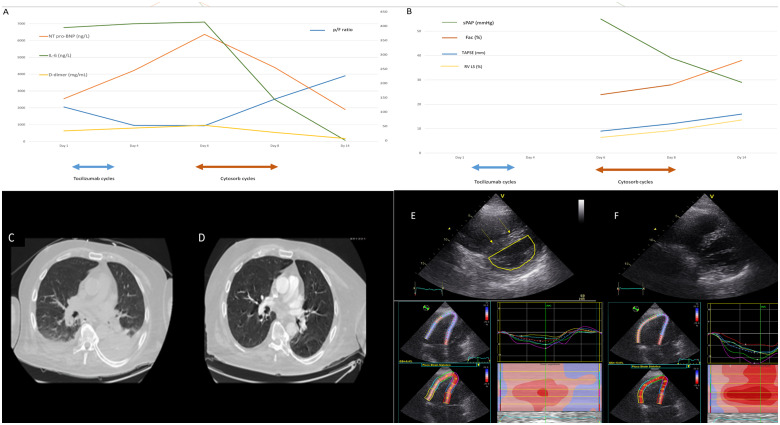
A 75-year-old man was admitted for COVID-19-related respiratory failure (p/F ratio 205 on Day 1). He was treated with intravenous dexamethasone (6 mg per day), enoxaparin (4000 international units once daily), and non-invasive ventilation. Levels of cardiac damage and inflammatory biomarkers, including high-sensitivity troponin T (25 pg/mL, normal values 0–14 pg/mL), N-terminal pro-brain natriuretic peptide (2546 ng/L, normal values 0–125 ng/L), D-dimer (633 ng/mL, normal values 0–500 ng/mL), and interleukin-6 (6768 ng/L, normal values 0–7 ng/L), were significantly elevated (Supplementary material online and Panel A). On Days 2 and 3 from admission, the patient received two cycles of tocilizumab therapy (two intravenous bolus of 400 mg over 2 days) but during the following 72 h his clinical conditions deteriorated due to severe respiratory failure with severe hypoxaemia (p/F ratio 95), hypotension, and hypoperfusion. He was intubated and transferred to COVID-19 intensive care. Contrast-enhanced chest computed tomography (CT) showed bilateral ground-glass lesions, subpleural consolidations, pleural effusions, and subsegmental pulmonary embolism (Panel C). Echocardiography showed normal left ventricular function but signs of acute cor pulmonale with reduced tricuspid annular systolic excursion plane, fractional area change, and right ventricular (RV) longitudinal strain with increased systolic pulmonary artery pressure (Panels B and E). Despite treatment with high-dose vasoactive drugs, unfractionated heparins and antibiotics, he developed refractory shock with anuria. Due to the presence of persisting anuria with hyperkaliaemia (6.0 mmol/L), we started continuous renal replacement therapy (CRRT) and immunoadsorption with Cytosorb™ (Cytosorbents Corporation, NJ, USA) system. After 72 h, we observed a significant haemodynamic improvement together with an important decline of inflammatory and cardiac damage markers levels (Supplementary material online, Panel A) and, due to the presence of spontaneous diuresis with negative fluid balance, we stopped CRRT and immunoadsorption therapy. Control chest CT showed significant reduction of consolidations, pleural effusions and ground-glass lesions (Panel D), while echocardiography documented significant improvement of RV function (Panels B and F). The patient was extubated 3 days later and on Day 14 (p/F ratio 390) transferred to a respiratory rehabilitation centre with stable haemodynamics and no need for CRRT. After 6 months, the patient has completely recovered, with normal RV function.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: None declared.
Funding: None declared.
Ethic independent committee approval: We obtained the approval of our ethic independent committee for this manuscript.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.