Abstract
Immune response of a human body to the uncertain factors leads to the accelerated inflammatory proliferation of the ailing cells of the skin known as Psoriasis. Although the condition found described many decades ago, the etiology and treatment look under-researched. In Ayurveda, many herbs have proven efficacy in psoriasis, but the multifaceted etiology of the disease needs a multimodal treatment approach. We report about Ayurveda treatment in a 68-year-old female patient with plaque psoriasis presented with erythematous plaques on the anterior surface of the legs, right forehand, and neck region. The Auspitz sign and Koebner phenomenon were positive. The treatment protocol was adopted as per Ayurvedic samprapti (pathophysiology) and the patient cured completely without reporting any adverse events after the one year of treatment. No recurrence observed even after one year of the halted treatment. The importance of a wholesome diet as a health promoter is also revalidated. Photographic documentation was recorded with the proper consent of the patient during successive treatment and regular follow-ups. Altogether, multimodal Ayurveda treatment led to speedy and substantial recovery from a chronic case of psoriasis.
Keywords: Psoriasis, Auspitz sign, Ayurveda, Kushtha, Herbs, Case report
1. Introduction
Psoriasis is a chronic immune-mediated inflammatory condition mainly affecting the skin and joint. Its prevalence in India is about 0.44–2.8 percent. Males are being affected by psoriasis two times more common than females [1]. Various sites of the body such as scalp, face, trunk, limbs, palms, and soles involve in psoriasis. The diagnosis of psoriasis depends on tissue biopsy and distribution of skin damage. Plaque psoriasis (Psoriasis vulgaris), Inverse psoriasis, Guttate psoriasis, Pustular psoriasis, and Erythrodermic psoriasis are a few of the clinical patterns reported in psoriasis cases [2]. The chronic nature, recurring pattern, and visibility of psoriasis produce a great adverse impact on the psychological and social aspects of patients’ life. Psychosocial disability affects their daily work as well as social interactions. In Ayurveda, skin diseases have collectively considered under a common term of Kushtha. Most of the formulations described in Kushtha chikitsa have efficiently been used by the physicians to treat different skin ailments. However, due to the complex pathophysiology and chronic and relapsing nature of psoriasis, the multimodal treatment approach has been adopted covering the Jirnajwara chikitsa, Vatarakta chikitsa, and Rasayana chikitsa along with Kushtha chikitsa. In the present case, the multimodal Ayurveda treatment approach resulted in early recovery from psoriatic lesions with no recurrence so far.
1.1. Patient information
A 68-year-old female homemaker had been diagnosed as plaque psoriasis and was treated by a consulting dermatologist wherefrom the patient was taking allopathic treatment for three years with regular follow-ups. Topical and systemic immunosuppressive therapy was resulted in symptomatic relief during the last treatment. Personal history revealed that the patient’s general health was good. All the blood tests (routine tests) were within a normal range. No concomitant illness was found associated. However, due to a recurring pattern caused by the unknown aggravating factors, the patient discontinued allopathic treatment and consulted for Ayurveda treatment.
2. Clinical findings
The patient presented with erythematous plaques on the anterior surface of the shin bone, forehand, and neck region. The affected skin was found with a variable shade of red color and the surface covered with large silvery scales (Fig. 1a and b). The patient was suffering from itching and burning all over the body. At the time of the case presentation, the Auspitz sign and Koebner phenomenon found positive. No signs of psoriatic arthritis and nail bed psoriasis were found.
Fig. 1.
Periodic clinical outcomes in response to Ayurveda treatment.
2.1. General examination
Body temperature (97.6 °F), Pulse (88/min), and Blood Pressure (118/86) were within normal limit.
2.2. Systemic examination
In systemic examination, respiratory and cardiovascular system found normal. The patient was restless due to itching and burning sensation over psoriatic lesions.
2.3. Asthavidha pariksha
Nadi (pulse) – Pittakaphaja; Mala (stool)– Sandra-picchila, bowel habit was regular; Mutra (urine) – Prakrita; Jivha (tongue)– Shveta-picchila, Sama (coated); Shabda – Prakrita; Sparsha (touch)– Ushna; Drika (vision) – Prakrita; Aakriti – Madhyam (medium built).
