Abstract
Background:
The new emerging application of decompression combined with fusion comes with a concern of cost performance, however, it is a lack of big data support. We aimed to evaluate the necessity or not of the addition of fusion for decompression in patients with lumbar degenerative spondylolisthesis.
Methods:
Potential studies were selected from PubMed, Web of Science, and Cochrane Library, and gray relevant studies were manually searched. We set the searching time spanning from the creating date of electronic engines to August 2020. STATA version 11.0 was exerted to process the pooled data.
Results:
Six RCTs were included in this study. A total of 650 patients were divided into 275 in the decompression group and 375 in the fusion group. No statistic differences were found in the visual analog scales (VAS) score for low back pain (weighted mean difference [WMD], –0.045; 95% confidence interval [CI], –1.259–1.169; P = .942) and leg pain (WMD, 0.075; 95% CI, –1.201–1.35; P = .908), Oswestry Disability Index (ODI) score (WMD, 1.489; 95% CI, –7.232–10.211; P = .738), European Quality of Life-5 Dimensions (EQ-5D) score (WMD, 0.03; 95% CI, –0.05–0.12; P = .43), Odom classification (OR, 0.353; 95% CI 0.113–1.099; P = .072), postoperative complications (OR, 0.437; 95% CI, 0.065–2.949; P = .395), secondary operation (OR, 2.541; 95% CI 0.897–7.198; P = .079), and postoperative degenerative spondylolisthesis (OR = 8.59, P = .27). Subgroup analysis of VAS score on low back pain (OR = 0.77, 95% CI, 0.36–1.65; P = .50) was demonstrated as no significant difference as well.
Conclusion:
The overall efficacy of the decompression combined with fusion is not revealed to be superior to decompression alone. At the same time, more evidence-based performance is needed to supplement this opinion.
Keywords: decompression alone, decompression combined with fusion, lumbar degenerative spondylolisthesis
1. Introduction
Lumbar degenerative spondylolisthesis (LDS) belongs to a common disease in spinal surgery. Anatomically, it presents as one vertebral body displace the latter from anterior sagittal orientation while remaining intact arch, and accompanied by spinal stenosis in most conditions.[1,2] Meanwhile, the L4–5 is impaired frequently among all centrums,[1,3] which seems to be explained by where the main force places when people stand upright. Clinically, it manifests by radiating pain from buttock to leg and mechanical backache in the lower part.[3,4] It is reported that LDS accounts for 4.1% of the general population,[2] with women and the aged over 60 mostly involved.[5,6] The spine patient outcomes research trial (SPORT)[7] verified that the surgery advantages were over conservative treatment and decompression alone. As an initially emerged surgical procedure, it benefits the patients with less invasive operations[8] and relieved them from suffering of neural compression symptoms.[3] Some surgeons combined decompression with lumbar fusion in today's operations. Recent systemic reviews on this issue have supported that decompression plus fusion brings about promising clinical outcomes.[9,10] The fusion with or without instrumented assistance also yields good clinical outcomes (such as decreased pain and longer relaxed term).[11,12] It is widely used and even as the “golden standard.”[13] A study conducted in the United States showed that the rate of combined treatment is high up to 96%.[14] However, different voices are existing: whether fusion is the necessary option still ignites great controversy.[15,16] Notably, the expenses go up as the procedures get complicated. Besides, there are some other hesitations on account of the uncertain comparing results between the 2 approaches.[11,17] Therefore, we aimed to seek the superiorities yet inferiorities of these 2 groups by expounding the clinical efficacies between decompression alone and decompression combined with lumbar fusion for LDS patients.
2. Materials and methods
2.1. Data sources and searches
This review work is restricted closely along with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines.[18] The online search engines including PubMed (1970.01–2020.08), Web of Science (1970.01–2020.08), and Cochrane Library (1970.01–2020.08) are searched for potential studies. The searching terms are shown as follows: fenestration or hemilaminectomy or laminotomy or laminectomy or decompression, lumbar canal stenosis or lumbar spondylolisthesis or lumbar spinal stenosis or degenerative lumbar spondylolisthesis, arthrodesis or fusion. Besides, previous relevant references and related original studies are manually searched as well.
2.2. Inclusion and exclusion criteria
The inclusion of this analysis is limited to randomized controlled trials (RCTs); topics on the comparison between decompression alone and decompression combined with lumbar fusion; English language; contents consist of at least one aspect in the clinical efficacy and/or complications.
In contrast, animal trials, conference or commentary articles, letters, systematic review, meta-analyses, case reports and series; studies without comparison between 2 groups; the included items <10; patients with isthmic spondylolisthesis or other diseases such as the spinal tumor, bone fracture, systemic diseases, and other irrelevant diseases during the recruitment period; articles focusing on the surgical techniques and internal fixed instruments are excluded from our analysis.
2.3. Data extraction and outcome measures
We assigned 2 authors to independently complete this part. A third author would join the extraction process in case of disagreements. The basic demographic information (the age, sex, diagnosis, the number of included cases, stenosis degree at the moment of grouping, follow-up time, and outcomes) was extracted based on a preplanned form. The primary outcomes included patients’ satisfaction (Odom classification), restored walking ability postoperative, the improvement ratio of European Quality of Life-5 Dimensions (EQ-5D), of the visual analog scales (VAS) score, of Oswestry Disability Index (ODI) for low back pain and leg pain. The secondary outcomes referred to the complications (the secondary operation, operation time, adjacent segment degenerative/disease [ASD], bleeding amount, and the development of centrum slippage after an operation).
