Abstract
Background
Dyspepsia (Amlapitta) is the commonest ailment found in the present time. Nowadays due to unawareness about Prakriti (psychosomatic constitution) people are practising inappropriate diet and lifestyle which leads to disturbances in digestive system. Due to this pitta is imbalanced and common consequences are Amlapitta. If this pitta takes an upward course, then it is called Urdhwaga Amlapitta.
Objective
This study was conducted to assess the effectiveness of Ayurveda treatment for UrdhwagaAmlapitta in terms of improvement in symptoms, cure rate, satisfaction and side effects if any.
Material and methods
This was a single-arm exploratory open-label clinical trial. Patient with symptom of Urdhwaga Amlapitta were diagnosed as per Rome IV criteria and were further assessed as per eligibility criteria. Thirty patients were enrolled. They were given different herbo-mineral preparation as per ones Prakriti. These drugs were given for 28 days and patients were followed weekly in OPD for assessment of their symptom severity scores.
Result
Tiktamlodgar (acid eructation) and Gurukoshthatva (heaviness in abdomen) was the most commonly occurring symptom in 93% (n = 28) of participants. Seventy Percent (n = 21) of participants had Avipak severity of grade 2 or 3 followed by Gaurav in 50%. The patient was symptomatically relieved by all the symptoms of Urdhwaga Amlapitta by 3rd visit (21st day) and the difference in score was statistically significant. All participants express willingness take Ayurveda medicine in future.
Conclusion
Combination of Ayurveda drugs as per ones Prakriti and severity of symptoms, given to the patient of Urdhwaga Amlapitta was found to effectively cure patients within 28 days. These drugs were found to be well-tolerated, safe and acceptable.
Keywords: Amlapitta, Ayurveda, Clinical trial, Dyspepsia, Prakriti
1. Introduction
In Ayurveda, it is believed that Agnimandya (indigestion) is the root cause of all the diseases [1]. The major reason behind Agnimandya is faulty dietary habits such as Adhyashana (eating after meal), Vishamashana (diet on irregular time and quantity), and wrong behavioural patterns such as Vegadharana (suppression of urges) leads to vitiation of Doshas (fundamental bodily bio-elements) either independently or synonymously. Due to the present lifestyle and unawareness of ones Prakriti, digestive disorders are very common in all age groups and also highly ignored issues.
Dyspepsia is one of the commonly accruing disorder, the majority of them remain uninvestigated. American Society of Gastrointestinal society recommended the use of endoscopy only in the presence of alarm features [2]. It is advocated to evaluate the patient with noninvasive testing for Helicobacter pylori, with subsequent treatment if positive (the “test and treat” approach) and empiric trial of acid suppression [3]. Systematic review in year 2008 had confirmed, between two strategies of “test and treat” approach and empirical Proton pump inhibitors (PPI), there is no difference in symptom resolution and treatment cost. Such cases with new or recurrent dyspeptic symptoms in whom no investigations have previously been undertaken are referred to as Uninvestigated dyspepsia [4]. Long term use of antacids and acid-suppressing medicines leads to adverse effects like hypersensitivity, alkalosis, calculi, constipation, etc. [5,6] In Ayurveda, pitta is of two types as Adhoga and Urdhwaga Amlapitta. If this pitta takes an upward course i. e vomiting, burning sensation, headache, loss of appetite, then it is called Urdhwaga Amlapitta.
Urdhwaga Amlapitta includes different symptoms like Aruchi (anorexia), Gurukoshthatva (heaviness in abdomen), Gaurav (Lethargy), Vibandh (Constipation), Shiroruja (Headache), Utklesh (Nausea), Tiktamlodgar (acid eructation) [7,8]. Urdhwaga Amlapitta is mainly caused by intake of Aharas which is not suited to ones Prakriti i.e faulty diet e.g Amla (sour), Katu (pungent), Lavana (salty), Guru (heavy meal), Snigdha (oily/excessive liquid), Abhishandhi (food that is difficult to digest) aharas [9]. Besides, addictions like smoking, alcohol, tobacco chewing, excessive stress, condiments also lead to Urdhwaga Amlapitta. Drugs like NSAID's, corticosteroids, also cause dyspepsia. Ayurveda physicians are treating dyspepsia since long time with the help of knowledge as given in classical Ayurveda text (causative factors, pathogenesis, treatment plan, and preventive tool) but there is a lack of evidence as per modern standards.
