Abstract
Background
Although cardiac rehabilitation (CR) is a Class I Guideline recommendation, shown to be a cost-effective intervention following a cardiac event, it has been reimbursed at levels insufficient to cover hospital operating costs. In January 2011, Medicare increased payment for CR in hospital outpatient settings by approximately 180%. We evaluated the association between this payment increase and participation in CR of eligible Medicare beneficiaries to better understand the relationship between reimbursement policy and CR utilization.
Methods
From a 5% Medicare claims sample, we identified patients with acute myocardial infarction, coronary artery bypass surgery, percutaneous coronary intervention, or cardiac valve surgery between January 1, 2009 and September 30, 2012, alive 30 days after their event, with continuous enrollment in Medicare fee-for-service, Part A/B for four months. Trends and changes in CR participation were estimated using an interrupted time series approach with a hierarchical logistic model, hospital random intercepts, adjusted for patient, hospital, market, and seasonality factors. Estimates were expressed using average marginal effects on a percent scale.
Results
Among 76,695 eligible patients, average annual CR participation was 19.5% overall. In the period prior to payment increase, adjusted annual participation grew by 1.1 percentage points (95% Confidence Interval (CI): 0.48, 2.4). No immediate change occurred in CR participation when the new payment was implemented. In the period after payment increase, on average 20% of patients participated in CR annually. The annual growth rate in CR participation slowed in the post-period by 1.3 percentage points (95% CI: −2.4, −0.12) compared to the prior period. Results were somewhat sensitive to time window variations.
Conclusions
The 2011 increase in Medicare reimbursement for CR was not associated with an increase in participation. Future studies should evaluate whether payment did not reach a threshold to incentivize hospitals or if hospitals were not sensitive to reimbursement changes.
Keywords: cardiac rehabilitation, Medicare, payment, utilization, hospital
INTRODUCTION
Cardiac rehabilitation (CR) is an outpatient, exercise-based, multidisciplinary treatment approach with demonstrated improvement in outcomes1 and is a Class I Guideline recommendation for patients with eligible cardiac diagnoses.2,3 CR has been shown to be a cost-effective treatment,4 but financial analysis suggests that historically, reimbursement did not cover operational costs of maintaining a service facility.5 The Centers for Medicare and Medicaid Services (CMS) reimbursement rates for CR increased steadily from a national average of $68 to $104 per hour-long session between 2011 and 2014. However, in 2011, the hospital payment rates increased by approximately 180%, from the prior national average of $38 to $68; a substantial jump from previous incremental increases.6
It is unknown whether this 2011 increase to CR reimbursement translated to a change in patient participation that could suggest hospitals respond to changes to CR payment. Although some healthcare services, especially non-emergent ones, are moderately price sensitive for consumers,7 it has been more difficult to understand the extent to which hospitals respond to reimbursement changes, especially relative to services such as CR.8 Examples of hospital responsiveness to payment changes might be provided by bundled payment initiatives, such as the Medicare Acute Care Episode9 demonstration and the Bundled Payments for Care Improvement10 initiative. Both were directed at improving hospital care quality and lowering costs. Overall, these voluntary bundled payment initiatives have not produced significant changes in care quality or costs.11 However, net cost savings were observed for coronary revascularization procedures,9 as were improvements in 90-day mortality for patients following acute myocardial infarct (AMI).11 Thus, questions remain about the extent to which hospitals are responsive to bundled payment incentives for cardiovascular diagnoses11,12 and whether insight about such responsiveness would translate to utilization of CR.13 Despite these and other ongoing explorations into novel payment models, no Medicare initiatives have been implemented to explicitly encourage greater participation in CR, and no data exist on whether hospitals are responsive to reimbursement changes for CR.
The objective of this study was to test the association between the 2011 increase in payment for CR to hospitals and CR participation among Medicare fee-for-service beneficiaries with AMI, coronary artery bypass graft (CABG) surgeries, percutaneous coronary intervention (PCI), or cardiac valve surgeries. Based on historical trends for gradual and incremental shifts in the uptake of other secondary prevention programs,14,15 we hypothesized that there would be no immediate shift from baseline in January 2011 when the policy was implemented, but that an increase in growth of CR participation would be observed following the payment increase. The implications of such a result could be that hospitals are sensitive to financial incentives for CR participation and that additional payment strategies may spur modifications in hospital care practices such that more eligible patients participate in CR.
METHODS
Data Sources
The study was conducted using a 5% random sample of Limited Data Set (LDS), Medicare Fee-For-Service claims, including inpatient, outpatient, and carrier files, from 2009 through 2012. LDS files include limited Personal Health Information (dates of service, limited date of death information, age at end of calendar year, and state and county of residence). Hospital characteristics were ascertained from the Healthcare Cost Report Information System (HCRIS),16 Area Health Resources Files (AHRF),17 and American Hospital Association (AHA) Survey data.18
The Colorado Multiple Institutional Review Board deemed this study exempt with waiver of consent on June 20, 2017 in accordance with federal regulations (45 CFR 46.102(f)). Due to the specific data use agreement applicable to this research (CMS Data Use Agreement number 28321), the data cannot be made available to other researchers for the purposes of reproducing the results or replicating the procedure.
Study Population
From inpatient files, we identified patients eligible for CR using the first or second diagnosis billing codes for AMI (410.x) from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). From inpatient and outpatient claims, additional eligible patients were identified using ICD-9-Procedure Codes, Healthcare Common Procedure Coding System (HCPCS) codes, and Current Procedural Terminology (CPT) codes for CABG (36.1x, 36.2, 335xx, and S220x), PCI (0.66, 36.0x, and 929xx), and cardiac valve surgeries (35.x, 33361–33417, 33418–33430, 33460–33468, and 33470–33478).
