Abstract
Simple Summary
Hepatocellular carcinoma (HCC) recurrence is the major obstacle concerning patients’ survival. Tertiary prevention by antiviral therapies could reduce HCC recurrence rate in both chronic hepatitis B virus (HBV) or hepatitis C virus (HCV) infected patients. In chronic hepatitis B (CHB) patients, nucleos(t)ide analogues (Nuc) provide a more effective HCC tertiary prevention effect than an interferon (IFN)-based regimen. In chronic hepatitis C (CHC) patients, the tertiary prevention effect by direct acting antiviral agents (DAAs) was reported non-inferior to that by IFN-based therapy. Chronic hepatitis C patients left untreated had the worst survival benefit as well as shorted recurrence-free interval than those treated by either type of antiviral regimen. Although the risk of HCC recurrence could only be decreased but not diminished by antiviral therapies due to host and microenvironmental factors beyond virus infection, antiviral therapy helps to preserve and improve liver function which makes multi-modality anticancer treatment feasible to improve survival.
Abstract
Hepatocellular carcinoma (HCC) ranks as a leading cause of common cancer and cancer-related death. The major etiology of HCC is due to chronic hepatitis virus including HBV and HCV infections. Scheduled HCC surveillance in high risk populations improves the early detection rate and the feasibility of curative treatment. However, high HCC recurrence rate still accounts for the poor prognosis of HCC patients. In this article, we critically review the pathogenesis of viral hepatitis-related hepatocellular carcinoma and the evidence of tertiary prevention efficacy by current available antiviral treatment, and discuss the knowledge gap in viral hepatitis-related HCC tertiary prevention.
Keywords: carcinogenesis, cirrhosis, direct acting antiviral agents, interferon, nucleos(t)ide analogues, sustained virologic response
1. Introduction
Hepatocellular carcinoma (HCC) ranks as the seventh most common tumor and the fourth most common cause of cancer-related death worldwide [1], with the overall 5-year survival rate in the past four decades <20% globally [2]. HCC is not only a major health problem in Asian countries, where it is endemic with chronic hepatitis B virus (HBV) infection, but is also a growing issue in Western countries as a consequence of chronic hepatitis C infections. Secondary liver cirrhosis from chronic inflammation due to virus activity is the major cause of HCC [3].
The propagation of HCC surveillance programs in high risk populations including chronic hepatitis B (CHB)- or chronic hepatitis C (CHC)-infected patients increases the probability of early detection and curative management [4]. In early stage HCC patients, curative treatment including intrahepatic local treatment and surgical resection has increased the survival from 3-year 13–26% in untreated patients to 5-year 37–75% [5,6]. Even so, high HCC recurrence rate and decreased residual liver reserves in cirrhotic livers are factors in the poor survival rate of patients receiving curative HCC treatment [7,8,9,10]. However, these survival data were reported in the era before highly potent nucleos(t)ide analogues (Nuc), including entecavir (ETV) and tenofovir, for HBV viral suppression and direct acting antiviral agents (DAAs) for HCV eradication were available. This review examines the impact of advances in antiviral therapy on HCC tertiary prevention and progress towards the unmet goal of a sustained HCC cure.
1.1. Viral Factors Associated with HCC Recurrence: HBV
Although surgical resection or local ablation therapy provides an acceptable 5- and 10-year survival rate of 60–75% and 35–50% in patients with HBV-related HCC, the high 5-year recurrence rate, 60–80%, leads to dismal long-term outcomes [11,12,13,14,15,16]. Around 70% of recurrence occurs within 2 years of curative treatment, also defined as “early recurrence,” while recurrence after this period is defined as “late recurrence” [17]. Based on comparative genomic hybridization analysis, early recurrence is more likely to have the same clonal origin as the original tumor, indicating that it is a metastatic tumor from the original tumor, while late recurrence shows distinct clonal origins from the original tumor, implying that it might be a de novo second primary tumor [18].
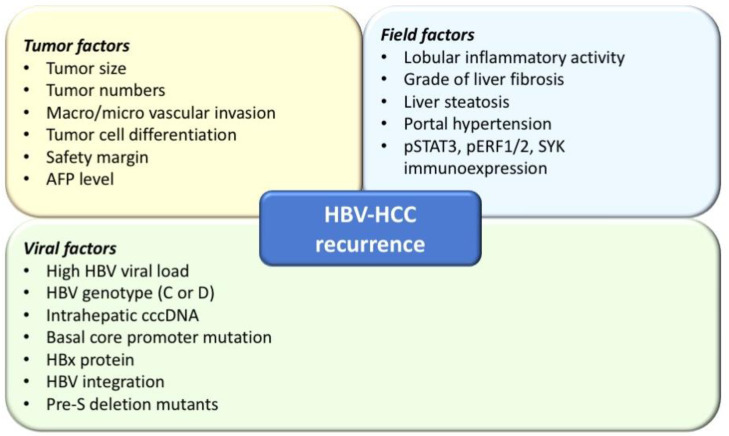
Several factors associated with tumor recurrence have been identified (Figure 1), including tumor factors (tumor numbers, large tumor size, presence of microscopic vascular invasion, poor tumor cell differentiation, non-anatomical resection, narrow cut margin, high serum alpha-fetoprotein levels, etc.), field factors in the non-tumor liver parenchyma (grade of liver fibrosis and steatosis, stage of liver fibrosis, and degree of portal hypertension, as well as liver functional reserve), and HBV viral factors (including active HBV viral replication, genotypes, and mutations) [13,19,20,21,22,23,24,25,26]. Among these factors, tumor factors are associated with early HCC tumor recurrence while intrahepatic environmental factors including high serum HBV DNA levels and higher Ishak inflammation scores are predictive of late recurrence [17]. In a recent study of 645 HCC patients receiving curative surgical resection, cirrhosis, moderate/severe lobular inflammatory activity, and immunoexpression of pSTAT3, pERF1/2, and SYK proteins were predictors for late HCC recurrence [27].
Figure 1.
Risk factors associated with hepatocellular carcinoma (HCC) recurrence in chronic hepatitis B (CHB) patients.
In addition to high HBV viral load, HBV genotypes (C or D), presence of basal core promotor mutations, nuclear expression of HBx protein, HBV integration, and pre-S deletion mutants are associated with increased risk of HCC occurrence and recurrence in CHB patients [28,29,30,31]. HBx is a key regulatory nonstructural protein of the virus, related to host cell cycle regulation, the intersection of HBV infection, and replication and carcinogenesis [32]. The full-length HBx and HBx C-terminal truncation can activate FXR signaling, leading to carcinogenesis [33]. From a histology-based study comparing 328 HBV-associated HCC and 155 matched non-tumor tissue samples, the presence of nuclear HBx-positive HCCs indicated shorter disease free survival (DFS) (35 vs. 126 months) and higher HCC recurrence rate (58.3% vs. 39.2%, p = 0.015) than for those without nuclear HBx protein present [30]. In a recent study of 50 patients with HBV-related HCC (HBV-HCC), HBV integration was identified in 44 HCC tissue samples. Among the 44 patients receiving curative surgery, 10 (23.3%) had detectable plasma virus-host chimera DNA 2 months after surgery and 9 of the 10 patients experienced HCC recurrence within 1 year [31].
The deletion mutations in the pre-S region of HBV correlate with the virus escaping from host immune attack. In one mouse model study, pre-S mutants accumulated in the endoplasmic reticulum (ER), increasing ER stress and promoting hepatocyte proliferation as well as chromosome instability through the upregulation of cyclin A [34,35]. Clinical studies have also demonstrated that the presence of pre-S deletion mutants occurred in 33.8–38.9% in patients with HBV-related HCC [21,36]. Moreover, it has been shown to be an independent risk factor predicting tumor recurrence after curative surgical resection (hazard ratio (HR) 1.564, 95% confidence interval (CI): 1.057–2.314, p = 0.025) [21]. These findings indicate that the adverse effect of pre-S deletion mutants might be based on active HBV viral replication, in turn suggesting oncogenic risk could be reduced by antiviral therapy. In HBV-HCC patients under viral suppression, intrahepatic cccDNA level is an independent factor for intrahepatic and extrahepatic metastasis [37]. Hence, antiviral therapy may reduce but not eliminate the risk of HCC recurrence in HBV-HCC patients since current therapy can hardly deplete intrahepatic cccDNA amount.
1.2. Tertiary Prevention for Patients with HBV-Related HCC Following Curative Therapy: Interferon-Based Therapy
Current available antiviral treatments for chronic hepatitis B infection include interferon (IFN) and Nucs. Through a finite treatment of 48–52 weeks in duration, IFN-based regimens have immunomodulatory, antiviral, and antiproliferative effects. IFN therapy has been proven to reduce liver disease progression, incidence of HCC, and even fibrosis, especially in those with a durable response to therapy [38,39]. In a prospective randomized controlled trial (RCT) of 16 CHB-HCC patients receiving curative tumor ablation treatment, a 24-month IFN-based adjuvant therapy reduced HCC recurrence rate from 100% to 33.3% (p = 0.0384) [40]. However, in a larger retrospective cohort study of 568 CHB-HCC patients receiving curative surgical resection, 101 patients undergoing IFN therapy had a higher 5-year overall survival (OS) rate (69.2% vs.53.2%, p = 0.009) but similar 5-year recurrence-free survival (RFS) rate compared to the 467 patients without antiviral therapy (37.5% vs. 33.5%, p = 0.082) [41]. Moreover, another three RCTs also failed to confirm the tertiary prevention effect of IFN-based therapy in patients with HBV-related HCC who had curative resection surgery [42,43,44]. In a meta-analysis of 531 patients with HBV-HCC, IFN therapy seemed to reduce the risk of recurrence in HBV-related HCC following resection surgery, but the effect was not statistically significant (HR 0.87, 95% CI 0.70–1.09) [45]. In a recent RCT of 477 HBV-HCC patients receiving curative tumor treatment, patients who received co-administration of ETV plus Peg-IFN-α2a for 1 year and a reduction in HBsAg by >1500 IU/mL at week 48 had significantly lower recurrence and mortality rate than those who had additional IFN therapy after 1 year of Nuc treatment, underwent Nuc monotherapy, or were in the non-antiviral treated group [46]. It is still controversial whether IFN-based monotherapy has tertiary prevention effects on patients with HBV-related HCC following curative therapies, and there have not yet been the large-scale prospective randomized control studies needed to prove its efficacy [47].
1.3. Tertiary Prevention for Patients with HBV-Related HCC Following Curative Therapy: Nuc Therapy
Nuc therapy may achieve biochemical remission, ameliorate hepatic necroinflammation, and even regress liver fibrosis through viral suppression in CHB patients [48,49,50]. Based on several retrospective cohorts and studies using health databases, the risk of disease progression and incidence of HCC are both reduced by Nuc therapy, especially in patients with cirrhosis [51,52,53,54,55,56]. The tertiary prevention effect of Nucs in patients with HBV-HCC who receive curative tumor treatment is also demonstrated by RCTs, cohort studies, population-based studies, and meta-analysis [21,55,57,58,59,60,61,62,63,64,65,66] (Table 1). In a RCT of 200 patients with HBV-HCC undergoing surgical resection, those receiving adjuvant adefovir for 5 years had a significantly lower rate of late recurrence than those in the control group (12% vs. 29%, p = 0.002), although rates of early recurrence were comparable [62]. In a meta-analysis of 13 trials with 6350 patients, patients who received adefovir for HCC tertiary prevention showed a significant improvement in both OS (HR 0.56, 95% CI 0.43–0.73, p < 0.0001) and RFS (HR 0.66, 95% CI 0.54–0.80, p < 0.0001) [61]. Since Nucs are more tolerable, have fewer side effects, are applicable in patients with thrombocytopenia (commonly observed in cirrhotic patients), and are more effective for HCC tertiary prevention, applying Nucs as an adjuvant therapy is suggested in patients with HBV-HCC after curative tumor treatment.
Table 1.
