Abstract
Introduction
Uncemented unicompartmental knee replacement offers a minimally invasive approach, faster rehabilitation and good levels of function, supported by evidence reporting low intra-operative fracture rate and mid-term stability with no implant migration at 5-years. Our aim was to examine the clinical outcomes in 289 consecutive Oxford unicompartmental knee arthroplasties (257 patients), five years post-operatively.
Methods
A retrospective study of patients treated between 2008 and 2014 in a non-inventor centre by a single surgeon was performed. Patients with anteromedial bone on bone uni-compartmental arthritis were included. Oxford Knee Scores (OKSs) at last follow-up were recorded, intra-operative complications reported with commentary on revision cases.
Results
Mean age of patients was 66 years (SD 9.6, 45–88 years). 122 (42%) patients were female and 135 (58%) were male. Patient in our study were ASA 1 (36%), ASA 2 (62%) and ASA 3 (01%). There were no intra-operative complications, particularly tibia fractures during impaction. The average oxford knee score was 40.1 (n = 232, Range 06 to 48, SD 8.46) at an average 6 years and 3 months from surgery, including revised patients. Six patients had their prosthesis revised within five-years of the index surgery. Five-year cumulative implant survival rate was 97.8% (95% CI 97.62 to 97.98, SE 0.09). Indications for revision were: lateral side wear (n = 1); dislocated spacer (n = 4); instability and spacer subluxation (n = 1). Thirteen patients died within five years of surgery Five-year cumulative survival rate was 94.9% (95% CI 94.87 to 94.925, SE 0.013).
Conclusion
The proportion of patients requiring revision at five-years is lower than that generally reported for UKR. These findings add support for the use of the cementless oxford UKR outside the design centre.
Keywords: Unicompartmental knee replacement, Knee arthroplasty
1. Introduction
The uni-compartmental knee replacement (UKR) has been has been demonstrated to be an effective treatment for patients with anteromedial compartment knee arthritis.1 Patient reported outcomes are comparable to total knee arthroplasty (TKA). The TOPKAT trial reported improved Oxford knee scores (OKS) in patients undergoing UKR compared to TKA at one-year with no difference reported at five-years.2 Mean length of stay and readmissions are also lower for patients undergoing UKR. Literature observes intraoperative complications, blood transfusion, venous thromboembolism, stroke and myocardial infarctions are significantly less likely for UKR compared to TKA.3.
According to the United Kingdom (UK) national joint registry 11.1% of all knee arthroplasty performed is a UKR. There is evidence to support high volume surgeons achieving improved results.4 The median age of patients undergoing UKR is also five-years younger compared to TKA. The Oxford UKR is the most commonly used UKR in the UK.5.
Early reoperation rates for any reason are higher for TKA however, revision of implant remains higher for UKR.6 The five-year revision rate according to registry data is 5.96% for the Oxford UKR. Data reported by Beverland et al. has demonstrated revision of implant to be 2.8% at 5 years.7 This non-inventor centre revision rate is considerably lower than national registry data. An analysis of 7407 cementless Oxford UKRs performed by Murray et al. identified the most common reasons for revisions of cementless OUKR were osteoarthritis progression (0.74%), unexplained pain (0.46%) and asceptic loosening (0.42).8 Uncemented implants have half the risk of revision for aseptic loosening compared to cemented OUKR.9 Beveland et al. have reported 5 year patient survival to be 93.3% for patients undergoing cementless OUKR.10.
An uncemented prothesis was introduced to eliminate the challenging technical steps reported during cementation of the original prosthesis. 11. The implant used in our study was the Biomet cementless UKR (Phase 3). The oxford UKR is an evolution of the original meniscal arthroplasty, which was first used in 1976. The femoral component is made of cobalt chromium molybdenum alloy for strength and wear resistance. The twin peg femoral component provides rotational stability and is highly polished.12.
This study builds upon existing evidence from the inventor centre and Beverland et al.
The primary aim is to define the five-year implant survival of patients undergoing an uncemented UKR at a non-inventor centre. The endpoint being defined as revision for any further operative intervention that includes change of polyethylene insert. Our secondary objectives were to quantify functional outcome at five-years by using oxford knee scores, record intra-operative complications and five-year mortality.
2. Methods
A prospective database of patients recorded patient demographics, surgical implants, complications and follow-up parameters. This database comprised of 257 patients operated on between 2008 and 2014. Patients with antero-medial bone on bone unicompartmental osteoarthritis were included, as described previously by Hamilton et al.13.
For implant survival data fields extrapolated were date of surgery, last follow-up and case specific evaluation of failures leading to revision. A failure was defined as a change of components (including spacer) or revision to total knee replacement. If follow-up was less than five-years patients were contacted by letter or telephone to attend clinic or submit postal questionnaires. Revision data was verified by the National joint registry to identify revisions performed at other centres.
For secondary outcomes, medical notes were reviewed and information was collated on operative complications, Oxford knee scores, radiographic complications and additional treatment. Mortality data was verified by hospital mortality register.
Postoperatively all surviving patients were followed for up by the primary surgical team. For patients who were alive, the minimum follow up was five-years. No control for co-morbidity, gender or age occurred when performing survival analysis for all-cause mortality.
All of the procedures were undertaken by a single surgeon at two surgical centres. The surgeon was fellowship trained in unicompartmental knee replacement, eliminating the learning curve. Patients had anteromedial bone on bone arthritis confirmed on radiographs, with additional Rosenburg and skyline patella projections when indicated. MRI was used sparingly to confirm integrity of cruciate ligaments and to assess integrity of the contralateral compartment.