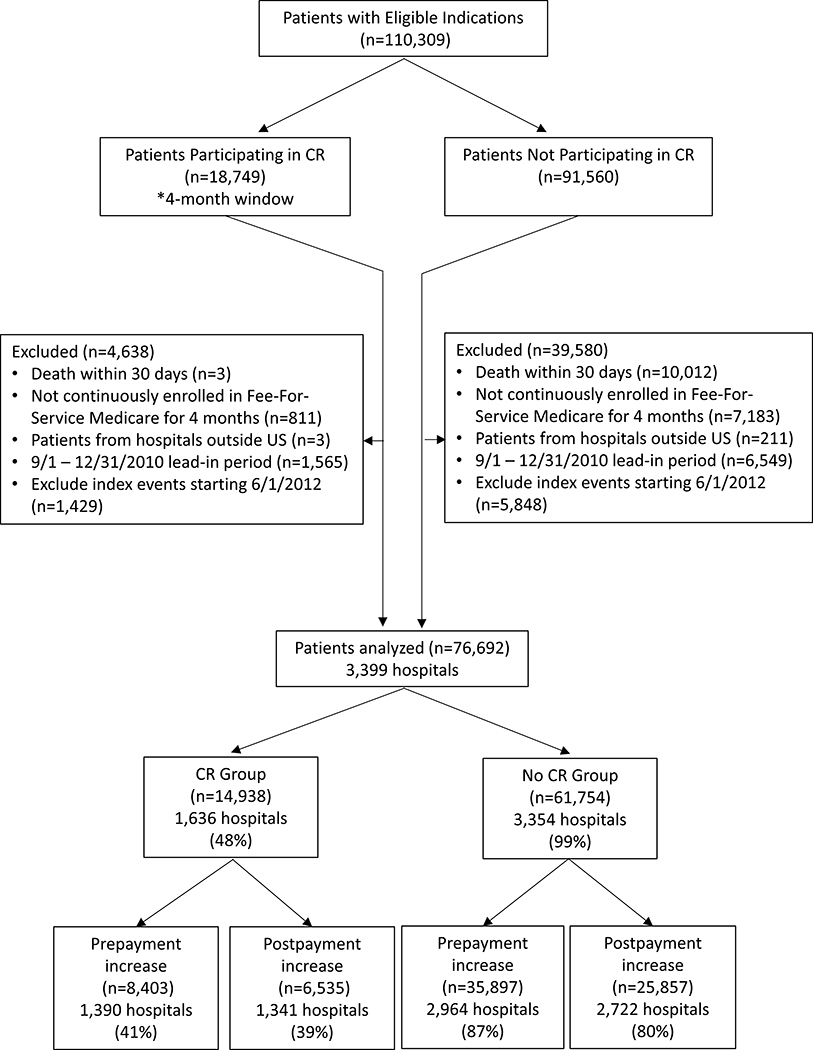
Patients eligible for CR following an AMI, CABG, PCI, or cardiac valve surgery were included (Figure 1). Only a patient’s first qualifying event during the period from January 1, 2009 to May 31, 2012 was included for analysis. Patients with more than one eligible indication were assigned a single indication for the analysis using the hierarchy of 1-AMI, 2-CABG, 3-PCI, and 4-cardiac valve surgery. Patients were excluded if they did not have continuous fee-for-service enrollment in Medicare Parts A and B in the four months following their index event or if they died within 30 days of the index event, to mitigate selection bias in the CR participation group due to missing claims data or acute illness, respectively. Patients with an index event occurring between September 1, 2010 to December 31, 2010 were excluded as a transitional lead-in period to eliminate those whose four-month episodic window spanned the date of the payment implementation. This exclusion also considered that knowledge of the payment increase was available to hospitals, so they may have been preparing in anticipation of its implementation if they were going to make changes.
Figure 1.
Flowchart Showing Extraction Criteria for Cardiac Rehabilitation (CR) Eligible Sample.
Primary Outcome: Participation in CR
Participation in CR was defined as a patient participating in at least one CR session at any place of service, including hospital outpatient settings, doctors’ offices, Critical Access Hospitals, or Federally Qualified Health Centers. Participation was determined using HCPCS codes 93797, 93798, G0422, and G0423 from outpatient and carrier claims. Because more than 90% of all patients who initiated CR within a year began within four months of their index event, and because patients who start CR after four months are likely to be different from those that start within that period (e.g., sicker, recurrent events, other extenuating circumstances), we evaluated CR participation only within four months of the index event.
Covariates
Patient characteristics were ascertained from the Medicare LDS denominator files and included sex, race (white, black, and other), and age at the end of the index event calendar year. The Charlson Comorbidity Index (CCI) was included for the month the index event occurred to assess general disease severity, as well as the CR-indicated event category (AMI, CABG, PCI, or valve surgeries) that qualified the patient. Current Medicare entitlement status was included to control for end stage renal disease and disability status. The type of facility where a patient participated in CR was obtained from outpatient and carrier claims.
Hospital characteristics extracted from the HCRIS data files included: census region (Northeast, Midwest, South, and West), ownership type (non-profit, for-profit, and non-federal government), number of beds, hospital type (general or specialty hospital), rurality, and medical school affiliation. Whether the hospital was part of a healthcare system was obtained from AHA Survey data. Medicare claims were used to determine whether the hospital offered a CR program based on whether a provider identification number was associated with CR service claims. Market factors were ascertained from the HCRIS and AHRF data files. Percent of Medicare discharges by hospital and market competitiveness, estimated using hospital discharges to construct a Herfindahl-Hirschman Index (HHI) for each Hospital Referral Region (HRR), were obtained from the HCRIS database. The percent uninsured by county and the percentage Medicare Advantage penetration in the hospital’s county by year, aggregated to the HRR, were extracted from the AHRF data files.
Statistical Analysis
We calculated descriptive statistics for patient and hospital characteristics for the two time periods. Percent missing was less than 0.8% of patients and 4.4% of hospitals for some hospital covariates and were imputed as as the mean of ten multivariate imputed values using an iterative Markov Monte Carlo method (Supplemental Table I). Correct linkages of hospital ID codes were confirmed between databases by comparing merged datasets. Chi-square tests were used for categorical variables and two-sample t-tests were used for continuous variables in univariate analyses. A formal power calculation was not conducted because our sample met suggested guidelines for power previously described for interrupted time series.19,20
Using methods previously described,19,21 we used an interrupted time series model to test our hypothesis. To estimate changes in CR use following the payment increase, we fit a hierarchical logistic regression model for probability of CR participation for patients nested within index hospitals, where the dependent variable was whether a patient participated in at least one CR session and the intervention of interest was the increase in reimbursement that began on January 1, 2011. We controlled for patient, hospital, and market covariates. Seasonality was controlled for using eleven binary variables that indicated in which month each index event occurred, relative to January. Time variables indicated elapsed time by month in the pre-period and elapsed month in the post-period. Whether the index event occurred in the pre-period or the post-period was represented by a binary payment variable. We used a mixed effects model with random intercept (melogit in Stata, StataCorp, College Station, TX, USA) to control for unexplained random variation between hospitals, which we assumed was normally distributed. Effects were quantified on the percent CR participation scale using average marginal effects. Robust standard errors were calculated to correct for potential serial correlation in the data.22
Additional Analyses
First, we tested whether there was a change after the payment increased relative to a hospital offering a CR program. Hospitals that offered CR were identified in two ways: a) using the CR offered variable that indicated whether a hospital had a CR claim billed from its Medicare billing code anywhere in the available 5% LDS claims set and, b) identifying those hospitals where the Medicare billing codes from patients’ index hospitals could be matched with the CR facility where they participated. In both cases, subgroups of patients with index events at hospitals with and without CR were tested separately in the model, and then the entire cohort was tested in a model that included interaction terms for each time series variable (pre-payment slope, at the time of implementation, and post-payment slope change) with the variable indicating whether a hospital offered CR.
