Abstract
Clopidogrel is a widely-used antiplatelet drug. It is important for the treatment and prevention of coronary heart disease. Clopidogrel can effectively reduce platelet activity and therefore reduce stent thrombosis. However, some patients still have ischemic events despite taking the clopidogrel due to the alteration in clopidogrel metabolism attributable to various genetic and non-genetic factors. This review aims to summarise the mechanisms and causes of clopidogrel resistance (CR) and potential strategies to overcome it. This review summarised the possible effects of genetic polymorphism on CR among the Asian population, especially CYP2C19 *2 / *3 / *17, where the prevalence rate among Asians was 23.00%, 4.61%, 15.18%, respectively. The review also studied the effects of other factors and appropriate strategies used to overcome CR. Generally, CR among the Asian population was estimated at 17.2–81.6%. Therefore, our overview provides valuable insight into the causes of RC. In conclusion, understanding the prevalence of drug metabolism-related genetic polymorphism, especially CYP2C19 alleles, will enhance clinical understanding of racial differences in drug reactions, contributing to the development of personalised medicine in Asia.
Keywords: clopidogrel 2, antiplatelet 3, clopidogrel resistance 4, CYP2C19 polymorphism 5, personalized medicine
1. Introduction
Decreased response to clopidogrel among the Asian population is typical due to genetic polymorphism and other factors associated with clopidogrel resistance, estimated to be 70% in some Asian societies. Studying the Asian population is necessary, especially since many Asians have moved to all parts of the world due to increased immigration, making the current guidelines for genetic testing or platelet response testing not generally applicable before prescribing clopidogrel. Therefore, it is essential for clinicians treating Asian patients to consider inter-individual variability in response to clopidogrel when prescribing the drug [1].
Current guidelines suggest the use of dual antiplatelet therapy (DAPT), involving aspirin with a P2Y12 receptor inhibitor to prevent atherothrombotic events in patients with acute coronary syndrome (ACS) and those undergoing percutaneous coronary intervention (PCI) [2,3,4]. Clopidogrel is currently one of the most widely used P2Y12 receptor inhibitors [4,5,6]. Many large clinical trials have confirmed the antiplatelet effect of clopidogrel. One such trial found the use of aspirin in conjunction with clopidogrel antiplatelet therapy in patients with ACS, can reduce adverse coronary events by 20% [7]. This finding agrees with the Clopidogrel and Metoprolol in Myocardial Infarction Trial/Second Chinese Cardiac Study (COMMIT/CCS-2) research that showed that the use of clopidogrel (75 mg) in conjunction with aspirin in a group of myocardial infarction patients was found to reduce major vascular events and mortality [8].
Although clopidogrel has a significant effect on antiplatelet aggregation, studies have shown that platelets’ response to clopidogrel varies significantly between people [9,10]. Some patients can also develop recurrent ischemic events such as stent thrombosis and myocardial infarction during treatment with clopidogrel. This failure of platelet aggregation inhibition in clopidogrel users is referred to as clopidogrel resistance (CR) or platelet hyperresponsiveness [11,12,13]. Studies have shown that 4 to 30% of patients have CR, and 5 to 6% of patients have DAPT resistance after implanting the stent [14,15]. Matetzky et al. (2004) also found that up to 25% of patients with severely raised acute ST-segment elevation myocardial infarction demonstrated CR, which is associated with a higher risk of developing cardiovascular disease [16]. Muller et al. (2003) found that 4.7% of patients who take clopidogrel after PCI have low platelet inhibition rates, which is associated with an increased risk of clinical thrombosis [17]. Based on several studies, the prevalence of CR in the Asian population was reported to be between 17.2 to 81.6%. (Table 1).
Table 1.
Prevalence of clopidogrel resistance (CR) in various studies in the Asian population.
| Investigators | Country | Number of Patients | Clopidogrel Loading Dose (mg) | CR |
|---|---|---|---|---|
| Ma et al. 2019 [18] | China | 441 | 300 | 17.2% |
| Pareed et al. 2020 [19] | India | 200 | 300 | 32% |
| Namazi et al. 2012 [20] | Iran | 112 | 600 | 25.90% |
| Sahib et al. 2016 [21] | Iraq | 127 | 300 | 24% |
| Park et al. 2011 [22] | Korea | 114 | 75/150 | 46% |
| Amin et al., 2017 [23] | Malaysia | 71 | 600 | 38% |
| Sakr et al., 2016 [24] | Saudi Arabia | 49 172 83 |
75 300 600 |
81.6% 66.3% 55.4% |
| Tekkeşin et al. 2016 [25] | Turkish | 1.238 | 600 | 30.2% |
| Range | 17.2–81.6% |
Various genetic and non-genetic factors affect clopidogrel resistance. This review aims to summarise the mechanisms and causes of clopidogrel resistance (CR) and the potential strategies to overcome it.
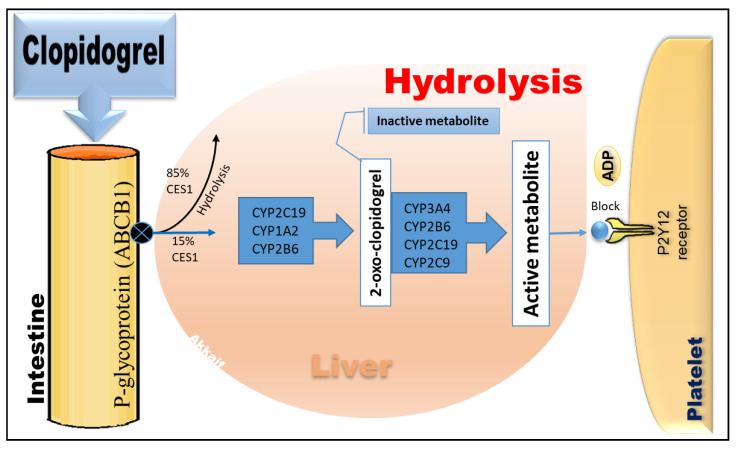
2. The Pharmacological Effects of Clopidogrel
Clopidogrel is a thiophene pyridine prodrug that needs to be absorbed by the intestines and transformed into active components by the metabolism of various enzymes in the liver to exert its platelet anti-aggregation effect [26]. The P-glycoprotein (P-gp), encoded by the ABCB1 gene, regulates clopidogrel absorption in the small intestine [27]. P-gp is a transmembrane protein with the primary function of pumping the drug out of the cell and into the blood circulation. This pumping mechanism may affect the drug’s bioavailability. After clopidogrel absorption in the intestine, 85% is hydrolysed by carboxylesterase 1 (CES1) to inactive metabolites and excreted in urine or faeces [28]. Only 15% is passed through cytochrome P450 in the liver, where clopidogrel is first converted into intermediate metabolite (2-oxo-clopidogrel) by CYP2C19, CYP1A2, and CYP2B6 and then catalysed by CYP2C19, CYP2C9, CYP3A4, and CYP2B6 to produce an active metabolite. It selectively and irreversibly binds to the adenosine diphosphate (ADP) P2Y12 receptor on the platelet membrane to reduce ADP. The binding site blocks the ADP-mediated binding of fibrinogen to its receptor glycoprotein IIb/IIIa, inhibits platelet activation and aggregation, and exerts antiplatelet effects [29,30]. The metabolic pathway of clopidogrel is depicted in Figure 1.
Figure 1.
The metabolic pathway of clopidogrel and its target receptors.
3. Definition of Clopidogrel Resistance
There is currently no uniform definition of CR, but the most accepted is that the drug has lost its target of the action. It is generally believed that CR means that a patient still has a thrombotic event after receiving clopidogrel treatment, and laboratory tests show that platelet function is not inhibited [31]. Some researchers refer to it as clinical resistance among patients who have experienced thromboembolism and other adverse events following long-term oral clopidogrel therapy [1]. The incidence of CR varies among different regions and races. According to literature reports, the incidence of CR in Western countries is 5 to 44%, while in Asian populations, it may be as high as 20 to 65% [1,32].
There are several methods commonly used to evaluate platelet function. The oldest and more accurate way is optical turbidimetry, which is often considered the gold standard. This method assesses the responsiveness of platelets to ADP through the function of P2Y1 and P2Y12 receptors. However, because of the repetition rate and the lack of a specific P2Y12 pathway, its use is limited. At present, vasodilator-stimulated phosphoprotein (VASP) phosphorylation assay (VerifyNow) and bedside monitoring are widely used due to the relatively easy operation [11,33]. Tantry and colleagues (2014), in their follow-up studies on CR, confirmed that the available evidence does not support routine screening for hypo/non-responsiveness in patients who started treatment with clopidogrel [34]. So far, there is still a lack of standard experimental methods for diagnosing CR. Clinically, platelet function can be tested to determine the patient’s platelet reaction after medication intake to identify the potential risk of increased cardiovascular or bleeding events. The incidence of CR in elderly patients may be higher than that in younger patients, and the risk of bleeding with clopidogrel is also increased [35,36,37].
The use of platelet function tests (PFTs) to allocate a better selection of antiplatelet drugs to patients with cardiovascular disease has been discussed over the past ten years [38]. These studies mitigated the escalation of antiplatelet therapy according to the results of PFTs for potential clinical benefit. Furthermore, the 2011 American College of Cardiology/American Heart Association guidelines issued a Class IIb recommendation for the use of PFTs among patients taking P2Y12 inhibitors [39]. Still, this classification was downgraded to a Category III recommendation in 2016 [40]. In ACS cases, the latest European guidelines indicate that de-escalation, but not escalation, of P2Y12 inhibitors directed by PFT, with a Class IIb rating, can be considered [41].
4. Factors Associated with CR
The mechanism of CR is still unclear. Relevant studies have shown that CR may be influenced by various factors such as race, age, weight, genetic polymorphism, drug interaction, diabetes, inflammation, immature platelets, atherosclerosis, medication compliance and other factors. Despite these various contributing factors of clopidogrel resistance, the exact mechanism is currently unknown [1,37,42,43,44,45,46,47,48,49].
4.1. Gene Polymorphism
Many studies have been done to determine the relationship between P2Y12 receptor gene polymorphism and CR (Table 2). Zoheir et al. (2013) found that P2Y12 receptor gene polymorphism is closely related to platelet activity [50]. The P-gp encoded by ABCB1 regulates the absorption of clopidogrel in the intestines. Earlier studies by Mega et al. (2009) found that ABCB1 gene polymorphism affects the degree of platelet inhibition, which is closely related to the risk of major adverse cardiac events (MACE) [5]. However, in recent years, studies on the Chinese population have shown no association between ABCB1 gene polymorphism and CR [51,52,53].
Table 2.
