Abstract
Prostate cancer (PCa) is globally the second most diagnosed cancer type and the most common cause of cancer-related deaths in men. Family history of PCa, hereditary breast and ovarian cancer (HBOC) and Lynch syndromes (LS), are among the most important risk factors compared to age, race, ethnicity and environmental factors for PCa development. Hereditary prostate cancer (HPCa) has the highest heritability of any major cancer in men. The proportion of PCa attributable to hereditary factors has been estimated in the range of 5–15%. To date, the genes more consistently associated to HPCa susceptibility include mismatch repair (MMR) genes (MLH1, MSH2, MSH6, and PMS2) and homologous recombination genes (BRCA1/2, ATM, PALB2, CHEK2). Additional genes are also recommended to be integrated into specific research, including HOXB13, BRP1 and NSB1. Importantly, BRCA1/BRCA2 and ATM mutated patients potentially benefit from Poly (ADP-ribose) polymerase PARP inhibitors, through a mechanism of synthetic lethality, causing selective tumor cell cytotoxicity in cell lines. Moreover, the detection of germline alterations in MMR genes has therapeutic implications, as it may help to predict immunotherapy benefits. Here, we discuss the current knowledge of the genetic basis for inherited predisposition to PCa, the potential target therapy, and the role of active surveillance as a management strategy for patients with low-risk PCa. Finally, the current PCa guideline recommendations are reviewed.
Keywords: hereditary prostate cancer, genetic testing, genotype–phenotype correlation, surveillance
1. Introduction
Prostate cancer (PCa) is globally the second most diagnosed cancer type in men [1] and the most common cause of cancer-related deaths, with an estimated 1,600,000 cases and 366,000 deaths annually [2]. Established risk factors include older age, African American race, and a positive family history of PCa [3].
PCa is clinically a very heterogeneous disease; indeed, many patients show an aggressive disease with progression and metastasis while other patients show a slow disease with low propensity to progression [2]. Histologically, these tumors are measured in terms of the Gleason score that evaluates how much the biotic prostatic specimen is similar to the normal prostate gland [2].
Compared to sporadic cases, HPCa is characterized by an early age onset, an aggressive disease progress and locally advanced stage. Furthermore, men with HPCa have a higher risk of recurrence after surgery, while there is not much difference between HPCa and sporadic PCa regarding overall survival [4].
Family history of PCa, hereditary breast and ovarian cancer (HBOC) syndrome and Lynch syndrome (LS) are among the most important risk factors compared to age, race, ethnicity and environmental factors for the development of PCa [5,6,7,8,9] and this risk is estimated at 40%−50 % [3]. Men with a brother or father diagnosed with prostate cancer have a two- to four-fold greater risk of developing PCa [10].
Hereditary prostate cancer (HPCa) has the highest heritability of any major cancer in men [11]. Since PCa is asymptomatic in the early stage of the disease, it is critical to develop an individualized approach for early detection [12]. Patients with early onset of PCa associated to family members affected with PCa or other heritable cancers are suitable candidates to undergo a genetic testing [6]. Over time, about 170 susceptibility loci for HPCa, accounting for ~33% of familial prostate cancer risks, have been identified with genome wide association studies (GWAS) [13,14]. Further insights have suggested that mutations in the different DNA damage repair (DDR) genes (BRCA1, BRCA2, CHEK2, ATM and PALB2) and in the DNA mismatch repair genes (MMR) (MLH1, MSH2, MSH6 and PMS2), are biomarkers of HPCa [6,15,16]. Importantly, while many genes have a clear association with HPCa risk, others carry a still unknown clinical significance with a poorly defined cancer risk [16]. Besides, there is strong emerging evidence that mutation in some genes may predict the response to poly-ADO ribose polymerase (PARP) inhibitors and platinum-based chemotherapy in prostate cancer [17].
Here, we report on the current knowledge of the genetic basis for inherited predisposition to PCa, the potential target therapy, and the role of active surveillance as a management strategy for patients with low-risk PCa. Finally, the current PCa guideline recommendations are reported.
2. Epidemiology of Hereditary Prostate Cancer
The proportion of PCa attributable to hereditary factors has been estimated to be 5–15% [6]. HPCa is due to gene mutations with autosomal dominant inheritance and characterized by early onset [18]. Heidegger et al. reported that the cumulative proportion of PCa cases attributable to high-risk susceptibility alleles is 43% for men diagnosed <55 years, but only 9% for men >85 years [6].
HPCa incidence is two and three times higher in African Americans men than European and Asian men, respectively [12,15]. This outcome may be influenced by lifestyles such as diet and obesity, as well as screening patterns within an ethnic/racial community [15]. Likewise, genetic etiology differs among population diversity [6]. For example, single-nucleotide polymorphisms (SNPs) that had been previously reported in white or Asian populations were not found in Afro-American men. In line with these studies, other genome-wide association studies (GWAS) did not replicate most of the previously reported loci identified in European or Asian descent populations [6]. Accordingly, a novel locus on chromosome 10p14 (SNP, rs7918885), exclusively detected in African men, has been described [6]. This SNP, rs7918885, is localized at 10p14 within an intron of a long non-coding RNA (lncRNA RP11-543F8.2) 360 kb centromeric of GATA3 [19]. Additionally, several BRCA1/2 variants of unknown significance (VUS) were observed in African American patients more frequently than in Caucasian Americans (4.6 % vs. 1.6 %, respectively) [1].
On the other hand, there is one specific chromosomal locus at 8q24 (near the MYC proto-oncogene) where several SNPs have been associated with PCa susceptibility among various ethnicities [15].
3. Genes Involved in the Predisposition to Hereditary Prostate Cancer
HPCa susceptibility loci were found on all chromosomes except 15, 16, 21, and 23 [11].
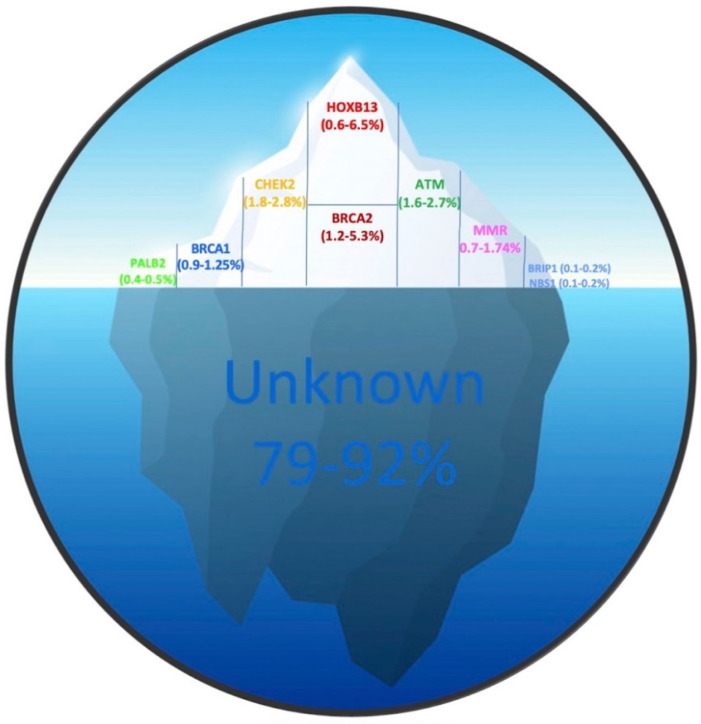
In 0.6–6.25% of cases HPCa is due to HOXB13 mutations, in 1.2–5.3% to BRCA2, in 1.8–2.8% to CHECK2, in 1.6–2.7% to ATM, in 0.7–1.74% to MMR, in 0.9–1.25% to BRCA1, in 0.4–0.5% to PALB2, in 0.1–0.2% to BRP1 and NBS1 and in the remaining percentage to other currently unknown genes (Figure 1) [13,15,18,20,21].
Figure 1.
Frequency of mutations found in HPCa related genes. The proportion of PCa attributable to hereditary factors has been estimated to be 5–15%. The upper part of the iceberg constitutes 7.4–21% and indicates the gene mutation frequencies known so far, while the lower part, constituting 79–92%, represents the portion of genes not yet identified. Partner and localizer of BRCA2 (PALB2); Breast cancer type1 (BRCA1); Checkpoint kinase 2 (CHEK2); Breast cancer type2 (BRCA2); Homeobox B13 (HOXB13); ATM serine/threonine kinase (ATM); Mismatch Repair (MMR); BRCA1 interacting protein C-terminal helicase 1 (BRIP1); Nijmegen Breakage Syndrome 1 (NBS1).
To date, the genes more consistently associated to HPCa susceptibility have been reported by the National Comprehensive Cancer Network (NCCN) guidelines and include LS associated genes (MLH1, MSH2, MSH6, and PMS2) and homologous recombination genes (BRCA1/2, ATM, PALB2, CHEK2) [22]. Additional genes, including the above mentioned HOXB13, BRP1 and NSB1, are also recommended in specific research or clinical contexts.