Second, because only hospitals received the increased payment, we tested whether receipt of CR at either non-hospital ambulatory care centers, including Critical Access Hospitals and Federally Qualified Health Centers, or doctor’s offices, shifted relative to receipt of CR at a hospital following the payment increase; the hospital where the qualifying index event occurred may not have been where the corresponding CR session occurred. This analysis was done by testing for associations between the payment increase and changes in CR participation for the subgroups of patients who participated in CR at a) a hospital setting versus a doctor’s office, and b) a hospital setting versus a non-hospital ambulatory care facility.
Third, to determine whether small groups of patients were driving the results, we tested whether excluding patients with qualifying index events at Critical Access Hospitals and Federally Qualified Health Centers, or doctor’s offices changed the association between the increased payment and CR participation. To test the association between the increased payment and participation among groups of patients who participated in CR outside the designated time window, we changed the episodic window for CR participation from four months to three months and also to twelve months. Two additional specifications were tested that excluded deaths up to three months with a three-month episodic window and deaths up to four months with the four-month episodic window to assess if these deaths affected the models. Models were also run excluding hospitals with fewer than twelve eligible patients per period.
Fourth, we tested sensitivity of the model to the length of the pre- and post-payment time windows. By monthly increment, index events were excluded from the pre-payment period, the post-payment period, and both ends of the study period.
Finally, specificity of the model was tested by changing the payment implementation date to a false date of March 23, 2010 to emulate the legislative passage of the Affordable Care Act (ACA). This date was used because increases to CR payment were not part of the ACA provisions and changes for Medicare beneficiaries would not be expected; therefore, it is unlikely that a change to CR participation would be observed at that time.
RESULTS
The analytic sample consisted of 76,692 patients with eligible index events and four months continuous enrollment in fee-for-service, Part A and Part B Medicare, occurring at 3,399 hospitals from January 1, 2009 through September 30, 2012 (Figure 1). In the period prior to the payment increase, 44,300 patients were included. In the period following the payment increase, 32,392 patients were included. Across the entire study period, 14,938 patients (19.5% of patients) from 1,636 hospitals (48% of hospitals) participated in CR within four months of their event, with 8,403 patients participating in the period before the payment increase (19.0%), and 6,535 participating in the period following the payment increase (20.2%) (Figure 2).
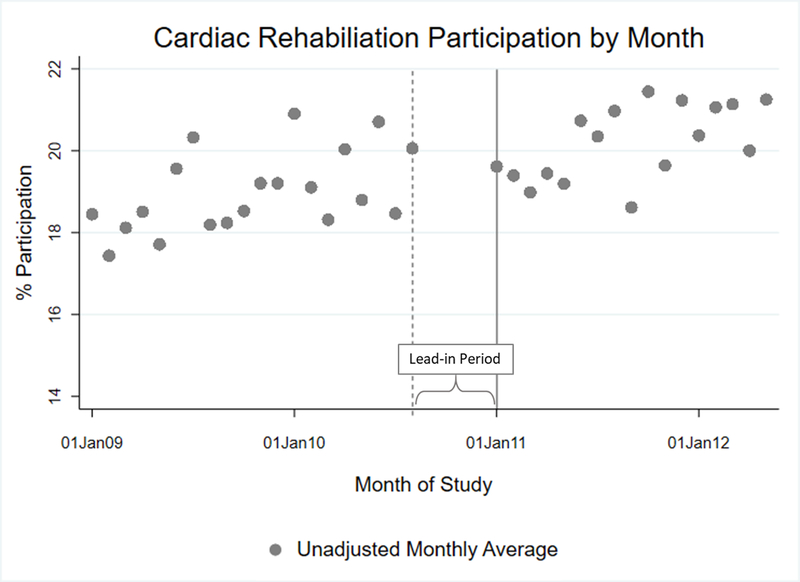
Figure 2.
Mean Unadjusted Percent Cardiac Rehabilitation Participation Rate by Month.
Unadjusted mean percent cardiac rehabilitation (CR) participation by month. The gray circles represent the mean percent of CR-eligible patients who participated in at least one CR session within four months of their index event. The solid vertical line represents the date the payment increase was implemented, January 1, 2011. The dashed vertical line represents the start of the lead-in period. Patients whose index events occurred between September 1, 2010 and December 31, 2010 were excluded during this lead-in period because their 4-month episodic window spanned the date the new payment was implemented.
Hospital Characteristics
Univariate analyses indicate that the characteristics of the groups of hospitals did not substantially change between the two time periods (Table1). The proportions of hospitals in each period with at least one CR participant, ownership status, distribution across census regions, proportions of specialty hospitals, teaching hospitals, and the proportion of hospitals offering CR remained consistent. In the period following the payment increase, hospitals tended to be larger, more urban, and more likely to be a part of a larger hospital system (Table 1). Additionally, Medicare Advantage penetration and the percent insured by county increased in the post-period (Table 1).
Table 1.
