Abstract
The coronavirus disease 2019 (COVID-19) is a highly contagious novel infection that predominantly presents with fever and respiratory symptoms. However, COVID-19 can masquerade as an acute coronary syndrome, leg pain or swelling with venous thrombosis, loss of consciousness with cerebral venous thrombosis, confusion, limb weakness with brain infarction, facial neuralgia, acute conjunctivitis, acute appendicitis, and testicular pain. We report on a 42-year-old man who presented with mild symptoms of COVID-19. The patient's electrocardiogram showed an ST-segment elevation myocardial infarction (STEMI) due to a left coronary thrombosis. The patient was managed conservatively with medicines and had an uneventful recovery. Emergency physicians should have a high index of suspicion for the unusual presentations of COVID-19.
Keywords: Abdominal pain, Acute coronary syndrome, COVID-19, Unusual presentations, Venous thrombosis
الملخص
فيروس كورونا ٢٠١٩ (كوفيد-١٩) هو مرض وبائي شديد العدوى وفي الغالب يكون مصحوبا بالحمى والأعراض التنفسية، ولكنه قد يأتي متنكرا بمتلازمة الشريان التاجي الحادة، أو ألم أو تورم للساق مع تجلط وريدي، أو فقدان الوعي مع تخثر وريدي دماغي، أو ارتباك، أو ضعف الأطراف مع احتشاء الدماغ، أو ألم العصب الوجهي، أو التهاب ملتحمة العين الحاد، أو ألم الحفرة الحرقفي اليمنى مثل التهاب الزائدة أو ألم الخصية. هنا قدمنا حالة لمريض ذكر في ٤٢ من عمره كان يعاني من أعراض كوفيد-١٩ خفيفة، وتطورت إلى احتشاء في عضلة القلب بسبب تخثر في الشريان التاجي الأيسر. تمت معالجة المريض بالأدوية وتحسنت حالته. يجب أن يكون أطباء الطوارئ يقظين للأعراض غير الاعتيادية التي قد يأتي بها مرضى كوفيد-١٩ وخاصة أثناء الجائحة.
الكلمات المفتاحية: كوفيد-١٩, أعراض غير اعتيادية, متلازمة الشريان التاجي الحادة, تخثر وريدي, آلام البطن
Introduction
The novel coronavirus disease 2019 (COVID-19) is a highly contagious disease that originated in Wuhan, China in December 2019. The disease is caused by infection with the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The World Health Organization declared a global pandemic in March 2020.1 COVID-19 patients typically present with fever, cough, myalgia, or fatigue. Less common features are sputum, headache, haemoptysis, and diarrhoea.2 Some patients may develop dyspnoea and need intensive care. Anosmia and loss of taste are atypical symptoms that have been reported in some cases.3 Patients may present with unusual or atypical clinical features that are not related to the respiratory system, which may mislead the diagnosis of COVID-19.4 COVID-19 can present with or be complicated by several extrapulmonary manifestations like thrombosis, myocardial problems, acute coronary syndrome (ACS), acute renal injury, hepatocellular injury, gastrointestinal symptoms and signs, elevated blood sugar problems, neurological manifestations, ocular symptoms and signs, and dermatological features.5
In our case, we report on a COVID-19 patient with atypical presentation. This work aimed to highlight the unusual, atypical, and strange clinical presentations of COVID-19 to alert physicians about them, especially during the ongoing pandemic. A brief literature review was performed using a PubMed search for the term “unusual presentation of COVID-19.” The review included published case reports available through PubMed in the English language from January 2020 to August 2020.
Case presentation
A 42-year-old male patient presented to the emergency department with fever, dry cough, anosmia, and fatigue, and his nasopharyngeal swab reverse transcriptase-polymerase chain reaction (RT-PCR) test confirmed the diagnosis of COVID-19. The patient was advised to isolate at home and was given hydroxychloroquine 400 mg/day, azithromycin 500 mg/day, zinc 30 mg/day, and Paracetamol as needed.