Genetic polymorphism distribution and allele frequencies in clopidogrel-resistant and non-clopidogrel-resistant groups.
| Author | Population | Population Sample | Gene | SNP | Genotype | Allele Frequencies | Total (n/%) |
p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| CR Group (n/%) |
NCR Group (n/%) |
||||||||
| Li et al., 2020 [62] | China | 126 | CYP2C19*2 | rs4244285 | GG (*1/*1) GT (*1/*2) TT (*2/*2) |
9 (23.1%) 21 (53.8%) 9 (23.1%) |
48 (55.2%) 30 (34.5%) 9 (10.3%) |
57 (45.2%) 51 (40.5%) 18 (14.3%) |
0.001 0.041 0.093 |
| CYP2C19*3 | rs4986893 | GG (*1/*1) GT (*1/*3) TT (*3/*3) |
27 (69.2%) 10 (25.6%) 2 (5.1%) |
75 (86.2%) 11 (12.6%) 1 (1.2%) |
102 (80.9%) 21 (16.7%) 3 (2.4%) |
0.025 0.070 0.176 |
|||
| Al-Azzam et al., 2013 [63] | Jordan | 240 | CYP2C19*2 | rs4244285 | GG (*1/*1) GT (*1/*2) TT (*2/*2) |
22 (22.9%) 38 (31.7%) 16 (67.7%) |
74 (77.1%) 82 (68.3%) 8 (33.3%) |
96(40%) 120(50%) 24(10%) |
<0.001 |
| Lee et al., 2009 [64] | Korean | 387 | CYP2C19*2 | rs4244285 | GG GA AA |
55(49.1%) 40(35.7%) 13(11.6%) |
155(56.4%) 93(33.8%) 26(9.5%) |
210(54.3%) 133(34.4%) 39(10.1%) |
0.287 |
| CYP2C19*3 | rs4986893 | GG GA AA |
80(71.4%) 31(27.7%) 1(0.9%) |
236(85.8%) 37(13.5%) 1(0.4%) |
316(81.7%) 68(17.6%) 2(0.5%) |
0.001 | |||
| Amin et al., 2017 [23] | Malaysia | 71 | CYP2C19*2 | rs4244285 | GG (*1/*1) GT (*1/*2) TT (*2/*2) |
11 (40.7%) 8 (29.6%) 8 (29.6%) |
19 (43.2%) 22 (50.0%) 3 (6.8%) |
30 (42.3%) 30 (42.3%) 11(15.5) |
0.026 |
| Alhazzani, et al., 2017 [65] | Saudi Arabia | 50 | CYP2C19*2 | rs4244285 | GG GA + AA |
21(84%) 4(16%) |
10(40%) 15(60%) |
31(62%) 19((38%) |
0.001 |
| CYP2C19*3 | rs4986893 | GG GA + AA |
20(80%) 5(20%) |
13(52%) 12((48%) |
33(66%) 17(34%) |
0.036 | |||
| Shijun et al., 2014 [66] | China | 95 | CYP3A4*G1 | rs2242480 | (GG) (GA + AA) |
24 (61.50%) 15 (38.50%) |
33 (58.90%) 23 (41.10%) |
57 (60.00%) 38 (40.00) |
0.798 |
| Namazi, et al. 2012 [20] | Iran | 112 | CYP3A5 | rs776746 | (*1/*1) (*1/*3) (*3/*3) |
- | - | 9 (8.00%) 42 (37.50%) 61(54.50%) | >0.05 |
| Al-Husein et al., 2018 [67] | Jordan | 280 | CYP3A4 | rs2242480 | (*1/*1) (*1/*3+ *3/*3) |
80(28.6%) 1 (0.4%) |
196 (70%) 3 (1.1%) |
276 (98.6%) 4 (1.4%) |
>0.9999 |
| CYP3A5 | rs776746 | (*1/*1) (*1/*3) (*3/*3) |
57 (20.4%) 23(8.2%) 119(42.5%) |
24(8.6%) 10(3.6%) 47(16.8%) |
81(28.9%) 33(11.8%) 166(59.3%) |
0.961 | |||
| Lee et al., 2009 [64] | Korean | 387 | CYP3A4 | rs2246709 | TT TC CC |
42(37.5%) 57(50.9%) 12(10.7%) |
103(37.5%) 139(50.5%) 28(10.2%) |
145(37.5%) 196(50.6%) 40(10.3%) |
0.925 |
| rs2242480 | GG GA AA |
74(66.1%) 32(28.6%) 6(5.4%) |
172(62.5%) 90(32.7%) 13(4.7%) |
246(63.6%) 122(31.5%) 19(4.9%) |
0.568 | ||||
| CYP3A5 | rs776746 | GG GA AA |
61(54.5%) 41(36.6%) 6(5.4%) |
154(56.0%) 102(37.1%) 12(4.4%) |
215(55.6%) 143(37.0%) 18(4.7%) |
0.808 | |||
| Shasha et al., 2020 [68] | China | 741 | ABCB1 | rs1045642 | GG GA + AA |
94(38.5%) 222(70.3%) |
161(44.4%) 264(62.1%) |
255(34.4%) 486(65.6%) |
0.021 |
| Chen et al., 2021 [69] | China | 204 | MDR1 | rs 1128503 | CC CT TT |
12 (24%) 17 (34.7%) 20 (40.8%) |
40 (25.8%) 65 (41.9%) 50 (32.3%) |
52 (25.5%) 82 (40.2%) 70 (34.3%) |
0.521 |
| Li et al., 2020 [62] | China | 126 | P2Y12 | rs6809699 | GG GT TT |
15 (38.5%) 21 (53.8%) 3 (7.7%) |
67 (79.3%) 18 (20.7%) 2 (2.3%) |
82 (66.7%) 39 (30.9%) 5 (2.4%) |
0.000 0.000 0.152 |
| Namazi et al., 2012 [20] | Iran | 112 | rs2046934 | CC CT + TT |
- | - | 104(92.9%) 8 (7.1%) |
>0.05 | |
| Lee et al., 2009 [64] | Korean | 387 | rs2046934 | TT TC CC |
81(72.3%) 26(23.2%) 4(3.6%) |
177(64.4%) 89(32.4%) 8(2.9%) |
258(66.7%) 115(29.7%) 12(3.1%) |
0.139 | |
CR, clopidogrel resistance; NCR, non-clopidogrel resistance; GG, CC, AA, TT, *1/*1, *2/*2, *3/*3, homozygous; GC, GA, GT, CT, *1/*2, *1/*3, heterozygous.
CYP3A4/5 are among the essential enzymes in clopidogrel activation. Previously, Lau et al. (2004) have shown that lower CYP3A4 activity, determined using an erythromycin breath test, is associated with a lower antiplatelet effect of the drug [54].
One study aimed to determine the effect of the CYP3A homologs of sub-enzymes (allelic variants of CYP3A4 * 22 and CYP3A5 * 3) on the efficacy of clopidogrel in patients with ACS undergoing percutaneous coronary intervention. The study results found that CYP3A4 / 5 activity was not associated with platelet aggregation rates, as well as the genotyping and phenotyping of CYP3A4 / CYP3A5 did not predict the antiplatelet effect of clopidogrel. The researcher recommended more extensive research to prove its clinical relevance [55].
The genetic variations in CYP450 isoenzymes genes (CYP1A2, CYP2B6, CYP2C9, CYP2C19, and CYP3A4), which are involved in drug metabolism, can influence the variation of pharmacodynamic response to clopidogrel, especially the genetic variation in the CYP2C19 isoenzyme. This enzyme contributes significantly to the two sequential oxidative steps in the biotransformation of clopidogrel into active metabolites [56,57]. Hence, genetic polymorphism of CYP2C19 could play a crucial role in wide inter-individual and inter-ethnic variabilities in clinical response towards clopidogrel [58,59,60,61].
The choice of antiplatelet therapy (clopidogrel, ticagrelor, or prasugrel) based on individual patient characteristics, such as treatment choice based on genetic data related to clopidogrel metabolism as well as considerations regarding the clinical features of patients may result in a significantly lower rate of ischemic and hemorrhagic events compared to usual practice [70]. The choice of antiplatelet therapy based on both CYP2C19 gain of function (GOF) and loss of function (LOF) alleles appears to be a preferred approach over universal clopidogrel and universal variant P2Y12 inhibitor therapy for ACS patients with PCI [71,72]. CYP2C19-guided escalation and de-escalation are common as clopidogrel persistence in nonfunctional allele carriers is associated with adverse outcomes [73].
Genetic polymorphisms in CYP2C19 were classified into groups and referred to as alleles. The preliminarily identified alleles include 36 alleles such as CYP2C19 *1,*2, *3, *4, *5, *6, *7 or *8 etc. of which the most significant impact on clopidogrel is *2/*3 mutation sites (weak metabolites) and *17 mutation sites (strong metabolites). The frequency of other variations in most population groups is low [74]. According to clinical guidelines issued by the Clinical Pharmacogenetics Implementation Consortium (CPIC), genotype-related individual variability in metabolic enzyme function is divided into four predicted CYP2C19 metabolic phenotypes: Poor metabolisers (PMs), intermediate metabolisers (IMs), Extensive metabolisers (EMs), and Ultrarapid metabolisers (UMs) [75] (Table 3).
Table 3.
The categorisation of the predicted CYP2C19 metabolic phenotypes based on the CYP2C19 genotypes [75].
| Likely Phenotype | Genotypes | Examples of Diplotypes |
|---|---|---|
| Ultrarapid metaboliser: Normal or increased activity (−5–30% of patients) | An individual carrying two increased activity alleles (*17) or one functional allele (*1) plus one increased-activity allele (*17) |
*1/*17,
*17/ *17 |
| Extensive metaboliser: Homozygous wild-type or normal activity (~35–50% of patients) | An individual carrying two functional (*1) alleles. | *1/*1 |
| Intermediate metaboliser: Heterozygote or intermediate activity (~18–45% of patients) | An individual carrying one functional allele (*1) plus one loss-of-function allele (*2-*8) or one loss-of-function allele (*2-*8) plus one increased-activity allele (*17) |
*1/ *2,
*1/*3, *2/*17 |
| Poor metaboliser: Homozygous variant, mutant, low, or deficient activity (~2–15% of patients) | An individual carrying two loss-of-function alleles (*2-*8) |
*2/*2,
*2/*3, *3/*3 |
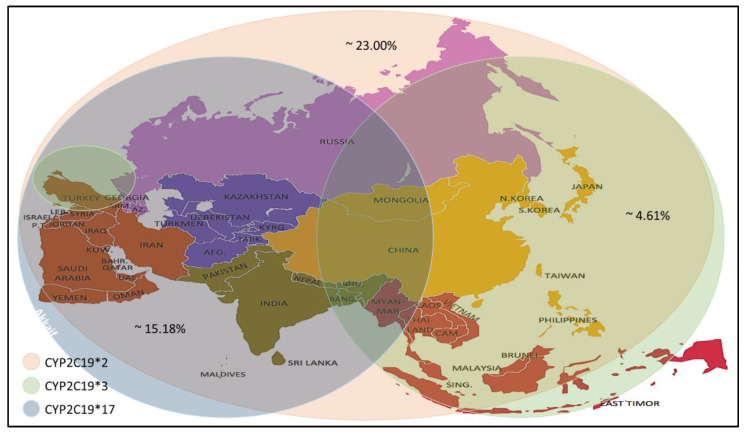
Many studies have reported wide inter-ethnic variability in CYP2C19 polymorphism. Asian populations (~ 55.0 to 70.0%) have a higher prevalence rate of CYP2C19 LOF variant alleles (CYP2C19 *2 and *3) as compared with white populations (~ 25.0 to 35.0%) and black populations (~35.0 to 45.0%) [76,77]. On the other hand, Asian populations (~4.0%) have a low prevalence of the CYP2C19 GOF variant allele (CYP2C19 *17) as compared to white populations (~18.0%) [78,79].
Recent studies have reported a variation in the prevalence of individuals carrying CYP2C19 alleles among the Asian population (Table 4). The CYP2C19 * 2 allele was found in individuals of the selected countries, with prevalence rates ranging between 4.0–59.6%, with an average prevalence rate of 23.00%. The percentage prevalence of CYP2C19 * 2 allele in Saudi Arabia, Qatar and Jordan was less than 10% (residents of the Arabian Peninsula), which is low compared to others. Meanwhile, the CYP2C19 * 3 allele prevalence was found at rates up to 0–13.03% with an average prevalence rate of 4.61%. It is noticed that the spread of this allele is higher in the countries of Southeast and East Asia. Still, its prevalence rates are lower in India, located in the south of Asia, Russia, which is in its north and most countries in West Asia, excluding Turkey. From the CYP2C19 * 17 allele prevalence data, it is noticed that the prevalence rates ranged between (1- 28.72) %, with an average rate of 15.18%, as it is seen here that there are high prevalence rates in the North, South and West Asia. Medium to low rates are observed in some Central and Southeast Asia (Figure 2).