2.4. Risk of bias and quality assessment
Cochrane Handbook for Systematic Review of Interventions (version 5.0) was used to evaluate the quality of related controlling factors of included literature. Specifically, each study was accessed for random sequence generation, blinding of participants and personnel, allocation concealment, selective reporting, blinding of outcome assessment, incomplete outcome data, and other sources of bias.
2.5. Data synthesis and analysis
All meta-analyses of eligible results were conducted using the STATA version 11.0 (Stata Corporation, College Station, TX). Heterogeneity among studies was estimated using a Chi-squared test, the I2 value was identified to describe the percentage variance in trials attributable to heterogeneity. We regarded I2 > 50% as high heterogeneity, and a random-effect model was conducted. Otherwise, the fixed-effect model was used. The continuous outcomes (VAS score, ODI score, and EQ-5D score) were presented as weighted mean differences (WMD) with 95% confidence intervals (CIs). For binary variables (Odom classification, complications, reoperation), odds ratios (ORs) with 95% CIs were applied for the evaluation. A P-value <.05 was regarded as statistically significant.
3. Result
3.1. Search results
A total of 2437 publications were presented via searching electronic databases, there were 997 publications after removing duplicates. Strictly along with our inclusion and exclusion criteria, 33 studies were included. Afterward, we retained 10 full-text articles assessed for eligibility. Six studies[1,3,4,11,19,20] were eventually accepted. More details were shown in Fig. 1.
Figure 1.
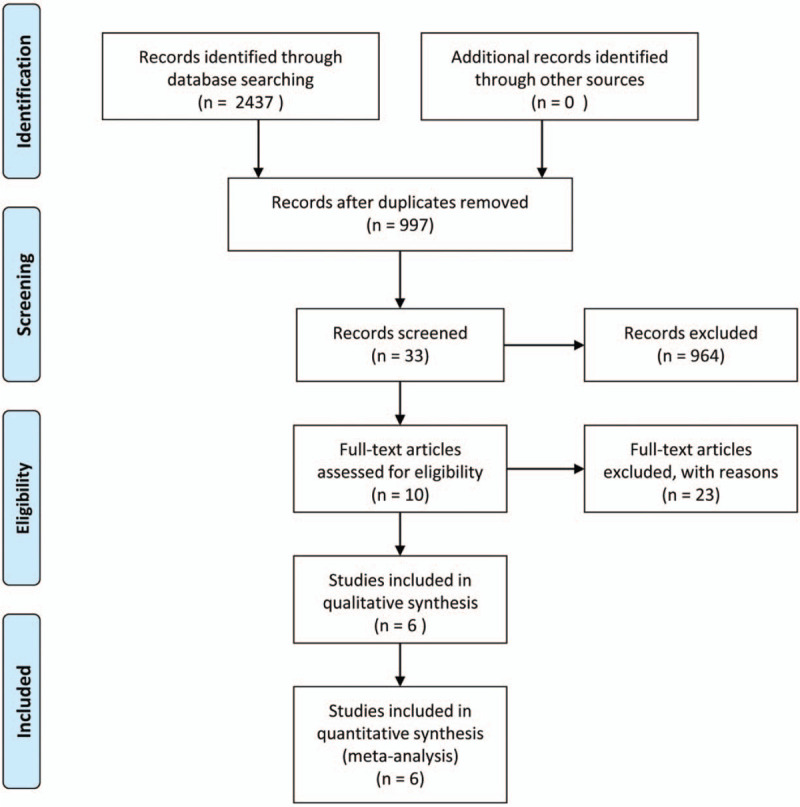
Flowchart of the study selection process.
3.2. Quality assessment and demographics
Two-thirds of the included studies showed a low risk of bias for sequence generation and selective reporting, all showed a low risk for blinding of outcome assessment and incomplete outcome data. The allocation concealment of Herkowitz and Kurz study[11] was assessed as high risk, the other 5 studies did not mention this criterion. More details about the quality assessment of trials were provided in Table 1.
Table 1.
Cochrane Collaboration tool for quality assessment in the included studies.
| Trials | Sequence generation | Allocation concealment | Blinding of outcome assessors | Incomplete outcome data | Selective outcome reporting | Others |
| Herkowitz et al | Low | High | Low | Low | Low | Low |
| Bridwell et al | Low | Unclear | Low | Low | Low | Low |
| Aihara et al | High | Unclear | Low | Low | Unclear | Low |
| Kleinstuect et al | Unclear | Unclear | Low | Low | Unclear | Unclear |
| Ghogawa et al | Low | Unclear | Low | Low | Low | Low |
| Forsth et al | Low | Unclear | Low | Low | Low | Low |
A total of 650 patients diagnosed with LDS were enrolled, hailing from USA, Sweden, and Japan. Of these 650 patients, 275 were randomized to the decompression (D) group versus 375 to the decompression combined with the fusion (D+F) group. Recruitment periods approximately ranged from 3 to 7 years. No statistic value was found in average age and sex between the D and D+F groups. More details were depicted in Table 2.