The world is recognizing the importance of system biology and moving towards a holistic approach. There is a need to create evidence to develop universal acceptance of this ancient science for the betterment of quality of life. Randomized control trial is not ethically permissible unless documented scientific evidence of efficacy and safety of Ayurveda drug used for Urdhwaga amlapitta is documented [10]. To best of our knowledge, we could not find an interventional study on effect of combination of oral Ayurveda drugs for Urdhwaga Amlapitta. Therefore, this pilot study was conducted with an objective to assess the effectiveness of Ayurveda treatment for Urdhwaga Amlapitta in terms of cure rate, improvement in symptoms, satisfaction of participants and side effects if any.
2. Methodology
A single-arm exploratory open-label clinical trial of Ayurveda treatment among patients of Urdhwaga Amlapitta (un-investigated dyspepsia) was planned.
Sample size: According to the central limit theorem and Browne's (1995) estimate of sample size for the pilot study, a sample size of 30 was considered [11,12].
2.1. Recruitment of patient and data collection
Patients attending the O·P.D. of Ayurveda with symptoms of Urdhwaga Amlapitta, as first assessed by Rome IV diagnostic criteria [13] by the first author. These patients were not investigated further and therefore are referred to as uninvestigated dyspepsia. Patients fulfilling the eligibility criteria were selected for the present study.
2.1.1. Inclusion criteria
Patients fulfilling the above diagnostic criteria were included in the study. Their age should be in the range of 20–60 yrs. The included those participants, willing to take up Ayurveda Treatment.
2.1.2. Exclusion criteria
Already diagnosed patient of chronic diseases (cardiovascular diseases, cancer, chronic respiratory diseases, diabetes, chronic orthopedic conditions) with early or late complication. Patient with the known organic cause of dyspepsia i.e gastric/duodenal ulcer. Patient on long term use of analgesic (atleast for 3 months). Patient with past history of Gastrointestinal (GI) surgery. Patient not suitable/contraindicated for therapy as assessed by the physician. Pregnant/lactating mothers. Patient with alarm features [3] as Family history of upper GI malignancy in a first-degree relative, Unintended weight loss more than 5% of normal body weight over last 6–12 months, Occult (elicited by past history) or overt GI bleeding (recent history of past 15 days to one month) or iron deficiency anemia, Dysphagia, Odynophagia, Persistent vomiting –considered when there was more than 3 episodes of vomiting in 24 h in past 15 days to one month
An elaborative case taking proforma (Annexure 1) was designed for taking a history of dosha involvement and assessing the Nidan (causative factor). The patient was recruited after taking the written informed consent.
2.1.3. Intervention
Different herbo-mineral preparations given in the text of Ayurveda (Rastantra sar and Sidhaprayogasangrah Part −1) which works in Annavah Strotas (gastrointestinal system) were used. Name of preparations which we used in varying ratio in depending on Prakriti (Annexure 2), severity of symptom and weight of patient is Kamdudha ras 125 mg–375 mg bd [14]. Giloy satva 125 mg–500 mg bd [15]. Shankh bhasm 125 mg–500 mg bd [16]. Avipattikar churn 1–6 gm bd [17]. Chitrakadi vati 2–4 tablets bd [18].
2.2. Rationale of treatment
To determine the dosage and treatment, we did Prakruti assessment and pareekshan at the baseline including specific symptoms of Aruchi, Gaurav, and Vibandha, that indicates Aama conditions.