Hospital Characteristics Before and After Payment Increase for Cardiac Rehabilitation
| Hospitals before payment increase n=3,000 n (%) |
Hospitals after payment increase n=2,768 n (%) |
p-value | |
|---|---|---|---|
| At least 1 cardiac rehab participant | 1,390 (46.3) | 1,341 (48.4) | 0.12 |
| Hospital ownership | 0.23 | ||
| Non-profit | 2,089 (69.6) | 1,949 (70.4) | |
| For-profit | 470 (15.7) | 454 (16.4) | |
| Non-federal government | 441 (14.7) | 365 (13.2) | |
| Bed size | 0.09 | ||
| ≤ 99 | 800 (26.7) | 656 (23.7) | |
| 100–199 | 766 (25.5) | 704 (25.4) | |
| 200–299 | 518 (17.3) | 499 (18.0) | |
| 300–399 | 364 (12.1) | 353 (12.7) | |
| ≥ 400 | 552 (18.4) | 556 (20.1) | |
| Average beds, mean (standard error) | 253 (4.21) | 267 (4.48) | 0.02 |
| Census region | 0.91 | ||
| Northeast | 506 (16.9) | 476 (17.2) | |
| Midwest | 784 (26.1) | 705 (25.5) | |
| South | 1,167 (38.9) | 1,094 (39.5) | |
| West | 543 (18.1) | 493 (17.8) | |
| Part of a hospital system | 1,921 (64.03) | 1,869 (67.5) | <0.01 |
| Rural locale | 929 (31.0) | 746 (26.9) | <0.01 |
| Specialty hospital | 31 (1.0) | 27 (1.0) | 0.83 |
| Teaching hospital | 87 (2.9) | 93 (3.4) | 0.32 |
| Cardiac rehab offered by hospital | 1,779 (59.3) | 1,695 (61.2) | 0.13 |
| Market factors, mean (standard error) | |||
| % hospital Medicare discharges | 38.8 (0.23) | 38.3 (0.23) | 0.12 |
| % uninsured in county | 17.6 (0.10) | 17.2 (0.11) | 0.02 |
| % Medicare Advantage penetration | 22.4 (0.25) | 24.2 (0.26) | <0.01 |
| Herfindahl-Hirschman Index | 0.15 (0.002) | 0.15 (0.002) | 0.30 |
Patient Characteristics
Univariate characteristics of patient groups before and after the payment increase did not substantially change (Table 2). Age and sex were consistent between the two periods. An increase in the proportion of non-white patients and an increase in mean patient comorbidity scores were observed in the period following the payment increase (Table 2). There was an increase in the rates of AMI and valve surgeries in the post-period that corresponded to decreases in the rates of CABG and PCI between the two periods (Table 2).
Table 2.
Patient Characteristics Before and After Payment Increase for Cardiac Rehabilitation
| Patients in pre-period n=44,300 n (%) |
Patients in post-period n=32,392 n (%) |
p-value | |
|---|---|---|---|
| Age | 0.14 | ||
| <65 | 6,435 (14.5) | 4,743 (14.6) | |
| 65–75 | 19,322 (43.6) | 14,085 (43.5) | |
| 76–85 | 13,892 (31.4) | 10,010 (30.9) | |
| >85 | 4,651 (10.5) | 3,554 (11.0) | |
| Female | 18,982 (42.8) | 13,779 (42.5) | 0.39 |
| Race | <0.01 | ||
| White | 38,738 (87.4) | 28,087 (86.7) | |
| Black | 3,565 (8.0) | 2,726 (8.4) | |
| Other | 1,997 (4.51) | 1,579 (4.9) | |
| Qualifying Indication | <0.01 | ||
| AMI (1st position) | 15,423 (34.8) | 11,994 (37.0) | |
| AMI (2nd position) | 4,175 (9.4) | 3,575 (11.0) | |
| AMI (1st or 2nd position) | 19,577 (44.2) | 15,546 (48.0) | |
| CABG | 5,739 (12.9) | 3,948 (12.2) | |
| PCI | 16,648 (37.6) | 10,897 (33.6) | |
| Valve surgeries | 2,336 (5.3) | 2,001 (6.2) | |
| ≥ 2 events on index date | 9,040 (20.4) | 7,393 (22.8) | <0.01 |
| Current reason for Medicare entitlement | 0.08 | ||
| Aged without ESRD | 37,869 (85.5) | 27,678 (85.5) | |
| Aged with ESRD | 1,035 (2.3) | 776 (2.4) | |
| Disabled without ESRD | 4,642 (10.5) | 3,353 (10.4) | |
| Disabled with ESRD | 703 (1.6) | 564 (1.7) | |
| ESRD only | 51 (0.1) | 21 (0.1) | |
| Charlson Comorbidity Index in month of index event, mean (95% CI) | 4.41 (4.38–4.81) | 4.78 (4.74–4.81) | <0.01 |
AMI=acute myocardial infarct(ion); CABG=coronary artery bypass surgery; PCI=percutaneous coronary intervention; ESRD=end-stage renal disease
Factors Predictive of CR Participation
In the fully adjusted multivariable model, patient factors that were associated with a lower likelihood of CR participation included non-white race, older age, female, and more severe CCI scores (p<0.01) (Table 3). Patients with diagnoses of AMI were less likely to participate in CR than those with CABG, PCI, and valve surgeries (p<0.05). Patients with end-stage renal disease (ESRD) or who were disabled were less likely to participate in CR than patients without those conditions (p<0.01).
Table 3.
