Abstract
Prostate cancer remains a leading cause of cancer-related morbidity in men. Potentially important regulators of prostate cancer progression are members of the metzincin superfamily of proteases, principally through their regulation of the extracellular matrix. It is therefore timely to review the role of the metzincin superfamily in prostate cancer and its progression to better understand their involvement in this disease. A systematic-like search strategy was conducted. Articles that investigated the roles of members of the metzincin superfamily and their key regulators in prostate cancer were included. The extracted articles were synthesized and data presented in tabular and narrative forms. Two hundred and five studies met the inclusion criteria. Of these, 138 investigated the role of the Matrix Metalloproteinase (MMP) subgroup, 34 the Membrane-Tethered Matrix Metalloproteinase (MT-MMP) subgroup, 22 the A Disintegrin and Metalloproteinase (ADAM) subgroup, 8 the A Disintegrin and Metalloproteinase with Thrombospondin Motifs (ADAMTS) subgroup and 53 the Tissue Inhibitor of Metalloproteinases (TIMP) family of regulators, noting that several studies investigated multiple family members. There was clear evidence that specific members of the metzincin superfamily are involved in prostate cancer progression, which can be either in a positive or negative manner. However, further understanding of their mechanisms of action and how they may be used as prognostic indicators or molecular targets is required.
Keywords: metzincin, prostate cancer, Matrix Metalloproteinase, Tissue Inhibitor of Metalloproteinases, A Disintegrin and Metalloproteinase, A Disintegrin and Metalloproteinase with Thrombospondin Motifs
1. Introduction
Prostate cancer (PrCa) is one of the major causes of cancer-related morbidity in men worldwide [1,2]. The early stages of PrCa are androgen-dependent, but during PrCa progression, the tumors become independent of androgens [1,3]. The detection of PrCa is difficult, with symptoms often not being apparent until metastasis has occurred [1]. The use of the Prostate-Specific Antigen (PSA) test is considered a gold standard, yet remains flawed, with a considerable false-positive rate [1,4]. The survival rates for men diagnosed with PrCa have increased, although the treatment options can have significant side effects [1,2]. An increased understanding of the etiology of this disease provides the potential to develop more specific detection methods and/or alternative treatment modalities.
The metzincin superfamily represents a large group of proteases named after a specialized structural component, a zinc ion-binding methionine turn sequence within their catalytic domain [5,6,7]. The superfamily can be divided into families and subgroups on the basis of other structural and functional features (Figure 1). The Matrixin family consists of the soluble Matrix Metalloproteinase (MMP) and Membrane-Tethered Matrix Metalloproteinase (MT-MMP) subgroups that are principally regulated by the Tissue Inhibitor of Metalloproteinases (TIMP) family, and the Astracin family comprises the BMP1/TLL and Meprin subgroups, whereas the Adamalysin family consists of the A Disintegrin and Metalloproteinase (ADAM) and A Disintegrin and Metalloproteinase with Thrombospondin Motifs (ADAMTS) subgroups [8]. The metzincins are well-known for their roles in development and disease, largely through remodeling of the extracellular matrix (ECM) [9,10,11,12,13].
Figure 1.
Structure of the metzincin superfamily members found in humans and their key regulators. Schematic representation of the structural components of the metzincin subgroups found in humans, grouped by family, along with the Tissue Inhibitor of Metalloproteinases (TIMP) family of regulators.
Members of the metzincin superfamily have been increasingly implicated in cancer progression, including a key role in the metastatic process via their ability to remodel the ECM of tumors [13,14,15]. However, the exact role varies, with some being tumor-promoting, others having an antitumorigenic function and others seemingly not playing a role [13,14,16,17,18]. The metzincin superfamily is therefore of interest as a potential source of biomarkers and/or targets for therapeutic interventions, although the results of the clinical trials to date have been discouraging [19]. However, given the pressing need for both biomarkers and therapeutics in PrCa, it is timely to conduct this systematic-like review in order to synthesize the role of the metzincin superfamily in this disease.
2. Results
Extensive database searching was undertaken to identify studies that investigated the role of metzincin superfamily members in PrCa progression, as described in Materials and Methods. This identified 205 articles that are presented in five tables, each covering a specific subgroup of the metzincin superfamily or their regulators—specifically, the Matrixin family subgroups MMPs and MT-MMPs, the TIMPs and the Adamalysin family subgroups ADAMs and ADAMTSs. A number of studies involved more than one of these groups and so are included in more than one table. No articles on the BMP/TLL or Meprin subgroups within the Astracin family were identified.
2.1. Soluble Matrix Metalloproteinases (MMPs)
The most extensively studied metzincin superfamily subgroup are the soluble MMPs, with 138 articles included (Table 1). Generally, MMPs have been demonstrated to act in a protumorigenic manner—particularly, MMP-2, MMP-7 and MMP-9, which have been the most widely studied of this subgroup.
Table 1.
Studies on soluble Matrix Metalloproteinases (MMPs) in prostate cancer (PrCa).
| Authors | Year | MMP | PrCa Platform | Role |
|---|---|---|---|---|
| Aalinkeel et al. [20] | 2004 | MMP-9 * | Yes—Prostate cell lines | MMP-9 expression increased in metastatic PrCa lines. Enforced expression of MMP-9 increased invasiveness, whereas ablation of expression decreased invasiveness. |
| Aalinkeel et al. [21] | 2011 | MMP-9 | Yes—Prostate cell lines | Enforced expression of MMP-9 increased invasiveness, whereas ablation decreased invasiveness, with no change in migration. |
| Adabi et al. [22] | 2015 | MMP-2 | Yes—Prostate samples | MMP-2 polymorphism not associated with PrCa risk or degree of metastasis. |
| Albayrak et al. [23] | 2007 | MMP-1 | Yes—Prostate samples | MMP-1 polymorphism not associated with PrCa risk. |
| Assikis et al. [24] | 2004 | MMP-9 | Yes—Prostate samples | MMP-9 expression low in PrCa. |
| Babichenko et al. [25] | 2014 | MMP-9* | Yes—Prostate samples | MMP-9 expression negatively correlated with Gleason score and proliferation index. |
| Baspinar et al. [26] | 2017 | MMP-9 | Yes—Prostate samples | MMP-9 expression increased in samples with high metastatic potential scores and staging. |
| Bekes et al. [27] | 2011 | MMP-9 | Yes—Prostate cell lines | Increased MMP-9-positive neutrophils in highly disseminated PrCa correlated with angiogenic potential. |
| Białkowska et al. [28] | 2018 | MMP-1, 2, 7 and 13 | Yes—Prostate samples | Polymorphism in MMP-7 (but not MMP-1, 2 and 13) correlated with increased PrCa risk. |
| Bok et al. [29] | 2003 | MMP-2, 3, 7& 9 | Yes-Mice | Active forms of MMP-2 and 9 present in late stage PrCa in mouse model, but MMP-3 not expressed and MMP-7 only focal expression. |
| Bonaldi et al. [30] | 2015 | MMP-13 | Yes—Prostate samples | MMP-13 expression not changed in PrCa compared to healthy controls. |
| Boxler et al. [31] | 2010 | MMP-2, 3, 7, 9, 13 and 19 | Yes—Prostate samples | Expression of MMP-9 (but not MMP-2, 3, 7, 13 or 19) negatively correlated with overall, recurrence-free and disease-specific survival. |
| Brehmer et al. [32] | 2003 | MMP-2 and 9 * | Yes—Prostate samples | MMP-2 expressed significantly in more advanced PrCa tumors, and MMP-9 significantly less. |
| Bruni-Cardoso et al. [33] | 2010 | MMP-9 | Yes—Mice and rats | MMP-9 expression in osteoclasts contributed to PrCa tumor growth in the bone through increased angiogenesis. |
| Cardillo et al. [34] | 2006 | MMP-1, 7 and 9 * | Yes—Prostate samples | Expression of MMPs significantly increased in the epithelium than the stroma, and of MMP-7 and 9 (but not MMP-1) with Gleason score. |
| Carozzi et al. [35] | 2016 | MMP-2 and 9 | Yes—Prostate samples | Expression of MMP-2 and 9 negatively correlated with survival. |
| Castellana et al. [36] | 2009 | MMP-2, 3, 7, 9 and 13 * | Yes—Prostate cell lines | Tumor-derived microvesicles induced MMP-9 expression that correlated with increased migration and resistance to apoptosis. |
| Coulson-Thomas et al. [37] | 2010 | MMP-1 and 9 * | Yes—Prostate cell lines | MMP-1 and 9 differentially expressed following co-culture with metastatic PrCa. |
| Daja et al. [38] | 2003 | MMP-1 and 13 * | Yes—Prostate cell lines | MMP-1 and 13 expression higher in more aggressive sublines |
| De Cicco et al. [39] | 2008 | MMP-2 and 9 * | Yes—Prostate samples | Low serum MMP-2 (but not MMP-9) associated with increased risk of disease progression. |
| Di Carlo et al. [40] | 2010 | MMP-2 and 9 | Yes—Prostate samples/urine | Active MMP-9 in urine (but not MMP-2) decreased in PrCa versus benign prostatic hyperplasia. |
| Dong et al. [41] | 2001 | MMP-9 | Yes—Prostate cell lines and mice | Pro-MMP-9 expression levels enhanced during PrCa co-culture, including in bone implants in mice. |
| dos Reis et al. [42] | 2009 | MMP-1, 2, 7 and 9 | Yes—Prostate samples | Polymorphisms in MMP-1, 2 and 9 (but not MMP-7) lower in PrCa versus controls. |
| dos Reis et al. [43] | 2010 | MMP-2 | Yes—Prostate samples | Polymorphism in MMP-2 more frequent in PrCa, including in higher Gleason scores, compared to those in MMP-9 that were associated with lower scores. |
| dos Reis et al. [44] | 2008 | MMP-1, 2, 7 and 9 | Yes—Prostate samples | Polymorphisms in MMP-1, 2 and 9 (but not MMP-7) lower in PrCa versus controls. |
| Eiro et al. [45] | 2017 | MMP-2, 9 and 11 | Yes—Prostate samples | MMP-2 expression lower and MMP-11 higher in cancer-associated fibroblasts in PrCa. |
| El-Chaer et al. [46] | 2020 | MMP-1 | Yes—Prostate samples/Serum | Genotype adjusted MMP-1 expression higher in PrCa compared to benign prostatic hyperplasia. |
| Eryilmaz et al. [47] | 2019 | MMP-2 and 9 | Yes—Prostate samples | MMP-2 expression associated with increased PrCa risk. |
| Escaff et al. [48] | 2010 | MMP-1, 2, 7, 9, 11 and 13 * | Yes—Prostate samples | Increased expression of MMP-11 and 13 associated with significant probability of biochemical recurrence. |
| Escaff et al. [49] | 2011 | MMP-1, 2, 7, 9, 11 and 13 * | Yes—Prostate samples | Expression of MMP-2 in fibroblasts and MMP-9 in mononuclear inflammatory cells associated with PrCa. |
| Escaff et al. [50] | 2011 | MMP-1, 2, 7, 9, 11 and 13 * | Yes—Prostate samples | Expression of MMP-9 and 13 in fibroblasts. MMP-13 in tumor cells associated with biological recurrence. |
| Favaro et al. [51] | 2012 | MMP-2 | Yes—Prostate samples | MMP-2 expression increased in periacinar retraction during PrCa. |
| Fernandez-Gomez et al. [52] | 2011 | MMP-1, 2, 7, 9, 11 and 13 * | Yes—prostate samples | Expression of MMP-2 negatively associated with high tumor grade, MMP-7 expression negatively associated with Prostate-Specific Antigen (PSA), whereas MMP-13 expression positively associated with PSA. |
| Festuccia et al. [53] | 1996 | MMP-2 and 9 | Yes—Prostate samples and prostate cell lines | MMP-2 and 9 highly expressed in PrCa. High MMP-9 expression and activity relative to MMP-2 associated with high Gleason grade. |
| Gohji et al. [54] | 1998 | MMP-2 | Yes—Prostate samples/Serum | Serum MMP-2 higher in patients with PrCa and higher in those with metastasis. |
| Gravina et al. [55] | 2013 | MMP-2 and 9 * | Yes—Prostate cell lines | MMP-2 consistently secreted by PrCa, whereas MMP-9 secretion sporadic. |
| Grindel et al. [56] | 2014 | MMP-7 | Yes—Prostate cell lines | MMP-7 expression associated with increased invasiveness. |
| Gupta et al. [57] | 2013 | MMP-9 | Yes—Prostate cell lines | MMP-9 knockdown resulted in increased adhesion and cell spreading. |
| Hamdy et al. [58] | 1994 | MMP-9 | Yes—Prostate samples | MMP-9 activity increased in malignant PrCa tissue compared to benign. |
| Hanqing et al. [59] | 2003 | MMP-2 and 9 | Yes—Prostate samples | MMP-2 and 9 expression higher in PrCa tissue. |
| Hashimoto et al. [60] | 1998 | MMP-7 (matrilysin) * | Yes—Prostate samples | MMP-7 levels and MMP-7/TIMP-1 ratio higher in advanced PrCa, and correlated with pathological stage, lymph node metastasis, histological differentiation, as well as vascular and lymphatic invasion. |
| Hetzl et al. [61] | 2012 | MMP-2 and 9 | Yes—Prostate samples | MMP-2 and 9 expression increased in PrCa versus controls. |
| Incorvaia et al. [62] | 2007 | MMP-2 and 9 | Yes—Prostate samples | Circulating MMP-9 (but not MMP-2) showed significant correlation with PSA. |
| Jaboin et al. [63] | 2011 | MMP-7 (matrilysin) | Yes—Prostate samples | MMP-7 polymorphism associated with PrCa recurrence. |
| Jędroszka et al. [64] | 2017 | MMP-2, 3 and 9 | Yes—Prostate samples | Expression of MMP-2, 3 and 9 increased in Gleason grade 8 and 9 tissues. |
| Jennbacken et al. [65] | 2006 | MMP-2 and 9 * | Yes—Prostate cell lines | MMP-9 expression increased in PrCa, but MMP-2 expression not detected. |
| Jung et al. [66] | 1998 | MMP * | Yes—Prostate samples | MMP levels decreased but MMP/TIMP ratio increased in PrCa. |
| Jung et al. [67] | 2003 | MMP-2 and 9 | Yes—Rats | Expression of MMP-9 (but not MMP-2) increased in advanced PrCa. |
| Jung et al. [68] | 1997 | MMP-1 and 3 * | Yes—Prostate samples | MMP-3 (but not MMP-1) highly expressed in PrCa patients with metastasis. |
| Jurasz et al. [69] | 2003 | MMP-2 | Yes—Prostate samples/Serum | Platelet MMP-2 levels increased in metastatic versus localized PrCa. |
| Kalantari et al. [70] | 2019 | MMP-13 | Yes—Prostate samples | MMP-13 highly expressed in PrCa tissue and associated with Gleason score. |
| Kaminski et al. [71] | 2006 | MMP-1 | Yes—Prostate cell lines | PrCa conditioned medium increased MMP-1 expression in fibroblasts. |
| Kanoh et al. [72] | 2002 | MMP-2 | Yes—Prostate samples/Serum | Serum MMP-2 increased in PrCa and bone metastasis, but not correlated with PSA. |
| Knox et al. [73] | 1996 | MMP-7 (matrilysin) | Yes—Prostate samples | MMP-7 expressed in PrCa. |
| Koshida et al. [74] | 2004 | MMP-1 and 2 | Yes—Prostate cell lines | MMP-1 and 2 expressed in PrCa, but only MMP-2 expression increased following implantation. |
| Kuniyasu et al. [75] | 2000 | MMP-2 and 9 | Yes—Prostate samples | Expression of MMP-2 and 9 in high grade tumors and associated with Gleason score. |
| Kuniyasu et al. [76] | 2003 | MMP-2 and 9 | Yes—Prostate samples | Increased MMP/E-cadherin ratio correlated with increased stage. |
| Larsson et al. [77] | 2020 | MMP-9 | Yes—Prostate samples, Prostate cell lines and mice | High MMP-9 expression associated with poor prognosis. |
| Latil et al. [78] | 2003 | MMP-9 * | Yes—Patient samples | MMP-9 expressed in PrCa tissue. |
| Lein et al. [79] | 1999 | MMP-2 and 3 * | Yes—Prostate samples/Serum | Plasma MMP-3 (but not MMP-2) increased in PrCa. |
| Leshner et al. [80] | 2016 | MMP-2 and 9 * | Yes—Prostate samples | MMP-9 gene repositioned in PrCa and MMP-2 in both PrCa and hyperplasia. |
| Liao et al. [81] | 2018 | MMP-1 | Yes—Prostate samples/Serum | MMP-1 promotor polymorphisms not a risk factor for PrCa. |
| Lichtinghagen et al. [82] | 2002 | MMP-2 and 9 * | Yes—Prostate samples | Expression of MMP-2 gene decreased and MMP-9 unchanged, but MMP-9 protein higher in cancerous tissue, with no change in MMP-2 protein. |
| Lichtinghagen et al. [83] | 2003 | MMP-1, 2, 7, 9 and 11 * | Yes—Prostate samples | Expression of MMP-2 and 11 decreased, and MMP-9 increased in PrCa, but no correlations with grade, stage or PSA. |
| Littlepage et al. [84] | 2010 | MMP-2, 7, 9 and 13 * | Yes—Mice | Expression of MMP-2, 7 and 9 increased with PrCa progression. MMP-2 knockout mice showed reduced tumor burden, prolonged survival, decreased lung metastasis, and decreased blood vessel density. Knockout of MMP-7 or MMP-9 did not impact tumor growth or survival but affected blood vessel formation. |
| Liu et al. [85] | 2017 | MMP-9 | Yes—Prostate samples and prostate cell lines | MMP-9 expression increased in metastatic cancer. |
| Lokeshwar et al. [86] | 1993 | MMP-2 and 9 * | Yes—Prostate samples/Serum | MMP-2 and 9 secretion, including of the active form of MMP-2, increased in neoplastic tissue. |
| London et al. [87] | 2003 | MMP-9 | Yes—Prostate cell lines | Ablation of MMP-9 caused decreased tumor invasion, migration, and growth. |
| Lynch et al. [88] | 2005 | MMP-7 (matrilysin) | Yes—Rat | MMP-7 expression increased at tumor/bone interface. MMP-7 knockout mice showed reduced tumor-induced osteolysis. |
| Marin-Aguilera et al. [89] | 2015 | MMP-9 | Yes—Prostate samples | MMP-9 upregulated in PrCa and correlated with poorer overall survival. |
| Maruta et al. [90] | 2010 | MMP-10 | Yes—Prostate samples | MMP-10 expression correlated with stage, cell renewal and vascular invasion. |
| Medina-González et al. [91] | 2020 | MMP-2, 9, 11 and 13 * | Yes—Prostate samples | Expression of MMP-2 and 9 increased (but MMP-11 and 13 unchanged) in PrCa. |
| Miyake et al. [92] | 2010 | MMP-2 and 9 | Yes—Prostate samples | MMP-2 and 9 expression correlated with stage, recurrence, proliferation, and invasion. |
| Montironi et al. [93] | 1995 | MMP-2 (type IV collagenase) * |
Yes—Prostate samples | MMP-2 protein expression identified in cells in contact with the stroma |
| Montironi et al. [94] | 1996 | MMP-2 (type IV collagenase) |
Yes—Prostate samples | MMP-2 expression correlated with progression. |
| Morgia et al. [95] | 2005 | MMP-2, 3 and 13 * | Yes—Prostate samples | Plasma levels of MMP-2 and 9 (but not MMP-13) increased in metastatic PrCa. |
| Moses et al. [96] | 1998 | MMP-2 and 9 | Yes—Prostate samples/Urine | Active MMP-2 and 9 in urine were independent predictor of organ-confined PrCa. |
| Muñoz et al. [97] | 2017 | MMP-2 and 9 | Yes—Prostate samples/Urine | No difference in urine levels of MMP-2 or MMP-9 species in PrCa. |
| Nabha et al. [98] | 2006 | MMP-9 | Yes—Mice | MMP-9 knockout resulted in no difference in tumor incidence, growth or microvascularity. |
| Nagle et al. [99] | 1994 | MMP-7 (matrilysin) | Yes—Prostate samples | MMP-7 expression in PrCa located in dilated ducts when inflamed and atrophic glands. |
| Nalla et al. [100] | 2010 | MMP-9 | Yes—Prostate cell lines | Ablation of MMP-9 reduced migration and invasion and induced apoptosis. |