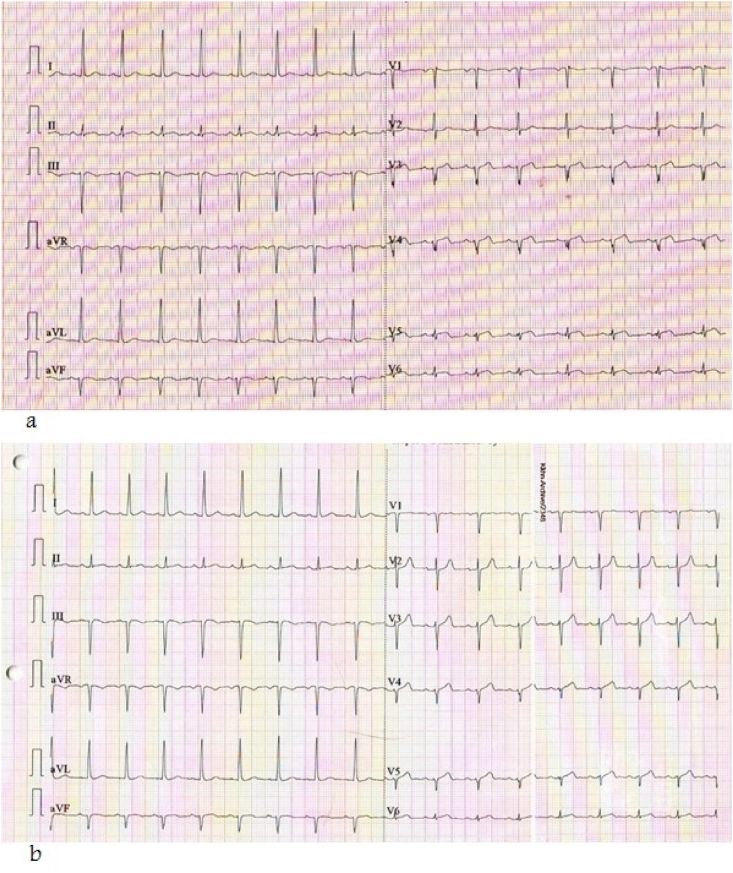
On the ninth day, the patient returned to the emergency department with recurrent retrosternal chest pain attacks radiating to the left shoulder and associated with nausea. The patient's temperature was 36.8°, his respiratory rate was 18 cycles/minute, his heart rate was 83 beats/minute, and his blood pressure was 130/80 mmHg. The results of his respiratory and cardiovascular clinical examination were unremarkable. The results of his chest x-ray were also unremarkable. Electrocardiogram (ECG) showed a normal sinus rhythm with left ventricular hypertrophy detected using aVL voltage and ST elevation in V3 to V6 that improved after two days of primary care (Figure 1a and b). Serial cardiac troponin T (TnT) was elevated [first result was normal, second was 0.51, and third was 0.78 (normal is up to 0.04 ng per millilitre)]. Echocardiogram (ECHO) showed normal left ventricular systolic function, and ejection fraction (EF) was 60%, with normal wall motion and normal valves. The patient was admitted to the intensive care unit (ICU) dedicated to COVID-19 patients.
Figure 1.
Serial electrocardiogram (ECG) showing a) normal sinus rhythm with left ventricular hypertrophy detected using aVL voltage and ST elevation in V3 to V6, and b) normal sinus rhythm with left ventricular hypertrophy detected using aVL voltage and slight ST elevation in V3 to V5 (improvement after two days of treatment).
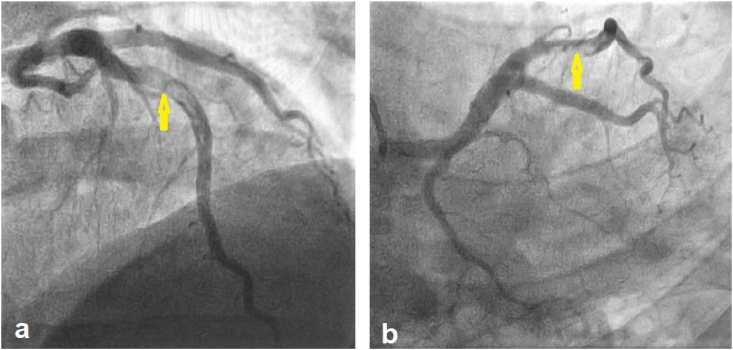
On the tenth day, chest pain attacks increased, ECG showed ST elevation and biphasic T inversion with poor R progression in V3 to V6. The patient was diagnosed as ST-segment elevation myocardial infarction (STEMI) and referred to a catheter laboratory (Cath lab) for possible primary percutaneous coronary intervention (PPCI) according to the local guidelines of STEMI during COVID-19. Coronary angiography through a right femoral approach was done, revealing a large thrombus in the middle left anterior descending (LAD) artery with post-interventional thrombolysis in myocardial infarction (TIMI) flow 3 and no significant stenosis (Figure 2a and b). The left circumflex coronary artery and the right coronary artery (RCA) were normal. The patient was managed conservatively with Aspirin, Clopidogrel, beta blockers, Tirofiban, and low dose Heparin infusions for 72 h and continued on Enoxaparin for seven days. A follow up ECHO showed no new abnormalities, with normal systolic function and an EF of 69%.