Table 4.
CYP2C19 allele frequencies (* 2, * 3 and * 17) % among Asian ethnic groups.
| Author | Population | Population Sample | Method | Allele Frequency (%) | ||
|---|---|---|---|---|---|---|
| CYP2C19*2 | CYP2C19*3 | CYP2C19*17 | ||||
| Zhong et al., (2017) [80] | China | 6686 | PCR and DNA Sequencing | 31.06 | 4.61 | ND |
| T. Wang et al., (2020) [81] | China | 1129 | TaqMan-Real-Time PCR | ND | ND | 2.5 |
| (Anichavezhi, Chakradhara Rao, Shewade, Krishnamoorthy, & Adithan, (2012) [82] | India | 206 | PCR-RFLP | 40.2 | 0 | 19.2 |
| Dehbozorgi et al., (2018) [83] | Iran | 1,229 | PCR and DNA Sequencing | 21.4 | 1.7 | 27.1 |
| Sahib, Mohammed, & Abdul-Majid, (2015) [84] | Iraq | 221 | PCR and DNA Sequencing | 15.2 | 0.2 | 19.5 |
| Sugimoto, Uno, Yamazaki, & Tateishi, (2008) [79] | Japanese | 265 | PCR-RFLP | 27.9 | 12.8 | 1.13 |
| (Sviri, Shpizen, Leitersdorf, Levy, & Caraco, (1999) [85] | Jewish Israeli | 136 | PCR-RFLP | 15 | 1 | ND |
| Rjoub et al., 2018 [86] | Jordanian | 148 | PCR-RFLP | 9.8 | ND | 28.72 |
| Kim, Song, Kim, & Park, (2010) [87] | Korean | 271 | PCR and pyrosequencing | 28.4 | 10.1 | 1.5 |
| Amin et al., (2017) [88] | Malaysia | 89 | PCR and DNA Sequencing | 59.6 | 6.74 | ND |
| Riaz et al., (2019) [89] | Pakistan | 1028 | ASA-PCR | 29.0 | ND | 23.70 |
| (Ayesh, Al-Astal, & Yassin, (2019) [90] | Palestinian | 110 | PCR-RFLP | 15.5 | 2.3 | ND |
| Elewa, Ali, & Bader, (2018) [91] | Qatar | 129 | TaqMan-Real-Time PCR | 4 | 0 | 10 |
| Mirzaev et al., (2017) [92] | Russia | 512 | TaqMan-Real-Time PCR | 11.25 | 1.2 | 22 |
| Al-Jenoobi et al., 2013 [93] | Saudi Arabia | 192 | PCR and DNA Sequencing | 8.2 | 0 | 26.9 |
| Sukasem et al., (2013) [94] | Thai | 1051 | AmpliChip CYP450 test | 41.95 | 13.03 | 4.30 |
| (Arici & Özhan, (2017) [95] | Turkish | 160 | PCR-RFLP | 12 | 13 | 25 |
| Vu et al., (2019) [96] | Vietnam | 100 | PCR-RFLP | 20.5 | 2.5 | 1 |
| Total | 13662 | |||||
| Average | 23.00 | 4.61 | 15.18 | |||
Population sample: The number of screened individuals. ND: No data.
Figure 2.
Prevalence of the CYP2C19 * 2/*3/*17 alleles in the Asian population.
In general, the high allele frequency of CYP2C19 * 2 and * 17 in the Asian population led to the recommendation of a pre-treatment test to monitor for clopidogrel response, dose and to avoid adverse drug reactions after treatment.
4.2. Drug Interactions
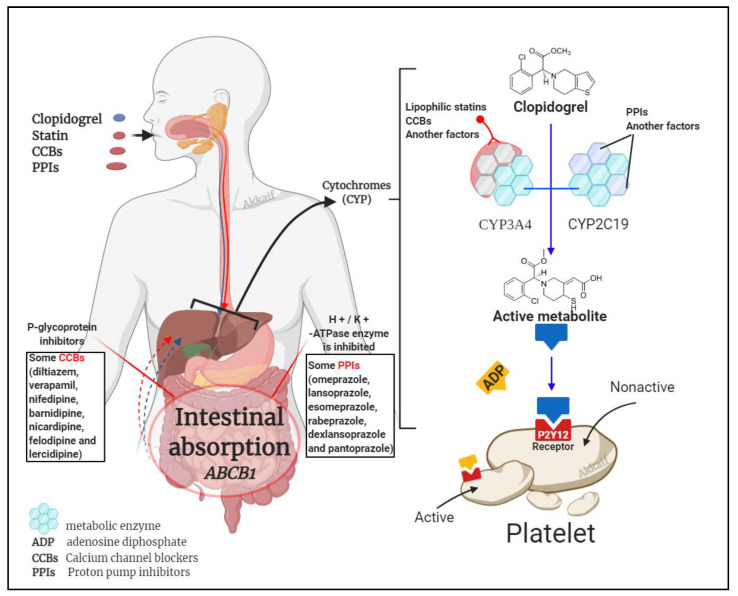
It is known that clopidogrel is converted into an effective product through the metabolic pathway mediated by CYP enzymes. This process involves a variety of isoenzymes. Such as CYP2C19, CYP3A4, CYP1A2, CYP2C9, etc., but the most important ones are CYP3A4 (~40%) and CYP2C19 (~45%) that contribute to the formation of the active metabolite of clopidogrel; so, the combined use of CYP3A4 and CYP2C19 inhibitors may affect the metabolism of clopidogrel [57,97]. Besides clopidogrel, the CYP3A4 pathway also metabolises statins and calcium channel blockers, and the CYP2C19 pathway metabolises proton pump inhibitors (PPIs) [28,98]. Figure 3 illustrates the mechanism by which these three compounds affect clopidogrel.
Figure 3.
Drug interaction mechanism of clopidogrel with statins, calcium channel blockers (CCBs) and proton pump inhibitors (PPIs).
4.2.1. Clopidogrel Interaction with Statins
Drug interactions between clopidogrel and statins have been examined and documented over several years. Although most data indicate drug interaction between these drugs, the clinical significance is the determining factor when considering the therapeutic benefit over risk. Statins serve as a lipid-lowering agent, while clopidogrel acts as an inhibitor of platelets. Doctors usually prescribe both drugs to patients for primary prevention of cardiovascular disease and secondary prevention of cardiovascular atherosclerosis (ASCVD) disease among high-risk patients [99,100].
Statins inhibit 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA)-reductase, which is responsible for reducing the rate of cholesterol formation. Except for pravastatin, statins undergo extensive hepatic metabolism by multiple cytochrome P450 (CYP) enzymes. The main metabolising enzymes of both clopidogrel and a statin include CYP3A4 and CYP2C9. CYP3A4 mainly metabolises atorvastatin, lovastatin, and simvastatin, whereas CYP2C9 metabolises fluvastatin and rosuvastatin. The level of metabolic activity of CYP3A4 is inversely related to the antiplatelet effects of clopidogrel [28,101].
When statins and clopidogrel are used in combination they may interact via the CYP3A4 metabolic pathway, due to binding site competition. This combination may reduce the antiplatelet activity of clopidogrel, although the effects are still controversial. Lau et al. (2004) had reported that atorvastatin affects clopidogrel level via the CYP3A4 metabolic pathway, while the effect was not present in pravastatin which was not a substrate to CYP3A4 [102]. The report has attracted widespread attention [100,103,104,105]. However, other related studies have not confirmed the effect of CYP3A4 metabolism of statins on the antiplatelet effect of clopidogrel [106,107]. A meta-analysis on the effects of the concomitant administration of clopidogrel and statins reported that statin use decreases patients’ mortality rate with clopidogrel therapy without influencing platelet activation and aggregation [108]. A clinical trial of 190 elective PCI candidates demonstrated that they were already using statins and/or other lipid-lowering agents such as fibrates. The results showed that the administration of a high reload dose of atorvastatin within 24 h prior to the PCI significantly reduced the frequency of myocardial infarction [109]. A study by Karaźniewicz-Łada et al. was the first study identifying the effect of atorvastatin and rosuvastatin on the pharmacokinetics of clopidogrel and its metabolites, and the report had confirmed that systemic exposure to clopidogrel in patients after coronary stent implantation did not depend on statins [110].
4.2.2. Calcium Channel Blockers
Calcium channel blockers (CCBs) are frequently used in patients with high blood pressure, CAD, and arrhythmias. CCBs are metabolized by CYP3A4 to inactive metabolites [111,112]. This may affect the metabolism of clopidogrel via CYP3A4, which is a secondary metabolic enzyme for clopidogrel [113]. Recently, researchers have been interested in the interaction of clopidogrel with CCBs and its effect on clopidogrel efficacy, both in vitro and in vivo [114]. Lee et al., 2020 had indicated that CCBs metabolised by CYP3A4 could reduce the effectiveness of clopidogrel, which is reflected in platelet inhibition. However, the findings on drug interactions between CCBs and clopidogrel are controversial. Amlodipine, which is metabolised by CYP3A4 but not a substrate to P-gp, has been shown to cause alterations in clopidogrel response. Conversely, the co-administration of clopidogrel and verapamil/diltiazem has not been shown to impair the antiplatelet effects induced by clopidogrel. These different results may be explained by the presence or absence of an inhibitory effect of P-gp. P-gp inhibited by CCBs could increase clopidogrel plasma concentration and may attenuate the effect of the interaction between clopidogrel and CCBs through CYP3A4. However, there is no firm evidence that this potential drug interaction between amlodipine and clopidogrel affects clinical outcomes [115].
4.2.3. Proton Pump Inhibitors (PPIs)
PPIs are primary medications that do not require enzyme activity to convert them to their active metabolites. In parietal stomach cells, the H+ / K+ -ATPase enzyme is inhibited, reducing stomach acid production. This drug class includes omeprazole, lansoprazole, esomeprazole, rabeprazole, dexlansoprazole, and pantoprazole. CYP2C19 and CYP3A4 are mainly involved in transforming the PPIs into inactive metabolites [116].
It has been inconclusive for patients who use PPI and clopidogrel simultaneously whether the combination of these two would impact the clopidogrel response. Although several studies have shown no interaction between clopidogrel and PPIs, several questions have been raised about why the antiplatelet inhibition of clopidogrel is reduced with PPIs. Studies published between 2012 to 2016 found that this combined use was associated with significantly higher adverse cardiac events such as major adverse cardiovascular events (MACEs) and ST-Elevation Myocardial Infarction (STEMI) after PCI; however, long-term mortality is not related [117]. It led to a black box warning admonition by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) in 2009–2010. Importantly, with each PPI, pharmacokinetics/pharmacodynamics tests have shown that drug-drug interactions are different between clopidogrel and PPIs. Therefore, this is not a class effect but a drug-specific effect involving agents that interfere mainly with the action of CYP2C19. The FDA labels were changed according to individual PPIs in 2011–2012, which warn against the concomitant use of omeprazole and esomeprazole with clopidogrel and to highlight the lack of interaction between pantoprazole, lansoprazole and dexlansoprazole with clopidogrel [115].