| Neuhaus et al. [101] | 2017 | MMP-3, 7, 13 and 20 * | Yes—Prostate samples | Decreased MMP-3/TIMP ratio in PrCa, but other MMPs not altered. |
| Oguić et al. [102] | 2014 | MMP-2 and 9 | Yes—Prostate samples | Higher MMP-2 and 9 expression in positive surgical margins. MMP-9 expression associated with biochemical recurrence. |
| Ok Atılgan et al. [103] | 2020 | MMP-9 | Yes—Patient samples | MMP-9 expression positively associated with WHO grade, tumor stage, extracapsular extension, positive surgical margin lymphovascular, perineural invasion and decreased disease-free survival. |
| Ouyang et al. [104] | 2001 | MMP-7 (matrilysin) | Yes—Rats | MMP-7 expressed in premalignant and malignant tissue. |
| Ozden et al. [105] | 2013 | MMP-1 and 9 * | Yes—Prostate samples | MMP-1 expression in tumors correlated with higher grades and Gleason scores. MMP-9 expression in normal glands correlated with low PSA and Gleason scores. |
| Pajouh et al. [106] | 1991 | MMP-7 (matrilysin) | Yes—Prostate cell lines | MMP-7 expressed in invasive metastatic primary human PrCa. |
| Pang et al. [107] | 2004 | MMP-13 | Yes—Prostate samples and prostate cell lines | MMP-13 expressed in PrCa. |
| Pettaway et al. [108] | 2008 | MMP-2 and 9 | Yes—Prostate samples | MMP-2 and MMP-9/E-cadherin ratio increased at tumor edge and correlated with disease, biochemical recurrence, and pathological stage. |
| Pouyanfar et al. [109] | 2016 | MMP-9 | Yes—Prostate samples | MMP-9 expression higher in PrCa patients related to Gleason score and age, but not PSA, metastasis, or survival. |
| Powell et al. [110] | 1993 | MMP-7 (matrilysin) | Yes—Prostate cell lines and mice | Enforced MMP-7 expression led to increased invasion. |
| Prior et al. [111] | 2010 | MMP-2 | Yes—Prostate samples | Increased MMP-2 levels in urine/blood associated with PrCa progression. |
| Reis et al. [112] | 2012 | MMP-2 * | Yes—Prostate samples | MMP-2 expression reduced in PrCa samples but increased in higher grades. |
| Reis et al. [113] | 2015 | MMP-2&9 * | Yes—Prostate samples | MMP-2 and 9 expressed in most PrCa but no prognostic value. |
| Reis et al. [114] | 2011 | MMP-9 * | Yes—Prostate samples | Higher MMP-9 expression associated with increased PSA and recurrence, but not Gleason score. |
| Riddick et al. [115] | 2005 | MMP-2, 10, 23 and 25 * | Yes—Prostate samples | Increased expression of MMP-10 and 25, but MMP-2 and 23 decreased in PrCa. |
| Ross et al. [116] | 2003 | MMP-2 * | Yes—Prostate samples | MMP-2 expressed in more advanced PrCa and correlated with prognostic variables. |
| Sakai et al. [117] | 2005 | MMP-2 and 9 | Yes—Prostate samples | Increased expression of MMP-2 and 9 in peripheral zone cancers compared to transitional zone. |
| San Francisco et al. [118] | 2004 | MMP-9 | Yes—Prostate cell lines | MMP-9 expression not changed in PrCa. |
| Sauer et al. [119] | 2004 | MMP-2 and 9 | Yes—Prostate samples/Serum | MMP-9 serum levels increased in PrCa patients and correlated with grade, but tissue MMP-9 activity not related to stage or grade. MMP-2 activity correlated with disease progression. |
| Schäfer et al. [120] | 2012 | MMP-9 | Yes—Prostate cell lines and mice | Enforced MMP-9 expression enhanced tumor regression and impacted metastasis. |
| Schveigert et al. [121] | 2013 | MMP-9 | Yes—Prostate samples | MMP-9 polymorphism and increased expression associated with PrCa, with polymorphism related to pathological stage and prognostic group, and expression with survival. |
| Sehgal et al. [122] | 1998 | MMP-9 | Yes—Mice | Ablation of MMP-9 reduced metastatic potential. |
| Sehgal et al. [123] | 2003 | MMP-1, 2 and 9 * | Yes—Prostate cell lines | Expression of MMP-1 (but not MMP-2 or MMP-9) decreased in more metastatic PrCa. |
| Serretta et al. [124] | 2018 | MMP-3 | Yes—Prostate samples | MMP-3 expression not associated with Gleason score 4 and 5. |
| Sfar et al. [125] | 2007 | MMP-9 | Yes—Prostate samples | MMP-9 polymorphism associated with increased risk of advanced PrCa. |
| Sfar et al. [126] | 2009 | MMP-9 | Yes—Prostate samples | MMP-9 polymorphism associated with increased risk of developing PrCa. |
| Shah et al. [127] | 2016 | MMP-9 | Yes—Prostate cell lines | Increased MMP-9 expression in PrCa cells co-cultured with dermal lymphatic microvascular endothelial cells. |
| Shajarehpoor Salavati et al. [128] | 2017 | MMP-2 | Yes—Prostate sample | MMP-2 polymorphism not associated with PrCa risk. |
| Shi et al. [129] | 2017 | MMP-9 | Yes—Prostate samples/Urine | MMP-9 detected in urine of PrCa patients. |
| Silva et al. [130] | 2015 | MMP-2 | Yes—Prostate samples | Increased MMP-2 expression in reactive stroma. |
| Srivastava et al. [131] | 2012 | MMP-2 * | Yes—Prostate samples | MMP-2 polymorphism associated with PrCa risk but not staging. |
| Stearns et al. [132] | 1996 | MMP-2 | Yes—Prostate samples and prostate cell lines | MMP-2 expression increased in higher PrCa grades. |
| Stearns et al. [133] | 1996 | MMP-2 | Yes—Prostate samples | MMP-2a expressed in glandular epithelial cells and increased in PrCa samples with high Gleason score. |
| Still et al. [134] | 2000 | MMP-2 * | Yes—Prostate samples | MMP-2 localized to malignant cells, with increased MMP-2/TIMP-2 ratio associated with high grade and stage. |
| Szarvas et al. [135] | 2018 | MMP-7 (matrilysin) | Yes—Prostate samples | Serum MMP-7 level significantly higher in docetaxel-resistant PrCa and associated with poor survival. |
| Trudel et al. [136] | 2008 | MMP-2 * | Yes—Prostate samples | MMP-2 expression in basal epithelial cells and stromal cells associated with shorter disease-free survival. |
| Trudel et al. [137] | 2003 | MMP-2 | Yes—Prostate samples | MMP-2 expression in malignant cells associated with disease-free survival. |
| Trudel et al. [138] | 2010 | MMP-9 | Yes—Prostate samples | MMP-9 expression correlated with Gleason score but not disease-free survival. |
| Tsuchiya et al. [139] | 2009 | MMP-1 | Yes—Prostate samples | MMP-1 promotor polymorphisms (and increased expression) associated with pathological stage but not PrCa susceptibility or progression. |
| Upadhyay et al. [140] | 1999 | MMP-2 * | Yes—Prostate samples | MMP-2 localization altered in PrCa. |
| Vallbo et al. [141] | 2005 | MMP-2 and 9 | Yes-Rat | MMP-2 (but not MMP-9) expressed in malignant cells. |
| Wang et al. [142] | 2014 | MMP-1 | Yes—Prostate samples | MMP-1 expression significantly increased in PrCa and associated with higher Gleason score, metastasis and pathological stage, as well as reduced overall and recurrence-free survival. |
| Wiesner C [143] | 2007 | MMP-9 | Yes—Prostate cell lines and mice | Increased MMP-9 activity when PrCa cells interact with bone. |
| Wilson et al. [144] | 2002 | MMP-2 and 9 | Yes—Prostate samples and prostate cell lines | Epithelial cells secreted little MMP-2 or MMP-9, whereas pro-MMP-2 (but not MMP-9) secreted by stromal cells. |
| Wilson et al. [145] | 1993 | MMP | Yes—Prostate cell lines and mice | MMP isoforms differentially altered in PrCa. |
| Wood et al. [146] | 1997 | MMP-2 and 9 * | Yes—Prostate samples | Increased expression of MMP-2&9 in high grade samples. |
| Xie et al. [147] | 2016 | MMP-7 (matrilysin) | Yes-Mice | MMP-7 expression elevated in PrCa. |
| Xu et al. [148] | 2010 | MMP-9 | Yes—Prostate cell lines and mice | Ablation of MMP-9 led to decreased cell invasion. |
| Yaykaşli et al. [149] | 2014 | MMP-2 * | Yes—Prostate samples | MMP-2 polymorphisms increased in PrCa patients. |
| Zellweger et al. [150] | 2005 | MMP-2 | Yes—Prostate samples | MMP-2 expressed in PrCa, but not altered across different types. |
| Zhang et al. [151] | 2002 | MMP-2 and 7 * | Yes—Prostate samples and prostate cell lines | MMP-2 expressed in stromal cells and MMP-7 expressed in epithelial cells. Differential expression between cell lines. |
| Zhang et al. [152] | 2004 | MMP-2 and 9 | Yes—Prostate samples and Prostate cell lines | Expression of MMP-9 (but not MMP-2) increased in malignant samples. |
| Zhang et al. [153] | 2008 | MMP-2 and 9 | Yes—Prostate samples and prostate cell lines | Expression of MMP-2 and 9 increased in PrCa. |
| Zhang et al. [154] | 2018 | MMP-1 | Yes—Prostate cell lines | Expression of MMP-1 increased in more metastatic lines. Ablation of MMP-1 decreased invasion and migration. |
| Zhao et al. [155] | 2003 | MMP-9 and 26 | Yes—Prostate samples and prostate cell lines | Expression of MMP-26 (but not MMP-9) increased in PrCa. Blocking of either reduced invasion. |
| Zhong et al. [156] | 2008 | MMP-1, 2 and 9 | Yes—Prostate samples | MMP-1, 2 and 9 expression significantly higher in PrCa. MMP-2 expression correlated with TMN grade and Gleason score. |
| Zhu et al. [157] | 1999 | MMP-2 and 9 | Yes—Prostate cell lines | MMP-2 expression enhanced when PrCa co-cultured. |
* Included in at least one other table.
The strongest evidence for protumorigenicity relates to MMP-9. Multiple publications have identified an increased expression in PrCa [59,61,78,83,109,113,129,153,156], including positive associations with more advanced PrCa [67,75,84,103] and, specifically, with higher grade/stage [26,34,53,92,138] and enhanced metastatic properties [20,21,58,65,85,146], as well as increased recurrence [92,102] and poorer prognosis [35,77,89]. Others show no association [24,47,48,52,118], and a small number show negative associations [25,31,40] with PrCa progression, indicating that MMP-9 is not universally important. However, functional studies serve to confirm its significant role, particularly in PrCa spreading, with MMP-9 ablation repeatedly shown to decrease its invasion and/or migration [57,87,100,148]. Interestingly, no differences in tumorigenesis were observed in a mouse MMP-9 knockout model [98], suggesting that expression within the tumor is important for this enzyme.
Many studies similarly showed an increased expression of MMP-2 in PrCa [49,53,59,61,62,91,150,153,156]. This also generally correlated with more advanced PrCa [32,75,84,92,94,119,132,133,141,146], including metastatic disease [54,69], as well as increased risk [47] and decreased survival [35,52,136]. In contrast, other publications showed no association [67,79,97] or a negative association [52,82,83,112,115]. In this case, a mouse MMP-2 knockout model exhibited reduced tumor burden [84], suggesting expression within the tumor is not necessarily essential for MMP-2.
Several publications have also demonstrated increased MMP-7 in PrCa [34,56,73,84,99,104,147,151], including correlations with metastasis [106] and chemoresistance [135]. However, others have identified no change in expression in PrCa [42] or, indeed, a negative correlation with disease [52], including when examining the levels of the active form of this enzyme [29,101]. For MMP-7, gene polymorphisms may be important in terms of the risk of the disease [28] and recurrence [63], while the relative levels of the inhibitors may also influence the impact of MMP-7 on PrCa progression [60]. An enforced expression of MMP-7 in PrCa cells has been shown to mediate an increased invasion [110], while a mouse MMP-7 knockout model exhibited reduced tumor-induced osteolysis [88], indicating the source of this enzyme may not be critical.
For other MMPs, there was some limited evidence that they also may play a cancer-promoting role. This includes the association of expression with PrCa for MMP-3 [64,68,79,101], MMP-10 [90,115], MMP-23 [115] and MMP-25 [115], as well as MMP-26, for which some functional evidence also exists [155].
Finally, other MMPs appear to be less significantly involved in PrCa. Thus, most studies reported no association between PrCa and MMP-1 in terms of the expression [31,48,52,68,74,83], activation [29] or polymorphism [28,44,60,63,64,68,74,81,88,90,110,155]. However, other studies have reported associations between expression and PrCa [46], including grade/stage [105,139] and metastatic properties, with MMP-1 ablation shown to reduce invasion [154]. Similarly, MMP-13 expression has typically not been associated with PrCa [31,48,84,91,95], but some studies do provide evidence of this [50,52,70]. Publications investigating MMP-11 also range from identifying no correlation [91] to a negative correlation [83] to a positive correlation [45,48], while the only study on MMP-23 points toward a negative correlation [115].
2.2. Membrane-Tethered Matrix Metalloproteinases (MT-MMPs)
Thirty-four articles were identified detailed the role of membrane-type MMPs in PrCa (Table 2). The majority of these related to MT1-MMP (formerly MMP-14). There were conflicting reports about whether MT1-MMP was upregulated [38,65,158] or downregulated [78,112] in PrCa, which may be partially explained by studies describing its expression as being variable across the stages of PrCa progression [67,83,101,140], with PrCa cells eliciting altered MT1-MMP expression in surrounding noncancer cells [34,36,37,151]. However, functional studies have consistently shown MT1-MMP to contribute to a more invasive/migratory phenotype [158,159,160,161,162] and, potentially, tumor growth [163,164].
Table 2.
Studies on Membrane-Tethered Matrix Metalloproteinase (MT-MMPs) in PrCa.
| Authors | Year | MT-MMP | PrCa Platform | Role |
|---|---|---|---|---|
| Aalinkeel et al. [20] | 2004 | MT1- and MT4-MMP * | Yes—Prostate cell lines | MT4-MMP expression higher in metastatic PrCa cells lines. |
| Bair et al. [159] | 2005 | MT1-MMP | Yes—Prostate samples and prostate cell lines | Ablation of MT1-MMP decreased migration and invasion. |
| Bonfil et al. [163] | 2007 | MT1-MMP | Yes—Prostate samples and prostate cell lines | MT1-MMP expressed in PrCa bone metastasis. Enforced expression of MT1-MMP enhanced tumor growth and osteolysis. |
| Cao et al. [158] | 2008 | MT1-MMP | Yes—Prostate cell lines | MT1-MMP expression increased in PrCa. Enforced expression of MT1-MMP induced epithelial to mesenchymal transition associated with metastatic ability. |
| Cardillo et al. [34] | 2006 | MT1-MMP * | Yes—Prostate samples | MT1-MMP expression increased in epithelial and stromal tissues in PrCa. |
| Castellana et al. [36] | 2009 | MT1-MMP * | Yes—Prostate cell lines | MT1-MMP protein levels high in PrCa microvesicles. |
| Cheng et al. [165] | 2017 | MT6-MMP | Yes—Prostate samples/Serum | MT6-MMP expression upregulated in serum and tissue in PrCa. |
| Chu et al. [166] | 2006 | MT3-MMP | Yes—Prostate cell lines and mice | MT3-MMP expressed in PrCa tumors, especially in lymph node metastases. |
| Coulson-Thomas et al. [37] | 2010 | MT1-MMP * | Yes—Prostate cell lines | MT1-MMP expressed in the stromal cells during co-culture with metastatic PrCa cells, extending into the ECM |
| Daja et al. [38] | 2003 | MT1-, MT2- and MT3-MMP * | Yes—Prostate cell lines | MT1&3-MMP (but not MT2-MMP) expressed highly, particularly processed versions, in aggressive PrCa cell lines. |
| Jennbacken et al. [65] | 2006 | MT1-MMP * | Yes—Prostate cell lines | MT1-MMP expression increased in more invasive PrCa subline. |
| Jiang et al. [167] | 2017 | MT3-MMP | Yes—Prostate samples and prostate cell lines | High levels of MT3-MMP associated with advanced tumor stage and metastasis. Ablation of MT3-MMP decreased migration. |
| Jung et al. [168] | 2003 | MT1- and MT5-MMP | Yes—Prostate samples and prostate cell lines | MT1 and 5-MMP expressed in most PrCa cell lines and prostate tissue, with variable expression in metastatic lines and malignant tumors, with no correlation to tumor classification. |
| Khamis et al. [169] | 2016 | MT6-MMP | Yes—Prostate samples and prostate cell lines | MT6-MMP expression up-regulated in high grade prostate intraepithelial neoplasia but decreased with PrCa progression, with MT6-MMP expressing cells prone to apoptosis. |
| Latil et al. [78] | 2003 | MT1-MMP * | Yes—Patient samples | MT1-MMP expression decreased in PrCa tissue. |
| Lee et al. [170] | 2006 | MT6-MMP | Yes—Prostate samples | MT6-MMP expression increased in high-grade prostatic intraepithelial neoplasia but reduced in invasive cancer. |
| Lichtinghagen et al. [83] | 2003 | MT1-MMP * | Yes—Prostate samples | MT1-MMP expression observed in PrCa, but no correlation with grade, stage, or serum PSA. |
| Lin et al. [171] | 2013 | MT3-MMP | Yes—Prostate samples | MT3-MMP single nucleotide polymorphisms associated with PrCa aggressiveness. |
| Lin et al. [172] | 2016 | MT3-MMP | Yes—Prostate samples | MT3-MMP expression associated with PrCa aggressiveness. |
| Littlepage et al. [84] | 2010 | MT1-MMP * | Yes—Mice | Broad MMP inhibitor reduced tumor burden. |
| Liu et al. [173] | 2010 | MT1-MMP | Yes—Prostate cell lines | MT1-MMP ablation reduced susceptibility to immune-mediated killing. |
| Nagakawa et al. [174] | 2000 | MT1-MMP | Yes—Prostate cell lines | MT1-MMP expression increased in more metastatic PrCa lines. |
| Neuhaus et al. [101] | 2017 | MT1-MMP * | Yes—Prostate samples | MT1-MMP expression decreased in PrCa but increased in benign prostatic hyperplasia. |
| Nguyen et al. [161] | 2011 | MT1-MMP | Yes—Prostate cell lines | Enforced MT1-MMP expression increased invasion. |
| Reis et al. [112] | 2012 | MT1-MMP * | Yes—Prostate samples | MT1-MMP under-expressed in PrCa. |
| Riddick et al. [115] | 2005 | MT2-, MT5- and MT6-MMP * | Yes—Prostate samples | MT2- and MT6-MMP (but not MT5-MMP) expression correlated positively with Gleason score. |
| Sabbota et al. [160] | 2010 | MT1-MMP | Yes—Prostate cell lines | Enforced MT1-MMP expression enhanced tumor migration. |
| Sroka et al. [175] | 2008 | MT1-MMP | Yes—Prostate samples and prostate cell lines | MT1-MMP expression in apical regions in PIN and PrCa. |
| Udayakumar et al. [176] | 2003 | MT1-MMP | Yes—cells and patients | Ablation of MT1-MMP enhanced cell migration. |
| Upadhyay et al. [140] | 1999 | MT1-MMP * | Yes—Prostate samples | MT1-MMP localized in benign glands changing to cytoplasmic staining and then heterogenous as PrCa progressed. Increased vasculature when MT1-MMP co-localized with MMP-2. |
| Wang et al. [164] | 2009 | MT1-MMP | Yes—Prostate cell lines and mice | MT1-MMP expression increased in tumor cells.Enforced expression increased tumor growth in mice. |
| Zarrabi et al. [162] | 2011 | MT1-MMP | Yes—Prostate cell lines | MT1-MMP inhibition decreased cell migration, but not growth. |
| Zhang et al. [151] | 2002 | MT1- and MT3-MMP * | Yes—Prostate samples and prostate cell lines | MT1 and 3-MMP expressed in stromal and epithelial cells in PrCa. |
| Zhao et al. [155] | 2003 | MT6-MMP * | Yes—Prostate samples and prostate cell lines | MT6-MMP highly expressed in PrCa samples. Inhibition of MT6-MMP decreased invasion. |
* Included in at least one other table.