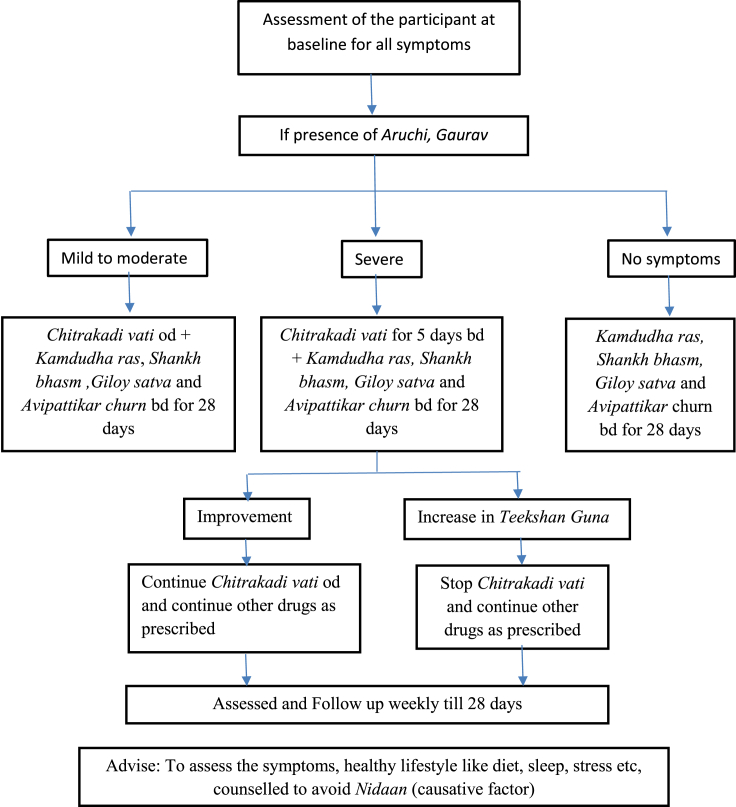
If Aruchi and Gaurav were severe then we started Chitrakadi vati for initial 5 days in kapha kala [16] with food in the morning and evening, so that the digestion of Aama starts without increasing the teekshan guna of pitta. We advised the patient to stop Chitrakadi vati if someone feel increase in symptoms like Amlodgar and Shirahshool which may be due to increase in teekshan guna of pitta. If the patient had improvement in hunger, lightness in body then we advised him/her to take Chitrakadi vati only in the morning at kapha kala with food. After one hour of food in pitta kala patient was advised to take pre mixed packet containing calculated dosage of Kamdudha ras, Shankh bhasm, Giloy satva and Avipattikar churn twice a day as given in Fig. 1.
Fig. 1.
Flow chart of treatment of patient.
Details of dosage and regimen for other conditions is given in Table 1. Duration of treatment was for 4 weeks. Except for reducing the frequency of Chitrakadi Vati to once a day after 5 days in case of severe Aruchi and Gaurav symptom, no other changes were made in dosage of other four drugs as calculated at baseline after adjusting for underweight or overweight.
Table 1.
Dosage of drug preparations for different condition as per Prakriti
| Condition | Dosage |
|---|---|
| Severe Aruchi and Gaurav | For initial 5 days: Chitrakadi vati 2 tabs in the morning and evening; Avipattikar churn 3 gm; Kamdudha ras 250 mg; Shankh bhasm −350 mg; and Giloy satva – 500 mg. Later till 28 days: Chitrakadi vati 2 tabs in the morning; continue other medicines as advised earlier |
| Mild to moderate Aruchi and Gaurav | Avipattikar churn 3 gm; Kamdudha ras 250 mg; Shankh bhasm 250 mg; Giloy satva 500 mg and Chitrakadi vati od X 28 days |
| Moderate to severe Vibandha | Avipattikar churn 4 gm; Kamdudha ras 250 mg; Shankh bhasm 125 mg; Giloy satva 500 mg and Chitrakadi vati od X 28 days |
| Pitta symptoms like (Amlodgar; Shirahshool) | Avipattikar churn 3 gm; Kamdudha ras 350 mg; Shankh bhasm 250 mg; Giloy satva 500 mg and Chitrakadi vati od. X 28 days |
| Not reported Aruchi; Gaurav or Vibandha | Avipattikar churn 3 gm; Kamdudha ras 250 mg; Shankh bhasm 250 mg and Giloy satva 500 mg ∗ X 28 days |
∗No Chitrakadi vati
2.3. Clinical assessment
According to Classical text Samhita and experience of symptoms of Urdhwaga Amlapitta in Ayurveda OPD below symptoms were chosen for weekly clinical assessment. These were Aruchi (anorexia), Gurukoshthatva (heaviness in abdomen), Gaurav (lethargy), Vibandh (Constipation), Shiroruja (Headache), Utklesh (Nausea), Tiktamlodgar (Acid eructation), Klama (exhaustion) and Hrid- Kanta Daha (heartburn). We could not find exact synonyms of Ayurveda symptoms in modern medicine, however tried to be as accurate as possible. Five experts including three of Ayurveda and two from Allopathy were invited for process of content validation of items as given by Davis [19]. Item-level Content validity index for all items except Klama and Hrid- Kanta Daha was above 0.8. Klama was reported to be non-specific and Hrid kanta daha was also related to Gastrooesophageal reflux disorder. These two items were later deleted. Graded Score was assigned after discussion with all experts (Table 2).
