Abstract
Preterm birth is the leading cause of death in newborns and the survivors are prone to health complications. Threatened preterm labor (TPL) is the most common cause of hospitalization in the second half of pregnancy. The current methods used in clinical practice to diagnose preterm labor, the Bishop score or cervical length, have high negative predictive values but not positive ones. In this work we analyzed the performance of computationally efficient classification algorithms, based on electrohysterographic recordings (EHG), such as random forest (RF), extreme learning machine (ELM) and K-nearest neighbors (KNN) for imminent labor (<7 days) prediction in women with TPL, using the 50th or 10th–90th percentiles of temporal, spectral and nonlinear EHG parameters with and without obstetric data inputs. Two criteria were assessed for the classifier design: F1-score and sensitivity. RFF1_2 and ELMF1_2 provided the highest F1-score values in the validation dataset, (88.17 ± 8.34% and 90.2 ± 4.43%) with the 50th percentile of EHG and obstetric inputs. ELMF1_2 outperformed RFF1_2 in sensitivity, being similar to those of ELMSens (sensitivity optimization). The 10th–90th percentiles did not provide a significant improvement over the 50th percentile. KNN performance was highly sensitive to the input dataset, with a high generalization capability.
Keywords: electrohysterogram, uterine myoelectrical activity, tocolytic therapy, random forest, extreme learning machine, K-nearest neighbors, imminent labor prediction
1. Introduction
Preterm labor is defined as natural or induced labor prior to 37 weeks of gestation [1]. Currently, preterm birth and its consequences are a serious problem in health systems in most developed countries, and despite the fact that the treatment protocols for these deliveries have evolved considerably and reduced the mortality of neonates, it is still associated with 35% of newborn deaths [2]. It has not been possible to reduce the prevalence of preterm births, which continues to increase year after year, assuming between 8% and 13% of total deliveries worldwide, affecting some 15 million families [3]. This increase is fundamentally associated with a more advanced mean age of pregnant woman and the increased use of fertility treatments, resulting in a higher risk of preterm delivery. Preterm deliveries increase health spending not only due to the immediate treatment required by preterm infants, but also due to normally chronic problems that tend to develop due to early deliveries, ranging from respiratory, gastrointestinal and immune problems to more severe neurological, cognitive and motor problems [4].
Prompt preterm labor diagnosis is vitally important to be able to administer uterine inhibitory drugs in time so that the corticosteroids can accelerate fetal lung development, reduce perinatal and neonatal death risk, intra ventricular hemorrhage, and underdevelopment in childhood [5]. Although great efforts have been made and obstetrical parameters such as cervical length (CL) by themselves or in combination with other biochemical markers such as fetal fibronectin (fFN) have shown a certain degree of usefulness in detecting preterm births, currently there is no technique that allows assessing time-to-delivery objectively and accurately and whether or not it will be premature [6]. A study measuring fFN and CL in women between 22 and 30 weeks’ gestation showed an AUC of 0.59 in preterm birth prediction, an AUC of 0.67 for cervical length alone and a very similar value for the combination of both [7]. Although cervical length and fFN have high negative predictive values, their positive predictive values are lower and do not identify the patients who are actually going to deliver prematurely [8].
The problem not only lies in premature births but also in the threat of premature labor (TPL), this being the most common cause of hospitalization in the second trimester of pregnancy. This involves prolonged clinical stays, drug treatment with possible side effects, significant distress for the pregnant woman and her family, reduced care for her other children (if any) and a high economic cost derived from the hospitalization and absence of the pregnant woman from work [9]. As the literature reports that only 34% of the women who go to the emergency room with threatened preterm labor give birth preterm [10], predicting whether a woman with TPL will give birth prematurely can help to optimize labor management, allowing decisions to be made that lead to the best result from the point of view of maternal-fetal health and hospital resource management [9].
The studies in the literature state that the mechanisms that trigger labor start several days or even weeks before it and involve changes in the electrical potential of myometrial muscle cells. This myoelectrical activity, known as an electrohysterogram (EHG), can be recorded on the surface of the abdomen. The bursts of action potentials in the EHG is associated with uterine contractions [11,12]. The EHG has been proposed as a promising technique for preterm labor prediction due to the fact that uterine activity increases its intensity and synchronization near labor [13,14,15]. The increased number of myometrial cells recruited in uterine contractions when labor is near results in a greater EHG amplitude, while the intensified cell excitability shifts the EHG spectral content to higher frequencies [16,17], and the labor onset entails changes in myometrial cell connectivity that modifies the regularity of the measured EHG signal: EHG predictability increases while signal complexity is reduced [18,19,20].
Labor or preterm labor prediction algorithms have been developed with over 90% accurate metrics [21,22,23,24] when using EHG recordings from women during clinical checkups under physiological conditions. However tocolytic drugs are usually administered to inhibit uterine contractions at the first sign of threatened preterm labor and modify the EHG features [25,26]. The feasibility of imminent preterm labor prediction in women with TPL undergoing tocolytic treatment by means of an artificial neural network (ANN) algorithm has been proved using median values of EHG parameters in 120 s analysis windows and obstetric data inputs [27]. Despite being one of the most frequently used classification algorithms, ANN has certain drawbacks, such as a low learning speed associated with the backpropagation algorithm and the fact that it can easily get into local optima [28]. In the present study we focus on three different computationally efficient algorithms, random forest (RF), extreme learning machine (ELM) and K-nearest neighbors (KNN), which have been used in biological classification problems to distinguish between gestational or labor contractions or term/preterm deliveries from EHG recordings from routine checkups [28]. A recent study revealed that the 90th and 10th percentiles of the EHG parameters computed in 120 s whole analysis windows outperformed median values in discerning between different obstetric scenarios, as term vs. preterm labor, in recordings from routine checkups [20]. The better ability of the 10th–90th percentiles of EHG parameters to discriminate were associated with being more representative of the contractile segments in the recording session [20], choosing the 10th or 90th percentile of the EHG parameters according to their expected trend as delivery approaches [20]. In addition, the optimization criterion in the classifier design was not clearly indicated in the literature regarding term/preterm birth or labor/nonlabor prediction, regardless of the classification algorithm employed [24,29,30,31]. In applications such as the prediction of preterm labor or imminent delivery in women with TPL, it is of vital importance to develop prediction systems with high sensitivity values.
The aim of the present work was therefore to assess and optimize the performance of EHG based computationally efficient classification algorithms (RF, ELM and KNN) for imminent labor (<7 days) prediction in women with TPL. It was also intended to determine whether the 10th–90th percentiles of EHG parameters computed in 120 s analysis windows with or without obstetric input features contain more information for imminent labor prediction in women with TPL than median values, and to determine how the optimization criteria in the classifier design affect their performance.
2. Materials and Methods
2.1. EHG Database and Characterization
A database of 140 30-min EHG recordings conducted on 84 singleton-pregnant women with TPL symptoms such as uterine dynamics and/or cervical effacement or dilatation taken at the “Hospital Universitari i Politècnic la Fe” (Valencia, Spain) from 2015 to 2019 was used in the study, which was approved by the hospital’s Institutional Review Board. Women with preterm membrane rupture were excluded. The women were informed of the aims of the study and asked to give their written consent. Most EHG signals were recorded during or after the administration of the Atosiban tocolytic agent, which blocks uterine contractility. Thirty records in the database were from women who gave imminent birth (time to delivery (TTD) ≤ 7 days) and 110 gave birth in more than 7 days. For the TTD ≤ 7 days group, 13 recordings were performed during tocolytic treatment, 13 post-tocolytic treatment and four were obtained before tocolytic treatment. In the TTD > 7 group, 47 records were taken during tocolytic treatment, 43 post-tocolytic treatment and 20 before tocolytic treatment. Obstetrical data picked up were gestational and maternal age, cervical length at the recording, parity, gestations, and abortions. This information can be found in [27].
A single bipolar EHG signal was recorded as described in [27] by means of two disposable Ag/AgCl electrodes (3M red dot 2560, wet with solid hydrogel) placed on the abdomen over the navel symmetrically to the median axis with an interelectrode distance of 8 cm (electrodes M1 and M2). Two additional electrodes were placed on the patient’s hips acting as ground and reference electrodes. Signals were digitized with a 24 bit ADC at 500 Hz and downsampled to 20 Hz. A bipolar recording was computed as the difference of the two monopolar recordings from M1 and M2 in the 0.1–4 Hz bandwidth to diminish common-mode interference. Signal segments with motion artefacts or with considerable respiratory interference were discarded in a visual inspection by experts in a double-blinded process. The EHG characteristics were worked out in 120 s windows with a 50% overlap, and were a tradeoff between saving representative sections of the recordings and a rational computational cost [25]. This avoids burst annotation and is more appropriate for future ‘real-time’ applications, bringing EHG closer to clinical practice.
Twenty-three temporal, spectral, complexity and regularity parameters were worked out in the whole EHG bandwidth, 0.1–4 Hz (unless otherwise noted), to characterize the recordings (see Table 1). Amplitude in temporal domain tends to increase as labor approaches due to the growth of cells recruited in uterine contractions [21,22]. Spectral parameters are used to assess the shift of EHG spectral content to higher frequencies as labor approaches [12,17,32]. We computed the dominant frequencies in the bandwidth 0.2–1 Hz (DF1) and in 0.34–1 Hz (DF2), considering that the Fast Wave Low of the EHG ranges from 0.2 to 0.34 Hz and Fast Wave High, which includes EHG components above 0.34 Hz, limiting the high frequency to 1 Hz to diminish ECG and respiration interference [13,33]; the high-to-low frequency energy ratio (H/L ratio, as the ratio of energy in 0.34–1 Hz to energy in 0.2–0.34 Hz); deciles of the power spectrum and the spectral moment ratio (SMR) [20,34].
