Abstract
Background:
Insulin is an essential therapy for treating diabetes, but many patients lack standard insulin injection skills.
Purpose:
We developed a standard training procedure based on a new simulation tool. Then we conducted a study to investigate the effect of this standard training on the ability of diabetic patients to inject themselves with insulin.
Methods:
After follow-up, a total of 120 patients with diabetes mellitus were included. These patients needed insulin therapy depending on their condition and had not previously learned insulin injection. We randomly divided them into the intervention group (60 cases) and the control group (60 cases). The control group was trained on insulin injection before being discharged according to the traditional method, and the intervention group was trained based on an improved simulation tool. All participants were trained as individuals or groups. Finally, we evaluated the learning effects of both groups.
Results:
The time spent at the training stage in the intervention group was shorter than the control group. We found that after applying simulation devices to mimic operations, the learning time for patients was reduced.
The first subcutaneous injection success rate was 73.33% in the intervention group, which was significantly higher than that in the control group by 46.67%. The score of the first subcutaneous injection and pre-discharge score in the test group was significantly higher than that of the control group. One month later, the score for injection skills in the 2 groups was higher than that before discharge, and the score in the trial group was still higher than that in the control group. The incidence of subcutaneous fat hyperplasia in the trial group was lower than that in the control group (3.3% vs 15%, P < .05). Moreover, the incidence of hypoglycemia (16.7% vs. 26.7%) was higher in the control group, but the difference was not statistically significant (P = .184).
Conclusions/implications for practice:
After applying simulation tools plus operating video and guideline as the standard procedure to train diabetic patients on insulin injection, all patients had a good grasp of using the insulin injection technique. This education method is safe, efficient, and worth promoting worldly.
Keywords: diabetes, insulin injection, simulation tools
1. Introduction
The prevalence of diabetes is high, and is expected to increase in the next decades in developing countries or regions, such as China, India, Brazil, and Southeast Asia.[1] The control of blood glucose involves diet, exercise, and medication, with many patients requiring insulin supplements as part of their treatment. Therefore, patients require insulin injection skills to properly use insulin outside the hospital. China is an emerging country with many Chinese diabetic patients lacking proper training on insulin injection skills.[2]
Therefore, training patients on standard insulin injection techniques is key to treating diabetes. The lack of opportunities to practice is an important reason for insufficient insulin injections in China.[3] We have developed a set of training procedures that use simulation tools to increase the opportunities for patients to practice their injection skills. In addition, we performed a study to investigate the efficacy of the optimized process. All the patients in the study were using the insulin pen for the first time.
2. Materials and methods
2.1. Study design
This was an open-label, single-site, single-visit, 2-arm, quasi-experimental design study, conducted from May 2017 to December 2019. The patients were randomly assigned into 2 groups. The first patient was assigned to the tools plus a video-assisted intervention group (Group T). The second patient was assigned to the traditional trial group (Group C) for training. The rest of the participants were assigned to the groups in a similar manner. The insulin injection techniques of patients were assessed before discharge and then reevaluated 1 month after discharge using a scale.
The study design is shown in Figure 1.
Figure 1.
The study design.
2.2. Ethical considerations
We conducted this study based on the Declaration of Helsinki, and the hospital's clinical research ethics committee approved the study (No.20175056). The study's purpose and procedure were explained to the participants, and written informed consent was obtained. The control group was also given conventional training containing a guide booklet and video about insulin injection when they agreed to initiate insulin therapy.
2.3. Population and sampling
The sample size for this study was estimated to be 100 using the PASS software using the following values: α = 0.05, β = 0.10, and 1 β = 0.90. However, we used a sample size of 110 to mitigate against loss to follow-up due to factors such as change in the status of the patient, change of city of residence, inability to use insulin, death, and change in contact information.
2.4. Inclusion criteria
-
1.
Meet the World Health Organization 1999 diagnostic criteria for diabetes.[4]
-
2.
Flow thinking and language communication, and can read texts and videos smoothly.
-
3.
First time users of the insulin pen and willingness to continue use of insulin treatment after discharge.
-
4.
Willingness to participate in the study and sign an informed consent form.
2.5. Exclusion criteria
-
1.
Patients with serious comorbidities.
-
2.
Patients with history of failure to use the insulin pen.
-
3.
Alcohol or drug abuse/addiction.
-
4.
Patients with Alzheimer's or other mental illnesses making it difficult to cooperate with this study: severe visual, hearing, or mobility impairment.
-
5.
Patients with poor compliance.
