Abstract
Aim
The aim of this study was to examine whether high social support has a protective effect on mental health for critical care nurses during the coronavirus disease 2019 (COVID‐19) pandemic.
Methods
This cross‐sectional anonymous web‐based survey was conducted from November 5 to December 5, 2020, in Japan and included critical care nurses. The invitation was distributed via mailing lists.
Results
Of the 334 responses that were obtained, 64.4% were from female respondents, and their mean age was 37.4. Of the total, 269 (80.5%) were taking care of COVID‐19 patients at the time the study was conducted. Participants with post‐traumatic stress disorder (PTSD) symptoms were found to be older (P < 0.05), and those with an education level of a 4‐year college degree or higher had fewer PTSD symptoms (P < 0.05). Those experiencing anxiety and depressive symptoms had lower social support scores. Having a 4‐year college degree and higher (odds ratio [OR] 0.622, 95% confidence interval [CI] 0.39–0.99) was significantly associated with a lower probability of PTSD. Social support scores and the female sex were not associated with PTSD. Regarding anxiety symptoms, being female and having lower social support were independently associated with a higher probability. Regarding depression symptoms, lower social support was independently associated with a higher probability (OR 0.953, 95% CI 0.93–0.97).
Conclusion
It was found that social support was not associated with PTSD; however, it was associated with depression and anxiety symptoms for intensive care nurses during the COVID‐19 pandemic.
Keywords: COVID‐19, intensive care unit, mental health, nurses, social support
This study suggests that the social support is not associated with post‐traumatic stress disorder; however, it is associated with depression and anxiety symptoms for intensive care nurses during the coronavirus disease 2019 (COVID‐19) pandemic.
Background
Coronavirus disease 2019 (COVID‐19) has spread across the world alarmingly quickly, including Japan. It was reported that the mortality rate (among severe patients) of the first wave of COVID‐19 in Japan was 12.5%. 1 The mental health of health‐care professionals has been an important issue during the COVID‐19 pandemic, as it influences the quality of care and patient turnover in a hospital. A meta‐analysis including 55 sources examined the mental health of the health‐care professionals who cared for COVID‐19 patients, including their depression, anxiety, and post‐traumatic stress disorder (PTSD), which were experienced by 15.9%, 15.1%, and 21.9%, respectively. In addition, a French multicenter study of intensive care unit (ICU) nurses caring for either moderately or more severely ill patients with COVID‐19 reported that the prevalence of anxiety and depression was 48% and 16%, respectively. 2
Social support is an important factor associated with mental health. 3 It is defined as the network of psychological and material resources available to an individual while coping with stress. There are various types of social support: structural, functional, emotional, instrumental/material, and informational. 4
Several studies have shown that high social support has a protective effect on PTSD in the health‐care profession under the COVID‐19 pandemic situation 5 , 6 ; however, this relationship was not examined among health‐care professions during the ongoing pandemic in Japan. As social support differs among countries, ethnicities, and culture, 7 the aim of this study was to clarify relationships between social support and mental health among nurses during the COVID‐19 pandemic. The findings may contribute to the establishment of psychosocial support for health‐care workers during the ongoing pandemic in Japan.
Methods
Study design
The aim of this study was to examine whether higher social support was associated with a higher mental health status for critical care nurses in the ICU during the COVID‐19 pandemic. The primary outcome was PTSD, and the secondary outcome was anxiety and depression. The survey was a cross‐sectional anonymous web‐based survey.
Setting
The invitation was distributed via the mailing lists of the Japan Society of Intensive Care Medicine and the Japan Society of Physicians and Trainees in Intensive Care; the message requested that the invitation be forwarded to nurses working in the acute care unit. We also posted the invitation on community mailing lists, social network services, such as the Japan Association of Certified Intensive Care Nurses, and local mailing lists that listed the critical care nurses. Data were collected from November 5 to December 5, 2020. The study protocol was approved by the Research Ethics Committee of Kokura Memorial Hospital, and it conforms to the provisions of the Declaration of Helsinki (Approval No. 20091451). Only those who agreed to the informed consent along with the policy of the survey were allowed to answer the questionnaire. This survey was an anonymous web survey and did not include personal information in the responses.
Participants
We included all participants who were nurses working in the acute care unit, including ICUs and progressive care units, regardless of the involvement of care for COVID‐19 patients.