Table 1.
Summary of electrohysterographic recordings (EHG) features and obstetric data inputs.
| EHG Temporal Parameters | EHG Spectral Parameters | EHG Nonlinear Parameters | Obstetric Data |
|---|---|---|---|
| Peak-to-peak amplitude | DF1 DF2 H/L ratio Deciles [D1–D9] SMR |
Binary Lempel-Ziv Multistate Lempel-Ziv (n = 6) Sample entropy Spectral entropy Fuzzy entropy Time reversibility SD1 SD2 SD1/SD2 |
Cervical length Gestational age at moment of recording Maternal age Gestations Parity Abortions |
A set of representative complexity and regularity parameters to distinguish between preterm and term labor were also calculated to characterize the EHG signal, as in the related literature [20]: Lempel-Ziv (Binary and multistate n = 6), which assesses signal complexity from the number of different patterns in the signals [35]; sample, fuzzy and spectral entropy, which measure regularity based on the self-similarity in temporal and spectral domains [36,37,38,39]; and time reversibility [40], which estimates the similarity of a time series when time goes forward or back. A Poincare plot [41] of consecutive EHG signal samples was obtained and parameters SD1, SD2 were also computed to assess corresponding short- and long-term EHG changes, and SD1/SD2 to measure EHG randomness [42]. To avoid redundant information, other nonlinear parameters were not calculated as in [31,43].
To obtain representative values for each EHG parameter in each recording we worked out the 50th (median) and 10th–90th percentiles of the parameters for all the analyzed windows [20]. The 50th percentile mainly assesses basal activity rather than uterine contractions in nonlabor recordings. This is because, considering uterine electrophysiology throughout pregnancy, during the 30-min recording session the time-percentage of EHG-bursts (associated with uterine contraction) is expected to be relatively low, especially in pregnancy recordings (maximum contraction rhythm: 3 in 10-min during active phase of labor). To characterize uterine contractions (EHG-Bursts) the 10th and 90th percentiles of all the analyzed windows were thus calculated. For EHG parameters with an increasing trend in contractile periods as labor approaches, as amplitude, DF1, DF2, deciles and H/L and time reversibility, the 90th percentile was computed. In contrast, for the EHG parameters whose values decrease in contractile periods as labor approaches the 10th percentile was worked out, as was the case of SMR, Binary and Multistate Lempel-Ziv (n = 6), Sample Entropy, Fuzzy Entropy, Spectral Entropy, SD1, SD2 and SD1/SD2.
2.2. Classifiers Design and Assessment
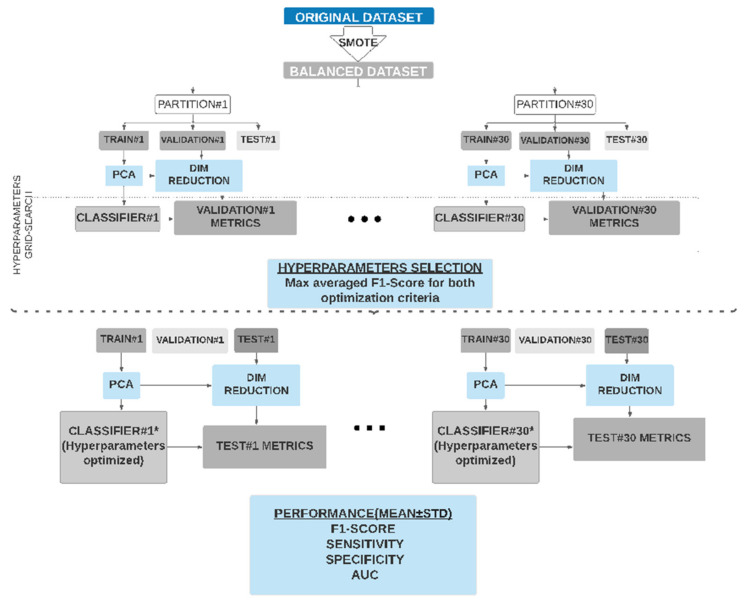
The database was clearly imbalanced towards the patients who gave birth after 7 days (TTD ≤ 7 days 21.4%, TTD > 7 days 78.6%). To overcome this well-known problem of imbalanced data training, which may induce a clear bias towards the majority class predictions, the synthetic oversampling technique (SMOTE) [44] was used. This technique has been broadly used to deal with imbalanced classification problems [21,31,32,45]. SMOTE was applied by using five neighbors to interpolate the minority samples in a ratio of 3:1. This led to a balanced database with 110 recordings from the majority class and 90 recordings from the minority class (TTD ≤ 7 days 47%, TTD > 7 days 53%). To check the robustness of the classifiers under different data conditions a holdout method was applied 30 times by randomly splitting the database into training, validation and test subsets each time. The main purpose of repeating each experiment 30 times was to be able to reduce the possible bias induced by a particular distribution of the subsets and to ensure the strength of the statistical tests (nonparametric Wilcoxon paired test) performed to optimize the hyperparameters, based in statistically relevant differences in the validation subset. For each experiment repetition (partition), the subset percentages were distributed as follows: 1/3 for test, so as to evaluate the classifiers’ generalization capacity, and 2/3 for the classifiers’ design, training (2/3 * 2/3) and validation (2/3 * 1/3). The percentages were thus 44% training (89 samples), 23% validation (45 samples) and 33% test (66 samples), see Figure 1. For each subset (train, validation and test) we maintained the proportion of TTD ≤ 7 and TTD > 7 data, 47% of the minority class and 53% majority class. The same 30 partitions were conserved over all “stages” in the classifiers design (train and validation) and test. No randomness was involved in the case of KNN classifier training, but ELM initial weights and RF random sampling and feature selection were dealt with by initializing each classifier with the same hyperparameter combination 30 times and different fixed seeds (corresponding to 100 initializations). Trained algorithms were assessed under the validation subset and the best seed was chosen and stored as an “additional” hyperparameter, ensuring reproducibility and consistency between different trials. This seed acted in RF by forcing the algorithm to select a similar subset of features in each trial and in ELM by forcing the initial layer weights to be the same over different trials. Therefore, besides maintaining the same 30 partitions for all classifiers, for the ELM and RF ones the same combination of seeds and weights optimized in validation were used for the test. To avoid overfitting problems due to the number of input features being larger than the number of recordings (23 EHG and six obstetric), a principal component analysis (PCA) was carried out retaining 98% variance but reducing the number of input parameters [23,37,46].
Figure 1.
Scheme of the method used to train, validate and test the imminent labor prediction classifiers (time to delivery (TTD ≤ 7) based on EHG in women with threatened preterm labor. This was performed with two optimization criteria in the classifier design: F1-score and sensitivity.
The performance of three computationally efficient classification algorithms was assessed in this study: the extreme learning machine (ELM), K-nearest neighbors (KNN) and random forest (RF), all of these implemented on public packages of R. The public Ranger package for RF classifiers was used to develop random forest. This is an efficient parallel implementation of the RF algorithm proposed by Breiman in [47,48]. The number of trees, the maximum depth of these trees and the cost of division based on the criterion of gain of information were optimized. The elmNNRcpp package, based on the implementation proposed by Huang was selected for the ELM classifier [49]. The hyperparameters to be optimized were in this case the number of neurons in the hidden layer, and the activation function. KNN was implemented in the R KNN algorithm, which uses the Minkowski distance and a weighting based on a probabilistic kernel [50]. The hyperparameters to optimize were number of neighbors and the Kernel used for weighting the distances. In an appendix to this article we included four tables (Table A1, Table A2, Table A3 and Table A4) detailing the gridsearch carried out for the parameters and the optimized values for the classifiers.
As previously mentioned, as classifiers with high sensitivity values are required for preterm labor or imminent delivery prediction in women with TPL, we dealt with two different optimization criteria for the classifiers’ design, the F1-Score (harmonic mean of precision and recall) and sensitivity [51]. In both cases we carried out a hyperparameter grid search (see Figure 1) and after obtaining the metrics of the classifiers in each of the 30 partitions, they were averaged, choosing the hyperparameters which gave the highest mean F1-Score in validation subsets (for both criteria). This was decided because F1 would avoid the overdetection of false positives, as happens today in clinics, where uterine inhibitors are administered to all the women with TPL symptoms. After selecting the optimal hyperparameters, their performance in the test data was assessed. For each classifier four sets of input features were appraised: (1) the 10th–90th percentiles of EHG parameters and obstetric data; (2) the 50th percentile of EHG data and obstetric data; (3) the 10th–90th percentiles of EHG parameters; (4) the 50th percentile of EHG data. Table 2 summarizes the classifiers developed according to their input dataset and optimization criterion, F1-score or sensitivity.
Table 2.
