Abstract
Background:
Tumor necrosis factor-alpha (TNF-α), a ” major inflammatory cytokine,” not only plays an important role in periodontal destruction but also is extremely toxic to the host. Till date, there are not many studies comparing the levels of TNF-α in serum and its relationship to periodontal disease.
Aim:
Our study aimed to compare the serum TNF-α among the two study groups, namely, healthy controls and chronic periodontitis patients and establish a correlation between serum TNF-α and various clinical parameters. Hence, an attempt is made to estimate the level of TNF-α in serum, its relationship to periodontal disease and to explore the possibility of using the level of TNF-α in serum as a biochemical “ marker” of periodontal disease.
Materials and Methods:
Forty individuals participated in the study and were grouped into two subgroups. Group A – 20 systemically and periodontally healthy controls. Group B – twenty patients with generalized chronic periodontitis. The serum samples were assayed for TNF-α levels by enzyme-linked immunosorbent assay method.
Results:
The mean serum TNF-α cytokines for Group B Generalized chronic periodontitis (GCP) was 2.977 ± 1.011, and Group A (healthy) was 0.867 ± 0.865. The range of serum TNF-α was from (0.867 to 2.977). Serum TNF-α cytokines had highly significant correlation with all clinical parameters (plaque index, probing pocket depth, clinical attachment loss, and gingival index) among all study participants (P = 0.001).
Conclusion:
These observations suggest a positive association between periodontal disease and increased levels of TNF-α in serum. It can be concluded that there is a prospect of using the estimation of TNF-α in serum as a “marker” of periodontal disease in future. However, it remains a possibility that the absence or low levels of TNF-α in serum might indicate a stable lesion and elevated levels might indicate an active site but only longitudinal studies taking into account, the disease “activity” and “inactivity” could suggest the possibility of using TNF-α in serum as an “Indicator” of periodontal disease.
Keywords: Generalized chronic periodontitis, Inflammation, Tumor necrosis factor alpha
Introduction
Oral health is indispensable to overall healthy being. Man has been suffering from ailments of oral cavity since time immemorial. Oral diseases, especially caries and periodontitis are known for their high prevalence and rapid morbidity. Periodontal diseases are a group of chronic, progressive bacterial infections resulting in inflammation, and destruction of tooth supporting tissues.[1] The periodontal disease is known to have complex pathogenesis with both bacterial and host factors contributing to the destruction of periodontium. The role of host immune response is most important factor in periodontitis as it determines both disease progression and severity.[2]
Difficulty in determining active disease and ongoing destruction in periodontal tissue by traditional diagnostic aids such as probing depth and attachment loss has proved them to be inadequate in the modern era of periodontal therapeutics.[3,4,5] Search for a biomarker for periodontitis has resulted in researchers trying out and finding new molecules that can guide a clinician in many a decision regarding the patient's condition.
Tumor necrosis factor-alpha (TNF-α) is a pro-inflammatory cytokine released by macrophages which is known for its substantial role in periodontitis mediated bone loss.[6] This can be detected in saliva, gingival crevicular fluid (GCF), and serum in both health and periodontitis.[7] Increased concentration observed in periodontitis correlate closely with the tissue destruction and immune response.[8,9]
Enhanced expressions of serum TNF-α have been observed in rheumatoid arthritis (RA) and chronic obstructive pulmonary disease. In addition, upregulation of its expression in keratinocytes in chronic inflammatory skin diseases such as psoriasis has also been observed.[10] This clearly indicates the role of TNF-α in chronic inflammation. In addition, serum cytokines are increasingly being correlated with periodontal status and oral inflammatory burden in recent times.[8,11]
In general, pathogenic species and their products can stimulate the production of a number of pro-in?ammatory cytokines, including interleukin (IL)-1b and IL-6 and TNF-α, which coordinate a local in?ammatory response.[12,13]
The role of TNF-α in the host immune response to local infection has been well documented in the literature. This cytokine triggers the production of adhesion molecules, pro-in?ammatory cytokines, and chemokines, such as IL-1a, IL-1b, IL-6, and IL-8 and matrix metalloproteinases.[14]
In addition, TNF-α may signi?cantly stimulate local bone resorption by inducing osteoclastogenesis and in?uencing the production of the essential osteoclast differentiation factors, such as receptor activator of nuclear factor-kappa B ligand and its soluble decoy receptor, osteoprotegerin.[15,16,17,18,19,20]
Hence, the present study was carried out to compare and to correlate TNF-α levels between chronic periodontitis patients and healthy individuals.
Materials and Methods
A total of forty patients were selected from the outpatient department of Periodontology, People's College of Dental Sciences and Research Centre, Bhanpur, Bhopal. They were divided into four groups of patients aged between 24 and 60 years.
The total study population was divided into two groups:
Group A – 20 systemically and periodontally healthy controls
Group B – twenty patients with generalized chronic periodontitis.
Inclusion criteria
Patients should have at least 20 permanent teeth.
For chronic periodontitis – periodontal pockets ≥4 mm as well as clinical attachment loss (CAL) and bleeding on probing at more than 30% of sites (Armitage 1999)
For healthy periodontium – periodontal probing depth as well as clinical attachment level ≤3 mm.
Exclusion criteria
Patients suffering from chronic systemic diseases
Pregnant and lactating females
Patients taking any medication 6 months before study other than vitamins or occasional analgesics
Patients undergoing radiotherapy to head-and-neck region.
The nature and purpose of the study was explained to the patients, and informed consent was obtained from every patient. A detailed case history was recorded in a prepared pro forma which included information regarding the patient's age, gender, medical history and dental history including various clinical parameters.
