057/s41271-016-0015-2. [DOI] [PubMed] [Google Scholar]
- 44.Yahya H. Healthcare-related smartphone use among doctors in hospitals in Kaduna, Nigeria–A Survey. Niger. J. Clin. Pract. 2019;22(7):897. doi: 10.4103/njcp.njcp_454_18. [DOI] [PubMed] [Google Scholar]
- 45.Sutcliffe C.G., Thuma P.E., van Dijk J.H., Sinywimaanzi K., Mweetwa S., Hamahuwa M. Use of mobile phones and text messaging to decrease the turnaround time for early infant HIV diagnosis and notification in rural Zambia: an observational study. BMC Pediatr. 2017;17:1–9. doi: 10.1186/s12887-017-0822-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Udugama B., Kadhiresan P., Kozlowski H.N., Malekjahani A., Osborne M., Li V.Y. Diagnosing COVID-19: the disease and tools for detection. ACS Nano. 2020 doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 47.Bassi A., Arfin S., John O., Jha V. An overview of mobile applications (apps) to support the coronavirus disease-2019 response in India. Indian J. Med. Res. 2020 doi: 10.4103/ijmr.IJMR_1200_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ahmadi S., Bempong N.-E., De Santis O., Sheath D., Flahault A. The role of digital technologies in tackling the Zika outbreak: a scoping review. J. Publ. Health Epidemiol. 2018;2:20. [Google Scholar]
- 49.Danquah L.O., Hasham N., MacFarlane M., Conteh F.E., Momoh F., Tedesco A.A. Use of a mobile application for Ebola contact tracing and monitoring in northern Sierra Leone: a proof-of-concept study. BMC Infect. Dis. 2019;19(1):810. doi: 10.1186/s12879-019-4354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Govender K., Beckett S., Masebo W., Braga C., Zambezi P., Manhique M. Effects of a short message service (SMS) intervention on reduction of HIV risk behaviours and improving HIV testing rates among populations located near roadside wellness clinics: a cluster randomised controlled trial in South Africa, Zimbabwe, and Mozambique. AIDS Behav. 2019;23(11):3119–3128. doi: 10.1007/s10461-019-02427-6. [DOI] [PubMed] [Google Scholar]
- 51.Shabut A.M., Tania M.H., Lwin K.T., Evans B.A., Yusof N.A., Abu-Hassan K.J. An intelligent mobile-enabled expert system for tuberculosis disease diagnosis in real-time. J. Exp. Syst. Appl. 2018;114:65–77. [Google Scholar]
- 52.Zhang D., Advani S., Waller J., Cupertino A.-P., Hurtado-de-Mendoza A., Chicaiza A. Mobile technologies and cervical cancer screening in low-And middle-income countries: a systematic review. JCO Glob. Oncol. 2020;6:617–627. doi: 10.1200/JGO.19.00201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Younes J., Darashkevich L. 2017. Portable Heart Disease Diagnostic Systems “Pulse”. [Google Scholar]
- 54.Bhatt S., Evans J., Gupta S. Barriers to the scale of digital health systems for cancer care and control in Last-Mile settings. J. Glob. Oncol. 2017;4:1–3. doi: 10.1200/JGO.2016.007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bhatt S., Isaac R., Finkel M., Evans J., Grant L., Paul B. Mobile technology and cancer screening: lessons from rural India. J. Glob. Health. 2018;8(2) doi: 10.7189/jogh.08.020421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Raghu A, Devarsetty P, Peiris D, Clifford G, Tarassenko L. Mobile Health for Cardiovascular Disease Risk Screening and Management in Resource-Constrained Environments.