Table 2.
Overview of included studies.
| Participants (n) | Gender (M/W) | Age (mean ± standard) | ||||||||
| Author | Country | Years | Type of study | Recruitment period | D | D+F | D | D+F | D | D+F |
| Herkowitz et al | USA | 1991 | RCT | NA | 25 | 25 | 1.50 | 0.25 | 65.0 | 63.5 |
| Bridwell et al | USA | 1993 | RCT | 1985.2–1990.3 | 9 | 34 | 0.28 | 0.31 | 72.3 | 64.6 |
| Aihara et al | Japan | 2012 | RCT | 2005.5–2008.8 | 33 | 17 | 1.36 | 0.55 | 63.0 ± 10.2 | 65.0 ± 9.2 |
| Kleinstueck et al | Sweden | 2012 | RCT | 2004.3–2008.5 | 56 | 157 | 0.70 | 0.29 | 73.0 ± 8.0 | 67.4 ± 9.4 |
| Ghogawa et al | USA | 2016 | RCT | 2002.3–2009.8 | 35 | 31 | 0.30 | 0.19 | 66.5 ± 8.0 | 66.7 ± 7.2 |
| Forsth et al | Sweden | 2016 | RCT | 2006.10–2012.6 | 117 | 111 | 0.41 | 0.61 | 67.0 ± 7.0 | 68.0 ± 7.0 |
D+F = decompression combined fusion, D = decompression, M/W = man/woman, NA = not available, RCT = randomized controlled trial.
3.3. Outcomes
3.3.1. VAS score
VAS grades varied from 0, meaning no pain, to 10, representing maximal pain.[21] There were 4 RCTs[3,4,11,19] that mentioned the improvement ratio of the VAS score of low back pain before and after receiving decompression or fusion treatment. Postoperative pain easement assessed by VAS did not show significant value in this study (WMD, –0.045; 95% CI, –1.259–1.169; P = .942, Fig. 2), and the heterogeneity was non-negligible (I2 = 75.1%; P = .007). Two RCTs[3,4] worked out no statistic difference on the number of those who got improved VAS scores after taking surgery between the 2 groups (OR, 0.77; 95% CI, 0.36–1.65; P = .50). Three trials[3,4,11] described the VAS score of the leg pain pre- and postoperation, and this meta-analysis worked out the postoperative easement between the 2 groups as no significant difference (WMD, 0.075; 95% CI, –1.201–1.351; P = .908, Fig. 3).
Figure 2.
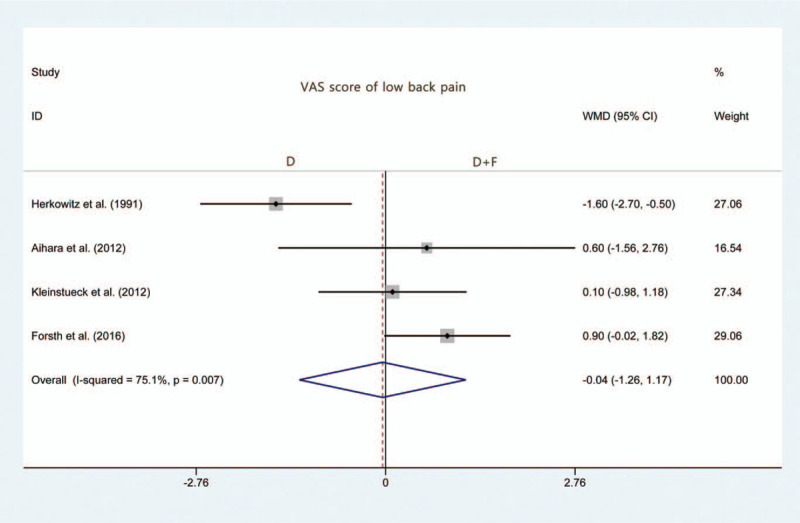
Forest plot of weighted mean difference (WMD) of VAS score of low back pain improvement with decompression versus decompression combined with fusion. VAS = visual analog scales.
Figure 3.
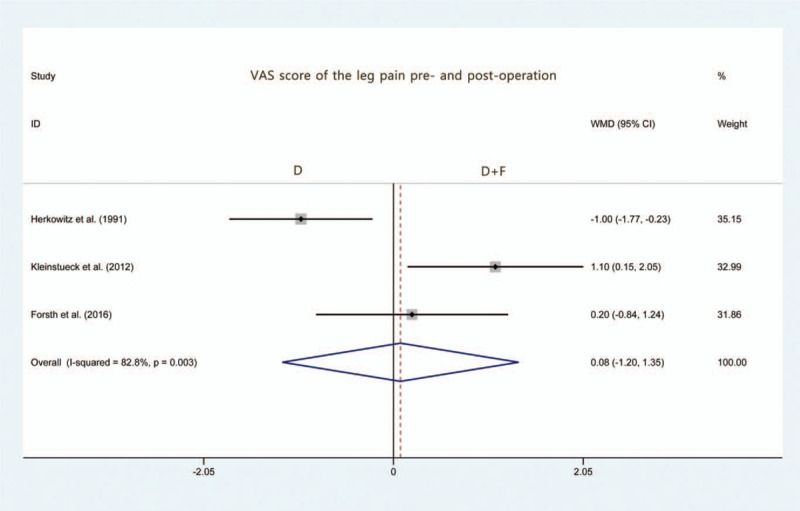
Forest plot of weighted mean difference (WMD) of VAS score of leg pain improvement with decompression versus decompression combined with fusion. VAS = visual analog scales.