HOXB13 is a homeobox transcription factor, localized on chromosome 17. Mutations have been observed in 0.7% to 1.4% cases of prostate cancer and in 6% of PCa with early onset [23]. In 2012, a study demonstrated for the first time that patients with the recurring germline mutation G84E in HOXB13 had significantly higher odds for developing PCa than men without the mutation [24]. Subsequent studies have confirmed a more modest association with an increased risk of PCa, particularly in the hereditary setting [25]. In a more recent study, HOXB13 mutation has been associated with an increased HPCa risk (OR = 6.6) [6]. To date, HOXB13 remains the most widely replicated and specific PCa susceptibility gene [26].
It is well known that BRCA genes are considered as the principal biomarkers for the genetic study of hereditary breast and ovarian cancers [27]; however, several authors have also reported an association in patients affected with HPCa, which is part of HBOC syndrome [8,15,28]. BRCA1 and BRCA2 are tumor suppressor genes, localized on chromosomes 17 and 13, respectively, involved in repairing DNA double strand breaks by the conservative approach of homologous recombination (HR) [29]. The germline BRCA1 mutations increase the risk of HPCa by 3.8-fold in men aged <65 years, and germline BRCA2 mutations by 8.6-fold [8]. In a study performed on a cohort of 2019 HPCa patients, 0.9% germline mutations in BRCA1 and 3% in BRCA2 were observed [30]. Moreover, Edwards et al. reported a median overall survival (OS) of all BRCA2 mutation carriers of 4.8 years vs. 8.5 years for non-carriers [28]. Additionally, as expected, in isolated and/or consanguineous populations, heterozygous carriers of one founder BRCA mutation exhibited increased susceptibility to HPCa [28]. Otherwise, some authors have reported different data. Indeed, Rantapero et al. described a frequency of zero cases of pathogenic BRCA2 variants in 122 lethal cases, suggesting that BRCA2 could not play a major role in aggressive and lethal PCa [14]. Another study has shown that BRCA2 deletions accounted for a very small number of HPCa (1–2%) even in cases with early onset and proven family history [6].
The CHEK2 gene, localized on chromosome 22, encodes for a tumor suppressor that participates in the DNA-damage signaling pathway. Alterations in CHEK2 have been found in HBOC syndrome, with an increased risk of breast, ovarian, colon, thyroid and kidney cancer, and have been linked to Li-Fraumeni syndrome [15]. Germline CHEK2 mutations have been also associated with increased HPCa risk with an overall risk of 1.9–3.3% [6]. In a study performed on metastatic PCa patients from Sweden CHEK2 was also the most frequently mutated DNA repair gene (3.8%) highlighting the importance of CHEK2 mutations for aggressive PCa in the Nordic population [31].
Another gene of interest for HPCa is ATM, as recently reviewed in [32]. ATM is positioned on chromosome 11 and represents a key player in the DNA damage response pathway. Homozygous loss-of-function mutations in ATM cause ataxia telangiectasia syndrome. Of note, it is also one of the known HBOC susceptibility genes; indeed, ATM mutation carriers have an increased risk for breast, colorectal, gastric and pancreatic cancers. More recently, the use of sequencing panels containing DNA-repair genes has also allowed the identification of germline ATM alterations in men with PCa. [15]. The relative risk of metastatic prostate cancer in ATM carriers was 6.3% [6].
Interestingly, patients with germline mutations in the MMR genes, MLH1, MSH2, MSH6 and PMS2, located on chromosome 3, 2, 2 and 7, respectively, have a HPCa risk [30,33]. However, the estimated prevalence of MMR gene mutations is low when compared to alterations in genes of other DDR pathways [34]. As already known, the MMR genes are associated with LS that predisposes to colorectal and endometrial cancer, although several other extracolonic cancers have been reported, including gastric, small bowel, pancreatic, brain, prostate and urothelial [35,36]. The relative risk of HPCa in MMR mutation carriers has been estimated in the interval 2.0–3.7% [23], even though a previous study reported a nearly five-fold increased risk of HPCa onset in LS men, but without earlier onset or a more aggressive phenotype [37]. Additionally, studies have also highlighted a considerably higher PCa risk for MSH2 mutation carriers compared to MLH1 and MSH6 [38].
PALB2 is localized on chromosome 16; originally identified as a BRCA2-interacting protein, it is an essential component of the BRCA complex formation. Indeed, PALB2 acts as a bridge between BRCA1 and BRCA2 to form a BRCA complex that initiates homologous recombination [39]. Various PALB2 mutations are involved in HBOC predisposition, particularly associated with breast and pancreatic cancers, whereas few studies have reported PALB2 variants in HPCa patients. In the analysis by Pritchard et al., PALB2 germline mutations were detected in 0.4% of HPCa cases [18]. Nicolosi reported pathogenic PALB2 germline variants in 0.5% of unselected PCa patients [18,40]. Apart from the rarity of reported PALB2 alterations, recent findings have supported an increasing role of PALB2 in HPCa disease [41].
A few less-studied candidate genes have been proposed to be associated with HPCa predisposition, which are involved in a small percentage of HBOC cases. One of the candidate genes is BRIP1. This gene is localized on chromosome 17, encodes a DNA helicase, which binds directly to the BRCT repeats of BRCA1, and is therefore involved in DSB repair [42]. To date, few studies have reported potentially damaging BRIP1 variants in PCa patients; particularly, Kote-Jarai et al. found a moderate risk of PCa in a set of familial and young-onset PCa patients carrying a recurrent BRIP1 truncating variant [43].
Another gene of interest is NBS1, which is located on chromosome 8 and encodes another protein involved in DSB repair since it is responsible for the localization of the complex and for the interactions with other proteins belonging to repair signaling complexes [44]. A specific founder variant (c.657del5) has been associated with a three-fold increased risk of PCa in patients under 60 years, and a four-fold increased risk for male carriers with a positive family history [45].
Other inherited alterations in genes associated with DNA repair have been identified in HPCa studies, including RAD51C, RAD51D, and TP53 genes. Unfortunately, very little data is currently available about the existence of such associations. Thus, further studies with an expanded set of genes are warranted to validate these and other proposed candidates as HPCa susceptibility genes [18,46].
4. Pathogenetic Mechanisms of PCa Onset
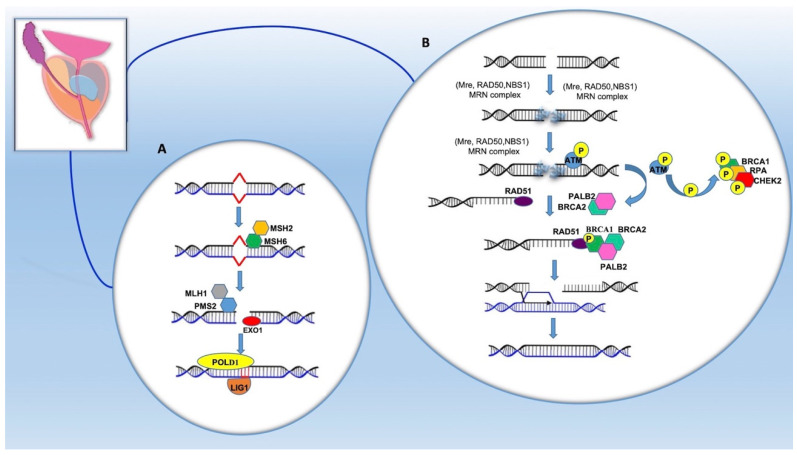
Alterations in the DNA damage repair (DDR) pathways have been recently recognized as an important contributor to PCa [17]. The DDR system includes multiple distinct pathways, two of which are: (a) homologous recombination (HR), which relies on BRCA1, BRCA2 and ATM, and (b) mismatch repair (MMR), which involves MLH1, MSH2, MSH6 and PMS2 [47]. Repair of the breaks in the DNA double strand (DSB) requires the intervention of several proteins encoded by genes such as BRCA1, BRCA2, ATM, RAD51, PALB2 and others. These genes are tumor suppressors and some of them cooperate with each other (Figure 2).
Figure 2.
DNA repair pathway in the prostate epithelium involving hereditary prostate cancer (HPCa) related genes: mismatch repair or MMR (A); homologous recombination or HR (B). See text for detailed description. mutS homolog 2 (MSH2); mutS homolog 6 (MSH6); mutL homolog 1 (MLH1); PMS1 homolog 2 (PMS2); Exonuclease 1 (EXO1); δ polymerase (POLD1); DNA ligase I (LIG1); Meiotic recombination 11 (MRE11); Double strand break repair protein (RAD50); Nijmegen disruption syndrome proteins (NBS1); Replication protein A (RPA); ATM serine/threonine kinase (ATM); Breast cancer type1 (BRCA1); Checkpoint kinase 2 (CHEK2); RAD51 recombinase (RAD51); Breast cancer type2 (BRCA2); Partner and localizer of BRCA2 (PALB2).
HR is activated during the synthesis, or S phase, of the cell cycle, and requires a sister chromatid as a template to repair damaged DNA. If repair does not occur, the damage can lead to deletions, chromosomal aberrations and aneuploidies [48].
In the event of damage, the disruption of the DSB is recognized by the poly (ADP-ribose) polymerase 1 (PARP1) complex, a protein that scans the genome and detects DSB lesions [49]. PARP1 marks the site of damage by binding the ribose ADP molecules to chromatin-bound proteins surrounding the break [50]. ADP-ribose units are essential for the recruitment of MRN complex, formed by MRE11 (meiotic recombination 11), RAD50 and NBS1 (Nijmegen disruption syndrome) proteins.