- 57.Beratarrechea A., Diez-Canseco F., Irazola V., Miranda J., Ramirez-Zea M., Rubinstein A. Use of m-health technology for preventive interventions to tackle cardiometabolic conditions and other non-communicable diseases in Latin America- challenges and opportunities. Prog. Cardiovasc. Dis. 2016;58(6):661–673. doi: 10.1016/j.pcad.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 58.Majumdar A., Kar S.S., Ganesh Kumar S., Palanivel C., Misra P. mHealth in the prevention and control of non-communicable diseases in India: current possibilities and the way forward. J. Clin. Diagnos. Res.: J. Clin. Diagn. Res. 2015;9(2):LE06. doi: 10.7860/JCDR/2015/11555.5573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Farah S., Andréa B.R., Silva RCd, Monteiro A. Telecardiology on the diagnostic support of chest pain in twenty-two emergency care units (UPA 24h) in the state of Rio de Janeiro. Int. J. Cardiovasc. Sci. 2019;32(2):158–162. [Google Scholar]
- 60.Eilu E. Current and Emerging mHealth Technologies. Springer; 2018. Improving access to health services in sub-Saharan Africa using mobile and wireless technologies; pp. 225–240. [Google Scholar]
- 61.Vokinger K.N., Nittas V., Witt C.M., Fabrikant S.I., von Wyl V. Digital health and the COVID-19 epidemic: an assessment framework for apps from an epidemiological and legal perspective. Swiss Med. Wkly. 1920;2020:150. doi: 10.4414/smw.2020.20282. [DOI] [PubMed] [Google Scholar]
- 62.Watkins J.A., Goudge J., Gómez-Olivé F.X., Huxley C., Dodd K., Griffiths F. mHealth text and voice communication for monitoring people with chronic diseases in low-resource settings: a realist review. BMJ Glob. Health. 2018;3(2) doi: 10.1136/bmjgh-2017-000543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abaza H., Marschollek M. mHealth application areas and technology combinations: a comparison of literature from high and low/middle-income countries. Methods Inf. Med. 2017;56(Suppl 1):e105. doi: 10.3414/ME17-05-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jalabneh R., Zehra Syed H., Pillai S., Hoque Apu E., Hussein M.R., Kabir R. Use of mobile phone apps for contact tracing to control the COVID-19 pandemic: a literature review. J. Anwarul. 2020 [Google Scholar]
- 65.Mtema Z., Changalucha J., Cleaveland S., Elias M., Ferguson H.M., Halliday J.E. Mobile phones as surveillance tools: implementing and evaluating a large-scale intersectoral surveillance system for rabies in Tanzania. PLoS Med. 2016;13(4) doi: 10.1371/journal.pmed.1002002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kazi D.S., Greenough P.G., Madhok R., Heerboth A., Shaikh A., Leaning J. Using mobile technology to optimize disease surveillance and healthcare delivery at mass gatherings: a case study from India's Kumbh Mela. J. Publ. Health. 2017;39(3):616–624. doi: 10.1093/pubmed/fdw091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Toda M., Njeru I., Zurovac D., Tipo S.O., Kareko D., Mwau M. Effectiveness of a mobile short-message-service–based disease outbreak alert system in Kenya. Emerg. Infect. Dis. 2016;22(4):711. doi: 10.3201/eid2204.151459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Castelnuovo B. Review of compliance with anti-tuberculosis treatment and risk factors for defaulting treatment in Sub Saharan Africa. Afr. Health Sci. 2010;10(4) [PMC free article] [PubMed] [Google Scholar]
- 69.Menon V., Selvakumar N., Kattimani S., Andrade C. Therapeutic effects of mobile-based text message reminders for medication adherence in bipolar I disorder: are they maintained after intervention cessation? J. Psychiatr. Res. 2018;104:163–168. doi: 10.1016/j.jpsychires.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 70.DeSilva M., Vu C.N., Bonawitz R., Van Lam N., Gifford A.L., Haberer J. The Supporting Adolescent Adherence in Vietnam (SAAV) study: study protocol for a randomized controlled trial assessing an mHealth approach to improving adherence for adolescents living with HIV in Vietnam. Trials. 2019;20(1):1–13. doi: 10.1186/s13063-019-3239-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stankievich E., Malanca A., Foradori I., Ivalo S., Losso M. Utility of mobile communication devices as a tool to improve adherence to antiretroviral treatment in HIV-infected children and young adults in Argentina. Pediatr. Infect. Dis. J. 2018;37(4):345–348. doi: 10.1097/INF.0000000000001807. [DOI] [PubMed] [Google Scholar]