A single study reported that MT2-MMP is downregulated in PrCa [38], but in contrast, MT3-MMP expression was increased and correlated with enhanced aggressiveness/metastatic potential [38,166,167,172]. Likewise, MT6-MMP expression was generally observed to be increased in PrCa [155,165], including one study that indicated a correlation with the PrCa grade [115]. The sole functional study suggested that this MT-MMP also makes a contribution to enhanced invasion [155].
2.3. Tissue Inhibitors of Metalloproteinases (TIMPs)
The TIMPs represent direct regulators of the metzincin superfamily—particularly, members of the MMP subgroup (Table 3). Fifty-three studies investigated the role of TIMPs in PrCa progression, which collectively indicated that these proteins typically act to suppress PrCa progression. For TIMP-1, the expression was generally reduced in PrCa [66,82,95,123,146,177], including specifically in the transition from benign to neoplastic disease [25,55,178], and was also decreased in the recurrent [113] and metastatic [179] forms of the disease. However, some studies reported increased expression in more advanced/aggressive/malignant forms [20,38,48,60,68]. This difference may in part be due to its known upregulation by inflammatory cytokines [180] that might independently impact the expression in more advanced PrCa, as well as the mode of analysis, with the protein and mRNA levels not always in correlation [82].
Table 3.
Studies on the Tissue Inhibitor of Metalloproteinases (TIMPs) in PrCa.
| Authors | Year | TIMP | PrCa Platform | Role |
|---|---|---|---|---|
| Aalinkeel et al. [20] | 2004 | TIMP-1, 3 and 4 * | Yes—Prostate cell lines | TIMP-1 and 4 (but not TIMP-3) expressed higher in more metastatic PrCa cells. |
| Adissu et al. [181] | 2015 | TIMP-3 | Yes—Mice | TIMP-3 mouse knockout exhibited enhanced PrCa tumor growth and invasion. |
| Ashida et al. [178] | 2004 | TIMP-1 | Yes—Prostate samples | TIMP-1 expression down-regulated in the transition to PrCa. |
| Babichenko et al. [25] | 2014 | TIMP-1 * | Yes—Prostate samples | TIMP-1 expression lower in PrCa adenocarcinoma compared to benign prostatic hyperplasia. |
| Baker et al. [182] | 1994 | TIMP-1 and 2 * | Yes—Prostate samples | TIMP-1 expression higher and TIMP-2 lower in PrCa patients. |
| Brehmer et al. [32] | 2003 | TIMP-1 and 2 * | Yes—Prostate samples | TIMP-1 expression decreased in PrCa compared to normal tissue, whereas TIMP-2 expression not significantly different. |
| Daja et al. [38] | 2003 | TIMP-1 * | Yes—Prostate cell lines | TIMP-1 expression higher in more aggressive PrCa cell lines. |
| De Cicco et al. [39] | 2008 | TIMP-1 and 2 * | Yes—Prostate samples/Serum | TIMP-1 and 2 serum levels do not correlate with PrCa progression. |
| Deng et al. [183] | 2006 | TIMP-3 | Yes—Prostate cell lines | Enforced TIMP-3 expression caused apoptosis and increased sensitivity to chemotherapeutic agents. |
| Escaff et al. [48] | 2010 | TIMP-1, 2 and 3 * | Yes—Prostate samples | TIMP-1 expression significantly increased in PrCa and associated with Gleason score. |
| Escaff et al. [49] | 2011 | TIMP-1, 2 and 3 * | Yes—Prostate samples | Expression of TIMP-3 (but not TIMP-1 and 2) increased in mononuclear inflammatory cells in PrCa carcinoma. |
| Fernandez-Gomez et al. [52] | 2011 | TIMP-1, 2 and 3 * | Yes—Prostate samples | TIMP-2 expression in mononuclear inflammatory cells significantly associated with decreased tumor grade. TIMP-3 expression in stromal fibroblasts correlated with histological grade. |
| Gong et al. [184] | 2015 | TIMP-1 | Yes—Prostate samples and prostate cell lines | TIMP-1 highly expressed in tumors from castration-resistant PrCa patients. |
| Gravina et al. [55] | 2013 | TIMP-1, 2 and 3 * | Yes—Prostate cell lines | TIMP-1, 2 and 3 expression reduced in PrCa compared to benign prostatic hyperplasia. |
| Gustavsson et al. [185] | 2008 | TIMP-2 and 3 * | Yes—Prostate cell lines and mice | Expression of TIMP-2 (but not TIMP-3) higher in PrCa xenografts. |
| Hashimoto et al. [60] | 1998 | TIMP-1 * | Yes—Prostate samples | MMP-7/TIMP-1 ratio higher in advanced PrCa and correlated with increased invasion and elevated PSA. |
| Hoque et al. [186] | 2005 | TIMP-3 | Yes—Prostate samples/Urine | TIMP-3 gene promoter methylated in urine samples of PrCa patients. |
| Jerónimo et al. [187] | 2004 | TIMP-3 | Yes—Prostate samples | TIMP-3 gene promoter methylation significant in high-grade prostatic intraepithelial neoplasia and benign prostatic hyperplasia. |
| Jung et al. [66] | 1998 | TIMP-1 * | Yes—Prostate samples | TIMP-1 expression lower in PrCa versus normal tissue. |
| Jung et al. [68] | 1997 | TIMP-1 * | Yes—Prostate samples | TIMP-1 highly expressed in PrCa patients with metastasis compared to benign prostatic hyperplasia. TIMP-1 correlated with PrCa staging not grade. |
| Kamińska et al. [188] | 2019 | TIMP-2 | Yes—Prostate cell lines | TIMP-2 promoter hypermethylation resulting in decreased expression in PrCa. |
| Karan et al. [189] | 2003 | TIMP-3 * | Yes—Prostate samples and prostate cell lines | TIMP-3 not expressed in PrCa cell lines, only in benign prostatic hyperplasia. |
| Kim et al. [179] | 2012 | TIMP-1 * | Yes—Prostate samples | TIMP-1 expression downregulated in metastatic PrCa. |
| Kuefer et al. [190] | 2006 | TIMP-2 * | Yes—Prostate samples and prostate cell lines | TIMP-2 over-expressed in PrCa tissue. |
| Kwabi-Addo et al. [191] | 2010 | TIMP-3 | Yes—Patient samples | TIMP-3 promoter more highly methylated in PrCa versus controls. |
| Lee et al. [192] | 2012 | TIMP-2 | Yes—Prostate cell lines and mice | TIMP-2 administration decreased tumor growth. |
| Lein et al. [79] | 1999 | TIMP-1 * | Yes—Prostate samples | TIMP-1 plasma concentration significantly higher in PrCa and correlated with tumor stage. |
| Leshner et al. [80] | 2016 | TIMP-2 and 3 * | Yes—Prostate samples | TIMP-2 and 3 genes do not reposition during PrCa progression. |
| Lichtinghagen et al. [82] | 2002 | TIMP-1 * | Yes—Prostate samples | TIMP-1 protein, but not mRNA, decreased in PrCa tissue. |
| Lichtinghagen et al. [83] | 2003 | TIMP-1, 2 and 3 * | Yes—Prostate samples | Expression of TIMP-2 and 3 (but not TIMP-1) decreased in PrCa tissue, with TIMP-2 correlating with stage. |
| Liu et al. [177] | 2005 | TIMP-1 | Yes—Prostate samples | TIMP-1 protein levels decreased in PrCa samples, being located in secretory cells. |
| Lokeshwar et al. [86] | 1993 | TIMP * | Yes—Prostate samples | TIMP expression high in normal, but not neoplastic prostate. |
| Morgia et al. [95] | 2005 | TIMP-1 * | Yes—Prostate samples | TIMP-1 expression reduced in patients with metastatic PrCa. |
| Oh et al. [193] | 2011 | TIMP-1 | Yes—Prostate samples | Elevated plasma TIMP-1 correlated with decreased survival in metastatic PrCa. |
| Ozden et al. [105] | 2013 | TIMP-1 * | Yes—Prostate samples | TIMP-2 expression in normal glands associated with lower Gleason grade. |
| Pulukuri et al. [194] | 2007 | TIMP-2 | Yes—Prostate samples and prostate cell lines | Re-expression of TIMP-2 reduced tumor invasion. |
| Reis et al. [112] | 2012 | TIMP-2 * | Yes—Prostate samples | TIMP-2 under expressed in PrCa samples, but expression increased in higher grades. |
| Reis et al. [113] | 2015 | TIMP-1 and 2 * | Yes—Prostate samples | Reduced TIMP-1 expression associated with recurrence, whereas TIMP-2 expression negative in all cases. |
| Reis et al. [114] | 2011 | TIMP-1 * | Yes—Prostate samples | TIMP-1 under-expressed in PrCa samples but over-expressed in benign samples. |
| Riddick et al. [115] | 2005 | TIMP-3 and 4 * | Yes—Prostate samples | TIMP-3 and 4 expression negatively correlated with Gleason score. |
| Ross et al. [116] | 2003 | TIMP-2 * | Yes—Prostate samples | TIMP-2 expression correlated with advanced PrCa. |
| Ross et al. [195] | 2012 | TIMP-1 | Yes—Prostate samples | TIMP-1 expression in blood cells upregulated in PrCa. |
| Sehgal et al. [123] | 2003 | TIMP-1 * | Yes—Prostate cell lines | TIMP-1 expression reduced in metastatic PrCa subline. |
| Shinojima et al. [196] | 2012 | TIMP-3 | Yes—Prostate samples | TIMP-3 expression down regulated in PrCa versus normal due to promoter hypermethylation. |
| Srivastava et al. [131] | 2012 | TIMP-2 * | Yes—Prostate specimens | TIMP-2 GC polymorphism associated with PrCa progression not initiation, as well as cancer risk. |
| Stearns et al. [180] | 1995 | TIMP-1 * | Yes—Prostate cell lines | TIMP-1 expressed in PrCa cells. |
| Still et al. [134] | 2000 | TIMP-2 * | Yes—prostate specimens | MMP-2/TIMP-2 ratio increased in tumors of higher grade and stage. |
| Trudel et al. [136] | 2008 | TIMP-2 * | Yes—Prostate specimens | Higher TIMP-2 expression associated with longer disease-free survival. |
| Wood et al. [146] | 1997 | TIMP-1 and 2 * | Yes—Prostate samples | TIMP-1 and 2 expressed in stromal inversely correlated with Gleason score, with reduced expression in metastatic PrCa samples. |
| Yamanaka et al. [197] | 2003 | TIMP-3 | Yes—Prostate samples | TIMP-3 promoter methylation low, and unchanged between PrCa and benign samples. |
| Yaykaşli et al. [149] | 2014 | TIMP-2 * | Yes—Prostate samples | TIMP-2 polymorphism under-represented in PrCa patients. |
| Zhang et al. [151] | 2002 | TIMP-1 and 2 * | Yes—Prostate samples and prostate cell lines | TIMP-1 and 2 expressed in both stromal and epithelial cells in PrCa, with no difference between fibroblasts and smooth muscle cells. Tendency for higher TIMP-2 expression in cells derived from malignant PrCa tissue. |
| Zhang et al. [198] | 2010 | TIMP-3 | Yes—Prostate samples, Prostate cell lines and mice | Enforced TIMP-3 expression inhibited proliferation, survival, migration, invasion, and adhesion of cells, with reduced incidence and size of tumors in mice. |
* Included in at least one other table.
For TIMP-2, the included studies typically reported a reduction in expression in PrCa [55,83,112,182,188], including a negative correlation of the expression to tumor grade [105,146] and metastasis [146], with promoter hypermethylation representing one mechanism by which the expression could be lost [188]. There were also a number of conflicting studies [116,151,185,190]. However, functional investigations have demonstrated that TIMP-2 administration reduced the tumor growth [192], and enforced TIMP-2 expression reduced the tumor invasion [194].
The publications on TIMP-3 provided a similar picture, with most showing a reduced expression in PrCa [20,55,189,196], including a negative correlation with the grade [115], and with promoter hypermethylation again representing a key mechanism [191], although a couple of studies were in disagreement with this interpretation [49,52]. The functional investigations were quite definitive, however, with the ablation of TIMP-3 in mice leading to enhanced tumor growth and invasion [181] and enforced expression decreasing the proliferation, survival, migration and invasion [198], as well as increasing apoptosis and chemosensitivity [183].
Finally, there were only two studies identified on TIMP-4, one of these demonstrating an increased expression in PrCa [20] and the other one indicating a negative correlation with the grade [115].
2.4. A Disintegrin and Metalloproteinases (ADAMs)
Twenty-two studies investigated members of the ADAM subgroup in the context of PrCa (Table 4). A number of these provided strong evidence of positive involvement in various aspects of the disease progression. Thus, ADAM-15 expression in PrCa positively correlated with the stage, grade, metastasis and recurrence, with its ablation decreasing both the migration and metastasis [190,199,200]. ADAM-17 expression was also shown to be significantly increased in PrCa and correlated with invasiveness, with ablation decreasing the proliferation and invasiveness [201,202]. ADAM-28 expression was similarly demonstrated to be higher in PrCa, with enforced expression enhancing the proliferation and migration [203].
Table 4.
Studies on A Disintegrin and Metalloproteinases (ADAMs) in PrCa.
| Authors | Year | ADAM | PrCa Platform | Role |
|---|---|---|---|---|
| Arima et al. [204] | 2007 | ADAM-10 | Yes—Prostate cell lines and prostate samples | ADAM-10 nuclear localization significantly increased in PrCa compared to benign and correlated with Gleason score. Ablation of ADAM-10 decreased cell proliferation. |
| Bilgin Doğru et al. [205] | 2014 | ADAM-12 | Yes—Prostate samples/urine | Serum and urine ADAM-12 levels significantly higher in PrCa patients compared to healthy controls, but no correlation with stage. |
| Burdelski et al. [199] | 2017 | ADAM-15 | Yes—Prostate samples | ADAM-15 expression correlated to stage, Gleason grade, lymph node metastasis and PSA recurrence. |
| Fritzsche et al. [206] | 2006 | ADAM-8 | Yes—Prostate samples | ADAM-8 expression correlated with higher Gleason score, but not PSA relapse-free survival. |
| Fritzsche et al. [207] | 2008 | ADAM-9 | Yes—Prostate samples | ADAM-9 expression significantly higher in PrCa compared to normal tissue, and associated with shortened PSA relapse-free survival, especially in androgen-ablated patients. |
| Hoyne et al. [208] | 2016 | ADAM-19 | Yes—Prostate samples and prostate cell lines | ADAM-19 expression decreased in PrCa compared to normal tissue, and positively correlated with lower grade and reduced relapse. Over-expression of ADAM-19 reduced proliferation and migration, but increased cell death. |
| Josson et al. [209] | 2011 | ADAM-9 | Yes—cells | Ablation of ADAM-9 increased apoptosis, increased sensitivity to radiation and chemotherapy, and induced epithelial phenotype. |
| Karan et al. [189] | 2003 | ADAM-9, 10 and 17 * | Yes—cells and patients | Expression of ADAM-17 (but not ADAM-9 or ADAM-10) increased in PrCa compared to benign samples. |
| Kuefer et al. [190] | 2006 | ADAM-15 * | Yes—Prostate samples and prostate cell lines | Expression of ADAM-15 significantly higher in PrCa and associated with increased Gleason score and angioinvasion. |
| Lin et al. [201] | 2012 | ADAM-17 | Yes—Prostate cell lines | Enforced ADAM-17 expression increased cell proliferation. |
| Lin et al. [210] | 2012 | ADAM-9 | Yes—Prostate samples | ADAM-9 expression reduced in castrate-resistant PrCa compared to hormone-sensitive PrCa, with low expression in castrate-resistant PrCa associated with shorter overall survival. |
| Liu et al. [211] | 2013 | ADAM-9 | Yes—Prostate cell lines and mice | Ablation of ADAM-9 decreased proliferation in vivo and tumor growth in mice. |
| McCulloch et al. [212] | 2000 | ADAM-9, 10, 11, 15 and 17 | Yes—Prostate cell lines | ADAM-9, 10, 11, 15 and 17 expressed in PrCa cell lines, with androgens increasing expression of ADAM-9 and 10 while ADAM-17 was downregulated. |
| McCulloch et al. [213] | 2004 | ADAM-10 | Yes—Prostate samples and prostate cell lines | ADAM-10 localized to secretory cells in PrCa with additional basal cell in benign glands. |
| Najy et al. [200] | 2008 | ADAM-15 | Yes—Cells | Ablation of ADAM-15 reduced migration and adhesion in vitro and decreased bone metastasis in mice. |
| Peduto et al. [214] | 2006 | ADAM-12 | Yes—Mice | ADAM-12 expressed in stromal cells adjacent to epithelial cells in PrCa. ADAM12 knock-out mice showed delayed tumor progression. |
| Peduto et al. [215] | 2005 | ADAM-9 | Yes—Mice | ADAM-9 expression elevated in mouse PrCa model. ADAM-9 knock-out resulted in well differentiated tumors. Overexpression of ADAM-9 led to epithelial hyperplasia and intraepithelial neoplasia. |
| Pen et al. [216] | 2012 | ADAM-9 | Yes—Prostate samples, prostate cell lines and mice | ADAM-9 nuclear expression observed in hormone refractory PrCa and in relapse patients, with levels correlated with the risk of relapse. |
| Rudnicka et al. [203] | 2016 | ADAM-28 | Yes—Prostate samples and prostate cell lines | ADAM-28 expression increased in PrCa samples compared to normal tissue and in PrCa cell lines. Over-expression of ADAM-28 stimulated proliferation and migration, whereas ablation of expression or activity reduced these phenotypes. |
| Shigemura et al. [217] | 2007 | ADAM-9 | Yes—Prostate cell lines | ADAM-9 expressed in AR-positive PrCa cells. |
| Sung et al. [218] | 2006 | ADAM-9 | Yes—Prostate samples and prostate cell lines | ADAM-9 expression elevated in in malignant compared to benign prostate tissue. ADAM-9 expression correlated to transition to androgen-independence and cellular stress. |
| Xiao et al. [202] | 2012 | ADAM-17 | Yes—Prostate cell lines | ADAM-17 expression correlated with invasiveness. Enforced expression of ADAM-17 increased invasiveness, whereas ablation decreased invasiveness. |
* Included in at least one other table.