Variables/Measurement
We collected data on age, gender, educational level, nursing experience, and type of acute care unit. We also asked whether participants had direct involvement with confirmed or suspected COVID‐19 patients and/or had experience in end‐of‐life care for that patient population.
Instruments
The Multidimensional Scale of Perceived Social Support 8 measures the degree of social support, which is a determinant of maintaining mental health. The social support scale is a 12‐item questionnaire that consists of three subscales: family support, support of loved ones, and friends’ support. Each item on the social support scale was measured using a 7‐point self‐report scale, ranging from 1 (strongly disagree) to 7 (strongly agree). The sum (range 7–84) of the three subscales represents the total level of social support, where the higher the score, the higher the level of social support. The validity and reliability of the social support scale were also verified.
Hospital Anxiety and Depression Scale (HADS)
The Hospital Anxiety and Depression Scale (HADS) 9 is a commonly used tool that assesses levels of anxiety and depression. The questionnaire comprises 14 questions, 7 each for anxiety and depression; the higher the score (score range: 0–42 points), the stronger the anxiety and depression. The cut‐off values were divided into ranges, with 0–7 points indicating no anxiety and depression, and 8 points or more being evaluated as having anxiety and depression. The validity and reliability of the HADS have already been verified.
Impact of Event Scale‐6 (IES‐6)
The Impact of Event Scale (IES)‐6 has six items (total score range: 0–24) for assessing PTSD symptoms. 10 The IES‐6 was developed based on the widely used IES‐R. The validity and reliability of the IES‐6 were well evaluated. The IES‐6 was rated on a 5‐point Likert scale (0: none–4: very) for the degree of stress within the last week. The cut‐off point was 1.75, with 1.75 or higher indicative of having PTSD symptoms.
Bias
Because our recruitment method involved using mailing lists and social networking services, the response rate could not be calculated. Thus, election bias was not avoided; however, our aim did not include assessing the prevalence of PTSD, anxiety, and depression but, rather, focused on the association between various risk factors and mental health.
Study size
The sample size was calculated using the Pwr package working in the R statistics 3.6.3 environment. For this study, we set a covariate of 9, a significance level of .05, a power of 0.8, and an effect size (Cohen f 2) of 0.05. The sample size of this study was 320 participants.
Statistical methods
Descriptive statistical analyses were conducted, and the variables were presented as median (interquartile range) or percentage. We evaluated the relationships between social support and mental health as exposure and outcomes using a generalized linear model. We predefined confounders, including age, sex, nursing experience, type of acute care unit, and experience of care, for confirmed or suspected COVID‐19 or patients. Data were analyzed using the statistical package SPSS for Windows 18.0J (SPSS, Tokyo, Japan).
Results
We obtained 334 responses, and all were analyzed. The response rate could not be calculated based on our recruitment methodology.
Characteristics
The demographic characteristics of the participants are presented in Table 1. The mean age of participants was 37.4, and 64.4% were female. The mean number of years of clinical experience was 9.4, and three of four respondents worked in the medical‐surgical ICU. Of the total, 229 (68.6%) had housemates, 148 (44.3%) had an education level of 4‐year college or higher, and 269 (80.5%) were taking care of COVID‐19 patients.
Table 1.
Characteristics of participants
| Characteristics | n = 334 |
|---|---|
| Age, mean (SD) | 37.4 (7.6) |
| Sex, n (%) | |
| Female | 215 (64.4) |
| Missing | 1 (0.3) |
| Years of clinical experience, mean (SD) | 9.4 (6.0) |
| Department, n (%) | |
| Medical‐surgical ICU | 248 (74.3) |
| Emergency ICU | 69 (20.7) |
| COVID‐19‐dedicated ICU | 12 (3.6) |
| Other | 5 (1.4) |
| Housemate, n (%) | |
| Yes | 229 (68.6) |
| Missing | 2 (0.6) |
| Highest educational level, n (%) | |
| Vocational school | 170 (50.9) |
| Junior college | 10 (3.0) |
| Four‐year university | 94 (28.1) |
| Graduate school | 54 (16.2) |
| Others | 6 (1.8) |
| Directly involved in COVID‐19 patient care, n (%) | |
| Yes | 269 (80.5) |
| Experience in providing end‐of‐life care for COVID‐19 patients, n (%) | |
| Yes | 77 (23.1) |
| Missing | 1 (0.3) |
| Total social support score, median (IQR) | 67 (17) |
COVID‐19, coronavirus disease 2019; ICU, intensive care unit; IQR, interquartile range; SD, standard deviation.