Supplementary standards: Patients who met the indication for insulin use but could not inject themselves were also included in the study if a family member was willing to help inject the insulin. In such cases, the age of the family member was used for data analysis.
2.6. Data collection tools
According to the “China Diabetes Drug Injection Technology Guide,”[5] “DESSA Diabetes Insulin Injection Technology Guide” and related literature,[6,7] a self-designed insulin pen usage and related knowledge questionnaire was designed. The questionnaire evaluated 20 factors with each factor accounting for 1 point. The specific options are listed in Table 1.
Table 1.
questionare for evaluating insulin injection tequniques.
| Questions | Score (yes = 1; no = 0) |
| 1. Disinfection preparation | Yes/no |
| 2. Wash hands before injection | Yes/no |
| 3. The details of keeping the spare cartridge or insulin pen | Yes/no |
| 4. Insulin pen matches right insulin cartidge | Yes/no |
| 5. Cartridge and needle are installed correctly | Yes/no |
| 6. Make sure the insulin can be drained after changing the cartridge | Yes/no |
| 7. Shake insulin before injection (for premixed insulin) | Yes/no |
| 8. Knowing the right body injection sites | Yes/no |
| 9. Rotating the sites for injection | Yes/no |
| 10. Each injection site is separated by 1 cm at least | Yes/no |
| 11. Ejecting the excess air away before each injection | Yes/no |
| 12. Changing a new needle for each injection | Yes/no |
| 13. Injection dose adjustment | Yes/no |
| 14. Grasping the injection site in the proper position during injection | Yes/no |
| 15. Correct injection angle | Yes/no |
| 16. Whether the posture of holding the insulin pen is correct | Yes/no |
| 17. After penetrating the skin, pushing the injector piston correctly | Yes/no |
| 18. Removing the needle after right time | Yes/no |
| 19. After the needle is pulled, the injection site is pressed correctly (by cotton swab) | Yes/no |
| 20. Removing the needle with the same penetration angle. | Yes/no |
2.7. Intervention
2.7.1. Preliminary preparation
We retrieved copyright free videos on insulin pen injection from the internet and prepared some manuals. We then developed a simulation tool composed of artificial skin (silicone), sponge, and cloth bags. The simulated skin was on the outside and the sponge (simulated fat layer) was in the middle, and both were covered in a square cloth pouch to form a sandwich structure. The simulation tool was then fixed to the waist using the belt on both sides of the pouch (Figures 2–4).
Figure 2.
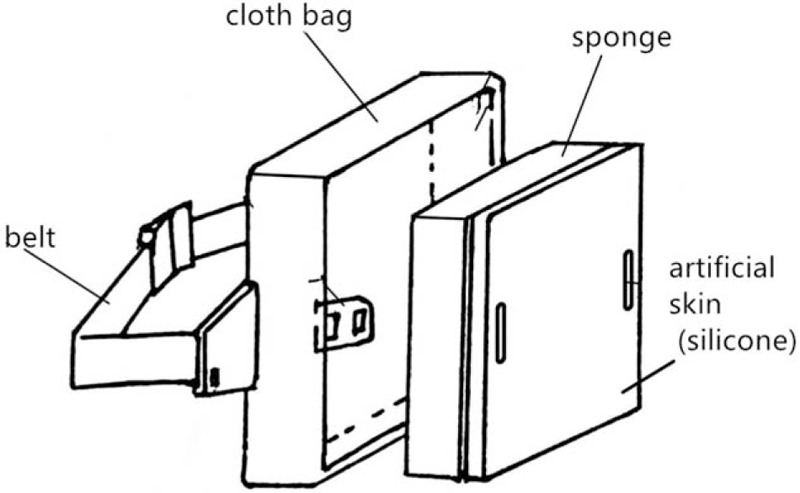
Structure diagram of improved simulation tool.
Figure 4.