The localization of MRN triggers the signaling of downstream repair factors, mediated by ATM and ATR kinases. ATM is then recruited to the rupture sites by the MRN complex, self-phosphorylates and monomerizes. Once activated, ATM phosphorylates various substrates including BRCA1, the MRN complex and Replication protein A (RPA). Moreover, ATM phosphorylates histone H2AX which induces a signal cascade involving protein mediators such as CHEK2 [34]. The exonuclease activity of MRN complex produces single-stranded DNA (ssDNA) surrounding the break [50,51,52,53]. RPA recognizes ssDNA and recruits ATR, thereby activating an additional cascade that includes ATR substrates such as CHEK1 and other effector proteins. Once activated, ATM phosphorylates various substrates including BRCA1, the MRN complex and RPA. MRN remodels the ends leaving ssDNA to which RAD51 is linked, localized by BRCA2, which assumes a multimeric filamentous structure and mediates the invasion of the helix of the homologous chromosome to look for a homology region with which to repair the damage. PALB2 acts as a bridge between BRCA1 and BRCA2 to form a BRCA complex that then binds RAD51 [54]. Holliday junctions are created, also characteristic of crossing-over; finally, thanks to δ polymerase, the structure is resolved, and the damage is repaired [34].
The MMR pathway recognizes and removes DNA base pair mismatches occurring because of replication errors [55]. Genes encoding for MSH and MLH family proteins are involved in this pathway. These MutSa Complex heterodimers (MSH2/MSH6) and MutLb (MLH1/PMS1) or MutSb (MSH2/MSH3) and MutLa (MLH1/PMS2) bind to the surrounding DNA [56]. Initially, there is the recognition of the mismatch by the heterodimer MSH2/MSH6, followed by the recruitment of MLH1/PMS2. The activity of the PMS2 endonuclease determines synchronous stranded nicks close to the mismatch, where the EXO1 exonuclease interacts with the nuclear antigen of proliferating cells (PCNA), starting the resection of the DNA from 5’ to 3’. Finally, the strand is resynthesized by the δ polymerase (POLD1) and bound by DNA ligase I (LIG1) [56].
Disruption of these DNA repair pathways leads to increased mutagenesis and genomic instability with the consequent accumulation of genomic aberrations [57]. It is established that PCa tissues display recurrent genomic aberrations, including alterations at 8p (containing the prostate-specific tumor suppressor NKX3–1), 8q (c-MYC amplification), 10q23 (PTEN loss), 17q (TP53 locus) and Xq12 (AR gene amplification) as well as TMPRSS2:ERG gene fusion or other fusion events involving additional ETS family members [58]. Although a clear relationship between these alterations and germline mutations in HPCa has not yet been demonstrated, they could be, at least in part, due to the disruption of DNA repair pathways. Indeed, PCa tumors with germline BRCA2 mutations displayed significantly more copy number alterations (CNA) than sporadic tumors. Specifically, the deletion of chromosome 8p was observed as the most recurrent somatic CNA, whereas chromosome 8q alteration, at 8q24.21, was the most frequent gain. Interestingly, this study also revealed that high CNA level was already present in 50% of the morphologically normal prostate tissue from BRCA2 mutation carriers [59].
Besides, although carried out on metastases from castrate-resistant PCa, a study evidenced a correlation between some alterations of critical tumorigenesis regulators and structural variants. For instance, deletions were significantly higher in tumors with biallelic BRCA2 pathogenic variants (including germline mutations). Additionally, biallelic CDK12 inactivation was associated with a significant increase of tandem duplications whereas biallelic TP53 inactivation was significantly associated with elevated inverted rearrangement frequency. Overall, these data suggest that specific genomic alteration signatures could develop from different germline mutations [60].
5. Mutations and Genotype–Phenotype Correlation
The G84E mutation of HOXB13 gene was found to be more prevalent in European families, suggesting a possible founder effect [5,61]. Additional HOXB13 mutations have also been detected in PCa cases in other racial or ethnic groups, including African (G216C and R229G) and Asian (G135E) populations, but the frequency and impact of these mutations on the PCa risk remains to be confirmed [20]. It has been highlighted that HOXB13 G84E mutation is associated with early-onset, familial and high-risk of PCa [15,62].
Regarding BRCA genes, 64% of the BRCA2 mutations found in HPCa are frameshift, 31% missense and 5% splice. In BRCA1 gene, 63% of the mutations found are missense, 31% frameshift and 6% splice [38]. Besides, in a study conducted on PCa patients mutated in BRCA1/2, a more aggressive phenotype was observed [30,62].
Remarkably, germline alterations were independent factors of a diagnosis at younger age and of a more aggressive phenotype. Besides, BRCA2 mutation carriers exhibited a poorer survival rate (61.8%) compared to men without a BRCA2 mutation (94.3%). BRCA2 pathogenic variants were also associated with an increased risk of high-grade disease and progression to metastatic castrate resistant prostate cancer (mCRPC). Besides, BRCA2 germline mutations provided a greater contribution to PCa increased risk compared to BRCA1 [3,8,11,15,23,28,63].
BRCA1 mutation carriers younger than 65 years showed a two-fold increase of PCa relative risk, whereas no evidence of an elevated risk in men aged 65 or older was observed. The BRCA1 Q356R was preferentially transmitted to affected men of white families with early-onset HPCa at an estimated odds ratio of 2.25 [20]. Several studies have evaluated the contribution of BRCA1 (185delAG and 5382insC) and BRCA2 (6174delT) founder mutations to PCa risk among Ashkenazi Jewish men. Overall, BRCA2 mutations conferred at least a three-fold elevated risk of high grade PCa, while BRCA1 mutations conferred a lower risk [38,64,65].
In the CHEK2 gene, 44% of the mutations found in HPCa are frameshift, 31% missense and 25% splice. CHEK2 variants have been associated with PCa predisposition in several studies, highlighting the importance of CHEK2 mutations for aggressive PCa [14]. Moreover, a significantly higher prevalence of germline alterations in the CHEK2 gene was observed in the metastatic cases, although no association with age at diagnosis was reported [15]. Of note, the c.1100delC mutation was the most commonly observed CHEK2 mutation and was found to have a significantly higher frequency in lethal cases compared than in the low-risk PCa patients, supporting the importance of this mutation for lethal PCa [14]. Moreover, the c.1100delC mutation and I157T increased the PCa risk by 3.3% and 1.8%, respectively [15].
As regards the ATM gene, 50% of mutations found in HPCa are missense, 37% frameshift and 13% splice. ATM variants were associated to aggressive and lethal phenotype of HPCa disease [66]. Recently, ATM deficiency has been shown to promote the progression of castration-resistant PCa [14]. Moreover, the ATM 3161G (P1054R) variant was significantly associated with an increased risk of developing PCa [20].
Concerning MMR genes, 47% of the mutations found in HPCa are frameshift, 44% missense and 9% splice. In a recent study, the MMR gene mutation carriers with PCa displayed microsatellite instability and loss of MMR gene expression, implicating this pathway in prostate cancer formation. The PCa patients with MMR deficiency showed aggressive clinical and pathological features [67]. Significantly, MMR gene mutation carriers developed PCa in earlier age and at a higher frequency than expected. Moreover, MMR mutation carriers displayed a 3% higher risk of PCa compared to the general population [20].
In PALB2 gene, 83% of the mutations found in HPCa are frameshift and 17% missense. Despite the rarity of reported PALB2 aberrations, recent findings have supported an increasing role of PALB2 in PCa, particularly in metastatic cases [68].
Additional genomic studies based on Next-Gen Sequencing (NGS) can allow the identification of other genes potentially involved in HPCa onset. Moreover, future studies on genotype-phenotype correlation would be needed and these studies they should converge in a meta-analysis that could provide a greater understanding of HPCa.
6. Therapeutic Target
The therapeutic landscape of PCa is constantly evolving thanks to clinical trial benefits, new therapeutics, use of NGS, advanced functional imaging and the better use of existing therapies in the early-stage disease. PCa initiation and disease progression are driven by AR signaling [69]. It is known that the PCa is unique in its dependence on androgen for growth and progression, and androgen deprivation therapy (ADT) is an effective treatment for patients with advanced disease over 75 years [70]. However, when a castration-resistant state occurs, the patient is more likely to die of PCa than other causes [71]. Alterations in AR signaling in metastatic castration resistant PCa (mCRPC) cause persistent AR activation, which in turn leads to AR amplification, AR splice variants and intra-tumoral androgen biosynthesis [70]. Therapeutic strategies involve the use of enzalutamide, an AR antagonist that blocks AR translocation function, and abiraterone which inhibits androgen biosynthesis [67].
Recently, mCRPC patients with germline defects in DNA damage repair showed a decreased response to AR targeted therapy [6]. In contrast, other authors reported an improved response to second generation ADT with administration of drugs, including abiraterone or enzalutamide, in men with BRCA or ATM mutations compared to those without deleterious germline mutations [67].