2.4. Nidana panchaka
Nidana – Viruddhahara sevana (simultaneous use of milk and salty snacks) and Raktadushtikar Ahara-vihara (excessive use of salty food, sour food like pickles, curd and sitting a long time in direct sunlight); Samprapti – Dosha – Pitta, Kapha and Rakta; Dushya – Rasadhatu, Raktadhatu and Mamsadhatu; Agni – Mandagni; Aam – Jatharagni and Dhatvagni janya; Strotasa – Rasavaha, Raktavaha and Mamsavaha; Adhisthana – Twaka; Rogamarga – Bahya; Vyadhi Swabhava – Chirakari (chronic); Sadhyasadhyata – Kricchrasadhya (difficult to treat); Poorva roopa – Abhyantara daha (feeling of warmth), Kandu (itching), Mukhapaka (mouth ulcers) and Mandagni (anorexia); Roopa: Jwara (fever), Trishna (thurst), Daha (burning sensation), Kandu, Tvakavaivarnyata (in present case, skin with a variable shade of red color and the surface covered with large silvery scales.), Balahani (generalized weakness); Upashaya – Bahya shita sparsha and Abhyanga (improvement on wet cold sponging and oil application); Anupashaya – Ushna sparsha (increased symptoms on work in hot and humid climate).
2.5. Diagnostic assessment
All routine blood tests were within a normal range. The patient was not ready for tissue biopsy due to unaffordable cost. Therefore, based on clinical presentation, distribution of the skin damage, and positive Auspitz sign, the case diagnosis was confirmed as plaque psoriasis.
3. Therapeutic interventions
All oral and topical modern medications stopped. In this case, the involvement of pitta and kapha dosha ascertained by observing the clinical presentation such as Daha (burning sensation), Kandu (itching), Raktavarnata (redness), and the nature of skin lesions. Vitiated pitta and kapha dosha found involved in the pathological progress. The details of the internal and external medications prescribed have been mentioned in Table 1.
Table 1.
List of internal and external medications with dose, adjuvant, and duration.
| Sr. No. | Formulation | Dose, frequency and time | Adjuvant | Durationa |
|---|---|---|---|---|
| 1. | Patolakaturohinyadi kashaya (Herbal decoction) | 20 mL of kashaya, twice daily on an empty stomach | 50 mL of lukewarm water | 6 Month |
| 2. | Kaishor guggulu (Tablet) | 1 gm (2 tablets) twice daily, after meal | Lukewarm water | 6 Month |
| 3. | Mahatiktaka ghrita (Capsule of medicated ghee) | 2 gm (4 capsules), once daily on an empty stomach at early morning | Warm water | 6 Month |
| 4. | Gandhaka rasayana (Tablet) | 250 mg (2 tablets) twice daily, after breakfast | Water | 6 Month |
| 5. | Khadirarishta (Herbal fermented liquid) | 20 mL of arishta, twice daily after meal | 50 mL of normal water | 6 Month |
| 6. | Winsoria oil (Herbal coconut base oil) | Twice a day, Topical application | – | 1 Year |
| 7. | Strict dietary plan | Restricted use of salt, sour food items, curd, old butter, milk and sweet products, meat and fish, overeating etc. | – | 2 Years |
(All the internal medicines continued for the next six months by reducing their aforementioned prescribed doses to the half and with the same frequency, time, and adjuvant.).
The details of all the prescribed medicines including their classical reference, ingredients, and indications are given in Supplementary Table 1.
4. Timeline
In the present case, all the treatment was continued for one year. Pathyahara (A strict dietary plan) continued for the next one year after the end of active treatment to check the recurrence of psoriasis.
5. Follow up and outcomes
The Follow-ups details with timeline, treatment protocol, and periodic clinical outcome have been mentioned in Table 2. The psoriatic lesions with all its signs and symptoms cured. No adverse events witnessed during the treatment. Photographs of affected areas before and after the treatment are shown in Fig. 1. The patient kept only on a strict dietary regimen for the next year but no recurrence observed. Photographs captured with the consent of the patient revealed the same results after the two years (Fig. 1g,h).
Table 2.