- 72.Pérez-Sánchez I.N., Candela Iglesias M., Rodriguez-Estrada E., Reyes-Terán G., Caballero-Suárez N.P. Design, validation and testing of short text messages for an HIV mobile-health intervention to improve antiretroviral treatment adherence in Mexico. AIDS Care. 2018;30(sup1):37–43. doi: 10.1080/09540121.2018.1524115. [DOI] [PubMed] [Google Scholar]
- 73.Georgette N., Siedner M.J., Petty C.R., Zanoni B.C., Carpenter S., Haberer J.E. Impact of a clinical program using weekly Short Message Service (SMS) on antiretroviral therapy adherence support in South Africa: a retrospective cohort study. BMC Med. Inf. Decis. Making. 2017;17(1):18. doi: 10.1186/s12911-017-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ronen K., Unger J.A., Drake A.L., Perrier T., Akinyi P., Osborn L. SMS messaging to improve ART adherence: perspectives of pregnant HIV-infected women in Kenya on HIV-related message content. AIDS Care. 2018;30(4):500–505. doi: 10.1080/09540121.2017.1417971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kamal A.K., Shaikh Q., Pasha O., Azam I., Islam M., Memon A.A. A randomized controlled behavioral intervention trial to improve medication adherence in adult stroke patients with prescription tailored Short Messaging Service (SMS)-SMS4Stroke study. BMC Neurol. 2015;15(1):1–11. doi: 10.1186/s12883-015-0471-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Haberer J.E., Musiimenta A., Atukunda E.C., Musinguzi N., Wyatt M.A., Ware N.C. Short message service (SMS) reminders and real-time adherence monitoring improve antiretroviral therapy adherence in rural Uganda. AIDS (London, England) 2016;30(8):1295. doi: 10.1097/QAD.0000000000001021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nhavoto J.A., Grönlund Å., Klein G.O. Mobile health treatment support intervention for HIV and tuberculosis in Mozambique: perspectives of patients and healthcare workers. PloS One. 2017;12(4) doi: 10.1371/journal.pone.0176051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ratchakit-Nedsuwan R., Nedsuwan S., Sawadna V., Chaiyasirinroje B., Bupachat S., Ngamwithayapong-Yanai J. Ensuring tuberculosis treatment adherence with a mobile-based CARE-call system in Thailand: a pilot study. Infect. Dis. 2020;52(2):121–129. doi: 10.1080/23744235.2019.1688862. [DOI] [PubMed] [Google Scholar]
- 79.Hirsch-Moverman Y., Daftary A., Yuengling K.A., Saito S., Ntoane M., Frederix K. Using mHealth for HIV/TB treatment support in Lesotho: enhancing patient-provider communication in the START study. J. Acquir. Immune Defic. Syndr. 2017;74(Suppl 1):S37. doi: 10.1097/QAI.0000000000001202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nelissen H.E., Cremers A.L., Okwor T.J., Kool S., van Leth F., Brewster L. Pharmacy-based hypertension care employing mHealth in Lagos, Nigeria - a mixed-methods feasibility study. BMC Health Serv. Res. 2018;18(1):934. doi: 10.1186/s12913-018-3740-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Moodley J., Constant D., Botha M.H., van der Merwe F.H., Edwards A., Momberg M. Exploring the feasibility of using mobile phones to improve the management of clients with cervical cancer precursor lesions. BMC Wom. Health. 2019;19(1) doi: 10.1186/s12905-018-0702-1. N.PAG-N.PAG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ibraheem R.M., Akintola M.A. Acceptability of reminders for immunization appointments via mobile devices by mothers in Ilorin, Nigeria: a cross-sectional study. Oman Med. J. 2017;32(6):471. doi: 10.5001/omj.2017.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Marufu C., Maboe K.A. Utilisation of mobile health by medical doctors in a Zimbabwean health care facility. Health SA Gesondheid. 2017;22:228–234. [Google Scholar]
- 84.Al Najjar S., Al Shaer T. Factors affecting adherence to an appointment system in the clinic for non-communicable diseases in UNRWA's Khan Younis Health Centre and the role of mobile phone text messages to improve adherence: a descriptive cross-sectional study. The Lancet. 2018;391:S42. doi: 10.1016/S0140-6736(18)30408-2. [DOI] [PubMed] [Google Scholar]