Table 2.
Clinical symptom assessment scoring for the patient of Urdhwaga amlapitta.
| Grading score | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Avipaka (indigestion) | No indigestion | Indigestion on only by heavy food. | Delayed digestion of lighter food | Impaired indigestion of even lighter food |
| Gaurav (lethargy) | No lethargy | Occasional but can do daily work | Continuous tiredness that hampers daily work | Due to tiredness avoid any routine work |
| Utklesha (nausea) | No salivation | Occasional but not daily | Daily and after taking solid food for sometime | Frequently and feel Amlata |
| Tikta Amla Udgara (acid eruption. belching) | No Tikta | Appears 1–5 times/day only on consumption of sour and spicy food | Appears 6–10 times/day on the consumption of any type of food | Appears 10 times/day on the consumption of any type of food |
| Gurukoshthatwa (heaviness in abdomen) | Nogurukoshthtwa | Occasional with a normal quantity of food | Continuous while taking normal food with an average quantity | Continuous while taking less food |
| Aruchi (anorexia) | No Aruchi | Patient feels aruchi but takes food time to time | Patient sometimes takes food and sometimes avoid it | Patient avoids the food many times |
| Vibandh (constipation) | No Vibandh | Intermittent relieved by pathya ahar vihar | Continuous relieved by mild laxative (Mrudu Virechan) | Continuous only relieved by strong medication (Teekshan virechan) |
| Shirorujah (Headache) | No headache | Intermittent reliever by pathya | Continuous not relieved by medicine | Continuous only relieved by medicine |
Patients were scored on this scoring criteria weekly by independent outcome assessors (Ayurveda Practioners) who were blinded to duration of undergoing treatment to prevent investigator bias.
2.3.1. Follow-up
Follow-up of the patient was taken up weekly until 4 weeks. If any patient missed any follow-up in OPD, then follow-up finding was recorded by phone. Patients were also assessed for any difficulty faced while following the advice, compliance to diet, treatment, lifestyle and any side effects experienced due to medicine.
2.3.2. Confidentiality
Although the data was taken by the name later it was coded by the investigator. To maintain confidentiality all data was kept in a locked cupboard.
The study was approved by Institutional Ethics committee approval was taken Study protocol no is −151/IEC/IM/NF/2017, Reg.no: ECR/736/Inst/UK/2015.
2.3.3. Data analysis
Data was entered in MS excel 2010 and analysed using IBM SPSS statistics version 24. Discreet data was presented in proportion. Friedman test (non-parametric) was used to test, significance in decline in clinical symptom severity score from first to the last visit.
3. Results
Out of 30 study participants, half of them were male (50%) and female respectively. Nineteen (63%) were in the age group of 20–40 years and rest fall under 40–60 years with an almost equal proportion of males and females in each group. Most of the participants were of having pitta (n = 21) followed by kaphaprakriti (n = 9). Although most of the symptoms were present in participants, Shiroruja and Tiktamlodgar were more severe symptom in pitta type of prakriti while Gaurav, Aruchi and Gurukoshthtwa were common and severe in kapha prominent prakriti. Table 3 shows the distribution of study participants according to clinical assessment severity score at first visit. Tiktamlodgar (acid eructation) and Gurukoshthatva (heaviness in abdomen) were the most commonly occurring symptom in 93% (n = 28) of participants. Seventy percent (n = 21) of participants fall under grade 2 and 3 scoring of Avipak (indigestion) followed by 50% (n = 15) with Gurukoshthatva (heaviness in abdomen) and 40% (n = 12) with Tiktamlodgar (acid eructation). Table 4 shows variation in clinical assessment score from 1st visit (Initial visit) to 4th visit (last visit) in study participants receiving Ayurveda treatment for Urdhwaga Amlapitta. The patient was symptomatically relieved by all the symptoms of Urdhwaga Amlapitta by third visit (21st day). There was a statistically significant decline in clinical assessment score of symptoms in all visits. Post hoc analysis with Wilcoxon signed-rank tests with a Bonferroni correction applied also shows statistically significant reduction in clinical assessment score of all symptoms from first to second visit and further to fourth (last) visit. During treatment, Kapha Prakriti participant started getting relief in their symptoms soon after the aama pachan but pitta type of participant only began to get relief in symptoms when complete herbomineral combination was introduced.