3.3.2. ODI score and EQ-5D score
ODI ranges from 0 to 100, EQ-5D ranges from 0 to 1, respectively, ODI score is parallel with the severity of the disability, so is EQ-5D score with the quality of life.[22] Two RCTs[4,20] referred to ODI and EQ-5D indicators. But this meta-analysis used random-effect model and performed no statistic difference between the D and D+F groups in ODI score (WMD, 1.489; 95% CI, –7.232–10.211; P = .738; Fig. 4) and EQ-5D score (WMD, 0.03; 95% CI, –0.05–0.12; P = .43).
Figure 4.
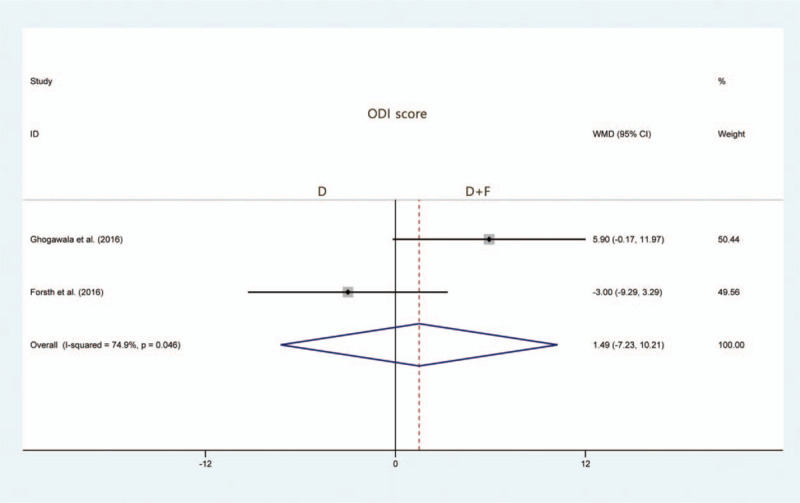
Forest plot of weighted mean difference (WMD) of Oswestry Disability Index (ODI) score improvement with decompression versus decompression combined with fusion.
3.4. Odom classification
Postoperative patients’ satisfaction was evaluated by Odom classification. Our meta-analysis worked out no statistical difference between the D and D+F groups (OR, 0.353; 95% CI, 0.113–1.099; P = .072; Fig. 5). Restored walking ability was only seen in Forsth literature,[4] and reported no statistical difference in the incidence of patients in the increase of walking distance at 2 years as well.
Figure 5.
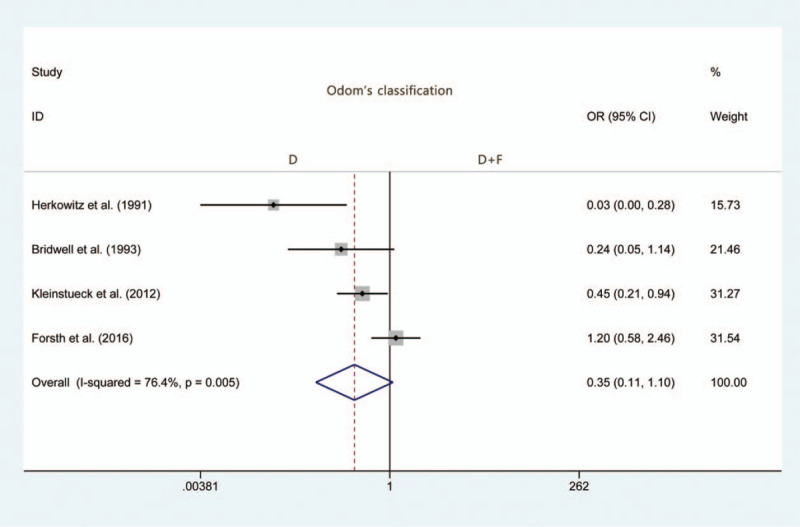
Forest plot of odds ratio (OR) of postoperative satisfaction of patients with decompression versus decompression combined with fusion.
3.5. Complications
Five articles[1,3,4,19,20] recorded the incidence of complications, among which there were 2 articles[4,20] mentioned ASD. Forsth trial[4] was eliminated because of recording both spondylolysis and non-spondylolysis. Analysis towards the other 4 publications was regarded as no statistic difference between the D and D+F groups (OR = 0.437; 95% CI, 0.065–2.949; P = .395; Fig. 6). Ghogawala et al[20] recorded the cases of ASD in the 2 groups respectively as 12 and 4, both were adjacent segment disease and took the secondary surgery.
Figure 6.