- 85.Alvis-Estrada J.P., Davis D.A., Guevara K.G., Santa Luce R.L., Loya-Montiel M.I., Northbrook S. A mobile application to monitor mode, content, and duration of health navigation services for people living with HIV in Guatemala. AIDS Care. 2020:1–6. doi: 10.1080/09540121.2020.1734173. [DOI] [PubMed] [Google Scholar]
- 86.Smith R., Menon J., Rajeev J.G., Feinberg L., Kumar R.K., Banerjee A. Potential for the use of mHealth in the management of cardiovascular disease in Kerala: a qualitative study. BMJ Open. 2015;5(11) doi: 10.1136/bmjopen-2015-009367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cormick G., Ciganda A., Cafferata M.L., Ripple M.J., Sosa-Estani S., Buekens P. Text message interventions for follow-up of infants born to mothers positive for Chagas disease in Tucumán, Argentina: a feasibility study. BMC Res. Notes. 2015;8(1):508. doi: 10.1186/s13104-015-1498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mugo P.M., Wahome E.W., Gichuru E.N., Mwashigadi G.M., Thiong’o A.N., Prins H.A. Effect of text message, phone call, and in-person appointment reminders on uptake of repeat HIV testing among outpatients screened for acute HIV infection in Kenya: a randomized controlled trial. PloS One. 2016;11(4) doi: 10.1371/journal.pone.0153612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mbuthia F., Reid M., Fichardt A. mHealth communication to strengthen postnatal care in rural areas: a systematic review. BMC Pregnancy Childbirth. 2019;19(1):406. doi: 10.1186/s12884-019-2531-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kumar A.A., De Costa A., Das A., Srinivasa G.A., D'Souza G., Rodrigues R. Mobile health for tuberculosis management in South India: is video-based directly observed treatment an acceptable Alternative? JMIR Mhealth Uhealth. 2019;7(4) doi: 10.2196/11687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Atallah N., Khalifa M., El Metwally A., Househ M. The prevalence and usage of mobile health applications among mental health patients in Saudi Arabia. J. Comp. Methods Programs Biomed. 2018;156:163–168. doi: 10.1016/j.cmpb.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 92.Olamoyegun M., Emuoyibofarhe O., Ala O., Ugwu E. Mobile phone use in the management of diabetes in Nigeria: a new potential weapon. J. West Afr. J. Med. 2020;37(3):201–208. [PubMed] [Google Scholar]
- 93.Chirambo G.B., Hardy V., Heavin C., O’Connor Y., O’Donoghue J., Mastellos N. Perceptions of a mobile health intervention for community case management in Malawi: opportunities and challenges for health surveillance assistants in a community setting. J. Malawi Med. J. 2018;30(1):6–12. doi: 10.4314/mmj.v30i1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Atnafu A., Otto K., Herbst C.H. The role of mHealth intervention on maternal and child health service delivery: findings from a randomized controlled field trial in rural Ethiopia. mHealth. 2017;3:39. doi: 10.21037/mhealth.2017.08.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mushamiri I., Luo C., Iiams-Hauser C., Amor Y.B. Evaluation of the impact of a mobile health system on adherence to antenatal and postnatal care and prevention of mother-to-child transmission of HIV programs in Kenya. BMC Publ. Health. 2015;15(1):102. doi: 10.1186/s12889-015-1358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Colaci D., Chaudhri S., Vasan A. mHealth interventions in low-income countries to address maternal health: a systematic review. Ann. Glob. Health. 2016;82(5):922–935. doi: 10.1016/j.aogh.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 97.Tang S., Ghose B., Hoque M.R., Hao G., Yaya S. Women using mobile phones for health communication are more likely to use prenatal and postnatal services in Bangladesh: cross-sectional study. JMIR mHealth uHealth. 