Table 3.
Distribution of study participants receiving Ayurveda treatment for Urdhwaga Amlapitta according to clinical assessment severity score at first visit.
| Symptoms | Grade 0 n (%) | Grade 1 n (%) | Grade 2 n (%) | Grade 3 n (%) | Total n (%) |
|---|---|---|---|---|---|
| Avipak (Indigestion) | 3 (10) | 6 (20) | 16 (53.3) | 5 (16.7) | 30 (100) |
| Gaurav (Lethargy) | 3 (10) | 10 (33.3) | 12 (40) | 5 (16.7) | 30 (100) |
| Utklesh (Nausea) | 7 (23.3) | 14 (46.7) | 6 (20) | 3 (10) | 30 (100) |
| Tiktamlodgar (Acid eructation) | 2 (6.7) | 16 (53.3) | 7 (23.3) | 5 (16.7) | 30 (100) |
| Gurukoshthatva (Heaviness in abdomen) | 2 (6.7) | 13 (43.4) | 8 (26.7) | 7 (23.3) | 30 (100) |
| Aruchi (Anoraxia) | 10 (33.3) | 14 (46.7) | 5 (16.7) | 1 (3.3) | 30 (100) |
| Vibandh (Constipation) | 6 (20) | 12 (40) | 8 (26.7) | 4 (13.3) | 30 (100) |
| Shiroruja (Headache) | 6 (20) | 15 (50) | 5 (16.7) | 4 (13.3) | 30 (100) |
Table 4.
Change in Clinical assessment Score from 1st visit (Initial visit) to 4th visit (28 days) in study participants receiving Ayurveda treatment for Urdhwaga Amlapitta (n = 29).
| Time of visit | Mean ± SD | Median (IQR) | Friedman test (P-value) | |
|---|---|---|---|---|
| Avipak (Indigestion) | 1st visit | 1.76 ± 0.85 | 2 (2–2) | 70.7 (0.000)a |
| 2nd visit | 1 ± 0.8 | 1 (1–2) | ||
| 3rd visit | 0.46 ± 0.57 | 0 (0–1) | ||
| 4th visit | 0.03 ± 0.18 | 0 (0–0) | ||
| Gaurav(Lethargy) | 1st visit | 1.6 ± 0.9 | 2 (1–2) | 67.9 (0.000)a |
| 2nd visit | 0.8 ± 0.6 | 1 (0–1) | ||
| 3rd visit | 0.2 ± 0.4 | 0 (0–0) | ||
| 4th visit | 0.1 ± 0.3 | 0 (0–0) | ||
| Utklesh(Nausea) | 1st visit | 1.1 ± 0.9 | 1 (0.75–2) | 59.1 (0.000)a |
| 2nd visit | 0.5 ± 0.7 | 0 (0–1) | ||
| 3rd visit | 0.0 ± 0.0 | 0 (0–0) | ||
| 4th visit | 0.0 ± 0.0 | 0 (0–0) | ||
| Tiktamlodgar(Acid eructaion) | 1st visit | 1.5 ± 0.9 | 1 (1–2) | 71.4 (0.000)a |
| 2nd visit | 0.6 ± 0.7 | 0.5 (0–1) | ||
| 3rd visit | 0.06 ± 0.2 | 0 (0–0) | ||
| 4th visit | 0.00 | 0 (0–0) | ||
| Gurukoshthatva(Heaviness in abdomen) | 1st visit | 1.7 ± 0.9 | 1.5 (1–2.25) | 68.7 (0.000)a |
| 2nd visit | 0.7 ± 0.7 | 1 (0–1) | ||
| 3rd visit | 0.2 ± 0.4 | 0 (0–0) | ||
| 4th visit | 0.06 ± 0.2 | 0 (0–0) | ||
| Aruchi(Anoraxia) | 1st visit | 0.9 ± 0.8 | 1 (0–1) | 49.8 (0.000)a |
| 2nd visit | 0.3 ± 0.5 | 0 (0–1) | ||
| 3rd visit | 0.03 ± 0.2 | 0 (0–0) | ||
| 4th visit | 0.000 | 0 (0–0) | ||
| Vibandh(Constipation) | 1st visit | 1.3 ± 0.9 | 1 (1–2) | 60.2 (0.000)a |
| 2nd visit | 0.8 ± 0.7 | 1 (0–1) | ||
| 3rd visit | 0.3 ± 0.4 | 0 (0–1) | ||
| 4th visit | 0.1 ± 0.3 | 0 (0–0) | ||
| Shiroruja (Headache) | 1st visit | 1.2 ± 0.9 | 1 (1–2) | 50.3 (0.000)a |
| 2nd visit | 0.8 ± 1.9 | 0 (0–1) | ||
| 3rd visit | 0.1 ± 0.3 | 0 (0–0) | ||
| 4th visit | 0.2 ± 0.5 | 0 (0–0) |
Statistically significant.