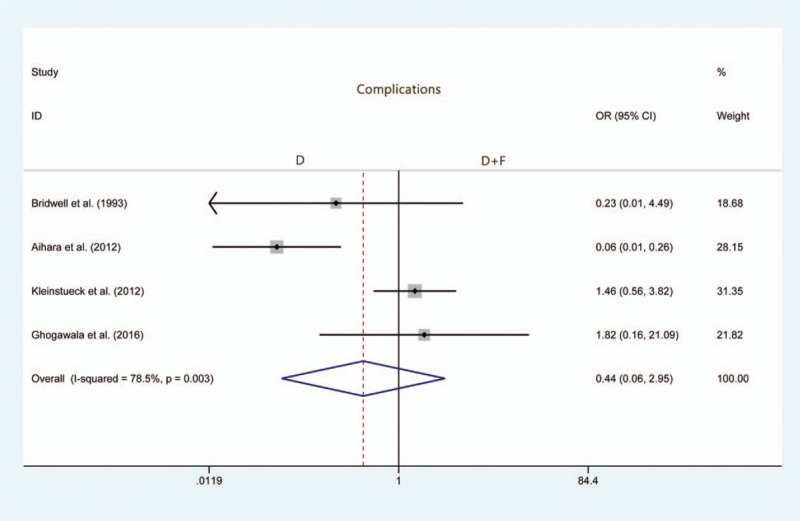
Forest plot of odds ratio (OR) of the incidence of postoperative complications with decompression versus decompression combined with fusion.
3.6. Reoperation
Three publications[1,19,20] reported the incidence of reoperation. The average rate in the D group was 18.2%, while another one in the D+F group was 7.3%. And no statistical difference was found between the 2 groups (OR, 2.541; 95% CI, 0.897–7.198; P = .079; Fig. 7).
Figure 7.
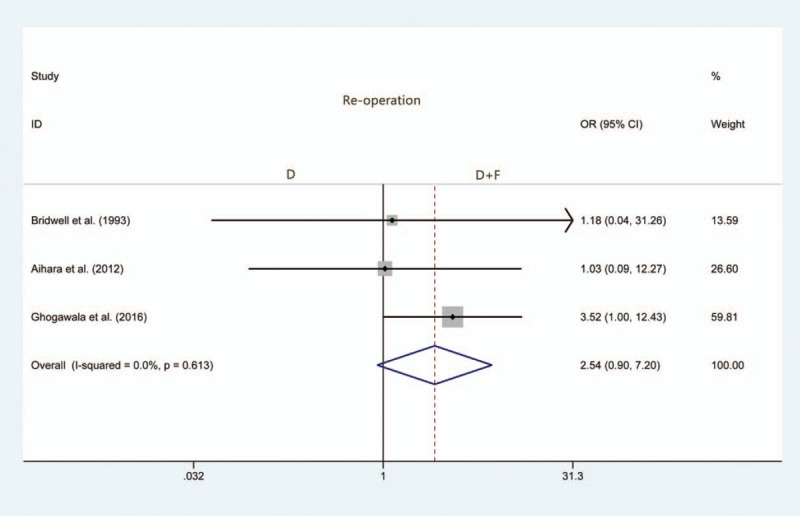
Forest plot of odds ratio (OR) of the rate of reoperation with decompression versus decompression combined with fusion.
3.7. Postoperative degenerative spondylolisthesis progression
In both groups, a certain proportion of postoperative degenerative spondylolisthesis happened at follow-up and immediate postoperation. Two RCTs[1,11] showed the number of degenerative spondylolisthesis progression and were verified no statistics difference (OR = 8.59, P = .27). More details about the outcomes were shown in Table 3.
Table 3.
Results of the meta-analysis comparison of decompression versus decompression combined with fusion.
| Groups | Overall effect | Heterogeneity | ||||||
| Outcome | Studies | Decompression | Fusion | Effect estimates | 95% CI | P-value | I2 (%) | P-value |
| LBP VAS score | 4 | 231 | 310 | –0.045 | –1.259, 1.169 | .942 | 75.1% | .007 |
| LP VAS score | 3 | 198 | 293 | 0.075 | –1.201, 1.351 | .908 | 82.8% | .003 |
| ODI score | 2 | 173 | 268 | 1.489 | –7.232, 10.211 | .738 | 74.9% | .046 |
| Odom classification | 3 | 77 | 82 | 0.353 | 0.113, 1.099 | .072 | 76.4% | .005 |
| Complications | 5 | 250 | 350 | 0.437 | 0.065, 2.949 | .395 | 78.5% | .003 |
| Re-operation | 3 | 77 | 82 | 2.541 | 0.897, 7.198 | .079 | 0.0% | .613 |
EQ-5D = European Quality of Life-5 Dimensions, LBP = low back pain, LP = leg pain, ODI = Oswestry Disability Index, VAS = visual analog scales.
4. Discussion
Clinicians never stop inventing new and advanced techniques to defeat diseases. In the terms of LDS, ongoing debates on the issue of decompression and/or fusion treatment have been strongly intense. The new emerging application of decompression combined with the fusion comes with a concern of cost performance. Whereas it is a lack of big data support, given this, we perform this meta-analysis, including 6 RCTs, quantifying and comparing the clinical outcomes. Our result showed that decompression plus fusion treatment was not found to be superior to decompression alone.