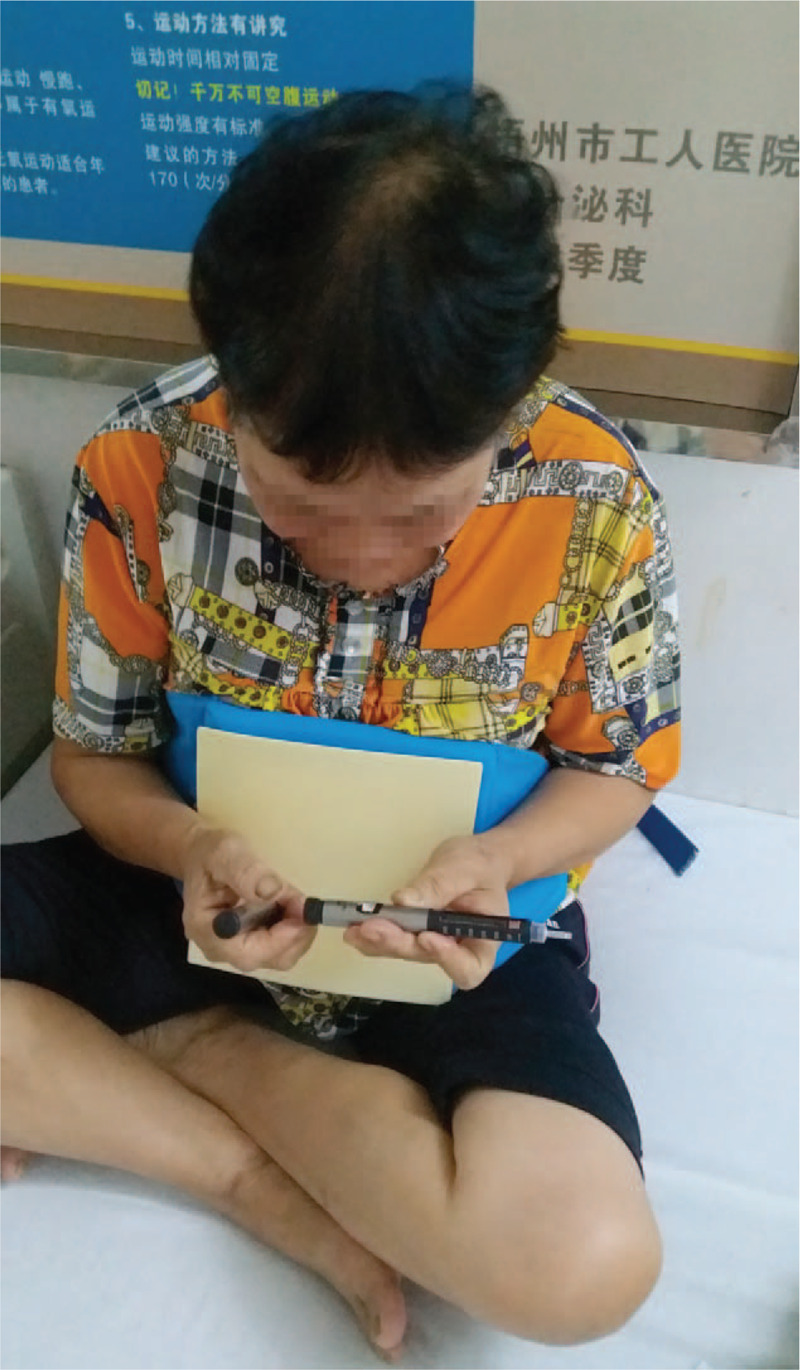
The patient wears this simulation model.
Figure 3.

Patient wears this simulation model.
2.7.2. Education staff
Specialized nurses who were trained and proficient in insulin injection supervised both groups.
2.7.3. Educational approach
The Nurses trained the patients through one-on-one individualized training sessions. Where the number of patients was large or the nurses were too busy, training was conducted in groups. Group-training refers to a group of 3 people who were guided by the supervising nurse to perform correct exercises.
2.8. Two training programs
2.8.1. Definition of the STP (standard training procedure)
Simple teaching stage: A specialist nurse dictated and demonstrated the insulin injection technique, including steps and precautions.
Detailed teaching stage: The patients were guided to practice the technique while asking questions about the procedure.
The patients were required to recall the process and were frequently asked questions on the injection of insulin.
The patients were required to repeat the procedure until they were proficient.
The simulation device was used throughout the detailed teaching stage.
Review stage: On the training day, the next day, and the third day, we provided the video, booklets, and simulated skin for the patients to practice in turns. After being discharged from the hospital, the patients were required to review videos and text guidelines.
2.8.2. Definition of the TTP (traditional training procedure)
Simple teaching stage: Same with the standard training procedure but without simulation devices.
Detailed teaching stage: Same with the standard training procedure but without simulation devices.
Review stage: A manual and video were issued during hospitalization. The patients were also asked to review the videos and text guidelines after discharge (Table 2).
Table 2.