Collection of blood
From the selected patients, 5 ml of blood was withdrawn from the antecubital vein to evaluate the levels of TNF-α in serum through human serum enzyme-linked immunosorbent assay (ELISA) detection.
Biochemical analysis
Biochemical analysis was carried out at Centre for Scientific Research and Development, People's University, Bhopal.
Enzyme-linked immunosorbent assay KITs
TNF-α is a potent lymphoid factor which exerts cytotoxic effects on a wide range of tumor cells and certain other target cells. Human TNF-α is a 17.4 kD protein containing 157 amino acid residues.
Intended use
Human ELISA Kits are specifically designed for the accurate quantification of human TNF-α, from cell culture supernatant, serum, plasma, or other bodily fluids. It is ready-to-use, accurate, and sensitive.
Statistical analysis
The data obtained was subjected to statistical analysis with the consult of a statistician. The data so obtained was compiled systematically. A master table was prepared, and the total data were subdivided and distributed meaningfully and presented as individual tables along with graph.
Statistical procedures were carried out in two steps:
Data compilation and presentation
Statistical analysis.
Statistical analysis was done using Statistical Package of Social Science (SPSS Version 20; Chicago Inc., IL, USA). Data comparison was done by applying specific statistical tests to find out the statistical significance of the comparisons. Quantitative variables were compared using mean values and qualitative variables using proportions.
The significance level was fixed at P < 0.05.
Interpretation of the results
Periodontitis is a chronic bacterial infection characterized by persistent inflammation, connective tissue breakdown, and alveolar bone destruction mediated by pro-inflammatory mediators. TNF-α is a pro-inflammatory cytokine released by macrophages which is known for its substantial role in periodontitis mediated bone loss.[6] This can be detected in saliva, GCF, and serum in both health and periodontitis.[7] Increased concentration observed in periodontitis correlate closely with the tissue destruction and immune response.[8]
When the mean of serum TNF-α values was compared between healthy and generalized chronic periodontitis patients, it was found that the values were significantly higher for patients with GCP than for healthy controls as shown in Table 1 and Graph 1. Increased level of TNF-α in serum is related with an inflammatory state. High numbers of inflammatory cells in the connective tissue and gingival crevice can lead to the release of TNF-α on stimulation by the bacterial products[67]
Table 1.
Comparison of mean serum tumor necrosis factor-alpha cytokines among healthy and chronic generalized periodontitis patients
| Groups | n | Serum TNF-α cytokines | ||
|---|---|---|---|---|
| Mean±SD | Median | Range | ||
| Healthy | 20 | 0.867±0.865 | 0.47 | 0.116-2.87 |
| CGP | 20 | 2.977±1.011 | 3.26 | 1.11-4.50 |
| Kruskal-Wallis test: χ2 | 49.979 | |||
| Significance P | 0.001 (HS) | |||
TNF-α: Tumor necrosis factor-alpha; CGP: Chronic generalized periodontitis; SD: Standard deviation; HS: Highly significant
Graph 1.
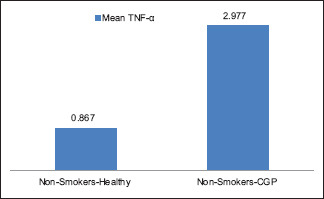
Comparison of mean serum tumor necrosis factor-alpha cytokines among healthy and chronic generalized periodontitis patients
Stashenko et al.[70] have reported that there were increased levels of TNF-α in gingival tissues of periodontitis patients. They suggested that TNF-α is related with the inflammatory condition of the periodontium. TNF-α may be synthesized and secreted by the local periodontal connective tissue cells, such as fibroblasts and endothelial cells or by infiltrating leukocytes, i.e., mononuclear cells, macrophages, and neutrophils.
The results of our study was in accordance with a study conducted by Varghese et al. (2015), to estimate the salivary TNF-α in chronic and aggressive periodontitis and control participants. They concluded that salivary TNF-α levels are significantly higher in chronic periodontitis than in healthy controls; however, there was no significant correlation with the clinical parameters.
Correlation of tumor necrosis factor alpha with various clinical parameters
In our study, the results show that serum TNF-α cytokines had a strong positive highly significant correlation with plaque index (PI), probing pocket depth (PPD), and CAL and there was a moderate positive significant correlation between TNF-α and gingival index (GI). Serum TNF-α cytokines had a highly significant correlation with all clinical parameters among all study participants (P = 0.001) as shown in Graphs 2-4 and Tables 1-5.
Graph 2.
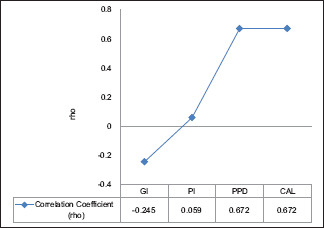
Spearman's correlation of serum tumor necrosis factor-alpha cytokines with all clinical parameter among healthy study participants
Graph 4.
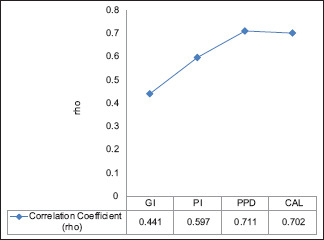
Spearman's Correlation of serum tumor necrosis factor-alpha cytokines with all clinical parameter among all study participants
Table 5.
Spearman’s correlation of serum tumor necrosis factor-alpha cytokines with all clinical parameter among all study participants
| Clinical parameter | Serum TNF-α cytokines | ||
|---|---|---|---|
| Correlation coefficient (ρ) | P | Inference | |
| GI | 0.441* | 0.001 (HS) | Moderate correlation |
| PI | 0.597** | 0.001 (HS) | Strong correlation |
| PPD | 0.711** | 0.001 (HS) | Strong correlation |
| CAL | 0.702** | 0.001 (HS) | Strong correlation |
TNF-α: Tumor necrosis factor-alpha; GI: Gingival index; PI: Plaque index; PPD: Probing pocket depth; CAL: Clinical attachment loss; HS: Highly significant; Significance P 0.001 (HS)
Graph 3.