Outcome variables
Table 2 shows the IES‐R‐6 and HADS scores. The median IES‐R‐6 was 7. The proportion of respondents with PTSD was 36.8%. The median HADS‐Anxiety score was 7, and the HADS‐Depression score was 8. Of the total respondents, 47.6% had anxiety and 56.0% had depression.
Table 2.
Results of IES‐R‐6 and HADS scores
| IES‐R‐6 | |
| Total score, median (IQR) | 7 (5) |
| ≧1.75, n (%) | 123 (36.8) |
| <1.75, n (%) | 210 (62.9) |
| Missing | 1 (0.3) |
| HADS | |
| Total score, median (IQR) | 16 (11) |
| HADS‐Anxiety score, median (IQR) | 7 (6) |
| HADS‐Anxiety | |
| ≦7, n (%) | 159 (47.6) |
| <8, n (%) | 175 (52.4) |
| HADS‐Depression score, median (IQR) | 8 (6) |
| ≦7, n (%) | 187 (56.2) |
| <8, n (%) | 146 (43.8) |
HADS, Hospital Anxiety and Depression Scale, IES‐R‐6, Impact of Event Scale 6; IQR, interquartile range.
Univariate analysis
The univariate analysis identified several characteristics of participants associated with PTSD symptoms. Those having PTSD symptoms were older (P < 0.05). However, those with an education level of 4‐year college or higher had fewer PTSD symptoms (P < 0.05; Table 3).
Table 3.
Relationships between participant’s characteristics and PTSD
| PTSD symptoms | P | ||
|---|---|---|---|
|
Yes n = 123 |
No n = 210 |
||
| Age, mean (SD) | 38.5 (7.7) | 35.8 (7.5) | 0.03 |
| Female, n (%) | 88 (71.5) | 127 (60.5) | 0.10 |
| Clinical experience, year, mean (SD) | 9.7 (6.4) | 9.3 (5.8) | 0.53 |
| Housemate | |||
| Yes, n (%) | 82 (66.7) | 147 (70.0) | 0.70 |
| Highest educational level | |||
| Four‐year university and graduate school, n (%) | 46 (37.4) | 102 (48.6) | 0.03 |
| Directly involved in COVID‐19 patient care, n (%) | 100 (81.3) | 169 (79.3) | 0.85 |
| Experience in providing end‐of‐life care for COVID‐19 patients | |||
| Yes, n (%) | 28 (22.8) | 49 (23.0) | 0.730 |
| Total social support score, median (IQR) | 65 (12) | 68 (14) | 0.47 |
COVID‐19, coronavirus disease 2019; IQR, interquartile range; PTSD, post‐traumatic stress disorder; SD, standard deviation.
Anxiety symptoms were more common in females (P < 0.006). Participants with anxiety and depressive symptoms had lower social support scores (64 versus 68, 62 versus 70, respectively; P < 0.01; Tables 4 and 5).
Table 4.
Relationships between participant’s characteristics and anxiety symptoms
| Anxiety symptoms | P | ||
|---|---|---|---|
|
Yes n = 159 |
No n = 175 |
||
| Age, mean (SD) | 37.5 (7.9) | 37.4 (7.4) | 0.68 |
| Female, n (%) | 115 (72.3) | 100 (57.1) | <0.010 |
| Years of clinical experience, mean (SD) | 9.5 (6.5) | 9.4 (3.5) | 0.88 |
| Housemate, n (%) | 104 (65.4) | 125 (71.4) | 0.47 |
| Highest educational level | |||
| Four‐year university and graduate school, n (%) | 64 (40.3) | 84 (48.0) | 0.14 |
| Directly involved in COVID‐19 patient care, n (%) | 128 (80.5) | 141 (80.6) | 0.92 |
| Experience in providing end‐of‐life care for COVID‐19 patients, n (%) | 37 (23.3) | 40 (22.9) | 0.57 |
| Total social support score, median (IQR) | 64 (15) | 68 (16) | <0.01 |
COVID‐19, coronavirus disease 2019; IQR, interquartile range; SD, standard deviation.