Characteristics of large-scale studies reporting hepatitis B virus (HBV)-related HCC recurrence rates after anti-viral therapy.
| Author/Year | Patients No. | HCC Tx | F/U(Median) | HCC Recurrence Rate | HR | Ref. | ||
|---|---|---|---|---|---|---|---|---|
| IFN vs. Control | ||||||||
| IFN | Control | IFN | Control | |||||
| Sun 2006 (RCT) |
118 | 118 | Resection | 36.5 months | Median RFS: 31.2 (95% CI: 14.8–47.7) months |
Median RFS: 17.7 (95% CI: 9.2–26.3) months |
p = 0.1425 | [42] |
| Lo 2007 (RCT) |
40 (35 HBV) |
40 (37 HBV) |
Resection | 5 years | 5-year recurrence: 21/40 (52.5%) |
5-year recurrence: 22/40 (55%) | p = 0.311 | [43] |
| Qu 2010 | 101 | 467 | Resection | 53.3 months | year RFS: 86.1% 5-year RFS: 37.5% |
year RFS: 73.9% 5-year RFS: 33.5% |
0.786 (95% CI: 0.597–1.035), p = 0.086 |
[41] |
| Chen 2012 (RCT) |
133 (106 HBV) |
135 (109 HBV) |
Resection | 63.8 months | year RFS: 71.7% 5-year RFS: 41.7% |
year RFS: 75.1% 5-year RFS: 41.3% |
p = 0.766 | [44] |
| Sun 2014 (meta-analysis) |
264 | 267 | Resection | NR | NR | NR | 0.87 (95% CI: 0.70–1.09), p = 0.23 |
[45] |
| NA vs. Control | ||||||||
| NA | Control | NA | Control | |||||
| Chan 2011 | 42 (38: LAM;4: ETV) |
94 | Resection | NR | year RFS: 66.5% 5-year RFS: 51.4% |
year RFS: 48.9% 5-year RFS: 33.8% |
p = 0.05 | [57] |
| Wu 2012 (PSM) |
518 | 4051 | Resection | NA: 2.18 (IQR 1.21–3.69) years Control: 1.57 (IQR:0.77–3.15) years |
6-year recurrence rate: 45.6% (95%CI: 36.5–54.6%) | 6-year recurrence rate: 54.6% (95% CI: 52.5–56.6%) | 0.66 (95% CI: 0.55–0.81), p < 0.001 |
[58] |
| Ke 2013 (PSM) |
141 (LAM) |
337 | Resection | 24 months | year RFS: 73.1% 5-year RFS: 44.5% |
year RFS: 68.8% 5-year RFS: 43.0% |
p = 0.503 | [59] |
| Yin 2013 (RCT) |
81 (LAM) |
82 | Resection | 39.9 (IQR: 27.3–47.8) months | 2-year RFS: 55.6% 4-year RFS: 37.3% |
2-year RFS: 19.5% 4-year RFS: 12.1% |
p < 0.001 | [60] |
| Su 2013 | 62 | 271 | Resection | 45.9 (IQR: 22.4–78.9) months | year RFS: 90.2% 5-year RFS: 57.5% |
year RFS :63.6% 5-year RFS :34.1% |
2.296 (95%CI:1.451–3.632), p < 0.001 | [21] |
| Sun 2014 (meta-analysis) |
1194 (LAM) |
5052 | Resection; RFA |
NR | NR | NR | 0.66 (95% CI: 0.54–0.80), p < 0.0001 |
[61] |
| Huang 2015 (RCT) |
100 (ADV) |
100 | Resection | 60 (range: 4–70) months | year RFS: 85.0% 5-year RFS: 46.1% |
year RFS: 84.0% 5-year RFS: 27.1% |
0.651 (95% CI: 0.451–0.938), p = 0.021 | [62] |
| Chong 2015 | 254 (ETV: 61.0%; LAM: 30.3%; ADV: 5.5%) |
150 | Resection | 52.4 months | year RFS: 74.8% 5-year RFS: 44.7% |
11-year RFS: 61.1% 5-year RFS: 38.1% |
p = 0.166 | [63] |
| Lee 2016 (PSM) |
133 | 266 | RFA | 0.69 (95% CI: 0.50–0.95), p = 0.02 | 2-year recurrence rate: 41.8% (95%CI: 32.9–50.6%) |
2-year recurrence rate: 54.3% (95%CI: 48.0–60.6%) |
[64] | |
| Wong 2016 | 968 | 1230 | Resection; RFA; TACE; |
2.8 (IQR: 1.4–4.9) years | Incidence of recurrence: 10.7 (95% CI: 9.3–12.2) per 100 person-years |
Incidence of recurrence: 16.6 (95% CI: 15.1–18.2) per 100 person-years |
0.63 (95% CI: 0.49–0.80), p < 0.001 | [55] |
| Chen 2017 (meta-analysis) |
2546 | 6463 | Resection | NR | NR | NR | 0.68 (95% CI: 0.51–0.67, p< 0.001) |
[65] |
| NA vs. NA | ||||||||
| NA | NA | NA | NA | |||||
| Cho 2018 (IPDW) |
High-potency NA: 256 |
Low-potency NA: 90 |
Resection; RFA |
53.6 months | High-potency NA Median RFS: 88.2 (IQR: 27.0–103.6) months |
Low-potency NA Median RFS: 25.1 (IQR: 9.7–61.5) months |
0.470 (95% CI: 0.338–0.652), p < 0.001 |
[67] |
| Choi 2020 (PSM) |
ETV: 567 | TDF: 567 | Resection | ETV: 4.4 years TDF: 2.6 years |
ETV 3-year RFS: 64.1% |
TDF 3-year RFS: 73.2% |
0.82 (95% CI: 0.68–0.98), p = 0.03 |
[68] |
Abbreviations: F/U: follow-up duration; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HR, hazard ratio; IFN, interferon; RCT, randomized control trial; RFS, recurrence-free survival; CI, confidence interval; NR, not reported; LAM, lamivudine; PSM, propensity score matching; IQR, interquartile range; Ref: reference; RFA, radiofrequency ablation; ADV, adefovir; ETV, entecavir; TACE, transarterial chemoembolization; IPDW, inverse probability-of-treatment weighting; TDF: tenofovir disoproxil fumarate.
Further, highly potent Nucs, including ETV, tenofovir disoproxil fumarate (TDF), and tenofovir alafenamide (TAF), are suitable candidates for first line regimen as they decrease the possibility of drug resistance [69]. In a study of 90 patients treated with low-potency Nucs (lamivudine, telbivudine, clevudine, or adefovir) and 256 patients receiving ETV or TDF as tertiary prevention after HCC curative treatment (radiofrequency ablation (RFA) and surgery), RFS was higher in patients using ETV or TDF than those treated with low-potency Nuc treatments (88.2 months vs. 25.1 months, p < 0.001) [67]. The emergence of YMDD mutation or suboptimal viral suppression during Nuc therapy was associated with increased HCC risks and shorter overall survival [67,70,71]. This suggests that highly potent Nucs give improved tertiary prevention in patients with HBV-related HCC after curative treatments.
In a Korean study of 1134 HBV-HCC patients treated with ETV or TDF after curative therapy, patients treated with TDF had a better OS and RFS than those using ETV after a propensity score matching analysis of host, viral, and tumor factors [68]. Moreover, the adjuvant TDF group had a significantly lower HCC recurrence rate for both early and late recurrence than the ETV group (early: HR 0.79, 95% CI 0.64–0.97, p = 0.03; late: HR 0.68, 95% CI 0.47–0.97, p = 0.03). However, the median follow-up duration was significantly shorter in the TDF arm than in the ETV arm (2.6 vs. 4.4 years), insufficient to compare the 5-year recurrence rate, meaning that conclusions should be drawn cautiously [72].
1.4. Carcinogenesis in Chronic Hepatitis C Patients
Chronic hepatitis C (CHC) infection is one of the leading risk factors for HCC, especially in Western countries, with an annual HCC risk of 2–8% in patients with cirrhosis [73,74]. Under one forecasting model, 14.4% of all HCV-infected patients are predicted to develop HCC [75]. The multi-step process of HCV-induced hepatocarcinogenesis consists of a combination of pathway alterations caused by viral factors and/or the effect of immune mediators. HCV core protein increases the levels of reactive oxygen species (ROS), leading to hepatocyte damage at both the genetic and metabolic level, eventually causing cell death. The HCV-altered environment leads to chromosomal instability and irreversible genetic changes [76,77]. HCV protein NS5A is associated with the epithelial mesenchymal transition (EMT) pathway, which promotes fibrogenesis, tumor development, and metastases [78]. In addition, somatic mutations in the telomerase reverse transcriptase (TERT) promoter that enhance TERT expression were shown to be among the earliest and most prevalent neoplastic event in HCV-related HCC (HCV-HCC) [79]. These changes promote hepatocyte neoplastic transformation and the malignant clones progression.
1.5. The Alteration of Host Immune System by Antiviral Therapy Differs between IFN and DAA Treatment in CHC-HCC Patients
Before DAAs were available, interferon (IFN)-α plus ribavirin was the mainstay treatment regimen for chronic hepatitis C [80]. The combination of pegylated IFN with ribavirin for 48 weeks leads to a sustained virological response (SVR) rate as high as 70%, better than IFN monotherapy [81,82]. IFN-α exerts potent antiviral activity via stimulation of IFN-stimulated genes (ISGs) and its downstream signaling pathway [83]. IFN-α can also suppress hepatocellular carcinogenesis by anti-proliferative activity including down-regulation of the Wnt pathway and extracellular signal-regulated kinase (ERK) 1/2 activation. It also causes a host immune modulation effect, anti-telomerase activity, and anti-angiogenesis activity, all of which contribute to HCC reduction [84,85,86,87,88,89].
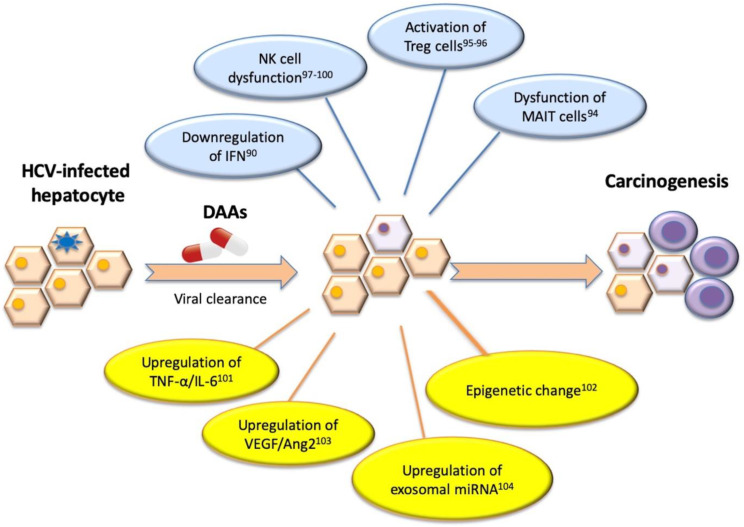
In contrast, DAAs target HCV replication instead of acting on host immunomodulation. DAAs lack the IFN activation or antiproliferative effect on tumor regulation of angiogenesis, suggesting the growth of malignant cells may be tolerated [90]. The pathogenesis involved in HCC recurrence includes: 1. immune cell dysfunction; 2. change in immune cytokine network; 3. activation of angiogenesis [91]. The dysfunction of mucosal associated invariant T (MAIT) and natural killer (NK) cells, sustained immune suppression by regulatory T cells (Treg) as well as myeloid-derived suppressor cells (MDSCs), changes in the immune cytokine network (TNF-α, IL-6, IL-10, or transforming growth factor (TGF-beta)), increased expression of inhibitory molecules (programmed cell death protein 1(PD-1), cytotoxic T-Lymphocyte antigen 4 (CTLA-4)), and the activation of angiogenesis may inhibit tumor cytolysis and lead to the re-emergence of HCC during or after DAA treatment (Figure 2) [92,93,94,95,96,97,98,99,100,101]. Epigenetic changes such as H3K27ac modifications, exosomal miRNA expression of miR-211-3p, 6826-3p, 1236-3p, and 4448, and the increase of vascular endothelial growth factor (VEGF) and angiopoietin-2 levels after DAA treatment have also been reported to increase HCC recurrence risk [102,103,104].
Figure 2.
Molecular mechanism associated with HCC recurrence in chronic hepatitis C patients achieved sustained virologic response after DAA treatment. Different pathogenetic hypotheses have been postulated to investigate the development of HCC mainly based on some possible potential mechanisms including immune cell dysfunction, change in immune cytokine network, activation of angiogenesis, and epigenetic change after DAA therapy. Abbreviations: Ang2, angiopoietin-2; DAA, direct acting antiviral agents; IFN, interferon; MAIT, mucosal associated invariant T; miRNA, microRNA; NK, nature killer; TNF, tumor necrosis factor; Treg, regulatory T cell; VEGF, vascular endothelial growth factor.
1.6. The Tertiary Prevention for Patients with HCV-Related HCC Following Curative Therapy: Interferon-Based Therapy
Pegylated IFN may halt and reverse liver fibrosis after successful HCV eradication besides host immune modulation. In a large pooled study of 3010 IFN-treated CHC patients, necroinflammation improved in 39–73% of cases, while fibrosis regressed in 49% of 153 patients with baseline cirrhosis [105]. Several small-scale RCT studies and a national health insurance database study suggest the tertiary prevention effect of IFN in HCC patients receiving not only curative [106,107] but also palliative treatment [108]. In a prospective multi-center study of 105 CHC-HCC patients treated with PegIFN/RBV, patients who achieved SVR had lower HCC recurrence rate than those without (16/56 vs. 27/49, p < 0.01). The HCC recurrence rate was even higher in those non-SVR patients with high MHC class I polypeptide-related chain A (MICA) level >100 pg/mL [109]. In a systemic review of 13 RCTs involving 1344 patients with HCV-HCC after curative therapy, IFN reduced both early and late recurrence by 5 year follow-up (RR and P value for 1-, 2-, 3-, 4- and 5-year recurrence rate: 0.84, 0.76, 0.82, 0.79, and 0.83, respectively, all p < 0.01) [110]. In another meta-analysis, it was shown that SVR achieved by Peg-IFN/RBV was associated with improved overall survival and recurrence free survival in patients with HCV who have undergone resection or locoregional therapy for HCC as well as associated with a significant absolute risk reduction of recurrence (32%; 95% CI 22–42%) [111]. The tertiary prevention effect from IFN was more frequently reported as reducing late recurrence rather than early recurrence [112,113,114], and this effect was mainly attributed to patients achieving SVR [115,116].