Follow-up history and clinical outcomes.
| Timeline | Dates | Treatment plan | Periodic clinical outcomes |
|---|---|---|---|
| Onset of treatment | 20/04/2018 | As per Table 1 | Ayurveda treatment started. |
| Follow-up 1 | 29/05/2018 | As per Table 1 | Subjective improvement in signs and symptoms. Itching and redness reduced. |
| Follow-up 2 | 28/06/2018 | As per Table 1 | Observational changes in signs and symptoms (Fig. 1c, d). Auspitz Sign found negative. |
| Follow-up 3 | 31/07/2018 | As per Table 1 | Significant improvement in all signs and symptoms. No itching and burning sensation. |
| Follow-up 4 | 28/08/2018 | As per Table 1 | Recovered completely (Fig. 1e, f). No itching and burning sensation. |
| Follow-up 5 | 23/10/2018 | Dose of medicines reduced to half | No recurrence found. Normal biochemical profile. |
| Follow-up 6 | 16/04/2019 | Only dietary regimen continued | No recurrence found. |
| Follow-up 7 (telephonic conversation) | 22/10/2019 | Only dietary regimen continued | No relapse in any sign and symptom. |
| Follow-up 8 | 30/04/2020 | Only dietary regimen continued | No relapse in any sign and symptom (Fig. 1g, h). |
6. Discussion
Psoriasis is an autoimmune disease where genetic and environmental factors have a significant role [3]. Moreover, cytokines, inflammatory cascade, and keratinocytes play an important role in the pathogenesis of psoriasis [4]. Among different types of psoriasis, plaque psoriasis (psoriasis vulgaris) is the most common form of psoriasis where silvery-white scales with raised areas of reddened skin are known as Plaques [2]. Being an autoimmune disease, it is quite difficult to treat. Therefore, the treatment principles of Jirnajwara chikitsa, Vatarakta chikitsa, Rasayana chikitsa, and Kushtha chikitsa have been implemented together.
In the present case, pitta, kapha, and rakta were the Doshas, and Rasadhatu, Raktadhatu, and Mamsadhatu were the Dushyas. Dosha-dushya samurcchana (pathological progress) was taken place due to the circulation of vitiated Doshas and their Sthanasamshraya (site of pathological changes) at Tvaka (skin) with the clinical presentation of Vyadhilakshnanas (signs and symptoms of psoriasis). The treatment protocol was adopted for Samprapti bhedana (to counteract the pathophysiology) where Pitta-kaphahara, Jirnajwarahara, Vataraktahara, and Rasayana along with Kushthaghna aushadhiyogas (medicines) were preferred. Also, the Agnidipana (improvement of the biological fire), Ampachana, Rasaprasadana (improvement in the quality of blood), and Raktaprasadana (purification of the blood) were achieved with the help of all the internal medicines. The intake of Viruddha ahara (the unwholesome dietary practices) is one of the important causative factors in the etiopathogenesis of skin diseases. The patient should avoid Viruddha ahara for better treatment response, speedy recovery, and to avert the recurrence in chronic skin ailments. In present case, the patient was following the excess use of salty and sour food items, old butter and curd, spicy food, simultaneous use of milk products and salty snacks, etc. The patient was taking modern medications without sidestepping the causative factors as par Ayurveda. Therefore, temporary relief had observed with a relapsing pattern during the allopathic treatment. Thus, in the present case, the strict dietary regimen (Pathya) has been advised as the mitigating intervention along with Ayurveda medicines.
The ongoing pathological changes were attenuated and corrected following internal medications such as Patolakaturohinyadi kashaya [5], Kaishor guggulu [6], Mahatiktaka ghrita [7], Gandhaka rasayana [8], and Khadirarishta [9]. The multimodal Ayurveda treatment approach was adopted by considering all the possible pathomechanism.
Patolkaturohinyadi kashaya has mentioned under Shodhanadi gana in Astangahridaya. It is enriched with Tikta rasa (bitter) dravyas that help in the Rasadhatu and Raktadhatu prasadana by pacifying vitiated kapha and pitta doshas. It has kushthaghna (corrects skin ailments), Jwaraghna (antipyretic), and Vishaghna (anti-poison) properties [5]. It is useful in skin diseases associated with itching, pigmentation, and burning sensation. It is also an effective medicine for liver detoxification. According to Ayurveda, the liver is an important organ for the normal functioning of pitta dosha and raktadhatu. It improves appetite and aids in digestion due to Amapachana and Agnivardhana properties.