LDS patients may get an iatrogenic slip or increased spondylolisthesis degree after taking decompression surgery alone.[23] Though lacking consensus on LDS, it is deemed to be an unsteady state, and surgeons may choose the decompression plus fusion as a potential therapy for avoiding postoperative instability and restenosis. Besides, some publications believe that the efficacy of decompression alone is significantly better than the one of fusion.[24] Forsth et al[4] performed a trial involving 247 patients and found no clinical benefit even adding fusion to decompression treatment after 2 years at the cost of higher hospital charges. Meanwhile, several cohort studies have concluded no substantial benefit in taking decompression plus fusion method.[24–27]
Compared with preoperative, Forsth trial demonstrated no significant difference was found in postoperative low back pain relief.[4] Similarly, our result showed no significant value on VAS scores evaluating low back pain. Furthermore, we performed a subgroup analysis of postoperative VAS scores and found meaningless results. Same consequence came to the evaluation of leg pain. According to 3 RCTs, our analysis demonstrated negative results, which might be due to the limitation of sample size, or be explained by the quality of included RCTs, or truly indicated that the addition of fusion treatment was clinically valueless. Given the evaluation implementation of VAS, largely affected by doctors and/or patients’ subjective judge, we should combine it with other results to achieve a comprehensive understanding.
Ghogawala et al[20] wrote a paper published in N Engl J Med and concluded that no significant difference was revealed in the reduction of ODI scores between the 2 groups, and they illustrated more than twice on the improvement of ODI scores for the decompression plus fusion compared with decompression alone.[28] Nevertheless, our results demonstrated that there was no significant statistical difference between the 2 groups, which was similar to the conclusion of Brodke et al.[29] ODI scores could get influenced by the high loss rate of follow-up in 4 to 5 years, while the short-term follow-up was usually limited by a small sample size. Thus, we used EQ-5D, referencing the included 2 RCTs mentioned above, to evaluate the postoperative quality of life, and no significant value was shown between the 2 groups. Though most cases presented as 1 or 2 segments got a spondylolisthesis, fusion failed to significantly improve patients’ lives. Fusion could cause an increase in the amount of blood loss and operation time. In a word, the meaningless results could be indicated by the redundancy of fusion based on decompression.
Odom classification was applied in this meta-analysis based on 4 articles[1,3,4,11] evaluated Odom degree. It covered the item of excellent, good, fair, and poor. We defined the excellent and the good as the standard of meeting the patients’ needs. The negative result may indicate the uselessness of fusion treatment at patients’ subjective perceptions. Restored walking ability was usually regarded as a primary outcome after an operation, and it was reported that the loss for walking speed was 1.6% yearly among the elder.[30] No statistical difference was found between the 2 groups in terms of the increase in the postoperative walking distance within 2 years. It may be explained by the relatively low loss of walking ability or the independence between the improvement of walking ability and the surgery method, which means fusion is not necessary for LDS patients.
Complications involve surgery relevant complications such as intraoperative dural rupture, loose internal fixation, and systemic complications like pulmonary embolism and myocardial infarction. The major complication attributes to ASD (80%), followed by relapse/non-alleviation (15%) and internal fixation (5%). It would be more complete to do further analysis of the complication category, but this part was restrained due to the small sample size. It was reported that the increase in both spondylolisthesis degree and age were risk factors for the high incidence of complications.[31,32] Ghogawala et al calculated the reoperation rates in 4 years after surgery,[20] in the decompression group it was 34% while in the fusion group it was 14%. Dailey et al[33] deemed no association between reoperation rates of surgical segments and adjacent segments and the surgical methods. Similarly, we illustrated no statistical difference between the 2 therapy. Reoperation is more likely to be a surgeon's suggestion than a patient's appeal. A veteran surgeon would not put reoperation on the schedule unless there was no treatment option remained, and the satisfaction of patients is inversely proportional to the reoperation event to some extent. Though fusion technique could improve the unstable condition of lumbar spondylolisthesis, it holds the possibility of incurring more complications and a second operation as well.
There were 2 meta-analyses similar to our work, 1[34] included 5 RCTs with 438 patients. Another[35] included 4 RCTs and 14 non-RCTs with 77,994 patients. Both of them concluded that there are no significant differences between the 2 groups for the ODI score, EQ-5D score, the degree of satisfaction and the rate of reoperation, which is similar to our results. Given these 3 publications, if counting our work in, it is truly a hesitation to perform fusion or not in addition to only decompression for LDS patients! There were some limitations existing in our study as well. Not all indexes were compared between the pre- and postoperative group owing to not all included RCTs collected preoperative data. More vertical comparison studies were needed for further RCTs. Though low back pain and leg pain presented as the primary symptoms of LDS, a specific definition of the involved body part was a lack of consensus, which might slightly affect the outcome. The age of included patients varied from 63 to 73, we didn’t perform a smaller age span analysis due to the unavailability of original data. It was a rationale to assume that proper surgery procedures maximized the benefit for patients of a certain age. Because all our included works were English publications, we spent no spirits in considering that the language bias may potentially exist.
5. Conclusion
Based on the current results, the addition of fusion on decompression fails to reach anticipated outcomes satisfying to the price patients paid, namely, decompression alone seems to be sufficient to solve the problem. Given that the limitations arose from this analysis, a growing number of high qualities of RCTs are needed, at better with larger sample size and longer follow-up years.