Table 5.
Relationships between participant’s characteristics and depression symptoms
| Depression symptoms | P | ||
|---|---|---|---|
|
Yes n = 187 |
No n = 146 |
||
| Age, mean (SD) | 38.1 (7.7) | 36.6 (7.5) | 0.07 |
| Female, n (%) | 130 (69.5) | 85 (58.2) | 0.06 |
| Years of clinical experience, mean (SD) | 9.7 (6.2) | 9.0 (5.8) | 0.19 |
| Housemate, n (%) | 126 (67.4) | 103 (70.5) | 0.39 |
| Highest educational level | |||
| Four‐year university or graduate school, n (%) | 80 (42.8) | 68 (46.6) | 0.43 |
| Directly involved in COVID‐19 patient care, n (%) | 147 (78.6) | 122 (83.6) | 0.26 |
| Experience in providing end‐of‐life care for COVID‐19 patients, n (%) | 45 (24.1) | 32 (21.9) | 0.60 |
| Total social support score, median (IQR) | 62 (12) | 70 (12) | <0.01 |
COVID‐19, coronavirus disease 2019; IQR, interquartile range; SD, standard deviation.
Multivariate analysis
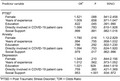
Binary logistic regression analysis was used to clarify the risk of PTSD, anxiety, and depressive symptoms (Table 6).
Table 6.
Binary logistic regression analysis of PTSD, anxiety, and depression risk factor
| Predictor variable | OR | P | 95% CI |
|---|---|---|---|
| PTSD | |||
| Female | 1.521 | 0.088 | 0.941–2.458 |
| Years of experience | 1.009 | 0.658 | 0.971–1.047 |
| Education | 0.622 | 0.045 | 0.391–0.990 |
| Directly involved in COVID‐19 patient care | 1.084 | 0.783 | 0.610–1.928 |
| Social support | 0.999 | 0.881 | 0.982–1.016 |
| Anxiety | |||
| Female | 1.780 | 0.016 | 1.12–2.829 |
| Years of experience | 0.994 | 0.755 | 0.958–1.032 |
| Education | 0.786 | 0.292 | 0.502–1.230 |
| Directly involved in COVID‐19 patient care | 1.094 | 0.753 | 0.624–1.920 |
| Social support | 0.979 | 0.017 | 0.962–0.996 |
| Depression | |||
| Female | 1.349 | 0.210 | 0.844–2.156 |
| Years of experience | 1.012 | 0.562. | 0.973–1.052 |
| Education | 1.021 | 0.928 | 0.644–1.619 |
| Directly involved in COVID‐19 patient care | 0.759 | 0.360 | 0.421–1.369 |
| Social support | 0.953 | <0.001 | 0.934–0.972 |
CI, confidence interval; COVID‐19, coronavirus disease 2019; OR, odds ratio; PTSD, post‐traumatic stress disorder.
Having a bachelor’s degree or higher (odds ratio [OR] 0.622, 95% confidence interval [CI] 0.39–0.99) was significantly associated with a lower probability of PTSD. Social support scores and being female were not associated with PTSD. For anxiety symptoms, females and lower social support were independently associated with a higher probability of anxiety symptoms (OR 1.78, 95% CI 1.12–2.83 and OR 0.979, 95% CI 0.96–0.99, respectively). For depression symptoms, lower social support was independently associated with a higher probability of depression symptoms (OR 0.953, 95% CI 0.93–0.97). Being directly involved in dealing with COVID‐19 patients was not significantly associated with any mental health problems.
Discussion
According to a fixed point on the number of critically ill patients provided by the ECMOnet (the extracorporeal membrane oxygenation network) in Japan, 11 at the beginning of the study, there were 130 COVID‐19 patients in Japan requiring mechanical ventilation, but as of the end of the study, the number had increased to 450. The increase in critically ill patients reflected the third wave of COVID‐19 in Japan. In this study, more than 80% of respondents provided direct care for COVID‐19 patients. The percentage of respondents who had symptoms of PTSD, anxiety, and depression were 36.8%, 47.6%, and 60.0%, respectively. Social support was not associated with PTSD symptoms. An education level of a 4‐year college degree or higher was associated with fewer PTSD symptoms. Surprisingly, being directly involved in treating COVID‐19 patients was not an independent factor for the development of mental illness in nurses. Anxiety and depressive symptoms were more common in women, with higher social support being associated with a lower prevalence of anxiety and depression.