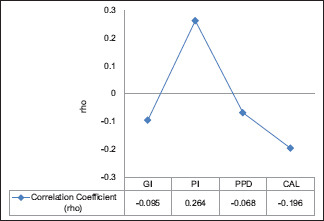
Spearman's correlation of serum tumor necrosis factor-alpha cytokines with all clinical parameter among chronic generalized periodontitis patients
Table 2.
Comparison of mean serum TNF-α cytokines among smokers & non-smokers healthy subjects
| Groups | n | Serum TNF-α cytokines | ||
|---|---|---|---|---|
| Mean±SD | Median | Range | ||
| Healthy | 15 | 0.867±0.865 | 0.47 | 0.116-2.87 |
| CGP | 15 | 2.977±1.011 | 3.26 | 1.11-4.50 |
| Mann-Whitney U-test value | 28.000 | |||
| Significance P | 0.001 (HS) | |||
TNF-α: Tumor necrosis factor-alpha; CGP: Chronic generalized periodontitis; SD: Standard deviation; HS: Highly significant
Table 3.
Spearman’s correlation of serum tumor necrosis factor-alpha cytokines with all clinical parameter among healthy study participants
| Clinical parameter | Serum TNF-α cytokines | ||
|---|---|---|---|
| Correlation coefficient (ρ) | P | Inference | |
| GI | −0.245 | 0.297 | Weak correlation |
| PI | 0.059 | 0.804 | No linear relationship |
| PPD | 0.672** | 0.001 | Strong correlation |
| CAL | 0.672** | 0.001 | Strong correlation |
TNF-α: Tumor necrosis factor-alpha; GI: Gingival index; PI: Plaque index; PPD: Probing pocket depth; CAL: Clinical attachment loss; Significance P 0.001 (HS)
Table 4.
Spearman’s correlation of serum tumor necrosis factor-alpha cytokines with all clinical parameter among chronic generalized periodontitis patients
| Clinical parameter | Serum TNF-α cytokines | ||
|---|---|---|---|
| Correlation coefficient (ρ) | P | Inference | |
| GI | −0.095 | 0.691 | No linear relationship |
| PI | 0.264 | 0.260 | Weak correlation |
| PPD | −0.068 | 0.777 | No linear relationship |
| CAL | −0.196 | 0.408 | Weak correlation |
TNF-α: Tumor necrosis factor-alpha; GI: Gingival index; PI: Plaque index; PPD: Probing pocket depth; CAL: Clinical attachment loss
In a previous study by Engebretson et al.,[47] TNF-α showed a significant positive correlation with attachment loss, but not probing depth and PI. A dose-response relationship was observed between periodontitis severity and TNF-α.
Ikezawa et al. in their study reported a significant positive correlation between GCF TNF-α levels with pocket depth in chronic periodontitis patients.[71] Kurtis et al. also reported a positive correlation between salivary TNF-α levels and clinical parameters such as probing depth, CAL, PI, and GI in GCF samples of patients with chronic and aggressive periodontitis.[72]
Mean gingival index score
Mean GI for chronic generalized periodontitis (CGP) patients was (1.32 ± 0.37) and among healthy controls were (0.032 ± 0.011) There was statistically highly significant difference in mean gingival index among both the groups (P = 0.001) as shown in Table 6.
Table 6.
Comparison of mean gingival index among healthy and chronic generalized periodontitis patients
| Groups | n | GI | ||
|---|---|---|---|---|
| Mean±SD | Median | Range | ||
| Healthy | 20 | 0.032±0.011 | 0.030 | 0.02–0.06 |
| CGP | 20 | 1.32±0.37 | 1.42 | 0.67–1.88 |
| Kruskal-Wallis test: χ2 | 49.116 | |||
| Significance P | 0.001 (HS) | |||
GI: Gingival index; CGP: Chronic generalized periodontitis; SD: Standard deviation; HS: Highly significant
Mean plaque index score
Mean PI were highest among CGP patients. It was (2.76 ± 0.39) among CGP, and (0.029 ± 0.013) among healthy controls. There was statistically highly significant difference in mean PI among both the groups (P = 0.001) as shown in Table 7.
Table 7.
Comparison of mean plaque index among healthy and chronic generalized periodontitis patients
| Groups | n | PI | ||
|---|---|---|---|---|
| Mean±SD | Median | Range | ||
| Healthy | 20 | 0.029±0.013 | 0.030 | 0.01-0.06 |
| CGP | 20 | 2.76±0.39 | 2.72 | 2.05-2.85 |
| Kruskal-Wallis test: χ2 | 53.103 | |||
| Significance P | 0.001 (HS) | |||
PI: Plaque index; CGP: Chronic generalized periodontitis; SD: Standard deviation; HS: Highly significant
Mean probing pocket depth
The mean PPD were (5.33 ± 0.51) among CGP, and (1.49 ± 0.18) among healthy controls as shown in Table 8. There was statistically highly significant difference in mean PPD among both the groups (P = 0.001).
Table 8.
Comparison of mean probing pocket depth among healthy and chronic generalized periodontitis patients
| Groups | n | PPD | ||
|---|---|---|---|---|
| Mean±SD | Median | Range | ||
| Healthy | 20 | 1.49±0.18 | 1.46 | 1.15-1.87 |
| CGP | 20 | 5.33±0.51 | 5.09 | 4.73-6.51 |
| Kruskal-Wallis test: χ2 | 61.909 | |||
| Significance P | 0.001 (HS) | |||
PPD: Probing pocket depth; CGP: Chronic generalized periodontitis; SD: Standard deviation; HS: Highly significant
Mean clinical attachment loss
The mean CAL was (4.97 ± 0.53) among CGP, and (1.49 ± 0.18) among healthy controls as shown in Table 9. There was statistically highly significant difference in mean CAL among both the study groups (P = 0.001).