Two training strategies.
| Standard training procedure | Traditional training procedure |
| Step1: Simple teaching stage with simulation tools | Step1: Simple teaching stage without simulation tools |
| Step2: Detailed teaching stage with simulation tools | Step2: Detailed teaching stage without simulation tools |
| Step3: Review with manual, videos and simulation tools | Step3: Review with manual and videos not simulation devices |
| Step4: Manuals and videos are provided to review after leaving the hospital | Step4: Manuals and videos are provided to review after leaving the hospital |
(Note: Because it is a prehospital exercise, and there is no simulation tool, there cannot be too many practice opportunities).
During hospitalization, patients in the control group were trained on the insulin injection technique. The intervention group used Standard training procedure to guide the patients to practice. After discharge, we asked all patients to copy the operation video and watch it at home.
Follow-up time and manner: One month after discharge, a follow-up was completed through face-to-face, phone call, or WeChat.
2.9. Observation indicators
We tested the patients’ use of the insulin pen and relevant knowledge in the hospital and one month after discharge.
The specific indicators are as follows:
-
1.
Time spent at simple teaching stage.
-
2.
Time spent at detailed teaching stage.
-
3.
Time spent for mastery (initial from the end of the detailed teaching stage).
-
4.
Time required for once insulin injection.
-
5.
Success rate of the first actual subcutaneous operation.
-
6.
Score in the first real subcutaneous operation.
-
7.
Score at pre-discharge.
-
8.
Score one month after discharge.
-
9.
Rate of subcutaneous fat hyperplasia.
-
10.
The rate of hypoglycemia (hypoglycemia is considered to occur when the patient feels palpitations, sweating, fatigue, and other symptoms or self-tested blood glucose values are <3.9 mmol/L).
(Note: the time record is accurate to the minute).
2.10. Statistical analysis
Data analysis was carried out using IBM SPSS Statistics 22 software. The measurement data were expressed as means and standard deviations, whereas data that were not normally distributed were expressed as median (25;75-percentile). The count data were expressed as percentages (%). Data that conformed to the normal distribution and homogeneity of variance were analyzed using the independent samples t test or paired-samples t test. Otherwise, the nonparametric test was used for analysis and comparison. χ2 test was used for frequency comparison. P < .05 was considered to be statistically significant.
3. Results
A total of 130 diabetic patients who had attended our hospital from May 2017 to December 2019 were enrolled in the study. Ten participants were lost to follow-up due to loss of phone contacts, change in the status of the patients, and refusal to use insulin for personal reasons. In the end, data from 120 participants was used for analysis, giving a loss to follow-up rate of <10%.
The participants were divided into the test group (Group T) and the control group (Group C) with each group being randomly assigned 60 participants. The ratio of male participants to female participants in the test group was 30:30, with the age ranging from 27 to 81 years, with an average of 57.45 ± 12.35 years. The duration of disease was 7 days to 30 years, with a median of 2.5 years. The ratio of male participants to female participants in the control group was 27: 33, aged 18 to 82 years, average (59.47 ± 13.07 years); the course of disease ranged from 7 days to 30 years, with a median of 3 years.
There were no significant differences in the general characteristics such as sex, age, insulin dosage, education status, and family agent between the 2 groups (Table 3).
Table 3.
Participant characteristics.
| Statistics N | Group C 60 cases | Group T 60 cases | P | |
| Age, y | Mean ± SD, range | 59.47 ± 13.07 18–82 | 57.45 ± 12.35 27–81 | t Test t = 0.869 P = .387 |
| Age distribution, y | χ 2 | |||
| <18 | n (%) | 1 (1.7) | 0 | K = 1.574 |
| 18–40 | n (%) | 5 (8.3) | 7 (11.7) | P = .713 |
| 40–65 | n (%) | 32 (53.3) | 34 (56.7) | |
| ≥65 | n (%) | 22 (36.7) | 19 (31.7) | |
| Sex | χ 2 | |||