1.7. The Tertiary Prevention Efficacy for Patients with HCV-Related HCC Following Curative Therapy: DAA
DAAs target various points of the HCV replication cycle, binding directly to components of the replicase complex or initiating RNA chain termination, and result in > 95% SVR in CHC patients regardless of HCV genotype, cirrhosis, or prior interferon treatment failure history within 8–24 weeks of treatment [117]. The high SVR rate and rapid elimination of chronic inflammation by DAA treatment together reduce portal hypertension, improve liver dysfunction, and regress fibrosis [118,119,120], leading to an expectation of a drastic decline in HCC recurrence. However, several studies with single-arm DAA-treated HCV-HCC patients found an increased HCC recurrence rate after antiviral treatment [121,122,123,124,125,126,127] while conflicting results have been reported in other studies, including single-arm [128,129,130] studies and studies comparing DAA treated patients to untreated [131,132,133,134,135,136,137,138,139,140] or IFN-treated groups [116,136,141,142,143,144,145]. The single-arm and comparison studies are summarized in Table 2 and the comparison studies are discussed in more detail below.
Table 2.
Characteristics of studies reporting HCC recurrence rates after anti-viral therapy in chronic hepatitis C patients.
| Author/Year | Patients No. | HCC Tx | Start of F/U, Median F/U | HCC Recurrence Rate | HR | Ref. | |||
|---|---|---|---|---|---|---|---|---|---|
| DAA Alone | |||||||||
| Reig 2016 | 58 | Resection RFA TACE |
HCV Tx, 3.5 months | 27.6% | - | [121] | |||
| Conti 2016 | 59 | Resection RFA TACE |
HCV Tx, 5.5 months | 28.8% | - | [122] | |||
| Cabibbo 2017 | 143 | Resection RFA TACE |
HCV Tx, 8.7 months | 1 year: 26.6% | - | [124] | |||
| Bielen 2017 | 41 | Resection RFA TACE |
HCV Tx, 6 months | 0.5 year: 14.6% | - | [128] | |||
| Ogawa 2018 | 152 | Resection RFA TACE RT |
HCV Tx, 17 months | 1 year: Non-cirrhosis: 6.5% Cirrhosis: 23.1% |
- | [125] | |||
| Calleja 2017 | 70 | NR | HCV Tx, 12 months | 1 year: 30.0% | - | [126] | |||
| Cheung 2016 | 29 | NR | HCV Tx, 15 months | 0.5 year:6.9% | - | [129] | |||
| Yoshimasu 2019 | 23 | NR | HCV Tx, 21 months | 1 year: 13% | - | [130] | |||
| Nakano 2019 | 459 | Resection RFA |
HCV Tx, 29.4 months | 1 year: 27.1% | - | [127] | |||
| DAA vs. Untreated | |||||||||
| DAA | Untreated | DAA | Untreated | ||||||
| ANRS 2016 (CO22 HEPATHER) |
189 | 78 | NR | HCV Tx DAA: 20 months Untreated: 26 months |
0.73 vs. 0.66/100 person-months (aHR: 1.04, 95% CI: 0.53–2.07) |
0.88 | [131] | ||
| ANRS 2016 (CO12 CirVir) |
13 | 66 | Resection RFA |
HCV Tx, 21.3 months | 1.11 vs. 1.73/100 person-months (aHR: 0.40, 95% CI: 0.05–3.03) |
0.75 | [131] | ||
| Kassas 2017 (IPTW) |
53 | 63 | Resection RFA |
HCC Tx, DAA: 16 months Untreated: 23 months |
37.7% | 25.4% | <0.01 | [146] | |
| Virlogeux 2017 | 23 | 45 | Resection RFA TACE |
HCC Tx, DAA: 17 months Untreated: 10 months |
1.7 vs. 4.2/100 person-months (aHR: 0.24, 95% CI: 0.10–0.55) |
0.01 | [133] | ||
| Ikeda 2017 (PSM) |
89 | 89 | Resection RFA TACE |
HCV Tx, 20.7 months | 2 years: 21.8% | 2 years: 46.5% | <0.01 | [135] | |
| Huang 2018 (IPTW) |
62 | 87 | Resection RFA TACE |
HCC Tx DAA: 31 months Untreated: 22 months |
1 year: 47.0% | 1 year: 49.8% | 0.93 | [138] | |
| Singal 2019 (PSM) |
304 | 489 | Resection RFA TACE TARE/RT |
HCC Tx, 10.4 months | aHR: 0.91, 95%CI: 0.69–1.19 | >0.05 | [139] | ||
| Cabibbo 2019 (PSM) |
102 | 102 | Resection RFA |
HCV Tx, DAA: 21 months Untreated: 18 months |
1 year: 15% 2 years: 27% |
1 year: 20% 2 years: 40% |
0.15 | [140] | |
| IFN vs. DAA | |||||||||
| IFN | DAA | IFN | DAA | ||||||
| Waziry 2017 (meta-analysis) |
1485 | 867 | NR | HCC Tx, IFN: 60 months DAA: 15.6 months |
9.2 vs. 12.2/100 person-years (RR 0.62; 95%CI 0.11–3.45) |
0.56 | [147] | ||
| Petta 2017 | 57 | 58 | Resection RFA |
HCC Tx, IFN: 34 months DAA: 18 months |
2 years:15.2% | 2 years: 26.3% | 0.49 | [116] | |
| Nagata 2017* (PSM) |
22 | 22 | Resection RFA |
HCC Tx, IFN: 74 months DAA: 27 months |
5 years: 54.2% | 5 years: 45.1% | 0.54 | [143] | |
| Mashiba 2018* (PSM) |
56 | 56 | NR | HCV Tx, IFN: 25.5 months DAA: 7.7 months |
NR | NR | 0.21 | [145] | |
| Kinoshita 2018* (PSM) |
61 | 61 | RFA | HCV Tx, IFN: 86.4 months DAA: 21.6 months |
2 years: 61% | 2 years: 60% | 0.43 | [142] | |
| Nagaoki 2018 (PSM) |
32 | 32 | Resection RFA RT |
HCC Tx, IFN: 63.6 months DAA: 33.6 months |
1 year: 0% 3 years: 34% |
1 year: 5% 3 years: 26% |
0.36 | [144] | |
| Teng 2019 (PSM) |
50 | 50 | Resection RFA TACE |
HCV Tx, IFN: 74.4 months DAA: 30.0 months |
1 year: 22% 2 years: 48% |
1 year: 48% 2 years: 58% |
0.04 | [148] | |
IFN-based therapy included PegIFN, RBV and simeprevir (SMV) or telaprevir (TVR). Abbreviations: DAA, direct acting antiviral agents; HCC, F/U: follow-up duration; hepatocellular carcinoma; IFN, interferon; IPTW, inverse probability of treatment weighting; LT, liver transplantation; NR, not reported; PSM, propensity score matching; Ref: reference; RFA, radiofrequency ablation; RT, radiation therapy; TACE, transarterial chemoembolization.
1.8. DAA Versus Untreated
In the prospective multi-center ANRS study, no increased HCC recurrence risk was observed in DAA treated patients when compared to untreated HCV-HCC patients [131]. In both the ANRS CO22 (HEPATHER) cohort and ANRS CO12 (CirVir) cohort, the recurrence rate was comparable between DAA-treated and untreated patients (p = 0.88 for overall and p = 0.75 for cirrhotic patients) [131]. However, an Egyptian prospective study reported a 4-fold increase in the HCC recurrence rate in DAA treated patients over untreated patients by 16 month follow-up [146]. In contrast to this, in a French study of 68 HCV-HCC patients who were all cirrhotic and receiving curative HCC treatment, the HCC recurrence rate was significantly lower among patients treated with DAAs compared with untreated patients (1.7/100 vs. 4.2/100 person-months, p = 0.01) [133]. In another study of 178 patients receiving DAAs after curative HCC treatment, the 2-year recurrence rate was lower in DAA treated patients than in untreated patients after adjusting host and tumor factors (2-year recurrence rate: 21.8% vs. 46.5%, Log-rank p < 0.01) [135]. In a recent large multicenter retrospective cohort comparing the recurrence rate between 304 patients receiving adjuvant DAA therapy and 489 patients untreated after curative HCC treatment, patients in the DAA-treated arm had an HCC recurrence rate comparable to untreated patients (HR 0.90, 95% CI 0.70–1.16) over a median follow-up duration of 10.4 months, after adjustment for study site, age, sex, Child–Pugh score, AFP level, tumor burden, and HCC treatment modality [139]. This finding has been validated by another prospective study of 163 CHC-HCC BCLC stage O/A patients with cirrhosis (HR 0.70, 95% CI: 0.44–1.13, p = 0.15), which applied propensity-score-matching for adjustment of the difference between DAA-treated and untreated arms including host factors, liver function, and cancer-related characteristics [140]. In addition to showing no increase in early recurrence of HCC, DAA treatment improved liver reserve and reduced mortality from hepatic decompensation, typically one of the major causes of death for CHC-HCC patients, in these patients [149].
1.9. DAA Versus IFN-Based Therapy
The argument that DAA is inferior to IFN treatment in tertiary prevention arises from two small studies composed of 58 and 59 CHC-HCC patients, both reporting “unexpected high” HCC recurrence rates of 27.6–28.8% within 6 months after DAA treatment with >17% of these recurrences showing more aggressive, multifocal, and infiltrative patterns [121,122]. However, these results are not significantly higher than rates reported in cirrhotic patients treated with adjuvant DAA (23.1%) [125] and in those undergoing adjuvant peg-IFN plus RBV treatment (22.2%) [150]. In a study of 443 CHC-HCC BCLC stage 0/A patients, the 2- and 5-year recurrence rate was much lower in patients receiving adjuvant IFN-based or DAA treatment (IFN vs. DAA, 2-, 5-year: 15.2% and 41.1% vs. 26.3% and 39.1%, p = 0.49) than in those untreated (2-, 5-year: 40.6% and 64.5%) and the recurrence was even lower in those achieving SVR regardless of antiviral regimen [116]. Similarly, several Japanese studies found no difference in recurrence pattern between IFN and DAA groups after adjustments were made for different characteristics and possible confounders [142,143,144,145]. The discrepant reports of DAA tertiary prevention effect for CHC-HCC patients may result from the differing definitions of follow-up timeframe (from HCC curative treatment or from antiviral treatment to HCC recurrence) [116,142,143,144,145].
In a recent study of 301 CHC-HCC patients with curative HCC treatment which adopted the time-varying exposure of different time frames, the incidence rate of HCC recurrence was higher in the DAA arm than in the Peg-IFN/RBV arm during anti-viral therapy (2724.4 vs. 665.8/104 person-years, log-rank p = 0.042) and for a 2-year period after SVR (5259.4 vs. 3277.6/104 person-years, log-rank p = 0.048) [148], suggesting that the tertiary prevention effect of DAA was brief during antiviral therapy and reduced/absent after the end of treatment. In contrast, a meta-analysis of 15 studies and 2352 CHC-HCC patients found that adjuvant DAA therapy was not associated with higher HCC recurrence (RR 0.62; 95% CI 0.11–3.45; p = 0.56) after adjustment for host and tumor factors [147]. In another systemic review and meta-analysis of nine more recent studies with a total of 1157 CHC-HCC patients, all receiving adjuvant DAA, the pooled recurrence rate was 24.4% with >77% HCC recurrence in early stages, no worse than that reported in adjuvant IFN studies and superior to that of untreated patients [136].
1.10. The Optimal Timing of Adjuvant DAA Treatment for Tertiary Prevention of CHC-HCC
A major concern for adjuvant DAA treatment is whether too short an interval (<4 months) between HCC curative treatment and DAA initiation will result in higher early recurrence [121,125]. Deferring adjuvant DAA therapy may allow sufficient time for immune surveillance of microscopic HCC clones as well as for the verification of HCC complete response. The sensitivity of onetime computed tomography (CT) or magnetic resonance imaging (MRI) for small HCC lesions is low, with sensitivities of only 40–50% for subcentimeter lesions and 60–70% for 1- to 2-cm lesions [151]. Given the lack of urgency for HCV therapy after HCC complete response, it therefore appears prudent to wait at least 4–6 months after HCC complete response to initiate DAA therapy, which would typically allow for 2–3 interim multiphase CT or MRI scans to confirm durable HCC response, as advised by the American Gastroenterological Association (AGA) institute [152]. Furthermore, a decrease in SVR among patients with active HCC and competing risk of HCC-related mortality has been reported in two studies [153,154] and one meta-analysis [102]. These data highlight that, when possible, treating HCV in the absence of HCC is the optimal strategy. However, the optimal period to wait before starting DAA therapy after HCC curative treatment is unknown, and whether a longer interval will increase HCC recurrence risk still awaits clarification.