Average Marginal Effects for Probability of Cardiac Rehabilitation Participation by Month with Hospital Random Effects
| Model 1: Unadjusted | Model 2: Fully adjusted | |||||
|---|---|---|---|---|---|---|
| Independent variables | AME estimates (95% CI) | AME estimates (95% CI) | ||||
| Pre-period slope (monthly) | 0.0006 | (0.0001, 0.001) | † | 0.0009 | (0.0003, 0.002) | † |
| Implementation of payment increase (level change) | −0.003 | (−0.014, 0.007) | 0.0029 | (−0.009, 0.015) | ||
| Post-period slope change (monthly) | 0.0002 | (−0.001, 0.001) | −0.0011 | (−0.002, −0.0001) | † | |
| Age in year of event, in decades | −0.051 | (−0.055, −0.047) | ‡ | |||
| Female | −0.026 | (−0.031, −0.020) | ‡ | |||
| Race (reference: White) | ||||||
| Black | −0.042 | (−0.053, −0.031) | ‡ | |||
| Other | −0.056 | (−0.069, −0.043) | ‡ | |||
| CR eligible indication (reference: AMI 1st or 2nd position) | ||||||
| CABG | 0.225 | (0.214, 0.237) | ‡ | |||
| PCI | 0.012 | (0.004, 0.019) | ‡ | |||
| Valve surgeries | 0.150 | (0.135, 0.164) | ‡ | |||
| Charlson Comorbidity Index in month of event | −0.014 | (−0.015, −0.013) | ‡ | |||
| Medicare entitlement status (reference: Aged without ESRD) | ||||||
| Aged with ESRD | −0126 | (−0.142, −0.109) | ‡ | |||
| Disabled, no ESRD | −0.118 | (−0.126, −0.110) | ‡ | |||
| Disabled, ESRD | −0.152 | (−0.167, −0.138) | ‡ | |||
| ESRD only | −0.178 | (−0.212, −0.143) | ‡ | |||
| Hospital ownership (reference: Non-profit) | ||||||
| For-profit | −0.010 | (−0.025, 0.005) | ||||
| Non-federal government | −0.019 | (−0.034, −0.003) | † | |||
| Number of beds in 100s | −0.00001 | (−0.002, 0.002) | ||||
| Part of a hospital system | −0.003 | (−0.014, 0.008) | ||||
| Hospital offers CR | 0.105 | (0.095, 0.115) | ‡ | |||
| Teaching hospital | 0.018 | (−0.007, 0.043) | ||||
| Specialty hospital | 0.036 | (−0.021, 0.093) | ||||
| Rural hospital | −0.020 | (−0.035, −0.006) | † | |||
| Census region of index hospital (reference: South) | ||||||
| Northeast | −0.013 | (−0.029, 0.004) | ||||
| Midwest | 0.086 | (0.071, 0.102) | ‡ | |||
| West | 0.024 | (0.008, 0.040) | † | |||
| Percent Medicare discharges by hospital | −0.0001 | (−0.001, 0.0004) | ||||
| Medicare Advantage penetration by HRR | −0.00003 | (−0.0005, 0.0004) | ||||
| Percent uninsured by county | −0.004 | (−0.005, −0.002) | ‡ | |||
| Herfindahl-Hirschman Index by HRR | 0.086 | (0.044, 0.127) | ‡ | |||
| Unexplained random variation between hospitals§ | 0.962 | (0.872, 1.062) | 0.467 | (0.417, 0.523) | ||
| Residual intraclass correlation§ | 0.226 | (0.209, 0.244) | 0.124 | (0.113, 0.137) | ||
p<0.10
p<0.05
p<0.001; Calculated with Robust Standard Errors
presented in average log-odds.
AME=average marginal effects; CR=cardiac rehabilitation; AMI=acute myocardial infarct(ion); CABG=coronary artery bypass surgery; PCI=percutaneous coronary intervention; ESRD=end-stage renal disease; HRR=hospital referral region.
Few hospital and market characteristics were predictive of CR. Hospitals that owned a CR program were associated with higher CR participation (p<0.01). Hospitals that were non-federal government owned (p=0.02) or rural (p<0.01) were associated with lower participation in CR. Patients from hospitals located in the South or Northeast were less likely to participate in CR than those from hospitals in the Midwest or West (p<0.01). Higher uninsured rates by county were associated with less CR participation (p<0.01). More highly concentrated markets (less competitive) were associated with more CR participation (p<0.01). Seasonality by month was not a significant predictive factor for CR participation in the models.
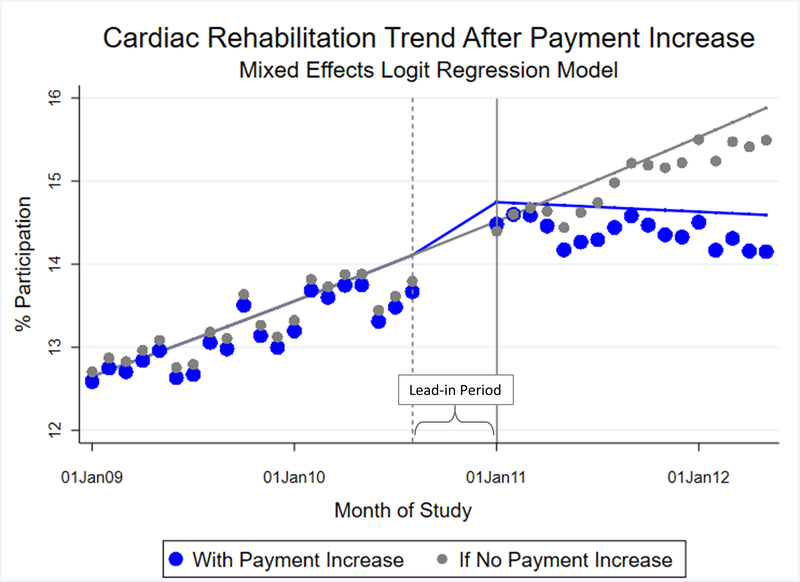
Association of Payment Increase with CR Participation
The primary outcome of the study was CR participation in the period following the payment increase, which was from January 1, 2011 to September 30, 2012. Following regression adjustment for patient, hospital, market, and seasonal factors (Table 3), there was growth in the rate of CR participation before reimbursement increased (0.09 percentage points per month, 95% Confidence Interval (CI): 0.04, 0.2; cumulatively, 1.1 percentage points per year, p<0.05). No discrete change in participation occurred at the point the new payment was implemented in January 2011 (95% CI: −0.9, 1.5). However, the rate of growth of CR slowed in the post-period by 0.11 percentage points per month (95% CI: −0.2, −0.01, p<0.05), or 1.3 percentage points per year relative to the pre-period trend, translating to a nearly flat growth rate of CR (Figure 3).
Figure 3.
Average Predicted Cardiac Rehabilitation Participation by Month with Fitted Model, from 2009 to 2012.
Adjusted trends evaluated at the mean of the covariates and coefficients from the mixed effects regression model are presented. The solid vertical line represents the date the payment for cardiac rehabilitation increase was implemented, January 1, 2011. The dashed vertical line represents the start of the lead-in period. Patients whose index events occurred between September 1, 2010 and December 31, 2010 were excluded during this lead-in period because their 4-month episodic window spanned the date the new payment was implemented. Model predictions were estimated using covariate means at each timepoint. Large blue circles represent the values predicted by the model for the periods before and after the payment increase, which includes the fixed covariate effects and hospital (group) random effects. Small gray circles represent values predicted if the payment had not increased (counterfactual). To plot the systematic relationship between payment and CR participation, we predicted the fixed covariate effect without the hospital random effects for the adjusted regression model (blue) and the counterfactual (grey).