The results regarding ADAM-9 were more complex, with one study showing no change in expression in PrCa [189] and others showing an increased expression that correlates with malignancy and reduced survival [207,216] but another reporting a decrease in expression in castrate-resistant compared to androgen-sensitive PrCa [210]. However, the ablation of ADAM-9 reduced the proliferation and tumor growth and increased the differentiation, decreasing the metastatic ability while increasing the sensitivity to chemotherapeutic drugs [209]. For ADAM-10, the nuclear localization rather than expression was increased in PrCa, with ablation decreasing the growth [204]. For ADAM-12, the serum levels have been demonstrated to be increased in PrCa, with expression found in stromal tissue, and progression delayed in knockout mice [205,214].
The clear exception in this family was ADAM-19, which was found to be more highly expressed in normal tissue compared to PrCa and negatively correlated to the grade and relapse, with the enforced expression leading to decreased proliferation, metastatic ability and survival [208].
2.5. A Disintegrin and Metalloproteinase with Thrombospondin Motifs (ADAMTSs)
Eight studies were identified that related to the ADAMTS subgroup in PrCa progression (Table 5). The majority focused on ADAMTS-1, providing evidence of a tumor-suppressing function. ADAMTS-1 expression was typically decreased in PrCa samples, patients with metastatic disease, and a PrCa cell line variant with higher metastatic potential but elevated in slower-growing PrCa tumors in mice [65,179,219,220]. This was supported by functional data from the cells in which ADAMTS-1 expression had been modulated, which suggested a role in growth, although this appeared to depend on the cell line used [219]. ADAMTS-15 was also shown to be able to suppress tumor growth and migration, although it augmented survival [221]. Other members of the ADAMTS subgroup have also been shown to be expressed in PrCa cell lines, but their role in PrCa progression remains elusive [222].
Table 5.
Studies on A Disintegrin and Metalloproteinase with Thrombospondin Motifs (ADAMTSs) in PrCa.
| Authors | Year | ADAMTS | PrCa Platform | Role |
|---|---|---|---|---|
| Binder et al. [221] | 2020 | ADAMTS-15 | Yes—Prostate samples, prostate cell lines and mice | ADAMTS-15 expressed and active in PrCa samples. Enforced ADAMTS-15 expression decreased migration and proliferation but increased survival in vitro and suppressed tumor growth in mice. |
| Cross et al. [222] | 2005 | ADAMTS-1, 4, 5, 9 and 15 | Yes—Prostate cell lines | ADAMTS-1, ADAMTS-4, ADAMTS-5, ADAMTS-9 and ADAMTS-15 expressed in PrCa. |
| Gustavsson et al. [185] | 2008 | ADAMTS-1 * | Yes—Prostate cell lines and mice | ADAMTS-1 expression decreased in PrCa cell line with enhanced angiogenic and tumorigenic properties, compared to parent. |
| Gustavsson et al. [220] | 2009 | ADAMTS-1 | Yes—Prostate samples | ADAMTS-1 expression decreased in prostate cancer cells compared to benign prostate glands. No correlation with Gleason score, but expression lower in patients with metastatic disease. |
| Gustavsson et al. [219] | 2010 | ADAMTS-1 | Yes—Prostate cell lines and mice | ADAMTS-1 ablation decreased tumor growth, but in other PrCa cells enforced expression inhibited tumor growth. |
| Jennbacken et al. [65] | 2009 | ADAMTS-1 | Yes—Prostate cell lines and mice | ADAMTS-1 expression increased in slow growing tumors in mice. |
| Kim et al. [179] | 2012 | ADAMTS-1 * | Yes—Prostate samples | ADAMTS-1 mRNA overexpressed in PrCa samples. |
| Molokwu et al. [223] | 2010 | ADAMTS-1 and 15 | Yes—Prostate cell lines | ADAMTS-15 (but not ADAMTS-1) expressed in PrCa. |
* Included in at least one other table.
3. Discussion
3.1. Overview
This study used a systematic-like review strategy to identify publications examining the role of metzincins in PrCa progression. While limited to articles in PUBMED and MEDLINE and those written in English, this approach was likely to yield the vast majority of relevant research publications. It is evident from a close examination of the 205 articles identified that the contributions made by members of the metzincin superfamily to PrCa disease progression are complex. For many individual members and, indeed, the entire Astracin family, there is currently no evidence of involvement. However, a significant number of metzincins are positively associated with PrCa, supported by functional evidence in a number of cases, while others were negatively associated with this disease. The positive associations were particularly strong with specific members of the MMP, MT-MMP and ADAM subgroups, while those within the ADAMTS subgroup or the important TIMP family of regulators were more likely to show negative associations.
3.2. Positive Associations
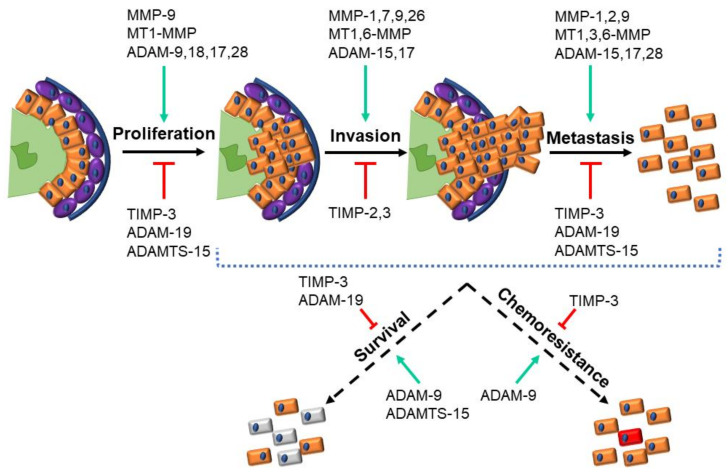
The clearest evidence for positive contributions to PrCa and its progression was for MMP-2, MMP-7, MMP-9, MT1-MMP, ADAM-15, ADAM-17 and ADAM-28, with supporting evidence for MMP-1, MT3-MMP, MT6-MMP and ADAM-9 (Table 1, Table 2 and Table 4). This is underpinned by studies that have identified associations between the expression and PrCa, which, in the case of MMP-7 expression [60,63,73,88,99,104,106,110,135,147] and ADAM-15 expression [190,199,200], correlated with the pathological stage and poorer outcomes for patients. This was supported by functional analyses that consistently identified enhancements in the proliferation, invasion/spread and metastasis/migration facilitated by them [56,106,110,200] (Figure 2). This identified these specific metzincins as likely tumor-promoting factors and so represented the obvious candidates as disease biomarkers or as potential targets for therapeutic agents.
Figure 2.
Metzincins and their regulators in prostate cancer. Schematic representation of prostate cancer progression highlighting the key cellular functions that are modulated by the indicated metzincin superfamily members, along with the regulatory Tissue Inhibitor of Metalloproteinase (TIMP) proteins (green: Lumen, orange: Luminal cells, purple: Basal cells, and blue: Basement membrane).
3.3. Negative Associations
The strongest evidence for negative contribution to PrCa is for TIMP-2 and TIMP-3, as well as ADAM-19, ADAMTS-1 and ADAMTS-15 (Table 3, Table 4 and Table 5). Such a role for the ADAMTS proteins is somewhat counterintuitive, since these enzymes cleave ECM components like other metzincins [224], including those involved in PrCa disease progression [220,221]. However, the functional evidence points to these enzymes inhibiting key phenotypes, including proliferation and metastasis/migration, although not survival (Figure 2), presumably due to the different specificities for ECM components compared to other metzincins [220,221]. ADAM-19 was also implicated in the proliferation, metastasis/migration and survival (Figure 2), although this could relate to the known nonenzymatic functions for these enzymes. A negative role for the TIMP family was less surprising, given their primary role in the inhibition of MMP enzymes [225], with this impact extending across the entire gamut of relevant cell functions (Figure 2). These molecules can also be considered biomarker candidates to aid in prognosis. Therapeutic approaches targeting these proteins would likely be more limited, however, since they would need to augment, rather than inhibit, their function.
3.4. Mixed Associations
For other metzincins, the evidence for their involvement in PrCa was even more variable and contradictory, such as for MMP-11. Indeed, even those metzincins or regulators with consistent positive or negative correlations with PrCa were often reported in some studies to have no correlation or, indeed, the opposite correlation. This suggests a complex interplay between metzincins and PrCa.
3.5. Understanding the Complexity
In interpreting the variable and, at times, conflicting data, there are a number of factors that need to be considered. Firstly, different studies have utilized alternate approaches, such as analyzing the expression at the gene versus protein levels, that do not always correlate [24,68,82,83,91,101,140,189] or examining the enzymatic activity, which is not always reflective of metzincin expression [119,226], or, instead, considering the cellular localization [140]. Moreover, different samples have been analyzed in the literature, including plasma/serum, urine and tumor biopsies from PrCa patients, with several studies highlighting the differences between tissues [119], while the exact PrCa stage is also critical [117]. Other studies have employed PrCa cell lines and xenotransplanted tumors in mice, the relevance of which to human disease is assumed but not guaranteed. Secondly, it is clear that the factors controlling the expression of these enzymes and their regulators are complex. Thus, many metzincins have been demonstrated to be regulated by androgens [107,213,217,223,227,228], which can clearly be a complicating factor given the environment in which these cancers develop. In addition, expression is also impacted by oncogenes [85,147], inflammation and inflammatory cytokines [99,229], as well as angiogenic factors such as vascular endothelial factor [216], which are intrinsic features of any cancer. The cellular environment can further influence both expression [127] and activation [143]. Therefore, discerning the direction of causality between the expression and PrCa is not always straightforward.
In most cases, the effects of the metzincin superfamily member (or inhibitor) have been presumed to relate to the primary role for metzincins in regulating components of the ECM, which is known to be a particularly key element of metastasis [9,13]. However, which substrates are important? The cleavage of laminin [159,176], perlecan [56] and beta-4 integrin [230] have all been shown to correlate with the effects of protumorigenic metzincins, particularly on metastasis, whereas versican has been identified as a target of the antitumorigenic ADAMTS-15 [221]. Clearly, more research is required to understand this important aspect of metzincin pathobiology. Moreover, other roles should also be considered, especially given reports suggesting that nuclear localization may be important in some situations [204,213,216], with both ADAMs and ADAMTSs known to have nonenzymatic roles.
There also remains a lack of depth in our understanding of how metzincins are regulated at the protein level, including by other metzincins. TIMPs are clearly important for the negative regulation of MMPs [114]. TIMPs are typically downregulated as cancer progresses and can act as independent correlates of PrCa progression [25,32,95,112,114,116,177,178,179], especially when combined with MMP expression [83,105,116]. TIMP-2 and TIMP-3 have also been shown to inhibit ADAMTS-1 [185]. Are there equivalents for ADAM and other ADAMTS enzymes? In addition, MT1-MMP has been shown to exert its role at least in part through the direct activation of MMP-2 [140,159]. Is this crosstalk common across metzincins? More research is needed to gain further insight in this area.
4. Materials and Methods
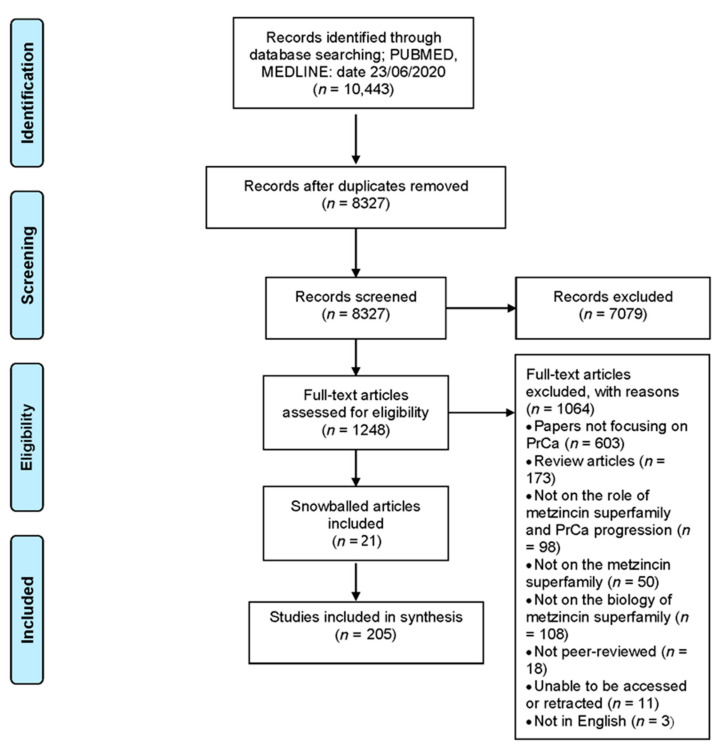
This study represents a systematic-like review of the role of the metzincin superfamily of proteases in PrCa progression. The search terms were identified through a PCC (population, context and concept) format by the research team with keywords, Boolean operators, truncations and Medical Subject Headings (MeSH) used to develop a database search strategy in collaboration with a specialist health librarian. In reporting the review, the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) was utilized.
4.1. Search Strategy
A preliminary search was undertaken using MEDLINE and then a full search run through both the PUBMED and MEDLINE databases.
4.2. Inclusion and Exclusion Criteria
All studies were considered based on the inclusion and exclusion criteria shown in Table 6. Search terms for inclusion were “metzinzin”, “metalloproteases”, “metalloproteinase”, “MMP”, “TIMP”, “ADAM”, “ADAMTS”, “BMP1” or “meprin” and “neoplasm”, “neoplasia”, “cancer”, “tumor” or “cysts”. Reasons for exclusion after the full-text review are detailed in Figure 3. No restrictions were put on the date that articles were published.
Table 6.
Search terms and inclusion/exclusion criteria used in this systematic-like review.
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population | Men, mice/rats or cells. | Involved other animal species or cells not related to PrCa progression. |
| Concept | All human metzincin superfamily members, including members of the MMP, MT-MMP, ADAM, ADAMTS, BMP1/TLL and Meprin subgroups, as well as the TIMP family of regulators. | Examining proteins other than metzincin superfamily members or TIMPs, or in different cancer types, other diseases, or normal biology. |
| Context | Studies that investigated the role of the metzincin superfamily in PrCa progression. | Did not specially look at the role of metzincin superfamily members in PrCa cancer progression. |
Figure 3.
Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) overview of the systematic-like review. Flow chart of the systematic-like review process undertaken, including the details of identification, screening and assessment for eligibility.
4.3. Study Selection and Data Extraction
Searches of the published literature were conducted by M.J.B. in collaboration with a specialist health librarian. Titles and abstracts were retrieved from the search and screened. Full-text article review and data extraction was then conducted, with the reasons for exclusion documented. The reference lists of the included articles were also reviewed to identify further potential articles for inclusion in the review.
4.4. Data Analysis
Database searching identified 10,443 publications. After duplicate removal, the titles and abstracts from 8327 were reviewed against the inclusion criteria. Full-text versions of 1248 articles were then further reviewed, identifying 205 articles for inclusion (Figure 2). The reasons for exclusion were a lack of focus on PrCa (n = 603) or the metzincin superfamily (n = 50) or the role of the metzincin superfamily family in PrCa progression (n = 98) or on the biology of the metzincin superfamily (n = 108) or not peer reviewed (n = 18) or being review articles (n = 173) or articles unable to be accessed or retracted (n = 11) or not in English (n = 3). The 205 included articles covered members of the Matrixin family subgroups MMP and MT-MMPs, the TIMPs and the Adamalysin family subgroups ADAMs and ADAMTSs, but there were none regarding the Astracin family subgroups BMP/TLL or Meprin.
Acknowledgments
The authors would like to acknowledge and thank Rebecca Muir for her assistance with the search strategy.