Various scientific reports reveal the promising effects of Guggulu (Commiphora mukul Hook ex Stocks.) against different chronic diseases such as psoriasis, dermatitis, skin diseases, infectious diseases, arthritis, etc. It is due to its anti-inflammatory and anti-oxidant effects by targeting multiple signaling pathways [10]. Terpenoidal constituents, steroids, flavonoids, guggultetrols, lignans, sugars, and amino acids present in Guggulu are responsible for its therapeutic effects [11]. Guggulu is well known for its yogavahi (synergism) property in Ayurveda. Guggulu can act as a drug carrier by entrapping active pharmaceutical ingredients and mediate their sustained release action [12]. Gugulipid found as effective as tetracycline in the treatment of nodulocystic acne proving the anti-infective and antibacterial properties of Guggulu [13]. K. guggulu is a polyherbal preparation indicated in Vatarakta and well known for its Kantikara (restores skin’s natural radiance and suppleness) property in Ayurveda [6]. It reduces inflammation and pain associated with Vatarakta by purifying blood. Furthermore, K. guggulu acts as an antiallergic, antibacterial, and blood purifying agent [14]. Therefore, it helps to reduce redness, inflammation and acts as a natural blood cleanser by its pacifying effects on deep sited vitiated doshas of psoriasis.
M. ghrita, a medicated ghee has administered internally for shamana (pacifying effect on dosha) purpose. A capsulated form of ghee (3 mL/capsule) was used instead of the classical dosage form to overcome the palatability problem due to its very bitter taste. In the case of Kushtha (skin diseases), doshas exist in dhatus such as Rasa, Rakta, Mamsa, and Meda. Ghee has sukshmastrotogamitva action and it can reach and also nourish the Shukra dhatu. Moreover, in Kushtha the medicated ghee fortified with Tikta and Kashaya rasa has been recommended for internal and external use. Various active phytoconstituents extracted in the Mahatiktaka ghrita work synergistically to cure psoriasis, possibly through the liposomal drug delivery system [15].
Gandhak (sulfur) in Ayurveda has Kushthaghna property. It’s Garavishahar (anti-poisonous) and Rasayana (rejuvenation) properties help to cure and correct the causes of skin diseases [16]. According to modern science, sulfur possesses an anti-inflammatory and anti-oxidant property which plays an important role in the treatment of autoimmune diseases such as psoriasis and psoriatic arthritis [17]. It is known for its Kushthaghna, Kledaghna, Ampachana, Raktaprasadana, and Rasayana properties. In Gandhak rasayana, purified sulfur has been treated with different medicinal herbs to improve its pharmacological actions to many folds [8].
Arista Kalpana is a continuous hydro-alcoholic extraction method wherein various phytoconstituents from raw herbs reach into the medium. Arista shows better therapeutic efficacy due to biological transformations into phytochemical compounds mediated by microbes [18]. Khadirarista has recommended for all types of Kushtha. Most of the ingredients of Khadirarista possess antipsoriatic action. The heartwood decoction of Khadir (Acacia catechu Willd.) has since long been used to treat skin ailments including psoriasis in a traditional practice. It helps to purify the blood. It has immunomodulatory action that may activate both cell-mediated as well as humoral immunity. Among various phytoconstituents present in Acacia catechu, catechins may contribute to its anti-inflammatory and antioxidant activities [19]. In an experimental study, the water extract of Acacia catechu showed inhibition of pro-inflammatory cytokine TNF-α and a significant increase in cytokine IL-10. IL-10 helps to control the secretion of pro-inflammatory cytokines by augmenting the proliferation of B cells, mast cells, and thymocytes [20]. Darvi (Berberis aristata DC.) has anti-inflammatory activity. In skin diseases, the aqueous extract of B. aristata is found effective internally as well as externally [21]. Topically applied B. aristata extract loaded transferosomal gel showed marked improvement in inflammatory changes of psoriatic skin of experimental animals [22]. Since ages, Bakuchi (Psoralia corylifolia Linn.) has also been used for its promising results in various skin ailments. It contains various phytoconstituents such as flavonoids, alkaloids, coumarins, meroterpens, and essential oils which contribute to its multifaceted pharmacological actions including anti-inflammatory, antioxidant, anti-leprotic, antipsoriatic, antibacterial, anticancer and immunomodulatory activities [23,24]. Dhataki pushpa (flowers of Woodfordia fruticosa Kurz.) is useful in inflammation and skin diseases [25].