4.3. Dose Factors
The anti-platelet effect of clopidogrel is dose-dependent [17]. The 300 mg loading dose of clopidogrel reaches a steady state after 4 to 24 h. If there is no load, it takes 4 to 7 days to reach a steady-state [118]. Allier et al. found that the antiplatelet effect of clopidogrel 600 mg administered for the first time was equivalent to that of long-term 75 mg patients. Clopidogrel 600 mg administered during long-term treatment can further inhibit platelet aggregation [119]. Due to the increase in thrombus load before treatment, the standard loading dose is not enough to achieve effective platelet inhibition for patients with severe symptoms. Therefore, CR will still occur with conventional-dose treatment [120].
4.4. Other Factors
Among other factors, patients’ compliance also directly affects the effectiveness of clopidogrel. Other than that, the antiplatelet effect of clopidogrel is limited in type 2 diabetes patients because this disease is often associated with atherosclerotic disease manifestations; clopidogrel is commonly used in these patients [121]. Diabetes is also a risk factor for reduced antiplatelet effects by clopidogrel [121,122]. There is also a vital relationship found between the level of inflammatory factors and CR caused by abnormal platelet function [123,124,125].
5. Strategies to Overcome CR
5.1. Increase the Dose of Clopidogrel
Increasing the dose can increase the biological effect of clopidogrel and reduce the incidence of CR. Simultaneously, large doses of clopidogrel can reduce patients’ platelet aggregation rate with CR [126]. For PCI patients, the 600 mg loading dose has a faster response than the 300 mg loading dose and has a more substantial platelet inhibitory effect. In this way, the incidence of CR is significantly reduced [127,128]. At the same time, studies have shown that CR or platelet hyperresponsiveness is still common after the administration of clopidogrel 600 mg load, but increasing the dose can reduce the risk of death from cardiovascular disease, myocardial infarction, and stent thrombosis [5]. In patients with stable coronary heart disease, CYP2C19*2 heterozygous carriers taking 225 mg of clopidogrel per day were shown to achieve the same antiplatelet effect with CYP2C19 wild-type patients taking 75 mg of clopidogrel per day. In contrast, CYP2C19*2 homozygous patients cannot achieve the desired antiplatelet effect even if they take the 300 mg clopidogrel maintenance dose [129]. CR in patients treated with PCI between high maintenance dose (150 mg · d −1) than conventional maintenance dose (75 mg · d −1) can more effectively prevent major adverse cardiac events (MACE). In the 1-month follow-up after PCI, the incidence of in-stent thrombosis was lower among the group receiving 150 mg · d −1 as compared to the group receiving 75 mg · d −1 (1.1% and 4.9%, p = 0.03). Simultaneously, cardiovascular events incidence was also significantly lower in the group with higher doses (2.7% and 7.6%, p = 0.03) [130]. However, some studies have shown that high-dose clopidogrel after PCI did not reduce the mortality of cardiovascular events or stent thrombosis incidence than standard doses [131]. Moreover, high-dose clopidogrel may lead to an increased probability of bleeding complications; therefore, the use of high-dose clopidogrel maintenance treatment to avoid treatment resistance requires further research.
5.2. Combined Use of Other Antiplatelet Drugs
Ainetdinova et al. [132] found that the probability of resistance to aspirin, clopidogrel, and the combination of these two drugs were 25.7%, 17.1%, and 5.7%, respectively. Therefore, DAPT with aspirin and clopidogrel was shown to reduce the occurrence of drug resistance. Another potential combination therapy uses the GPIIb/IIIa receptor antagonists (such as abciximab, tirofiban and eptifibatide), which can directly block the final pathway of platelet activation, adhesion, and aggregation. Based on clopidogrel therapy, the combined use of GPIIb/IIIa receptor antagonists can further inhibit platelet aggregation [133,134].
5.3. Replacement of New P2Y12 Receptor Antagonists
The new P2Y12 inhibitors, ticagrelor and prasugrel, will substantially reduce platelet hyperresponsiveness and improve clinical outcomes relative to the regular clopidogrel dose. Most patients who do not respond to clopidogrel can significantly inhibit the platelet aggregation rate after switching to prasugrel [135] because prasugrel can better inhibit ADP-induced platelet aggregation, which is faster and stronger than clopidogrel. The longer-lasting antiplatelet effect of prasugrel can significantly reduce the occurrence of ischemic events [136]. On the other hand, ticagrelor does not require liver metabolism and not affected by CYP2C19 gene polymorphism. It was also shown to significantly reduce mortality related to cardiovascular events, myocardial infarction [137]. A study showed that in STEMI patients undergoing PCI for the first time, a loading dose of 180 mg of ticagrelor was more effective than a loading dose of 600 mg of clopidogrel in reducing microvascular damage [138]. There is also literature mentioning that cangrelor has a powerful platelet inhibitory effect. Its effect may be more significant than clopidogrel. Moreover, its half-life is shorter, does not require liver activation, and is a direct antagonist of P2Y12 [26].
5.4. Other Management of CR
Active control of blood sugar in patients with coronary heart disease can reduce the incidence of CR. Avoiding the simultaneous application of other drugs that require CYP metabolisms, such as statins, calcium channel blockers, and PPI, would ensure a better response to clopidogrel therapy.
In a randomised trial of TROPICAL-ACS [139,140], a targeted de-escalation regimen with early switching from prasugrel to clopidogrel was established as an effective alternative treatment strategy in ACS patients. However, the study found that patient age was the primary determinant of outcome after PCI, [141,142], especially when using P2Y12 receptor inhibitors during and after PCI [143,144]. Therefore, TROPICAL-ACS performed a randomised assessment of the effect of age on reducing the escalation of antiplatelet therapy. Significant variation was found among the younger patients who showed an increased net clinical benefit resulting from reduced bleeding complications. These results suggest that targeted de-escalation may be a safe and attractive alternative therapy concept for all ACS patients after PCI, while a significant bleeding benefit could be achieved in younger patients [145].
6. Conclusions
Clopidogrel plays an essential role in treating coronary heart disease. However, various factors can affect the response to this drug, such as genetic polymorphism, especially CYP2C19 *2 / *3 / *17 in the Asian population. Although there are many methods for detecting platelet resistance, there is a lack of internationally unified standards and laboratory testing systems. There is also a lack of evidence-based medicine for managing CR. We should continue to explore the influencing factors of clopidogrel resistance and the potential strategies to overcome it. Optimising clopidogrel resistance prevention and treatment strategies is vital for identifying and treating high-risk patients as soon as possible.
Author Contributions
Conceptualization, literature review, and writing the manuscript, M.A.A. and B.I.; manuscript revision, N.A.A.D., A.S., M.L.N., M.A.S.A.K. and D.A.M.N.; supervision, B.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hasan M.S., Basri H.B., Hin L.P., Stanslas J. Genetic polymorphisms and drug interactions leading to clopidogrel resistance: Why the Asian population requires special attention. Int. J. Neurosci. 2013;123:143–154. doi: 10.3109/00207454.2012.744308. [DOI] [PubMed] [Google Scholar]
- 2.Amsterdam E.A., Wenger N.K., Brindis R.G., Casey D.E., Jr., Ganiats T.G., Holmes D.R., Jr., Jaffe A.S., Jneid H., Kelly R.F., Kontos M.C. 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:2354–2394. doi: 10.1161/CIR.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 3.Valgimigli M., Bueno H., Byrne R.A., Collet J.-P., Costa F., Jeppsson A., Jüni P., Kastrati A., Kolh P., Mauri L. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur. J. Cardio-Thora. Surg. 2018;53:34–78. doi: 10.1093/ejcts/ezx334. [DOI] [PubMed] [Google Scholar]
- 4.Han Y.-L. De-escalation of anti-platelet therapy in patients with acute coronary syndromes undergoing percutaneous coronary intervention: A narrative review. Chin. Med. J. 2019;132:197–210. doi: 10.1097/CM9.0000000000000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mega J.L., Close S.L., Wiviott S.D., Shen L., Hockett R.D., Brandt J.T., Walker J.R., Antman E.M., Macias W.L., Braunwald E. CLINICAL PERSPECTIVE. Circulation. 2009;119:2553–2560. doi: 10.1161/CIRCULATIONAHA.109.851949. [DOI] [PubMed] [Google Scholar]
- 6.Xie H.-G., Zou J.-J., Hu Z.-Y., Zhang J.-J., Ye F., Chen S.-L. Individual variability in the disposition of and response to clopidogrel: Pharmacogenomics and beyond. Pharmacol. Ther. 2011;129:267–289. doi: 10.1016/j.pharmthera.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Yusuf S., Zhao F., Mehta S.R., Chrolavicius S., Tognoni G., Fox K.K. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N. Engl. J. Med. 2001;345:494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 8.Chen Z., Jiang L., Chen Y. COMMIT (ClOpidogrel and Metoprolol in Myorardial Infarction Trial). Dobavleniye klopidogrelya k aspirinu u 45,852 patsiyentov s ostrym infarktom miokarda: Randomizirovannoyep latsebo-kontroliruyemoyeissledovaniye. Lancet. 2005;366:1607–1621. [Google Scholar]
- 9.Michelson A.D., Bhatt D.L. How I use laboratory monitoring of antiplatelet therapy. Blood J. Am. Soc. Hematol. 2017;130:713–721. doi: 10.1182/blood-2017-03-742338. [DOI] [PubMed] [Google Scholar]
- 10.Gorog D.A., Fuster V. Platelet function tests in clinical cardiology: Unfulfilled expectations. J. Am. Coll. Cardiol. 2013;61:2115–2129. doi: 10.1016/j.jacc.2012.11.080. [DOI] [PubMed] [Google Scholar]
- 11.Bonello L., Tantry U.S., Marcucci R., Blindt R., Angiolillo D.J., Becker R., Bhatt D.L., Cattaneo M., Collet J.P., Cuisset T. Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J. Am. Coll. Cardiol. 2010;56:919–933. doi: 10.1016/j.jacc.2010.04.047. [DOI] [PubMed] [Google Scholar]