| Male | n (%) | 27 (45) | 30 (50.0) | K = 0.301 |
| female | n (%) | 33 (55) | 30 (50.0) | P = .583 |
| Type of diabetes | ||||
| Type 2 diabetes | n (%) | 58 (96.7) | 60 (100) | |
| Pregnancy with diabetes | n (%) | 2 (3.3) | No | |
| Duration of diabetes | Median (IQR) | 3 yrs (7 d, 30 yrs) | 2.5yrs (7d,8.75yrs) | |
| Overview | Range | 7 d–30 yrs | 7d–30yrs | |
| <1 y | n (%) | 16 (26.7) | 21 (35) | |
| 1–5 y | n (%) | 21 (35) | 17 (28.3) | |
| 6–10 y | n (%) | 12 (20.0) | 14 (23.3) | |
| 11–20 y | n (%) | 10 (16.6) | 7 (11.7) | |
| Above 20 y | n (%) | 1 (1.7) | 1 (1.7) | |
| Educational status | ||||
| Primary school or less | n (%) | 15 (25.0) | 16 (26.7) | χ 2 |
| Junior high school | n (%) | 20 (33.3) | 19 (31.7) | K = 1.467 |
| Technical secondary school | n (%) | 4 (6.7) | 5 (8.3) | P = .949 |
| High school | n (%) | 12 (20.0) | 14 (23.3) | |
| College | n (%) | 6 (10.0) | 5 (8.3) | |
| University graduate or more | n (%) | 3 (5.0) | 1 (1.7) | |
| Occupation | ||||
| Worker | n (%) | 42 (70.0) | 46 (76.7) | |
| Farmer | n (%) | 7 (11.7) | 5 (8.3) | |
| Retired | n (%) | 10 (16.7) | 6 (10.0) | |
| Student | n (%) | 1 (1.7) | No | |
| Self-employed | n (%) | No | 3 (5.0) | |
| Insulin pen syringe combination | ||||
| Gansulin pen | n (%) | 17 (28.3) | 15 (25.0) | |
| Novo Pen 4 | n (%) | 40 (66.7) | 43 (71.7) | |
| Novo Pen 4+ Clikstar | n (%) | 3 (5.0) | No | |
| Gansulin pen+ Novo Pen 4 | n (%) | No | 2 (3.3) | |
| Treatment of insulin | ||||
| 30/70 Mixture recombinant human insulin | n (%) | 16 (26.7) | 15 (25.0) | |
| Insulin aspartame 30/70 | n (%) | 37 (61.7) | 39 (65.0) | |
| Rapid-effect insulin + basal insulin | n (%) | 2 (3.3) | 0 (0) | |
| Short-acting insulin + basal insulin | n (%) | 5 (8.3) | 6 (10.0) | |
| Frequency of insulin injections | ||||
| Twice | n (%) | 24 (40.0) | 21 (35.0) | |
| 3 Times | n (%) | 29 (48.3) | 34 (56.7) | |
| 4 times | n (%) | 7 (11.7) | 5 (8.3) | |
| Insulin dosage, U | Median (25/75 percentile) range | 24 (18, 33) 7–54 | 24 (18.25, 29.5) 8–44 | Nonparametric test Z = 0.639 P = .809 |
| Whether family member help to inject insulin as an agent | ||||
| Yes | n (%) | 12 (80.0) | 9 (15.0) | χ 2 |
| No | n (%) | 48 (20.0) | 51 (85.0) | K = 0.519 P = .471 |
IQR = interquartile range.
The ability of the study participants to learn the insulin injection technique is dependent on the knowledge level and cognitive ability of each participant. An intelligence quotient (IQ) test is required to assess the knowledge level and cognitive ability of an individual. However, most of the study participants were not willing to take the test.
Since none of the study participants was illiterate, it was assumed that there was no difference in the education status between the 2 groups. In addition, the cognitive abilities of all the participants were considered to be normal. This was an indication that the ability to learn the insulin injection technique was similar in both groups. Moreover, all the study participants were learning the technique for the first time.
The time spent at the simple teaching stage was similar between the 2 groups (median, 25/75-percentile 6.0 minutes, 4/8 vs5.5 minutes, 4/8, P = .377). However, the time taken to complete the detailed teaching stage was shorter for the test group compared to that of the control group (median, 25/75-percentile 8.0 minutes, 6/11 vs10.0 minutes, 8/13, P = .001). In addition, the time taken to master the technique in the trial group was shorter than that in the traditional group (median, 25/75-percentile 10.0 minutes, 8/13 vs 16.0 minutes, 13/18, P < .001). These 3 parameters were associated with the cognitive ability of the patient as well as the training skills of the trainer. We found that the use of simulation devices to mimic operations reduced the time taken by the participants to learn the technique.
The success rate of the first subcutaneous injection was 73.33% in the intervention group, which was significantly higher than that of the control group by 46.67% (P = .006). Similarly, the score of the first subcutaneous injection in the test group was significantly higher than that in the control group (median, 25/75-percentile 18.0 points,16/19 vs 12.0 points,11/14, P < .001).