After the treatment of the first six months, the prescribed doses of all the internal medicines were reduced to the half by considering the age, gender, roga and rugna Bala (severity of the disease and the condition of the patient) and, rogavastha (stages of the disease) [6].
In the present case, winsoria oil has prescribed for external use. In winsoria oil, coconut oil (Cocos nucifera (L.) Kuntze.) has processed with Vidaphala (Wrightia tinctoria R. Br.), Manjishta (Rubia cordifolia Linn.), and Sariva (Hemidesmus indicus R. Br.). Winsoria oil carries all the active pharmaceutical ingredients from these herbs and helps to cure psoriasis by enhancing their permeation across the skin. It retards hyperkeratinization, silvery scales, inflammatory responses, reduce exfoliation, and discoloration of the skin. It also prevents itching and formation of scales and sores. Vidaphala is useful in psoriasis [26]. It has anti-inflammatory and anti-dandruff properties and it is commonly used in hair oil preparations. In 777 Oil, a coconut oil-based herbal preparation for psoriasis, the leaf extract of W. tinctoria has been used [27]. Manjishtha is known for its Raktashuddhikara, Pitta-kaphahara, Vranaropana (wound healing), and Kushthaghna properties. It also has an antipsoriatic activity. Ethyl acetate fraction of ethanolic extract of its root formulated in the form of topical gel exhibited inhibitory action on keratinocyte proliferation in the mouse tail model [28]. Sariva has also reported for anti-inflammatory, immunomodulatory, and antioxidant properties. It is effective in psoriasis due to its raktaprasadana, dahaprashamana (reduces burning sensation), and shothahara (anti-inflammatory) properties [29]. Coconut oil improves the symptoms of skin disorders by its moisturizing, soothing, and emollient effects. It possesses anti-inflammatory activity. It suppresses the inflammatory markers such as cytokines, prostaglandins, leukotrienes, and protects the skin by improving skin barrier function. In psoriasis, epidermal keratinocytes react to pro-inflammatory cytokines like tumor necrosis factor-α (TNF-α) and interferon-γ (IFN-γ). Interleukin 6 (IL-6) causes epidermal hyperplasia in the psoriatic epithelium. Coconut oil intervenes in anti-inflammatory activity by reducing the secretion of IL-6 level. Uncontrolled cytokine expression can lead to dysfunction of the epidermal barrier as seen in psoriasis. The topical application of coconut oil inhibits the various cytokine levels including TNF-α, IFNγ, IL-6, IL-5, and IL-8 [30].
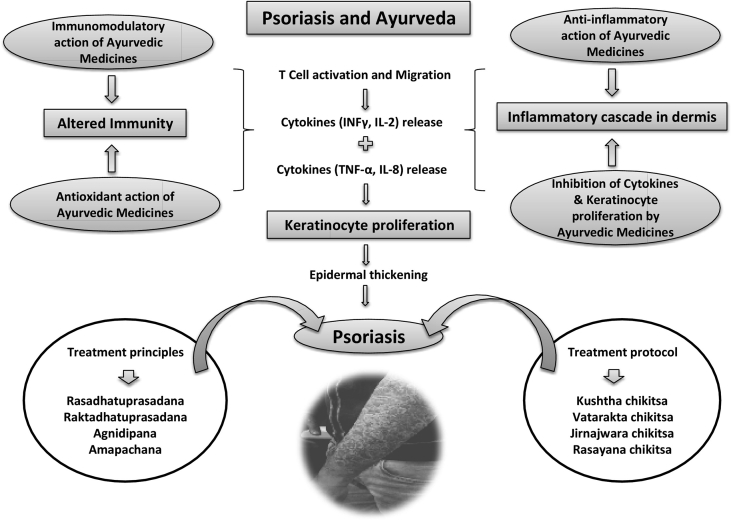
The promising outcomes in the present case are a combined effect of all the Ayurveda medicines, pathya sevana (a strict diet plan), and regular follow-ups by the patient. The possible mechanism and role of Ayurveda medicines in the Samprapti-vighatana (counteracting the pathophysiology) of psoriasis have depicted in Fig. 2.
Fig. 2.
The possible actions of Ayurveda drugs in Psoriasis.