1.11. The Role of Immune Checkpoint Inhibitors in HBV and HCV-Related HCC Patients
Immunotherapies with immune checkpoint inhibitors (ICIs), such as anti-programmed cell death-1 (PD-1) antibodies (nivolumab and pembrolizumab) [155,156,157] and anti-programmed cell death ligand 1 (PD-L1) antibodies (atezolizumab) [158] have greatly improved the survival of patients with advanced HCC due to chronic HBV or HCV infections. There was no increased incidence of major safety issues such as HBV reactivation during ICIs treatment. In a study of 60 CHB-HCC patients, no patients on antiviral therapy (regardless of HBV viral load at baseline) developed HBV reactivation, and one out of six not receiving Nucs had HBV reactivation [159]. In another large cohort of 397 patients, HBV reactivation only occurred in 2 HBsAg-positive patients (<1%) [160]. HCV reactivation is less studied in HCC patients but appears to be safe in patients with melanoma [161] and non-small cell lung cancer [162].
2. Conclusions and Perspective
As concerning the review papers presented in this review, we should consider some limitations. First, other adjuvant therapies for prevention of HCC recurrence, such as target therapy, immunotherapy, or chemoprevention such as metformin, statin, and so on, have not been discussed here. Second, it is difficult to compensate for the various confounding factors influencing the antiviral therapy tertiary prevention effect, including the heterogeneity in treatments for HCC, the precise definition of response, the use of antivirals, and differing follow-up timeframes.
In conclusion, although antiviral therapies can only reduce, not eliminate, the risk of HCC recurrence in patients who have already presented with intrahepatic oncogenesis, they do reduce the risk of hepatic decompensation, improve liver function, and reverse liver fibrosis in chronic HBV- or HCV-related HCC patients. By preserving or improving liver reserve, multiple and/or more radical HCC treatments may be feasible which can ultimately improve overall survival. Combination with other adjuvant therapies may also help restore host immunity or improve the intrahepatic microenvironment and thus further lower HCC recurrence in comparison to antiviral treatment alone. Further investigation of possible integrated tertiary prevention strategies is required to further reduce the HCC recurrence rate using current adjuvant antiviral therapies.
Abbreviations
| ADV | adefovir |
| AFP | Alpha-fetoprotein |
| BCLC | Barcelona Clinic Liver Cancer classification |
| CHB | chronic hepatitis B |
| CHC | chronic hepatitis C |
| CI | confidence interval |
| CTLA-4 | cytotoxic T-Lymphocyte antigen 4 |
| DAA | direct acting antiviral agents |
| DFS | disease free survival |
| EMT | epithelial mesenchymal transition |
| ER | endoplasmic reticulum |
| ERK | extracellular signal-regulated kinase |
| ETV | entecavir |
| FXR | Farnesoid X receptor |
| HBsAg | hepatitis B surface antigen |
| HBV | hepatitis B virus |
| HBV-HCC | HBV related HCC |
| HCC | hepatocellular carcinoma |
| HCV | hepatitis C virus |
| HCV-HCC | HCV related HCC |
| HR | hazard ratio |
| IFN | interferon |
| LAM | lamivudine |
| MAIT | mucosal associated invariant T |
| NK | natural killer cell |
| Nuc | nucleos(t)ide analogues |
| OS | overall survival |
| PD-1 | programmed cell death protein 1 |
| Peg-IFN | pegylated interferon |
| RCT | randomized control trial |
| RFA | radiofrequency ablation |
| RFS | recurrence-free survival |
| ROS | reactive oxygen species |
| SVR | sustained virologic response |
| TAF | tenofovir alafenamide |
| TDF | tenofovir disoproxil fumarate |
| TERT | telomerase reverse transcriptase |
| TDF-β | transforming growth factor |
| Treg | regulatory T cell. |
Author Contributions
Manuscript drafting: W.T., Y.-C.L., C.-W.S. and W.-J.J.; manuscript revision and supervision: C.-W.S. and W.-J.J. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by grants from the Taipei Veterans General Hospital (Center of Excellence for Cancer Research MOHW110-TDU-B-211-144019), Chang Gung Memorial Hospital (CMRPG3J1342, CMRPG3G1281-2, CMRPG3K0841-2, CMRPG3I0271-2), and National Science Council, Taiwan (NMRPG3H0473).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
There are no potential conflicts of financial and non-financial interests in this study. Chien-Wei Su: Speakers’ bureau: Gilead Sciences, Bristol-Myers Squibb, AbbVie, Bayer, and Roche. Advisory arrangements: Gilead Sciences. Grants: Bristol-Myers Squibb, and Eiger.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO Latest Global Cancer Data: Cancer Burden Rises to 19.1 Million New Cases and 9.6 Million Cancer Deaths in 2018. [(accessed on 12 September 2018)]; Available online: https://www.who.int/cancer/PRGlobocanFinal.pdf.
- 2.Singal A.G., Lok A.S., Feng Z., Kanwal F., Parikh N.D. Conceptual Model for the Hepatocellular Carcinoma Screening Continuum: Current Status and Research Agenda. Clin. Gastroenterol. Hepatol. 2020 doi: 10.1016/j.cgh.2020.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang H.I., Yeh S.H., Chen P.J., Iloeje U.H., Jen C.L., Su J., Wang L.Y., Lu S.N., You S.L., Chen D.S., et al. Associations between hepatitis B virus genotype and mutants and the risk of hepatocellular carcinoma. J. Natl. Cancer Inst. 2008;100:1134–1143. doi: 10.1093/jnci/djn243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deng L.X., Mehta N. Does Hepatocellular Carcinoma Surveillance Increase Survival in At-Risk Populations? Patient Selection, Biomarkers, and Barriers. Dig. Dis. Sci. 2020;65:3456–3462. doi: 10.1007/s10620-020-06550-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Llovet J.M., Bru C., Bruix J. Prognosis of hepatocellular carcinoma: The BCLC staging classification. Semin. Liver Dis. 1999;19:329–338. doi: 10.1055/s-2007-1007122. [DOI] [PubMed] [Google Scholar]
- 6.Predictive factors for long term prognosis after partial hepatectomy for patients with hepatocellular carcinoma in Japan. The Liver Cancer Study Group of Japan. Cancer. 1994;74:2772–2780. doi: 10.1002/1097-0142(19941115)74:10<2772::AID-CNCR2820741006>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 7.Balsells J., Charco R., Lazaro J.L., Murio E., Vargas V., Allende E., Margarit C. Resection of hepatocellular carcinoma in patients with cirrhosis. Br. J. Surg. 1996;83:758–761. doi: 10.1002/bjs.1800830610. [DOI] [PubMed] [Google Scholar]
- 8.Yeh C.N., Chen M.F., Lee W.C., Jeng L.B. Prognostic factors of hepatic resection for hepatocellular carcinoma with cirrhosis: Univariate and multivariate analysis. J. Surg. Oncol. 2002;81:195–202. doi: 10.1002/jso.10178. [DOI] [PubMed] [Google Scholar]
- 9.Forner A., Llovet J.M., Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245–1255. doi: 10.1016/S0140-6736(11)61347-0. [DOI] [PubMed] [Google Scholar]
- 10.Tiong L., Maddern G.J. Systematic review and meta-analysis of survival and disease recurrence after radiofrequency ablation for hepatocellular carcinoma. Br. J. Surg. 2011;98:1210–1224. doi: 10.1002/bjs.7669. [DOI] [PubMed] [Google Scholar]
- 11.Su C.W., Lei H.J., Chau G.Y., Hung H.H., Wu J.C., Hsia C.Y., Lui W.Y., Su Y.H., Wu C.W., Lee S.D. The effect of age on the long-term prognosis of patients with hepatocellular carcinoma after resection surgery: A propensity score matching analysis. Arch. Surg. 2012;147:137–144. doi: 10.1001/archsurg.2011.288. [DOI] [PubMed] [Google Scholar]
- 12.Roayaie S., Jibara G., Tabrizian P., Park J.W., Yang J., Yan L., Schwartz M., Han G., Izzo F., Chen M., et al. The role of hepatic resection in the treatment of hepatocellular cancer. Hepatology. 2015;62:440–451. doi: 10.1002/hep.27745. [DOI] [PubMed] [Google Scholar]
- 13.Chan A.W.H., Zhong J., Berhane S., Toyoda H., Cucchetti A., Shi K., Tada T., Chong C.C.N., Xiang B.-D., Li L.-Q., et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J. Hepatol. 2018;69:1284–1293. doi: 10.1016/j.jhep.2018.08.027. [DOI] [PubMed] [Google Scholar]
- 14.Vibert E., Schwartz M., Olthoff K.M. Advances in resection and transplantation for hepatocellular carcinoma. J. Hepatol. 2020;72:262–276. doi: 10.1016/j.jhep.2019.11.017. [DOI] [PubMed] [Google Scholar]
- 15.Shiina S., Tateishi R., Arano T., Uchino K., Enooku K., Nakagawa H., Asaoka Y., Sato T., Masuzaki R., Kondo Y., et al. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am. J. Gastroenterol. 2012;107:569–577. doi: 10.1038/ajg.2011.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kao W.Y., Su C.W., Chiou Y.Y., Chiu N.C., Liu C.A., Fang K.C., Huo T.I., Huang Y.H., Chang C.C., Hou M.C., et al. Hepatocellular Carcinoma: Nomograms Based on the Albumin-Bilirubin Grade to Assess the Outcomes of Radiofrequency Ablation. Radiology. 2017;285:670–680. doi: 10.1148/radiol.2017162382. [DOI] [PubMed] [Google Scholar]
- 17.Wu J.C., Huang Y.H., Chau G.Y., Su C.W., Lai C.R., Lee P.C., Huo T.I., Sheen I.J., Lee S.D., Lui W.Y. Risk factors for early and late recurrence in hepatitis B-related hepatocellular carcinoma. J. Hepatol. 2009;51:890–897. doi: 10.1016/j.jhep.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 18.Chen Y.J., Yeh S.H., Chen J.T., Wu C.C., Hsu M.T., Tsai S.F., Chen P.J., Lin C.H. Chromosomal changes and clonality relationship between primary and recurrent hepatocellular carcinoma. Gastroenterology. 2000;119:431–440. doi: 10.1053/gast.2000.9373. [DOI] [PubMed] [Google Scholar]
- 19.Hung I.F., Poon R.T., Lai C.L., Fung J., Fan S.T., Yuen M.F. Recurrence of hepatitis B-related hepatocellular carcinoma is associated with high viral load at the time of resection. Am. J. Gastroenterol. 2008;103:1663–1673. doi: 10.1111/j.1572-0241.2008.01872.x. [DOI] [PubMed] [Google Scholar]
- 20.Hamaguchi Y., Kaido T., Okumura S., Kobayashi A., Shirai H., Yao S., Yagi S., Kamo N., Seo S., Taura K., et al. Preoperative Visceral Adiposity and Muscularity Predict Poor Outcomes after Hepatectomy for Hepatocellular Carcinoma. Liver Cancer. 2019;8:92–109. doi: 10.1159/000488779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su C.W., Chiou Y.W., Tsai Y.H., Teng R.D., Chau G.Y., Lei H.J., Hung H.H., Huo T.I., Wu J.C. The Influence of Hepatitis B Viral Load and Pre-S Deletion Mutations on Post-Operative Recurrence of Hepatocellular Carcinoma and the Tertiary Preventive Effects by Anti-Viral Therapy. PLoS ONE. 2013;8:e66457. doi: 10.1371/journal.pone.0066457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Su C.W., Chau G.Y., Hung H.H., Yeh Y.C., Lei H.J., Hsia C.Y., Lai C.R., Lin H.C., Wu J.C. Impact of Steatosis on Prognosis of Patients with Early-Stage Hepatocellular Carcinoma After Hepatic Resection. Ann. Surg. Oncol. 2015;22:2253–2261. doi: 10.1245/s10434-014-4221-5. [DOI] [PubMed] [Google Scholar]