Table 9.
Comparison of mean clinical attachment loss among healthy chronic generalized periodontitis patients
| Groups | n | CAL | ||
|---|---|---|---|---|
| Mean±SD | Median | Range | ||
| Healthy | 20 | 1.49±0.18 | 1.46 | 1.15-1.87 |
| CGP | 20 | 4.97±0.53 | 4.94 | 4.01-6.0 |
| Kruskal-Wallis test: χ2 | 61.766 | |||
| Significance P | 0.001 (HS) | |||
CAL: Clinical attachment loss; CGP: Chronic generalized periodontitis; SD: Standard deviation; HS: Highly significant
Discussion
Cytokines are key modulators of inflammation. They participate in acute and chronic inflammation in a complex network of interactions. Several cytokines exhibit some redundancy in function and share overlapping properties as well as subunits of their cell surface receptors.[21]
Periodontal diseases are characterized by the classic hallmarks of the inflammatory response, including erythema and edema. Late sequelae of periodontal diseases include the loss of alveolar bone, periodontal ligament attachment, and ultimately, teeth. Therefore, periodontal disease can be viewed as a chronic inflammatory process in which bacteria-induced localized gingival inflammation results in the destruction of bone and the attachment apparatus of the teeth.[22,23,24,25,26,27,28,29,30,31,32,33,34], It has also been considered a risk for a variety of systemic conditions, including cardiovascular disease, diabetes mellitus, RA, and respiratory disorders.[35,36,37,38,39,40,41,42] When the relationship between periodontitis and RA was examined, the findings suggested that circulating TNF-α is related to periodontal inflammation with regard to tissue destruction and vascular reaction in patients with RA.[41]
Role of tumor necrosis factor-alpha in pathogenesis of periodontitis
Periodontitis is initiated by specic bacteria, and the local host response to these bacteria includes the recruitment of leukocytes and the subsequent release of in?ammatory mediators and cytokines such as IL-1, IL-6, IL-8, IL-10, IL-12, and TNF-α, which are thought to play an important role in the pathogenesis of the disease. These increased levels of several cytokines are involved in periodontal tissue destruction[43,44,45,46,47,48,49,50,51,52] (Genco 1992).
TNF-α is also a monocyte-derived protein that has a wide range of pro-inammatory and immunomodulatory effects on a number of different cell populations. TNF-α can stimulate ?broblasts including gingival ?broblasts, to produce collagenase (Meikle et al. 1989), an enzyme implicated in the tissue destruction of periodontal disease, and to stimulate bone resorption (Bertolini et al. 1986). TNF-α activates monocytes and stimulates the production of IL-1b, platelet activating factor, and prostaglandins (Decker 2000). Monocyte stimulation by lipopolysaccharide enhances the production of TNF-α, which has also been shown to induce collagenase release and bone resorption in vivo (Erdemir EO).[52,53,54,55,56,57,58,59,60,61,62]
Pro-inflammatory cytokines (TNF-α, IL-1a, and IL-1 β) are necessary for initiating an effective inflammatory process against infection. TNF-α also activates osteoclasts and thus induces bone resorption and has synergistic effects with the bone-resorptive actions of IL-1 β.[41]
Studies have shown a positive correlation between IL-1 β and TNF-α in chronic periodontitis patients (Vahabi et al.)[63]
Reddy et al. have shown a positive correlation of TNF-α concentration with the extent of periodontal destruction.[64] Level of circulating TNF-α in serum has been seen to have decreased following periodontal therapy.[65] The concentration of IL-1 β was reported to be higher in GCF in cases of chronic periodontitis patients than in gingivitis and control group.
Tumor necrosis factor alpha and its association with systemic diseases
The levels of these cytokines were found to be positively correlated with systemic disease. The levels of IL-1 β and TNF-α were higher in serum of diabetic patients with periodontal disease (Dag A).[66] IL-6 and TNF-α concentrations were little higher in the serum of patients with type-2 diabetes mellitus than that of the control group (Monea A).[67]
The level of TNF-α level was significantly higher in patients with osteoporosis. It was concluded that osteoporosis patients are prone to overproduce TNF-α, which also activates the B-cells and promotes the B-cell activity in the periodontal inflammatory sites, aggravating the periodontal disease[68]
TNF-α level in serum act as diagnostic marker of periodontal disease in patients with Alzheimer disease (Kanakdande V).[69]
Limitations
Although bacteria are the primary etiologic factors in periodontal disease, the patient's host response is a determinant of disease susceptibility. The presence of excessive amount of subgingival and supragingival plaque makes the evaluation of the effect of smoking on periodontal health extremely dif?cult.[43]
Difficulty in determining active disease and ongoing destruction in periodontal tissue by traditional diagnostic aids such as probing depth and attachment loss has proved them to be inadequate in the modern era of periodontal therapeutics.[5] Search for a biomarker for periodontitis has resulted in researchers trying out and finding new molecules that can guide a clinician in many a decision regarding the patient's condition.