The pre-discharge score in the test group was higher than that in the control group (median, 25/75-percentile 18.0 points, 16/19 vs 13.0 points, 11/15, P < .001); the time required for once insulin injection in the test group was significantly less than that in the control group (median, 25/75-percentile 2.0 points, 1/2 vs 2.45 points, 1.8/2.98, P < .001). One month later, the score for operation skill in the 2 groups was higher than that before discharge (P < .01), and the score in the trial group was higher than that in the control group (median, 25/75-percentile 18.0 points, 17/19 vs 13.0points, 12/15, P < .001).
We compared the incidence of subcutaneous fat hyperplasia and hypoglycemia between the 2 groups. The level of subcutaneous fat hyperplasia in the trial group was significantly lower compared to the control group (3.3% vs 15.0%; P = .027), whereas the incidence of hypoglycemia was higher in the control group compared to the test group, although it was not statistically significant ((16.7% vs 26%; P = .184) (Table 4).
Table 4.
Comparison between the 2 groups.
| Group C (control) | Group T (trial) | Z (χ2) value | P | |
| cases | 60 | 60 | ||
| Time at simple teaching, min | 6 (4,8) | 5.5 (4,8) | −0.884 | .377 |
| Time at detailed teaching, min | 10 (8,13) | 8 (6,11) | −3.278 | .001 |
| Time for mastery, min | 16 (13,18) | 10 (8,13) | −7.541 | .000 |
| Success rate of the first actual subcutaneous operation | 28 (60) 46.67% | 44 (60) 73.33% | 10.375 | .006 |
| Score in first real subcutaneous operation (points) | 12 (11,14) | 18 (16,19) | −9.457 | .000 |
| Time required for once insulin injection, min | 2.45 (1.8,2.98) | 2.00 (1,2) | −6.146 | .000 |
| Score at pre-discharge (points) | 13 (11,15) | 18 (16,19) | −9.061 | .000 |
| Score at 1 month after discharge (points) | 13 (12,15) | 18 (17,19) | −9.226 | .000 |
| Rate of subcutaneous fat hyperplasia | 9 (60) 15.0% | 2 (60) 3.3% | 4.904 | .027 |
| Rate of hypoglycemia | 16 (60) 26.7% | 10 (60) 16.7% | 1.768 | .184 |
| Z = −3.274<!-—<LBREAK"/>-->∗P < .01 | Z = −3.071<!-—<LBREAK"/>-->∗P < .01 |
P indicates the comparison of the indicators of both groups before and after discharge.
4. Discussion
Diabetes is a common chronic disease that causes complications that threaten human health. Insulin is one of the essential therapeutic agents for diabetes with many patients requiring its short-term or life-time administration. For insulin treatment to be effective, it not only requires the appropriate type and dosage to be determined, but also the use of standardized injection techniques. These techniques directly affect blood glucose control and patient compliance.[8]
Many patients with diabetes in China lack guidance on appropriate insulin injection skills. According to a study involving 171 centers in 16 countries worldwide, only <10% of patients in China had the correct insulin injection skills.[9] Ruan et al surveyed the insulin injection capacity among diabetic patients in the Shanghai community and found that many of the patients did not use standard injection skills, suggesting that the status of education on insulin injection was poor.[10]
There were several factors accounting for the use of non-standardized injection skills. These included the fear of pain and the fear of the needle penetrating the abdominal cavity if the needle was not inserted properly (although most of the existing needles are not long enough to enter the abdominal cavity).[11] Standardized injection techniques ensure that the insulin is delivered appropriately to the subcutaneous tissue to exert its effect, and reduce incidences of pain, and skin complications at the injection site.[12] Consequently, patients who master the insulin injection technique experience less incidences of pain and therefore eliminate the fear of insulin use to a certain extent.
Another factor accounting for nonstandardized injection skills is the lack of opportunities to practice the skills. Presently, the most common training on insulin injection in China is usually done 1 to 2 days before discharge. The training is usually conducted by the nurse in charge. However, Zhang et al found that there are insufficient diabetes specialist nurses in charge of diabetes education in China, and even physicians do part-time diabetes education while undertaking clinical work. Due to the busy schedule of the nurses, they do not have enough time to train patients, and consequently patients have few opportunities to repeat insulin injections.[13]
Audio-visual tools can be used to fill the gaps in the training of patients on insulin injection skills.[3] Multimedia is characterized by vivid and intuitive features, which stimulate the learning interest of patients and enhance their memory through images, text, and sound.[14] Cheng et al used videos to guide training on insulin injection which provided timely error-correction.[15] In addition, Celik et al instructed diabetic patients on how to use insulin pens correctly through cell phone text messages.[16] These measures deepened the understanding of the patients and increased the rate of standardization of the injection skills.