Sensitivity and Specificity Analyses
The sensitivity of the models relative to whether a hospital offered CR services indicated that there were no differences in either time period for groups of patients with an index event at a hospital that offered CR compared to those at a hospital that did not (p-values for interactions each >0.2). For CR services provided by non-hospital ambulatory care centers or doctor’s offices, no increase or decrease in CR participation was observed either before, at the time of, or after the payment increase (p-values for interactions >0.1) (Supplemental Table II). Sensitivity analyses using a three-month episodic window, twelve-month episodic window, three- and four-month death exclusions, as well as excluding low volume hospitals, resulted in similar associations as those in the primary analysis (Supplemental Table III).
The analysis was was somewhat sensitive to shortening the length of the time periods. As the pre-period, the post-period, or both time periods were shortened, the point estimates stayed relatively stable, but the confidence intervals widened, and the p-values rose to greater than 0.05 (Supplemental Table IV). These changes may have reflected a loss of statistical power that can occur in interrupted time series analyses when the number of time units is decreased or the time periods become less balanced. 19,20 Finally, using a false implementation date for the payment increase resulted in estimates that showed no association between time or policy and participation in CR (p-values for the time variables > 0.3) (Supplemental Table III)).
DISCUSSION
In this study we evaluated the association between increased Medicare reimbursement for CR at hospitals and utilization of CR. Results from the hierarchical interrupted time series models adjusting for patient, hospital, and market factors demonstrate that in the twenty months prior to the payment increase, the rates for CR-eligible Medicare patient-participation was growing by approximately 1.1 percentage points per year. No shift in CR participation was observed in January 2011 when the payment increase was implemented, suggesting that there was not an immediate effect of the added payment. After the payment increase, the rate of growth of CR participation flattened with an annual drop over time of 1.3 percentage points from the pre-intervention rate, giving a net negative trend in participation of −0.2 percentage points per year. These findings suggest that this payment increase was associated with a slight, statistically significant drop in the growth of CR participation.
To translate this clinically, if 20% of eligible patients participated in CR in 2010, for every 100,000 patients who were eligible for CR in 2011, on average, 1,300 fewer patients would have participated. This may suggest no clinically relevant change occurred after the payment increased. Further, this finding was somewhat sensitive to truncating the time windows, becoming statistically non-significant as the window shortened, suggesting a loss of power. Regardless of how this trend is interpreted (i.e., as a statistically significant or insignificant decrease or a clinically null result), these results are counter to our hypothesis that participation would increase with the increase in payment. Further, with the longstanding underutilization of CR, any deteriorating or stagnant growth rate is cause for concern.3,23,24
Minimal, incremental changes are not uncommon for secondary prevention programs reimbursed under Medicare. A similarly themed therapy to CR, the Medicare Obesity Benefit, was used by 0.35% of eligible obese beneficiaries in the first year and 0.60% in the second year after its approval in 2011. These rates were determined using the number of Medicare claims billed for this therapy and from estimated state prevalence of obesity in Medicare beneficiaries, ascertained from the 2012 Behavioral Risk Factor Surveillance System.15 Such gradual increases in utilization after CMS coverage determinations have been reported for other Medicare programs as well, although those effects were seen after programs were newly implemented and not as a response to an increase in payment such as in our analysis.14,15
Unobserved mechanisms may underly these results. The 2011 payment increase from $38 to $68, while substantial, may not have reached a threshold that incentivized hospital administrators to allocate resources to their CR programs and encourage more patients to participate. We assume that changes to CR participation following the payment increase would be directly associated with changes to hospital administrative policy, rather than with patient-facing CR staff, who may not know about reimbursement changes, and who should remain agnostic to payment as they enroll patients. Even if the 2011 payment increase enabled hospitals to make a small profit margin for CR,25 the changes may not have been enough to drive a meaningful change to hospitals’ administrative policy or financial results. Alternatively, a longer time period might have picked up responses that lagged past the end of our study, but because several ACA programs were initiated in October 2012 or later, we truncated the analysis to try to disentangle the payment increase from program implementation. The availability of more recent data may have demonstrated a threshold for which hospital administrators were incentivized, since CR reimbursement continued to increase incrementally in subsequent years, with Medicare payment reaching $103 in 2014, and $118 in 2019.6 Future research should evaluate hospital responsiveness to payment increases and what, if any, threshold of payment would incentivize hospitals to improve CR participation.
Another potential explanation for these findings may be related to patient cost-sharing. As traditional fee-for-service Medicare reimbursement increases, patients’ coinsurance also increases.26 There is mixed evidence to suggest that patient out-of-pocket costs are relevant to participation in CR.27,28 However, new evidence suggests there is an inverse, dose-response relationship between patient cost sharing and CR utilization. Farah et al. found that for each $10 increase in patient co-pay, there was an associated 1.5 fewer CR sessions attended.29 Because our data did not include information on patients’ supplemental insurance, we could not adjust for how much patients actually paid for CR. If patients are shown to be sensitive to these pricing increases, it could represent an unintended consequence of increasing reimbursement to hospitals, in which financial incentives to hospitals may be offset by the additional burden on patients. Future studies should address this question.
Regardless of the underlying mechanisms at play, these results suggest that hospitals may require additional incentives to help motivate CR use. Payment reform programs piloted by CMS have not included CR. CMS has been piloting payment reform programs since the early 1990’s in an attempt to ease the financial burden on the healthcare system due to high-risk, high-cost conditions such as cardiovascular disease.9,30,31 These programs have included bundled and episodic payments,30,32 gainsharing models,31 coordinated patient care models,33 performance incentives,34 and payment penalties for excess hospital readmissions.35 AMI and heart failure have featured prominently in these programs, while CR has not.
CR was a specific target of payment reform late in 2017 with CMS’ planned CR Incentive Payment Model, which would have financially incentivized hospitals for each patient who participated in CR, increasing as a patient participated in more sessions.36 However, prior to its implementation in 2017, it was cancelled.37 As Medicare considers new incentives for CR as alternatives to that program, it will be important to anticipate to what level financial payments can incentivize hospitals to boost their patients’ likelihood of participation without creating additional barriers.