Conclusion
These observations suggest a positive association between periodontal disease and increased levels of TNF-α in serum. It can be concluded that there is a prospect of using the estimation of TNF-α in serum as a ” marker” of periodontal disease in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pucher J, Stewart J. Periodontal disease and diabetes mellitus. Curr Diab Rep. 2004;4:46–50. doi: 10.1007/s11892-004-0011-y. [DOI] [PubMed] [Google Scholar]
- 2.Seymour GJ, Gemmell E, Reinhardt RA, Eastcott J, Taubman MA. Immunopathogenesis of chronic inflammatory periodontal disease: Cellular and molecular mechanisms. J Periodontal Res. 1993;28:478–86. doi: 10.1111/j.1600-0765.1993.tb02108.x. [DOI] [PubMed] [Google Scholar]
- 3.Sopori M. Effects of cigarette smoke on the immune system. Nat Rev Immunol. 2002;2:372–7. doi: 10.1038/nri803. [DOI] [PubMed] [Google Scholar]
- 4.Moimaz SA, Zina LG, Saliba O, Garbin CA. Smoking and periodontal disease: Clinical evidence for an association. Oral Health Prev Dent. 2009;7:369–76. [PubMed] [Google Scholar]
- 5.Fine DH, Mandel ID. Indicators of periodontal disease activity: An evaluation. J Clin Periodontol. 1986;13:533–46. doi: 10.1111/j.1600-051x.1986.tb01502.x. [DOI] [PubMed] [Google Scholar]
- 6.Boyce BF, Li P, Yao Z, Zhang Q, Badell IR, Schwarz EM, et al. TNF-αlpha and pathologic bone resorption. Keio J Med. 2005;54:127–31. doi: 10.2302/kjm.54.127. [DOI] [PubMed] [Google Scholar]
- 7.Rossomando EF, White L. A novel method for the detection of TNF-αlpha in gingival crevicular fluid. J Periodontol. 1993;64:445–9. [PubMed] [Google Scholar]
- 8.Teles RP, Likhari V, Socransky SS, Haffajee AD. Salivary cytokine levels in subjects with chronic periodontitis and in periodontally healthy individuals: A cross-sectional study. J Periodontal Res. 2009;44:411–7. doi: 10.1111/j.1600-0765.2008.01119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zou C, Shao J. Role of adipocytokines in obesity-associated insulin resistance. J Nutr Biochem. 2008;19:277–86. doi: 10.1016/j.jnutbio.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Jeong SH, Park JH, Kim JN, Park YH, Shin SY, Lee YH, et al. Up-regulation of TNF-αlpha secretion by cigarette smoke is mediated by Egr-1 in HaCaT human keratinocytes. Exp Dermatol. 2010;19:e206–12. doi: 10.1111/j.1600-0625.2009.01050.x. [DOI] [PubMed] [Google Scholar]
- 11.Gümüs P, Nizam N, Lappin DF, Buduneli N. Saliva and serum levels of B-cell activating factors and tumor necrosis factor-a in patients with periodontitis. J Periodontol. 2014;85:270–80. doi: 10.1902/jop.2013.130117. [DOI] [PubMed] [Google Scholar]
- 12.Medzhitov R. Recognition of microorganisms and activation of the immune response. Nature. 2007;449:819–26. doi: 10.1038/nature06246. [DOI] [PubMed] [Google Scholar]
- 13.Wajant H, Pfeffer K, Pfizenmaier K, Scheurich P. Tumor necrosis factors in 1998. Cytokine Growth Factor Rev. 1998;9:297–302. doi: 10.1016/s1359-6101(98)00013-6. [DOI] [PubMed] [Google Scholar]
- 14.Wang S, Liu J, Zhang J, Lin J, Yang S, Yao J, et al. Glycemic control and adipokines after periodontal therapy in patients with Type 2 diabetes and chronic periodontitis. Braz Oral Res. 2017 Nov 27;31:e90. doi: 10.1590/1807-3107BOR-2017.vol31.0090. doi: 10.1590/1807-3107BOR-2017.vol31.0090. PMID: 29185604. [DOI] [PubMed] [Google Scholar]
- 15.Rossomando EF, Kennedy JE, Hadjimichael J. Tumour necrosis factor alpha in gingival crevicular fluid as a possible indicator of periodontal disease in humans. Arch Oral Biol. 1990;35:431–4. doi: 10.1016/0003-9969(90)90205-o. [DOI] [PubMed] [Google Scholar]
- 16.Shapira L, Soskolne WA, Sela MN, Offenbacher S, Barak V. The secretion of PGE2, IL-1 beta, IL-6, and TNF alpha by adherent mononuclear cells from early onset periodontitis patients. J Periodontol. 1994;65:139–46. doi: 10.1902/jop.1994.65.2.139. [DOI] [PubMed] [Google Scholar]
- 17.Delima AJ, Oates T, Assuma R, Schwartz Z, Cochran D, Amar S, et al. Soluble antagonists to interleukin-1 (IL-1) and tumor necrosis factor (TNF) inhibits loss of tissue attachment in experimental periodontitis. J Clin Periodontol. 2001;28:233–40. doi: 10.1034/j.1600-051x.2001.028003233.x. [DOI] [PubMed] [Google Scholar]
- 18.Gamonal J, Sanz M, O'Connor A, Acevedo A, Suarez I, Sanz A, et al. Delayed neutrophil apoptosis in chronic periodontitis patients. J Clin Periodontol. 2003;30:616–23. doi: 10.1034/j.1600-051x.2003.00350.x. [DOI] [PubMed] [Google Scholar]
- 19.Gaspersic R, Stiblar-Martincic D, Osredkar J, Skaleric U. In vivo administration of recombinant TNF-αlpha promotes bone resorption in mice. J Periodontal Res. 2003;38:446–8. doi: 10.1034/j.1600-0765.2003.00662.x. [DOI] [PubMed] [Google Scholar]