Summary of the classifiers developed, their input features and optimization criterion (F1-score or sensitivity). RF: random forest, ELM: extreme learning machine, K-nearest neighbors (KNN).
| RF | ELM | KNN | |||||
|---|---|---|---|---|---|---|---|
| Criterion | F1-Score | Sensitivity | F1-Score | Sensitivity | F1-Score | Sensitivity | |
| Input Features | |||||||
| EHG 10th–90th percentiles + Obstetric data | RFF1_1 | RFSEN_1 | ELMF1_1 | ELMSEN_1 | KNNF1_1 | KNNSEN_1 | |
| EHG 50th + Obstetric data | RFF1_2 | RFSEN_2 | ELMF1_2 | ELMSEN_2 | KNNF1_2 | KNNSEN_2 | |
| EHG 10th–90th percentiles | RFF1_3 | RFSEN_3 | ELMF1_3 | ELMSEN_3 | KNNF1_3 | KNNSEN_3 | |
| EHG 50th percentile | RFF1_4 | RFSEN_4 | ELMF1_4 | ELMSEN_4 | KNNF1_4 | KNNSEN_4 | |
To assess the models’ performance, a set of metrics (F1-score, sensitivity, and specificity) was obtained for each partition in training, validating and testing the data. They were computed as follows:
| (1) |
| (2) |
| (3) |
where, TP, TN, FP, and FN are true positives, true negatives, false positives, and false negatives, respectively. In this work, a true positive is labor TTD ≤ 7 days correctly predicted by the algorithm. The Wilcoxon signed rank test was used to check for any statistically significant differences between pairs of classifier metrics. This was done first for all classifier metrics from the validation dataset to find any statistically significant differences for the same classifier when changing the optimization criteria (e.g., ELMF1_2 vs. ELMSENS_2). Secondly, we looked for any statistically significant differences regarding the classifier input dataset (e.g., ELMF1_2 vs. ELMF1_1) in the optimization criteria and metrics. It should be noted that validation and test results were not mixed in any case. The coefficient of variation of the above-mentioned metrics were worked out for the 30 test datasets to analyze the strength of the algorithms when using new and different sets. Finally, the receiver operating curve (ROC) was obtained and represented for the classifier with the best performance.
3. Results
Regarding the nature of the classifiers used in the present study, as the metrics obtained for the training subset, for which the classifiers were trained, were in most cases 100% they were not considered relevant for our purpose and are not included here.
3.1. Random Forest (RF)
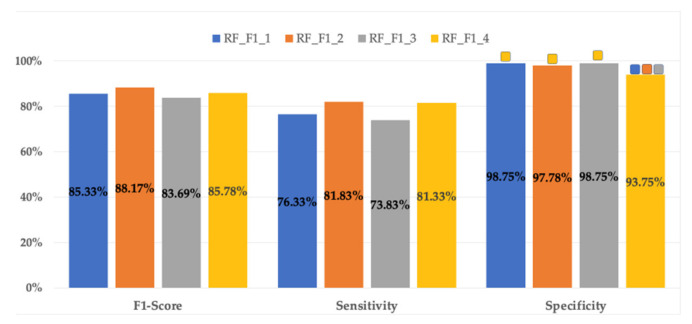
Regardless of the optimization criterion (F1-score or sensitivity), the best classifiers for each data input set showed the same optimal hyperparameters, that is: RFF1_1 = RFSEN_1; RFF1_2 = RFSEN_2; RFF1_3 = RFSEN_3; RFF1_4 = RFSEN_4. Figure 2 shows a bar plot of the metrics of the RF classifiers in the validation dataset for each set of input features. It can be seen in this figure that the highest mean F1-score is for RFF1_2 (88.17 ± 8.34%), which also has the highest sensitivity (81.83 ± 12.9%). As for RF classifiers, adding obstetric data to EHG parameters as data inputs slightly improves their performance over using only EHG parameters (i.e., RFF1_1 vs. RFF1_3 and RFF1_2 vs. RFF1_4) without statistically significant differences between them (except in specificity RF_F1_2 vs. RF_F1_4). On the other hand, the use of the 10th–90th percentiles vs. 50th percentile of the EHG parameters as inputs (i.e., RFF1_1 vs. RFF1_2 and RFF1_3 vs. RFF1_4) reduced F1-score and sensitivity, with no statistically significant differences. There were only statistically significant differences in terms of specificity between the RF_F1_4 and the rest with a mean specificity value of 93.75 ± 5.97%, whereas the mean specificity values for the other RF classifiers range from 97.78 ± 4.2% to 98.75 ± 2.48%. RF metrics for the validation dataset showed high mean values for specificity, but modest sensitivity (from 73.83 ± 12.08% to 81.83 ± 12.9%). The mean values of the RFs metrics for the test group are shown in Figure 2. As occurs in the validation group, the highest F1-score for the test belongs to RFF1_2, but dropping its values to 80.35 ± 6.78%. The RF classifiers stand out especially for their high specificity metrics (over 90% for all test datasets), but with low sensitivities, ranging from 65.78 ± 11.61% to 74 ± 10.41%, this latter for RFF1_2. The high variability of the RF classifier metrics is also noticeable in the test group (Table 3), especially for sensitivity, with coefficients of variation between 14.1% and 17.6%, which is a major drawback in predicting preterm labor.
Figure 2.
Mean values of different RF classifier metrics for validation datasets in the 30 data partitions optimized by F1-score. The same results were obtained when optimizing by sensitivity. For each metric the significant differences (p < 0.05) for each input dataset are marked with:  10th–90th percentiles of EHG parameters + obstetric input data;
10th–90th percentiles of EHG parameters + obstetric input data;  50th percentile of EHG + obstetric input data;
50th percentile of EHG + obstetric input data;  10th–90th percentiles of EHG parameters;
10th–90th percentiles of EHG parameters;  50th percentile of EHG parameters.
50th percentile of EHG parameters.
Table 3.
Mean ± standard deviation and coefficient of variation (in brackets) of RF classifiers performance metrics in test dataset for predicting imminent birth (TTD ≤ 7days) in women with threatened preterm labor (TPL) using EHG data or a combination of EHG and obstetric data. The maximum value for each metric is shown in bold. F1: F1-score, Sens: Sensitivity, Spec: Specificity.
| Opt. Criterion | Inputs | Classifier | Test_F1 | Test_Sens | Test_Spec |
|---|---|---|---|---|---|
| F1-Score Sensitivity |
EHGP10–P90 + Obs | RFF1_1 | 77.51 ± 7.58% (9.8%) | 66.22 ± 11.70% (17.7%) | 97.12 ± 4.13% (4.3%) |
| EHGP50 + Obs | RFF1_2 | 80.35 ± 6.78% (8.4%) | 74.00 ± 10.41% (14.1%) | 92.25 ± 5.35% (5.8%) | |
| EHGP10–P90 | RFF1_3 | 77.81 ± 8.71% (11.2%) | 65.78 ± 11.61% (17.6%) | 98.29 ± 2.51% (2.6%) | |
| EHGP50 | RFF1_4 | 77.7 ± 6.6% (8.5%) | 71.44 ± 10.99% (15.4%) | 90.72 ± 4.58% (5.0%) |
3.2. Extreme Learning Machine (ELM)
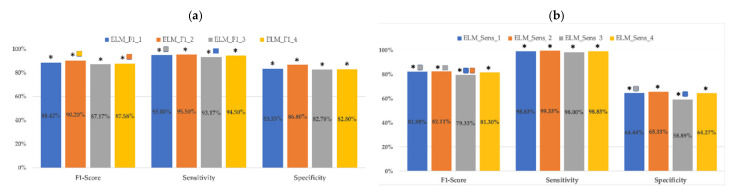
Figure 3 shows a bar plot of the metrics of the ELM classifiers for each set of input parameters in the validation dataset when optimizing with F1-score and sensitivity. First of all, it should be noted that optimizing ELM classifiers with the F1-score or sensitivity criteria resulted in statistically significant differences (ELMF1_X vs. ELMSEN_X) in all their metrics for the same input dataset. ELMF1 outperforms ELMSEN classifiers in F1-score and specificity metrics, but gives lower values for sensitivity. This latter increase in ELMSEN sensitivity metrics (about 3.5%) was at the cost of a notable reduction in specificity (about 20%). For instance, comparing ELMSen_2 and ELMF1_2, an improvement of around 4% (95.5 + 4.61% vs. 99.33 + 1.73) in sensitivity led to a reduction of more than 20% in specificity (86.8 + 7.14% vs. 65.33 + 10.78%) and to a statistically significant reduction in the F1-score from 90.2 + 4.43% to 82.11 + 4.5%. It should also be noted that, unlike what happened with the RF classifiers, the ELMF1 classifiers presented high sensitivity values, with mean values between 93.17 ± 5% and 95.5 ± 4.61% for the validation dataset. This performance is of special importance when developing imminent labor predictive systems in women with TPL and for preterm labor prediction in general
Figure 3.
Mean values of different ELM classifier metrics for validation datasets in the 30 data partitions (a) optimizing F1-score (b) optimizing sensitivity. For each optimization criteria and metric, the significant differences (p < 0.05) for each input dataset are marked with  10th–90th percentiles of EHG parameters + obstetric input data;
10th–90th percentiles of EHG parameters + obstetric input data;  50th percentile of EHG + obstetric input data;
50th percentile of EHG + obstetric input data;  10th–90th percentiles of EHG parameters;
10th–90th percentiles of EHG parameters;  50th percentile of EHG parameters. Significant differences between the two optimization criteria for the same input data set are marked with *.
50th percentile of EHG parameters. Significant differences between the two optimization criteria for the same input data set are marked with *.
Analyzing the effect of the input features in the classifier performance, regardless of the optimization criteria, the highest F1-score was reached by the classifiers that used the 50th percentile of EHG parameters and obstetric data, ELMF1_2 (90.2 ± 4.43%) and ELMSEN_2 (82.11 ± 4.5%). ELMF1_2 and ELMSEN_2 also reported the highest sensitivities (95.5 ± 4.61% and 99.33 ±1.73%) and specificities (86.8 ± 7.14% and 65.33 ± 10.78%) for each optimization criteria. For the same optimization criteria, these metrics did not present statistically significant differences with those of classifiers using the 10th–90th percentile of EHG parameters and obstetric data as inputs (ELMX_1 vs. ELMX_2). Using only EHG parameters as data inputs slightly worsens ELM classifier metrics compared to the combined use of EHG and obstetric data (ELMX_1 vs. ELMX_3 and ELMX_ vs. ELMX_4).