2019;7(2) doi: 10.2196/10645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Feroz A., Perveen S., Aftab W. Role of mHealth applications for improving antenatal and postnatal care in low and middle-income countries: a systematic review. BMC Health Serv. Res. 2017;17(1):704. doi: 10.1186/s12913-017-2664-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Modi D., Dholakia N., Gopalan R., Venkatraman S., Dave K., Shah S. mHealth intervention “ImTeCHO” to improve the delivery of maternal, neonatal, and child care services—a cluster-randomized trial in tribal areas of Gujarat, India. PLoS Med. 2019;16(10) doi: 10.1371/journal.pmed.1002939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tobe R.G., Haque S.E., Ikegami K., Mori R. Mobile-health tool to improve maternal and neonatal health care in Bangladesh: a cluster randomized controlled trial. BMC Preg. Childbirth. 2018;18(1):102. doi: 10.1186/s12884-018-1714-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.McNabb M., Chukwu E., Ojo O., Shekhar N., Gill C.J., Salami H. Assessment of the quality of antenatal care services provided by health workers using mobile phone decision support application in northern Nigeria: a pre/post-intervention study. PloS One. 2015;10(5) doi: 10.1371/journal.pone.0123940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Piette J.D., Marinec N., Janda K., Morgan E., Schantz K., Yujra A.C.A. Structured caregiver feedback enhances engagement and impact of mobile health support: a randomized trial in a lower-middle-income country. Telemed. e-Health. 2016;22(4):261–268. doi: 10.1089/tmj.2015.0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kamal A.K., Shaikh Q., Pasha O., Azam I., Islam M., Memon A.A. A randomized controlled behavioral intervention trial to improve medication adherence in adult stroke patients with prescription tailored Short Messaging Service (SMS)-SMS4Stroke study. BMC Neurol. 2015;15(1):1–11. doi: 10.1186/s12883-015-0471-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Alghamdi M., Gashgari H., Househ M. A systematic review of mobile health technology use in developing countries. J. Stud. Health Technol. Informat. 2015;213:223–226. [PubMed] [Google Scholar]
- 105.Hacking D., Haricharan H.J., Brittain K., Lau Y.K., Cassidy T., Heap M. Hypertension health promotion via text messaging at a community health center in South Africa: a mixed-methods study. JMIR mHealth uHealth. 2016;4(1):e22. doi: 10.2196/mhealth.4569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Demena B.A., Artavia-Mora L., Ouedraogo D., Thiombiano B.A., Wagner N. A systematic review of mobile phone interventions (SMS/IVR/calls) to improve adherence and retention to antiretroviral treatment in low-and middle-income countries. AIDS Patient Care STDS. 2020;34(2):59–71. doi: 10.1089/apc.2019.0181. [DOI] [PubMed] [Google Scholar]
- 107.Parimbelli E., Bottalico B., Losiouk E., Tomasi M., Santosuosso A., Lanzola G. Trusting telemedicine: a discussion on risks, safety, legal implications, and liability of involved stakeholders. Int. J. Med. Inf. 2018;112:90–98. doi: 10.1016/j.ijmedinf.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 108.Patel A., Praveen D., Maharani A., Oceandy D., Pilard Q., Kohli M.P.S. Association of multifaceted mobile technology-enabled primary care intervention with cardiovascular disease risk management in rural Indonesia. JAMA Cardiol. 2019;4(10):978–986. doi: 10.1001/jamacardio.2019.2974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chow C.K., Ariyarathna N., Islam S.M., Thiagalingam A., Redfern J. mHealth in Cardiovascular Health Care. Heart, lung & circulation. 2016;25(8):802–807. doi: 10.1016/j.hlc.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 110.Uqaili A., Qaiser F., Abbas K., Rahman A.A. Smartphone use among young doctors and their impact on patients of Liaquat University Hospital Jamshoro. Imperial. J. Interdiscip. Res. 2017;3:161–164. [Google Scholar]
- 111.Kassianos A., Emery J., Murchie P., Walter F.M. Smartphone applications for melanoma detection by the community, patient and generalist clinician users: a review. Br. J. Dermatol. 2015;172(6):1507–1518. doi: 10.1111/bjd.13665. [DOI] [PubMed] [Google Scholar]
- 112.Boceta J., Samper D., de la Torre A., Sánchez-de la Rosa R., González G. Usability, acceptability, and usefulness of an mhealth app for diagnosing and monitoring patients with breakthrough cancer pain. JMIR Cancer. 2019;5(1) doi: 10.2196/10187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Treacy C., McCaffery F., Finnegan A. 2015. Mobile Health & Medical Apps: Possible Impediments to Healthcare Adoption. [Google Scholar]