Thus, the mutation status of genes involved in HPCa may have an impact on therapeutic strategies [16,72]. For instance, mutated patients potentially benefit from PARP inhibitors such as Olaparib, rucaparib, niraparib and telazoparib [1,18], through a mechanism of synthetic lethality, causing selective tumor cell cytotoxicity in cell lines.
The Food and Drug Administration (FDA) approved the drug Olaparib for the treatment of patients with mCRPC, mutated in BRCA1/BRCA2 and ATM genes. In line with previously described results, in patients with germinal BRCA2 or ATM mutations, treatment with the PARP inhibitor Olaparib has a durable antitumor activity [73]. Moreover, based on further studies, PARP inhibitor rucaparib was also added for mCRPC patients with deleterious BRCA alterations previously treated with ADT, but not for patients with ATM mutations [74]. Besides, other studies have shown that the presence of DDR defects may also be predictive of a higher likelihood of a response to carboplatin-based chemotherapy in patients with mCRPC [75].
The detection of germline alterations in MMR genes also has therapeutic implications, as it may help to predict immunotherapy benefits. Recent studies have suggested that metastatic PCa patients with germline MMR pathogenic variants may have a particular sensitivity to hormonal therapies, as well as a possible response to PD−1 inhibitors [76]. Additional clinical studies reported either a complete or a partial response to PD−1 inhibitors in mCRPC patients [77]. Based on these findings, the FDA has recently approved the PD−1 inhibitor pembrolizumab (KEYTRUDA) for the treatment of patients with microsatellite instability-high (MSI-H)/MMR-deficient [78]. The use of genetically based therapies sustains the importance of applying genetic testing in the clinical management of these PCa patients.
The PD−1 pathway includes the programmed death protein−1 (PD−1) and its ligands, PD-L1 (B7-H1) and PD-L2 (B7-DC). This pathway has emerged as a mechanism for immune tolerance whereby tumor cells can suppress an antitumor immune response. Taking into account the high aggressivity of PCa, particularly mCRPC, and the success of PD−1/PD-L1 blockade in other cancers, patients with mCRPC could benefit from correct modulation of the immune system and, hence, from the use of checkpoint inhibitors [18]. The activity of the checkpoint inhibitors is limited to a certain percentage of patients, depending on the tumor type. This is especially important in tumors with low objective response rates to immunotherapy, such as PCa. Tumor cell PD-L1 expression is a predictive biomarker for PD−1 inhibitor sensitivity. Examples of subgroups of PCa patients with enriched PD-L1 expression are patients with aggressive tumors and with tumors harboring somatic or germline DDR mutations, including patients with HPCa. The presence of DDR or MMR mutations may favor the activity of checkpoint immunotherapy. Therefore, the use of PD−1/PD-L1 inhibitors for advanced prostate cancer should be encouraged in the setting of clinical trials and to identify the patient subgroups that can benefit from these therapies. Furthermore, it would be interesting and useful to develop a biomarker panel to predict benefit and response of these and other checkpoint inhibitors [78].
Current National Comprehensive Cancer Network (NCCN) guidelines recommend three gene expression-based tests for PCa prognosis in men with low or favorable intermediate risk disease: Decipher, Oncotype DX Prostate, and Prolaris [79]. Particularly, the current recommendations evaluate the role of each of the panels in both prostate biopsy and post-surgery settings. Overall, these tests provide more precise estimates of disease aggressiveness, beyond clinical factors, and they could help to guide on appropriate disease management and therapy. Thus, they could also be used for active surveillance in HPCa. Among the current commercially available tests are ExoDx and Liquid CDx. The test ExoDxTM Prostate (IntelliScore) detects RNA from three genes (ERG, PCA3, and SPDEF) that have been linked to the development and progression of prostate cancer. The RNA is encapsulated in lipid membrane-coated structures called exosomes that are excreted by cancer cells into urine. FoundationOne Liquid CDx is an FDA-approved next generation sequencing-based in vitro diagnostic device that targets 324 genes utilizing circulating cell-free DNA (cfDNA) isolated from plasma derived from the anti-coagulated peripheral whole blood of cancer patients [80]. The latter test includes HPCa related genes. The detection of a mutation and, hence, of a positivity to the somatic test in the genes related to HPCa, must be confirmed in the germline. In this way, identifying the mutation in the HPCa susceptibility gene, the test allows an early diagnosis of HPCa.
7. Genetic Counselling, Guidelines for Genetic Test and Surveillance
Early onset of aggressive PCa combined with family history of PCa or other heritable cancers are strong predictors for a hereditary component arguing that those patients are candidates to undergo genetic testing.
To date, guidelines give no consistent recommendations about which patients, and at what stage of the disease, should undergo genetic testing [6]. In Table 1 we report a summary of the current guidelines on HPCa.
Table 1.
Summary of the current guidelines on hereditary prostate cancer.
| Johns Hopkins group (1998) [83] | One of the following criteria must be included for the consideration of familial prostate cancer (PCa): 1. Three or more first-degree relatives with PCa; 2. Three successive generations of PCa; 3. Two relatives with PCa diagnosed at age ≤55 years |
| American College of Medical Genetics (2015) [84] | Genetic testing should be considered if one of the following criteria is met: 1. Three or more first-degree relatives with PCa; 2. Two or more first-degree relatives diagnosed with PCa at age ≤55 years; 3. Gleason grade > 7 PCa and a family history of ≥2 individuals with breast, ovarian, or pancreatic cancer |
| American Society of Urology (AUA 2017) European Association of Urology (EAU 2019) [6] |
Recommend offering germline genetic testing for BRCA1, BRCA2, ATM, PALB2, and FANCA to all patients with high risk or metastatic disease regardless of family history. For those patients with a lower-risk disease, germline genetic testing should be considered when: 1. There is a strong family history (brother or father or multiple family members diagnosed with PCa <60 years), 2. Known germline abnormalities and/or more than one family member with breast, ovarian, or pancreatic cancer (suggestive of BRCA2 mutations), 3. More than one family member with Lynch syndrome (LS) |
| National Comprehensive Cancer Network (2018) [22] | Recommend genetic testing of BRCA in PCa patients with one of the conditions listed below: 1. A history of Gleason grade ≥7 PCa regardless of age and ≥1 close relative with breast cancer (age ≤ 50 years) and/or invasive ovarian cancer; 2. Patients with prostate cancer (Gleason ≥ 7) who have two relatives with breast, pancreatic, or PCa (Gleason ≥ 7) diagnosed at any age; 3. A personal history of metastatic PCa (radiographic evidence of or biopsy-proven disease) |
| National Comprehensive Cancer Network (updated version 2019) [6] | States that. if next generation sequencing (NGS) is used, the panel must include BRCA1, BRCA2, ATM, CHEK2, PALB2, MLH1, MSH2, MSH6, and PMS2 |
Men with highly aggressive PCa typically receive treatment whereas active surveillance is recommended for patients with low grade PCa and with non-metastatic PCa; therefore, they are unlikely to be harmed by their cancer during a period of observation. The much-debated topic concerns the characteristics that make a patient eligible for surveillance; indeed, different centers have proposed different criteria to guide clinicians in determining the eligibility of a patient for active surveillance. Commonly used criteria include low-grade and low-volume tumor on biopsy and low prostatic specific antigen (PSA) level [81].
PSA is a serine protease produced by both malignant and normal cells [82]. However, in healthy individuals, it is secreted into glandular ducts in concentrations million times higher than in plasma whereas, in PCa affected patients, a damage occurring in the secretory pathways leads to PSA leaking into the extracellular space [82]. Consequently, increased PSA level in serum can be observed, thus representing a sign of both inflammatory and neoplastic processes in the prostate [82]. A more recently used method to measure PSA is prostate health Index (PHI), which combines PSA, free PSA and p2PSA4. To date, compared to traditional PSA methods, the accuracy of PHI value still remains to be defined [82].
In Western countries, the widely accepted threshold value of PSA is 4.0 ng/mL. For value > 4.0 ng/mL, it is recommended to perform a biopsy to verify or exclude the presence of PCa. However, this cut-off value is not uniform across the ethnicities [82].
It is well known that the PSA test is widely used for PCa screening; however, it can also provide false positive data causing unnecessary prostate biopsies and inaccurate diagnosis of low-risk PCa. Indeed, careful studies support that a PSA screening every two years reduces the death rate for PCa of about 80% compared with annual screening while decreasing both the number of tests and the chance of a false-positive test by 50% and overdiagnosis by 30%. However, the various organizations declare in their guidelines that the ideal screening interval, is unknown. Indeed, The American Cancer Society recommends screening every two years screening for men aged ≥50 years and with a PSA level of <2.5 ng/mL and testing every year for PSA level ≥2.5 ng/mL. The AUA recommends biennial testing for men aged 55–69 years. The NCCN recommends 2- to 4-year intervals for men aged 45–74 years with PSA <1 ng/mL and 1–2 years for men with PSA ≥1 ng/mL. Recently, the US Preventive Services Task Force (USPSTF) suggests more observational studies are needed to evaluate the harms and the benefits of the different screening intervals [85].
The Gleason Score is a grade that the pathologist assigns after prostate biopsy or during trans-urethral resection for prostatic hyperplasia. It describes the aggressiveness of the cancer and directs the urologist to a definitive treatment or active surveillance of the patient [86].