- 23.Marasco G., Colecchia A., Colli A., Ravaioli F., Casazza G., Bacchi Reggiani M.L., Cucchetti A., Cescon M., Festi D. Role of liver and spleen stiffness in predicting the recurrence of hepatocellular carcinoma after resection. J. Hepatol. 2019;70:440–448. doi: 10.1016/j.jhep.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 24.Chang C.Y., Hsieh W.Y., Chau G.Y., Chen P.H., Su C.W., Hou M.C., Lei H.J., Huo T.I., Huang Y.H., Lin H.C., et al. Esophageal varices are not predictive of patient prognosis after surgical resection of hepatocellular carcinoma. Eur. J. Gastroenterol. Hepatol. 2018;30:1368–1377. doi: 10.1097/MEG.0000000000001193. [DOI] [PubMed] [Google Scholar]
- 25.Liu W.R., Tian M.X., Jin L., Yang L.X., Ding Z.B., Shen Y.H., Peng Y.F., Zhou J., Qiu S.J., Dai Z., et al. High levels of hepatitis B surface antigen are associated with poorer survival and early recurrence of hepatocellular carcinoma in patients with low hepatitis B viral loads. Ann. Surg. Oncol. 2015;22:843–850. doi: 10.1245/s10434-014-4043-5. [DOI] [PubMed] [Google Scholar]
- 26.Sohn W., Paik Y.H., Kim J.M., Kwon C.H., Joh J.W., Cho J.Y., Gwak G.Y., Choi M.S., Lee J.H., Koh K.C., et al. HBV DNA and HBsAg levels as risk predictors of early and late recurrence after curative resection of HBV-related hepatocellular carcinoma. Ann. Surg. Oncol. 2014;21:2429–2435. doi: 10.1245/s10434-014-3621-x. [DOI] [PubMed] [Google Scholar]
- 27.Nahm J.H., Lee H.S., Kim H., Yim S.Y., Shin J.H., Yoo J.E., Ahn S.H., Choi J.S., Lee J.S., Park Y.N. Pathologic Predictive Factors for Late Recurrence of Hepatocellular Carcinoma in Chronic Liver Disease. Liver Int. 2021 doi: 10.1111/liv.14835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen C.H., Changchien C.S., Lee C.M., Hung C.H., Hu T.H., Wang J.H., Wang J.C., Lu S.N. Combined mutations in pre-s/surface and core promoter/precore regions of hepatitis B virus increase the risk of hepatocellular carcinoma: A case-control study. J. Infect. Dis. 2008;198:1634–1642. doi: 10.1086/592990. [DOI] [PubMed] [Google Scholar]
- 29.Kao J.H., Liu C.J., Jow G.M., Chen P.J., Chen D.S., Chen B.F. Fine mapping of hepatitis B virus pre-S deletion and its association with hepatocellular carcinoma. Liver Int. 2012;32:1373–1381. doi: 10.1111/j.1478-3231.2012.02826.x. [DOI] [PubMed] [Google Scholar]
- 30.Jin J., Jung H.Y., Lee K.H., Yi N.J., Suh K.S., Jang J.J., Lee K.B. Nuclear Expression of Hepatitis B Virus X Protein Is Associated with Recurrence of Early-Stage Hepatocellular Carcinomas: Role of Viral Protein in Tumor Recurrence. J. Pathol. Transl. Med. 2016;50:181–189. doi: 10.4132/jptm.2016.03.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li C.L., Ho M.C., Lin Y.Y., Tzeng S.T., Chen Y.J., Pai H.Y., Wang Y.C., Chen C.L., Lee Y.H., Chen D.S., et al. Cell-Free Virus-Host Chimera DNA From Hepatitis B Virus Integration Sites as a Circulating Biomarker of Hepatocellular Cancer. Hepatology. 2020 doi: 10.1002/hep.31230. [DOI] [PubMed] [Google Scholar]
- 32.Ng S.A., Lee C. Hepatitis B virus X gene and hepatocarcinogenesis. J. Gastroenterol. 2011;46:974–990. doi: 10.1007/s00535-011-0415-9. [DOI] [PubMed] [Google Scholar]
- 33.Niu Y., Chen L., Wu M., Huang W., Wu X., Huang D., Xie Y., Shi G. Partial abrogation of FXR-KNG1 signaling by carboxyl-terminal truncated HBx-C30 in hepatitis B virus-associated hepatocellular carcinoma. Virus Res. 2021;293:198264. doi: 10.1016/j.virusres.2020.198264. [DOI] [PubMed] [Google Scholar]
- 34.Wang L.H., Huang W., Lai M.D., Su I.J. Aberrant cyclin A expression and centrosome overduplication induced by hepatitis B virus pre-S2 mutants and its implication in hepatocarcinogenesis. Carcinogenesis. 2012;33:466–472. doi: 10.1093/carcin/bgr296. [DOI] [PubMed] [Google Scholar]
- 35.Teng Y.C., Neo J.C., Wu J.C., Chen Y.F., Kao C.H., Tsai T.F. Expression of a hepatitis B virus pre-S2 deletion mutant in the liver results in hepatomegaly and hepatocellular carcinoma in mice. J. Pathol. 2017;241:463–474. doi: 10.1002/path.4850. [DOI] [PubMed] [Google Scholar]
- 36.Yen C.J., Ai Y.L., Tsai H.W., Chan S.H., Yen C.S., Cheng K.H., Lee Y.P., Kao C.W., Wang Y.C., Chen Y.L., et al. Hepatitis B virus surface gene pre-S-2 mutant as a high-risk serum marker for hepatoma recurrence after curative hepatic resection. Hepatology. 2018;68:815–826. doi: 10.1002/hep.29790. [DOI] [PubMed] [Google Scholar]
- 37.Hsu C.W., Chu Y.D., Lai M.W., Lin C.L., Liang K.H., Lin Y.H., Yeh C.T. Hepatitis B Virus Covalently Closed Circular DNA Predicts Postoperative Liver Cancer Metastasis Independent of Virological Suppression. Cancers. 2021;13:538. doi: 10.3390/cancers13030538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Su C.W., Yang Y.Y., Lin H.C. Impact of etiological treatment on prognosis. Hepatol. Int. 2018;12:56–67. doi: 10.1007/s12072-017-9807-0. [DOI] [PubMed] [Google Scholar]
- 39.Marcellin P., Lau G.K., Bonino F., Farci P., Hadziyannis S., Jin R., Lu Z.M., Piratvisuth T., Germanidis G., Yurdaydin C., et al. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N. Engl. J. Med. 2004;351:1206–1217. doi: 10.1056/NEJMoa040431. [DOI] [PubMed] [Google Scholar]
- 40.Lin S.M., Lin C.J., Hsu C.W., Tai D.I., Sheen I.S., Lin D.Y., Liaw Y.F. Prospective randomized controlled study of interferon-alpha in preventing hepatocellular carcinoma recurrence after medical ablation therapy for primary tumors. Cancer. 2004;100:376–382. doi: 10.1002/cncr.20004. [DOI] [PubMed] [Google Scholar]
- 41.Qu L.S., Jin F., Huang X.W., Shen X.Z. Interferon-alpha therapy after curative resection prevents early recurrence and improves survival in patients with hepatitis B virus-related hepatocellular carcinoma. J. Surg. Oncol. 2010;102:796–801. doi: 10.1002/jso.21741. [DOI] [PubMed] [Google Scholar]
- 42.Sun H.C., Tang Z.Y., Wang L., Qin L.X., Ma Z.C., Ye Q.H., Zhang B.H., Qian Y.B., Wu Z.Q., Fan J., et al. Postoperative interferon alpha treatment postponed recurrence and improved overall survival in patients after curative resection of HBV-related hepatocellular carcinoma: A randomized clinical trial. J. Cancer Res. Clin. Oncol. 2006;132:458–465. doi: 10.1007/s00432-006-0091-y. [DOI] [PubMed] [Google Scholar]
- 43.Lo C.M., Liu C.L., Chan S.C., Lam C.M., Poon R.T.P., Ng I.O.L., Fan S.T., Wong J. A randomized, controlled trial of postoperative adjuvant interferon therapy after resection of hepatocellular carcinoma. Ann. Surg. 2007;245:831–842. doi: 10.1097/01.sla.0000245829.00977.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen L.T., Chen M.F., Li L.A., Lee P.H., Jeng L.B., Lin D.Y., Wu C.C., Mok K.T., Chen C.L., Lee W.C., et al. Long-term results of a randomized, observation-controlled, phase III trial of adjuvant interferon Alfa-2b in hepatocellular carcinoma after curative resection. Ann. Surg. 2012;255:8–17. doi: 10.1097/SLA.0b013e3182363ff9. [DOI] [PubMed] [Google Scholar]
- 45.Sun P., Yang X., He R.Q., Hu Q.G., Song Z.F., Xiong J., Zheng Q.C. Antiviral therapy after curative treatment of hepatitis B/C virus-related hepatocellular carcinoma: A systematic review of randomized trials. Hepatol. Res. 2014;44:259–269. doi: 10.1111/hepr.12115. [DOI] [PubMed] [Google Scholar]
- 46.Qi W., Zhang Q., Xu Y., Wang X., Yu F., Zhang Y., Zhao P., Guo H., Zhou C., Wang Z., et al. Peg-interferon and nucleos(t)ide analogue combination at inception of antiviral therapy improves both anti-HBV efficacy and long-term survival among HBV DNA-positive hepatocellular carcinoma patients after hepatectomy/ablation. J. Viral Hepat. 2020;27:387–396. doi: 10.1111/jvh.13236. [DOI] [PubMed] [Google Scholar]
- 47.Surveillance Group. Diagnosis Group. Staging Group. Surgery Group. Local Ablation Group. TACE/TARE/HAI Group. Target Therapy/Systemic Therapy Group. Radiotherapy Group. Prevention Group. Drafting Group Management consensus guideline for hepatocellular carcinoma: 2016 updated by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J. Formos. Med Assoc. 2018;117:381–403. doi: 10.1016/j.jfma.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 48.Marcellin P., Gane E., Buti M., Afdhal N., Sievert W., Jacobson I.M., Washington M.K., Germanidis G., Flaherty J.F., Schall R.A., et al. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: A 5-year open-label follow-up study. Lancet. 2013;381:468–475. doi: 10.1016/S0140-6736(12)61425-1. [DOI] [PubMed] [Google Scholar]
- 49.Terrault N.A., Lok A.S.F., McMahon B.J., Chang K.M., Hwang J.P., Jonas M.M., Brown R.S., Jr., Bzowej N.H., Wong J.B. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–1599. doi: 10.1002/hep.29800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gill U.S., Kennedy P.T.F. The impact of currently licensed therapies on viral and immune responses in chronic hepatitis B: Considerations for future novel therapeutics. J. Viral Hepat. 2019;26:4–15. doi: 10.1111/jvh.13040. [DOI] [PubMed] [Google Scholar]
- 51.Liaw Y.F., Sung J.J.Y., Chow W.C., Farrell G., Lee C.Z., Yuen H., Tanwandee T., Tao Q.M., Shue K., Keene O.N., et al. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N. Engl. J. Med. 2004;351:1521–1531. doi: 10.1056/NEJMoa033364. [DOI] [PubMed] [Google Scholar]
- 52.Su T.H., Hu T.H., Chen C.Y., Huang Y.H., Chuang W.L., Lin C.C., Wang C.C., Su W.W., Chen M.Y., Peng C.Y., et al. Four-year entecavir therapy reduces hepatocellular carcinoma, cirrhotic events and mortality in chronic hepatitis B patients. Liver Int. 2016;36:1755–1764. doi: 10.1111/liv.13253. [DOI] [PubMed] [Google Scholar]
- 53.Wu C.Y., Lin J.T., Ho H.J., Su C.W., Lee T.Y., Wang S.Y., Wu C., Wu J.C. Association of nucleos(t)ide analogue therapy with reduced risk of hepatocellular carcinoma in patients with chronic hepatitis B: A nationwide cohort study. Gastroenterology. 2014;147:143–151. doi: 10.1053/j.gastro.2014.03.048. [DOI] [PubMed] [Google Scholar]
- 54.Lin D., Yang H.I., Nguyen N., Hoang J., Kim Y., Vu V., Le A., Chaung K., Nguyen V., Trinh H., et al. Reduction of chronic hepatitis B-related hepatocellular carcinoma with anti-viral therapy, including low risk patients. Aliment. Pharmacol. Ther. 2016;44:846–855. doi: 10.1111/apt.13774. [DOI] [PubMed] [Google Scholar]
- 55.Wong G.L., Tse Y.K., Chan H.L., Yip T.C., Tsoi K.K., Wong V.W. Oral nucleos(t)ide analogues reduce recurrence and death in chronic hepatitis B-related hepatocellular carcinoma. Aliment. Pharmacol. Ther. 2016;43:802–813. doi: 10.1111/apt.13548. [DOI] [PubMed] [Google Scholar]
- 56.Watanabe T., Tokumoto Y., Joko K., Michitaka K., Mashiba T., Hiraoka A., Ochi H., Koizumi Y., Tada F., Hirooka M., et al. Effects of long-term entecavir treatment on the incidence of hepatocellular carcinoma in chronic hepatitis B patients. Hepatol. Int. 2016;10:320–327. doi: 10.1007/s12072-015-9647-8. [DOI] [PubMed] [Google Scholar]
- 57.Chan A.C., Chok K.S., Yuen W.K., Chan S.C., Poon R.T., Lo C.M., Fan S.T. Impact of antiviral therapy on the survival of patients after major hepatectomy for hepatitis B virus-related hepatocellular carcinoma. Arch. Surg. 2011;146:675–681. doi: 10.1001/archsurg.2011.125. [DOI] [PubMed] [Google Scholar]
- 58.Wu C.Y., Chen Y.J., Ho H.J., Hsu Y.C., Kuo K.N., Wu M.S., Lin J.T. Association between nucleoside analogues and risk of hepatitis B virus-related hepatocellular carcinoma recurrence following liver resection. JAMA. 2012;308:1906–1914. doi: 10.1001/2012.jama.11975. [DOI] [PubMed] [Google Scholar]