Figure 2.
Selected images of a left CAG a) cranial view and b) caudal view showing a large thrombus in the LAD artery (arrows).
On the twentieth day, a follow-up coronary angiogram (CAG) showed partial resolution of the left anterior descending (LAD) artery thrombus with residual particles in situ (Figure 3). The patient continued with triple treatment, with Aspirin, Clopidogrel, and Apixaban, and a CAG was arranged for after two months.
Figure 3.
Selected image of a follow-up left CAG in cranial view showing that most of the LAD thrombus was resolved.
Discussion
SARS-CoV-2, which causes COVID-19, usually presents with fever and respiratory symptoms. However, it may present with unusual or atypical clinical features that are not related to the respiratory system and may mislead from a COVID-19 diagnosis. In this case report and brief review, we focused on the unusual and atypical clinical presentations of COVID-19. In the literature, we found cases reported with unusual or atypical presentations, like leg pain or swelling with venous thrombosis,6, 7, 8 loss of consciousness with cerebral venous sinus thrombosis,9 confusion,10 acute conjunctivitis,11,12 left facial drop and arm weakness with brain infarction,13 facial neuralgia with herpes zoster,14 right iliac fossa pain like appendicitis,15 and abdominal pain accompanied by testicular pain16 (Table 1).
Table 1.
The literature review includes case reports of COVID-19 with atypical and unusual presentations reported in medical journals indexed in PubMed during the period of the pandemic from January 2020 to August 2020.
| Author(s) | Age | Gender | Presentation | Medical imaging findings | RT-PCR |
|---|---|---|---|---|---|
| Kaur et al.6 | 43-y-o | Male | Acute right leg pain with shortness of breath and fever for a week | CXR→ bilateral hazy infiltrates CTA→ Thrombus in right proximal superficial femoral artery |
+ve |
| Davoodi et al.7 | 57-y-o | Female | Painful swelling and redness of left leg | CXR→ bilateral patch GGO CTA→ unremarkable Doppler→ left lower limb DVT |
+ve |
| Visveswaran et al.8 | 12-y-o | Female | Painful swelling of left leg evaluated before 5 days for erythema and diagnosed as cellulitis | Venography→ extensive popliteal to common iliac vein thrombosis | +ve SARS-COV-2 IgM -ve SARS-COV-2 IgG |
| Hemasian et al.9 | 62-y-o | Male | Loss of consciousness | Brain CT & MRI→ haemorrhagic infarction Brain MRV→ sinus thrombosis in right transverse & sigmoid Chest CT → GGO |
+ve |
| Alkeridy et al.10 | 73-y-o | Male | Acute confusion | Brain CT→ unremarkable Brain CTA→ unremarkable CXR → diffuse bilateral lung interstitial infiltrates |
+ve |
| Ozturker et al.11 | 32-y-o | Male | Eye redness, stinging, watery discharge, and photophobia | CXR→ unremarkable Chest CT→ unremarkable |
+ve |
| Sirakaya et al.12 | 40-y-o | Male | Bilateral acute conjunctivitis | NA | +ve |
| Doo et al.13 | 55-y-o | Male | Left wrist droop, left facial droop, and left arm weakness | CTA of the head and neck→ large thrombus in the right CCA and acute right frontal infarction (PRES-like) | +ve |
| de Freitas et al.14 | 39-y-o | Male | Left hemi facial herpes zoster with sharp pain preceded by fatigue, diarrhoea, and fever | NA | +ve |
| Abdalhadi et al.15 | 40-y-o | Female | Right iliac fossa pain, nausea, vomiting, fever, and loss of appetite for 3 days | CT → normal appendix with patchy consolidation and GGO in bilateral peripheral basal of lungs | +ve |
| Kim et al.16 | 42-y-o | Male | Abdominal, testicular, and back pain for 8 days | CXR→ unremarkable Abdominal CT → GGO and consolidation in lung bases |
NA |
COVID-19: Coronavirus disease 2019, SARS-COV-2: severe acute respiratory syndrome coronavirus-2, RT-PCR: reverse transcriptase-polymerase chain reaction, CXR: chest x-ray, CT: computed tomography, CTA: CT angiography, GGO: ground-glass opacity, DVT: deep venous thrombosis, NA: not available, -ve: negative, +ve: positive, y: year, o: old.