On the other hand, the performances of the ELM classifiers for the test datasets are consistent with those obtained in the validation dataset, although all the metrics are reduced (see Table 4). The highest F1-score, sensitivity and specificity were reached by ELMF1_2 with corresponding 82.14 ± 5.88%, 89.89 ± 7.14% and 76.4 ± 8.12% values. Similarly, when optimizing by sensitivity criteria, the highest F1-score, sensitivity and specificity values for the test dataset are for ELMSEN_2, but dropping its F1-score to 75.42 ± 3.96%, mainly due to the low specificity of 52.25 ± 9.58%, regardless of the high sensitivity of 96.00 ± 5.13%. Indeed, the results of the ELM classifiers for test datasets reveal that specificity has the greatest variability, especially when the sensitivity optimization criterion is applied, reaching 19.5% (ELMSEN_4) in this case.
Table 4.
Mean ± standard deviation and coefficient of variation (in brackets) of ELM classifiers’ performance metrics in test dataset for predicting imminent birth (TTD ≤ 7 days) in women with TPL using EHG data or a combination of EHG and obstetric data. The maximum value for each metric and optimization criterion is shown in bold. F1: F1-score, Sens: sensitivity, Spec: specificity.
| Opt. Criterion | Inputs | Classifier | Test_F1 | Test_Sens | Test_Spec |
|---|---|---|---|---|---|
| F1-score | EHGP10–P90 + Obs | ELMF1_1 | 80.00 ± 4.98% (6.0%) | 87.56 ± 8.53% (9.7%) | 74.77 ± 7.32% (9.8%) |
| EHGP50 + Obs | ELMF1_2 | 82.14 ± 5.88% (7.2%) | 89.89 ± 7.14% (7.9%) | 76.40 ± 8.12% (10.6%) | |
| EHGP10–P90 | ELMF1_3 | 78.41 ± 4.55% (5.8%) | 85.89 ± 7.91% (9.2%) | 73.24 ± 6.93% (9.5%) | |
| EHGP50 | ELMF1_4 | 79.00 ± 5.06% (6.4%) | 86.22 ± 6.65% (7.7%) | 73.87 ± 8.64% (11.7%) | |
| Sensitivity | EHGP10–P90 + Obs | ELMSEN_1 | 74.83 ± 3.88% (5.2%) | 95.44 ± 4.59% (4.8%) | 51.35 ± 9.28% (18.1%) |
| EHGP50 + Obs | ELMSEN_2 | 75.42 ± 3.96% (5.3%) | 96.00 ± 5.13% (5.3%) | 52.25 ± 9.58% (18.3%) | |
| EHGP10–P90 | ELMSEN_3 | 73.13 ± 3.10% (4.2%) | 94.78 ± 4.61% (4.9%) | 47.57 ± 8.83% (18.6%) | |
| EHGP50 | ELMSEN_4 | 73.83 ± 3.24% (4.4%) | 94.89 ± 5.01% (5.3%) | 49.37 ± 9.63% (19.5%) |
3.3. K-Nearest Neighbors (KNN)
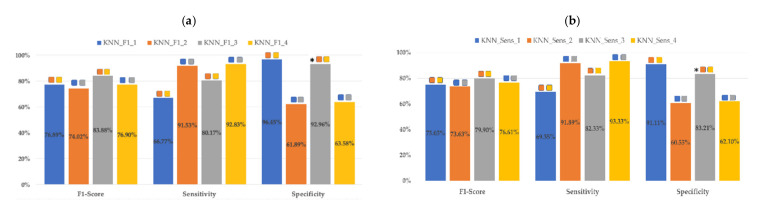
As can be seen in Figure 4, KNN classifier metrics do not present statistically significant differences according to the optimization criteria, except in the case of the specificity between KNNF1_3 and KNNSENS_3. The highest F1 score in the validation dataset for each optimization criteria is for KNNF1_3 (83.88 ± 10.31%) and KNNSENS_3 (79.9 ± 9.72%) with the 10th–90th percentiles of EHG parameters as inputs.
Figure 4.
Mean values of different KNN classifier metrics for validation datasets in the 30 data partitions: (a) optimizing F1-score (b) optimizing sensitivity. For each optimization criteria and metric, the significant differences (p < 0.05) for each input dataset are marked with  10th–90th percentiles of EHG parameters + obstetric input data;
10th–90th percentiles of EHG parameters + obstetric input data;  50th percentile of EHG + obstetric input data;
50th percentile of EHG + obstetric input data;  10th–90th percentiles of EHG parameters;
10th–90th percentiles of EHG parameters;  50th percentile of EHG parameters. Significant differences between the two optimization criteria for the same input dataset are marked with *.
50th percentile of EHG parameters. Significant differences between the two optimization criteria for the same input dataset are marked with *.
As regards the influence of the classifier input dataset on their performance, KNNF1_3 did not present statistically significant differences in any of its metrics with respect to KNNF1_1. The same occurred with KNNF1_2 vs. KNNF1_4. That is, having added obstetric inputs did not improve KNN classifier metrics. However, using the 50th or 10th–90th percentiles of EHG gave significant differences in all KNN metrics for the validation dataset. For instance, KNNF1_1 showed statistically higher specificity than KNNF1_2 (96.45 ± 3.99% vs. 61.89 ± 12.02%) and lower sensitivity (66.77 ± 13.85% vs. 91.53 ± 7.92%). This also occurred in KNNF1_3 and KNNF1_4. It should be noted that the highest mean sensitivity was reached by KNNF1_4 (92.83 ± 6.11%) without significant differences with KNNF1_2 (91.53 ± 7.92%) but at the cost of a considerable reduction in specificity, with corresponding values of 63.58 ± 10.57% and 61.89 ± 12.02%. As previously mentioned, the same behavior was observed in KNNSens classifiers: the use of 10th–90th or 50th percentiles of EHG parameters modified KNNSENS performance with significant differences in all metrics (see Figure 4). Sensitivity is greater when using the 50th percentile and F1-score, and specificity when using the 10th–90th percentiles. The inclusion of obstetric inputs did not improve KNNSENS’ metrics either.
Mean values for the KNN metrics for test dataset are summarized in Table 5 and are consistent with those from the validation dataset: in this case, the optimization criteria caused noticeable differences in classifier metric values for the same data input, but with similar tendencies. For F1-score optimization, the highest F1-score corresponded to KNNF1_3 (84.67 ± 8.46%) and was similar to that of KNNF1_1 (84.18 ± 9.47%), associated with high specificity metrics (93.42 ± 6.34% and 92.7 ± 8.81%) and moderate sensitivities (79.33 ± 13.23% and 80.56 ± 12.57%). For sensitivity optimization, the highest F1-score corresponded to KNNSENS_1 (79.8 ± 8.29%), similar to that of KNNSENS_3 (78.63 ± 8.6%) and was lower than that of F1-score optimization criteria. In this case, for the test group the greatest variability in F1-score and sensitivity are associated with classifiers with input parameters that use the P10–90 percentiles of the EHG parameters, while in the case of specificity it is for those that use the 50th percentile as inputs. Indeed, for the test dataset, the use of the 50th percentile of EHG parameters improved sensitivity for the test dataset while dramatically reducing specificity when using sensitivity optimization criteria.
Table 5.
Mean ± standard deviation and coefficient of variation (in brackets) of KNN classifier performance metrics in test dataset for predicting imminent birth (TTD ≤ 7 days) in women with TPL using EHG characteristics or a combination of EHG and obstetric data. The maximum value for each metric and optimization criterion is in bold. F1: F1-score, Sens: Sensitivity, Spec: Specificity.
| Opt. Criterion | Inputs | Classifier | Test_F1 | Test_Sens | Test_Spec |
|---|---|---|---|---|---|
| F1-score | EHGP10–P90 + Obs | KNNF1_1 | 84.18 ± 9.47% (11.2%) | 79.33 ± 13.23% (16.7%) | 93.42 ± 6.34% (6.8%) |
| EHGP50 + Obs | KNNF1_2 | 74.16 ± 5.07% (6.8%) | 93.33 ± 6.37% (6.8%) | 52.43 ± 9.59% (18.3%) | |
| EHGP10–P90 | KNNF1_3 | 84.67 ± 8.46% (10.0%) | 80.56 ± 12.57% (15.6%) | 92.70± 8.81% (9.5%) | |
| EHGP50 | KNNF1_4 | 74.13 ± 4.57% (6.2%) | 90.89 ± 6.55% (7.2%) | 55.77 ± 9.67% (17.3%) | |
| Sensitivity | EHGP10–P90 + Obs | KNNSEN_1 | 79.8 ± 8.29% (10.4%) | 82.78 ± 12.13% (14.7%) | 80.36 ± 9.76% (12.1%) |
| EHGP50 + Obs | KNNSEN_2 | 72.98 ± 4.00% (5.5%) | 94.22 ± 5.67% (6.0%) | 47.93 ± 8.98% (18.7%) | |
| EHGP10–P90 | KNNSEN_3 | 78.63 ± 8.60% (10.9%) | 83.56 ± 12.47% (14.9%) | 76.58 ± 14.2% (18.5%) | |
| EHGP50 | KNNSEN_4 | 73.19 ± 4.31% (5.9%) | 91.78 ± 7.15% (7.8%) | 52.07 ± 9.39% (18.0%) |
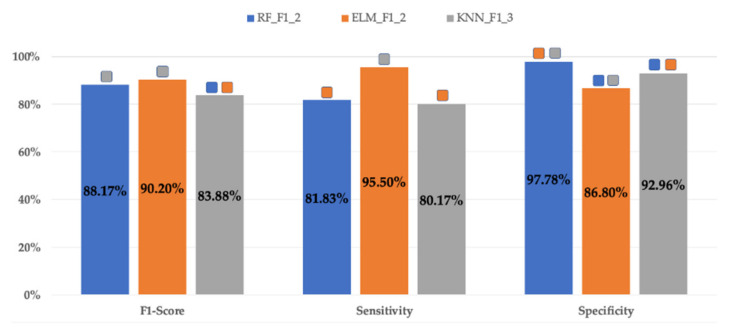
3.4. Comparison of Classifiers
The metrics for RF, ELM and KNN classifiers with the best performance (best F1-score in validation dataset) are shown in Figure 5. All of them corresponded to F1-score optimization criteria. ELMF1_2 achieved the highest F1-score (90.2 ± 4.43%) with statistically significant differences with KNNF1_3 (83.88 ± 10.31%) but not with RFF1_2 (88.17 ± 8.34%). RFF1_2 and ELMF1_2 presented statistically significant differences in terms of sensitivity and specificity, the sensitivity being highest for ELMF1_2 (95.5 ± 4.61% vs. 81.83 ± 12.9%) and the specificity for RFF1_2 (97.78 ± 4.2% vs. 86.8 ± 7.14%). Apart from having shown the lowest F1-score, KNNF1_3 showed the lowest sensitivity (80.17 ± 15.17%) and statistically lower specificity (92.96 ± 5.86%) than RFF1_2.