Several strengths and limitations to our analysis should be noted. Given that the data are administrative claims data, our analysis was limited because we did not have access to several known and important factors that predict the use of CR, such as physician referral, travel time to CR, patient out-of-pocket costs, and socio-economic factors.38,39 We could not fully disentangle our results from other contemporaneous factors, such as anticipation of other ACA policies that were rolling out in 2012 through 2014.35 Because the data are also observational and retrospectively collected, patients were not randomly assigned to groups, which can result in selection bias and residual confounding from unobserved variables that were not randomized. To counter those limitations, we adjusted for a broad range of patient, hospital, and market factors, including the percentage of uninsured individuals by county as a marker of socio-economic factors and rurality. Additionally, we used a hierarchical model with a random intercept for hospital effects to mitigate bias due to the nested structure of the data and to estimate the combined effects of omitted or unobserved factors.
Other strengths of this analysis are that Medicare claims datasets include a large national sample of patients and hospitals representative of practice patterns in the US; however, these results are not generalizable outside of this patient group. The interrupted time series approach cannot be used for causal inference; however, it is a well-documented model for establishing associative trends over time. We did not have access to data from a health system not subject to the payment increase (e.g., Veteran’s Administration). Future research with such data could provide a comparator group that may allow the use of a difference in difference analytic framework, from which causal inferences can be made.
CONCLUSION
After adjusting for hospital, patient, market, and seasonality factors, an approximately 180% increase in Medicare reimbursement for CR in 2011 was not associated with an increase in CR participation. Repeated attempts by proponents to improve participation in CR have provided only marginal improvements to its longstanding underutilization, and targeted financial incentives under Medicare have been delayed indefinitely. Our results underline the need for more research into understanding the ongoing effects of reimbursement changes on CR participation and whether hospitals or patients are sensitive to these changes.
Supplementary Material
ACKNOWLEDGMENTS
This work was reviewed by the Colorado Multiple Institutional Review Board and deemed exempt with waiver of consent on June 20, 2017 in accordance with federal regulations (45 CFR 46.102(f)). Data use was approved under CMS Data Use Agreement number 28321.
SOURCES OF FUNDING
This publication is supported in part by NIH/NCATS Colorado CTSA Grant Number UL1TR001082. Contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
DISCLOSURES
Dr. Peterson reports research grant funding from NHBLI (4R33HL143324-02). Dr. Ho is supported by grants from NHLBI and VA HSR&D. He serves as the Deputy Editor for Circulation: Cardiovascular Quality and Outcomes. All other authors have no conflicts to disclose.
NON-STANDARD ABBREVIATIONS AND ACRONYMS
- ACA
Affordable Care Act
- AHA
American Hospital Association
- AHRF
Area Health Resources Files
- AMI
acute myocardial infarct(ion)
- CABG
coronary artery bypass graft
- CCI
Charlson Comorbidity Index
- CFR
Code of Federal Regulations
- CI
confidence interval
- CMS
Centers for Medicare and Medicaid Services
- CPT
Current Procedural Terminology
- CR
cardiac rehabilitation
- ESRD
end-stage renal disease
- HCPCS
Healthcare Common Procedure Coding System
- HCRIS
Healthcare Cost Report Information System
- HHI
Herfindahl-Hirschman Index
- HRR
Hospital Referral Region
- ICD-9M
International Classification of Diseases, Ninth Revision, Clinical Modification
- LDS
limited data set
- PCI
percutaneous coronary intervention
REFERENCES
- 1.Anderson L, Thompson D, Oldridge N, Zwisler A, Rees K, Martin N, Taylor R. Exercise-Based Rehabilitation For Coronary Heart Disease (Review). Cochrane Database Syst Rev. 2016;1–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States Department of Health and Human Services. The Centers for Medicare and Medicaid Services. Decision Memo For Cardiac Rehabilitation (CR) Programs - Chronic Heart Failure (CAG-00437N) [Internet]. 2014. [Accessed February 01, 2019]. Available from: https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=270
- 3.Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, Ho PM, Keteyian SJ, King M, Lui K, Pack Q, Sanderson BK, Wang TY. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: A report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2018;11:1–29. [DOI] [PubMed] [Google Scholar]
- 4.Leggett LE, Hauer T, Martin BJ, Manns B, Aggarwal S, Arena R, Austford LD, Meldrum D, Ghali W, Knudtson ML, Norris CM, Stone JA, Clement F. Optimizing Value From Cardiac Rehabilitation: A Cost-Utility Analysis Comparing Age, Sex, and Clinical Subgroups. Mayo Clin Proc. 2015;90:1011–1020. [DOI] [PubMed] [Google Scholar]
- 5.Lee AJ, Shepard DS. Costs of Cardiac Rehabilitation and Enhanced Lifestyle Modification Programs. J Cardiopulm Rehabil Prev. 2009;29:348–357. [DOI] [PubMed] [Google Scholar]
- 6.United States Department of Health and Human Services, The Centers for Medicare and Medicaid Services. Medicare Hospital Outpatient Prospective Payment System Addendum A and Addendum B updates. [Internet]. 2019. [Accessed February 01, 2019; Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalOutpatientPPS/Addendum-A-and-Addendum-B-Updates
- 7.Morrisey MA. Price Sensitivity in Health Care: Implications For Health Care Policy. Washington, D.C.: 2005. [Google Scholar]
- 8.Kristensen SR, Fe E, Bech M, Mainz J. Is the quality of hospital care price sensitive? Regression kink estimates from a volume dependent price setting scheme. DaCHE Discuss Pap 2013–4, COHERE-Centre Heal Econ Res Univ South Denmark - Dache - Danish Cent Heal Econ. [Google Scholar]
- 9.Urdapilleta O, Weinberg D, Pedersen S, Kim G, Cannon-Jones S, Woodward J. Centers for Medicare and Medicaid Services Evaluation of the Medicare Acute Care Episode (ACE) Demonstration Final Evaluation Report. 2013.