- 12.Alnasser S., Huang W., Gore J., Steg P., Eagle K., Anderson F., Fox K., Gurfinkel E., Brieger D., Klein W., et al. Late Consequences of Acute Coronary Syndromes: Global Registry of Acute Coronary Events (GRACE) Follow-up. Am. J. Med. 2015;128:766–775. doi: 10.1016/j.amjmed.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Patti G., Micieli G., Cimminiello C., Bolognese L. The Role of Clopidogrel in 2020: A Reappraisal. Cardiovasc. Ther. 2020:8703627. doi: 10.1155/2020/8703627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gori A.M., Marcucci R., Migliorini A., Valenti R., Moschi G., Paniccia R., Buonamici P., Gensini G.F., Vergara R., Abbate R. Incidence and clinical impact of dual nonresponsiveness to aspirin and clopidogrel in patients with drug-eluting stents. J. Am. Coll. Cardiol. 2008;52:734–739. doi: 10.1016/j.jacc.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 15.Saraf S., Christopoulos C., Salha I.B., Stott D.J., Gorog D.A. Impaired endogenous thrombolysis in acute coronary syndrome patients predicts cardiovascular death and nonfatal myocardial infarction. J. Am. Coll. Cardiol. 2010;55:2107–2115. doi: 10.1016/j.jacc.2010.01.033. [DOI] [PubMed] [Google Scholar]
- 16.Matetzky S., Shenkman B., Guetta V., Shechter M., Beinart R., Goldenberg I., Novikov I., Pres H., Savion N., Varon D. Clopidogrel resistance is associated with increased risk of recurrent atherothrombotic events in patients with acute myocardial infarction. Circulation. 2004;109:3171–3175. doi: 10.1161/01.CIR.0000130846.46168.03. [DOI] [PubMed] [Google Scholar]
- 17.Müller I., Besta F., Schulz C., Massberg S., Schönig A., Gawaz M. Prevalence of clopidogrel non-responders among patients with stable angina pectoris scheduled for elective coronary stent placement. J. Thromb. Haemost. 2003;89:783–787. doi: 10.1055/s-0037-1613462. [DOI] [PubMed] [Google Scholar]
- 18.Ma Q., Chen G.-Z., Zhang Y.-H., Zhang L., Huang L.-A. Clinical outcomes and predictive model of platelet reactivity to clopidogrel after acute ischemic vascular events. Chin. Med. J. 2019;132:1053–1062. doi: 10.1097/CM9.0000000000000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pareed S.A., Vijayaraghavan G., Kartha C., Manoj M. Antiplatelet drug resistance in Indians. Ann. Clin. Cardiol. 2020;2:36. [Google Scholar]
- 20.Namazi S., Kojuri J., Khalili A., Azarpira N. The impact of genetic polymorphisms of P2Y12, CYP3A5 and CYP2C19 on clopidogrel response variability in Iranian patients. Biochem. Pharmacol. 2012;83:903–908. doi: 10.1016/j.bcp.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 21.Sahib H.A., Mohammad B.I., Abdul-Majid B.A. Therapeutic Effectiveness of Clopidogrel-Induced Platelets Inhibition: An Inter-Individual Response Variability among Iraqi Patients. World Heart J. 2016;8:23–28. [Google Scholar]
- 22.Park K.-J., Chung H.-S., Kim S.-R., Kim H.-J., Han J.-Y., Lee S.-Y. Clinical, pharmacokinetic, and pharmacogenetic determinants of clopidogrel resistance in Korean patients with acute coronary syndrome. Korean J. Lab. Med. 2011;31:91–94. doi: 10.3343/kjlm.2011.31.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amin A.M., Chin L.S., Noor D.A.M., Mostafa H., Kader M.A.S.A., Hay Y.K., Ibrahim B. The effect of CYP2C19 genetic polymorphism and non-genetic factors on clopidogrel platelets inhibition in East Asian coronary artery disease patients. Thromb. Res. 2017;158:22–24. doi: 10.1016/j.thromres.2017.07.032. [DOI] [PubMed] [Google Scholar]
- 24.Sakr H.I., Alamri H.S., Almoghairi A.M., Alkhudair A.A., AlMasood A.S. Prevalence and risk factors of clopidogrel non-response among Saudi patients undergoing coronary angiography. Saudi Med. J. 2016;37:166–172. doi: 10.15537/smj.2016.2.14263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tekkeşin A.İ., Kaya A., Çakıllı Y., Türkkan C., Hayıroğlu M.İ., Borklu E.B., Kalenderoğlu K., Gümüşdağ A., Yıldırımtürk Ö., Bozbeyoğlu E. The first six-month clinical outcomes and risk factors associated with high on-treatment platelet reactivity of clopidogrel in patients undergoing coronary interventions. Anatol. J. Cardiol. 2016;16:967–973. doi: 10.14744/AnatolJCardiol.2016.6855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang T.H., Bhatt D.L., Topol E.J. Aspirin and clopidogrel resistance: An emerging clinical entity. Eur. Heart J. 2006;27:647–654. doi: 10.1093/eurheartj/ehi684. [DOI] [PubMed] [Google Scholar]
- 27.Lock E., Saveliev A., Kennedy L. Methanol and dimethyl sulfide removal by pulsed corona part I: Experiment. Plasma Chem. Plasma Process. 2006;26:527–542. doi: 10.1007/s11090-006-9011-9. [DOI] [Google Scholar]
- 28.Bates E.R., Lau W.C., Angiolillo D.J. Clopidogrel–drug interactions. J. Am. Coll. Cardiol. 2011;57:1251–1263. doi: 10.1016/j.jacc.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 29.Howell L.A., Stouffer G.A., Polasek M., Rossi J.S. Review of clopidogrel dose escalation in the current era of potent P2Y12 inhibitors. Expert Rev. Clin. Pharmacol. 2015;8:411–421. doi: 10.1586/17512433.2015.1057571. [DOI] [PubMed] [Google Scholar]
- 30.Ding Z., Kim S., Dorsam R.T., Jin J., Kunapuli S.P. Inactivation of the human P2Y12 receptor by thiol reagents requires interaction with both extracellular cysteine residues, Cys17 and Cys270. Blood J. Am. Soc. Hematol. 2003;101:3908–3914. doi: 10.1182/blood-2002-10-3027. [DOI] [PubMed] [Google Scholar]
- 31.Patrono C., Coller B., Dalen J.E., Gerald G.A.F., Fuster V., Gent M., Hirsh J., Roth G. Platelet-active drugs: The relationships among dose, effectiveness, and side effects. Chest. 2001;119:39S–63S. doi: 10.1378/chest.119.1_suppl.39S. [DOI] [PubMed] [Google Scholar]
- 32.Jiang X.-L., Samant S., Lesko L.J., Schmidt S. Clinical pharmacokinetics and pharmacodynamics of clopidogrel. Clin. Pharmacokinet. 2015;54:147–166. doi: 10.1007/s40262-014-0230-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cuisset T., Morange P.-E., Alessi M.-C. Recent advances in the pharmacogenetics of clopidogrel. Human genetics. 2012;131:653–664. doi: 10.1007/s00439-011-1130-6. [DOI] [PubMed] [Google Scholar]
- 34.Tantry U.S., Hennekens C.H., Zehnder J.L., Gurbel P.A. In: Clopidogrel Resistance and Clopidogrel Treatment Failure. Leung L.L.K., Cutlip D., editors. UpToDate Inc.; Waltham, MA, USA: 2018. [Google Scholar]
- 35.Cay S., Cagirci G., Aydogdu S., Balbay Y., Sen N., Maden O., Demir A.D., Erbay A.R. Safety of clopidogrel in older patients. Drugs Aging. 2011;28:119–129. doi: 10.2165/11586380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 36.Carlquist J.F., Knight S., Horne B.D., Huntinghouse J.A., Rollo J.S., Muhlestein J.B., May H., Anderson J.L. Cardiovascular risk among patients on clopidogrel anti-platelet therapy after placement of drug-eluting stents is modified by genetic variants in both the CYP2C19 and ABCB1 genes. J. Thromb. Haemost. 2013;109:744–754. doi: 10.1160/TH12-05-0336. [DOI] [PubMed] [Google Scholar]
- 37.Park J.J., Park K.W., Kang J., Jeon K.-H., Kang S.-H., Ahn H.S., Han J.-K., Koh J.-S., Lee S.E., Yang H.-M. Genetic determinants of clopidogrel responsiveness in Koreans treated with drug-eluting stents. Int. J. Cardiol. 2013;163:79–86. doi: 10.1016/j.ijcard.2012.09.075. [DOI] [PubMed] [Google Scholar]
- 38.Fontana P., Roffi M., Reny J.-L. Platelet function test use for patients with coronary artery disease in the early 2020s. Med. Clin. Med. 2020;9:194. doi: 10.3390/jcm9010194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wright R.S., Anderson J.L., Adams C.D., Bridges C.R., Casey D.E., Ettinger S.M., Fesmire F.M., Ganiats T.G., Jneid H., Lincoff A.M. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2011;57:e215–e367. doi: 10.1016/j.jacc.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 40.Levine G.N., Bates E.R., Bittl J.A., Brindis R.G., Fihn S.D., Fleisher L.A., Granger C.B., Lange R.A., Mack M.J., Mauri L. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non–ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation. 2016;134:e123–e155. doi: 10.1161/CIR.0000000000000404. [DOI] [PubMed] [Google Scholar]
- 41.Neumann F.-J., Sousa-Uva M., Ahlsson A., Alfonso F., Banning A.P., Benedetto U., Byrne R.A., Collet J.-P., Falk V., Head S.J. 2018 ESC/EACTS Guidelines on myocardial revascularisation. Eur. Heart J. 2019;40:87–165. doi: 10.1093/eurheartj/ehy394. [DOI] [PubMed] [Google Scholar]
- 42.Wang Y., Zhao X., Lin J., Li H., Johnston S.C., Lin Y., Pan Y., Liu L., Wang D., Wang C. Association between CYP2C19 loss-of-function allele status and efficacy of clopidogrel for risk reduction among patients with minor stroke or transient ischemic attack. Jama. 2016;316:70–78. doi: 10.1001/jama.2016.8662. [DOI] [PubMed] [Google Scholar]
- 43.Sarno G., Garg S., Onuma Y., Buszman P., Linke A., Ischinger T., Klauss V., Eberli F., Corti R., Wijns W. The impact of body mass index on the one year outcomes of patients treated by percutaneous coronary intervention with Biolimus-and Sirolimus-eluting stents (from the LEADERS Trial) Am. J. Cardiol. 2010;105:475–479. doi: 10.1016/j.amjcard.2009.09.055. [DOI] [PubMed] [Google Scholar]
- 44.Weisz G., Smilowitz N.R., Kirtane A.J., Rinaldi M.J., Parvataneni R., Xu K., Stuckey T.D., Maehara A., Witzenbichler B., Neumann F.-J. Proton pump inhibitors, platelet reactivity, and cardiovascular outcomes after drug-eluting stents in clopidogrel-treated patients: The ADAPT-DES study. Circ. Cardiovasc. Interv. 2015;8:e001952. doi: 10.1161/CIRCINTERVENTIONS.114.001952. [DOI] [PubMed] [Google Scholar]
- 45.Mizobe M., Hokimoto S., Akasaka T., Arima Y., Kaikita K., Morita K., Miyazaki H., Oniki K., Nakagawa K., Ogawa H. Impact of CYP2C19 polymorphism on clinical outcome following coronary stenting is more important in non-diabetic than diabetic patients. Thromb. Res. 2014;134:72–77. doi: 10.1016/j.thromres.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 46.Elkind M.S., Luna J.M., McClure L.A., Zhang Y., Coffey C.S., Roldan A., Del Brutto O.H., Pretell E.J., Pettigrew L.C., Meyer B.C. C-reactive protein as a prognostic marker after lacunar stroke: Levels of inflammatory markers in the treatment of stroke study. Stroke. 2014;45:707–716. doi: 10.1161/STROKEAHA.113.004562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ibrahim H., Schutt R.C., Hannawi B., DeLao T., Barker C.M., Kleiman N.S. Association of immature platelets with adverse cardiovascular outcomes. J. Am. Coll. Cardiol. 2014;64:2122–2129. doi: 10.1016/j.jacc.2014.06.1210. [DOI] [PubMed] [Google Scholar]