- 114.Peiris D., Miranda J.J., Mohr D.C. BMJ Specialist Journals; 2018. Going beyond killer apps: building a better mHealth evidence base. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Krohn R. mHealth: a pathway to the intelligent hospital. Mhealth. 2015;1 doi: 10.3978/j.issn.2306-9740.2015.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wu A.C., Tse S.M., Balli F. Precision in Pulmonary, Critical Care, and Sleep Medicine. Springer; 2020. Mobile applications, and wearables for chronic respiratory disease monitoring; pp. 291–304. [Google Scholar]
- 117.Telehealth, mobile applications, and wearable devices are expanding cancer care beyond walls. Cannon C., editor. Semin. Oncol. Nurs. 2018 doi: 10.1016/j.soncn.2018.03.002. Elsevier. [DOI] [PubMed] [Google Scholar]
- 118.Steinman L., Heang H., van Pelt M., Ide N., Cui H., Rao M. Facilitators and barriers to chronic disease self-management and mobile health interventions for people living with diabetes and hypertension in Cambodia: qualitative study. JMIR mHealth uHealth. 2020;8(4) doi: 10.2196/13536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shao A.F., Rambaud-Althaus C., Swai N., Kahama-Maro J., Genton B., D’Acremont V. Can smartphones and tablets improve the management of childhood illness in Tanzania? A qualitative study from a primary health care worker’s perspective. BMC Health Serv. Res. 2015;15(1):135. doi: 10.1186/s12913-015-0805-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Blanas D.A., Ndiaye Y., MacFarlane M., Manga I., Siddiqui A., Velez O. Health worker perceptions of integrating mobile phones into community case management of malaria in Saraya, Senegal. Int. Health. 2015;7(3):176–182. doi: 10.1093/inthealth/ihu075. [DOI] [PubMed] [Google Scholar]
- 121.Laktabai J., Platt A., Menya D., Turner E.L., Aswa D., Kinoti S. A mobile health technology platform for quality assurance and quality improvement of malaria diagnosis by community health workers. PloS One. 2018;13(2) doi: 10.1371/journal.pone.0191968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kenny G., Heavin C., O’Connor Y., Eze E., Ndibuagu E. 2017. Making Mobile Health about the User: Understanding Primary Healthcare Workers’ Attitudes towards mHealth Adoption. [Google Scholar]
- 123.Eze E., Gleasure R., Heavin C. Mobile health solutions in developing countries: a stakeholder perspective. Health Syst. 2018:1–23. doi: 10.1080/20476965.2018.1457134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Peprah P., Abalo E.M., Agyemang-Duah W., Gyasi R.M., Reforce O., Nyonyo J. Knowledge, attitude, and use of mHealth technology among students in Ghana: a university-based survey. BMC Med. Inf. Decis. Making. 2019;19(1):220. doi: 10.1186/s12911-019-0947-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Adebara O.V., Adebara I.O., Olaide R., Emmanuel G.O., Olanrewaju O. Knowledge, attitude, and willingness to use mHealth technology among doctors at a semi-urban tertiary hospital in Nigeria. J. Adv. Med. Med. Res. 2017:1–10. [Google Scholar]
- 126.Abolfotouh M.A., BaniMustafa Aa, Salam M., Al-Assiri M., Aldebasi B., Bushnak I. Use of smartphone and perception towards the usefulness and practicality of its medical applications among healthcare workers in Saudi Arabia. BMC Health Serv. Res. 2019;19(1):826. doi: 10.1186/s12913-019-4523-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ramos R., Cheng P., de Castro F. Attitudes toward mhealth: a look at general attitudinal indices among selected Filipino undergraduates. J. Construct. Soc. Psychol.: Adv. Psychol. Psychol. Trends. 2015:186–202. [Google Scholar]