Men with a personal history of Gleason ≥7 PCa with a family history of a BRCA1/2 mutation, or one close relative with ovarian or breast cancer at age <50 years, or two relatives with breast, pancreas, or Gleason ≥ 7 PCa at any age, should undergo genetic counseling [6].Currently, the IMPACT multicenter observational study is evaluating the utility of performing these screenings, it being understood that men with age 40–69 are offered annual PSA and the threshold for prostatic biopsy is PSA > 3 ng/mL [30].
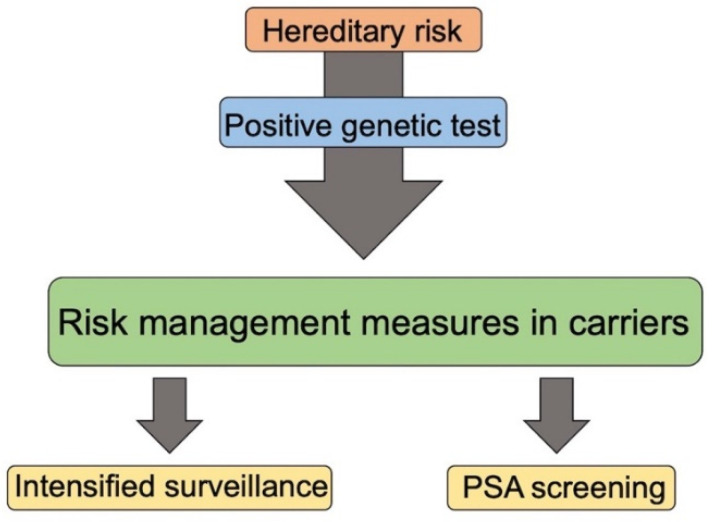
Regarding the surveillance to be carried out on unaffected men with mutations in DDR or MMR genes belonging to HBOC and LS families, there are no currently comprehensive guidelines regarding HPCa prevention. In a multicenter study concerning early diagnosis for men carrying BRCA2 mutations, systematic PSA screening was recommended (Figure 3) [87].
Figure 3.
Management of unaffected family members with positive genetic test.
The IMPACT study evaluated PSA screening in men with a known genetic PCa predisposition due to BRCA1/2 mutations and found that a value of PSA >3 ng/mL is more strongly predictive in BRCA carriers than noncarriers [16,88].
Other authors reported that BRCA mutations and MMR deficiency and HOXB13 are associated with a higher Gleason score [67,76,89]. However, their clinical application, including their utility in screening programs, is as yet undefined and, in any case, none have been found sensitive and specific enough to replace the PSA measure [30].
8. Liquid Biopsy
The frequency of alterations appears to differ among genes involved in the DNA-repair pathways at different stages of the PCa. The evaluation of the results of NGS sequencing performed on tumor cells does not always give accurate results, since the evolutionary history of the sub-clonal lineages of tumor cells present in the sample may not provide those alterations that were formed later and, hence, may not offer a sufficient vision of current disease biology. Specific strategies have now evolved to overcome the issues of inter- and intra-tumoral heterogeneity and of the chronological changes occurring during the disease progression. Among them, liquid biopsy allows the evaluation of circulating cell-free DNA from blood samples [15].
Although tissue biopsy is the “gold standard” for diagnosing cancer, the removal of tumor tissue by surgery or, in some cases, through needle biopsy, is an invasive process. In addition, sometimes the difficulty of reaching the tumor can limit the ability of sampling. Moreover, several studies have indicated that the genetic information contained in the circulating tumor cells may provide important information on the tumor, such as the probability of response or relapse after treatment or on the response to a specific therapy. Thus, liquid biopsy may represent a promising and non-invasive examination to be performed [90,91].
Liquid biopsy involves the analysis of tumor material from readily accessible body fluid samples. The main utilized approaches include the analyses of circulating tumor DNA (ctDNA), RNA, including micro RNAs, proteins, and mitochondrial DNA, as well as circulating tumor cells, or extracellular vesicles. The analysis of ctDNA was evaluated in the definition for profiling tumor genomics in patients with metastatic prostate cancer. Particularly, patients with metastatic carcinoma displayed high ctDNA values, while the values were very low in patients with localized carcinoma [92]. Therefore, this analysis could make a positive contribution to the early diagnosis of HPCa, which is a more aggressive disease. Liquid biopsies have also emerged as an attractive strategy to study the PCa molecular setting in a slightly invasive manner. Although it has been widely used in the study of PCa, this strategy still needs to be implemented before being adopted in the routine clinical use [90,91]. In this context, a suitable and comprehensive NGS panel with HPCa associated genes for mutational analysis is still lacking and should be established.
To date, there are still several issues in the interpretation of tumor-profiling results. To this purpose, the American College of Medical Genetics has promulgated guidelines to aid laboratories in best reporting of findings in hereditary cancer genes. It is recommended that in the presence of an alteration in a hereditary cancer gene, the patient should be referred to a cancer genetics program for further evaluation [15].
9. Conclusions
HPCa remains an important clinical entity, with a spectrum of epidemiologic and genetic risk factors. Advances in NGS sequencing will allow new discoveries of PCa genetic predisposition. A more accurate knowledge of the mechanisms of HPCa predisposition could be brought by individualized PCa screening and treatment. As for the main cancer predisposition syndromes, including Lynch and HBOC, commercial NGS panels contain a large number of cancer susceptibility genes to detect mutations in patients with inherited cancer predisposing syndromes [46,93]. This useful approach has the advantage of being cost effective and to have a relatively feasible handling of raw data through validated bioinformatics pipelines; moreover, the detection of VUS, which are difficult to interpret in the clinical management, is quite limited [46,93]. Noteworthy, targeted sequencing of 94 cancer genes has also been recently used in probands with early onset/familial prostate cancer and has allowed successful identification of novel putative PCa predisposing germline mutations [94]. However, by multigene panels genetic testing, between 70–92% of patients (depending on the cancer syndrome), still remain mutation-negative or undiagnosed [93,95]. Thus, the use of Whole Exome Sequencing (WES) and Whole Genome Sequencing (WGS) strategies will be the preferred method in the near future when decreased costs and improved pipeline analyses will also make these strategies more suitable in the clinical setting. In this context, NGS methods will be useful even in searching for novel common variants conferring small to modest effect sizes by GWAS in patients with PCa predisposition [96]. Furthermore, approaches like RNA sequencing may allow the identification of genetic causes that are not recognizable by genomic DNA screening [93].
The liquid biopsy approach could allow not only an early diagnosis but also an analysis of the genetic tumor characteristics that are already present and that are relevant to providing the best therapy. For instance, molecular testing is able to identify patients who could benefit from PARPi treatment or platinum chemotherapy and to determine the cancer risk in family members. Current ongoing clinical trials may provide new indications on combinations of PARPi and immune checkpoint inhibitors with alterations in MMR and HR genes. To date, guidelines give no uniformed recommendations on which patients should undergo genetic testing and, at the same time, on the tests to be performed. Therefore, a clear policy regarding genetic testing could point to a more accurate active surveillance as a management strategy for patients with low-risk PCa.
Author Contributions
Conceptualization, M.T.V.; data curation, G.D. and G.C.; visualization, G.C., L.P. and L.A.; writing—original draft preparation, G.D. and M.R.; writing—review and editing, A.C. and M.T.V.; supervision, A.C., M.C. and A.M.M. All authors have read and agree to the published version of the manuscript.