Author Contributions
Conceptualization, M.J.B. and A.C.W.; methodology, M.J.B.; formal analysis, M.J.B.; data curation, M.J.B.; writing—original draft preparation, M.J.B. and writing—review and editing, M.J.B. and A.C.W. Both authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rawla P. Epidemiology of prostate cancer. World J. Oncol. 2019;10:63–89. doi: 10.14740/wjon1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2020 doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Saraon P., Drabovich A.P., Jarvi K.A., Diamandis E.P. Mechanisms of androgen-independent prostate cancer. EJIFCC. 2014;25:42–54. [PMC free article] [PubMed] [Google Scholar]
- 4.Descotes J.-L. Diagnosis of prostate cancer. Asian J. Urol. 2019;6:129–136. doi: 10.1016/j.ajur.2018.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomis-Rüth F.X. Structural aspects of the metzincin clan of metalloendopeptidases. Mol. Biotechnol. 2003;24:157–202. doi: 10.1385/MB:24:2:157. [DOI] [PubMed] [Google Scholar]
- 6.Stöcker W., Bode W. Structural features of a superfamily of zinc-endopeptidases: The metzincins. Curr. Opin. Struct. Biol. 1995;5:383–390. doi: 10.1016/0959-440X(95)80101-4. [DOI] [PubMed] [Google Scholar]
- 7.Stöcker W., Grams F., Reinemer P., Bode W., Baumann U., Gomis-Rüth F.-X., Mckay D.B. The metzincins—Topological and sequential relations between the astacins, adamalysins, serralysins, and matrixins (collagenases) define a super family of zinc-peptidases. Protein Sci. 1995;4:823–840. doi: 10.1002/pro.5560040502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huxley-Jones J., Clarke T.K., Beck C., Toubaris G., Robertson D.L., Boot-Handford R.P. The evolution of the vertebrate metzincins; insights from Ciona intestinalis and Danio rerio. BMC Evol. Biol. 2007;7:63. doi: 10.1186/1471-2148-7-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonnans C., Chou J., Werb Z. Remodelling the extracellular matrix in development and disease. Nat. Rev. Mol. 2014;15:786–801. doi: 10.1038/nrm3904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu P., Takai K., Weaver V.M., Werb Z. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb. Perspect. Biol. 2011;3 doi: 10.1101/cshperspect.a005058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stamenkovic I. Extracellular matrix remodelling: The role of matrix metalloproteinases. J. Pathol. 2003;200:448–464. doi: 10.1002/path.1400. [DOI] [PubMed] [Google Scholar]
- 12.Tang B.L. ADAMTS: A novel family of extracellular matrix proteases. Int. J. Biochem. Cell Biol. 2001;33:33–44. doi: 10.1016/S1357-2725(00)00061-3. [DOI] [PubMed] [Google Scholar]
- 13.Binder M.J., McCoombe S., Williams E.D., McCulloch D.R., Ward A.C. The extracellular matrix in cancer progression: Role of hyalectan proteoglycans and ADAMTS enzymes. Cancer Lett. 2017;385:55–64. doi: 10.1016/j.canlet.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Seals D.F., Courtneidge S.A. The ADAMs family of metalloproteases: Multidomain proteins with multiple functions. Genes Dev. 2003;17:7–30. doi: 10.1101/gad.1039703. [DOI] [PubMed] [Google Scholar]
- 15.Kessenbrock K., Plaks V., Werb Z. Matrix metalloproteinases: Regulators of the tumor microenvironment. Cell. 2010;141:52–67. doi: 10.1016/j.cell.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turunen S.P., Tatti-Bugaeva O., Lehti K. Membrane-type matrix metalloproteases as diverse effectors of cancer progression. Biochim. Biophys. Acta Mol. Cell Res. 2017;1864:1974–1988. doi: 10.1016/j.bbamcr.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 17.Baker A.H., Edwards D.R., Murphy G. Metalloproteinase inhibitors: Biological actions and therapeutic opportunities. J. Cell Sci. 2002;115:3719–3727. doi: 10.1242/jcs.00063. [DOI] [PubMed] [Google Scholar]
- 18.Quintero-Fabián S., Arreola R., Becerril-Villanueva E., Torres-Romero J.C., Arana-Argáez V., Lara-Riegos J., Ramírez-Camacho M.A., Alvarez-Sánchez M.E. Role of matrix metalloproteinases in angiogenesis and cancer. Front. Oncol. 2019;9 doi: 10.3389/fonc.2019.01370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gong Y., Chippada-Venkata U.D., Oh W.K. Roles of matrix metalloproteinases and their natural inhibitors in prostate cancer progression. Cancer. 2014;6:1298–1327. doi: 10.3390/cancers6031298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aalinkeel R., Nair M.P.N., Sufrin G., Mahajan S.D., Chadha K.C., Chawda R.P., Schwartz S.A. Gene expression of angiogenic factors correlates with metastatic potential of prostate cancer cells. Cancer Res. 2004;64:5311–5321. doi: 10.1158/0008-5472.CAN-2506-2. [DOI] [PubMed] [Google Scholar]
- 21.Aalinkeel R., Nair B.B., Reynolds J.L., Sykes D.E., Mahajan S.D., Chadha K.C., Schwartz S.A. Overexpression of MMP-9 contributes to invasiveness of prostate cancer cell line LNCaP. Immunol. Invest. 2011;40:447–464. doi: 10.3109/08820139.2011.557795. [DOI] [PubMed] [Google Scholar]
- 22.Adabi Z., Mohsen Ziaei S.A., Imani M., Samzadeh M., Narouie B., Jamaldini S.H., Afshari M., Safavi M., Roshandel M.R., Hasanzad M. Genetic polymorphism of MMP2 gene and susceptibility to prostate cancer. Arch. Med. Res. 2015;46:546–550. doi: 10.1016/j.arcmed.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Albayrak S., Cangüven Ö., Göktaş C., Aydemir H., Köksal V. Role of MMP-1 1G/2G promoter gene polymorphism on the development of prostate cancer in the Turkish population. Urol. Int. 2007;79:312–315. doi: 10.1159/000109715. [DOI] [PubMed] [Google Scholar]
- 24.Assikis V.J., Do K.A., Wen S., Wang X., Cho-Vega J.H., Brisbay S., Lopez R., Logothetis C.J., Troncoso P., Papandreou C.N., et al. Clinical and biomarker correlates of androgen-independent, locally aggressive prostate cancer with limited metastatic potential. Clin. Cancer Res. 2004;10:6770–6778. doi: 10.1158/1078-0432.CCR-04-0275. [DOI] [PubMed] [Google Scholar]
- 25.Babichenko I.I., Andriukhin M.I., Pulbere S., Loktev A. Immunohistochemical expression of matrix metalloproteinase-9 and inhibitor of matrix metalloproteinase-1 in prostate adenocarcinoma. Int. J. Clin. Exp. Pathol. 2014;7:9090–9098. [PMC free article] [PubMed] [Google Scholar]
- 26.Baspinar S., Bircan S., Ciris M., Karahan N., Bozkurt K.K. Expression of NGF, GDNF and MMP-9 in prostate carcinoma. Pathol. Res. Pract. 2017;213:483–489. doi: 10.1016/j.prp.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Bekes E.M., Schweighofer B., Kupriyanova T.A., Zajac E., Ardi V.C., Quigley J.P., Deryugina E.I. Tumor-recruited neutrophils and neutrophil TIMP-free MMP-9 regulate coordinately the levels of tumor angiogenesis and efficiency of malignant cell intravasation. Am. J. Pathol. 2011;179:1455–1470. doi: 10.1016/j.ajpath.2011.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Białkowska K., Marciniak W., Muszyńska M., Baszuk P., Gupta S., Jaworska-Bieniek K., Sukiennicki G., Durda K., Gromowski T., Prajzendanc K., et al. Association of zinc level and polymorphism in MMP-7 gene with prostate cancer in Polish population. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0201065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bok R.A., Hansell E.J., Nguyen T.P., Greenberg N.M., McKerrow J.H., Shuman M.A. Patterns of protease production during prostate cancer progression: Proteomic evidence for cascades in a transgenic model. Prostate Cancer Prostatic Dis. 2003;6:272–280. doi: 10.1038/sj.pcan.4500676. [DOI] [PubMed] [Google Scholar]
- 30.Bonaldi C.M., Azzalis L.A., Junqueira V.B., de Oliveira C.G., Vilas Boas V.A., Gáscon T.M., Gehrke F.S., Kuniyoshi R.K., Alves B.C., Fonseca F.L. Plasma levels of E-cadherin and MMP-13 in prostate cancer patients: Correlation with PSA, testosterone and pathological parameters. Tumori. 2015;101:185–188. doi: 10.5301/tj.5000237. [DOI] [PubMed] [Google Scholar]
- 31.Boxler S., Djonov V., Kessler T.M., Hlushchuk R., Bachmann L.M., Held U., Markwalder R., Thalmann G.N. Matrix metalloproteinases and angiogenic factors: Predictors of survival after radical prostatectomy for clinically organ-confined prostate cancer? Am. J. Pathol. 2010;177:2216–2224. doi: 10.2353/ajpath.2010.091190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brehmer B., Biesterfeld S., Jakse G. Expression of matrix metalloproteinases (MMP-2 and -9) and their inhibitors (TIMP-1 and -2) in prostate cancer tissue. Prostate Cancer Prostatic Dis. 2003;6:217–222. doi: 10.1038/sj.pcan.4500657. [DOI] [PubMed] [Google Scholar]
- 33.Bruni-Cardoso A., Johnson L.C., Vessella R.L., Peterson T.E., Lynch C.C. Osteoclast-derived matrix metalloproteinase-9 directly affects angiogenesis in the prostate tumor-bone microenvironment. Mol. Cancer Res. 2010;8:459–470. doi: 10.1158/1541-7786.MCR-09-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cardillo M.A., Di Silverio F., Gentile V. Quantitative immunohistochemical and in situ hybridization analysis of metalloproteinases in prostate cancer. Anticancer Res. 2006;26:973–982. [PubMed] [Google Scholar]
- 35.Carozzi F., Tamburrino L., Bisanzi S., Marchiani S., Paglierani M., Di Lollo S., Crocetti E., Buzzoni C., Burroni E., Greco L., et al. Are biomarkers evaluated in biopsy specimens predictive of prostate cancer aggressiveness? J. Cancer Res. Clin. Oncol. 2016;142:201–212. doi: 10.1007/s00432-015-2015-1. [DOI] [PubMed] [Google Scholar]
- 36.Castellana D., Zobairi F., Martinez M.C., Panaro M.A., Mitolo V., Freyssinet J.-M., Kunzelmann C. Membrane microvesicles as actors in the establishment of a favorable prostatic tumoral niche: A role for activated fibroblasts and CX3CL1-CX3CR1 axis. Cancer Res. 2009;69:785–793. doi: 10.1158/0008-5472.CAN-08-1946. [DOI] [PubMed] [Google Scholar]
- 37.Coulson-Thomas V.J., Gesteira T.F., Coulson-Thomas Y.M., Vicente C.M., Tersariol I.L., Nader H.B., Toma L. Fibroblast and prostate tumor cell cross-talk: Fibroblast differentiation, TGF-β, and extracellular matrix down-regulation. Exp. Cell Res. 2010;316:3207–3226. doi: 10.1016/j.yexcr.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 38.Daja M.M., Niu X., Zhao Z., Brown J.M., Russell P.J. Characterization of expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in prostate cancer cell lines. Prostate Cancer Prostatic Dis. 2003;6:15–26. doi: 10.1038/sj.pcan.4500609. [DOI] [PubMed] [Google Scholar]
- 39.De Cicco C., Ravasi L., Zorzino L., Sandri M.T., Botteri E., Verweij F., Granchi D., de Cobelli O., Paganelli G. Circulating levels of VCAM and MMP-2 may help identify patients with more aggressive prostate cancer. Curr. Cancer Drug Targets. 2008;8:199–206. doi: 10.2174/156800908784293613. [DOI] [PubMed] [Google Scholar]
- 40.Di Carlo A., Mariano A., Terracciano D., Ferro M., Montanaro V., Marsicano M., Di Lorenzo G., Altieri V., Macchia V. Matrix metalloproteinase-2 and -9 in the urine of prostate cancer patients. Oncol. Rep. 2010;24:3–8. doi: 10.3892/or_00000821. [DOI] [PubMed] [Google Scholar]
- 41.Dong Z., Nemeth J.A., Cher M.L., Palmer K.C., Bright R.C., Fridman R. Differential regulation of matrix metalloproteinase-9, tissue inhibitor of metalloproteinase-1 (TIMP-1) and TIMP-2 expression in co-cultures of prostate cancer and stromal cells. Int. J. Cancer. 2001;93:507–515. doi: 10.1002/ijc.1358. [DOI] [PubMed] [Google Scholar]
- 42.Reis S.T., Pontes J., Villanova F.E., Borra P.M.d.A., Antunes A.A., Dall’oglio M.F., Srougi M., Leite K.R.M. Genetic polymorphisms of matrix metalloproteinases: Susceptibility and prognostic implications for prostate cancer. J. Urol. 2009;181:2320–2325. doi: 10.1016/j.juro.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 43.Reis S.T., Villanova F.E., Andrade P.M., Pontes J., de Sousa-Canavez J.M., Sañudo A., Antunes A.A., Dall’Oglio M.F., Srougi M., Moreira Leite K.R. Matrix metalloproteinase-2 polymorphism is associated with prognosis in prostate cancer. Urol. Oncol. 2010;28:624–627. doi: 10.1016/j.urolonc.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 44.Reis S.T., Villanova F.E., de Andrade P.M., Pontes J., Silva I.A., Canavez F.C., Sañudo A., Srougi M., Leite K.R.M. Polymorphisms of the matrix metalloproteinases associated with prostate cancer. Mol. Med. Rep. 2008;1:517–520. doi: 10.1016/S0022-5347(09)61349-5. [DOI] [PubMed] [Google Scholar]
- 45.Eiro N., Fernandez-Gomez J., Sacristán R., Fernandez-Garcia B., Lobo B., Gonzalez-Suarez J., Quintas A., Escaf S., Vizoso F.J. Stromal factors involved in human prostate cancer development, progression and castration resistance. J. Cancer Res. Clin. Oncol. 2017;143:351–359. doi: 10.1007/s00432-016-2284-3. [DOI] [PubMed] [Google Scholar]
- 46.El-Chaer W.K., Tonet-Furioso A.C., Morais Junior G.S., Souza V.C., Avelar G.G., Henriques A.D., Franco Moraes C., Nóbrega O.T. Serum Levels of Matrix Metalloproteinase-1 in Brazilian Patients with Benign Prostatic Hyperplasia or Prostate Cancer. Curr. Gerontol. Geriatr. Res. 2020;2020:6012102. doi: 10.1155/2020/6012102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eryilmaz I.E., Aytac Vuruskan B., Kaygısız O., Egeli U., Tunca B., Kordan Y., Cecener G. RNA-based markers in biopsy cores with atypical small acinar proliferation: Predictive effect of T2E fusion positivity and MMP-2 upregulation for a subsequent prostate cancer diagnosis. Prostate. 2019;79:195–205. doi: 10.1002/pros.23724. [DOI] [PubMed] [Google Scholar]
- 48.Escaff S., Fernández J.M., González L.O., Suárez A., González-Reyes S., González J.M., Vizoso F.J. Study of matrix metalloproteinases and their inhibitors in prostate cancer. Br. J. Cancer. 2010;102:922–929. doi: 10.1038/sj.bjc.6605569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Escaff S., Fernández J.M., González L.O., Suárez A., González-Reyes S., González J.M., Vizoso F.J. Comparative study of stromal metalloproteases expression in patients with benign hyperplasia and prostate cancer. J. Cancer Res. Clin. Oncol. 2011;137:551–555. doi: 10.1007/s00432-010-0906-8. [DOI] [PubMed] [Google Scholar]
- 50.Escaff S., Fernández J.M., González L.O., Suárez A., González-Reyes S., González J.M., Vizoso F.J. Collagenase-3 expression by tumor cells and gelatinase B expression by stromal fibroblast-like cells are associated with biochemical recurrence after radical prostatectomy in patients with prostate cancer. World J. Urol. 2011;29:657–663. doi: 10.1007/s00345-010-0595-6. [DOI] [PubMed] [Google Scholar]
- 51.Fávaro W.J., Hetzl A.C., Reis L.O., Ferreira U., Billis A., Cagnon V.H. Periacinar retraction clefting in nonneoplastic and neoplastic prostatic glands: Artifact or molecular involvement. Pathol. Oncol. Res. 2012;18:285–292. doi: 10.1007/s12253-011-9440-5. [DOI] [PubMed] [Google Scholar]
- 52.Fernandez-Gomez J., Escaf S., Gonzalez L.O., Suarez A., Gonzalez-Reyes S., González J., Miranda O., Vizoso F. Relationship between metalloprotease expression in tumour and stromal cells and aggressive behaviour in prostate carcinoma: Simultaneous high-throughput study of multiple metalloproteases and their inhibitors using tissue array analysis of radical prostatectomy samples. Scand. J. Urol. Nephrol. 2011;45:171–176. doi: 10.3109/00365599.2010.545074. [DOI] [PubMed] [Google Scholar]
- 53.Festuccia C., Bologna M., Vicentini C., Tacconelli A., Miano R., Violini S., Mackay A.R. Increased matrix metalloproteinase-9 secretion in short-term tissue cultures of prostatic tumor cells. Int. J. Cancer. 1996;69:386–393. doi: 10.1002/(SICI)1097-0215(19961021)69:5<386::AID-IJC6>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 54.Gohji K., Fujimoto N., Hara I., Fujii A., Gotoh A., Okada H., Arakawa S., Kitazawa S., Miyake H., Kamidono S., et al. Serum matrix metalloproteinase-2 and its density in men with prostate cancer as a new predictor of disease extension. Int. J. Cancer. 1998;79:96–101. doi: 10.1002/(SICI)1097-0215(19980220)79:1<96::AID-IJC18>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 55.Gravina G.L., Mancini A., Ranieri G., Di Pasquale B., Marampon F., Di Clemente L., Ricevuto E., Festuccia C. Phenotypic characterization of human prostatic stromal cells in primary cultures derived from human tissue samples. Int. J. Oncol. 2013;42:2116–2122. doi: 10.3892/ijo.2013.1892. [DOI] [PubMed] [Google Scholar]
- 56.Grindel B.J., Martinez J.R., Pennington C.L., Muldoon M., Stave J., Chung L.W., Farach-Carson M.C. Matrilysin/matrix metalloproteinase-7 (MMP7) cleavage of perlecan/HSPG2 creates a molecular switch to alter prostate cancer cell behavior. Matrix Biol. 2014;36:64–76. doi: 10.1016/j.matbio.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gupta A., Cao W., Sadashivaiah K., Chen W., Schneider A., Chellaiah M.A. Promising noninvasive cellular phenotype in prostate cancer cells knockdown of matrix metalloproteinase 9. Sci. World J. 2013;2013:493689. doi: 10.1155/2013/493689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hamdy F.C., Fadlon E.J., Cottam D., Lawry J., Thurrell W., Silcocks P.B., Anderson J.B., Williams J.L., Rees R.C. Matrix metalloproteinase 9 expression in primary human prostatic adenocarcinoma and benign prostatic hyperplasia. Br. J. Cancer. 1994;69:177–182. doi: 10.1038/bjc.1994.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hanqing Z., Yajun X., Gongchen L., Yong C. Immunohistochemical studies of the expression of matrix metalloproteinase-2 and metalloproteinase-9 in human prostate cancer. J. Huazhong Univ. Sci. Med. 2003;23:373–374. doi: 10.1007/BF02829421. [DOI] [PubMed] [Google Scholar]