- 20.Vieira BJ, de Souza AR, Aarestrup FM. Tumor necrosis factor-alpha expression and detection of apoptosis at the site of chronic periodontitis in AIDS patients. J Periodontal Res. 2003;38:606–10. doi: 10.1034/j.1600-0765.2003.00701.x. [DOI] [PubMed] [Google Scholar]
- 21.Feghali CA, Wright TM. Cytokines in acute and chronic inflammation. Front Biosci. 1997;2:d12–26. doi: 10.2741/a171. [DOI] [PubMed] [Google Scholar]
- 22.Gokul K. Estimation of the level of tumor necrosis factor-a in gingival crevicular fluid and serum in periodontal health and disease: A biochemical study. Indian J Dent Res. 2012;23:348–52. doi: 10.4103/0970-9290.102221. [DOI] [PubMed] [Google Scholar]
- 23.Erciyas K, Sezer U, Ustün K, Pehlivan Y, Kisacik B, Senyurt SZ, et al. Effects of periodontal therapy on disease activity and systemic inflammation in rheumatoid arthritis patients. Oral Dis. 2013;19:394–400. doi: 10.1111/odi.12017. [DOI] [PubMed] [Google Scholar]
- 24.Saxlin T, Suominen-Taipale L, Leiviskä J, Jula A, Knuuttila M, Ylöstalo P. Role of serum cytokines tumour necrosis factor-alpha and interleukin-6 in the association between body weight and periodontal infection. J Clin Periodontol. 2009;36:100–5. doi: 10.1111/j.1600-051X.2008.01350.x. [DOI] [PubMed] [Google Scholar]
- 25.Boas Nogueira AV, Chaves de Souza JA, Kim YJ, Damião de Sousa-Neto M, Chan Cirelli C, Cirelli JA, et al. Orthodontic force increases interleukin-1β and tumor necrosis factor-a expression and alveolar bone loss in periodontitis. J Periodontol. 2013;84:1319–26. doi: 10.1902/jop.2012.120510. [DOI] [PubMed] [Google Scholar]
- 26.Padial-Molina M, Volk SL, Rodriguez JC, Marchesan JT, Galindo-Moreno P, Rios HF, et al. Tumor necrosis factor-a and porphyromonas gingivalis lipopolysaccharides decrease periostin in human periodontal ligament fibroblasts. J Periodontol. 2013;84:694–703. doi: 10.1902/jop.2012.120078. [DOI] [PubMed] [Google Scholar]
- 27.Farhad SZ, Amini S, Khalilian A, Barekatain M, Mafi M, Barekatain M, et al. The effect of chronic periodontitis on serum levels of tumor necrosis factor-alpha in Alzheimer disease. Dent Res J (Isfahan) 2014;11:549–52. [PMC free article] [PubMed] [Google Scholar]
- 28.Yilmaz G, Kirzioglu FY, Doguç DK, Koçak H, Orhan H. Ghrelin levels in chronic periodontitis patients. Odontology. 2014;102:59–67. doi: 10.1007/s10266-012-0100-3. [DOI] [PubMed] [Google Scholar]
- 29.Singh P, Gupta ND, Bey A, Khan S. Salivary TNF-αlpha: A potential marker of periodontal destruction. J Indian Soc Periodontol. 2014;18:306–10. doi: 10.4103/0972-124X.134566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kosel O, Canakci V, Canakci CF, Yildirim A, Kerme E, Arabaci T, et al. The effects of obesity on local and circulating levels of tumor necrosis factor-a and interleukin-6 in patients with chronic periodontitis. J Periodontol Implant Dent. 2015;7:7–14. [Google Scholar]
- 31.Gonçalves TE, Zimmermann GS, Figueiredo LC, Souza Mde C, da Cruz DF, Bastos MF, et al. Local and serum levels of adipokines in patients with obesity after periodontal therapy: One-year follow-up. J Clin Periodontol. 2015;42:431–9. doi: 10.1111/jcpe.12396. [DOI] [PubMed] [Google Scholar]
- 32.Zhang P, Li YJ, Guo LY, Wang GF, Lu K, Yue EL, et al. Focal adhesion kinase activation is required for TNF-α-induced production of matrix metalloproteinase-2 and proinflammatory cytokines in cultured human periodontal ligament fibroblasts. Eur J Oral Sci. 2015;123:249–53. doi: 10.1111/eos.12191. [DOI] [PubMed] [Google Scholar]
- 33.Malarkodi T, Sathasivasubramanian S. Quantitative analysis of salivary TNF-α in oral lichen planus patients. Int J Dent. 2015;34:23–9. doi: 10.1155/2015/283465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jakovljevic A, Knezevic A, Karalic D, Soldatovic I, Popovic B, Milasin J, et al. Pro-inflammatory cytokine levels in human apical periodontitis: Correlation with clinical and histological findings. Aust Endod J. 2015;41:72–7. doi: 10.1111/aej.12072. [DOI] [PubMed] [Google Scholar]
- 35.Tan J, Zhou L, Xue P, An Y, Luo L, Zhang R, et al. Tumor necrosis factor-a attenuates the osteogenic differentiation capacity of periodontal ligament stem cells by activating PERK signaling. J Periodontol. 2016;87:e159–71. doi: 10.1902/jop.2016.150718. [DOI] [PubMed] [Google Scholar]
- 36.Zhao B, Jin C, Li L, Wang Y. Increased expression of TNF-α occurs before the development of periodontitis among obese Chinese children: A Potential marker for prediction and prevention of periodontitis. Oral Health Prev Dent. 2016;14:71–5. doi: 10.3290/j.ohpd.a35006. [DOI] [PubMed] [Google Scholar]