7. Patient perspective
The patient shared her perspective about the Ayurveda treatment in her local (Hindi) language. She had severe itching, burning sensation, and stress at the time of presentation, while she was free from all the signs and symptoms at the end of treatment.
8. Conclusion
In the present case, the treatment protocol was adopted as per Ayurvedic samprapti and the treatment response was observed much earlier as compared to previous allopathic treatment. No recurrence reported after the end of active treatment. The importance of a wholesome diet as a health promoter is also revalidated. The external and internal medications of Ayurveda help to correct the complex pathophysiology of psoriasis like chronic diseases. Altogether, multimodal Ayurveda treatment led to speedy and substantial recovery from a chronic case of psoriasis.
9. Informed consent
Consent of the patient was obtained for the photographs and before reporting the case report for publication.
Source(s) of funding
We are grateful to the Kerala Ayurveda Limited, Head Office, Athani Post, Aluva, Ernakulam District, Kerala – 683585, India, for sponsoring the Article Publishing Charges.
Conflict of interest
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2020.11.009.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Thappa D.M., Munisamy M. Research on psoriasis in India: where do we stand? Indian J Med Res. 2017;146(2):147–149. doi: 10.4103/ijmr.IJMR_1296_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rendon A., Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20:1475. doi: 10.3390/ijms20061475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reali E., Brembilla N.C. Editorial: immunology of psoriatic disease. Front Immunol. 2019;10:657. doi: 10.3389/fimmu.2019.00657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baliwag J., Barnes D.H., Johnston A. Cytokines in psoriasis. Cytokine. 2015;73(2):342–350. doi: 10.1016/j.cyto.2014.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaud B.L., editor. (reprint). Astanga hridaya of vagbhata, sootra sthana; shodhanadiganasamgraha: [chapter 15], verse 15. Chaukhambha Orientalia; Varanasi: 2013. p. 256. [Google Scholar]
- 6.Shrivastava S., editor. (reprint). Sharangadhar samhita of acharya sharangadhar, Madhyam khand; Vvataka Kalpana: chapter 7, verse 70-81, poorva khand; paribhasha: chapter 1, verse 37. Chaukhambha Orientalia; Varanasi: 2016. 204, 10. [Google Scholar]
- 7.Tripathi B., editor. (reprint). Charaka samhita of agnivesha, chikitsasthan; Kushtha chikitsa: chapter 7, verse 144-150. Chaukhambha Surbharati Prakashana; Varanasi: 2013. pp. 327–328. [Google Scholar]
- 8.Shastri L., editor. (reprint). Yogaratnakar, uttarardh; Rasayanadhikar: verse 1-8. Chaukhmbha Prakashan; Varanasi: 2010. pp. 501–502. [Google Scholar]
- 9.Shastri A., editor. (reprint). Bhaishajya ratnavali of Shri Govind Das, chapter 54, verse 365-370. Chaukhmbha Prakashan; Varanasi: 2012. p. 914. [Google Scholar]
- 10.Kunnumakkara A.B., Banik K., Bordoloi D., Harsha C., Sailo B.L., Padmavathi G. Googling the guggul (commiphora and boswellia) for prevention of chronic diseases. Front Pharmacol. 2018;9(686):1–19. doi: 10.3389/fphar.2018.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Francis J.A., Raja S.N., Nair M.G. Bioactive terpenoids and guggulusteroids from Commiphoramukul gum resin of potential anti-inflammatory interest. Chem Biodivers. 2004;1(11):1842–1853. doi: 10.1002/cbdv.200490138. [DOI] [PubMed] [Google Scholar]
- 12.Sarup P., Bala S., Kamboj S. Pharmacology and phytochemistry of oleo-gum resin of commiphora wightii (guggulu) Sci Tech Rep. 2015:138039. doi: 10.1155/2015/138039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thappa D.M., Dogra J. Nodulocystic acne: oral gugulipid versus tetracycline. J Dermatol (Tokyo) 1994;21(10):729–731. doi: 10.1111/j.1346-8138.1994.tb03277.x. [DOI] [PubMed] [Google Scholar]