- 128.Navabi N., Ghaffari F., Jannat-Alipoor Z. Older adults’ attitudes and barriers toward the use of mobile phones. 2016;11:1371. doi: 10.2147/CIA.S112893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Jemere A.T., Yeneneh Y.E., Tilahun B., Fritz F., Alemu S., Kebede M. Access to mobile phone and willingness to receive mHealth services among patients with diabetes in Northwest Ethiopia: a cross-sectional study. BMJ Open. 2019;9(1) doi: 10.1136/bmjopen-2018-021766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nichols M., Sarfo F.S., Singh A., Qanungo S., Treiber F., Ovbiagele B. Assessing mobile health capacity and task-shifting strategies to improve hypertension among Ghanaian stroke survivors. Am. J. Med. Sci. 2017;354(6):573–580. doi: 10.1016/j.amjms.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lewis K.D. 2017. Utilizing Perspectives from HIV-Infected Women, Male Partners, and Healthcare Providers to Design Family Planning mobile Health Messaging in Kenya: A Qualitative Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Jonas Stephan Michael, TMD, Buhimschi Catalin Sorin, Makin Jennifer, Choma Michael Andrew, Buhimschi Irina Alexandra. 2016. Smartphone-based Diagnostic for Preeclampsia: an mHealth Solution for Administering the Congo Red Dot (CRD) Test in Settings with Limited Resources. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vasiman A., Stothard J.R., Bogoch Mobile phone devices and handheld microscopes as diagnostic platforms for Malaria and neglected tropical diseases (NTDs) in low-resource settings: a systematic review, historical perspective, and future outlook. Adv. Parasitol. 2019;103:151–173. doi: 10.1016/bs.apar.2018.09.001. Elsevier. [DOI] [PubMed] [Google Scholar]
- 134.Coulibaly J.T., Ouattara M., D'Ambrosio M.V., Fletcher D.A., Keiser J., Utzinger J. Accuracy of mobile phone and handheld light microscopy for the diagnosis of schistosomiasis and intestinal Protozoa infections in cote d'Ivoire. PLoS Neglected Trop. Dis. 2016;10(6) doi: 10.1371/journal.pntd.0004768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ephraim R.K., Duah E., Cybulski J.S., Prakash M., D'Ambrosio M.V., Fletcher D.A. Diagnosis of Schistosoma haematobium infection with a mobile phone-mounted Foldscope and a reversed-lens CellScope in Ghana. Am. J. Trop. Med. Hyg. 2015;92(6):1253–1256. doi: 10.4269/ajtmh.14-0741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Jaworek-Korjakowska J., Eskin Kleczek P. A study on the smartphone application for early detection of malignant melanoma. J. Wireless Commun. Mobile Comput. 2018;2018 [Google Scholar]
- 137.Yang A., Bakhtari N., Langdon-Embry L., Redwood E., Lapierre S.G., Rakotomanga P. Kankanet: an artificial neural network-based object detection smartphone application and mobile microscope as a point-of-care diagnostic aid for soil-transmitted helminthiases. PLoS Neglected Trop. Dis. 2019;13(8) doi: 10.1371/journal.pntd.0007577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Urner E., Delavy M., Catarino R., Viviano M., Meyer-Hamme U., Benski A.-C. A smartphone-based approach for triage of human papillomavirus-positive sub-Saharan African women: a prospective study. JMIR mHealth uHealth. 2017;5(5):e72. doi: 10.2196/mhealth.6697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tran P.L., Benski C., Viviano M., Petignat P., Combescure C., Jinoro J. Performance of smartphone-based digital images for cervical cancer screening in a low-resource context. Int. J. Technol. Assess. Health Care. 2018;34(3):337–342. doi: 10.1017/S0266462318000260. [DOI] [PubMed] [Google Scholar]
- 140.Hameed S.S., Rawal I., Soni D., Ajay V.S., Goenka S., Prabhakaran D. Technology for diagnosis, treatment, and prevention of cardiometabolic disease in India. Prog. Cardiovasc. Dis. 2016;58(6):620–629. doi: 10.1016/j.pcad.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 141.Coulibaly J.T., Ouattara M., Keiser J., Bonfoh B., N'Goran E.K., Andrews J.R. Evaluation of malaria diagnoses using a handheld light microscope in a community-based setting in rural Côte d'Ivoire. Am. J. Trop. Med. Hyg. 2016;95(4):831–834. doi: 10.4269/ajtmh.16-0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Baldini K., Sall A., Cisse A., Berzolari F.G., Borrelli P., Parigi G. 2017. Cardiovascular Screening in Low-Income Settings Using a Novel 4-lead Smartphone-Based Electrocardiograph (D-Heart®) [DOI] [PubMed] [Google Scholar]
- 143.Gleason A.W. mHealth — opportunities for transforming global health care and barriers to adoption. J. Electron. Resour. Med. Libr. 2015;12(2):114–125. [Google Scholar]