- 60.Hashimoto K., Kihira Y., Matuo Y., Usui T. Expression of matri metalloproteinase-7 and tissue inhibitor of metalloproteinase-1 in human prostate. J. Urol. 1998;160:1872–1876. doi: 10.1016/S0022-5347(01)62435-2. [DOI] [PubMed] [Google Scholar]
- 61.Hetzl A.C., Fávaro W.J., Billis A., Ferreira U., Cagnon V.H.A. Steroid hormone receptors, matrix metalloproteinases, insulin-like growth factor, and dystroglycans interactions in prostatic diseases in the elderly men. Microsc. Res. Tech. 2012;75:1197–1205. doi: 10.1002/jemt.22049. [DOI] [PubMed] [Google Scholar]
- 62.Incorvaia L., Badalamenti G., Rini G., Arcara C., Fricano S., Sferrazza C.D.D.T., Gebbia N., Leto G. MMP-2, MMP-9 and activin A blood levels in patients with breast cancer or prostate cancer metastatic to the bone. Anticancer Res. 2007;27:1519–1525. [PubMed] [Google Scholar]
- 63.Jaboin J.J., Hwang M., Lopater Z., Chen H., Ray G.L., Perez C., Cai Q., Wills M.L., Lu B. The matrix metalloproteinase-7 polymorphism rs10895304 is associated with increased recurrence risk in patients with clinically localized prostate cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011;79:1330–1335. doi: 10.1016/j.ijrobp.2010.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jędroszka D., Orzechowska M., Hamouz R., Górniak K., Bednarek A.K. Markers of epithelial-to-mesenchymal transition reflect tumor biology according to patient age and Gleason score in prostate cancer. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0188842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jennbacken K., Gustavsson H., Welén K., Vallbo C., Damber J.-E. Prostate cancer progression into androgen independency is associated with alterations in cell adhesion and invasivity. Prostate. 2006;66:1631–1640. doi: 10.1002/pros.20469. [DOI] [PubMed] [Google Scholar]
- 66.Jung K., Lein M., Ulbrich N., Rudolph B., Henke W., Schnorr D., Loening S.A. Quantification of matrix metalloproteinases and tissue inhibitors of metalloproteinase in prostatic tissue: Analytical aspects. Prostate. 1998;34:130–136. doi: 10.1002/(SICI)1097-0045(19980201)34:2<130::AID-PROS8>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 67.Jung K., Krell H.-W., Ortel B., Hasan T., Römer A., Schnorr D., Loening S.A., Lein M. Plasma matrix metalloproteinase 9 as biomarker of prostate cancer progression in Dunning (Copenhagen) rats. Prostate. 2003;54:206–211. doi: 10.1002/pros.10183. [DOI] [PubMed] [Google Scholar]
- 68.Jung K., Nowak L., Lein M., Priem F., Schnorr D., Loening S.A. Matrix metalloproteinases 1 and 3, tissue inhibitor of metalloproteinase-1 and the complex of metalloproteinase-1/tissue inhibitor in plasma of patients with prostate cancer. Int. J. Cancer. 1997;74:220–223. doi: 10.1002/(SICI)1097-0215(19970422)74:2<220::AID-IJC14>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 69.Jurasz P., North S., Venner P., Radomski M.W. Matrix metalloproteinase-2 contributes to increased platelet reactivity in patients with metastatic prostate cancer: A preliminary study. Thromb. Res. 2003;112:59–64. doi: 10.1016/j.thromres.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 70.Kalantari E., Abolhasani M., Roudi R., Farajollahi M.M., Farhad S., Madjd Z., Askarian-Amiri S., Mohsenzadegan M. Co-expression of TLR-9 and MMP-13 is associated with the degree of tumour differentiation in prostate cancer. Int. J. Exp. Pathol. 2019;100:123–132. doi: 10.1111/iep.12314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kaminski A., Hahne J.C., Haddouti E.-M., Florin A., Wellmann A., Wernert N. Tumour-stroma interactions between metastatic prostate cancer cells and fibroblasts. Int. J. Mol. Med. 2006;18:941–950. doi: 10.3892/ijmm.18.5.941. [DOI] [PubMed] [Google Scholar]
- 72.Kanoh Y., Akahoshi T., Ohara T., Ohtani N., Mashiko T., Ohtani S., Egawa S., Baba S. Expression of matrix metalloproteinase-2 and prostate-specific antigen in localized and metastatic prostate cancer. Anticancer Res. 2002;22:1813–1817. [PubMed] [Google Scholar]
- 73.Knox J.D., Wolf C., McDaniel K., Clark V., Loriot M., Bowden G.T., Nagle R.B. Matrilysin expression in human prostate carcinoma. Mol. Carcinog. 1996;15:57–63. doi: 10.1002/(SICI)1098-2744(199601)15:1<57::AID-MC8>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 74.Koshida K., Konaka H., Imao T., Egawa M., Mizokami A., Namiki M. Comparison of two in vivo models for prostate cancer: Orthotopic and intratesticular inoculation of LNCaP or PC-3 cells. Int. J. Urol. 2004;11:1114–1121. doi: 10.1111/j.1442-2042.2004.00961.x. [DOI] [PubMed] [Google Scholar]
- 75.Kuniyasu H., Troncoso P., Johnston D., Bucana C.D., Tahara E., Fidler I.J., Pettaway C.A. Relative expression of type IV Collagenase, E-cadherin, and vascular endothelial growth factor/vascular permeability factor in prostatectomy specimens distinguishes organ-confined from pathologically advanced prostate cancers. Clin. Cancer Res. 2000;6:2295–2308. [PubMed] [Google Scholar]
- 76.Kuniyasu H., Ukai R., Johnston D., Troncoso P., Fidler I.J., Pettaway C.A. The relative mRNA expression levels of matrix metalloproteinase to E-cadherin in prostate biopsy specimens distinguishes organ-confined from advanced prostate cancer at radical prostatectomy. Clin. Cancer Res. 2003;9:2185–2194. [PubMed] [Google Scholar]
- 77.Larsson P., Syed Khaja A.S., Semenas J., Wang T., Sarwar M., Dizeyi N., Simoulis A., Hedblom A., Wai S.N., Ødum N., et al. The functional interlink between AR and MMP9/VEGF signaling axis is mediated through PIP5K1α/pAKT in prostate cancer. Int. J. Cancer. 2020;146:1686–1699. doi: 10.1002/ijc.32607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Latil A., Bièche I., Chêne L., Laurendeau I., Berthon P., Cussenot O., Vidaud M. Gene expression profiling in clinically localized prostate cancer: A four-gene expression model predicts clinical behavior. Clin. Cancer Res. 2003;9:5477–5485. [PubMed] [Google Scholar]
- 79.Lein M., Nowak L., Jung K., Laube C., Ulbricht N., Schnorr D., Loening S.A. Metalloproteinases and tissue inhibitors of matrix-metalloproteinases in plasma of patients with prostate cancer and in prostate cancer tissue. Ann. N. Y. Acad. Sci. 1999;878:544–546. doi: 10.1111/j.1749-6632.1999.tb07722.x. [DOI] [PubMed] [Google Scholar]
- 80.Leshner M., Devine M., Roloff G.W., True L.D., Misteli T., Meaburn K.J. Locus-specific gene repositioning in prostate cancer. Mol. Biol. Cell. 2016;27:236–246. doi: 10.1091/mbc.e15-05-0280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liao C.H., Wu H.C., Hu P.S., Hsu S.W., Shen T.C., Hsia T.C., Chang W.S., Tsai C.W., Bau D.T. The association of matrix metalloproteinase-1 promoter polymorphisms with prostate cancer in Taiwanese patients. Anticancer Res. 2018;38:3907–3911. doi: 10.21873/anticanres.12675. [DOI] [PubMed] [Google Scholar]
- 82.Lichtinghagen R., Musholt P.B., Lein M., Römer A., Rudolph B., Kristiansen G., Hauptmann S., Schnorr D., Loening S.A., Jung K. Different mRNA and protein expression of matrix metalloproteinases 2 and 9 and tissue inhibitor of metalloproteinases 1 in benign and malignant prostate tissue. Eur. Urol. 2002;42:398–406. doi: 10.1016/S0302-2838(02)00324-X. [DOI] [PubMed] [Google Scholar]
- 83.Lichtinghagen R., Musholt P.B., Stephan C., Lein M., Kristiansen G., Hauptmann S., Rudolph B., Schnorr D., Loening S.A., Jung K. mRNA expression profile of matrix metalloproteinases and their tissue inhibitors in malignant and non-malignant prostatic tissue. Anticancer Res. 2003;23:2617–2624. [PubMed] [Google Scholar]
- 84.Littlepage L.E., Sternlicht M.D., Rougier N., Phillips J., Gallo E., Yu Y., Williams K., Brenot A., Gordon J.I., Werb Z. Matrix metalloproteinases contribute distinct roles in neuroendocrine prostate carcinogenesis, metastasis, and angiogenesis progression. Cancer Res. 2010;70:2224–2234. doi: 10.1158/0008-5472.CAN-09-3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu B., Gu X., Huang T., Luan Y., Ding X. Identification of TMPRSS2-ERG mechanisms in prostate cancer invasiveness: Involvement of MMP-9 and plexin B1. Oncol. Rep. 2017;37:201–208. doi: 10.3892/or.2016.5277. [DOI] [PubMed] [Google Scholar]
- 86.Lokeshwar B.L., Selzer M.G., Block N.L., Gunja-Smith Z. Secretion of matrix metalloproteinases and their inhibitors (tissue inhibitor of metalloproteinases) by human prostate in explant cultures: Reduced tissue inhibitor of metalloproteinase secretion by malignant tissues. Cancer Res. 1993;53:4493–4498. [PubMed] [Google Scholar]
- 87.London C.A., Sekhon H.S., Arora V., Stein D.A., Iversen P.L., Devi G.R. A novel antisense inhibitor of MMP-9 attenuates angiogenesis, human prostate cancer cell invasion and tumorigenicity. Cancer Gene Ther. 2003;10:823–832. doi: 10.1038/sj.cgt.7700642. [DOI] [PubMed] [Google Scholar]
- 88.Lynch C.C., Hikosaka A., Acuff H.B., Martin M.D., Kawai N., Singh R.K., Vargo-Gogola T.C., Begtrup J.L., Peterson T.E., Fingleton B., et al. MMP-7 promotes prostate cancer-induced osteolysis via the solubilization of RANKL. Cancer Cell. 2005;7:485–496. doi: 10.1016/j.ccr.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 89.Marín-Aguilera M., Reig Ò., Lozano J.J., Jiménez N., García-Recio S., Erill N., Gaba L., Tagliapietra A., Ortega V., Carrera G., et al. Molecular profiling of peripheral blood is associated with circulating tumor cells content and poor survival in metastatic castration-resistant prostate cancer. Oncotarget. 2015;6:10604–10616. doi: 10.18632/oncotarget.3550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Maruta S., Miyata Y., Sagara Y., Kanda S., Iwata T., Watanabe S.-i., Sakai H., Hayashi T., Kanetake H. Expression of matrix metalloproteinase-10 in non-metastatic prostate cancer: Correlation with an imbalance in cell proliferation and apoptosis. Oncol. Lett. 2010;1:417–421. doi: 10.3892/ol_00000073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Medina-González A., Eiró-Díaz N., Fernández-Gómez J.M., Ovidio-González L., Jalón-Monzón A., Casas-Nebra J., Escaf-Barmadah S. Comparative analysis of the expression of metalloproteases (MMP-2, MMP-9, MMP-11 and MMP-13) and the tissue inhibitor of metalloprotease 3 (TIMP-3) between previous negative biopsies and radical prostatectomies. Actas Urol. Esp. 2020;44:78–85. doi: 10.1016/j.acuro.2019.10.004. [DOI] [PubMed] [Google Scholar]
- 92.Miyake H., Muramaki M., Kurahashi T., Takenaka A., Fujisawa M. Expression of potential molecular markers in prostate cancer: Correlation with clinicopathological outcomes in patients undergoing radical prostatectomy. Urol. Oncol. 2010;28:145–151. doi: 10.1016/j.urolonc.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 93.Monfironi R., Fabris G., Lucarini G., Biagini G. Location of 72-kd metalloproteinase (Type IV Collagenase) in untreated prostatic adenocarcinoma. Pathol. Res. Pract. 1995;191:1140–1146. doi: 10.1016/S0344-0338(11)80659-X. [DOI] [PubMed] [Google Scholar]
- 94.Montironi R., Lucarini G., Castaldini C., Galluzzi C.M., Biagini G., Fabris G. Immunohistochemical evaluation of type IV collagenase (72-kd metalloproteinase) in prostatic intraepithelial neoplasia. Anticancer Res. 1996;16:2057–2062. [PubMed] [Google Scholar]
- 95.Morgia G., Falsaperla M., Malaponte G., Madonia M., Indelicato M., Travali S., Mazzarino M.C. Matrix metalloproteinases as diagnostic (MMP-13) and prognostic (MMP-2, MMP-9) markers of prostate cancer. Urol. Res. 2005;33:44–50. doi: 10.1007/s00240-004-0440-8. [DOI] [PubMed] [Google Scholar]
- 96.Moses M.A., Wiederschain D., Loughlin K.R., Zurakowski D., Lamb C.C., Freeman M.R. Increased incidence of matrix metalloproteinases in urine of cancer patients. Cancer Res. 1998;58:1395–1399. [PubMed] [Google Scholar]
- 97.Muñoz D., Serrano M.K., Hernandez M.E., Haller R., Swanson T., Slaton J.W., Sinha A.A., Wilson M.J. Matrix metalloproteinase and heparin-stimulated serine proteinase activities in post-prostate massage urine of men with prostate cancer. Exp. Mol. Pathol. 2017;103:300–305. doi: 10.1016/j.yexmp.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 98.Nabha S.M., Bonfil R.D., Yamamoto H.A., Belizi A., Wiesner C., Dong Z., Cher M.L. Host matrix metalloproteinase-9 contributes to tumor vascularization without affecting tumor growth in a model of prostate cancer bone metastasis. Clin. Exp. Metastasis. 2006;23:335. doi: 10.1007/s10585-006-9042-x. [DOI] [PubMed] [Google Scholar]
- 99.Nagle R.B., Knox J.D., Wolf C., Bowden G.T., Cress A.E. Adhesion molecules, extracellular matrix, and proteases in prostate carcinoma. J. Cell Biochem. Suppl. 1994;19:232–237. [PubMed] [Google Scholar]
- 100.Nalla A.K., Gorantla B., Gondi C.S., Lakka S.S., Rao J.S. Targeting MMP-9, uPAR, and cathepsin B inhibits invasion, migration and activates apoptosis in prostate cancer cells. Cancer Gene Ther. 2010;17:599–613. doi: 10.1038/cgt.2010.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Neuhaus J., Schiffer E., Mannello F., Horn L.-C., Ganzer R., Stolzenburg J.-U. Protease expression levels in prostate cancer tissue can explain prostate cancer-associated seminal biomarkers-an explorative concept study. Int. J. Mol. Sci. 2017;18:976. doi: 10.3390/ijms18050976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Oguić R., Mozetič V., Cini Tešar E., Fučkar Čupić D., Mustać E., Dorđević G. Matrix metalloproteinases 2 and 9 immunoexpression in prostate carcinoma at the positive margin of radical prostatectomy specimens. Pathol. Res. Int. 2014;2014:262195. doi: 10.1155/2014/262195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ok Atılgan A., Özdemir B.H., Yılmaz Akçay E., Tepeoğlu M., Börcek P., Dirim A. Association between focal adhesion kinase and matrix metalloproteinase-9 expression in prostate adenocarcinoma and their influence on the progression of prostatic adenocarcinoma. Ann. Diagn. Pathol. 2020;45:151480. doi: 10.1016/j.anndiagpath.2020.151480. [DOI] [PubMed] [Google Scholar]
- 104.Ouyang X.S., Wang X., Lee D.T., Tsao S.W., Wong Y.C. Up-regulation of TRPM-2, MMP-7 and ID-1 during sex hormone-induced prostate carcinogenesis in the Noble rat. Carcinogenesis. 2001;22:965–973. doi: 10.1093/carcin/22.6.965. [DOI] [PubMed] [Google Scholar]
- 105.Ozden F., Saygin C., Uzunaslan D., Onal B., Durak H., Aki H. Expression of MMP-1, MMP-9 and TIMP-2 in prostate carcinoma and their influence on prognosis and survival. J. Cancer Res. Clin. Oncol. 2013;139:1373–1382. doi: 10.1007/s00432-013-1453-x. [DOI] [PubMed] [Google Scholar]
- 106.Pajouh M.S., Nagle R.B., Breathnach R., Finch J.S., Brawer M.K., Bowden G.T. Expression of metalloproteinase genes in human prostate cancer. J. Cancer Res. Clin. Oncol. 1991;117:144–150. doi: 10.1007/BF01613138. [DOI] [PubMed] [Google Scholar]
- 107.Pang S.T., Flores-Morales A., Skoog L., Chuan Y.C., Nordstedt G., Pousette A. Regulation of matrix metalloproteinase 13 expression by androgen in prostate cancer. Oncol. Rep. 2004;11:1187–1192. doi: 10.3892/or.11.6.1187. [DOI] [PubMed] [Google Scholar]
- 108.Pettaway C.A., Song R., Wang X., Sanchez-Ortiz R., Spiess P.E., Strom S., Troncoso P. The ratio of matrix metalloproteinase to E-cadherin expression: A pilot study to assess mRNA and protein expression among African American prostate cancer patients. Prostate. 2008;68:1467–1476. doi: 10.1002/pros.20812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pouyanfar N., Monabbati A., Sharifi A.A., Dianatpour M. Expression levels of MMP9 and PIWIL2 in prostate cancer: A case-control study. Clin. Lab. 2016;62:651–657. doi: 10.7754/Clin.Lab.2015.150817. [DOI] [PubMed] [Google Scholar]
- 110.Powell W.C., Knox J.D., Navre M., Grogan T.M., Kittelson J., Nagle R.B., Bowden G.T. Expression of the metalloproteinase matrilysin in DU-145 cells increases their invasive potential in severe combined immunodeficient mice. Cancer Res. 1993;53:417–422. [PubMed] [Google Scholar]
- 111.Prior C., Guillen-Grima F., Robles J.E., Rosell D., Fernandez-Montero J.M., Agirre X., Catena R., Calvo A. Use of a combination of biomarkers in serum and urine to improve detection of prostate cancer. World J. Urol. 2010;28:681–686. doi: 10.1007/s00345-010-0583-x. [DOI] [PubMed] [Google Scholar]
- 112.Reis S.T., Antunes A.A., Pontes-Junior J., Sousa-Canavez J.M.d., Dall’Oglio M.F., Piantino C.B., Cruz J.A.S.d., Morais D.R., Srougi M., Leite K.R.M. Underexpression of MMP-2 and its regulators, TIMP2, MT1-MMP and IL-8, is associated with prostate cancer. Int. Braz. J. Urol. 2012;38:167–174. doi: 10.1590/S1677-55382012000200004. [DOI] [PubMed] [Google Scholar]
- 113.Dos Reis S.T.d., Viana N.I., Iscaife A., Pontes-Junior J., Dip N., Antunes A.A., Guimarães V.R., Santana I., Nahas W.C., Srougi M., et al. Loss of TIMP-1 immune expression and tumor recurrence in localized prostate cancer. Int. Braz. J. Urol. 2015;41:1088–1095. doi: 10.1590/S1677-5538.IBJU.2014.0451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Reis S.T., Pontes-Junior J., Antunes A.A., de Sousa-Canavez J.M., Dall’Oglio M.F., Passerotti C.C., Abe D.K., Crippa A., da Cruz J.A., Timoszczuk L.M., et al. MMP-9 overexpression due to TIMP-1 and RECK underexpression is associated with prognosis in prostate cancer. Int. J. Biol. Markers. 2011;26:255–261. doi: 10.5301/JBM.2011.8831. [DOI] [PubMed] [Google Scholar]