Funding
This research was funded by ordinary funds from University of Campania “Luigi Vanvitelli”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Virtanen V., Paunu K., Ahlskog J.K., Varnai R., Sipeky C., Sundvall M. PARP Inhibitors in Prostate Cancer—The Preclinical Rationale and Current Clinical Development. Genes. 2019;10:565. doi: 10.3390/genes10080565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Testa U., Castelli G., Pelosi E. Cellular and Molecular Mechanisms Underlying Prostate Cancer Development: Therapeutic Implications. Medicines. 2019;6:82. doi: 10.3390/medicines6030082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giri V.N., Beebe-Dimmer J.L. Familial prostate cancer. Semin Oncol. 2016;43:560–565. doi: 10.1053/j.seminoncol.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thalgott M., Kron M., Brath J.M., Ankerst D.P., Thompson I.M., Gschwend J.E., Herkommer K. Men with family history of prostate cancer have a higher risk of disease recurrence after radical prostatectomy. World J. Urol. 2018;36:177–185. doi: 10.1007/s00345-017-2122-5. [DOI] [PubMed] [Google Scholar]
- 5.Cooney K.A. Inherited Predisposition to Prostate Cancer: From Gene Discovery to Clinical Impact. Trans. Am. Clin. Climatol. Assoc. 2017;128:14–23. [PMC free article] [PubMed] [Google Scholar]
- 6.Heidegger I., Tsaur I., Borgmann H., Surcel C., Kretschmer A., Mathieu R., Visschere P., Valerio M., van den Bergh R.C.N., Ost P., et al. EAU-YAU Prostate Cancer Working Party. Hereditary prostate cancer—Primetime for genetic testing? Cancer Treat. Rev. 2019;81:101927. doi: 10.1016/j.ctrv.2019.101927. [DOI] [PubMed] [Google Scholar]
- 7.Leongamornlert D., Saunders E., Dadaev T., Tymrakiewicz M., Goh C., Jugurnauth-Little S., Kozarewa I., Fenwick K., Assiotis I., Barrowdale D., et al. Frequent germline deleterious mutations in DNA repair genes in familial prostate cancer cases are associated with advanced disease. Br. J. Cancer. 2014;110:1663–1672. doi: 10.1038/bjc.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ren Z.J., Cao D.H., Zhang Q., Ren P.W., Liu L.R., Wei Q., Wei W.R., Dong Q. First-degree family history of breast cancer is associated with prostate cancer risk: A systematic review and meta-analysis. BMC Cancer. 2019;19:871. doi: 10.1186/s12885-019-6055-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giri V.N., Knudsen K.E., Kelly W.K., Abida W., Andriole G.L., Bangma C.H., Bekelman J.E., Benson M.C., Blanco A., Burnett A., et al. Role of Genetic Testing for Inherited Prostate Cancer Risk: Philadelphia Prostate Cancer Consensus Conference 2017. J. Clin. Oncol. 2018;36:414–424. doi: 10.1200/JCO.2017.74.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barber L., Gerke T., Markt S.C., Peisch S.F., Wilson K.M., Ahearn T., Giovannucci E., Parmigiani G., Mucci L.A. Family History of Breast or Prostate Cancer and Prostate Cancer Risk. Clin. Cancer Res. 2018;24:5910–5917. doi: 10.1158/1078-0432.CCR-18-0370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rebbeck T.R. Prostate Cancer Genetics: Variation by Race, Ethnicity, and Geography. Semin. Radiat. Oncol. 2017;27:3–10. doi: 10.1016/j.semradonc.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kohaar I., Petrovics G., Srivastava S. A Rich Array of Prostate Cancer Molecular Biomarkers: Opportunities and Challenges. Int. J. Mol. Sci. 2019;20:1813. doi: 10.3390/ijms20081813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sokolova A.O., Cheng H.H. Genetic Testing in Prostate Cancer. Curr. Oncol. Rep. 2020;22:5. doi: 10.1007/s11912-020-0863-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rantapero T., Wahlfors T., Kähler A., Hultman C., Lindberg J., Tammela T.L., Nykter M., Schleutker J., Wiklund F. Inherited DNA Repair Gene Mutations in Men with Lethal Prostate Cancer. Genes. 2020;11:314. doi: 10.3390/genes11030314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhen J.T., Syed J., Nguyen K.A., Leapman M.S., Agarwal N., Brierley K., Llor X., Hofstatter E., Shuch B. Genetic testing for hereditary prostate cancer: Current status and limitations. Cancer. 2018;124:3105–3117. doi: 10.1002/cncr.31316. [DOI] [PubMed] [Google Scholar]
- 16.Das S., Salami S.S., Spratt D.E., Kaffenberger S.D., Jacobs M.F., Morgan T.M. Bringing Prostate Cancer Germline Genetics into Clinical Practice. J. Urol. 2019;202:223–230. doi: 10.1097/JU.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 17.Nombela P., Lozano R., Aytes A., Mateo J., Olmos D., Castro E. BRCA2 and Other DDR Genes in Prostate Cancer. Cancers. 2019;11:352. doi: 10.3390/cancers11030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pritchard C.C., Mateo J., Walsh M.F., De Sarkar N., Abida W., Beltran H., Garofalo A., Gulati R., Carreira S., Eeles R., et al. Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer. N. Engl. J. Med. 2016;375:443–453. doi: 10.1056/NEJMoa1603144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook M.B., Wang Z., Yeboah E.D., Tettey Y., Biritwum R.B., Adjei A.A., Tay E., Truelove A., Niwa S., Chung C.C., et al. A genome-wide association study of prostate cancer in West African men. Hum. Genet. 2014;133:509–521. doi: 10.1007/s00439-013-1387-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tan S.H., Petrovics G., Srivastava S. Prostate Cancer Genomics: Recent Advances and the Prevailing Underrepresentation from Racial and Ethnic Minorities. Int. J. Mol. Sci. 2018;19:1255. doi: 10.3390/ijms19041255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pritzlaff M., Tian Y., Reineke P., Stuenkel A.J., Allen K., Gutierrez S., Jackson M., Dolinsky J.S., LaDuca H., Xu J., et al. Diagnosing hereditary cancer predisposition in men with prostate cancer. Genet. Med. 2020;22:1517–1523. doi: 10.1038/s41436-020-0830-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Comprehensive Cancer Network (NCCN) Genetic/Familial High-Risk Assessment: Breast and Ovarian. National Comprehensive Cancer Network; Plymouth Meeting, PA, USA: 2018. Version 1.2018. [Google Scholar]
- 23.Pilarski R. The Role of BRCA Testing in Hereditary Pancreatic and Prostate Cancer Families. Am. Soc. Clin. Oncol. Educ. Book. 2019;39:79–86. doi: 10.1200/EDBK_238977. [DOI] [PubMed] [Google Scholar]
- 24.Ewing C.M., Ray A.M., Lange E.M., Zuhlke K.A., Robbins C.M., Tembe W.D., Wiley K.E., Isaacs S.D., Johng D., Wang Y., et al. Germline mutations in HOXB13 and prostate-cancer risk. N. Engl. J. Med. 2012;12:141–149. doi: 10.1056/NEJMoa1110000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beebe-Dimmer J.L., Hathcock M., Yee C., Okoth L.A., Ewing C.M., Isaacs W.B., Cooney K.A., Thibodeau S.N. The HOXB13 G84E mutation is associated with an increased risk for prostate cancer and other malignancies. Cancer Epidemiol. Biomark. Prev. 2015;24:1366–1372. doi: 10.1158/1055-9965.EPI-15-0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei J., Shi Z., Na R., Wang C.H., Resurreccion W.K., Zheng S.L., Hulick P.J., Cooney K.A., Helfand B.T., Isaacs W.B., et al. Germline HOXB13 G84E mutation carriers and risk to twenty common types of cancer: Results from the UK Biobank. Br. J. Cancer. 2020;123:1356–1359. doi: 10.1038/s41416-020-01036-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vietri M.T., Caliendo G., D’Elia G., Resse M., Casamassimi A., Minucci P.B., Dello Ioio C., Cioffi M., Molinari A.M. Five Italian Families with Two Mutations in BRCA Genes. Genes. 2020;11:1451. doi: 10.3390/genes11121451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edwards S.M., Evans D.G., Hope Q., Norman A.R., Barbachano Y., Bullock S., Kote-Jarai Z., Meitz J., Falconer A., Osin P., et al. Prostate cancer in BRCA2 germline mutation carriers is associated with poorer prognosis. Br. J. Cancer. 2010;7:918–924. doi: 10.1038/sj.bjc.6605822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Powell S.N., Kachnic L.A. Roles of BRCA1 and BRCA2 in homologous recombination, DNA replication fidelity and the cellular response to ionizing radiation. Oncogene. 2003;22:5784–5789. doi: 10.1038/sj.onc.1206678. [DOI] [PubMed] [Google Scholar]
- 30.Castro E., Goh C.L., Eeles R.A. Prostate cancer screening in BRCA and Lynch syndrome mutation carriers. Am. Soc. Clin. Oncol. Educ. Book. 2013 doi: 10.14694/EdBook_AM.2013.33.e50. [DOI] [PubMed] [Google Scholar]
- 31.Mayrhofer M., De Laere B., Whitington T., Van Oyen P., Ghysel C., Ampe J., Ost P., Demey W., Hoekx L., Schrijvers D., et al. Cell-free DNA profiling of metastatic prostate cancer reveals microsatellite instability, structural rearrangements and clonal hematopoiesis. Genome Med. 2018;10:85. doi: 10.1186/s13073-018-0595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nanda N., Roberts N.J. ATM serine/threonine kinase and its role in pancreatic risk. Genes. 2020;11:108. doi: 10.3390/genes11010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cheng H.H., Sokolova A.O., Schaeffer E.M., Small E.J., Higano C.S. Germline and Somatic Mutations in Prostate Cancer for the Clinician. J. Natl. Compr. Cancer Network. 2019;17:515–521. doi: 10.6004/jnccn.2019.7307. [DOI] [PubMed] [Google Scholar]