- 59.Ke Y., Ma L., You X.M., Huang S.X., Liang Y.R., Xiang B.D., Li L.Q., Zhong J.H. Antiviral therapy for hepatitis B virus-related hepatocellular carcinoma after radical hepatectomy. Cancer Biol. Med. 2013;10:158–164. doi: 10.7497/j.issn.2095-3941.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yin J., Li N., Han Y., Xue J., Deng Y., Shi J., Guo W., Zhang H., Wang H., Cheng S., et al. Effect of antiviral treatment with nucleotide/nucleoside analogs on postoperative prognosis of hepatitis B virus-related hepatocellular carcinoma: A two-stage longitudinal clinical study. J. Clin. Oncol. 2013;31:3647–3655. doi: 10.1200/JCO.2012.48.5896. [DOI] [PubMed] [Google Scholar]
- 61.Sun P., Dong X., Cheng X., Hu Q., Zheng Q. Nucleot(s)ide analogues for hepatitis B virus-related hepatocellular carcinoma after curative treatment: A systematic review and meta-analysis. PLoS ONE. 2014;9:e102761. doi: 10.1371/journal.pone.0102761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang G., Lau W.Y., Wang Z.G., Pan Z.Y., Yuan S.X., Shen F., Zhou W.P., Wu M.C. Antiviral therapy improves postoperative survival in patients with hepatocellular carcinoma: A randomized controlled trial. Ann. Surg. 2015;261:56–66. doi: 10.1097/SLA.0000000000000858. [DOI] [PubMed] [Google Scholar]
- 63.Chong C.C., Wong G.L., Wong V.W., Ip P.C., Cheung Y.S., Wong J., Lee K.F., Lai P.B., Chan H.L. Antiviral therapy improves post-hepatectomy survival in patients with hepatitis B virus-related hepatocellular carcinoma: A prospective-retrospective study. Aliment. Pharmacol. Ther. 2015;41:199–208. doi: 10.1111/apt.13034. [DOI] [PubMed] [Google Scholar]
- 64.Lee T.Y., Lin J.T., Zeng Y.S., Chen Y.J., Wu M.S., Wu C.Y. Association between nucleos(t)ide analog and tumor recurrence in hepatitis B virus-related hepatocellular carcinoma after radiofrequency ablation. Hepatology. 2016;63:1517–1527. doi: 10.1002/hep.28266. [DOI] [PubMed] [Google Scholar]
- 65.Chen X.X., Cheng J.W., Huang A., Zhang X., Wang J., Fan J., Zhou J., Yang X.R. The effect of antiviral therapy on patients with hepatitis B virus-related hepatocellular carcinoma after curative resection: A systematic review and meta-analysis. OncoTargets Ther. 2017;10:5363–5375. doi: 10.2147/OTT.S150281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hui V.W., Chan S.L., Wong V.W., Liang L.Y., Yip T.C., Lai J.C., Yuen B.W., Luk H.W., Tse Y.K., Lee H.W., et al. Increasing antiviral treatment uptake improves survival in patients with HBV-related HCC. JHEP Rep. 2020;2:100152. doi: 10.1016/j.jhepr.2020.100152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cho H., Ahn H., Lee D.H., Lee J.H., Jung Y.J., Chang Y., Nam J.Y., Cho Y.Y., Lee D.H., Cho E.J., et al. Entecavir and tenofovir reduce hepatitis B virus-related hepatocellular carcinoma recurrence more effectively than other antivirals. J. Viral Hepat. 2018;25:707–717. doi: 10.1111/jvh.12855. [DOI] [PubMed] [Google Scholar]
- 68.Choi J., Jo C., Lim Y.S. Tenofovir Versus Entecavir on Recurrence of Hepatitis B Virus-Related Hepatocellular Carcinoma After Surgical Resection. Hepatology. 2020 doi: 10.1016/S0168-8278(20)30673-5. [DOI] [PubMed] [Google Scholar]
- 69.Chien R.N., Kao J.H., Peng C.Y., Chen C.H., Liu C.J., Huang Y.H., Hu T.H., Yang H.I., Lu S.N., Ni Y.H., et al. Taiwan consensus statement on the management of chronic hepatitis B. J. Formos. Med. Assoc. 2019;118:7–38. doi: 10.1016/j.jfma.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 70.Yeh C.T., Chen T., Hsu C.W., Chen Y.C., Lai M.W., Liang K.H., Chen T.C. Emergence of the rtA181T/sW172* mutant increased the risk of hepatoma occurrence in patients with lamivudine-resistant chronic hepatitis B. BMC Cancer. 2011;11:398. doi: 10.1186/1471-2407-11-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yip T.C., Wong G.L., Chan H.L., Tse Y.K., Lam K.L., Lui G.C., Wong V.W. HBsAg seroclearance further reduces hepatocellular carcinoma risk after complete viral suppression with nucleos(t)ide analogues. J. Hepatol. 2019;70:361–370. doi: 10.1016/j.jhep.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 72.Feld J.J., Krassenburg L.A.P. What Comes First: Treatment of Viral Hepatitis or Liver Cancer? Dig. Dis. Sci. 2019;64:1041–1049. doi: 10.1007/s10620-019-05518-5. [DOI] [PubMed] [Google Scholar]
- 73.Cronin K.A., Lake A.J., Scott S., Sherman R.L., Noone A.M., Howlader N., Henley S.J., Anderson R.N., Firth A.U., Ma J., et al. Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics. Cancer. 2018;124:2785–2800. doi: 10.1002/cncr.31551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thrift A.P., El-Serag H.B., Kanwal F. Global epidemiology and burden of HCV infection and HCV-related disease. Nat. Rev. Gastroenterol. Hepatol. 2017;14:122–132. doi: 10.1038/nrgastro.2016.176. [DOI] [PubMed] [Google Scholar]
- 75.Rein D.B., Wittenborn J.S., Weinbaum C.M., Sabin M., Smith B.D., Lesesne S.B. Forecasting the morbidity and mortality associated with prevalent cases of pre-cirrhotic chronic hepatitis C in the United States. Dig. Liver Dis. 2011;43:66–72. doi: 10.1016/j.dld.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 76.Hoshida Y., Fuchs B.C., Bardeesy N., Baumert T.F., Chung R.T. Pathogenesis and prevention of hepatitis C virus-induced hepatocellular carcinoma. J. Hepatol. 2014;61:S79–S90. doi: 10.1016/j.jhep.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mesri E.A., Feitelson M.A., Munger K. Human viral oncogenesis: A cancer hallmarks analysis. Cell Host Microbe. 2014;15:266–282. doi: 10.1016/j.chom.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Akkari L., Gregoire D., Floc’h N., Moreau M., Hernandez C., Simonin Y., Rosenberg A.R., Lassus P., Hibner U. Hepatitis C viral protein NS5A induces EMT and participates in oncogenic transformation of primary hepatocyte precursors. J. Hepatol. 2012;57:1021–1028. doi: 10.1016/j.jhep.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 79.Nault J.C., Zucman-Rossi J. TERT promoter mutations in primary liver tumors. Clin. Res. Hepatol. Gastroenterol. 2016;40:9–14. doi: 10.1016/j.clinre.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 80.Friedman R.M., Contente S. Treatment of hepatitis C infections with interferon: A historical perspective. Hepat. Res. Treat. 2010;2010:323926. doi: 10.1155/2010/323926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Manns M.P., McHutchison J.G., Gordon S.C., Rustgi V.K., Shiffman M., Reindollar R., Goodman Z.D., Koury K., Ling M.-H., Albrecht J.K. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: A randomised trial. Lancet. 2001;358:958–965. doi: 10.1016/S0140-6736(01)06102-5. [DOI] [PubMed] [Google Scholar]
- 82.Fried M.W., Shiffman M.L., Reddy K.R., Smith C., Marinos G., Gonçales Jr F.L., Häussinger D., Diago M., Carosi G., Dhumeaux D. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N. Engl. J. Med. 2002;347:975–982. doi: 10.1056/NEJMoa020047. [DOI] [PubMed] [Google Scholar]
- 83.Feld J.J., Hoofnagle J.H. Mechanism of action of interferon and ribavirin in treatment of hepatitis C. Nature. 2005;436:967. doi: 10.1038/nature04082. [DOI] [PubMed] [Google Scholar]
- 84.Stark G.R., Kerr I.M., Williams B.R., Silverman R.H., Schreiber R.D. How cells respond to interferons. Annu. Rev. Biochem. 1998;67:227–264. doi: 10.1146/annurev.biochem.67.1.227. [DOI] [PubMed] [Google Scholar]
- 85.Xu D., Erickson S., Szeps M., Gruber A., Sangfelt O., Einhorn S., Pisa P., Grandér D. Interferon α down-regulates telomerase reverse transcriptase and telomerase activity in human malignant and nonmalignant hematopoietic cells. Blood. 2000;96:4313–4318. doi: 10.1182/blood.V96.13.4313. [DOI] [PubMed] [Google Scholar]
- 86.Matsumoto K., Okano J.-I., Murawaki Y. Differential effects of interferon alpha-2b and beta on the signaling pathways in human liver cancer cells. J. Gastroenterol. 2005;40:722–732. doi: 10.1007/s00535-005-1616-x. [DOI] [PubMed] [Google Scholar]
- 87.Negrier S., Escudier B., Lasset C., Douillard J.-Y., Savary J., Chevreau C., Ravaud A., Mercatello A., Peny J., Mousseau M. Recombinant human interleukin-2, recombinant human interferon alfa-2a, or both in metastatic renal-cell carcinoma. N. Engl. J. Med. 1998;338:1272–1278. doi: 10.1056/NEJM199804303381805. [DOI] [PubMed] [Google Scholar]
- 88.Yano H., Iemura A., Haramaki M., Ogasawara S., Takayama A., Akiba J., Kojiro M. Interferon alfa receptor expression and growth inhibition by interferon alfa in human liver cancer cell lines. Hepatology. 1999;29:1708–1717. doi: 10.1002/hep.510290624. [DOI] [PubMed] [Google Scholar]
- 89.Klaus A., Birchmeier W. Wnt signalling and its impact on development and cancer. Nat. Rev. Cancer. 2008;8:387. doi: 10.1038/nrc2389. [DOI] [PubMed] [Google Scholar]
- 90.Pasquali S., Mocellin S. The anticancer face of interferon alpha (IFN-alpha): From biology to clinical results, with a focus on melanoma. Curr. Med. Chem. 2010;17:3327–3336. doi: 10.2174/092986710793176393. [DOI] [PubMed] [Google Scholar]
- 91.Villani R., Vendemiale G., Serviddio G. Molecular Mechanisms Involved in HCC Recurrence after Direct-Acting Antiviral Therapy. Int. J. Mol. Sci. 2018;20:49. doi: 10.3390/ijms20010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Burchill M.A., Golden-Mason L., Wind-Rotolo M., Rosen H.R. Memory re-differentiation and reduced lymphocyte activation in chronic HCV-infected patients receiving direct-acting antivirals. J. Viral Hepat. 2015;22:983–991. doi: 10.1111/jvh.12465. [DOI] [PubMed] [Google Scholar]
- 93.Martin B., Hennecke N., Lohmann V., Kayser A., Neumann-Haefelin C., Kukolj G., Böcher W.-O., Thimme R. Restoration of HCV-specific CD8+ T cell function by interferon-free therapy. J. Hepatol. 2014;61:538–543. doi: 10.1016/j.jhep.2014.05.043. [DOI] [PubMed] [Google Scholar]
- 94.Hengst J., Strunz B., Deterding K., Ljunggren H.G., Leeansyah E., Manns M.P., Cornberg M., Sandberg J.K., Wedemeyer H., Bjorkstrom N.K. Nonreversible MAIT cell-dysfunction in chronic hepatitis C virus infection despite successful interferon-free therapy. Eur. J. Immunol. 2016;46:2204–2210. doi: 10.1002/eji.201646447. [DOI] [PubMed] [Google Scholar]