Nevertheless, these methods have not increased the opportunities for the patients to practice, yet there is need for the patients to practice often in order to master the skills. At present, some companies have simulation tools used to train patients. Some of the simulation tools are human models (Fig. 5), which are not convenient to carry on the body. Another tool involves simulated skin, whose injection area is small, inconvenient to clean inside (single solid entity), and insufficient simulation (Fig. 6). To overcome the above shortcomings, a larger simulation tool was designed in this study (Fig. 2). At the same time, we combined video and the use of manuals (booklet) to train on the standard process.
Figure 5.

Human abdomen model (1 piece of silicone).
Figure 6.

The small device designed by some company.
The results showed that the time spent on simple teaching, detailed teaching, and mastery stage in the intervention group were less than those in the control group. This proves that simulation equipment and video can shorten the time of medical education and learning.
The success rate of the first actual subcutaneous operation, Score in the first real subcutaneous operation, score at pre-discharge, and score at 1 month after discharge in the intervention group were significantly higher than those of the control group. The time required for once insulin injection was also shorter in the trial group. Meanwhile, the intervention group was observed to be more proficient after one month. These data show that this standard procedure can improve the patient's learning outcome and overcome the fear of the first subcutaneous injection to a certain extent.
In addition, none of the patients reported any incidences of subcutaneous hemorrhage or skin infections caused by insulin injection during the study. This could be due to the small patient sample size, follow-up time, and compliance. The short follow-up time as well as the compliance by patients to use disposable needles could account for the lack of incidences of subcutaneous bleeding and skin infections.
However, there were still incidences of subcutaneous fat hyperplasia reported in both groups, with the traditional group reporting 9 (15.0%) patients, whereas the intervention group reporting 2 (3.3%) patients. This could be attributed to the infrequent rotation of the injection site by the patients. Nevertheless, incidences of subcutaneous fat hyperplasia were lower in the trial group, suggesting that proper training on insulin injection can reduce some adverse reactions caused by insulin injection.
After a month of follow-up, there was an increase in the scores in both groups. This implies that patients can improve proficiency through repeated practice, either through manual or video guidance after discharge. It also reflects the importance of practice. Nevertheless, the score of the intervention group was also higher than the traditional group, indicating that the training conducted during hospital stay had laid a good foundation.
Although the incidence of hypoglycemia was lower in the intervention group, there was no significant difference. Since there are too many factors affecting blood glucose, this study failed to exclude other factors, which may have resulted in the lack of a difference between the 2 groups.
The advantages of this improved equipment include low price (<3 dollars), can be produced in large quantities, simple structure, a large injection, easy to clean and maintain, a high degree of simulation, high safety, and no risk. It can be used repeatedly, allowing patients to get enough practice to master insulin injection skills in a short time.
The disadvantage is that the device size is only suitable for abdominal simulation. It cannot be tied to the arm or thigh to simulate injections at these sites. However, since most trainings on injections usually start at the abdomen, it is not difficult to practice at another site after proficiency.
This tool is not only useful in training patients on insulin injections in the Endocrinology department but it also helps diabetic patients practice in other clinical departments. It can also be used during medical training as a teaching aid in the training of nursing and medical students. Besides, since it is economical and simple to design, it can be used outside China in hospitals in the developing countries to improve the insulin injection skills of patients.
5. Limitation
First, since there were no illiterate people included in the study, it was difficult to determine the effect of education status on the ability to learn the insulin injecting techniques.
Second, due to various reasons, subsequent follow-up failed to obtain data on blood glucose and glycated hemoglobin in most patients after 1 or 3 months. Moreover, since several factors affect blood glucose, it was also difficult to determine the effect of the training on the glycemic control of the patients.
Third, the sample size for this study was small. One of the primary reasons is that there are more outpatients and fewer inpatients in the center. Therefore, we also included patients whose family members were willing to help with the insulin injection. At present, our diabetes clinic lacks the resources to conduct such instructional insulin injection training. The availability of sufficient human resources means that training on insulin injection can be considered in outpatient clinics, and multicenter research can be planned to expand the sample size.
However, the final sample size was larger than the estimated number in the study, and through the training of the standard process, it improved the standardization of insulin injection skills among the patients. This standardized education method can achieve the best educational effect without increasing human resources, which helps patients and relieves medical work intensity.
6. Conclusions
The use of simulation tools, combined with operating videos and manuals as the standard process for guiding patients in insulin injection training can ease the patient's fear of injection, provides more practice, and improve the insulin injection skills of the patients. This method works well with no adverse effects and is worth promoting throughout China and other developing countries.