- 115.Riddick A.C., Shukla C.J., Pennington C.J., Bass R., Nuttall R.K., Hogan A., Sethia K.K., Ellis V., Collins A.T., Maitland N.J., et al. Identification of degradome components associated with prostate cancer progression by expression analysis of human prostatic tissues. Br. J. Cancer. 2005;92:2171–2180. doi: 10.1038/sj.bjc.6602630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ross J.S., Kaur P., Sheehan C.E., Fisher H.A.G., Kaufman R.A., Kallakury B.V.S. Prognostic significance of matrix metalloproteinase 2 and tissue inhibitor of metalloproteinase 2 expression in prostate cancer. Mod. Pathol. 2003;16:198–205. doi: 10.1097/01.MP.0000056984.62360.6C. [DOI] [PubMed] [Google Scholar]
- 117.Sakai I., Harada K.-I., Hara I., Eto H., Miyake H. A comparison of the biological features between prostate cancers arising in the transition and peripheral zones. BJU Int. 2005;96:528–532. doi: 10.1111/j.1464-410X.2005.05678.x. [DOI] [PubMed] [Google Scholar]
- 118.San Francisco I.F., DeWolf W.C., Peehl D.M., Olumi A.F. Expression of transforming growth factor-beta 1 and growth in soft agar differentiate prostate carcinoma-associated fibroblasts from normal prostate fibroblasts. Int. J. Cancer. 2004;112:213–218. doi: 10.1002/ijc.20388. [DOI] [PubMed] [Google Scholar]
- 119.Sauer C.G., Kappeler A., Späth M., Kaden J.J., Michel M.S., Mayer D., Bleyl U., Grobholz R. Expression and activity of matrix metalloproteinases-2 and -9 in serum, core needle biopsies and tissue specimens of prostate cancer patients. Virchows Archiv. 2004;444:518–526. doi: 10.1007/s00428-004-1016-2. [DOI] [PubMed] [Google Scholar]
- 120.Schäfer S., Weibel S., Donat U., Zhang Q., Aguilar R.J., Chen N.G., Szalay A.A. Vaccinia virus-mediated intra-tumoral expression of matrix metalloproteinase 9 enhances oncolysis of PC-3 xenograft tumors. BMC Cancer. 2012;12:366. doi: 10.1186/1471-2407-12-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Schveigert D., Valuckas K.P., Kovalcis V., Ulys A., Chvatovic G., Didziapetriene J. Significance of MMP-9 expression and MMP-9 polymorphism in prostate cancer. Tumori. 2013;99:523–529. doi: 10.1177/030089161309900414. [DOI] [PubMed] [Google Scholar]
- 122.Sehgal G., Hua J., Bernhard E.J., Sehgal I., Thompson T.C., Muschel R.J. Requirement for matrix metalloproteinase-9 (gelatinase B) expression in metastasis by murine prostate carcinoma. Am. J. Pathol. 1998;152:591–596. [PMC free article] [PubMed] [Google Scholar]
- 123.Sehgal I., Forbes K., Webb M.A. Reduced secretion of MMPs, plasminogen activators and TIMPS from prostate cancer cells derived by repeated metastasis. Anticancer Res. 2003;23:39–42. [PubMed] [Google Scholar]
- 124.Serretta V., Abrate A., Siracusano S., Gesolfo C.S., Vella M., Di Maida F., Cangemi A., Cicero G., Barresi E., Sanfilippo C. Clinical and biochemical markers of visceral adipose tissue activity: Body mass index, visceral adiposity index, leptin, adiponectin, and matrix metalloproteinase-3. Correlation with Gleason patterns 4 and 5 at prostate biopsy. Urol Ann. 2018;10:280–286. doi: 10.4103/UA.UA_188_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sfar S., Saad H., Mosbah F., Gabbouj S., Chouchane L. TSP1 and MMP9 genetic variants in sporadic prostate cancer. Cancer Genet. Cytogenet. 2007;172:38–44. doi: 10.1016/j.cancergencyto.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 126.Sfar S., Saad H., Mosbah F., Chouchane L. Combined effects of the angiogenic genes polymorphisms on prostate cancer susceptibility and aggressiveness. Mol. Biol. Rep. 2009;36:37–45. doi: 10.1007/s11033-007-9149-4. [DOI] [PubMed] [Google Scholar]
- 127.Shah T., Wildes F., Kakkad S., Artemov D., Bhujwalla Z.M. Lymphatic endothelial cells actively regulate prostate cancer cell invasion. NMR Biomed. 2016;29:904–911. doi: 10.1002/nbm.3543. [DOI] [PubMed] [Google Scholar]
- 128.Shajarehpoor Salavati L., Tafvizi F., Manjili H.K. The association between MMP2 −1306 C > T (rs243865) polymorphism and risk of prostate cancer. Ir. J. Med. Sci. 2017;186:103–111. doi: 10.1007/s11845-016-1492-9. [DOI] [PubMed] [Google Scholar]
- 129.Shi T., Quek S.I., Gao Y., Nicora C.D., Nie S., Fillmore T.L., Liu T., Rodland K.D., Smith R.D., Leach R.J., et al. Multiplexed targeted mass spectrometry assays for prostate cancer-associated urinary proteins. Oncotarget. 2017;8:101887–101898. doi: 10.18632/oncotarget.21710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Silva M.M.d., Jr., Matheus W.E., Garcia P.V., Stopiglia R.M., Billis A., Ferreira U., Fávaro W.J. Characterization of reactive stroma in prostate cancer: Involvement of growth factors, metalloproteinase matrix, sexual hormones receptors and prostatic stem cells. Int. Braz. J. Urol. 2015;41:849–858. doi: 10.1590/S1677-5538.IBJU.2014.0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Srivastava P., Lone T.A., Kapoor R., Mittal R.D. Association of promoter polymorphisms in MMP2 and TIMP2 with prostate cancer susceptibility in North India. Arch. Med. Res. 2012;43:117–124. doi: 10.1016/j.arcmed.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 132.Stearns M., Stearns M.E. Evidence for increased activated metalloproteinase 2 (MMP-2a) expression associated with human prostate cancer progression. Oncol. Res. 1996;8:69–75. [PubMed] [Google Scholar]
- 133.Stearns M.E., Stearns M. Immunohistochemical studies of activated matrix metalloproteinase-2 (MMP-2a)expression in human prostate cancer. Oncol. Res. 1996;8:63–67. [PubMed] [Google Scholar]
- 134.Still K., Robson C.N., Autzen P., Robinson M.C., Hamdy F.C. Localization and quantification of mRNA for matrix metalloproteinase-2 (MMP-2) and tissue inhibitor of matrix metalloproteinase-2 (TIMP-2) in human benign and malignant prostatic tissue. Prostate. 2000;42:18–25. doi: 10.1002/(SICI)1097-0045(20000101)42:1<18::AID-PROS3>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 135.Szarvas T., Sevcenco S., Módos O., Keresztes D., Nyirády P., Csizmarik A., Ristl R., Puhr M., Hoffmann M.J., Niedworok C., et al. Matrix metalloproteinase 7, soluble Fas and Fas ligand serum levels for predicting docetaxel resistance and survival in castration-resistant prostate cancer. BJU Int. 2018;122:695–704. doi: 10.1111/bju.14415. [DOI] [PubMed] [Google Scholar]
- 136.Trudel D., Fradet Y., Meyer F., Harel F., Têtu B. Membrane-type-1 matrix metalloproteinase, matrix metalloproteinase 2, and tissue inhibitor of matrix proteinase 2 in prostate cancer: Identification of patients with poor prognosis by immunohistochemistry. Hum. Pathol. 2008;39:731–739. doi: 10.1016/j.humpath.2007.09.021. [DOI] [PubMed] [Google Scholar]
- 137.Trudel D., Fradet Y., Meyer F., Harel F., Têtu B. Significance of MMP-2 expression in prostate cancer: An Immunohistochemical Study. Cancer Res. 2003;63:8511–8515. [PubMed] [Google Scholar]
- 138.Trudel D., Fradet Y., Meyer F., Têtu B. Matrix metalloproteinase 9 is associated with Gleason score in prostate cancer but not with prognosis. Hum. Pathol. 2010;41:1694–1701. doi: 10.1016/j.humpath.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 139.Tsuchiya N., Narita S., Kumazawa T., Inoue T., Ma Z., Tsuruta H., Saito M., Horikawa Y., Yuasa T., Satoh S., et al. Clinical significance of a single nucleotide polymorphism and allelic imbalance of matrix metalloproteinase-1 promoter region in prostate cancer. Oncol. Rep. 2009;22:493–499. doi: 10.3892/or_00000462. [DOI] [PubMed] [Google Scholar]
- 140.Upadhyay J., Shekarriz B., Nemeth J.A., Dong Z., Cummings G.D., Fridman R., Sakr W., Grignon D.J., Cher M.L. Membrane type 1-matrix metalloproteinase (MT1-MMP) and MMP-2 immunolocalization in human prostate: Change in cellular localization associated with high-grade prostatic intraepithelial neoplasia. Clin. Cancer Res. 1999;5:4105–4110. [PubMed] [Google Scholar]
- 141.Vallbo C., Damber J.-E. Thrombospondins, metallo proteases and thrombospondin receptors messenger RNA and protein expression in different tumour sublines of the Dunning prostate cancer model. Acta Oncol. 2005;44:293–298. doi: 10.1080/02841860410002806. [DOI] [PubMed] [Google Scholar]
- 142.Wang J., Liu D., Zhou W., Wang M., Xia W., Tang Q. Prognostic value of matrix metalloprotease-1/protease-activated receptor-1 axis in patients with prostate cancer. Med. Oncol. 2014;31:968. doi: 10.1007/s12032-014-0968-6. [DOI] [PubMed] [Google Scholar]
- 143.Wiesner C., Bonfil R.D., Dong Z., Yamamoto H., Nabha S.M., Meng H., Saliganan A., Sabbota A., Cher M.L. Heterogeneous activation of MMP-9 due to prostate cancer-bone interaction. Urology. 2007;69:795–799. doi: 10.1016/j.urology.2007.01.093. [DOI] [PubMed] [Google Scholar]
- 144.Wilson M.J., Sellers R.G., Wiehr C., Melamud O., Pei D., Peehl D.M. Expression of matrix metalloproteinase-2 and -9 and their inhibitors, tissue inhibitor of metalloproteinase-1 and -2, in primary cultures of human prostatic stromal and epithelial cells. J. Cell Physiol. 2002;191:208–216. doi: 10.1002/jcp.10092. [DOI] [PubMed] [Google Scholar]
- 145.Wilson M.J., Sinha A.A. Plasminogen activator and metalloprotease activities of Du-145, PC-3, and 1-LN-PC-3-1A human prostate tumors grown in nude mice: Correlation with tumor invasive behavior. Cell Mol. Biol. Res. 1993;39:751–760. [PubMed] [Google Scholar]
- 146.Wood M., Fudge K., Mohler J.L., Frost A.R., Garcia F., Wang M., Stearns M.E. In situ hybridization studies of metalloproteinases 2 and 9 and TIMP-1 and TIMP-2 expression in human prostate cancer. Clin. Exp. Metastasis. 1997;15:246–258. doi: 10.1023/A:1018421431388. [DOI] [PubMed] [Google Scholar]
- 147.Xie Y., Lu W., Liu S., Yang Q., Goodwin J.S., Sathyanarayana S.A., Pratap S., Chen Z. MMP7 interacts with ARF in nucleus to potentiate tumor microenvironments for prostate cancer progression in vivo. Oncotarget. 2016;7:47609–47619. doi: 10.18632/oncotarget.10251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Xu D., McKee C.M., Cao Y., Ding Y., Kessler B.M., Muschel R.J. Matrix metalloproteinase-9 regulates tumor cell invasion through cleavage of protease nexin-1. Cancer Res. 2010;70:6988–6998. doi: 10.1158/0008-5472.CAN-10-0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yaykaşli K.O., Kayikçi M.A., Yamak N., Soğuktaş H., Düzenli S., Arslan A.O., Metın A., Kaya E., Hatıpoğlu Ö F. Polymorphisms in MMP-2 and TIMP-2 in Turkish patients with prostate cancer. Turk. J. Med. Sci. 2014;44:839–843. doi: 10.3906/sag-1305-63. [DOI] [PubMed] [Google Scholar]
- 150.Zellweger T., Ninck C., Bloch M., Mirlacher M., Koivisto P.A., Helin H.J., Mihatsch M.J., Gasser T.C., Bubendorf L. Expression patterns of potential therapeutic targets in prostate cancer. Int J. Cancer. 2005;113:619–628. doi: 10.1002/ijc.20615. [DOI] [PubMed] [Google Scholar]
- 151.Zhang J., Jung K., Lein M., Kristiansen G., Rudolph B., Hauptmann S., Schnorr D., Loening S.A., Lichtinghagen R. Differential expression of matrix metalloproteinases and their tissue inhibitors in human primary cultured prostatic cells and malignant prostate cell lines. Prostate. 2002;50:38–45. doi: 10.1002/pros.10030. [DOI] [PubMed] [Google Scholar]
- 152.Zhang L., Shi J., Feng J., Klocker H., Lee C., Zhang J. Type IV collagenase (matrix metalloproteinase-2 and -9) in prostate cancer. Prostate Cancer Prostatic Dis. 2004;7:327–332. doi: 10.1038/sj.pcan.4500750. [DOI] [PubMed] [Google Scholar]
- 153.Zhang S., Qi L., Li M., Zhang D., Xu S., Wang N., Sun B. Chemokine CXCL12 and its receptor CXCR4 expression are associated with perineural invasion of prostate cancer. J. Exp. Clin. Cancer Res. 2008;27:62. doi: 10.1186/1756-9966-27-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zhang S., Zheng C., Yao S., Wang Z., Xu L., Yang R., Meng X., Wu J., Zhou L., Sun Z. Proteomic analysis of human prostate cancer PC-3M-1E8 cells and PC-3M-2B4 cells of same origin but with different metastatic potential. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0206139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zhao Y.G., Xiao A.Z., Newcomer R.G., Park H.I., Kang T., Chung L.W., Swanson M.G., Zhau H.E., Kurhanewicz J., Sang Q.X. Activation of pro-gelatinase B by endometase/matrilysin-2 promotes invasion of human prostate cancer cells. J. Biol. Chem. 2003;278:15056–15064. doi: 10.1074/jbc.M210975200. [DOI] [PubMed] [Google Scholar]
- 156.Zhong W.D., Han Z.D., He H.C., Bi X.C., Dai Q.S., Zhu G., Ye Y.K., Liang Y.X., Qin W.J., Zhang Z., et al. CD147, MMP-1, MMP-2 and MMP-9 protein expression as significant prognostic factors in human prostate cancer. Oncology. 2008;75:230–236. doi: 10.1159/000163852. [DOI] [PubMed] [Google Scholar]
- 157.Zhu B., Block N.L., Lokeshwar B.L. Interaction between stromal cells and tumor cells induces chemoresistance and matrix metalloproteinase secretion. Ann. N. Y. Acad. Sci. 1999;878:642–646. doi: 10.1111/j.1749-6632.1999.tb07750.x. [DOI] [PubMed] [Google Scholar]
- 158.Cao J., Chiarelli C., Richman O., Zarrabi K., Kozarekar P., Zucker S. Membrane type 1 matrix metalloproteinase induces epithelial-to-mesenchymal transition in prostate cancer. J. Biol Chem. 2008;283:6232–6240. doi: 10.1074/jbc.M705759200. [DOI] [PubMed] [Google Scholar]
- 159.Bair E.L., Chen M.L., McDaniel K., Sekiguchi K., Cress A.E., Nagle R.B., Bowden G.T. Membrane type 1 matrix metalloprotease cleaves laminin-10 and promotes prostate cancer cell migration. Neoplasia. 2005;7:380–389. doi: 10.1593/neo.04619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sabbota A.L., Kim H.R., Zhe X., Fridman R., Bonfil R.D., Cher M.L. Shedding of RANKL by tumor-associated MT1-MMP activates Src-dependent prostate cancer cell migration. Cancer Res. 2010;70:5558–5566. doi: 10.1158/0008-5472.CAN-09-4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Nguyen H.L., Zucker S., Zarrabi K., Kadam P., Schmidt C., Cao J. Oxidative stress and prostate cancer progression are elicited by membrane-type 1 matrix metalloproteinase. Mol. Cancer Res. 2011;9:1305–1318. doi: 10.1158/1541-7786.MCR-11-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zarrabi K., Dufour A., Li J., Kuscu C., Pulkoski-Gross A., Zhi J., Hu Y., Sampson N.S., Zucker S., Cao J. Inhibition of matrix metalloproteinase 14 (MMP-14)-mediated cancer cell migration. J. Biol. Chem. 2011;286:33167–33177. doi: 10.1074/jbc.M111.256644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bonfil R.D., Dong Z., Trindade Filho J.C., Sabbota A., Osenkowski P., Nabha S., Yamamoto H., Chinni S.R., Zhao H., Mobashery S., et al. Prostate cancer-associated membrane type 1-matrix metalloproteinase: A pivotal role in bone response and intraosseous tumor growth. Am. J. Pathol. 2007;170:2100–2111. doi: 10.2353/ajpath.2007.060720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Wang X., Wilson M.J., Slaton J.W., Sinha A.A., Ewing S.L., Pei D. Increased aggressiveness of human prostate PC-3 tumor cells expressing cell surface localized membrane type-1 matrix metalloproteinase (MT1-MMP) J. Androl. 2009;30:259–274. doi: 10.2164/jandrol.108.006494. [DOI] [PubMed] [Google Scholar]
- 165.Cheng T., Li F., Wei R., Lv M.Q., Zhou Y., Dai Y., Yuan Y., Jiang G.Y., Ma D., Gao Q.L. MMP26: A potential biomarker for prostate cancer. J. Huazhong Univ. Sci. Technol. Med. Sci. 2017;37:891–894. doi: 10.1007/s11596-017-1823-8. [DOI] [PubMed] [Google Scholar]
- 166.Chu J.H., Sun Z.Y., Meng X.L., Wu J.H., He G.L., Liu G.M., Jiang X.R. Differential metastasis-associated gene analysis of prostate carcinoma cells derived from primary tumor and spontaneous lymphatic metastasis in nude mice with orthotopic implantation of PC-3M cells. Cancer Lett. 2006;233:79–88. doi: 10.1016/j.canlet.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 167.Jiang C., Wang J., Dong C., Wei W., Li J., Li X. Membranous type matrix metalloproteinase 16 induces human prostate cancer metastasis. Oncol. Lett. 2017;14:3096–3102. doi: 10.3892/ol.2017.6536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Jung M., Römer A., Keyszer G., Lein M., Kristiansen G., Schnorr D., Loening S.A., Jung K. mRNA expression of the five membrane-type matrix metalloproteinases MT1–MT5 in human prostatic cell lines and their down-regulation in human malignant prostatic tissue. Prostate. 2003;55:89–98. doi: 10.1002/pros.10194. [DOI] [PubMed] [Google Scholar]
- 169.Khamis Z.I., Iczkowski K.A., Man Y.-G., Bou-Dargham M.J., Sang Q.-X.A. Evidence for a proapoptotic role of matrix metalloproteinase-26 in human prostate cancer cells and tissues. J. Cancer. 2016;7:80–87. doi: 10.7150/jca.13067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lee S., Desai K.K., Iczkowski K.A., Newcomer R.G., Wu K.J., Zhao Y.-G., Tan W.W., Roycik M.D., Sang Q.-X.A. Coordinated peak expression of MMP-26 and TIMP-4 in preinvasive human prostate tumor. Cell Res. 2006;16:750–758. doi: 10.1038/sj.cr.7310089. [DOI] [PubMed] [Google Scholar]
- 171.Lin H.Y., Amankwah E.K., Tseng T.-S., Qu X., Chen D.-T., Park J.Y. SNP-SNP interaction network in angiogenesis genes associated with prostate cancer aggressiveness. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0059688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lin H.Y., Cheng C.H., Chen D.T., Chen Y.A., Park J.Y. Coexpression and expression quantitative trait loci analyses of the angiogenesis gene-gene interaction network in prostate cancer. Transl. Cancer Res. 2016;5 doi: 10.21037/tcr.2016.10.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Liu G., Atteridge C.L., Wang X., Lundgren A.D., Wu J.D. Cutting edge: The membrane type matrix metalloproteinase MMP14 mediates constitutive shedding of MHC Class I chain-related molecule a independent of a disintegrin and metalloproteinases. J. Immunol. 2010;184:3346–3350. doi: 10.4049/jimmunol.0903789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Nagakawa O., Murakami K., Yamaura T., Fujiuchi Y., Murata J., Fuse H., Saiki I. Expression of membrane-type 1 matrix metalloproteinase (MT1-MMP) on prostate cancer cell lines. Cancer Lett. 2000;155:173–179. doi: 10.1016/S0304-3835(00)00425-0. [DOI] [PubMed] [Google Scholar]