Figure 5.
Mean values of different classifier metrics for validation datasets in the 30 data partitions obtained for the best RF, ELM and KNN classifiers. Significant differences (p < 0.05) of the classifiers and metrics with the others are marked with  RFF1_2;
RFF1_2;  ELMF1_2;
ELMF1_2;  KNNF1_2.
KNNF1_2.
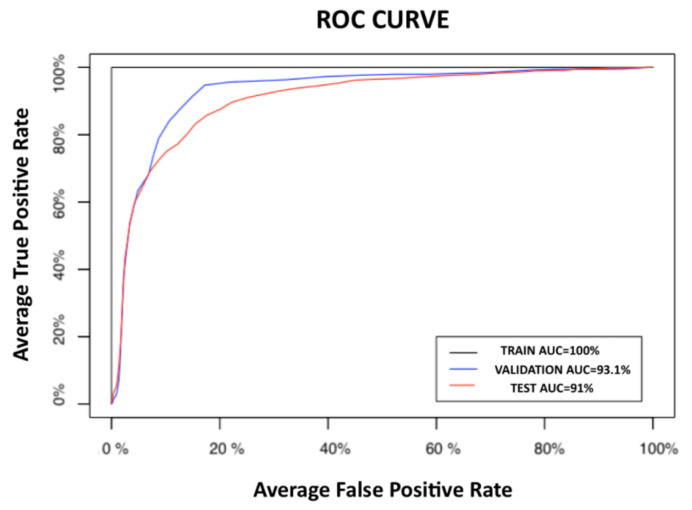
Bearing in mind that in the clinical scenario for the application of these classifiers, the prediction of preterm delivery, a false positive diagnosis is preferable to stopping treating a false negative (premature that has been identified as a false threat), the classifier with the best performance was the ELMF1_2, that is the one that makes a combined use of obstetric and the 50th percentile of EHG parameters. Figure 6 shows the average ROC curves for the ELMF1_2 classifier, with an AUC of 93.1% for the validation dataset and 91.0% for the test dataset.
Figure 6.
Average receiver operating curves (ROCs) for training, validation and test datasets for the ELMF1_2.
4. Discussion
Although several studies deal with the use of EHG for preterm labor prediction in women recorded during regular checkups in a drug-free physiological state [21,22,31,32,34,37,52], the literature is scarce on preterm labor predictive systems in women with TPL under the effect of tocolytic drugs [20], even though tocolytic drugs are usually clinically administered at the first signs of TPL. These drugs were found to modify the EHG characteristics and these changes are dependent on the phase of the drug administration in which the recordings were made [25,26]. Despite this, the usefulness of EHG for the prediction of imminent delivery in women with TPL under tocolytic treatment has already been checked in a previous study using ANN [27]. In the present work we aimed to overcome some limitations of that study, such as the low learning speed associated with ANN backpropagation, by using computationally efficient algorithms such as RF, ELM and KNN. We selected a random forest algorithm, which uses an ensemble of decision tree classifiers, because it is easy to implement and there are reports that it provides a better performance than other classification algorithms, such as ANN [53]. The ELM, a feedforward neural network with a single-hidden layer, accelerates the running speed of the identification model. ELM has been shown to be more stable than ANN, with lower variance of its metrics, and is more suitable for real-time applications in situations that require rapid reactions [54]. ELM has been used in obstetrics to identify labor and nonlabor contractions from EHG recordings [28]. Finally, KNN, a nonparametric and therefore low complex algorithm previously used in EHG classification [55,56], was also assessed in the present work. We studied how the optimization criteria used for the classifiers affected their performance, which has not been clearly indicated in most published studies, regardless of the classification algorithm employed [24,29,31]. We proposed two optimization criteria: F1-score and sensitivity. It is noteworthy that when using sensitivity as optimization criterion the optimal hyperparameters were considered those that provided the best average F1-score in the validation dataset so as to reach a trade-off between sensitivity and specificity. Otherwise, the option is to consider that all women with TPL will deliver prematurely and will therefore require tocolytic drugs and lung maturation corticosteroids, which is a widespread clinical practice nowadays.
Analyzing the influence of the two optimization criteria proposed—F1-score and sensitivity—RF resulted in a unique optimal RF structure, which did not occur for ELM and KNN classifiers, which could have been caused by the nonlinear hyperparameters involved as activation functions and kernels in ELM and KNN classifiers. For ELM, classifiers designed to optimize sensitivity achieved a slight improvement in their sensitivity metrics compared to optimizing the F1-score, at the cost of a decreasing specificity and F1-score. Indeed, in the case of ELM, for both optimization criteria (F1-score and sensitivity) the sensitivity metrics always exceed those of specificity, with values over 90% in validation and 86% in test. This behavior, not observed in KNN, is especially appropriate in the design of imminent labor predictive systems in women with TPL. On the other hand, the KNN metrics did not show statistically significant differences between both optimization criteria for the same input dataset.
The highest F1-score value in validation dataset were obtained for RFF1_2 (88.17 ± 8.34%) and ELMF1_2 (90.2 ± 4.43%), both with the 50th percentile of EHG and obstetric data inputs. They also showed the highest sensitivity (81.83 ± 12.9% and 95.5 ± 4.61%). The good performance of RF metrics agrees with previous studies. Idowu et al. analyzed the performance of several machine learning algorithms for preterm labor detection using the TPEHG database from Physionet and found that random forest performed the best, with a specificity of 86%, sensitivity of 97%, and AUROC of 94% compared with penalized logistic regression and a rule-based classifier [57]. Ren et al. compared the performance of several classifiers based on EHG signals from the TPEHG Physionet database (routine checkups) to differentiate term and preterm deliveries. They used empirical mode decomposition to obtain Intrinsic Mode Functions and then entropy values, and found that RF and AdaBoost outperformed support vector machine, multilayer perceptron, Bayesian network, and simple logistic regression [31].
We consider that ELMF1_2 provides a better performance than RFF1_2 due to its higher sensitivity, which is decisive in this application, as previously mentioned. In this regard, Chen and Hao developed an ELM classifier based on EHG to differentiate labor and nonlabor contractions, manually segmented from the PhysioNet Icelandic 16-electrode Electrohysterogram Database, also reporting high sensitivity metrics [28]. Chen et al. assessed the performance of stacked sparse autoencoder (SSAE), SVM and ELM to identify labor contractions using the Icelandic Database [30], obtaining a slightly better performance for SSAE but without carrying out statistical tests. ELMF1_2 metrics are slightly higher than those previously obtained using the same EHG recording database with an ANN classifier, for both validation and test groups (F1-score of 84.3 ± 5.0%, sensitivity of 86.5 ± 7.4% and specificity of 81.5 ± 7.3 for the validation dataset with ANN and F1-score of 80.3 ± 5.5%, sensitivity of 81.6 ± 9.4% and specificity of 78.8 ± 5.8% for the test dataset) [27]. Indeed, AUC values for ELMF1_2 in validation and test were over 93%, similar to those reported in the literature for preterm labor predictive systems based on EHG recordings during regular checkups [12,21,22,31,37,55,58], and slightly higher than those achieved in imminent labor prediction in women with TPL using ANN (AUC validation 91.8 ± 3.2%, AUC test 87.1 ± 4.3%) [27]. This could be due to the fact that in order to avoid overfitting, the two optimization criteria were applied to the validation dataset, whereas in our previous work the square root of the training and validation F1-score was optimized [27].
The F1-score and sensitivity metrics of the KNN classifiers underperformed RF and ELM in the validation dataset. These results are consistent with those obtained by Fergus et al. when using different classifiers to distinguish between preterm and term birth with the TPEHG database, without a test group but with cross validation [55]. KNN provided worse results than decision trees and polynomial classifiers. Indeed KNN is greatly reliant on the input features’ dimensionality and the training dataset [40,43], resulting in lower values for its metrics [59,60]. However, in the present study KNN classifiers showed a high generalization capability with very similar metrics between validation and test.