Social support was not associated with PTSD symptoms. Poor social support was associated with higher severity of PTSD symptoms. 12 However, higher social support at the time of exposure was not always associated with the severity of PTSD symptoms. Cool and Bickman 13 found that social support was not associated with psychological distress a week after a natural disaster; however, social support was significantly associated with psychological distress 6 weeks following the natural disaster. Therefore, social support may only influence the maintenance of PTSD and not the early phase of exposure. 14 In this cross‐sectional study, the duration between responding and exposure varied. In Japan, the first wave of COVID‐19 was in April. The second wave was relatively mild. During the recruitment of the sample, the third wave of COVID‐19 hit, leading to an increase in patients. Therefore, the population included in this study was with a mixture of those who had cared for COVID‐19 patients recently and those who had cared for them several months prior.
Being directly involved in caring for COVID‐19 patients was not associated with PTSD symptoms. Providing direct care to COVID‐19 patients has been reported in several previous studies to be a risk factor for PTSD. 15 , 16 However, in this study, directly caring for such patients was not significantly associated with PTSD symptoms. This may be due to the fact that PTSD symptoms have been suggested to be caused by direct and indirect exposure to stressful events. 17 Indirect exposure includes anticipation of a stressful event occurring in the future and obtaining damaging information about COVID‐19 infection from media reports. In this present study, even respondents who did not provide direct care to COVID‐19 patients may have expected that they might provide direct care to COVID‐19 patients in the near future, given the rapid spread of COVID‐19 leading to an increased number of critically ill patients. This may have led to PTSD symptoms.
An education level of 4‐year college or higher was associated with a lower frequency of PTSD symptoms. These findings were consistent with those of previous studies. 18 , 19 In a meta‐analysis that evaluated PTSD symptoms following an earthquake, people with high education levels and high social status had substantial social and economic resources and stated that the possibility of using better coping strategies may have influenced the reduction of PTSD symptoms. 19 Although social status was not measured in this study, it is possible that due to receiving a high level of education, various coping strategies for stressful events may have led to a reduction in PTSD symptoms.
High social support was associated with a lower prevalence of anxiety and depression. Previous studies have also reported that social support can reduce stress levels and anxiety in health‐care providers caring for COVID‐19 patients. 5 , 20
Anxiety and depressive symptoms appear as stress reactions when experiencing a stressful event for the first time. The presence of a person who supports them could provide emotional support, and it is conceivable that it functions to reduce those symptoms.
Limitations
Our study has several limitations. First, the population of this survey may not reflect the population working in the ICU due to the study design. However, our purpose was not to describe the prevalence of psychiatric symptoms but to test hypotheses that social support was associated with the development of PTSD; thus, we feel that this limitation did not influence our results.
Second, the duration between the exposure of events and response to the survey varied for each respondent. Psychiatric symptoms change over time; thus, it may reflect the pandemic status and region where the respondent worked. The reproducibility of this study is, therefore, challenging.
Third, we used the IES‐6, which is a short version of the IES‐R. The IES‐6 was used in the health‐care profession in a previous study; however, the IES‐R was essentially validated in patients with acute respiratory distress syndrome. In addition, it was used for screening, not for diagnosis. For a more accurate evaluation of PTSD, diagnostic interviews by psychiatrists are needed.
We found that directly dealing with COVID‐19 patients was not associated with PTSD symptoms, indicating that it can be caused by direct and indirect exposure to COVID‐19. Therefore, it is necessary to establish a mental health support system not only for nurses who directly care for COVID‐19 patients but also for all nurses working in ICUs.
Besides, social support has been shown to alleviate anxiety and depressive symptoms. In addition to emotional support such as encouragement, cheering, and listening, timely communication of updated COVID‐19 information, support for nurses’ own self‐care, and acknowledgement of their work are measures that can reduce stress and prevent the onset of PTSD. 4
Conclusions
Social support was not associated with PTSD; however, high social support was associated with a lower prevalence of anxiety and depression among intensive care nurses during the COVID‐19 pandemic. Furthermore, the participants being directly involved in care for COVID‐19 patients was not an independent factor for impaired mental health in this population. Thus, it can be concluded from the findings that mental support is needed regardless of whether care for COVID‐19 patients is involved.