In this paper, we reported a case of COVID-19 that was diagnosed early with mild respiratory symptoms and then complicated with coronary thrombosis and typical myocardial infarction features. A similar case of STEMI with coronary thrombosis was reported by Shams et al. and successfully managed with PPCI.17 Salido-Tahoces et al. reported another positive case of COVID-19 in a 62-year-old male who presented with asthenia and recurrent chest pain with ACS and proximal RCA stenosis and whose diagnosis was confirmed by CAG.18 Similarly, Tedeschi et al. reported acute STEMI with a large coronary thrombosis in a 60-year-old man; they explained this by pointing to the presence of high levels of post inflammatory mediators in patients with COVID-19.19 In addition, Harari et al. reported acute myocardial infarction (AMI) with extensive coronary thrombosis in a 40-year-old female.20 SARS-CoV-2 infections can cause harmful myocardial complications that include myocardial injury, arrhythmia, myocarditis, cardiomyopathy, arterial and venous thrombosis, cardiogenic shock, and even cardiac arrest.21 AMI's pathogenesis is complex, still incompletely understood, and sometimes explained by the uncontrolled release of post-inflammatory cytokines (cytokine storm) and the direct damage of cardiac myocytes due to hypoxemia or the virus itself.20, 21, 22 Ultimately, severe acute viral infection itself can promote the formation of ACS by increasing the risk of plaque rupture and micro-thrombi, owing to systemic inflammation or a cytokine storm, or by causing hypoxemia and coronary spasm, leading to a decreased oxygen supply to the myocardium.20,21,23,24
Conclusion
COVID-19 patients can present to emergency departments with vascular complications like acute coronary syndrome, as in the current case report. Other unusual and atypical presentations that have been reported include leg pain or swelling with venous thrombosis, loss of consciousness with cerebral venous thrombosis, confusion, acute conjunctivitis, limb weakness with infarction, facial neuralgia, right iliac fossa mimicking appendicitis, or testicular pain. Emergency physicians should be alert to the unusual presentations of COVID-19 during the pandemic.
Source of funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The patient has given informed consent allowing the authors to publish his case and images.
Authors contributions
SAA wrote the initial and final draft of the article. KHH collected and organised data. MAM provided research materials. AMH analysed and interpreted data. TSD provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Nabil A., Uto K., Elshemy M.M., Soliman R., Hassan A.A., Ebara M. Current coronavirus (SARS-CoV-2) epidemiological, diagnostic and therapeutic approaches: an updated review until June 2020. EXCLI J. 2020;19:992–1016. doi: 10.17179/excli2020-2554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [published correction appears in Lancet. 2020 Jan 30;:] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adil M.T., Rahman R., Whitelaw D., Jain V., Al-Taan O., Rashid F. SARS-CoV-2 and the pandemic of COVID-19. Postgrad Med. 2020 doi: 10.1136/postgradmedj-2020-138386. [published online ahead of print, 2020 Aug 11] postgradmedj-2020-138386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abobaker A., Raba A.A., Alzwi A. Extrapulmonary and atypical clinical presentations of COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.26157. [published online ahead of print, 2020 Jun 10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta A., Madhavan M.V., Sehgal K., Nair N., Mahajan S., Sehrawat T.S. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaur P., Posimreddy S., Singh B., Qaqa F., Habib H.A., Maroules M. COVID-19 presenting as acute limb ischaemia. Eur J Case Rep Intern Med. 2020;7(6) doi: 10.12890/2020_001724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davoodi L., Jafarpour H., Taghavi M., Razavi A. COVID-19 presented with deep vein thrombosis: an unusual presenting. J Investig Med High Impact Case Rep. 2020;8 doi: 10.1177/2324709620931239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Visveswaran G.K., Morparia K., Narang S., Sturt C., Divita M., Voigt B. SARS-CoV-2 infection and thrombosis: phlegmasia cerulea dolens presenting with venous gangrene in a child. J Pediatr. 