With reference to the discriminatory capacity of the classifiers depending on the four different input data sets, the 50th or 10th–90th percentiles of EHG parameters with or without obstetric parameters, different outcomes were observed. In general, the RF classifier metrics were little influenced by the input dataset, although the use of obstetric parameters seems to slightly improve their specificity. This is in agreement with previous studies: Obstetric parameters such as cervical length or fetal fibronectin show high negative predictive but low positive predictive capabilities [8,61]. ELM algorithms also presented very similar metrics for the four sets of proposed input parameters when using the same optimization criterion. In fact, when only EHG characteristics were used, there were no differences in any of the ELM classifier metrics and adding obstetric data improved specificity. On the other hand, the KNN classifier metrics were highly dependent on the input dataset. The best F1-score in the validation dataset for KNN was obtained for KNNF1_3 and KNNSens_3 (83.88 ± 10.31% and 79.9 ± 9.72%, respectively) for both optimization criteria, with the 10th–90th percentiles of EHG and obstetric data inputs. These results agree with Mas-Cabo et al., who obtained a higher discrimination capability between term and preterm births in the 10th and 90th percentiles of EHG parameters in women recorded during routine checkups [20].
Despite the good results obtained, the present study still has certain shortcomings. Firstly, a larger database would be more representative of the target population and would further corroborate the performance of this imminent labor prediction system. Increasing the database would also allow contextualization of the EHG records, allowing the phase of tocolytic treatment in which they were obtained to be considered, since previous works revealed a significant effect of this drug on the EHG parameters, especially on spectral and nonlinear ones [25]. Secondly, even with a larger database we would have to deal with inter-class data imbalance. In the present work there were about 25% fewer women delivering ≤7 days than >7 days, which is in agreement with preterm prevalence in women with TPL [62]. The SMOTE oversampling technique was used here to tackle this problem. Weighted classifiers or boosting ensemble learning could bring about more reliable prediction systems. Thirdly, the use of PCA to reduce the input parameters’ dimensionality makes it difficult to discern which of them are the best to discriminate imminent labor in women with TPL without considering nonlinear relationships, which are often present in biological systems [63]. In future work we aim to use other feature selection techniques that will allow us to determine an optimized feature subset, such as random forest or particle swarm optimization, among others [64,65], to develop low complexity classifiers that are easy to understand with improved metrics. Finally, a robust algorithm to automatically remove artefacted EHG signals or identify EHG-Bursts before feature extraction would help the development of imminent labor prediction systems for clinical practice. Even though some studies have already been carried out on this [66,67,68,69], it is still one of the main obstacles that prevents the clinical use of EHG
5. Conclusions
The present work confirms that it is possible to predict imminent labor in women with TPL undertaking tocolytic treatment by computationally efficient algorithms based on EHG and obstetric parameters. RF and ELM with the 50th percentile of EHG and obstetric input parameters provided the highest F1-score values for the validation dataset, but ELM outperformed RF sensitivity metrics. The use of the 10th–90th percentiles did not result in a significant improvement of these classifier metrics over the 50th percentile. As for the two optimization criteria analyzed for classifiers’ design (F1-score and sensitivity), RFs and KNN were barely affected, but for ELM optimizing sensitivity slightly increases sensitivity compared to optimizing F1-score, but seriously reduces specificity and therefore F1-score. KNN classifier performance was highly sensitive to the input dataset and the test metrics revealed a high generalization capability.
Appendix A
Table A1.
Hyperparameters optimized for each classifier and gridsearch carried out (in brackets).
| RF Hyperparameters |
ELM Hyperparameters |
KNN Hyperparameters |
|---|---|---|
| Number of trees (100, 200, 500, and 750) | Number of neurons in the hidden layer (100, 500, 750, 1000, 2000, and 30,000); | Number of neighbors (1, 3, 5, and 7) |
| Maximum depth of these trees (6, 10, and unlimited) | Activation function (hyperbolic tangent and sigmoid). | Kernel used for weighting the distances (triangular, Biweight and Epanechnikov). |
| Cost of division based on the criterion of gain of information were optimized (0.001, 0.2, and 0.5) |
Table A2.
Hyperparameters’ combination for the optimal RF classifiers in validation.
| Opt. Criterion | Inputs | Classifier | Number of Neurons | Activation Function |
|---|---|---|---|---|
| F1-score | EHGP10–P90 + Obs | ELMF1_1 | 500 | Sigmoid |
| EHGP50 + Obs | ELMF1_2 | 500 | Sigmoid | |
| EHGP10–P90 | ELMF1_3 | 500 | Sigmoid | |
| EHGP50 | ELMF1_4 | 500 | Sigmoid | |
| Sensitivity | EHGP10–P90 + Obs | ELMSEN_1 | 750 | Sigmoid |
| EHGP50 + Obs | ELMSEN_2 | 1000 | Sigmoid | |
| EHGP10–P90 | ELMSEN_3 | 750 | Sigmoid | |
| EHGP50 | ELMSEN_4 | 500 | Sigmoid |
Table A3.
Hyperparameters’ combination for the optimal ELM classifiers in validation.
| Opt. Criterion | Inputs | Classifier | Number of Neurons | Activation Function |
|---|---|---|---|---|
| F1-score | EHGP10–P90 + Obs | ELMF1_1 | 500 | Sigmoid |
| EHGP50 + Obs | ELMF1_2 | 500 | Sigmoid | |
| EHGP10–P90 | ELMF1_3 | 500 | Sigmoid | |
| EHGP50 | ELMF1_4 | 500 | Sigmoid | |
| Sensitivity | EHGP10–P90 + Obs | ELMSEN_1 | 750 | Sigmoid |
| EHGP50 + Obs | ELMSEN_2 | 1000 | Sigmoid | |
| EHGP10–P90 | ELMSEN_3 | 750 | Sigmoid | |
| EHGP50 | ELMSEN_4 | 500 | Sigmoid |
Table A4.
Hyperparameters’ combination for the optimal KNN classifiers in validation.
| Opt. Criterion | Inputs | Classifier | Number of Neighbors | Kernel |
|---|---|---|---|---|
| F1-score | EHGP10–P90 + Obs | KNNF1_1 | 2 | Triangular |
| EHGP50 + Obs | KNNF1_2 | 7 | Biweight | |
| EHGP10–P90 | KNNF1_3 | 2 | Triangular | |
| EHGP50 | KNNF1_4 | 7 | Biweight | |
| Sensitivity | EHGP10–P90 + Obs | KNNSEN_1 | 7 | Triangular |
| EHGP50 + Obs | KNNSEN_2 | 7 | Epanechnikov | |
| EHGP10–P90 | KNNSEN_3 | 5 | Triangular | |
| EHGP50 | KNNSEN_4 | 7 | Triangular |
Author Contributions
Conceptualization, G.P.-B., Y.Y.-L. and A.P.M.; methodology, G.P.-B. and Y.Y.-L.; software, J.P.-T.; validation, G.P.-B., Y.Y.-L. and J.P.-T.; formal analysis, G.P.-B.; and Y.Y.-L., investigation, G.P.-B., Y.Y.-L., J.P.-T. and J.G.-C.; resources, V.D., A.P.M., A.R.P. and R.M.-O.; data curation, R.M.-O. and V.D.; writing—original draft preparation G.P.-B.; writing—review and editing, G.P.-B., Y.Y.-L. and J.G.-C.; visualization, G.P.-B. and Y.Y.-L.; supervision, G.P.-B. and Y.Y.-L.; project administration, G.P.-B., Y.Y.-L., J.G.-C. and A.P.M.; funding acquisition, G.P.-B. and Y.Y.-L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Spanish Ministry of Economy and Competitiveness, the European Regional Development Fund (MCIU/AEI/FEDER, UE RTI2018-094449-A-I00-AR); by the Generalitat Valenciana (AICO/2019/220).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of the “Hospital Universitari i Politècnic la Fe” of Valencia (Spain) (protocol code 2018/0530 and date of 9th of January 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to contain information that could compromise the privacy of participants.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Behrman R.E., Butler A.S. Preterm Birth: Causes, Consequences, and Prevention. Preterm Birth: Causes, Consequences, and Prevention. National Academies Press; Washington, DC, USA: 2007. [DOI] [PubMed] [Google Scholar]
- 2.Levels and Trends in Child Mortality Report 2019 United Nations Children’s Fund; UN Inter-agency group for child mortality estimation.United Nations Children’s. [(accessed on 1 April 2021)]; Available online: https://www.unicef.org/media/79371/file/UN-IGME-child-mortality-report-2020.pdf.pdf.