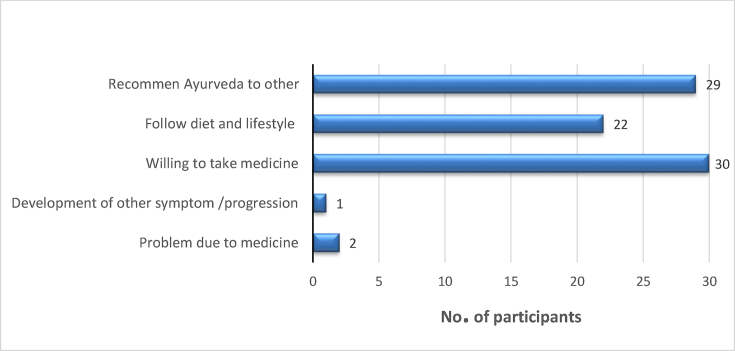
Twenty-five (83.3%) participants had taken allopathy treatment for Urdhwaga Amlapitta in past. According to Fig. 2, all of the study participants were willing to take Ayurveda medicine for other conditions in future while 29 (97%) said they will recommend it to others. Twenty-two participants (73%) followed lifestyle as suggested for treatment. Two participants had minor problems with the treatment protocol and one had progression in severity of symptom score after treatment. The cure rate was 96.6% (29/30).
Fig. 2.
Experience and Attitude of study participants after taking Ayurvedic treatment for Urdhwaga Amlapitta.
4. Discussion
There was a significant reduction in the Urdhwaga Amlapitta symptom score compared to the first visit. Relief from symptoms was reported by patient from the second visit (7 days) onwards. All participants were satisfied with effect of Ayurveda treatment for Urdhwaga Amlapitta. Only one participant had progression of symptom, the cause of which could not be established. None of the participant experienced a side effect of Ayurveda. The strength of the study is treatment by oral intake which is the most acceptable form of therapy for Urdhwaga Amlapitta. In Ayurveda, there are mainly two type of treatment is described Davvypashray and Yuktiyvapashray, here we used only shaman chikitsa (drug therapy) that comes under Yuktiyvapashray [20]. This is one kind of study that had taken ones Prakriti into account for decision on drug therapy as mentioned in classical Ayurveda text. In this study combination of different drugs that acts on digesting system having the properties to relieve symptoms and cure disease as per knowledge of classical text is utilized. The quality of drugs is assured as per the standards of Ayurvedic Formulary of India [21]. All the Medicines used in this study were Pitta Shamak which pacifies the Pitta Dosha, and Kapha balancing, drugs which work on whole digestive track and smoothen the activity of every part of digestive system like Avipaattikar churn.
Studies in the past had proven the effectiveness of Avipattikar churn in Amla pitta. It is acid neutralizer, mild laxative and also increases digestive fires [22]. Shankh Bhasma is calcium carbonate which has acid-neutralizing property in tablet format as assessed by Rosette Rice test [23]. Chitrakadi Vati also called Chitrakadi Gutika helps to digest undigested food particles and removes accumulated toxin due to malabsorption of food particles further improving digestion and metabolism of body which is the main cause of several diseases [24]. Kamdudha Ras has cooling potency, reduces heat in the body and alleviates sensation of burning. It is considered a potent antacid [24,25]. Giloy Satva is anti-microbial, anti-depressant, immunomodulatory and antioxidant [26]. However, we could not find studies on the varying combination of above drug therapies for treatment of Urdhwaga Amlapitta.