- 37.Silness J, Loe H. Periodontal disease in pregnancy and correlation between oral hygiene and periodontal conditions. Acta Odontol Scand. 1964;24:747–59. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 38.Loe H, Silness J. Periodontal disease in pregnancy.I Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 39.Listgarten MA, Mao R, Robinson PJ. Periodontal probing and the relationship of the probe tip to periodontal tissues. J Periodontol. 1976;47:511–3. doi: 10.1902/jop.1976.47.9.511. [DOI] [PubMed] [Google Scholar]
- 40.Preshaw PM, Kupp L, Hefti AF, Mariotti A. Measurement of clinical attachment levels using a constant-force periodontal probe modified to detect the cemento-enamel junction. J Clin Periodontol. 1999;26:434–40. doi: 10.1034/j.1600-051x.1999.260704.x. [DOI] [PubMed] [Google Scholar]
- 41.Mayer Y, Balbir-Gurman A, Machtei EE. Anti-tumor necrosis factor-alpha therapy and periodontal parameters in patients with rheumatoid arthritis. J Periodontol. 2009;80:1414–20. doi: 10.1902/jop.2009.090015. [DOI] [PubMed] [Google Scholar]
- 42.Sllamnikudalipi Z, Dragidella F, Disha M, Meqa K, Begolli L, Begolli G. Inflammatory biomarkers as potential mediators for the association between periodontal and systemic disease in Kosovo. J Int Dent Med Res. 2013;6:1–5. [Google Scholar]
- 43.Erdemir EO, Duran I, Haliloglu S. Effects of smoking on clinical parameters and the gingival crevicular fluid levels of IL-6 and TNF-αlpha in patients with chronic periodontitis. J Clin Periodontol. 2004;31:99–104. doi: 10.1111/j.0303-6979.2004.00454.x. [DOI] [PubMed] [Google Scholar]
- 44.Ikezawa I, Tai H, Shimada Y, Komatsu Y, Galicia JC, Yoshie H, et al. Imbalance between soluble tumour necrosis factor receptors type 1 and 2 in chronic periodontitis. J Clin Periodontol. 2005;32:1047–54. doi: 10.1111/j.1600-051X.2005.00832.x. [DOI] [PubMed] [Google Scholar]
- 45.Yongchaitrakul T, Lertsirirangson K, Pavasant P. Human periodontal ligament cells secrete macrophage colony-stimulating factor in response to tumor necrosis factor-alpha in vitro. J Periodontol. 2006;77:955–62. doi: 10.1902/jop.2006.050338. [DOI] [PubMed] [Google Scholar]
- 46.Talbert J, Elter J, Jared HL, Offenbacher S, Southerland J, Wilder RS, et al. The effect of periodontal therapy on TNF-αlpha, IL-6 and metabolic control in type 2 diabetics. J Dent Hyg. 2006;80:7. [PubMed] [Google Scholar]
- 47.Engebretson S, Chertog R, Nichols A, Hey-Hadavi J, Celenti R, Grbic J, et al. Plasma levels of tumour necrosis factor-alpha in patients with chronic periodontitis and type 2 diabetes. J Clin Periodontol. 2007;34:18–24. doi: 10.1111/j.1600-051X.2006.01017.x. [DOI] [PubMed] [Google Scholar]
- 48.Nilsson M, Kopp S. Gingivitis and periodontitis are related to repeated high levels of circulating tumor necrosis factor-alpha in patients with rheumatoid arthritis. J Periodontol. 2008;79:1689–96. doi: 10.1902/jop.2008.070599. [DOI] [PubMed] [Google Scholar]
- 49.Ikezawa-Suzuki I, Shimada Y, Tai H, Komatsu Y, Tanaka A, Yoshie H, et al. Effects of treatment on soluble tumour necrosis factor receptor type 1 and 2 in chronic periodontitis. J Clin Periodontol. 2008;35:961–8. doi: 10.1111/j.1600-051X.2008.01317.x. [DOI] [PubMed] [Google Scholar]
- 50.Dag A, Firat ET, Arikan S, Kadiroglu AK, Kaplan A. The effect of periodontal therapy on serum TNF-αlpha and HbA1c levels in type 2 diabetic patients. Aust Dent J. 2009;54:17–22. doi: 10.1111/j.1834-7819.2008.01083.x. [DOI] [PubMed] [Google Scholar]
- 51.Baser U, Cekici A, Tanrikulu-Kucuk S, Kantarci A, Ademoglu E, Yalcin F, et al. Gingival inflammation and interleukin-1 beta and tumor necrosis factor-alpha levels in gingival crevicular fluid during the menstrual cycle. J Periodontol. 2009;80:1983–90. doi: 10.1902/jop.2009.090076. [DOI] [PubMed] [Google Scholar]
- 52.Ortiz P, Bissada NF, Palomo L, Han YW, Al-Zahrani MS, Panneerselvam A, et al. Periodontal therapy reduces the severity of active rheumatoid arthritis in patients treated with or without tumor necrosis factor inhibitors. J Periodontol. 2009;80:535–40. doi: 10.1902/jop.2009.080447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Mendonça AC, Santos VR, César-Neto JB, Duarte PM. Tumor necrosis factor-alpha levels after surgical anti-infective mechanical therapy for peri-implantitis: A 12-month follow-up. J Periodontol. 2009;80:693–9. doi: 10.1902/jop.2009.080521. [DOI] [PubMed] [Google Scholar]
- 54.Bastos MF, Lima JA, Vieira PM, Mestnik MJ, Faveri M, Duarte PM, et al. TNF-αlpha and IL-4 levels in generalized aggressive periodontitis subjects. Oral Dis. 2009;15:82–7. doi: 10.1111/j.1601-0825.2008.01491.x. [DOI] [PubMed] [Google Scholar]