- 3.Howson C.P., Kinney M.V., McDougall L., Lawn J.E., Born Too Soon Preterm Birth Action Group Born too soon: Preterm birth matters. Reprod. Health. 2013;10(Suppl. 1):S1. doi: 10.1186/1742-4755-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Godeluck A., Godeluck A., Gérardin P., Lenclume V., Mussard C., Robillard P.Y., Sampériz S., Benhammou V., Truffert P., Ancel P.Y., et al. Mortality and severe morbidity of very preterm infants: Comparison of two French cohort studies. BMC Pediatr. 2019;19:360. doi: 10.1186/s12887-019-1700-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roberts D., Brown J., Medley N., Dalziel S.R. Antenatal Corticosteroids for Accelerating Fetal Lung Maturation for Women at Risk of Preterm Birth. Cochrane Database of Systematic Reviews. Volume 2017. John Wiley and Sons Ltd.; Hoboken, NJ, USA: 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garfield R.E., Maner W.L. Physiology and electrical activity of uterine contractions. Semin. Dev. Biol. 2007;18:289–295. doi: 10.1016/j.semcdb.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.E Esplin M.S., Elovitz M.A., Iams J.D., Parker C.B., Wapner R.J., Grobman W.A., Simhan H.N., Wing D.A., Haas D.M., Silver R.M., et al. Predictive accuracy of serial transvaginal cervical lengths and quantitative vaginal fetal fibronectin levels for spontaneous preterm birth among nulliparous women. JAMA J. Am. Med. Assoc. 2017;317:1047–1056. doi: 10.1001/jama.2017.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berghella V., Hayes E., Visintine J., Baxter J.K. Fetal Fibronectin Testing for Reducing the Risk of Preterm Birth. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd.; Hoboken, NJ, USA: 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lucovnik M., Chambliss L.R., Garfield R.E. Costs of unnecessary admissions and treatments for ‘threatened preterm labor’. Am. J. Obstet. Gynecol. 2013;209:217.e1–217.e3. doi: 10.1016/j.ajog.2013.06.046. [DOI] [PubMed] [Google Scholar]
- 10.Grover C.M., Posner S., Kupperman M., Washington E.A. Term delivery after hospitalization for preterm labor: Incidence and costs in california. Prim. Care Update Ob Gyns. 1998;5:178. doi: 10.1016/S1068-607X(98)00086-9. [DOI] [PubMed] [Google Scholar]
- 11.Most O., Langer O., Kerner R., Ben David G., Calderon I. Can myometrial electrical activity identify patients in preterm labor? Am. J. Obstet. Gynecol. 2008;199:378. doi: 10.1016/j.ajog.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Maner W.L., Garfield R.E. Identification of human term and preterm labor using artificial neural networks on uterine electromyography data. Ann. Biomed. Eng. 2007;35:465–473. doi: 10.1007/s10439-006-9248-8. [DOI] [PubMed] [Google Scholar]
- 13.Devedeux D., Marque C., Mansour S., Germain G., Duchêne J. Uterine electromyography: A critical review. Am. J. Obstet. Gynecol. 1993;169:1636–1653. doi: 10.1016/0002-9378(93)90456-S. [DOI] [PubMed] [Google Scholar]
- 14.Chkeir A., Fleury M.J., Karlsson B., Hassan M., Marque C. Patterns of electrical activity synchronization in the pregnant rat uterus. BioMedicine. 2013;3:140–144. doi: 10.1016/j.biomed.2013.04.007. [DOI] [Google Scholar]
- 15.Mas-Cabo J., Ye-Lin Y., Garcia-Casado J., Alberola-Rubio J., Perales A., Prats-Boluda G. Uterine contractile efficiency indexes for labor prediction: A bivariate approach from multichannel electrohysterographic records. Biomed. Signal Process. Control. 2018;46:238–248. doi: 10.1016/j.bspc.2018.07.018. [DOI] [Google Scholar]
- 16.Vinken M.P.G.C., Rabotti C., Mischi M., Oei S.G. Accuracy of frequency-related parameters of the electrohysterogram for predicting preterm delivery: A review of the literature. Obs. Gynecol. Surv. 2009;64:529–541. doi: 10.1097/OGX.0b013e3181a8c6b1. [DOI] [PubMed] [Google Scholar]
- 17.Horoba K., Jezewski J., Matonia A., Wrobel J., Czabanski R., Jezewski M. Early predicting a risk of preterm labour by analysis of antepartum electrohysterographic signals. Biocybern. Biomed. Eng. 2016;36:574–583. doi: 10.1016/j.bbe.2016.06.004. [DOI] [Google Scholar]
- 18.Mischi M., Chen C., Ignatenko T., de Lau H., Ding B., Oei S.G.G., Rabotti C. Dedicated Entropy Measures for Early Assessment of Pregnancy Progression From Single-Channel Electrohysterography. IEEE Trans. Biomed. Eng. 2018;65:875–884. doi: 10.1109/TBME.2017.2723933. [DOI] [PubMed] [Google Scholar]
- 19.Fele-Zorz G., Kavsek G., Novak-Antolic Z., Jager F., Fele-Žorž G., Kavšek G., Novak-Antolič Ž., Jager F., Fele-Zorz G., Kavsek G., et al. A comparison of various linear and non-linear signal processing techniques to separate uterine EMG records of term and pre-term delivery groups. Med. Biol. Eng. Comput. 2008;46:911–922. doi: 10.1007/s11517-008-0350-y. [DOI] [PubMed] [Google Scholar]
- 20.Mas-Cabo J., Ye-Lin Y., Garcia-Casado J., Díaz-Martinez A., Perales-Marin A., Monfort-Ortiz R., Roca-Prats A., López-Corral Á., Prats-Boluda G., Diaz-Martinez A., et al. Robust Characterization of the Uterine Myoelectrical Activity in Different Obstetric Scenarios. Entropy. 2020;22:743. doi: 10.3390/e22070743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fergus P., Idowu I., Hussain A., Dobbins C. Advanced artificial neural network classification for detecting preterm births using EHG records. Neurocomputing. 2016;188:42–49. doi: 10.1016/j.neucom.2015.01.107. [DOI] [Google Scholar]
- 22.Acharya U.R., Sudarshan V.K., Rong S.Q., Tan Z., Lim C.M., Koh J.E., Nayak S., Bhandary S.V., Qing S., Tan Z., et al. Automated detection of premature delivery using empirical mode and wavelet packet decomposition techniques with uterine electromyogram signals. Comput. Biol. Med. 2017;85:33–42. doi: 10.1016/j.compbiomed.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 23.Borowska M., Brzozowska E., Kuć P., Oczeretko E., Mosdorf R., Laudański P. Identification of preterm birth based on RQA analysis of electrohysterograms. Comput. Methods Programs Biomed. 2018;153:227–236. doi: 10.1016/j.cmpb.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 24.Degbedzui D.K., Yüksel M.E. Accurate diagnosis of term–preterm births by spectral analysis of electrohysterography signals. Comput. Biol. Med. 2020;119:1–8. doi: 10.1016/j.compbiomed.2020.103677. [DOI] [PubMed] [Google Scholar]
- 25.Mas-Cabo J., Prats-Boluda G., Perales A., Garcia-Casado J., Alberola-Rubio J., Ye-Lin Y. Uterine electromyography for discrimination of labor imminence in women with threatened preterm labor under tocolytic treatment. Med. Biol. Eng. Comput. 2019;57:401–411. doi: 10.1007/s11517-018-1888-y. [DOI] [PubMed] [Google Scholar]
- 26.Mas-Cabo J., Prats-Boluda G., Ye-Lin Y., Alberola-Rubio J., Perales A., Garcia-Casado J. Characterization of the effects of Atosiban on uterine electromyograms recorded in women with threatened preterm labor. Biomed. Signal Process. Control. 2019;52:198–205. doi: 10.1016/j.bspc.2019.04.001. [DOI] [Google Scholar]
- 27.Mas-Cabo J., Prats-Boluda G., Garcia-Casado J., Alberola-Rubio J., Monfort-Ortiz R., Martinez-Saez C., Perales A., Ye-Lin Y. Electrohysterogram for ann-based prediction of imminent labor in women with threatened preterm labor undergoing tocolytic therapy. Sensors. 2020;20:2681. doi: 10.3390/s20092681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen L., Hao Y. Feature Extraction and Classification of EHG between Pregnancy and Labour Group Using Hilbert-Huang Transform and Extreme Learning Machine. Comput. Math. Methods Med. 2017:1–9. doi: 10.1155/2017/7949507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peng J., Hao D., Yang L., Du M., Song X., Jiang H., Zhang Y., Zheng D. Evaluation of electrohysterogram measured from different gestational weeks for recognizing preterm delivery: A preliminary study using random Forest. Biocybern. Biomed. Eng. 2020;40:352–362. doi: 10.1016/j.bbe.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen L., Hao Y., Hu X. Detection of preterm birth in electrohysterogram signals based on wavelet transform and stacked sparse autoencoder. PLoS ONE. 2019;14:1–16. doi: 10.1371/journal.pone.0214712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ren P., Yao S., Li J., Valdes-Sosa P.A., Kendrick K.M. Improved Prediction of Preterm Delivery Using Empirical Mode Decomposition Analysis of Uterine Electromyography Signals. PLoS ONE. 2015;10:1–16. doi: 10.1371/journal.pone.0132116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mas-Cabo J., Prats-Boluda G., Garcia-Casado J., Alberola Rubio J., Perales Marín A.J., Ye Lin Y. Design and Assessment of a Robust and Generalizable ANN-Based Classifier for the Prediction of Premature Birth by means of Multichannel Electrohysterographic Records. J. Sens. 2019:1–13. doi: 10.1155/2019/5373810. [DOI] [Google Scholar]
- 33.Terrien J., Marque C., Karlsson B. Spectral characterization of human EHG frequency components based on the extraction and reconstruction of the ridges in the scalogram. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2007;2007:1872–1875. doi: 10.1109/IEMBS.2007.4352680. [DOI] [PubMed] [Google Scholar]