Disclosure
Approval of the Research Protocol: The study protocol was approved by the Research Ethics Committee of Kokura Memorial Hospital, Fukuoka, Japan (No. 20091451).
Informed Consent: Not applicable.
Registration and the Registration No. of the study/trial: Not applicable.
Animal Studies: Not Applicable.
Conflict of Interest: All authors declare no conflicts of interest in this article.
Acknowledgements
We thank Editage (www.editage.com) for English language editing.
Funding Information
No funding information provided.
References
- 1. Oda J, Muguruma T, Matsuyama S et al. JAAM nationwide survey on the response to the first wave of COVID‐19 in Japan. Part II: how did medical institutions overcome the first wave and how should they prepare for the future? Acute Med. Surg. 2020; 7: e614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Caillet A, Coste C, Sanchez R, Allaouchiche B. Psychological impact of COVID‐19 on ICU caregivers. Anaesth. Crit. Care Pain. Med. 2020; 39: 717–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cohen S. Social relationships and health. Am. Psychol. 2004; 59: 676–84. [DOI] [PubMed] [Google Scholar]
- 4. Sherbourne CD, Stewart AL. The Mos Social Support Survey. Soc. Sci. Med. 1991; 32: 705–14. [DOI] [PubMed] [Google Scholar]
- 5. Muller AE, Hafstad EV, Himmels JPW et al. The mental health impact of the COVID‐19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020; 293: 113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bonsaksen T, Heir T, Bredal IS, Ekeberg O, Skogstad L, Grimholt TK. Post‐traumatic stress and associated factors during the early stage of the COVID‐19 pandemic in Norway. Int. J. Environ. Res. Public Health. 2020; 17: 9210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sherman DK, Kim HS, Taylor S. Culture and social support: neural bases and biological impact. Prog. Brain Res. 2009; 178: 227–37. [DOI] [PubMed] [Google Scholar]
- 8. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J. Pers. Assess. 1988; 52: 32–41. [DOI] [PubMed] [Google Scholar]
- 9. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta. Psychiatr. Scand. 1983; 67: 361–70. [DOI] [PubMed] [Google Scholar]
- 10. Giorgi G, Perez FSF, D’Antonio AC et al. Psychometric properties of the impact of Event Scale‐6 in a sample of victims of bank robbery. Psychol. Res. Behav. Manag. 2015; 8: 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Japan ECMOnet for COVID‐19 . Nationwide system to centralize decisions around ECMO use for severe COVID‐19 pneumonia in Japan. J. Intensive Care. 2020; 8: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID‐19 pandemic‐A review. Asian J. Psychiatr. 2020; 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cook JD, Bickman L. Social support and psychological symptomatology following a natural disaster. J. Trauma Stress. 1990; 3: 541–56. [Google Scholar]
- 14. Robinaugh DJ, Marques L, Traeger LN et al. Understanding the relationship of perceived social support to post‐trauma cognitions and posttraumatic stress disorder. J. Anxiety Disord. 2011; 25: 1072–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson SU, Ebrahimi OV, Hoffart A. PTSD symptoms among health workers and public service providers during the COVID‐19 outbreak. PLoS One 2020; 15: e0241032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zandifar A, Badrfam R, Khonsari NM, Mohammadi MR, Asayesh H, Qorbani M. Prevalence and associated factors of posttraumatic stress symptoms and stigma among health care workers in contact with COVID‐19 patients. Iran J. Psychiatry. 2020; 15: 340–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bridgland VME, Moeck EK, Green DM et al. Why the COVID‐19 is a traumatic stressor. PLoS One 2021; 16: e0240146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reneses B, Garrido S, Navalon A et al. Psychiatric morbidity and predisposing factors in a primary care population in Madrid. Int. J. Soc. Psychiatry. 2015; 61: 275–86. [DOI] [PubMed] [Google Scholar]
- 19. Tang B, Deng Q, Glik D, Dong J, Zhang L. A meta‐analysis of risk factors for post‐traumatic stress disorder (PTSD) in adults and children after earthquakes. Int. J. Environ. Res. Public Health. 2017; 14: 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease (COVID‐19) in January and February 2020 in China. Med. Sci. Monit. 2020; 26: e923549. [DOI] [PMC free article] [PubMed] [Google Scholar]