Author contributions
Conceptualization: Jun Wu, Jingwei Zhang, Ting Xu, Baolong Cui, Yunlong Gao, Haiguang Yu, Xinquan Long, Yufan Zhou.
Data curation: Jun Wu, Jingwei Zhang, Ting Xu, Yongli Pan, Baolong Cui, Qingliang Huang, Yufan Zhou.
Formal analysis: Jun Wu, Jingwei Zhang, Ting Xu, Yongli Pan, Baolong Cui, Yunlong Gao, Qingliang Huang, Yufan Zhou.
Funding acquisition: Yongli Pan, Yufan Zhou.
Investigation: Jun Wu, Jingwei Zhang, Yongli Pan, Wei Wei, Yufan Zhou.
Methodology: Jingwei Zhang, Baolong Cui, Wei Wei, Yunlong Gao, Haiguang Yu, Xinquan Long, Yufan Zhou.
Project administration: Jingwei Zhang, Baolong Cui, Wei Wei, Yunlong Gao, Xinquan Long, Yufan Zhou.
Resources: Jun Wu, Jingwei Zhang, Yongli Pan, Yunlong Gao, Haiguang Yu, Yufan Zhou.
Software: Jun Wu, Jingwei Zhang, Yongli Pan, Wei Wei, Yunlong Gao, Haiguang Yu, Xinquan Long, Yufan Zhou.
Supervision: Jingwei Zhang, Yongli Pan, Yufan Zhou.
Validation: Xinquan Long, Yufan Zhou.
Visualization: Jun Wu, Yufan Zhou.
Writing – original draft: Jun Wu, Ting Xu, Yufan Zhou.
Writing – review & editing: Jun Wu, Jingwei Zhang, Ting Xu, Baolong Cui, Wei Wei.
Footnotes
Abbreviations: ASD = adjacent segment degenerative/disease, CIs = confidence intervals, D = decompression, D+F = decompression combined with fusion, EQ-5D = European Quality of Life-5 Dimensions, LDS = lumber degenerative spondylolisthesis, ODI = Oswestry Disability Index, ORs = odds ratios, PRISMA = preferred reporting items for systematic reviews and meta-analyses, RCT = randomized controlled trial, SPORT = spine patient outcomes research trial, VAS = visual analog scales, WMD = weighted mean difference.
How to cite this article: Wu J, Zhang J, Xu T, Pan Y, Cui B, Wei W, Gao Y, Yu H, Huang Q, Long Xq, Zhou Yf. The necessity or not of the addition of fusion to decompression for lumbar degenerative spondylolisthesis patients: a PRISMA compliant meta-analysis. Medicine. 2021;100:14(e24775).
JW, JZ, and TX have contributed equally to this work.
Funding: None.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Bridwell KH, Sedgewick TA, O’Brien MF, et al. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord 1993;6:461–72. [DOI] [PubMed] [Google Scholar]
- [2].Steiger F, Becker HJ, Standaert CJ, et al. Surgery in lumbar degenerative spondylolisthesis: indications, outcomes and complications. A systematic review. Eur Spine J 2014;23:945–73. [DOI] [PubMed] [Google Scholar]
- [3].Kleinstueck FS, Fekete TF, Mannion AF, et al. To fuse or not to fuse in lumbar degenerative spondylolisthesis: do baseline symptoms help provide the answer? Eur Spine J 2012;21:268–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Forsth P, Olafsson G, Carlsson T, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 2016;374:1413–23. [DOI] [PubMed] [Google Scholar]
- [5].Cummins J, Lurie JD, Tosteson TD, et al. Descriptive epidemiology and prior healthcare utilization of patients in the Spine Patient Outcomes Research Trial's (SPORT) three observational cohorts: disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spine (Phila Pa 1976) 2006;31:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jacobsen S, Sonne-Holm S, Rovsing H, et al. Degenerative lumbar spondylolisthesis: an epidemiological perspective: the Copenhagen Osteoarthritis Study. Spine (Phila Pa 1976) 2007;32:120–5. [DOI] [PubMed] [Google Scholar]
- [7].Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am 2009;91:1295–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kelleher MO, Timlin M, Persaud O, et al. Success and failure of minimally invasive decompression for focal lumbar spinal stenosis in patients with and without deformity. Spine (Phila Pa 1976) 2010;35:E981–7. [DOI] [PubMed] [Google Scholar]
- [9].Matz PG, Meagher RJ, Lamer T, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J 2016;16:439–48. [DOI] [PubMed] [Google Scholar]
- [10].Schulte TL, Ringel F, Quante M, et al. Surgery for adult spondylolisthesis: a systematic review of the evidence. Eur Spine J 2016;25:2359–67. [DOI] [PubMed] [Google Scholar]
- [11].Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 1991;73:802–8. [PubMed] [Google Scholar]
- [12].Martin CR, Gruszczynski AT, Braunsfurth HA, et al. The surgical management of degenerative lumbar spondylolisthesis: a systematic review. Spine (Phila Pa 1976) 2007;32:1791–8. [DOI] [PubMed] [Google Scholar]
- [13].Schroeder GD, Kepler CK, Kurd MF, et al. Rationale for the surgical treatment of lumbar degenerative spondylolisthesis. Spine (Phila Pa 1976) 2015;40:E1161–6. [DOI] [PubMed] [Google Scholar]