Acknowledgments
The authors express our gratitude to Freescience Editorial Team for their support on this article.
Author contributions
Resources: Jieping Nie, Jieqing Deng.
Writing – original draft & editing: Kaiyong Liang.
Writing – review & editing: Qiao Xie.
Footnotes
Abbreviations: IQ = intelligence quotient, STP = standard training procedure, TTP = traditional training procedure.
How to cite this article: Liang K, Xie Q, Nie J, Deng J. Study on the effect of education for insulin injection in diabetic patients with new simulation tools. Medicine. 2021;100:14(e25424).
Funding: The author (s) received no financial support for the research, authorship, and/or publication of this article.
The authors have no conflicts of interest to disclose.
Revised: The article has been revised by Paperpal Preflight and Freescience Editorial Team.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].International Diabetes Federation, Aguiree F, Brown A, Cho NH, et al. IDF Diabetes Atlas. 6th edition2013. [Google Scholar]
- [2].Pan C, Yang W, Jia W, et al. Management of Chinese patients with type 2 diabetes, 1998-2006: the Diabcare-China surveys. Curr Med Res Opin 2009;25:39–45. [DOI] [PubMed] [Google Scholar]
- [3].Ji J, Lou Q. Insulin pen injection technique survey in patients with type 2 diabetes in mainland China in 2010. Curr Med Res Opin 2014;30:1087–93. [DOI] [PubMed] [Google Scholar]
- [4].Puavilai G, Chanprasertyotin S, Sriphrapradaeng A. Diagnostic criteria for diabetes mellitus and other categories of glucose intolerance: 1997 criteria by the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (ADA), 1998 WHO consultation criteria, and 1985 WHO criteria. World Health Organization. Diabetes Res Clin Pract 1999;44:21–6. [DOI] [PubMed] [Google Scholar]
- [5].Ji LN, Guo XH, Huang J, et al. Chinese guideline for diabetic injection technology. Chin J Diabetes Mellitus 2017;9:79–105. [Google Scholar]
- [6].Davel H, Berg GI, Allie R, et al. Injection Technique Working Group of the Diabetes Education Society of South Africa (DESSA) Injection technique guidelines for diabetes: sharp and to the point. JEMDSA 2014;19:08–13. [Google Scholar]
- [7].Ogston-Tuck S. Subcutaneous injection technique: an evidence-based approach. Nurs Stand 2014;29:53–8. [DOI] [PubMed] [Google Scholar]
- [8].Misnikova I, Gubkina V, Lakeeva T, et al. A randomized controlled trial to assess the impact of proper insulin injection technique training on glycemic control. Diabetes Ther 2017;8:1309–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].De Coninck C, Frid A, Gaspar R, et al. Results and analysis of the 2008-2009 insulin injection technique questionnaire survey. J Diabetes 2010;2:168–79. [DOI] [PubMed] [Google Scholar]
- [10].Ruan Y, Yan QH, Xu JY, et al. Epidemiology of diabetes in adults aged 35 and older from Shanghai, China. Biomed Environ Sci 2016;29:408–16. [DOI] [PubMed] [Google Scholar]
- [11].Rubin RR, Peyrot M, Kruger DF, et al. Barriers to insulin injection therapy: patient and health care provider perspectives. Diabetes Educ J 2009;35:1014–22. [DOI] [PubMed] [Google Scholar]
- [12].Frid A, Hirsch L, Gaspar R, et al. New injection recommendations for patients with diabetes. Diabetes Metab 2010;36:03–18. [DOI] [PubMed] [Google Scholar]
- [13].Zhang X, Liu XL, Guo LX. Investigation and countermeasures for nurses’ problems in diabetes care. Diabetes New World 2014;19:77–177. (In Chinese). [Google Scholar]
- [14].Castaldini M, Saltmarch M, Luck S, et al. The development and pilot testing of a multimedia CD-ROM for diabetes education. Diabetes Educ 1998;24:285–6. 291-292, 295-296. [DOI] [PubMed] [Google Scholar]
- [15].Cheng LH, Zhang YL, Zhong YJ, et al. Effect of video guidance of insulin injection among diabetic patients. China Modern Doctor 2016;54:129–34. (In Chinese). [Google Scholar]
- [16].Celik S, Cosansu G, Erdogan S, et al. Using mobile phone text messages to improve insulin injection technique and glycaemic control in patients with diabetes mellitus: a multi-center study in Turkey. J Clin Nurs 2015;24:1525–33. [DOI] [PubMed] [Google Scholar]