- 55.Costa AM, Guimarães MC, de Souza ER, Nóbrega OT, Bezerra AC. Interleukin-6 (G-174C) and tumour necrosis factor-alpha (G-308A) gene polymorphisms in geriatric patients with chronic periodontitis. Gerodontology. 2010;27:70–5. doi: 10.1111/j.1741-2358.2009.00291.x. [DOI] [PubMed] [Google Scholar]
- 56.Nakajima T, Honda T, Domon H, Okui T, Kajita K, Ito H, et al. Periodontitis-associated up-regulation of systemic inflammatory mediator level may increase the risk of coronary heart disease. J Periodontal Res. 2010;45:116–22. doi: 10.1111/j.1600-0765.2009.01209.x. [DOI] [PubMed] [Google Scholar]
- 57.Lima HR, Gelani V, Fernandes AP, Gasparoto TH, Torres SA, Santos CF, et al. The essential role of toll like receptor-4 in the control of aggregatibacter actinomycetemcomitans infection in mice. J Clin Periodontol. 2010;37:248–54. doi: 10.1111/j.1600-051X.2009.01531.x. [DOI] [PubMed] [Google Scholar]
- 58.Jaganath S, Vijayendra R. Estimation of tumor necrosis factor-alpha in the gingival crevicular fluid of poorly, moderately and well controlled type 2 diabetes mellitus patients with periodontal disease – A clinical and biochemical study. Indian J Stomatol. 2011;2:159–64. [Google Scholar]
- 59.Rai B, Kaur J, Anand SC. Possible relationship between periodontitis and dementia in a North Indian old age population: A pilot study. Gerodontology. 2012;29:e200–5. doi: 10.1111/j.1741-2358.2010.00441.x. [DOI] [PubMed] [Google Scholar]
- 60.Fentoglu O, Kirzioglu FY, Ozdem M, Koçak H, Sütçü R, Sert T, et al. Proinflammatory cytokine levels in hyperlipidemic patients with periodontitis after periodontal treatment. Oral Dis. 2012;18:299–306. doi: 10.1111/j.1601-0825.2011.01880.x. [DOI] [PubMed] [Google Scholar]
- 61.Akman PT, Fentoglu O, Yilmaz G, Arpak N. Serum plasminogen activator inhibitor-1 and tumor necrosis factor-a levels in obesity and periodontal disease. J Periodontol. 2012;83:1057–62. doi: 10.1902/jop.2011.110548. [DOI] [PubMed] [Google Scholar]
- 62.Teles FR, Teles RP, Martin L, Socransky SS, Haffajee AD. Relationships among interleukin-6, tumor necrosis factor-a, adipokines, Vitamin D, and chronic periodontitis. J Periodontol. 2012;83:1183–91. doi: 10.1902/jop.2011.110346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vahabi S, Sattari M, Taheraslani M, Akbarzadeh Bagheban A. Correlation between interleukin-1β, interleukin-6 and tumor necrosis factor-a and clinical parameters in chronic and aggressive periodontal disease. J Periodontol Implant Dent. 2012;3:51–6. [Google Scholar]
- 64.Reddy NR, Babu DM, Reddy V, Sarath N, Reddy CV, Kumar AK. Estimation of tumor necrosis factor-a in chronic periodontitis and its co-relation with preterm gestation: A clinico biochemical study. J Orofac Sci. 2012;4:108. [Google Scholar]
- 65.Yun F, Firkova EI, Xun H, Jun-Qi L. Effects of surgical periodontal therapy on serum levels of TNF-αlpha in patients with chronic periodontitis. Folia Med (Plovdiv) 2007;49:37–40. [PubMed] [Google Scholar]
- 66.Kimak A, Strycharz-Dudziak M, Bachanek T, Kimak E. Lipids and lipoproteins and inflammatory markers in patients with chronic apical periodontitis. Lipids Health Dis. 2015;14:162. doi: 10.1186/s12944-015-0156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Page RC. The role of inflammatory mediators in the pathogenesis of periodontal disease. J Periodontal Res. 1991;26:230–42. doi: 10.1111/j.1600-0765.1991.tb01649.x. [DOI] [PubMed] [Google Scholar]
- 68.Ursarescu I, Pasarin L, Solomon S, Boatca RM, Martu A, Moise G, et al. The assessment of serum and GCF proinflammatory cytokines levels in patients with osteoporosis and periodontal disease. Roman J Oral Rehab. 2014;6:45–50. [Google Scholar]
- 69.Kanakdande V, Patil KP, Nayyar AS. Comparative evaluation of clinical, hematological and systemic inflammatory markers in smokers and non-smokers with chronic periodontitis. Contemp Clin Dent. 2015;6:348–57. doi: 10.4103/0976-237X.161885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stashenko P, Jandinski JJ, Fujiyoshi P, Rynar J, Socransky SS. Tissue levels of bone resorptive cytokines in periodontal disease. J Periodontol. 1991;62:504–9. doi: 10.1902/jop.1991.62.8.504. [DOI] [PubMed] [Google Scholar]
- 71.Acharya AB, Thakur S, Muddapur MV, Kulkarni RD. Tumor necrosis factor-a, interleukin-4 and -6 in the serum of health, chronic periodontitis, and type 2 diabetes mellitus. J Indian Soc Periodontol. 2016;20:509–13. doi: 10.4103/0972-124X.201694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kurtis B, Tüter G, Serdar M, Akdemir P, Uygur C, Firatli E, et al. Gingival crevicular fluid levels of monocyte chemoattractant protein-1 and tumor necrosis factor-alpha in patients with chronic and aggressive periodontitis. J Periodontol. 2005;76:1849–55. doi: 10.1902/jop.2005.76.11.1849. [DOI] [PubMed] [Google Scholar]