- 48.Chirumamilla A.P., Maehara A., Mintz G.S., Mehran R., Kanwal S., Weisz G., Hassanin A., Hakim D., Guo N., Baber U. High platelet reactivity on clopidogrel therapy correlates with increased coronary atherosclerosis and calcification: A volumetric intravascular ultrasound study. JACC: Cardiovasc. Imaging. 2012;5:540–549. doi: 10.1016/j.jcmg.2011.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rinfret S., Rodés-Cabau J., Bagur R., Déry J.-P., Dorais M., Larose É., Barbeau G., Gleeton O., Nguyen C.-M., Noël B. Telephone contact to improve adherence to dual antiplatelet therapy after drug-eluting stent implantation. Heart. 2013;99:562–569. doi: 10.1136/heartjnl-2012-303004. [DOI] [PubMed] [Google Scholar]
- 50.Zoheir N., Abd Elhamid S., Abulata N., Sobky M.E., Khafagy D., Mostafa A. P2Y12 receptor gene polymorphism and antiplatelet effect of clopidogrel in patients with coronary artery disease after coronary stenting. Blood Coagul. Fibrinolysis. 2013;24:525–531. doi: 10.1097/MBC.0b013e32835e98bf. [DOI] [PubMed] [Google Scholar]
- 51.Xie C., Ding X., Gao J., Wang H., Hang Y., Zhang H., Zhang J., Jiang B., Miao L. The effects of CES1A2 A (− 816) C and CYP2C19 loss-of-function polymorphisms on clopidogrel response variability among Chinese patients with coronary heart disease. Pharmacogenetics Genom. 2014;24:204–210. doi: 10.1097/FPC.0000000000000035. [DOI] [PubMed] [Google Scholar]
- 52.Tang X.-F., Wang J., Zhang J.-H., Meng X.-M., Xu B., Qiao S.-B., Wu Y.-J., Chen J., Wu Y., Chen J.-L. Effect of the CYP2C19* 2 and* 3 genotypes, ABCB1 C3435T and PON1 Q192R alleles on the pharmacodynamics and adverse clinical events of clopidogrel in Chinese people after percutaneous coronary intervention. Eur. J. Clin. Pharmacol. 2013;69:1103–1112. doi: 10.1007/s00228-012-1446-8. [DOI] [PubMed] [Google Scholar]
- 53.Zhuo Z.-L., Xian H.-P., Long Y., Liu C., Sun Y.-Y., Ma Y.-T., Gao H., Zhao J.-Z., Zhao X.-T. Association between CYP2C19 and ABCB1 polymorphisms and clopidogrel resistance in clopidogrel-treated Chinese patients. Anatol. J. Cardiol. 2018;19:123–129. doi: 10.14744/AnatolJCardiol.2017.8097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lau W.C., Gurbel P.A., Watkins P.B., Neer C.J., Hopp A.S., Carville D.G., Guyer K.E., Tait A.R., Bates E.R. Contribution of hepatic cytochrome P450 3A4 metabolic activity to the phenomenon of clopidogrel resistance. Circulation. 2004;109:166–171. doi: 10.1161/01.CIR.0000112378.09325.F9. [DOI] [PubMed] [Google Scholar]
- 55.Mirzaev K., Samsonova K., Potapov P., Andreev D., Grishina E., Ryzhikova K., Sychev D. Genotyping and phenotyping CYP3A4\CYP3A5: No association with antiplatelet effect of clopidogrel. Mjol. Biol. Resp. 2019;46:4195–4199. doi: 10.1007/s11033-019-04871-y. [DOI] [PubMed] [Google Scholar]
- 56.Brandt J.T., Close S., Iturria S., Payne C., Farid N., Ernest C., Lachno D., Salazar D., Winters K. Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J. Thromb. Haemost. 2007;5:2429–2436. doi: 10.1111/j.1538-7836.2007.02775.x. [DOI] [PubMed] [Google Scholar]
- 57.Kazui M., Nishiya Y., Ishizuka T., Hagihara K., Farid N.A., Okazaki O., Ikeda T., Kurihara A. Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab. Dispos. 2010;38:92–99. doi: 10.1124/dmd.109.029132. [DOI] [PubMed] [Google Scholar]
- 58.Kuliczkowski W., Witkowski A., Polonski L., Watala C., Filipiak K., Budaj A., Golanski J., Sitkiewicz D., Pregowski J., Gorski J. Interindividual variability in the response to oral antiplatelet drugs: A position paper of the Working Group on antiplatelet drugs resistance appointed by the Section of Cardiovascular Interventions of the Polish Cardiac Society, endorsed by the Working Group on Thrombosis of the European Society of Cardiology. Eur. Heart J. 2009;30:426–435. doi: 10.1093/eurheartj/ehn562. [DOI] [PubMed] [Google Scholar]
- 59.Simon T., Verstuyft C., Mary-Krause M., Quteineh L., Drouet E., Méneveau N., Steg P.G., Ferrières J., Danchin N., Becquemont L. Genetic determinants of response to clopidogrel and cardiovascular events. N. Engl. J. Med. 2009;360:363–375. doi: 10.1056/NEJMoa0808227. [DOI] [PubMed] [Google Scholar]
- 60.Chan M.Y. Clopidogrel pharmacogenetics of east, south and other Asian populations. Eur. Heart J. Suppl. 2012;14:A41–A42. doi: 10.1093/eurheartj/sur035. [DOI] [Google Scholar]
- 61.Brown S.-A., Pereira N. Pharmacogenomic impact of CYP2C19 variation on clopidogrel therapy in precision cardiovascular medicine. J. Pers. Med. 2018;8:8. doi: 10.3390/jpm8010008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li Z., Dong W., Yang D., Sun L., He X., Hu H., Zhang J., Wang C., Li Y., Zhao M. Body weight, CYP2C19, and P2Y12 receptor polymorphisms relate to clopidogrel resistance in a cohort of Chinese ischemic stroke patients with aspirin intolerance. Eur. J. Clin. Pharmacol. 2020;76:1517–1527. doi: 10.1007/s00228-020-02946-5. [DOI] [PubMed] [Google Scholar]
- 63.Al-Azzam S.I., Alzoubi K.H., Khabour O.F., Nusair M.B., Al-Hadidi H., Awidi A., Saleh A. Factors that contribute to clopidogrel resistance in cardiovascular disease patients: Environmental and genetic approach. Int. J. Clin. Pharmacol. Ther. 2013;51:179–186. doi: 10.5414/CP201784. [DOI] [PubMed] [Google Scholar]
- 64.Lee J.M., Park S., Shin D.-J., Choi D., Shim C.Y., Ko Y.-G., Kim J.-S., Shin E.-S., Chang C.W., Lee J.-E. Relation of genetic polymorphisms in the cytochrome P450 gene with clopidogrel resistance after drug-eluting stent implantation in Koreans. Am. J. Cardiol. 2009;104:46–51. doi: 10.1016/j.amjcard.2009.02.045. [DOI] [PubMed] [Google Scholar]
- 65.Alhazzani A.A., Munisamy M., Karunakaran G. Pharmacogenetics of CYP2C19 genetic polymorphism on clopidogrel response in patients with ischemic stroke from Saudi Arabia. Neurosciences. 2017;22:31–37. doi: 10.17712/nsj.2017.1.20160303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang S., Lai X., Li W., Jing Z., Xiong Z., Xu A., Ruan Y. VASP phosphorylation and genetic polymorphism for clopidogrel resistance in Chinese patients with non-cardioembolic ischemic stroke. Thromb. Res. 2014;134:1272–1277. doi: 10.1016/j.thromres.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 67.Al-Husein B.A., Al-Azzam S.I., Alzoubi K.H., Khabour O.F., Nusair M.B., Alzayadeen S. Investigating the effect of demographics, clinical characteristics, and polymorphism of MDR-1, CYP1A2, CYP3A4, and CYP3A5 on clopidogrel resistance. J. Cardiovasc. Pharmacol. 2018;72:296–302. doi: 10.1097/FJC.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 68.Zhang S., Wang J., Zhang A., Zhang X., You T., Xie D., Yang W., Chen Y., Zhang X., Di C. A SNP involved in alternative splicing of ABCB1 is associated with clopidogrel resistance in coronary heart disease in Chinese population. Aging (Albany NY) 2020;12:25684–25699. doi: 10.18632/aging.104177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen F., Zhang J., Bian C.-X., Zhang J., Xin X.-B., Pan Y.-Y., Zhang X. A Study on the Correlation Between MDR1 Polymorphism and Clopidogrel Resistance in Hui Patients Treated with Percutaneous Coronary Intervention. Int. J. Gen. Med. 2021;14:665–671. doi: 10.2147/IJGM.S293947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Notarangelo F.M., Maglietta G., Bevilacqua P., Cereda M., Merlini P.A., Villani G.Q., Moruzzi P., Patrizi G., Malagoli Tagliazucchi G., Crocamo A. Pharmacogenomic approach to selecting antiplatelet therapy in patients with acute coronary syndromes: The PHARMCLO trial. J. Am. Coll. Cardiol. 2018;71:1869–1877. doi: 10.1016/j.jacc.2018.02.029. [DOI] [PubMed] [Google Scholar]
- 71.Jiang M., You J.H. CYP2C19 LOF and GOF-guided antiplatelet therapy in patients with acute coronary syndrome: A cost-effectiveness analysis. Cardiovasc. Drug Ther. 2017;31:39–49. doi: 10.1007/s10557-016-6705-y. [DOI] [PubMed] [Google Scholar]
- 72.Máchal J., Hlinomaz O. Efficacy of P2Y12 receptor blockers after myocardial infarction and genetic variability of their metabolic pathways. Curr. Vasc. Pharmacol. 2019;17:35–40. doi: 10.2174/1570161116666180206110657. [DOI] [PubMed] [Google Scholar]
- 73.Martin J., Williams A.K., Klein M.D., Sriramoju V.B., Madan S., Rossi J.S., Clarke M., Cicci J.D., Cavallari L.H., Weck K.E. Frequency and clinical outcomes of CYP2C19 genotype-guided escalation and de-escalation of antiplatelet therapy in a real-world clinical setting. Genet. Med. 2020;22:160–169. doi: 10.1038/s41436-019-0611-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen D.-Y., Wang C.-Y., Wen M.-S., Lee T.-H., Chu Y., Hsieh M.-J., Chang S.-H., Lee C.-H., Wang J.-L., Chen C.-C. Paraoxonase-1 is not a major determinant of stent thrombosis in a Taiwanese population. PLoS ONE. 2012;7:e39178. doi: 10.1371/journal.pone.0039178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Scott S., Sangkuhl K., Stein C., Hulot J.S., Mega J., Roden D., Klein T., Sabatine M., Johnson J., Shuldiner A. Clinical Pharmacogenetics Implementation Consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin. Pharmacol. Ther. 2013;94:317–323. doi: 10.1038/clpt.2013.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Desta Z., Zhao X., Shin J.-G., Flockhart D.A. Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin. Pharmacokinet. 2002;41:913–958. doi: 10.2165/00003088-200241120-00002. [DOI] [PubMed] [Google Scholar]