- 95.Langhans B., Nischalke H.D., Kramer B., Hausen A., Dold L., van Heteren P., Huneburg R., Nattermann J., Strassburg C.P., Spengler U. Increased peripheral CD4(+) regulatory T cells persist after successful direct-acting antiviral treatment of chronic hepatitis C. J. Hepatol. 2017;66:888–896. doi: 10.1016/j.jhep.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 96.Dilek N., Poirier N., Hulin P., Coulon F., Mary C., Ville S., Vie H., Clemenceau B., Blancho G., Vanhove B. Targeting CD28, CTLA-4 and PD-L1 costimulation differentially controls immune synapses and function of human regulatory and conventional T-cells. PLoS ONE. 2013;8:e83139. doi: 10.1371/journal.pone.0083139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Serti E., Chepa-Lotrea X., Kim Y.J., Keane M., Fryzek N., Liang T.J., Ghany M., Rehermann B. Successful Interferon-Free Therapy of Chronic Hepatitis C Virus Infection Normalizes Natural Killer Cell Function. Gastroenterology. 2015;149:190–200.e192. doi: 10.1053/j.gastro.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pahl J., Cerwenka A. Tricking the balance: NK cells in anti-cancer immunity. Immunobiology. 2017;222:11–20. doi: 10.1016/j.imbio.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 99.Chu P.S., Nakamoto N., Taniki N., Ojiro K., Amiya T., Makita Y., Murata H., Yamaguchi A., Shiba S., Miyake R., et al. On-treatment decrease of NKG2D correlates to early emergence of clinically evident hepatocellular carcinoma after interferon-free therapy for chronic hepatitis C. PLoS ONE. 2017;12:e0179096. doi: 10.1371/journal.pone.0179096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rehermann B. Natural Killer Cells in Viral Hepatitis. Cell. Mol. Gastroenterol. Hepatol. 2015;1:578–588. doi: 10.1016/j.jcmgh.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Debes J.D., van Tilborg M., Groothuismink Z.M.A., Hansen B.E., Schulze Zur Wiesch J., von Felden J., de Knegt R.J., Boonstra A. Levels of Cytokines in Serum Associate With Development of Hepatocellular Carcinoma in Patients With HCV Infection Treated With Direct-Acting Antivirals. Gastroenterology. 2018;154:515–517.e513. doi: 10.1053/j.gastro.2017.10.035. [DOI] [PubMed] [Google Scholar]
- 102.Hamdane N., Juhling F., Crouchet E., El Saghire H., Thumann C., Oudot M.A., Bandiera S., Saviano A., Ponsolles C., Roca Suarez A.A., et al. HCV-Induced Epigenetic Changes Associated With Liver Cancer Risk Persist After Sustained Virologic Response. Gastroenterology. 2019;156:2313–2329.e2317. doi: 10.1053/j.gastro.2019.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Faillaci F., Marzi L., Critelli R., Milosa F., Schepis F., Turola E., Andreani S., Vandelli G., Bernabucci V., Lei B., et al. Liver Angiopoietin-2 Is a Key Predictor of De Novo or Recurrent Hepatocellular Cancer After Hepatitis C Virus Direct-Acting Antivirals. Hepatology. 2018;68:1010–1024. doi: 10.1002/hep.29911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Itami-Matsumoto S., Hayakawa M., Uchida-Kobayashi S., Enomoto M., Tamori A., Mizuno K., Toyoda H., Tamura T., Akutsu T., Ochiya T., et al. Circulating Exosomal miRNA Profiles Predict the Occurrence and Recurrence of Hepatocellular Carcinoma in Patients with Direct-Acting Antiviral-Induced Sustained Viral Response. Biomedicines. 2019;7:87. doi: 10.3390/biomedicines7040087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Poynard T., McHutchison J., Manns M., Trepo C., Lindsay K., Goodman Z., Ling M.H., Albrecht J. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122:1303–1313. doi: 10.1053/gast.2002.33023. [DOI] [PubMed] [Google Scholar]
- 106.Hsu Y.C., Ho H.J., Wu M.S., Lin J.T., Wu C.Y. Postoperative peg-interferon plus ribavirin is associated with reduced recurrence of hepatitis C virus-related hepatocellular carcinoma. Hepatology. 2013;58:150–157. doi: 10.1002/hep.26300. [DOI] [PubMed] [Google Scholar]
- 107.Chen Y.C., Teng W., Hsieh Y.C., Chen W.T., Jeng W.J., Huang C.H., Lin C.C., Chen Y.C., Lin S.M., Lin C.Y., et al. Timely eradication of HCV viremia by PegIFN/RBV is crucial in prevention of post RFA recurrence in CHC-HCC patients. J. Formos. Med. Assoc. 2019;118:1239–1246. doi: 10.1016/j.jfma.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 108.Teng W., Hsieh Y.C., Lui K.W., Chen W.T., Hung C.F., Huang C.H., Chen Y.C., Jeng W.J., Lin C.C., Lin C.Y., et al. Eradication of hepatitis C virus profoundly prolongs survival in hepatocellular carcinoma patients receiving transarterial chemoembolization. J. Viral Hepat. 2017;24:1160–1167. doi: 10.1111/jvh.12745. [DOI] [PubMed] [Google Scholar]
- 109.Huang J.F., Yeh M.L., Yu M.L., Dai C.Y., Huang C.F., Huang C.I., Tsai P.C., Lin P.C., Chen Y.L., Chang W.T., et al. The tertiary prevention of hepatocellular carcinoma in chronic hepatitis C patients. J. Gastroenterol. Hepatol. 2015;30:1768–1774. doi: 10.1111/jgh.13012. [DOI] [PubMed] [Google Scholar]
- 110.Zhuang L., Zeng X., Yang Z., Meng Z. Effect and safety of interferon for hepatocellular carcinoma: A systematic review and meta-analysis. PLoS ONE. 2013;8:e61361. doi: 10.1371/journal.pone.0061361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Manthravadi S., Paleti S., Pandya P. Impact of sustained viral response postcurative therapy of hepatitis C-related hepatocellular carcinoma: A systematic review and meta-analysis. Int. J. Cancer. 2017;140:1042–1049. doi: 10.1002/ijc.30521. [DOI] [PubMed] [Google Scholar]
- 112.Mazzaferro V., Romito R., Schiavo M., Mariani L., Camerini T., Bhoori S., Capussotti L., Calise F., Pellicci R., Belli G. Prevention of hepatocellular carcinoma recurrence with alpha-interferon after liver resection in HCV cirrhosis. Hepatology. 2006;44:1543–1554. doi: 10.1002/hep.21415. [DOI] [PubMed] [Google Scholar]
- 113.Kudo M., Sakaguchi Y., Chung H., Hatanaka K., Hagiwara S., Ishikawa E., Takahashi S., Kitai S., Inoue T., Minami Y. Long-term interferon maintenance therapy improves survival in patients with HCV-related hepatocellular carcinoma after curative radiofrequency ablation. Oncology. 2007;72:132–138. doi: 10.1159/000111719. [DOI] [PubMed] [Google Scholar]
- 114.Jeong S.C., Aikata H., Katamura Y., Azakami T., Kawaoka T., Saneto H., Uka K., Mori N., Takaki S., Kodama H. Effects of a 24-week course of interferon-α therapy after curative treatment of hepatitis C virus-associated hepatocellular carcinoma. World, J. Gastroenterol. WJG. 2007;13:5343. doi: 10.3748/wjg.v13.i40.5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kanogawa N., Ogasawara S., Chiba T., Saito T., Motoyama T., Suzuki E., Ooka Y., Tawada A., Kanda T., Mikami S. Sustained virologic response achieved after curative treatment of hepatitis C virus-related hepatocellular carcinoma as an independent prognostic factor. J. Gastroenterol. Hepatol. 2015;30:1197–1204. doi: 10.1111/jgh.12925. [DOI] [PubMed] [Google Scholar]
- 116.Petta S., Cabibbo G., Barbara M., Attardo S., Bucci L., Farinati F., Giannini E.G., Tovoli F., Ciccarese F., Rapaccini G.L., et al. Hepatocellular carcinoma recurrence in patients with curative resection or ablation: Impact of HCV eradication does not depend on the use of interferon. Aliment. Pharmacol. Ther. 2017;45:160–168. doi: 10.1111/apt.13821. [DOI] [PubMed] [Google Scholar]
- 117.Baumert T.F., Berg T., Lim J.K., Nelson D.R. Status of Direct-Acting Antiviral Therapy for Hepatitis C Virus Infection and Remaining Challenges. Gastroenterology. 2019;156:431–445. doi: 10.1053/j.gastro.2018.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Knop V., Hoppe D., Welzel T., Vermehren J., Herrmann E., Vermehren A., Friedrich-Rust M., Sarrazin C., Zeuzem S., Welker M.W. Regression of fibrosis and portal hypertension in HCV-associated cirrhosis and sustained virologic response after interferon-free antiviral therapy. J. Viral Hepat. 2016;23:994–1002. doi: 10.1111/jvh.12578. [DOI] [PubMed] [Google Scholar]
- 119.Foster G.R., Irving W.L., Cheung M.C., Walker A.J., Hudson B.E., Verma S., McLauchlan J., Mutimer D.J., Brown A., Gelson W.T., et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J. Hepatol. 2016;64:1224–1231. doi: 10.1016/j.jhep.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 120.Reddy K.R., Lim J.K., Kuo A., Di Bisceglie A.M., Galati J.S., Morelli G., Everson G.T., Kwo P.Y., Brown R.S., Jr., Sulkowski M.S., et al. All-oral direct-acting antiviral therapy in HCV-advanced liver disease is effective in real-world practice: Observations through HCV-TARGET database. Aliment. Pharmacol. Ther. 2017;45:115–126. doi: 10.1111/apt.13823. [DOI] [PubMed] [Google Scholar]
- 121.Reig M., Marino Z., Perello C., Inarrairaegui M., Ribeiro A., Lens S., Diaz A., Vilana R., Darnell A., Varela M., et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J. Hepatol. 2016;65:719–726. doi: 10.1016/j.jhep.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 122.Conti F., Buonfiglioli F., Scuteri A., Crespi C., Bolondi L., Caraceni P., Foschi F.G., Lenzi M., Mazzella G., Verucchi G., et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J. Hepatol. 2016;65:727–733. doi: 10.1016/j.jhep.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 123.Warzyszynska K., Jonas M., Wasiak D., Kosieradzki M., Malkowski P. Accelerated hepatocellular carcinoma recurrence rate after postoperative direct-acting antivirals treatment—preliminary report. Clin. Exp. Hepatol. 2017;3:194–197. doi: 10.5114/ceh.2017.71483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cabibbo G., Petta S., Calvaruso V., Cacciola I., Cannavo M.R., Madonia S., Distefano M., Larocca L., Prestileo T., Tine F., et al. Is early recurrence of hepatocellular carcinoma in HCV cirrhotic patients affected by treatment with direct-acting antivirals? A prospective multicentre study. Aliment. Pharmacol. Ther. 2017;46:688–695. doi: 10.1111/apt.14256. [DOI] [PubMed] [Google Scholar]
- 125.Ogawa E., Furusyo N., Nomura H., Dohmen K., Higashi N., Takahashi K., Kawano A., Azuma K., Satoh T., Nakamuta M., et al. Short-term risk of hepatocellular carcinoma after hepatitis C virus eradication following direct-acting anti-viral treatment. Aliment. Pharmacol. Ther. 2018;47:104–113. doi: 10.1111/apt.14380. [DOI] [PubMed] [Google Scholar]
- 126.Calleja J.L., Crespo J., Rincon D., Ruiz-Antoran B., Fernandez I., Perello C., Gea F., Lens S., Garcia-Samaniego J., Sacristan B., et al. Effectiveness, safety and clinical outcomes of direct-acting antiviral therapy in HCV genotype 1 infection: Results from a Spanish real-world cohort. J. Hepatol. 2017;66:1138–1148. doi: 10.1016/j.jhep.2017.01.028. [DOI] [PubMed] [Google Scholar]
- 127.Nakano M., Koga H., Ide T., Kuromatsu R., Hashimoto S., Yatsuhashi H., Seike M., Higuchi N., Nakamuta M., Shakado S., et al. Predictors of hepatocellular carcinoma recurrence associated with the use of direct-acting antiviral agent therapy for hepatitis C virus after curative treatment: A prospective multicenter cohort study. Cancer Med. 2019;8:2646–2653. doi: 10.1002/cam4.2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bielen R., Moreno C., Van Vlierberghe H., Bourgeois S., Mulkay J.P., Vanwolleghem T., Verlinden W., Brixco C., Decaestecker J., de Galocsy C., et al. The risk of early occurrence and recurrence of hepatocellular carcinoma in hepatitis C-infected patients treated with direct-acting antivirals with and without pegylated interferon: A Belgian experience. J. Viral Hepat. 2017;24:976–981. doi: 10.1111/jvh.12726. [DOI] [PubMed] [Google Scholar]
- 129.Cheung M.C.M., Walker A.J., Hudson B.E., Verma S., McLauchlan J., Mutimer D.J., Brown A., Gelson W.T.H., MacDonald D.C., Agarwal K., et al. Outcomes after successful direct-acting antiviral therapy for patients with chronic hepatitis C and decompensated cirrhosis. J. Hepatol. 2016;65:741–747. doi: 10.1016/j.jhep.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 130.Yoshimasu Y., Furuichi Y., Kasai Y., Takeuchi H., Sugimoto K., Nakamura I., Itoi T. Predictive factors for hepatocellular carcinoma occurrence or recurrence after direct-acting antiviral agents in patients with chronic hepatitis C. J. Gastrointestin. Liver Dis. 2019;28:63–71. doi: 10.15403/jgld.2014.1121.281.hpc. [DOI] [PubMed] [Google Scholar]