- 34.Athie A., Arce-Gallego S., Gonzalez M., Morales-Barrera R., Suarez C., Casals Galobart T., Hernandez Viedma G., Carles J., Mateo J. Targeting DNA Repair Defects for Precision Medicine in Prostate Cancer. Curr. Oncol. Rep. 2019;21:42. doi: 10.1007/s11912-019-0790-6. [DOI] [PubMed] [Google Scholar]
- 35.Vietri M.T., D’Elia G., Caliendo G., Casamassimi A., Federico A., Passariello L., Cioffi M., Molinari A.M. Prevalence of mutations in BRCA and MMR genes in patients affected with hereditary endometrial cancer. Med. Oncol. 2021;38:13. doi: 10.1007/s12032-021-01454-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen S.A., Leininger A. The genetic basis of Lynch syndrome and its implications for clinical practice and risk management. Appl. Clin. Genet. 2014;7:147–158. doi: 10.2147/TACG.S51483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Haraldsdottir S., Hampel H., Wei L., Wu C., Frankel W., Bekaii-Saab T., De La Chapelle A., Goldberg R.M. Prostate cancer incidence in males with Lynch syndrome. Genet. Med. 2014;16:553–557. doi: 10.1038/gim.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brandão A., Paulo P., Teixeira M.R. Hereditary Predisposition to Prostate Cancer: From Genetics to Clinical Implications. Int. J. Mol. Sci. 2020;21:5036. doi: 10.3390/ijms21145036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vietri M.T., Caliendo G., Schiano C., Casamassimi A., Molinari A.M., Napoli C., Cioffi M. Analysis of PALB2 in a cohort of Italian breast cancer patients: Identification of a novel PALB2 truncating mutation. Fam. Cancer. 2015;14:341–348. doi: 10.1007/s10689-015-9786-z. [DOI] [PubMed] [Google Scholar]
- 40.Nicolosi P., Ledet E., Yang S., Michalski S., Freschi B., O’Leary E., Esplin E.D., Nussbaum R.L., Sartor O. Prevalence of Germline Variants in Prostate Cancer and Implications for Current Genetic Testing Guidelines. JAMA Oncol. 2019;5:523–528. doi: 10.1001/jamaoncol.2018.6760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Bono J.S., Mateo J., Fizazi K., Saad F., Shore N., Sandhu S., Chi K.N., Sartor O., Agarwal N., Olmos D., et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2020;382:2091–2102. doi: 10.1056/NEJMoa1911440. [DOI] [PubMed] [Google Scholar]
- 42.Ramus S.J., Song H., Dicks E., Tyrer J.P., Rosenthal A.N., Intermaggio M.P., Fraser L., Gentry-Maharaj A., Hayward J., Philpott S., et al. Germline Mutations in the BRIP1, BARD1, PALB2, and NBN Genes inWomen With Ovarian Cancer. J. Natl. Cancer Inst. 2015;107:1. doi: 10.1093/jnci/djv214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kote-Jarai Z., Jugurnauth S., Mulholland S., Leongamornlert D.A., Guy M., Edwards S., Tymrakiewitcz M., O’brien L., Hall A., Wilkinson R., et al. A recurrent truncating germline mutation in the BRIP1/FANCJ gene and susceptibility to prostate cancer. Br. J. Cancer. 2009;100:426–430. doi: 10.1038/sj.bjc.6604847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rupnik A., Grenon M., Lowndes N. The MRN complex. Curr. Biol. 2008;18:R455–R457. doi: 10.1016/j.cub.2008.03.040. [DOI] [PubMed] [Google Scholar]
- 45.Cybulski C., Górski B., Debniak T., Gliniewicz B., Mierzejewski M., Masojć B., Jakubowska A., Matyjasik J., Złowocka E., Sikorski A., et al. NBS1 is a prostate cancer susceptibility gene. Cancer Res. 2004;64:1215–1219. doi: 10.1158/0008-5472.CAN-03-2502. [DOI] [PubMed] [Google Scholar]
- 46.Paulo P., Pinto P., Peixoto A., Santos C., Pinto C., Rocha P., Veiga I., Soares G., Machado C., Ramos F., et al. Validation of a Next-Generation Sequencing Pipeline for the Molecular Diagnosis of Multiple Inherited Cancer Predisposing Syndromes. J. Mol. Diagn. 2017;19:502–513. doi: 10.1016/j.jmoldx.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 47.Kornberg Z., Chou J., Feng F.Y., Ryan C.J. Prostate cancer in the era of “Omic” medicine: Recognizing the importance of DNA damage repair pathways. Ann. Transl. Med. 2018;6:161. doi: 10.21037/atm.2018.05.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jackson S.P., Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461:1071–1078. doi: 10.1038/nature08467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ciccia A., Elledge S.J. The DNA damage response: Making it safe to play with knives. Mol. Cell. 2010;40:179–204. doi: 10.1016/j.molcel.2010.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haince J.F., McDonald D., Rodrigue A., Dery U., Masson J.Y., Hendzel M.J., Poirier G.G. PARP1- dependent kinetics of recruitment of MRE11 and NBS1 proteins to multiple DNA damage sites. J. Biol. Chem. 2008;283:1197–1208. doi: 10.1074/jbc.M706734200. [DOI] [PubMed] [Google Scholar]
- 51.Dodson G.E., Limbo O., Nieto D., Russell P. Phosphorylation-regulated binding of Ctp1 to Nbs1 is critical for repair of DNA double-strand breaks. Cell Cycle. 2010;9:1516–1522. doi: 10.4161/cc.9.8.11260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huen M.S., Sy S.M., Chen J. BRCA1 and its toolbox for the maintenance of genome integrity. Nat. Rev. Mol. Cell Biol. 2010;11:138–148. doi: 10.1038/nrm2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.You Z., Bailis J.M. DNA damage and decisions: CtIP coordinates DNA repair and cell cycle checkpoints. Trends Cell Biol. 2010;20:402–409. doi: 10.1016/j.tcb.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sy S.M., Huen M.S., Zhu Y., Chen J. PALB2 regulates recombinational repair through chromatin association and oligomerization. J. Biol. Chem. 2009;284:18302–18310. doi: 10.1074/jbc.M109.016717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Modrich P. Mechanisms in eukaryotic mismatch repair. J. Biol. Chem. 2006;281:30305–30309. doi: 10.1074/jbc.R600022200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reilly N.M., Novara L., Di Nicolantonio F., Bardelli A. Exploiting DNA repair defects in colorectal cancer. Mol. Oncol. 2019;13:681–700. doi: 10.1002/1878-0261.12467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sundararajan S., Ahmed A., Goodman O.B., Jr. The relevance of BRCA genetics to prostate cancer pathogenesis and treatment. Clin. Adv. Hematol. Oncol. 2011;9:748–755. [PubMed] [Google Scholar]
- 58.Rubin M.A., Demichelis F. The Genomics of Prostate Cancer: A Historic Perspective. Cold Spring Harb. Perspect Med. 2019;9:a034942. doi: 10.1101/cshperspect.a034942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Castro E., Jugurnauth-Little S., Karlsson Q., Al-Shahrour F., Piñeiro-Yañez E., Van de Poll F., Leongamornlert D., Dadaev T., Govindasami K., Guy M., et al. UKGPCS, EMBRACE and IMPACT studies. High burden of copy number alterations and c-MYC amplification in prostate cancer from BRCA2 germline mutation carriers. Ann. Oncol. 2015;26:2293–2300. doi: 10.1093/annonc/mdv356. [DOI] [PubMed] [Google Scholar]
- 60.Quigley D.A., Dang H.X., Zhao S.G., Lloyd P., Aggarwal R., Alumkal J.J., Foye A., Kothari V., Perry M.D., Bailey A.M., et al. Genomic Hallmarks and Structural Variation in Metastatic Prostate Cancer. Cell. 2018;175:889. doi: 10.1016/j.cell.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 61.Chen Z., Greenwood C., Isaacs W.B., Foulkes W.D., Sun J., Zheng S.L., Condreay L.D., Xu J. The G84E mutation of HOXB13 is associated with increased risk for prostate cancer: Results from the REDUCE trial. Carcinogenesis. 2013;34:1260–1264. doi: 10.1093/carcin/bgt055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mitra A., Fisher C., Foster C.S., Jameson C., Barbachanno Y., Bartlett J., Bancroft E., Doherty R., Kote-Jarai Z., Peock S., et al. Prostate cancer in male BRCA1 and BRCA2 mutation carriers has a more aggressive phenotype. J. Cancer. 2008;98:502–507. doi: 10.1038/sj.bjc.6604132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hatano Y., Tamada M., Matsuo M., Hara A. Molecular Trajectory of BRCA1 and BRCA2 Mutations. Front Oncol. 2020 doi: 10.3389/fonc.2020.00361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gallagher D.J., Gaudet M.M., Pal P., Kirchhoff T., Balistreri L., Vora K., Bhatia J., Stadler Z., Fine S.W., Reuter V., et al. Germline BRCA mutations denote a clinicopathologic subset of prostate cancer. Clin. Cancer Res. 2010;16:2115–2121. doi: 10.1158/1078-0432.CCR-09-2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Agalliu I., Gern R., Leanza S., Burk R.D. Associations of High-Grade Prostate Cancer with Brca1 and Brca2 Founder Mutations. Clin. Cancer Res. 2009;15:1112–1120. doi: 10.1158/1078-0432.CCR-08-1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Na R., Zheng S.L., Han M., Yu H., Jiang D., Shah S., Ewing C.M., Zhang L., Novakovic K., Petkewicz J., et al. Germline Mutations in ATM and BRCA1/2 Distinguish Risk for Lethal and Indolent Prostate Cancer and are Associated with Early Age at Death. Eur. Urol. 2017;71:740–747. doi: 10.1016/j.eururo.2016.