- 77.Hwang S.-J., Jeong Y.-H., Kim I.-S., Koh J.-S., Kang M.-K., Park Y., Kwak C.H., Hwang J.-Y. The cytochrome 2C19* 2 and* 3 alleles attenuate response to clopidogrel similarly in East Asian patients undergoing elective percutaneous coronary intervention. Thromb. Res. 2011;127:23–28. doi: 10.1016/j.thromres.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 78.Sim S.C., Risinger C., Dahl M.L., Aklillu E., Christensen M., Bertilsson L., Ingelman-Sundberg M. A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants. Clin. Pharmacol. Ther. 2006;79:103–113. doi: 10.1016/j.clpt.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 79.Sugimoto K., Uno T., Yamazaki H., Tateishi T. Limited frequency of the CYP2C19* 17 allele and its minor role in a Japanese population. Br. J. Clin. Pharmacol. 2008;65:437–439. doi: 10.1111/j.1365-2125.2007.03057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhong Z., Hou J., Li B., Zhang Q., Liu S., Li C., Liu Z., Yang M., Zhong W., Zhao P. Analysis of CYP2C19 genetic polymorphism in a large ethnic Hakka population in southern China. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017;23:6186–6192. doi: 10.12659/MSM.905337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang T., Zhao T., Bao S., Jia L., Feng J., Yu A., Sun L., Guo X., Li H., Yu L. CYP2C19, PON1, and ABCB1 gene polymorphisms in Han and Uygur populations with coronary artery disease in Northwestern Xinjiang, China, From 2014 Through 2019. Medicine. 2020;99:e20582. doi: 10.1097/MD.0000000000020582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Anichavezhi D., Chakradhara Rao U., Shewade D., Krishnamoorthy R., Adithan C. Distribution of CYP2C19* 17 allele and genotypes in an Indian population. J. Clin. Pharmacol. Ther. 2012;37:313–318. doi: 10.1111/j.1365-2710.2011.01294.x. [DOI] [PubMed] [Google Scholar]
- 83.Dehbozorgi M., Kamalidehghan B., Hosseini I., Dehghanfard Z., Sangtarash M.H., Firoozi M., Ahmadipour F., Meng G.Y., Houshmand M. Prevalence of the CYP2C19* 2 (681 G> A),* 3 (636 G> A) and* 17 (-806 C> T) alleles among an Iranian population of different ethnicities. Mjol. Med. Rep. 2018;17:4195–4202. doi: 10.3892/mmr.2018.8377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sahib H.A., Mohammed B.I., Abdul-Majid B.A. Genetic Polymorphism of CYP2C19 in A sample of Iraqi Population. Int. J. Pharm. Biol. Sci. 2015;5:54–60. [Google Scholar]
- 85.Sviri S., Shpizen S., Leitersdorf E., Levy M., Caraco Y. Phenotypic-genotypic analysis of CYP2C19 in the Jewish Israeli population. Clin. Pharmacol. Ther. 1999;65:275–282. doi: 10.1016/S0009-9236(99)70106-2. [DOI] [PubMed] [Google Scholar]
- 86.Rjoub M., Saleh A., Hakooz N., Imraish A., Jarrar Y., Zihlif M. Allelic frequency of PON1 Q192R, CYP2C19* 2 and CYP2C19* 17 among Jordanian patients taking clopidogrel. Trop. J. Pharm. Res. 2018;17:2275–2280. doi: 10.4314/tjpr.v17i11.24. [DOI] [Google Scholar]
- 87.Kim K.A., Song W.K., Kim K.R., Park J.Y. Assessment of CYP2C19 genetic polymorphisms in a Korean population using a simultaneous multiplex pyrosequencing method to simultaneously detect the CYP2C19* 2, CYP2C19* 3, and CYP2C19* 17 alleles. J. Clin. Pharm. Ther. 2010;35:697–703. doi: 10.1111/j.1365-2710.2009.01069.x. [DOI] [PubMed] [Google Scholar]
- 88.Amin Mostafa A.M., Chin L.S., Mohamed Noor D.A., Amin Mostafa H.M., Ali SK Abdul Kader M., Hay Y.K., Ibrahim B. TCT-841 Integrative Pharmacometabonomics-Pharmacogenetics approach to predict clopidogrel response in Coronary Artery Disease (CAD) patients undergoing Interventional Angiographic Procedure (IAP) J. Am. Coll. Cardiol. 2017;70:B340. doi: 10.1016/j.jacc.2017.09.1049. [DOI] [Google Scholar]
- 89.Riaz S., Din S.M., Tareen M.U., Tariq F., Latif Y., Siddiqi S., Sultan A., Mansoor A. Genetic Polymorphism of CYP2C19 in Pakistani Population. Iran. J. Pharm. Res. IJPR. 2019;18:1097–1102. doi: 10.22037/ijpr.2019.1100644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ayesh B.M., Al-Astal I.R., Yassin M.M. The clinical effects of CYP2C19* 2 allele frequency on Palestinian patients receiving clopidogrel after percutaneous coronary intervention. Int. J. Clin. Pharm. 2019;41:96–103. doi: 10.1007/s11096-018-00782-3. [DOI] [PubMed] [Google Scholar]
- 91.Elewa H., Ali Z.O., Bader L. CYP2C19 Genetic Polymorphism Prevalence in Qataris; Proceedings of the Qatar Foundation Annual Research Conference Proceedings; Doha, Qatar. 19–20 March 2018; Issue 2; HBPD660. [Google Scholar]
- 92.Mirzaev K.B., Zelenskaya E.M., Barbarash O.L., Ganyukov V.I., Apartsin K.A., Saraeva N.O., Nikolaev K.Y., Ryzhikova K.A., Lifshits G.I., Sychev D.A. CYP2C19 polymorphism frequency in Russian patients in Central Russia and Siberia with acute coronary syndrome. Pharm. Pers. Med. 2017;10:107–114. doi: 10.2147/PGPM.S126305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Al-Jenoobi F.I., Alkharfy K.M., Alghamdi A.M., Bagulb K.M., Al-Mohizea A.M., Al-Muhsen S., Halwani R., Parvez M.K., Al-Dosari M.S. CYP2C19 genetic polymorphism in Saudi Arabians. Basic Clin. Pharmacol. Toxicol. 2013;112:50–54. doi: 10.1111/j.1742-7843.2012.00919.x. [DOI] [PubMed] [Google Scholar]
- 94.Sukasem C., Tunthong R., Chamnanphon M., Santon S., Jantararoungtong T., Koomdee N., Prommas S., Puangpetch A., Vathesatogkit P. CYP2C19 polymorphisms in the Thai population and the clinical response to clopidogrel in patients with atherothrombotic-risk factors. Pharmacogenomics Pers. Med. 2013;6:85–91. doi: 10.2147/PGPM.S42332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Arici M., Özhan G. CYP2C9, CYPC19 and CYP2D6 gene profiles and gene susceptibility to drug response and toxicity in Turkish population. Saudi Pharm. J. 2017;25:376–380. doi: 10.1016/j.jsps.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Vu N.P., Nguyen H.T.T., Tran N.T.B., Nguyen T.D., Huynh H.T.T., Nguyen X.T., Nguyen D.T., Nong H.V., Nguyen H.H. CYP2C19 genetic polymorphism in the Vietnamese population. Ann. Hum. Biol. 2019;46:491–497. doi: 10.1080/03014460.2019.1687750. [DOI] [PubMed] [Google Scholar]
- 97.Wang Z.-Y., Chen M., Zhu L.-L., Yu L.-S., Zeng S., Xiang M.-X., Zhou Q. Pharmacokinetic drug interactions with clopidogrel: Updated review and risk management in combination therapy. Ther. Clin. Risk Manag. 2015;11:449–467. doi: 10.2147/TCRM.S80437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.El Rouby N., Lima J.J., Johnson J.A. Proton pump inhibitors: From CYP2C19 pharmacogenetics to precision medicine. Expert Opin. Drug Metab. Toxicol. 2018;14:447–460. doi: 10.1080/17425255.2018.1461835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Grundy S.M., Stone N.J., Bailey A.L., Beam C., Birtcher K.K., Blumenthal R.S., Braun L.T., De Ferranti S., Faiella-Tommasino J., Forman D.E. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019;73:3168–3209. doi: 10.1016/j.jacc.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 100.Tantry U.S., Jeong Y.-H., Gurbel P.A. The Clopidogrel-Statin Interaction–Reopening Pandora’s Box–. Circulation. 2014;78:592–594. doi: 10.1253/circj.CJ-14-0068. [DOI] [PubMed] [Google Scholar]
- 101.Mansour V., Murdico A.T., Fudin J. Do Statins Interfere With Clopidogrel During Platelet Therapy? Pharm. Times. 2019;85 [Google Scholar]
- 102.Lau W.C., Carville D., Bates E.R. Clinical significance of the atorvastatin-clopidogrel drug-drug interaction. Circulation. 2004;110:e66. doi: 10.1161/01.CIR.0000137956.92971.4A. [DOI] [PubMed] [Google Scholar]
- 103.Brophy J.M., Babapulle M.N., Costa V., Rinfret S. A pharmacoepidemiology study of the interaction between atorvastatin and clopidogrel after percutaneous coronary intervention. Am. Heart J. 2006;152:263–269. doi: 10.1016/j.ahj.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 104.Gulec S., Ozdol C., Rahimov U., Atmaca Y., Kumbasar D., Erol C. Myonecrosis after elective percutaneous coronary intervention: Effect of clopidogrel-statin interaction. J. Of Invasive Cardiol. 2005;17:589–593. [PubMed] [Google Scholar]
- 105.Albadr Y., Bohassan A.K., Ming L.C., Khan T.M. An exploratory study investigating the potential drug–drug interactions in internal medicine department, Alahsa, Saudi Arabia. J. Pharm. Health Serv. Res. 2014;5:237–241. doi: 10.1111/jphs.12073. [DOI] [Google Scholar]
- 106.Wenaweser P., Eshtehardi P., Abrecht L., Zwahlen M., Schmidlin K., Windecker S., Meier B., Haeberli A., Hess O.M. A randomised determination of the Effect of Fluvastatin and Atorvastatin on top of dual antiplatelet treatment on platelet aggregation after implantation of coronary drug-eluting stents. J. Thromb. Haemost. 2010;104:554–562. doi: 10.1160/TH09-11-0765. [DOI] [PubMed] [Google Scholar]
- 107.Pelliccia F., Rosano G., Marazzi G., Vitale C., Spoletini I., Franzoni F., Speziale G., Polacco M., Greco C., Gaudio C. Pharmacodynamic effects of atorvastatin versus rosuvastatin in coronary artery disease patients with normal platelet reactivity while on dual antiplatelet therapy—The PEARL randomised cross-over study. Eur. J. Pharmacol. 2014;725:18–22. doi: 10.1016/j.ejphar.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 108.An K., Huang R., Tian S., Guo D., Wang J., Lin H., Wang S. Statins significantly reduce mortality in patients receiving clopidogrel without affecting platelet activation and aggregation: A systematic review and meta-analysis. Lipids Health Dis. 2019;18:121. doi: 10.1186/s12944-019-1053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Nafasi L., Rahmani R., Shafiee A., Salari A., Abdollahi A., Meysamie A. Can a high reloading dose of atorvastatin prior to percutaneous coronary intervention reduce periprocedural myocardial infarction? Curr. Res. Med. Opin. 2014;30:381–386. doi: 10.1185/03007995.2013.834249. [DOI] [PubMed] [Google Scholar]
- 110.Karaźniewicz-Łada M., Rzeźniczak J., Główka F., Gumienna A., Dolatowski F., Słomczyński M., Burchardt P. Influence of statin treatment on pharmacokinetics and pharmacodynamics of clopidogrel and its metabolites in patients after coronary angiography/angioplasty. Biomed. Pharmacother. 2019;116:108991. doi: 10.1016/j.biopha.2019.108991. [DOI] [PubMed] [Google Scholar]
- 111.Katoh M., Nakajima M., Shimada N., Yamazaki H., Yokoi T. Inhibition of human cytochrome P450 enzymes by 1, 4-dihydropyridine calcium antagonists: Prediction of in vivo drug–drug interactions. Eur. J. Clin. Pharmacol. 2000;55:843–852. doi: 10.1007/s002280050706. [DOI] [PubMed] [Google Scholar]
- 112.Siller-Matula J.M., Lang I., Christ G., Jilma B. Calcium-channel blockers reduce the antiplatelet effect of clopidogrel. J. Am. Coll. Cardiol. 2008;52:1557–1563. doi: 10.1016/j.jacc.2008.07.055. [DOI] [PubMed] [Google Scholar]
- 113.Seo K.-D., Kim Y.D., Yoon Y.-W., Kim J.-Y., Lee K.-Y. Antiplatelet effect of clopidogrel can be reduced by calcium-channel blockers. Yonsei Med. J. 2014;55:683–688. doi: 10.3349/ymj.2014.55.3.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Aggarwal S., Loomba R.S., Arora R.R. Effects of concurrent calcium channel blocker on antiplatelet efficacy of clopidogrel therapy: A systematic review. Am. J. Ther. 2016;23:e29–e36. doi: 10.1097/MJT.0000000000000225. [DOI] [PubMed] [Google Scholar]