- 175.Sroka I.C., McDaniel K., Nagle R.B., Bowden G.T. Differential localization of MT1-MMP in human prostate cancer tissue: Role of IGF-1R in MT1-MMP expression. Prostate. 2008;68:463–476. doi: 10.1002/pros.20718. [DOI] [PubMed] [Google Scholar]
- 176.Udayakumar T.S., Chen M.L., Bair E.L., Von Bredow D.C., Cress A.E., Nagle R.B., Bowden G.T. Membrane type-1-matrix metalloproteinase expressed by prostate carcinoma cells cleaves human laminin-5 beta3 chain and induces cell migration. Cancer Res. 2003;63:2292–2299. [PubMed] [Google Scholar]
- 177.Liu A.Y., Zhang H.U.I., Sorensen C.M., Diamond D.L. Analysis of prostate cancer by proteomics using tissue specimens. J. Urol. 2005;173:73–78. doi: 10.1097/01.ju.0000146543.33543.a3. [DOI] [PubMed] [Google Scholar]
- 178.Ashida S., Nakagawa H., Katagiri T., Furihata M., Iiizumi M., Anazawa Y., Tsunoda T., Takata R., Kasahara K., Miki T., et al. Molecular features of the transition from prostatic intraepithelial neoplasia (PIN) to prostate cancer: Genome-wide gene-expression profiles of prostate cancers and PINs. Cancer Res. 2004;64:5963–5972. doi: 10.1158/0008-5472.CAN-04-0020. [DOI] [PubMed] [Google Scholar]
- 179.Kim Y., Ignatchenko V., Yao C.Q., Kalatskaya I., Nyalwidhe J.O., Lance R.S., Gramolini A.O., Troyer D.A., Stein L.D., Boutros P.C., et al. Identification of differentially expressed proteins in direct expressed prostatic secretions of men with organ-confined versus extracapsular prostate cancer. Mol. Cell Proteomics. 2012;11:1870–1884. doi: 10.1074/mcp.M112.017889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Stearns M.E., Wang M., Stearns M. IL-10 blocks collagen IV invasion by "invasion stimulating factor" activated PC-3 ML cells: Upregulation of TIMP-1 expression. Oncol. Res. 1995;7:157–163. [PubMed] [Google Scholar]
- 181.Adissu H.A., McKerlie C., Di Grappa M., Waterhouse P., Xu Q., Fang H., Khokha R., Wood G.A. Timp3 loss accelerates tumour invasion and increases prostate inflammation in a mouse model of prostate cancer. Prostate. 2015;75:1831–1843. doi: 10.1002/pros.23056. [DOI] [PubMed] [Google Scholar]
- 182.Baker T., Tickle S., Wasan H., Docherty A., Isenberg D., Waxman J. Serum metalloproteinases and their inhibitors: Markers for malignant potential. Br. J. Cancer. 1994;70:506–512. doi: 10.1038/bjc.1994.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Deng X., Bhagat S., Dong Z., Mullins C., Chinni S.R., Cher M. Tissue inhibitor of metalloproteinase-3 induces apoptosis in prostate cancer cells and confers increased sensitivity to paclitaxel. Eur. J. Cancer. 2006;42:3267–3273. doi: 10.1016/j.ejca.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 184.Gong Y., Chippada-Venkata U.D., Galsky M.D., Huang J., Oh W.K. Elevated circulating tissue inhibitor of metalloproteinase 1 (TIMP-1) levels are associated with neuroendocrine differentiation in castration resistant prostate cancer. Prostate. 2015;75:616–627. doi: 10.1002/pros.22945. [DOI] [PubMed] [Google Scholar]
- 185.Gustavsson H., Jennbacken K., Welén K., Damber J.-E. Altered expression of genes regulating angiogenesis in experimental androgen-independent prostate cancer. Prostate. 2008;68:161–170. doi: 10.1002/pros.20672. [DOI] [PubMed] [Google Scholar]
- 186.Hoque M.O., Topaloglu O., Begum S., Henrique R., Rosenbaum E., Criekinge W.V., Westra W.H., Sidransky D. Quantitative methylation-specific polymerase chain reaction gene patterns in urine sediment distinguish prostate cancer patients from control subjects. J. Clin. Oncol. 2005;23:6569–6575. doi: 10.1200/JCO.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 187.Jerónimo C., Henrique R., Hoque M.O., Mambo E., Ribeiro F.R., Varzim G., Oliveira J., Teixeira M.R., Lopes C., Sidransky D. A quantitative promoter methylation profile of prostate cancer. Clin. Cancer Res. 2004;10:8472–8478. doi: 10.1158/1078-0432.CCR-04-0894. [DOI] [PubMed] [Google Scholar]
- 188.Kamińska K., Białkowska A., Kowalewski J., Huang S., Lewandowska M.A. Differential gene methylation patterns in cancerous and non-cancerous cells. Oncol. Rep. 2019;42:43–54. doi: 10.3892/or.2019.7159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Karan D., Lin F.C., Bryan M., Ringel J., Moniaux N., Lin M.F., Batra S.K. Expression of ADAMs (a disintegrin and metalloproteases) and TIMP-3 (tissue inhibitor of metalloproteinase-3) in human prostatic adenocarcinomas. Int. J. Oncol. 2003;23:1365–1371. doi: 10.3892/ijo.23.5.1365. [DOI] [PubMed] [Google Scholar]
- 190.Kuefer R., Day K.C., Kleer C.G., Sabel M.S., Hofer M.D., Varambally S., Zorn C.S., Chinnaiyan A.M., Rubin M.A., Day M.L. ADAM15 disintegrin is associated with aggressive prostate and breast cancer disease. Neoplasia. 2006;8:319–329. doi: 10.1593/neo.05682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Kwabi-Addo B., Wang S., Chung W., Jelinek J., Patierno S.R., Wang B.-D., Andrawis R., Lee N.H., Apprey V., Issa J.-P., et al. Identification of differentially methylated genes in normal prostate tissues from African American and Caucasian men. Clin. Cancer Res. 2010;16:3539–3547. doi: 10.1158/1078-0432.CCR-09-3342. [DOI] [PubMed] [Google Scholar]
- 192.Lee M.-S., Jung J.-I., Kwon S.-H., Lee S.-M., Morita K., Her S. TIMP-2 fusion protein with human serum albumin potentiates anti-angiogenesis-mediated inhibition of tumor growth by suppressing MMP-2 expression. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0035710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Oh W.K., Vargas R., Jacobus S., Leitzel K., Regan M.M., Hamer P., Pierce K., Brown-Shimer S., Carney W., Ali S.M., et al. Elevated plasma tissue inhibitor of metalloproteinase-1 levels predict decreased survival in castration-resistant prostate cancer patients. Cancer. 2011;117:517–525. doi: 10.1002/cncr.25394. [DOI] [PubMed] [Google Scholar]
- 194.Pulukuri S.M., Patibandla S., Patel J., Estes N., Rao J.S. Epigenetic inactivation of the tissue inhibitor of metalloproteinase-2 (TIMP-2) gene in human prostate tumors. Oncogene. 2007;26:5229–5237. doi: 10.1038/sj.onc.1210329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Ross R.W., Galsky M.D., Scher H.I., Magidson J., Wassmann K., Lee G.S., Katz L., Subudhi S.K., Anand A., Fleisher M., et al. A whole-blood RNA transcript-based prognostic model in men with castration-resistant prostate cancer: A prospective study. Lancet Oncol. 2012;13:1105–1113. doi: 10.1016/S1470-2045(12)70263-2. [DOI] [PubMed] [Google Scholar]
- 196.Shinojima T., Yu Q., Huang S.K., Li M., Mizuno R., Liu E.T., Hoon D.S., Lessard L. Heterogeneous epigenetic regulation of TIMP3 in prostate cancer. Epigenetics. 2012;7:1279–1289. doi: 10.4161/epi.22333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Yamanaka M., Watanabe M., Yamada Y., Takagi A., Murata T., Takahashi H., Suzuki H., Ito H., Tsukino H., Katoh T., et al. Altered methylation of multiple genes in carcinogenesis of the prostate. Int. J. Cancer. 2003;106:382–387. doi: 10.1002/ijc.11227. [DOI] [PubMed] [Google Scholar]
- 198.Zhang L., Zhao L., Zhao D., Lin G., Guo B., Li Y., Liang Z., Zhao X.J., Fang X. Inhibition of tumor growth and induction of apoptosis in prostate cancer cell lines by overexpression of tissue inhibitor of matrix metalloproteinase-3. Cancer Gene Ther. 2010;17:171–179. doi: 10.1038/cgt.2009.59. [DOI] [PubMed] [Google Scholar]
- 199.Burdelski C., Fitzner M., Hube-Magg C., Kluth M., Heumann A., Simon R., Krech T., Clauditz T., Büscheck F., Steurer S., et al. Overexpression of the a disintegrin and metalloproteinase ADAM15 is linked to a small but highly aggressive subset of prostate cancers. Neoplasia. 2017;19:279–287. doi: 10.1016/j.neo.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Najy A.J., Day K.C., Day M.L. ADAM15 supports prostate cancer metastasis by modulating tumor cell–endothelial cell interaction. Cancer Res. 2008;68:1092–1099. doi: 10.1158/0008-5472.CAN-07-2432. [DOI] [PubMed] [Google Scholar]
- 201.Lin P., Sun X., Feng T., Zou H., Jiang Y., Liu Z., Zhao D., Yu X. ADAM17 regulates prostate cancer cell proliferation through mediating cell cycle progression by EGFR/PI3K/AKT pathway. Mol. Cell Biochem. 2012;359:235–243. doi: 10.1007/s11010-011-1018-8. [DOI] [PubMed] [Google Scholar]
- 202.Xiao L.-J., Lin P., Lin F., Liu X., Qin W., Zou H.-F., Guo L., Liu W., Wang S.-J., Yu X.-G. ADAM17 targets MMP-2 and MMP-9 via EGFR-MEK-ERK pathway activation to promote prostate cancer cell invasion. Int. J. Oncol. 2012;40:1714–1724. doi: 10.3892/ijo.2011.1320. [DOI] [PubMed] [Google Scholar]
- 203.Rudnicka C., Mochizuki S., Okada Y., McLaughlin C., Leedman P.J., Stuart L., Epis M., Hoyne G., Boulos S., Johnson L., et al. Overexpression and knock-down studies highlight that a disintegrin and metalloproteinase 28 controls proliferation and migration in human prostate cancer. Medicine. 2016;95 doi: 10.1097/MD.0000000000005085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Arima T., Enokida H., Kubo H., Kagara I., Matsuda R., Toki K., Nishimura H., Chiyomaru T., Tatarano S., Idesako T., et al. Nuclear translocation of ADAM-10 contributes to the pathogenesis and progression of human prostate cancer. Cancer Sci. 2007;98:1720–1726. doi: 10.1111/j.1349-7006.2007.00601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Bilgin Doğru E., Dizdar Y., Akşit E., Ural F., Şanlı Ö., Yasasever V. EMMPRIN and ADAM12 in prostate cancer: Preliminary results of a prospective study. Tumour Biol. 2014;35:11647–11653. doi: 10.1007/s13277-014-2514-8. [DOI] [PubMed] [Google Scholar]
- 206.Fritzsche F.R., Jung M., Xu C., Rabien A., Schicktanz H., Stephan C., Dietel M., Jung K., Kristiansen G. ADAM8 expression in prostate cancer is associated with parameters of unfavorable prognosis. Virchows Archiv. 2006;449:628–636. doi: 10.1007/s00428-006-0315-1. [DOI] [PubMed] [Google Scholar]
- 207.Fritzsche F.R., Jung M., Tölle A., Wild P., Hartmann A., Wassermann K., Rabien A., Lein M., Dietel M., Pilarsky C., et al. ADAM9 expression is a significant and independent prognostic marker of PSA relapse in prostate cancer. Eur. Urol. 2008;54:1097–1108. doi: 10.1016/j.eururo.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 208.Hoyne G., Rudnicka C., Sang Q.-X., Roycik M., Howarth S., Leedman P., Schlaich M., Candy P., Matthews V. Genetic and cellular studies highlight that a disintegrin and metalloproteinase 19 is a protective biomarker in human prostate cancer. BMC Cancer. 2016;16:151. doi: 10.1186/s12885-016-2178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Josson S., Anderson C.S., Sung S.Y., Johnstone P.A., Kubo H., Hsieh C.L., Arnold R., Gururajan M., Yates C., Chung L.W. Inhibition of ADAM9 expression induces epithelial phenotypic alterations and sensitizes human prostate cancer cells to radiation and chemotherapy. Prostate. 2011;71:232–240. doi: 10.1002/pros.21237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Lin G.-W., Yao X.-D., Ye D.-W., Zhang S.-L., Dai B., Zhang H.-L., Ma C.-G. ADAM9 decreases in castration resistant prostate cancer and is a prognostic factor for overall survival. Chin. Med. J. 2012;125 [PubMed] [Google Scholar]
- 211.Liu C.-M., Hsieh C.-L., He Y.-C., Lo S.-J., Liang J.-A., Hsieh T.-F., Josson S., Chung L.W.K., Hung M.-C., Sung S.-Y. In vivo targeting of ADAM9 gene expression using lentivirus-delivered shRNA suppresses prostate cancer growth by regulating REG4 dependent cell cycle progression. PLoS ONE. 2013;8 doi: 10.1371/journal.pone.0053795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.McCulloch D.R., Harvey M., Herington A.C. The expression of the ADAMs proteases in prostate cancer cell lines and their regulation by dihydrotestosterone. Mol. Cell Endocrinol. 2000;167:11–21. doi: 10.1016/S0303-7207(00)00305-1. [DOI] [PubMed] [Google Scholar]
- 213.McCulloch D.R., Akl P., Samaratunga H., Herington A.C., Odorico D.M. Expression of the disintegrin metalloprotease, ADAM-10, in prostate cancer and its regulation by dihydrotestosterone, insulin-like growth factor I, and epidermal growth factor in the prostate cancer cell model LNCaP. Clin. Cancer Res. 2004;10:314–323. doi: 10.1158/1078-0432.CCR-0846-3. [DOI] [PubMed] [Google Scholar]
- 214.Peduto L., Reuter V.E., Sehara-Fujisawa A., Shaffer D.R., Scher H.I., Blobel C.P. ADAM12 is highly expressed in carcinoma-associated stroma and is required for mouse prostate tumor progression. Oncogene. 2006;25:5462–5466. doi: 10.1038/sj.onc.1209536. [DOI] [PubMed] [Google Scholar]
- 215.Peduto L., Reuter V.E., Shaffer D.R., Scher H.I., Blobel C.P. Critical function for ADAM9 in mouse prostate cancer. Cancer Res. 2005;65:9312–9319. doi: 10.1158/0008-5472.CAN-05-1063. [DOI] [PubMed] [Google Scholar]
- 216.Pen C.C., Liu C.M., Lin C.C., Lin C.C., Hsieh T.F., Josson S., He Y.C., Chung L.W., Lin K.L., Sung S.Y. Combined dynamic alterations in urinary VEGF levels and tissue ADAM9 expression as markers for lethal phenotypic progression of prostate cancer. Chin. J. Physiol. 2012;55:390–397. doi: 10.4077/CJP.2012.BAA075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Shigemura K., Sung S.-Y., Kubo H., Arnold R.S., Fujisawa M., Gotoh A., Zhau H.E., Chung L.W.K. Reactive oxygen species mediate androgen receptor- and serum starvation-elicited downstream signaling of ADAM9 expression in human prostate cancer cells. Prostate. 2007;67:722–731. doi: 10.1002/pros.20565. [DOI] [PubMed] [Google Scholar]
- 218.Sung S.Y., Kubo H., Shigemura K., Arnold R.S., Logani S., Wang R., Konaka H., Nakagawa M., Mousses S., Amin M., et al. Oxidative stress induces ADAM9 protein expression in human prostate cancer cells. Cancer Res. 2006;66:9519–9526. doi: 10.1158/0008-5472.CAN-05-4375. [DOI] [PubMed] [Google Scholar]
- 219.Gustavsson H., Tesan T., Jennbacken K., Kuno K., Damber J.-E., Welén K. ADAMTS1 alters blood vessel morphology and TSP1 levels in LNCaP and LNCaP-19 prostate tumors. BMC Cancer. 2010;10:288. doi: 10.1186/1471-2407-10-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Gustavsson H., Wang W., Jennbacken K., Welén K., Damber J.-E. ADAMTS1, a putative anti-angiogenic factor, is decreased in human prostate cancer. BJU Int. 2009;104:1786–1790. doi: 10.1111/j.1464-410X.2009.08676.x. [DOI] [PubMed] [Google Scholar]
- 221.Binder M.J., McCoombe S., Williams E.D., McCulloch D.R., Ward A.C. ADAMTS-15 has a tumor suppressor role in prostate cancer. Biomolecules. 2020;10 doi: 10.3390/biom10050682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Cross N.A., Chandrasekharan S., Jokonya N., Fowles A., Hamdy F.C., Buttle D.J., Eaton C.L. The expression and regulation of ADAMTS-1, -4, -5, -9, and -15, and TIMP-3 by TGFβ1 in prostate cells: Relevance to the accumulation of versican. Prostate. 2005;63:269–275. doi: 10.1002/pros.20182. [DOI] [PubMed] [Google Scholar]
- 223.Molokwu C.N., Adeniji O.O., Chandrasekharan S., Hamdy F.C., Buttle D.J. Androgen regulates ADAMTS15 gene expression in prostate cancer cells. Cancer Invest. 2010;28:698–710. doi: 10.3109/07357907.2010.489538. [DOI] [PubMed] [Google Scholar]
- 224.Rienks M., Barallobre-Barreiro J., Mayr M. The emerging role of the ADAMTS family in vascular diseases. Circ. Res. 2018;123:1279–1281. doi: 10.1161/CIRCRESAHA.118.313737. [DOI] [PubMed] [Google Scholar]
- 225.Arpino V., Brock M., Gill S.E. The role of TIMPs in regulation of extracellular matrix proteolysis. Matrix Biol. 2015;44–46:247–254. doi: 10.1016/j.matbio.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 226.Wilson M.J., Jiang A., Wiehr C., Wang X., Sinha A.A., Pei D. Limited processing of pro-matrix metalloprotease-2 (Gelatinase A) overexpressed by transfection in PC-3 human prostate tumor cells: Association with restricted cell surface localization of membrane-type matrix metalloproteinase-1. J. Androl. 2004;25:274–285. doi: 10.1002/j.1939-4640.2004.tb02788.x. [DOI] [PubMed] [Google Scholar]
- 227.Liao X., Thrasher J.B., Pelling J., Holzbeierlein J., Sang Q.X., Li B. Androgen stimulates matrix metalloproteinase-2 expression in human prostate cancer. Endocrinology. 2003;144:1656–1663. doi: 10.1210/en.2002-0157. [DOI] [PubMed] [Google Scholar]
- 228.Li B.Y., Liao X.B., Fujito A., Thrasher J.B., Shen F.Y., Xu P.Y. Dual androgen-response elements mediate androgen regulation of MMP-2 expression in prostate cancer cells. Asian J. Androl. 2007;9:41–50. doi: 10.1111/j.1745-7262.2007.00226.x. [DOI] [PubMed] [Google Scholar]
- 229.Montico F., Kido L.A., Hetzl A.C., Lorencini R.M., Cândido E.M., Cagnon V.H.A. Antiangiogenic therapy effects on age-associated matrix metalloproteinase-9 (MMP-9) and insulin-like growth factor receptor-1 (IGFR-1) responses: A comparative study of prostate disorders in aged and TRAMP mice. Histochem. Cell Biol. 2014;142:269–284. doi: 10.1007/s00418-014-1193-2. [DOI] [PubMed] [Google Scholar]
- 230.Von Bredow D.C., Nagle R.B., Bowden G.T., Cress A.E. Cleavage of β4 Integrin by Matrilysin. Exp. Cell Res. 1997;236:341–345. doi: 10.1006/excr.1997.3711. [DOI] [PubMed] [Google Scholar]