- 131.The ANRS Collaborative Study Group on Hepatocellular Carcinoma Lack of evidence of an effect of direct-acting antivirals on the recurrence of hepatocellular carcinoma: Data from three ANRS cohorts. J. Hepatol. 2016;65:734–740. doi: 10.1016/j.jhep.2016.05.045. [DOI] [PubMed] [Google Scholar]
- 132.Kolly P., Waidmann O., Vermehren J., Moreno C., Vögeli I., Berg T., Semela D., Zeuzem S., Dufour J.-F. Hepatocellular carcinoma recurrence after direct antiviral agent treatment: A European multicentre study. J. Hepatol. 2017;67:876–878. doi: 10.1016/j.jhep.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 133.Virlogeux V., Pradat P., Hartig-Lavie K., Bailly F., Maynard M., Ouziel G., Poinsot D., Lebosse F., Ecochard M., Radenne S., et al. Direct-acting antiviral therapy decreases hepatocellular carcinoma recurrence rate in cirrhotic patients with chronic hepatitis C. Liver Int. 2017;37:1122–1127. doi: 10.1111/liv.13456. [DOI] [PubMed] [Google Scholar]
- 134.Zavaglia C., Okolicsanyi S., Cesarini L., Mazzarelli C., Pontecorvi V., Ciaccio A., Strazzabosco M., Belli L.S. Is the risk of neoplastic recurrence increased after prescribing direct-acting antivirals for HCV patients whose HCC was previously cured? J. Hepatol. 2017;66:236–237. doi: 10.1016/j.jhep.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 135.Ikeda K., Kawamura Y., Kobayashi M., Kominami Y., Fujiyama S., Sezaki H., Hosaka T., Akuta N., Saitoh S., Suzuki F., et al. Direct-Acting Antivirals Decreased Tumor Recurrence After Initial Treatment of Hepatitis C Virus-Related Hepatocellular Carcinoma. Dig. Dis. Sci. 2017;62:2932–2942. doi: 10.1007/s10620-017-4739-z. [DOI] [PubMed] [Google Scholar]
- 136.Saraiya N., Yopp A.C., Rich N.E., Odewole M., Parikh N.D., Singal A.G. Systematic review with meta-analysis: Recurrence of hepatocellular carcinoma following direct-acting antiviral therapy. Aliment. Pharmacol. Ther. 2018;48:127–137. doi: 10.1111/apt.14823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Singh S., Nautiyal A., Loke Y.K. Oral direct-acting antivirals and the incidence or recurrence of hepatocellular carcinoma: A systematic review and meta-analysis. Frontline Gastroenterol. 2018;9:262–270. doi: 10.1136/flgastro-2018-101017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Huang A.C., Mehta N., Dodge J.L., Yao F.Y., Terrault N.A. Direct-acting antivirals do not increase the risk of hepatocellular carcinoma recurrence after local-regional therapy or liver transplant waitlist dropout. Hepatology. 2018;68:449–461. doi: 10.1002/hep.29855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Singal A.G., Rich N.E., Mehta N., Branch A., Pillai A., Hoteit M., Volk M., Odewole M., Scaglione S., Guy J., et al. Direct-Acting Antiviral Therapy Not Associated With Recurrence of Hepatocellular Carcinoma in a Multicenter North American Cohort Study. Gastroenterology. 2019 doi: 10.1053/j.gastro.2019.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Cabibbo G., Celsa C., Calvaruso V., Petta S., Cacciola I., Cannavò M.R., Madonia S., Rossi M., Magro B., Rini F., et al. Direct acting antivirals after successful treatment of early hepatocellular carcinoma improve survival in HCV-cirrhotic patients. J. Hepatol. 2019 doi: 10.1016/j.jhep.2019.03.027. [DOI] [PubMed] [Google Scholar]
- 141.Minami T., Tateishi R., Nakagomi R., Fujiwara N., Sato M., Enooku K., Nakagawa H., Asaoka Y., Kondo Y., Shiina S., et al. The impact of direct-acting antivirals on early tumor recurrence after radiofrequency ablation in hepatitis C-related hepatocellular carcinoma. J. Hepatol. 2016;65:1272–1273. doi: 10.1016/j.jhep.2016.07.043. [DOI] [PubMed] [Google Scholar]
- 142.Nishibatake Kinoshita M., Minami T., Tateishi R., Wake T., Nakagomi R., Fujiwara N., Sato M., Uchino K., Enooku K., Nakagawa H., et al. Impact of direct-acting antivirals on early recurrence of HCV-related HCC: Comparison with interferon-based therapy. J. Hepatol. 2018 doi: 10.1016/j.jhep.2018.09.029. [DOI] [PubMed] [Google Scholar]
- 143.Nagata H., Nakagawa M., Asahina Y., Sato A., Asano Y., Tsunoda T., Miyoshi M., Kaneko S., Otani S., Kawai-Kitahata F., et al. Effect of interferon-based and -free therapy on early occurrence and recurrence of hepatocellular carcinoma in chronic hepatitis C. J. Hepatol. 2017;67:933–939. doi: 10.1016/j.jhep.2017.05.028. [DOI] [PubMed] [Google Scholar]
- 144.Nagaoki Y., Imamura M., Nisihda Y., Daijo K., Teraoka Y., Honda F., Nakamura Y., Morio K., Fujino H., Nakahara T., et al. The impact of interferon-free direct-acting antivirals on clinical outcome after curative treatment for hepatitis C virus-associated hepatocellular carcinoma; comparison with interferon-based therapy. J. Med. Virol. 2018 doi: 10.1002/jmv.25352. [DOI] [PubMed] [Google Scholar]
- 145.Mashiba T., Joko K., Kurosaki M., Ochi H., Osaki Y., Kojima Y., Nakata R., Goto T., Takehiro A., Kimura H., et al. Does interferon-free direct-acting antiviral therapy for hepatitis C after curative treatment for hepatocellular carcinoma lead to unexpected recurrences of HCC? A multicenter study by the Japanese Red Cross Hospital Liver Study Group. PLoS ONE. 2018;13:e0194704. doi: 10.1371/journal.pone.0194704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.El Kassas M., Funk A.L., Salaheldin M., Shimakawa Y., Eltabbakh M., Jean K., El Tahan A., Sweedy A.T., Afify S., Youssef N.F., et al. Increased recurrence rates of hepatocellular carcinoma after DAA therapy in a hepatitis C-infected Egyptian cohort: A comparative analysis. J. Viral Hepat. 2018;25:623–630. doi: 10.1111/jvh.12854. [DOI] [PubMed] [Google Scholar]
- 147.Waziry R., Hajarizadeh B., Grebely J., Amin J., Law M., Danta M., George J., Dore G.J. Hepatocellular carcinoma risk following direct-acting antiviral HCV therapy: A systematic review, meta-analyses, and meta-regression. J. Hepatol. 2017;67:1204–1212. doi: 10.1016/j.jhep.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 148.Teng W., Jeng W.J., Yang H.I., Chen W.T., Hsieh Y.C., Huang C.H., Lin C.C., Lin C.Y., Lin S.M., Sheen I.S. Interferon Is Superior to Direct Acting Antiviral Therapy in Tertiary Prevention of Early Recurrence of Hepatocellular Carcinoma. Cancers. 2019;12:23. doi: 10.3390/cancers12010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Cabibbo G., Petta S., Barbara M., Attardo S., Bucci L., Farinati F., Giannini E.G., Negrini G., Ciccarese F., Rapaccini G.L., et al. Hepatic decompensation is the major driver of death in HCV-infected cirrhotic patients with successfully treated early hepatocellular carcinoma. J. Hepatol. 2017;67:65–71. doi: 10.1016/j.jhep.2017.01.033. [DOI] [PubMed] [Google Scholar]
- 150.Ogawa E., Furusyo N., Kajiwara E., Takahashi K., Nomura H., Maruyama T., Tanabe Y., Satoh T., Nakamuta M., Kotoh K., et al. Efficacy of pegylated interferon alpha-2b and ribavirin treatment on the risk of hepatocellular carcinoma in patients with chronic hepatitis C: A prospective, multicenter study. J. Hepatol. 2013;58:495–501. doi: 10.1016/j.jhep.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 151.Roberts L.R., Sirlin C.B., Zaiem F., Almasri J., Prokop L.J., Heimbach J.K., Murad M.H., Mohammed K. Imaging for the diagnosis of hepatocellular carcinoma: A systematic review and meta-analysis. Hepatology. 2018;67:401–421. doi: 10.1002/hep.29487. [DOI] [PubMed] [Google Scholar]
- 152.Singal A.G., Lim J.K., Kanwal F. AGA Clinical Practice Update on Interaction Between Oral Direct-Acting Antivirals for Chronic Hepatitis C Infection and Hepatocellular Carcinoma: Expert Review. Gastroenterology. 2019;156:2149–2157. doi: 10.1053/j.gastro.2019.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Prenner S.B., VanWagner L.B., Flamm S.L., Salem R., Lewandowski R.J., Kulik L. Hepatocellular carcinoma decreases the chance of successful hepatitis C virus therapy with direct-acting antivirals. J. Hepatol. 2017;66:1173–1181. doi: 10.1016/j.jhep.2017.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Beste L.A., Green P.K., Berry K., Kogut M.J., Allison S.K., Ioannou G.N. Effectiveness of hepatitis C antiviral treatment in a USA cohort of veteran patients with hepatocellular carcinoma. J. Hepatol. 2017;67:32–39. doi: 10.1016/j.jhep.2017.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.El-Khoueiry A.B., Sangro B., Yau T., Crocenzi T.S., Kudo M., Hsu C., Kim T.-Y., Choo S.-P., Trojan J., Welling T.H., et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): An open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhu A.X., Finn R.S., Edeline J., Cattan S., Ogasawara S., Palmer D., Verslype C., Zagonel V., Fartoux L., Vogel A., et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): A non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19:940–952. doi: 10.1016/S1470-2045(18)30351-6. [DOI] [PubMed] [Google Scholar]
- 157.Finn R.S., Ryoo B.Y., Merle P., Kudo M., Bouattour M., Lim H.Y., Breder V., Edeline J., Chao Y., Ogasawara S., et al. Pembrolizumab As Second-Line Therapy in Patients With Advanced Hepatocellular Carcinoma in KEYNOTE-240: A Randomized, Double-Blind, Phase III Trial. J. Clin. Oncol. 2020;38:193–202. doi: 10.1200/JCO.19.01307. [DOI] [PubMed] [Google Scholar]
- 158.Finn R.S., Qin S., Ikeda M., Galle P.R., Ducreux M., Kim T.Y., Kudo M., Breder V., Merle P., Kaseb A.O., et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020;382:1894–1905. doi: 10.1056/NEJMoa1915745. [DOI] [PubMed] [Google Scholar]
- 159.Lee P.-C., Chao Y., Chen M.-H., Lan K.-H., Lee I.C., Hou M.-C., Huang Y.-H. Risk of HBV reactivation in patients with immune checkpoint inhibitor-treated unresectable hepatocellular carcinoma. J. Immunother. Cancer. 2020;8 doi: 10.1136/jitc-2020-001072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wong G.L., Wong V.W., Hui V.W., Yip T.C., Tse Y.K., Liang L.Y., Lui R.N., Mok T.S., Chan H.L., Chan S.L. Hepatitis Flare During Immunotherapy in Patients With Current or Past Hepatitis B Virus Infection. Am. J. Gastroenterol. 2021 doi: 10.14309/ajg.0000000000001142. [DOI] [PubMed] [Google Scholar]
- 161.Davar D., Wilson M., Pruckner C., Kirkwood J.M. PD-1 Blockade in Advanced Melanoma in Patients with Hepatitis C and/or HIV. Case Rep. Oncol. Med. 2015;2015:737389. doi: 10.1155/2015/737389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Pertejo-Fernandez A., Ricciuti B., Hammond S.P., Marty F.M., Recondo G., Rangachari D., Costa D.B., Awad M.M. Safety and efficacy of immune checkpoint inhibitors in patients with non-small cell lung cancer and hepatitis B or hepatitis C infection. Lung Cancer. 2020;145:181–185. doi: 10.1016/j.lungcan.2020.02.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.