One patient had an increase in the severity of symptom (pitta prakritti) and was shifted to allopathy drugs after two weeks. This may be due to underlying pathology of dyspepsia which was not stringently ruled out by gastro-endoscopy before start of therapy. This was one of the limitations of the study. It may be recommended for further studies to rule out organic causes of dyspepsia or at least H pylori infection using Urease Breathe test. However, it should also be noted that endoscopy is not justifiable unless there is alarming symptoms. Therefore, the balance of cost-risk ratio has to be maintained. Being a pilot study, small sample size was the second limitation. Due to ethical concern, we restricted to single-arm study, no randomization. We performed only content validation of the clinical assessment scale, other psychometric properties need to be explored further. This study can be used to calculate the sample size and evidence of efficacy and safety to further conduct a randomized trial with allopathy regimen (PPI). Dyspepsia is subjective symptoms and can be confounded by physical, mental, emotional health of the patient or environmental factors. We tried to reduce the investigator bias by randomly assigning the outcome assessor and blinding to time of visit. Due to time and financial constraints, we could not follow up patients after 28 days for recurrence of their symptoms.
5. Conclusion
The study concludes that all the above combination of Ayurveda drugs given to the patient of Urdhwaga Amlapitta in appropriate combination and formulations as per classical Ayurveda text can symptomatically cure patients within 28 days with cure rate of 96%. These combination drugs were also found to be safe, well-tolerated and acceptable to the patient.
Source(s) of funding
None.
Conflict of interest
None.
Acknowledgment
We acknowledge all the participants who followed up for a period of one month. We are thankful to Dr Ravikant, Additional Professor, Dept of Medicine, for being the expert in content validation of symptom severity score and guiding us for diagnosis and management of patient with dyspepsia on Ayurveda treatment if and when needed. We are also thankful to Dr Meenaxi Jagzape, Senior Medical officer (Ayurveda) Dept of Ayush and Dr Mayank Bhatkoti (Associate Professor Dept. of Panchkarma, Gurukul campus Haridwar) for being one of the expert in content validation. We also acknowledge help given by outcome assessors. Sources of support in the form of infrastructure and space: Supported by All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2020.12.004.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Paradakara Shastri H.S., editor. Astanga hridaya of vagbhaṭa, nidana sthana. Ch. 12. Ver. 1. Chaukhambha Surabharati Prakashan; Varanasi: 2010. (Reprint ed) [Google Scholar]
- 2.Moayyedi P.M., Lacy B.E., Andrews C.N., Enns R.A., Howden C.W., Vakil N. ACG and CAG clinical guideline: management of dyspepsia. Am J Gastroenterol. July 2017;112(7):988–1013. doi: 10.1038/ajg.2017.154. [DOI] [PubMed] [Google Scholar]
- 3.Shaukat A., Wang A., Acosta R.D., Bruining D.H., Chandrasekhara V., Chathadi K.V. The role of endoscopy in dyspepsia. Gastrointest Endosc. 2015;82(2):227–232. doi: 10.1016/j.gie.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Jones R.H. Approaches to uninvestigated dyspepsia. Gut. 2002 May;50(Suppl 4):iv42–iv46. doi: 10.1136/gut.50.suppl_4.iv42. PMID: 11953347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilhelm S.M., Rjater R.G., Kale-Pradhan P.B. Perils and pitfalls of long-term effects of proton pump inhibitors. Expet Rev Clin Pharmacol. 2013 Jul;6(4):443–451. doi: 10.1586/17512433.2013.811206. PMID: 23927671. [DOI] [PubMed] [Google Scholar]
- 6.Kinoshita Y., Ishimura N., Ishihara S. Advantages and disadvantages of long-term proton pump inhibitor use. J Neurogastroenterol Motil. 2018;24(2):182–196. doi: 10.5056/jnm18001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joshi Y.G., editor. Charak Samhita; shlok number -1/111. 5th. Vaidyamitra Prakashana; Pune: 2003. [Google Scholar]