- 14.Bharati P.L., Agrawal P., Prakash O. A case study on the management of dry gangrene by kaishore guggulu, sanjivani vati and dashanga lepa. Ayu. 2019;40(1):48–52. doi: 10.4103/ayu.ayu_244_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh N., Chaudhary A. A comparative review study of Sneha Kalpana (Paka) vis-a-vis liposome. Ayu. 2011;32(1):103–108. doi: 10.4103/0974-8520.85740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shastri K., editor. Rasatarangini of shri sadanand sharma, astam tarang: chapter 8, verse 36. 11th ed. Motilal Banarasidas; Varanasi: 1979. p. 181. [Google Scholar]
- 17.Stephen W. Parcel, sulfur in human nutrition and applications in medicine. Altern Med Rev. 2002;7(1):22–44. [PubMed] [Google Scholar]
- 18.Chaudhary A., Singh N., Dalvi M., Wele A. A progressive review of Sandhan Kalpana (Biomedical fermentation): an advanced innovative dosage form of Ayurveda. Ayu. 2011;32(3):408–417. doi: 10.4103/0974-8520.93925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ismail S., Asad M. Immunomodulatory activity of Acacia catechu. Indian J Physiol Pharmacol. 2009;53(1):25–33. [PubMed] [Google Scholar]
- 20.Sunil M.A., Sunitha V.S., Radhakrishnan E.K., Jyothis M. Immunomodulatory activities of Acacia catechu, a traditional thirst quencher of South India. J Ayu Integr Med. 2019;10(3):185–191. doi: 10.1016/j.jaim.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Potdar D., Hirwani R.R., Dhulap S. Phytochemical and pharmacological applications of Berberisaristata. Fitoterapia. 2012;83:817–830. doi: 10.1016/j.fitote.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Nimisha Rizvi DA., Fatima Z., Neema, Kaur C.D. Antipsoriatic and anti-inflammatory studies of berberisaristata extract loaded nanovesicular gels. Phcog Mag. 2017;13(Suppl 3):S587–S594. doi: 10.4103/pm.pm_210_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khushboo P.S., Jadhav V.M., Kadam V.J., Sathe N.S. Psoralea corylifolia Linn. —“Kushtanashini”. Phcog Rev. 2010;4(7):69–76. doi: 10.4103/0973-7847.65331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X., Zhao W., Wang Y., Lu J., Chen X. The chemical constituents and bioactivities of Psoralea corylifolia Linn.: a review. Am J Chin Med. 2016;44(1):35–60. doi: 10.1142/s0192415x16500038. [DOI] [PubMed] [Google Scholar]
- 25.Srivastava A.K., Nagar H.K., Chandel H.S., Ranawat M.S. Antipsoriatic activity of ethanolic extract of Woodfordia fruticosa (L.) Kurz flowers in a novel in vivo screening model. Indian J Pharmacol. 2016;48(5):531–536. doi: 10.4103/0253-7613.190740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramchandra P., Basheermiya M., Krupadanam G.L., Srimannarayana G. Wrightial, a new terpene from Wrightia tinctoria. J Nat Prod. 1993;56(10):1811–1812. doi: 10.1021/np50100a022. [DOI] [Google Scholar]
- 27.Srivastava R. A review on phytochemical, pharmacological, and pharmacognostical profile of Wrightia tinctoria: adulterant of kurchi. Phcog Rev. 2014;8(15):36–44. doi: 10.4103/0973-7847.125528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin Z.X., Jiao B.W., Che C.T., Zuo Z., Mok C.F., Zhao M. Ethyl acetate fraction of the root of rubia cordifolia L. Inhibits keratinocyte proliferation in vitro and promotes keratinocyte differentiation in vivo: potential application for psoriasis treatment. Phytother Res. 2010;24(7):1056–1064. doi: 10.1002/ptr.3079. [DOI] [PubMed] [Google Scholar]
- 29.Nandy S., Mukherjee A., Pandey D.K., Ray P., Dey A. Indian Sarsaparilla (Hemidesmus indicus): recent progress in research on ethnobotany, phytochemistry and pharmacology. J Ethnopharmacol. 2020;254:112609. doi: 10.1016/j.jep.2020.112609. [DOI] [PubMed] [Google Scholar]
- 30.Varma S.R., Sivaprakasam T.O., Arumugam I., Dilip N., Raghuraman M., Pavan K.B. In vitro anti-inflammatory and skin protective properties of Virgin coconut oil. J Tradit Complement Med. 2019;9(1):5–14. doi: 10.1016/j.jtcme.2017.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.