- [14].Kepler CK, Vaccaro AR, Hilibrand AS, et al. National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine (Phila Pa 1976) 2014;39:1584–9. [DOI] [PubMed] [Google Scholar]
- [15].Nasca RJ. Rationale for spinal fusion in lumbar spinal stenosis. Spine (Phila Pa 1976) 1989;14:451–4. [DOI] [PubMed] [Google Scholar]
- [16].Johnsson KE, Redlund-Johnell I, Uden A, et al. Preoperative and postoperative instability in lumbar spinal stenosis. Spine (Phila Pa 1976) 1989;14:591–3. [DOI] [PubMed] [Google Scholar]
- [17].Resnick DK, Watters WC, 3rd, Sharan A, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: lumbar fusion for stenosis with spondylolisthesis. J Neurosurg Spine 2014;21:54–61. [DOI] [PubMed] [Google Scholar]
- [18].Moher D, Liberati A, Tetzlaff J, et al. Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Aihara T, Toyone T, Aoki Y, et al. Surgical management of degenerative lumbar spondylolisthesis: a comparative study of outcomes following decompression with fusion and microendoscopic decompression. J Musculoskelet Res 2012;15:1250020. [Google Scholar]
- [20].Ghogawala Z, Dziura J, Butler WE, et al. Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 2016;374:1424. [DOI] [PubMed] [Google Scholar]
- [21].Hackenberg L, Halm H, Bullmann V, et al. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 2005;14:551–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Strömqvist B, Fritzell P, Hägg O, et al. The Swedish Spine Register: development, design and utility. Eur Spine J 2009;18: (suppl): 294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Fox MW, Onofrio BM, Onofrio BM, et al. Clinical outcomes and radiological instability following decompressive lumbar laminectomy for degenerative spinal stenosis: a comparison of patients undergoing concomitant arthrodesis versus decompression alone. J Neurosurg 1996;85:793–802. [DOI] [PubMed] [Google Scholar]
- [24].Transfeldt EE, Topp R, Mehbod AA, et al. Surgical outcomes of decompression, decompression with limited fusion, and decompression with full curve fusion for degenerative scoliosis with radiculopathy. Spine (Phila Pa 1976) 2010;35:1872–5. [DOI] [PubMed] [Google Scholar]
- [25].Forsth P, Michaelsson K, Sanden B. Does fusion improve the outcome after decompressive surgery for lumbar spinal stenosis?: A two-year follow-up study involving 5390 patients. Bone Joint J 2013;95-B:960–5. [DOI] [PubMed] [Google Scholar]
- [26].Rampersaud YR, Fisher C, Yee A, et al. Health-related quality of life following decompression compared to decompression and fusion for degenerative lumbar spondylolisthesis: a Canadian multicentre study. Can J Surg 2014;57:E126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Sigmundsson FG, Jonsson B, Stromqvist B. Outcome of decompression with and without fusion in spinal stenosis with degenerative spondylolisthesis in relation to preoperative pain pattern: a register study of 1,624 patients. Spine J 2015;15:638–46. [DOI] [PubMed] [Google Scholar]
- [28].Ghogawala Z, Benzel EC, Amin-Hanjani S, et al. Prospective outcomes evaluation after decompression with or without instrumented fusion for lumbar stenosis and degenerative Grade I spondylolisthesis. J Neurosurg Spine 2004;1:267–72. [DOI] [PubMed] [Google Scholar]
- [29].Brodke DS, Prokopis A, Lawrence BD, et al. Reoperation and revision rates of 3 surgical treatment methods for lumbar stenosis associated with degenerative scoliosis and spondylolisthesis. Spine (Phila Pa 1976) 2013;38:2287–94. [DOI] [PubMed] [Google Scholar]
- [30].Mahant PR, Stacy MA. Movement disorders and normal aging. Neurol Clin 2001;19:553–63. [DOI] [PubMed] [Google Scholar]
- [31].Sansur CA, Reames DL, Smith JS, et al. Morbidity and mortality in the surgical treatment of 10,242 adults with spondylolisthesis. J Neurosurg Spine 2010;13:589–93. [DOI] [PubMed] [Google Scholar]
- [32].Steiger F, Becker H-J, Standaert CJ, et al. Surgery in lumbar degenerative spondylolisthesis: indications, outcomes and complications. A systematic review. Eur Spine J 2014;23:945–73. [DOI] [PubMed] [Google Scholar]
- [33].Andrew D, Harrop JS, France JC. High-energy contact sports and cervical spine neuropraxia injuries: what are the criteria for return to participation? Spine (Phila Pa 1976) 2010;35: (21 suppl): 193–201. [DOI] [PubMed] [Google Scholar]
- [34].Shen J, Xu S, Xu S, et al. Fusion or not for degenerative lumbar spinal stenosis: a meta-analysis and systematic review. Pain Physician 2018;21:01–8. [PubMed] [Google Scholar]
- [35].Chen Z, Xie P, Feng F, et al. Decompression alone versus decompression and fusion for lumbar degenerative spondylolisthesis: a meta-analysis. World Neurosurg 2018;111:e165–77. [DOI] [PubMed] [Google Scholar]