2020;(20):30875–30881. doi: 10.1016/j.jpeds.2020.07.032. [published online ahead of print, 2020 Jul 13] S0022-3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hemasian H., Ansari B. First case of Covid-19 presented with cerebral venous thrombosis: a rare and dreaded case. Rev Neurol (Paris) 2020;176(6):521–523. doi: 10.1016/j.neurol.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alkeridy W.A., Almaghlouth I., Alrashed R., Alayed K., Binkhamis K., Alsharidi A. A unique presentation of delirium in a patient with otherwise asymptomatic COVID-19. J Am Geriatr Soc. 2020;68(7):1382–1384. doi: 10.1111/jgs.16536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ozturker Z.K. Conjunctivitis as sole symptom of COVID-19: a case report and review of literature. Eur J Ophthalmol. 2020 doi: 10.1177/1120672120946287. [published online ahead of print, 2020 Jul 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sirakaya E., Sahiner M., Sirakaya H.A. A patient with bilateral conjunctivitis positive for SARS-CoV-2 RNA in conjunctival sample. Cornea. 2020 doi: 10.1097/ICO.0000000000002485. [published online ahead of print, 2020 Jul 2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doo F.X., Kassim G., Lefton D.R., Patterson S., Pham H., Belani P. Rare presentations of COVID-19: PRES-like leukoencephalopathy and carotid thrombosis. Clin Imag. 2020;69:94–101. doi: 10.1016/j.clinimag.2020.07.007. [published online ahead of print, 2020 Jul 16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Freitas Ferreira A.C.A., Romão T.T., SIlva Macedo Y., Pupe C., Nascimento O.J. COVID-19 and herpes zoster co-infection presenting with trigeminal neuropathy. Eur J Neurol. 2020 doi: 10.1111/ene.14361. [published online ahead of print, 2020 May 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdalhadi A., Alkhatib M., Mismar A.Y., Awouda W., Albarqouni L. Can COVID 19 present like appendicitis? IDCases. 2020;21 doi: 10.1016/j.idcr.2020.e00860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim J., Thomsen T., Sell N., Goldsmith A.J. Abdominal and testicular pain: an atypical presentation of COVID-19. Am J Emerg Med. 2020;38(7):1542.e1. doi: 10.1016/j.ajem.2020.03.052. 1541542.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shams A., Ata F., Mushtaq K., Munir W., Yousaf Z. Coronary thrombosis in a young male with COVID-19. IDCases. 2020;21 doi: 10.1016/j.idcr.2020.e00923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salido-Tahoces L., Sánchez-Recalde A., Pardo-Sanz A., Zamorano Gómez J.L. Unusual presentation of acute coronary syndrome in a patient with SARS-CoV-2 infection. Eur Heart J Cardiovasc Imaging. 2020 doi: 10.1093/ehjci/jeaa147. [published online ahead of print, 2020 May 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tedeschi D., Rizzi A., Biscaglia S., Tumscitz C. Acute myocardial infarction and large coronary thrombosis in a patient with COVID-19. Cathet Cardiovasc Interv. 2020 doi: 10.1002/ccd.29179. [published online ahead of print, 2020 Aug 7] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harari R., Bangalore S., Chang E., Shah B. COVID-19 complicated by acute myocardial infarction with extensive thrombus burden and cardiogenic shock. Cathet Cardiovasc Interv. 2020 doi: 10.1002/ccd.28992. [published online ahead of print, 2020 May 19] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang W., Zhao Y., Zhang F., Wang Q., Li T., Liu Z. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the Perspectives of clinical immunologists from China. Clin Immunol. 2020;214:108393. doi: 10.1016/j.clim.2020.108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corrales-Medina V.F., Madjid M., Musher D.M. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10(2):83–92. doi: 10.1016/S1473-3099(09)70331-7. [DOI] [PubMed] [Google Scholar]
- 23.Revzin M.V., Raza S., Srivastava N.C., Warshawsky R., D'Agostino C., Malhotra A. Multisystem imaging manifestations of COVID-19, Part 2: from cardiac complications to pediatric manifestations. Radiographics. 2020;40(7):1866–1892. doi: 10.1148/rg.2020200195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nishiga M., Wang D.W., Han Y., Lewis D.B., Wu J.C. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17(9):543–558. doi: 10.1038/s41569-020-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]