- 10.United States Department of Health and Human Services, The Centers for Medicare and Medicaid Services. Bundled Payments for Care Improvement Initiative: General Information [Internet]. 2020. [Accessed February 12, 2021]. Available from: https://innovation.cms.gov/innovation-models/bundled-payments
- 11.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Evaluation of Medicare’s Bundled Payments Initiative for Medical Conditions. N Engl J Med. 2018;379:260–269. [DOI] [PubMed] [Google Scholar]
- 12.Wadhera RK, Yeh RW, Joynt Maddox KE. The Rise and Fall of Mandatory Cardiac Bundled Payments. JAMA - J Am Med Assoc. 2018;319:335–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conrad DA. The Theory of Value-Based Payment Incentives and Their Application to Health Care. Health Serv Res. 2015;50:2057–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoerger TJ, Crouse WL, Zhuo X, Gregg EW, Albright AL, Zhang P. Medicare’s Intensive Behavioral Therapy For Obesity: An Exploratory Cost-Effectiveness Analysis. Am J Prev Med. 2015;48:419–425. [DOI] [PubMed] [Google Scholar]
- 15.Batsis JA, Bynum JPW. Uptake of the Centers for Medicare and Medicaid Obesity Benefit: 2012–2013. Obesity. 2016;24:1983–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.United States Department of Health and Human Services, The Centers for Medicare and Medicaid Services. Hospital Cost Report Public Use Files [Internet]. 2020. [Accessed February 17, 2021] Available from: https://www.cms.gov/Research-Statistics-Dataand-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Cost-Report/HospitalCostPUF].
- 17.United States Department of Health and Human Services, The Centers for Medicare and Medicaid Services. Area Health Resources Files, Health Resources and Services Administration [Internet]. 2010. [Accessed May 01, 2020]. Available from: https://data.hrsa.gov/data/download.
- 18.American Hospital Association. American Hospital Association (AHA) Annual Survey Database - FY2010 -FY2012. Health Forum, an American Hospital Association affiliate, 2011– 2013. [Google Scholar]
- 19.Bernal JL, Cummins S, Gasparrini A. Interrupted Time Series Regression For The Evaluation of Public Health Interventions: A Tutorial. Int J Epidemiol. 2017;46:348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang F, Wagner AK, Ross-Degnan D. Simulation-Based Power Calculation For Designing Interrupted Time Series Analyses of Health Policy Interventions. J Clin Epidemiol. 2011;64:1252–1261. [DOI] [PubMed] [Google Scholar]
- 21.Papke LE, Wooldridge JM. Econometric Methods For Fractional Response Variables With An Application To 401(k) Plan Participation Rates. J Appl Econom. 1996;11:619–632. [Google Scholar]
- 22.StataCorp. Xtreg Manual; 2013;1–29. URL: [http://www.stata.com/manuals13/xtxtreg.pdf]. Accessed [2020 May 1].
- 23.Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic Variation In Cardiac Rehabilitation Participation In Medicare And Veterans Affairs Populations: An Opportunity For Improvement? Circulation. 2018;137:1883–1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ades PA, Keteyian SJ, Wright JS, Hamm LF, Lui K, Newlin K, Shepard DS, Thomas RJ. Increasing cardiac rehabilitation participation from 20% to 70%: A road map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92:234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laskaris J Cardiac Rehab: CMS Increases Per-Patient Payment by $1,100. [Internet]. 2011. [Accessed January 1, 2018]; Available from: http://www.mdbuyline.com.
- 26.Merritt-Worden T Intensive Cardiac Rehabilitation : Value Creation in Today’s s FFS World and Reducing Cardiac Rehabilitation is One of the Most Cost-Effective Heart Treatments Available. Healthcare Financial Managers; 2015. [Google Scholar]
- 27.Parashar S, Spertus JA, Tang F, Bishop KL, Vaccarino V, Jackson CF, Boyden TF, Sperling L. Predictors of early and late enrollment in cardiac rehabilitation, among those referred, after acute myocardial infarction. Circulation. 2012;126:1587–1595. [DOI] [PubMed] [Google Scholar]
- 28.Gaalema DE, Savage PD, Rengo JL, Cutler AY, Higgins ST, Ades PA. Financial incentives to promote cardiac rehabilitation participation and adherence among Medicaid patients. Prev Med (Baltim). 2016;92:47–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farah M, Abdallah M, Szalai H, Berry R, Lagu T, Lindenauer PK, Pack QR. Association Between Patient Cost Sharing and Cardiac Rehabilitation Adherence. Mayo Clin Proc. 2019;94:2390–2398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Health Care Financing Administration. Medicare Participating Heart Bypass Center Demonstration. Health Care Financing Administration Extramural Research Report. 1998. [Google Scholar]
- 31.United States Department of Health and Human Services, The Center for Medicare and Medicaid. Evaluation of the Medicare Physician Hospital Collaboration Demonstration Draft Interim Report: Year One Analyses [Internet]. 2014. [Accessed November 16, 2017]. Available from: https://downloads.cms.gov/files/cmmi/PHC_FINAL-RPT_September2014.pdf
- 32.United States Department of Health and Human Services, The Center for Medicare and Medicaid. Medicare Acute Care Episode Demonstration [Internet]. 2014. [Accessed November 11, 2017]. Available from: https://innovation.cms.gov/files/x/ace-web-page.pdf
- 33.The Centers for Medicare and Medicaid Services. Medicare Shared Savings Program. CMS.gov. URL: [https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/about]. Accessed [2017 Nov 11]. [Google Scholar]
- 34.Husaini M, Joynt Maddox KE. Paying for Performance Improvement in Quality and Outcomes of Cardiovascular Care: Challenges and Prospects. Methodist Debakey Cardiovasc J 2020. Jul-Sep;16(3):225–231. doi: 10.14797/mdcj-16-3-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The Centers for Medicare and Medicaid Services. Readmissions Reduction Program (HRRP). CMS.gov. URL: [https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program]. Accessed [2017 Jan 1]. [Google Scholar]
- 36.Centers for Medicare & Medicaid Services (CMS), HHS. Medicare Program; Advancing Care Coordination Through Episode Payment Models (EPMs); Cardiac Rehabilitation Incentive Payment Model; and Changes to the Comprehensive Care for Joint Replacement Model (CJR). Final rule. Fed Regist. 2017. January 3;82(1):180–651. [PubMed] [Google Scholar]
- 37.The Centers for Medicare and Medicaid Services. Cancellation of Advancing Care Coordination Through Episodic Payment and Cardiac Rehabilitation Incentive Payment Models; Changes to Comprehensive Care for Joint Replacement Payment Model (CMS-5524-P). 2017. [Google Scholar]
- 38.Gravely-Witte S, Leung YW, Nariani R, Tamim H, Oh P, Chan VM, Grace SL. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nat Rev Cardiol. 2010;7:87–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghisi GLM, Polyzotis P, Oh P, Pakosh M, Grace SL. Physician factors affecting cardiac rehabilitation referral and patient enrollment: A systematic review. Clin Cardiol. 2013;36:323–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.