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Antonarakis E.S., Lu C., Luber B., Liang C., Wang H., Chen Y., Silberstein J.L., Piana D., Lai Z., Chen Y., et al. Germline DNA-repair Gene Mutations and Outcomes in Men with Metastatic Castration-resistant Prostate Cancer Receiving First-line Abiraterone and Enzalutamide. Eur. Urol. 2018;74:218–225. doi: 10.1016/j.eururo.2018.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Horak P., Weischenfeldt J., Von Amsberg G., Beyer B., Schutte A., Uhrig S., Gieldon L., Klink B., Feuerbach L., Hübschmann D., et al. Response to olaparib in a PALB2 germline mutated prostate cancer and genetic events associated with resistance. Cold Spring Harb Mol. Case Stud. 2019;5:a003657. doi: 10.1101/mcs.a003657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lonergan P.E., Tindall D.J. Androgen receptor signaling in prostate cancer development and progression. J. Carcinog. 2011;10:20. doi: 10.4103/1477-3163.83937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ku S.Y., Gleave M.E., Beltran H. Towards precision oncology in advanced prostate cancer. Nat. Rev. Urol. 2019;16:645–654. doi: 10.1038/s41585-019-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Teo M.Y., Rathkopf D.E., Kantoff P. Treatment of Advanced Prostate Cancer. Annu. Rev. Med. 2019;70:479–499. doi: 10.1146/annurev-med-051517-011947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dias A., Kote-Jarai Z., Mikropoulos C., Eeles R. Prostate Cancer Germline Variations and Implications for Screening and Treatment. Cold Spring Harb Perspect Med. 2018;8:a030379. doi: 10.1101/cshperspect.a030379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mateo J., Carreira S., Sandhu S.K., Miranda S., Mossop H., Perez-Lopez R., Rodrigues D.N., Robinson D., Omlin A., Tunariu N., et al. DNA-Repair Defects and Olaparib in Metastatic Prostate Cancer. N. Engl. J. Med. 2015;373:1697–1708. doi: 10.1056/NEJMoa1506859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Abida W., Cyrta J., Heller G., Prandi D., Armenia J., Coleman I., Cieslik M., Benelli M., Robinson D., Van Allen E.M., et al. Genomic correlates of clinical outcome in advanced prostate cancer. Proc. Natl. Acad. Sci. USA. 2019;116:11428–11436. doi: 10.1073/pnas.1902651116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zafeiriou Z., Bianchini D., Chandler R., Rescigno P., Yuan W., Carreira S., Barrero M., Petremolo A., Miranda S., Riisnaes R., et al. Genomic Analysis of Three Metastatic Prostate Cancer Patients with Exceptional Responses to Carboplatin Indicating Di_erent Types of DNA Repair Deficiency. Eur. Urol. 2018;75:184–192. doi: 10.1016/j.eururo.2018.09.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Antonarakis E.S., Shaukat F., Isaacsson Velho P., Kaur H., Shenderov E., Pardoll D.M., Lotan T.L. Clinical Features and Therapeutic Outcomes in Men with Advanced Prostate Cancer and DNA Mismatch Repair Gene Mutations. Eur. Urol. 2019;75:378–382. doi: 10.1016/j.eururo.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Le D.T., Durham J.N., Smith K.N., Wang H., Bartlett B.R., Aulakh L.K., Lu S., Kemberling H., Wilt C., Luber B.S., et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357:409–413. doi: 10.1126/science.aan6733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Velho P.I., Antonarakis e.S. PD-1/PD-L1 pathway inhibitors in advanced prostate cancer. Expert Rev. Clin. Pharmacol. 2018;11:475–486. doi: 10.1080/17512433.2018.1464388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Network NCC Prostate Cancer (Version 2.2018) 2018. [(accessed on 27 January 2021)]; Available online: https://www.nccn.org/professionals/physician_gls/default.aspx.
- 80.U.S. Food and Drug Administration, FoundationOne® Liquid CDx 2020. [(accessed on 27 January 2021)]; Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf19/P190032C.pdf.
- 81.Telang J.M., Lane B.R., Cher M.L., Miller D.C., Dupree J.M. Prostate cancer family history and eligibility for active surveillance: A systematic review of the literature. BJU Int. 2017;120:464–467. doi: 10.1111/bju.13862. [DOI] [PubMed] [Google Scholar]
- 82.Akizhanova M., Iskakova E.E., Kim V., Wang X., Kogay R., Turebayeva A., Sun Q., Zheng T., Wu S., Miao L., et al. PSA and Prostate Health Index based prostate cancer screening in a hereditary migration complicated population: Implications in precision diagnosis. J. Cancer. 2017;8:1223–1228. doi: 10.7150/jca.18012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bova G.S., Partin A.W., Isaacs S.D., Carter B.S., Beaty T.L., Isaacs W.B. and Walsh, P.C. Biological aggressiveness of hereditary prostate cancer: Long-term evaluation following radical prostatectomy. J. Urol. 1998;160:660–663. doi: 10.1016/S0022-5347(01)62748-4. [DOI] [PubMed] [Google Scholar]
- 84.Hampel H., Bennett R.L., Buchanan A., Pearlman R., Wiesner G.L. A practice guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: Referral indications for cancer predisposition assessment. Genet. Med. 2015;17:70–87. doi: 10.1038/gim.2014.147. [DOI] [PubMed] [Google Scholar]
- 85.US Preventive Services Task Force. Grossman D.C., Curry S.J., Owens D.K., Bibbins-Domingo K., Caughey A.B., Davidson K.W., Doubeni C.A., Ebell M., Epling J.W., Jr., et al. Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;319:1901–1913. doi: 10.1001/jama.2018.3710. [DOI] [PubMed] [Google Scholar]
- 86.Brunese L., Mercaldo F., Reginelli A., Santone A. Formal methods for prostate cancer Gleason score and treatment prediction using radiomic biomarkers. Magn. Reason. Imaging. 2020;66:165–175. doi: 10.1016/j.mri.2019.08.030. [DOI] [PubMed] [Google Scholar]
- 87.Page E.C., Bancroft E.K., Brook M.N., Assel M., Al Battat M.H., Thomas S., Taylor N., Chamberlain A., Pope J., Ni Raghallaigh H., et al. Interim Results from the IMPACT Study: Evidence for Prostate-specific Antigen Screening in BRCA2 Mutation Carriers. Eur. Urol. 2019;76:831–842. doi: 10.1016/j.eururo.2019.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mikropoulos C., Selkirk C.G.H., Saya S., Bancroft E., Vertosick E., Dadaev T., Brendler C., Page E., Dias A., Evans D.G., et al. IMPACT study collaborators. Prostate-specific antigen velocity in a prospective prostate cancer screening study of men with genetic predisposition. Br. J. Cancer. 2018;118:266–276. doi: 10.1038/bjc.2017.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Storebjerg T.M., Hoyer S., Kirkegaard P., Bro F., LuCamp Study Group. Orntoft T.F., Borre M., Sorensen K.D. Prevalence of the HOXB13 G84E mutation in Danish men undergoing radical prostatectomy and its correlations with prostate cancer risk and aggressiveness. BJU Int. 2016;118:646–653. doi: 10.1111/bju.13416. [DOI] [PubMed] [Google Scholar]
- 90.Casanova-Salas I., Athie A., Boutros P.C., Del Re M., Miyamoto D.T., Pienta K.J., Posadas E.M., Sowalsky A.G., Stenzl A., Wyatt A.W., et al. Quantitative and Qualitative Analysis of Blood-based Liquid Biopsies to Inform Clinical Decision-making in Prostate Cancer. Eur. Urol. 2021;7:S0302–S2838. doi: 10.1016/j.eururo.2020.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Campos-Fernández E., Barcelos L.S., de Souza A.G., Goulart L.R., Alonso-Goulart V. Research landscape of liquid biopsies in prostate cancer. Am. J. Cancer Res. 2019;9:1309–1328. [PMC free article] [PubMed] [Google Scholar]
- 92.Hennigan S.T., Trostel S.Y., Terrigino N.T., Voznesensky O.S., Schaefer R.J., Whitlock N.C., Wilkinson S., Carrabba N.V., Atway R., Shema S., et al. Low Abundance of Circulating Tumor DNA in Localized Prostate Cancer. JCO Precis. Oncol. 2019;3 doi: 10.1200/PO.19.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kamps R., Brandão R.D., Bosch B.J., Paulussen A.D., Xanthoulea S., Blok M.J., Romano A. Next-Generation Sequencing in Oncology: Genetic Diagnosis, Risk Prediction and Cancer Classification. Int. J. Mol. Sci. 2017;18:308. doi: 10.3390/ijms18020308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Paulo P., Maia S., Pinto C., Pinto P., Monteiro A., Peixoto A., Teixeira M.R. Targeted next generation sequencing identifies functionally deleterious germline mutations in novel genes in early-onset/familial prostate cancer. PLoS Genet. 2018;14:e1007355. doi: 10.1371/journal.pgen.1007355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Susswein L.R., Marshall M.L., Vogel Nusbaum R., Postula K.J., Weissman S.M., Yackowski L., Vaccari E.M., Bissonnette J., Booker J.K., Cremona M.L., et al. Pathogenic and likely pathogenic variant prevalence among the first 10,000 patients referred for next-generation cancer panel testing. Genet. Med. 2016;18:823–832. doi: 10.1038/gim.2015.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ni Raghallaigh H., Eeles R. Genetic predisposition to prostate cancer: An update. Fam. Cancer. 2021:24. doi: 10.1007/s10689-021-00227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.