- 8.Sharma H.P. Kashyap Samhita. Varanasi: chaukhaba sanskrut sansthan. 4th ed. 2010. [Google Scholar]
- 9.Tewari P., editor. Kasyapasamhita/vrddhajivakiya tantra. Chaukhambha Visvabharati; Varanasi: 2002. (Reprint Ed) [Google Scholar]
- 10.Patwardhan B. Ayurveda GCP Guidelines: need for freedom from RCT ascendancy in favor of whole system approach. J Ayurveda Integr Med. 2011 Jan;2(1):1–4. doi: 10.4103/0975-9476.78175. PMID: 21731379; PMCID: PMC3121247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwak S.G., Kim J.H. Central limit theorem: the cornerstone of modern statistics. Korean J Anesthesiol. 2017 Apr;70(2):144–156. doi: 10.4097/kjae.2017.70.2.144. Epub 2017 Feb 21. PMID: 28367284; PMCID: PMC5370305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Browne R.H. On the use of a pilot sample for sample size determination. Stat Med [Internet] 1995;14(17):1933–1940. doi: 10.1002/sim.4780141709. https://onlinelibrary.wiley.com/doi/full/10.1002/sim.4780141709 Available from: [DOI] [PubMed] [Google Scholar]
- 13.Stanghellini V. Functional dyspepsia and irritable bowel syndrome: beyond Rome IV. Dig Dis. 2017;35(Suppl 1):14–17. doi: 10.1159/000485408. Epub 2018 Feb 8. PMID: 29421792. [DOI] [PubMed] [Google Scholar]
- 14.Anonymous, rastantrasaar and siddhaprayog sangraha- Khand1. Krishna Gopal Ayurved Bhawan(Dharmarth Trust); Ajmer, Rajasthan, India: 2015. [Google Scholar]
- 15.GOI. Guduci. In: The ayurvedic pharmacopoeia of India-Part 1. Government of India, Ministry of Health and Family Welfare, Department of Ayush; page 53.Available from: http://www.ayurveda.hu/api/API-Vol-1.pdf.
- 16.Vidyanath R., editor. Asthanga sangrah (sutra sthana) 1st ed. Chaukhamba Surbharati Prakashan; Varanasi: 2006. [Google Scholar]
- 17.Kaviraj Govind Das Sen . Bhaisajya ratnavali. In: Mishra S., Rogadhikara Bala, editors. (Reprint ed.) chapter 71, verse171-176. Chaukhamba Surbharati Prakashan; Varanasi: 2013. p. 1094. [Google Scholar]
- 18.Kashinath shastri ed rasatarangini prasadani commentary by haridutta shastri. 11th ed. Motilal Banarasidas; New Delhi: 2000. [Google Scholar]
- 19.Davis L.L. Instrument review: getting the most from a panel of experts. Appl Nurs Res. 1992;5(4):194–197. doi: 10.1016/S0897-1897(05)80008-4. [DOI] [Google Scholar]
- 20.Yadavji Acharya V.D., editor. Ashtang hrudaya of vagbhat, sutra sthana; chapter-14/4. 2014 edition. Chaukhamba Surbharati prakashan; Varanasi: 2014. [Google Scholar]
- 21.Department of Drvyagunavinjana, e-Ayu, Formulary of India [internet], [cited 2019 Oct 3]; Govt.Ayurveda College, Thiruvananthapuram, Available from: https://dravyagunatvpm.wordpress.com/ayurvedic-formulary-of-india/.
- 22.Suryavanshi S.V. Prospective interventional study of avipattikar churna in relation with AMLAPITTA vyadhi. IOSR J Pharm Biol Sci Ver I [Internet] 2015;10(4):2319–7676. doi: 10.6084/M9.FIGSHARE.1470221.V1. [DOI] [Google Scholar]
- 23.Seth Ankit, Maurya S., Srivastava Ashish. Formulation development, characterization & estimation of acid neutralization capacity of Shankha Bhasma tablets for the treatment of dyspepsia. Int J Pharm Pharmaceut Sci. 2014;6(2):467–469. https://api.semanticscholar.org/CorpusID:3625149 Available from: [Google Scholar]
- 24.Saha D., Paul S., Hosen S.M., Emran T Bin, Rahim Z Bin. Role of Ayurvedic formulation in digestion. Int Res J Pharm Pharm. 2012 August;2(8):187–192. [Google Scholar]
- 25.Sanjore (Naringe) S.S., Kharche G.Y. Studies on Urdhwaga amlapitta (gastritis) and its management with shatavari ghruta. Asian J Pharmaceut Res Dev. 2019;7(3):78–93. https://ajprd.com/index.php/journal/article/view/518 [Internet] Available from: [Google Scholar]
- 26.Joshi G., Jalandhar S. Tinospora Cordifolia: a phytopharmacological review. Int J Pharma Sci Res. 2016;7(3):890–897. doi: 10.13040/IJPSR.0975-8232.7(3).890-97. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.