- 144.Gutierrez M., Moreno R., Rebelo M. Global Health Informatics. Elsevier; 2017. Information and communication technologies and global health challenges; pp. 50–93. [Google Scholar]
- 145.Kiberu V.M., Mars M., Scott R.E. Barriers and opportunities to implementation of sustainable e-Health programmes in Uganda: a literature review. Afr. J. Prim. Health Care Fam. Med. 2017;9(1):1–10. doi: 10.4102/phcfm.v9i1.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Botha A., Booi V. 2016. mHealth Implementation in South Africa. 2016 IST-Africa Week Conference; pp. 1–13. [Google Scholar]
- 147.van Olmen J., Erwin E., García-Ulloa A.C., Meessen B., Miranda J.J., Bobrow K. Implementation barriers for mHealth for non-communicable disease management in low and middle-income countries: a scoping review and field-based views from implementers. Wellcome Open Res. 2020;5 doi: 10.12688/wellcomeopenres.15581.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Medhanyie A.A., Little A., Yebyo H., Spigt M., Tadesse K., Blanco R. Health workers’ experiences, barriers, preferences, and motivating factors in using mHealth forms in Ethiopia. Hum. Resour. Health. 2015;13(1):1–10. doi: 10.1186/1478-4491-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Harding K., Biks G.A., Adefris M., Loehr J., Gashaye K.T., Tilahun B. A mobile health model supporting Ethiopia’s eHealth strategy. J. Digit. Med. 2018;4(2):54. doi: 10.4103/digm.digm_10_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Farquharson D., Jaramillo P., Samaras C. Sustainability implications of electricity outages in sub-Saharan Africa. Nat. Sustain. 2018;1(10):589–597. [Google Scholar]
- 151.Treacy C., McCaffery F. Data security overview for medical mobile apps assuring the confidentiality, integrity, and availability of data in transmission. Int. J. Adv. Secur. 2016;9(3 & 4):146–157. [Google Scholar]
- 152.Plachkinova M., Andrés S., Chatterjee S., editors. A Taxonomy of mHealth Apps--Security and Privacy Concerns. 2015 48th Hawaii International Conference on System Sciences. IEEE; 2015. [Google Scholar]
- 153.Bhuyan S.S., Kim H., Isehunwa O.O., Kumar N., Bhatt J., Wyant D.K. Privacy and security issues in mobile health: current research and future directions. Health Pol. Technol. 2017;6(2):188–191. [Google Scholar]
- 154.Shuvo T.A., Islam R., Hossain S., Evans J.L., Khatun F., Ahmed T. eHealth innovations in LMICs of Africa and Asia: a literature review exploring factors affecting implementation, scale-up. Sustainability. 2015;8:9. [Google Scholar]
- 155.Hermans S.M., Elbireer S., Tibakabikoba H., Hoefman B.J., Manabe YCJPp, adherence Text messaging to decrease tuberculosis treatment attrition in TB-HIV coinfection in Uganda. 2017;11:1479. doi: 10.2147/PPA.S135540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.van der Kop M.L., Muhula S., Nagide P.I., Thabane L., Gelmon L., Awiti P.O. Effect of an interactive text-messaging service on patient retention during the first year of HIV care in Kenya (WelTel Retain): an open-label, randomized parallel-group study. The Lancet Publ. Health. 2018;3(3):e143–e152. doi: 10.1016/S2468-2667(17)30239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Brinkel J., May J., Krumkamp R., Lamshoft M., Kreuels B., Owusu-Dabo E. Mobile phone-based interactive voice response as a tool for improving access to healthcare in remote areas in Ghana - an evaluation of user experiences. Trop. Med. Int. Health : TM & IH. 2017;22(5):622–630. doi: 10.1111/tmi.12864. [DOI] [PubMed] [Google Scholar]
- 158.Kruse C., Betancourt J., Ortiz S., Luna S.M.V., Bamrah I.K., Segovia N. Barriers to the use of mobile health in improving health outcomes in developing countries: a systematic review. J. Med. Internet Res. 2019;21(10) doi: 10.2196/13263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tchao E.T., Diawuo K., Ofosu W.K. Mobile telemedicine implementation with WiMAX technology: A case study of Ghana. J. Med. Syst. 2017;41(1):17. doi: 10.1007/s10916-016-0661-8. [DOI] [PubMed] [Google Scholar]
- 160.Niakan S., Mehraeen E., Noori T., Gozali E., editors. Web and Mobile Based HIV Prevention and Intervention Programs Pros and Cons-A Review. eHealth; 2017. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.