- 34.Alamedine D., Diab A., Muszynski C., Karlsson B., Khalil M., Marque C. Selection algorithm for parameters to characterize uterine EHG signals for the detection of preterm labor. Signal Image Video Process. 2014;8:1169–1178. doi: 10.1007/s11760-014-0655-2. [DOI] [Google Scholar]
- 35.Lemancewicz A., Borowska M., Kuć P., Jasińska E., Laudański P., Laudański T., Oczeretko E., Kuc P., Jasinska E., Laudanski P., et al. Early diagnosis of threatened premature labor by electrohysterographic recordings—The use of digital signal processing. Biocybern. Biomed. Eng. 2016;36:302–307. doi: 10.1016/j.bbe.2015.11.005. [DOI] [Google Scholar]
- 36.Vrhovec J., Macek-Lebar A., Rudel D. 11th Mediterranean Conference on Medical and Biomedical Engineering and Computing. Volume 16. Springer; Berlin/Heidelberg, Germany: 2007. Evaluating Uterine Electrohysterogram with Entropy; pp. 144–147. [Google Scholar]
- 37.Ahmed M.U., Chanwimalueang T., Thayyil S., Mandic D.P. A multi variate multiscale fuzzy entropy algorithm with application to uterine EMG complexity analysis. Entropy. 2017;19:1–18. [Google Scholar]
- 38.Zhang X.S.X.S., Roy R.J., Jensen E.W. EEG complexity as a measure of depth of anesthesia for patients. IEEE Trans. Biomed. Eng. 2001;48:1424–1433. doi: 10.1109/10.966601. [DOI] [PubMed] [Google Scholar]
- 39.Moslem B., Hassan M., Khalil M., Marque C., Diab M.O. Proceedings of the 2009 International Symposium On Bioelectronics; Bioinformatics. RMIT University; Melbourne, Australia: 2009. Monitoring the progress of pregnancy and detecting labor using uterine electromyography; pp. 160–163. [Google Scholar]
- 40.Diab A., Hassan M., Marque C., Karlsson B. Performance analysis of four nonlinearity analysis methods using a model with variable complexity and application to uterine EMG signals. Med. Eng. Phys. 2014;36:761–767. doi: 10.1016/j.medengphy.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 41.Karmakar C.K., Khandoker A.H., Gubbi J., Palaniswami M. Complex correlation measure: A novel descriptor for Poincaré plot. Biomed. Eng. Online. 2009;8:1–12. doi: 10.1186/1475-925X-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roy B., Ghatak S. Nonlinear Methods to Assess Changes in Heart Rate Variability in Type 2 Diabetic Patients. Arq. Bras. Cardiol. 2013;10:317–327. doi: 10.5935/abc.20130181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Naeem S.M., Seddik A.F., Eldosoky M.A. New technique based on uterine electromyography nonlinearity for preterm delivery detection New technique based on uterine electromyography nonlinearity for preterm delivery detection. J. Eng. Technol. Res. 2014;6:107–114. [Google Scholar]
- 44.Chawla N.V., Bowyer K.W., Hall L.O., Kegelmeyer W.P. SMOTE: Synthetic Minority Over-Sampling Technique. J. Artif. Intell. Res. 2002;16:321–357. doi: 10.1613/jair.953. [DOI] [Google Scholar]
- 45.Smrdel A., Jager F. Separating sets of term and pre-term uterine EMG records. Physiol. Meas. 2015;36:341–355. doi: 10.1088/0967-3334/36/2/341. [DOI] [PubMed] [Google Scholar]
- 46.Naeem S.M., Ali A.F., Eldosok Mohamed M.A. Comparison between Using Linear and Non-linear Features to classify Uterine Electromyography Signals of Term and Preterm Deliveries; Proceedings of the National Radio Science Conference, NRSC; Cairo, Egypt. 16–18 April 2013; pp. 1–11. [Google Scholar]
- 47.Bekkar M., Akrouf Alitouche T. Imbalanced Data Learning Approaches Review. Int. J. Data Min. Knowl. Manag. Process. 2013;3:15–33. doi: 10.5121/ijdkp.2013.3402. [DOI] [Google Scholar]
- 48.Wright M.N., Ziegler A. Ranger: A fast implementation of random forests for high dimensional data in C++ and R. J. Stat. Softw. 2017;77:1–17. doi: 10.18637/jss.v077.i01. [DOI] [Google Scholar]
- 49.Huang G.B., Zhu Q.Y., Siew C.K. Extreme learning machine: Theory and applications. Neurocomputing. 2006;70:489–501. doi: 10.1016/j.neucom.2005.12.126. [DOI] [Google Scholar]
- 50.Hechenbichler K., Schliep K. Weighted k-Nearest-Neighbor Techniques and Ordinal Classification Projektpartner Weighted k-Nearest-Neighbor Techniques and Ordinal Classification. Ludwig-Maximilians-Universität München; München, Germany: 2004. 2004 Discussion Paper 399, SFB 386. [DOI] [Google Scholar]
- 51.Flach P.A., Kull M. Precision-Recall-Gain Curves: PR Analysis Done Right. Adv. Neural Inf. Process. Syst. 2015;28:1–9. [Google Scholar]
- 52.Alamedine D., Khalil M., Marque C. Comparison of different EHG feature selection methods for the detection of preterm labor. Comput. Med. 2013;2013:1–9. doi: 10.1155/2013/485684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Esteves G., Mendes-Moreira J. Churn perdiction in the telecom business; Proceedings of the 11th International Conference on Digital Information Management, ICDIM 2016; Porto, Portugal. 19–21 September 2016; pp. 254–259. [Google Scholar]
- 54.Kayabasi A., Yildiz B., Aslan M.F., Durdu A. Comparison of ELM and ANN on EMG Signals Obtained for Control of Robotic-Hand; Proceedings of the 10th International Conference on Electronics, Computers and Artificial Intelligence, ECAI 2018; Iasi, Romania. 28–30 June 2018; pp. 1–5. [Google Scholar]
- 55.Fergus P., Cheung P., Hussain A., Al-Jumeily D., Dobbins C., Iram S. Prediction of preterm deliveries from EHG signals using machine learning. PLoS ONE. 2013;8:e77154. doi: 10.1371/journal.pone.0077154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mohamed Bedeeuzzaman A.S. Preterm Birth Prediction Using EHG Signals. Int. J. Sci. Res. Eng. Trends. 2019;5:2395–2566. [Google Scholar]
- 57.Idowu I.O., Fergus P., Hussain A., Dobbins C., Khalaf M., Casana Eslava R.V., Keight R. Artificial Intelligence for Detecting Preterm Uterine Activity in Gynacology and Obstertric Care; Proceedings of the 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing; Pervasive Intelligence and Computing; Liverpool, UK. 26–28 October 2015; pp. 215–220. [DOI] [Google Scholar]
- 58.You J., Kim Y., Seok W., Lee S., Sim D., Suk K.P., Park C. Multivariate Time–Frequency Analysis of Electrohysterogram for Classification of Term and Preterm Labor. J. Electr. Eng. Technol. 2019;14:897–916. doi: 10.1007/s42835-019-00118-9. [DOI] [Google Scholar]
- 59.Murthy H.S.N., Meenakshi D.M. ANN, SVM and KNN Classifiers for Prognosis of Cardiac Ischemia—A Comparison. Bonfring Int. J. Res. Commun. Eng. 2015;5:7–11. doi: 10.9756/BIJRCE.8030. [DOI] [Google Scholar]
- 60.Aditya S., Tibarewala D.N. Comparing ANN, LDA, QDA, KNN and SVM algorithms in classifying relaxed and stressful mental state from two-channel prefrontal EEG data. Int. J. Artif. Intell. Soft Comput. 2012;3:143. doi: 10.1504/IJAISC.2012.049010. [DOI] [Google Scholar]
- 61.Pandey M., Chauhan M., Awasthi S. Interplay of cytokines in preterm birth. Indian J. Med. Res. 2017;146:316–327. doi: 10.4103/ijmr.IJMR_1624_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Van Zijl M.D., Koullali B., Mol B.W.J., Pajkrt E., Oudijk M.A. Prevention of preterm delivery: Current challenges and future prospects. Int. J. Womens Health. 2016;8:633–645. doi: 10.2147/IJWH.S89317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hira Z.M., Gillies D.F. A review of feature selection and feature extraction methods applied on microarray data. Adv. Bioinform. 2015;2015:198363. doi: 10.1155/2015/198363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen R.C., Dewi C., Huang S.W., Caraka R.E. Selecting critical features for data classification based on machine learning methods. J. Big Data. 2020;7:1–26. doi: 10.1186/s40537-020-00327-4. [DOI] [Google Scholar]
- 65.Rostami M., Forouzandeh S., Berahmand K., Soltani M. Integration of multi-objective PSO based feature selection and node centrality for medical datasets. Genomics. 2020;112:4370–4384. doi: 10.1016/j.ygeno.2020.07.027. [DOI] [PubMed] [Google Scholar]
- 66.Ye-Lin Y., Garcia-Casado J., Prats-Boluda G., Alberola-Rubio J., Perales A. Automatic Identification of Motion Artifacts in EHG Recording for Robust Analysis of Uterine Contractions. Comput. Math. Methods Med. 2014;2014:1–11. doi: 10.1155/2014/470786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Happillon T., Muszynski C., Zhang F., Marque C., Istrate D. Detection of Movement Artefacts and Contraction Bursts Using Accelerometer and Electrohysterograms for Home Monitoring of Pregnancy. IRBM. 2018;39:379–385. doi: 10.1016/j.irbm.2018.10.008. [DOI] [Google Scholar]
- 68.Hao D., Peng J., Wang Y., Liu J., Zhou X., Zheng D. Evaluation of convolutional neural network for recognizing uterine contractions with electrohysterogram. Comput. Biol. Med. 2019;113:1–8. doi: 10.1016/j.compbiomed.2019.103394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Muszynski C., Happillon T., Azudin K., Tylcz J.-B., Istrate D., Marque C. Automated electrohysterographic detection of uterine contractions for monitoring of pregnancy: Feasibility and prospects. BMC Pregnancy Childbirth. 2018;18:1–8. doi: 10.1186/s12884-018-1778-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to contain information that could compromise the privacy of participants.