- 115.Lee C.H., Franchi F., Angiolillo D.J. Clopidogrel drug interactions: A review of the evidence and clinical implications. Expert Opin. Drug Metab. Toxicol. 2020;16:1079–1096. doi: 10.1080/17425255.2020.1814254. [DOI] [PubMed] [Google Scholar]
- 116.Robinson M., Horn J. Clinical pharmacology of proton pump inhibitors. Drugs. 2003;63:2739–2754. doi: 10.2165/00003495-200363240-00004. [DOI] [PubMed] [Google Scholar]
- 117.Bundhun P.K., Teeluck A.R., Bhurtu A., Huang W.-Q. Is the concomitant use of clopidogrel and Proton Pump Inhibitors still associated with increased adverse cardiovascular outcomes following coronary angioplasty?: A systematic review and meta-analysis of recently published studies (2012–2016) BMC Cardiovasc. Disord. 2017;17:3. doi: 10.1186/s12872-016-0453-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Patrono C., Bachmann F., Baigent C., Bode C., De Caterina R., Charbonnier B., Fitzgerald D., Hirsh J., Husted S., Kvasnicka J. Expert consensus document on the use of antiplatelet agents: The Task Force on the Use of Antiplatelet Agents in Patients With Atherosclerotic Cardiovascular Disease of the European Society of Cardiology. Eur. Heart J. 2004;25:166–181. doi: 10.1016/j.ehj.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 119.L’Allier P.L., Ducrocq G., Pranno N., Noble S., Ibrahim R., Grégoire J.C., Azzari F., Nozza A., Berry C., Doucet S. Clopidogrel 600-mg double loading dose achieves stronger platelet inhibition than conventional regimens: Results from the PREPAIR randomized study. J. Am. Coll. Cardiol. 2008;51:1066–1072. doi: 10.1016/j.jacc.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 120.De Miguel A., Ibanez B., Badimón J.J. Clinical implications of clopidogrel resistance. J. Thromb. Haemost. 2008;100:196–203. doi: 10.1160/TH08-01-0049. [DOI] [PubMed] [Google Scholar]
- 121.Angiolillo D.J., Jakubowski J.A., Ferreiro J.L., Tello-Montoliu A., Rollini F., Franchi F., Ueno M., Darlington A., Desai B., Moser B.A. Impaired responsiveness to the platelet P2Y12 receptor antagonist clopidogrel in patients with type 2 diabetes and coronary artery disease. J. Am. Coll. Cardiol. 2014;64:1005–1014. doi: 10.1016/j.jacc.2014.06.1170. [DOI] [PubMed] [Google Scholar]
- 122.Capodanno D., Angiolillo D.J. Antithrombotic Therapy for Atherosclerotic Cardiovascular Disease Risk Mitigation in Patients With Coronary Artery Disease and Diabetes Mellitus. Circulation. 2020;142:2172–2188. doi: 10.1161/CIRCULATIONAHA.120.045465. [DOI] [PubMed] [Google Scholar]
- 123.Gori A., Cesari F., Marcucci R., Giusti B., Paniccia R., Antonucci E., Gensini G., Abbate R. The balance between pro-and anti-inflammatory cytokines is associated with platelet aggregability in acute coronary syndrome patients. Atherosclerosis. 2009;202:255–262. doi: 10.1016/j.atherosclerosis.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 124.Ge H., Zhou Y., Liu X., Nie X., Wang Z., Guo Y., Chen W., Yang Q. Relationship between plasma inflammatory markers and platelet aggregation in patients with clopidogrel resistance after angioplasty. Angiology. 2012;63:62–66. doi: 10.1177/0003319711406432. [DOI] [PubMed] [Google Scholar]
- 125.Cirillo P., Taglialatela V., Pellegrino G., Morello A., Conte S., Di Serafino L., Cimmino G. Effects of colchicine on platelet aggregation in patients on dual antiplatelet therapy with aspirin and clopidogrel. J. Thromb. Thrombolysis. 2020;50:468–472. doi: 10.1007/s11239-020-02121-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Choi H., Ryu J., Seo H., Kang M., Kim E. Is a high maintenance dose of clopidogrel suitable for overcoming clopidogrel resistance in patients? Int. J. Clin. Pharm. 2015;37:758–761. doi: 10.1007/s11096-015-0118-z. [DOI] [PubMed] [Google Scholar]
- 127.Montalescot G., Sideris G., Meuleman C., Bal-dit-Sollier C., Lellouche N., Steg P.G., Slama M., Milleron O., Collet J.-P., Henry P. A randomised comparison of high clopidogrel loading doses in patients with non–ST-segment elevation acute coronary syndromes: The ALBION (Assessment of the Best Loading Dose of Clopidogrel to Blunt Platelet Activation, Inflammation and Ongoing Necrosis) trial. J. Am. Coll. Cardiol. 2006;48:931–938. doi: 10.1016/j.jacc.2006.04.090. [DOI] [PubMed] [Google Scholar]
- 128.Snoep J.D., Hovens M.M., Eikenboom J.C., van der Bom J.G., Jukema J.W., Huisman M.V. Clopidogrel non-responsiveness in patients undergoing percutaneous coronary intervention with stenting: A systematic review and meta-analysis. Am. Heart J. 2007;154:221–231. doi: 10.1016/j.ahj.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 129.Powers W.J., Clarke W.R., Grubb R.L., Videen T.O., Adams H.P., Derdeyn C.P., COSS Investigators F.T. Extracranial-intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: The Carotid Occlusion Surgery Study randomised trial. Jama. 2011;306:1983–1992. doi: 10.1001/jama.2011.1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Liang J., Wang Z., Shi D., Liu Y., Zhao Y., Han H., Li Y., Liu W., Zhang L., Yang L. High clopidogrel dose in patients with chronic kidney disease having clopidogrel resistance after percutaneous coronary intervention. Angiology. 2015;66:319–325. doi: 10.1177/0003319714538804. [DOI] [PubMed] [Google Scholar]
- 131.Stellbaum C., Ayral Y., Morguet A., Schultheiss H.-P., Rauch U. Doubling the clopidogrel dose in patients with reduced responsiveness to the standard dose is associated with a limited effectiveness as evaluated by impedance aggregometry. Cardiovasc. Revascularization Med. 2012;13:159–166. doi: 10.1016/j.carrev.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 132.Aĭnetdinova D., Udovichenko A., Sulimov V. Resistance to antiplatelet drugs in patients with non ST elevation acute coronary syndrome. Kardiologiia. 2008;48:35–39. [PubMed] [Google Scholar]
- 133.Fong A.Y.Y., Ling H.S. Dual Antiplatelet and Glycoprotein Inhibitors in Emergency PCI. In: Watson T., Ong P., Tcheng J., editors. Primary Angioplasty: A Practical Guide. Springer; Gateway East, Singapore: 2018. pp. 99–108. Chapter 8. [PubMed] [Google Scholar]
- 134.Schneider D.J. Anti-platelet therapy: Glycoprotein IIb-IIIa antagonists. Br. J. Clin. Pharmacol. 2011;72:672–682. doi: 10.1111/j.1365-2125.2010.03879.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jernberg T., Payne C.D., Winters K.J., Darstein C., Brandt J.T., Jakubowski J.A., Naganuma H., Siegbahn A., Wallentin L. Prasugrel achieves greater inhibition of platelet aggregation and a lower rate of non-responders compared with clopidogrel in aspirin-treated patients with stable coronary artery disease. Eur. Heart J. 2006;27:1166–1173. doi: 10.1093/eurheartj/ehi877. [DOI] [PubMed] [Google Scholar]
- 136.Shimamatsu J., Sasaki K.-I., Katsuki Y., Kawasaki T., Murasato Y., Ajisaka H., Yokoi H., Tashiro H., Harada A., Hirakawa Y. Prasugrel effectively reduces the platelet reactivity units in patients with genetically metabolic dysfunction of cytochrome P450 2C19 who are treated with long-term dual antiplatelet therapy after undergoing drug-eluting stent implantation. Heart Vessels. 2020;35:312–322. doi: 10.1007/s00380-019-01499-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Huber K., Hamad B., Kirkpatrick P. Ticagrelor. Nar. Rev. Drug Discov. 2011;10:255–256. doi: 10.1038/nrd3418. [DOI] [PubMed] [Google Scholar]
- 138.Park S.-D., Lee M.-J., Baek Y.-S., Kwon S.-W., Shin S.-H., Woo S.-I., Kim D.-H., Kwan J., Park K.-S. Randomised trial to compare a protective effect of Clopidogrel Versus TIcagrelor on coronary Microvascular injury in ST-segment Elevation myocardial infarction (CV-TIME trial) EuroIntervention J. Eur. Colab. Work. Group Interv. Cadriol. Eur. Soc. Cadriol. 2016;12:e964–e971. doi: 10.4244/EIJV12I8A159. [DOI] [PubMed] [Google Scholar]
- 139.Sibbing D., Aradi D., Jacobshagen C. TROPICAL-ACS Investigators. A randomised trial on platelet function-guided de-escalation of antiplatelet treatment in ACS patients undergoing PCI. Rationale and design of the Testing Responsiveness to Platelet Inhibition on Chronic Antiplatelet Treatment for Acute Coronary Syndromes (TROPICAL-ACS) Trial. J. Thromb. Haemost. 2017;117:188–195. doi: 10.1160/TH16-07-0557. [DOI] [PubMed] [Google Scholar]
- 140.Sibbing D., Aradi D., Jacobshagen C., Gross L., Trenk D., Geisler T., Orban M., Hadamitzky M., Merkely B., Kiss R.G. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): A randomised, open-label, multicentre trial. Lancet. 2017;390:1747–1757. doi: 10.1016/S0140-6736(17)32155-4. [DOI] [PubMed] [Google Scholar]
- 141.Boersma E., Pieper K.S., Steyerberg E.W., Wilcox R.G., Chang W.-C., Lee K.L., Akkerhuis K.M., Harrington R.A., Deckers J.W., Armstrong P.W. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation: Results from an international trial of 9461 patients. Circulation. 2000;101:2557–2567. doi: 10.1161/01.CIR.101.22.2557. [DOI] [PubMed] [Google Scholar]
- 142.Eagle K.A., Lim M.J., Dabbous O.H., Pieper K.S., Goldberg R.J., Van de Werf F., Goodman S.G., Granger C.B., Steg P.G., Gore J.M. A validated prediction model for all forms of acute coronary syndrome: Estimating the risk of 6-month postdischarge death in an international registry. Jama. 2004;291:2727–2733. doi: 10.1001/jama.291.22.2727. [DOI] [PubMed] [Google Scholar]
- 143.Larmore C., Effron M.B., Molife C., DeKoven M., Zhu Y., Lu J., Karkare S., Lieu H.D., Lee W.C., Vetrovec G.W. “Real-world” comparison of prasugrel with ticagrelor in patients with acute coronary syndrome treated with percutaneous coronary intervention in the United States. Catherter. Cardiovasc. Interv. 2016;88:535–544. doi: 10.1002/ccd.26279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wiviott S.D., Braunwald E., McCabe C.H., Montalescot G., Ruzyllo W., Gottlieb S., Neumann F.-J., Ardissino D., De Servi S., Murphy S.A. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N. Engl. J. Clin. Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482. [DOI] [PubMed] [Google Scholar]
- 145.Sibbing D., Gross L., Trenk D., Jacobshagen C., Geisler T., Hadamitzky M., Merkely B., Kiss R.G., Komócsi A., Parma R. Age and outcomes following guided de-escalation of antiplatelet treatment in acute coronary syndrome patients undergoing percutaneous coronary intervention: Results from the randomised TROPICAL-ACS trial. Eur. Heart J. 2018;39:2749–2758. doi: 10.1093/eurheartj/ehy332. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.