The procedure was performed through a small parapatellar incision, not dislocating the patella. Extra-medullary tibia and intra-medullary femur preparation using microplasty surgical instruments, balancing extension and flexion gaps and avoiding impingement. Routine post-operative care comprised radiographs, early full weight bearing mobilisation with an emphasis on early discharge. Routine follow-up at 6 weeks and 1 and 5 years with completion of outcome scores.
No ethical approval was required for the study. Informed consent was obtained.
2.1. Statistical analysis
Five year-survival was calculated using Kaplan-Meier estimates. Endpoint was defined as implant revision. Time to event survival curves and life-tables were generated. Log rank-test compared survival variables. Normally distributed data was compared using paired Student’s t-tests. Mann–Whitney U tests were used to compare medians in non-parametric distributions. The level of significance for all analyses was p < 0.05 and 95% confidence intervals (CIs) were also used. All analyses were performed using SPSS version 21.0 (IBM Corp., Armonk, New York).
3. Results
There were 289 cementless Oxford UKR performed. 32 patients had bilateral procedures and 122 patients were female. The mean age of patients was 66 years of age (range, 45 to 88). Using ASA as a surrogate for co-morbidities, ASA 1 36%, ASA 2 63% and 1% ASA 3. Fig. 1 charts annual recruitment of patients, loss to follow up and mortality. At five-years from surgery 14 patients were lost to follow-up, 13 patients had died, and 6 implants revised. Initial loss to follow-up, within 6 months of index surgery comprised solely of private patients (n = 6).
Fig. 1.
A flow chart quantifying the number of patents who had died, were lost to follow-up (LFU) or revised at sequential time intervals from index surgery.
3.1. Revision rates
A total of six patients underwent revision surgery within five-years of index surgery. The five-year cumulative survival of implant was 97.8% (95% CI 97.62 to 97.98, SE 0.009). Fig. 2 highlights cumulative implant survival. No other revisions had been identified according to joint registry data.
Fig. 2.
Kaplan---Meier curve with cumulative implant survival in months. Vertical lines indicate censoring.
In summary, of the six revisions one was due to lateral compartment symptoms and the remaining five due to polyethylene dislocations. A total knee replacement was done in two cases. There were no revisions for intra-operative fracture, component loosening or tibial subsidence.
3.2. Case summary of revisions
A 51 year old male complained of persistent lateral compartment pain within a year of index surgery (Fig. 3). Initial X-Ray and MRI supported unicompartmental knee replacement. He subsequently underwent revision to a total knee arthroplasty due to lateral compartment arthiritis. His oxford knee score was 33 at nine years and three months with residual lateral knee pain.
Fig. 3.
Post-operative AP radiograph of 51-year-old gentleman undergoing medial OKR with preservation of lateral joint articular cartilage.Medial joint line elevated and over-stuffing had occurred.
Four patients had revision surgery for bearing dislocation (1.3%). 1 patient had instability and polyethylene insert subluxation due to recurrent falls and was revised to an uncemented TKA (Fig. 4). His oxford knee score was 37 at last follow up, seven-years and six-months from index surgery. No evidence of impingement or radiological malalignment in any of these cases.
Fig. 4.
Lateral radiograph of patient with polyethylene insert dislocation of right knee.
3.3. Functional outcomes
The mean oxford knee score was 40.1 (n = 232, Range 06 to 48, SD 8.46) at an average of 6 years and 3 months following surgery. We found no difference in oxford knee scores based on gender (p = 0.801). There was no correlation with OKS and age at index surgery (p = 0.895). 88 patients reported an OKS 44–49 at time of last follow up with 3 patients reporting scores between 6 and 11. Table 1 below shows the patient OKS at last follow up.
Table 1.
Histogram quantifying the oxford knee score at last follow-up in patient having an UKR.
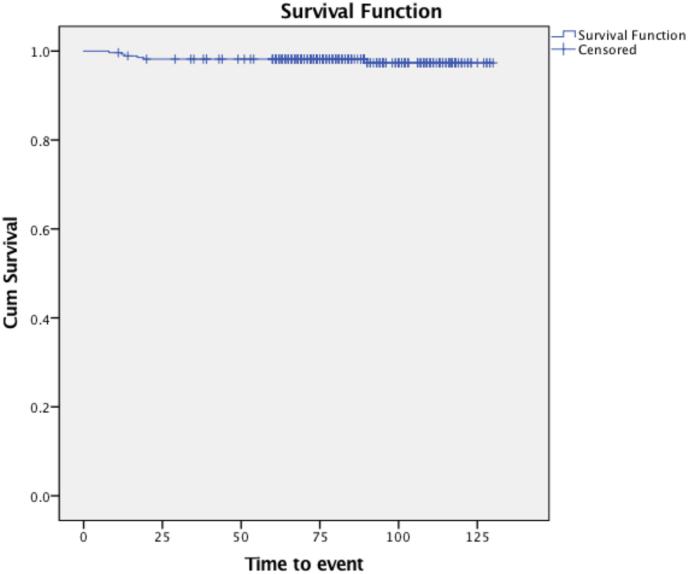
3.4. Mortality
13 patients had died within 5 years of the surgery. The cause of death was not investigated further however no deaths were related to immediate surgical factors. Five year cumulative survival with the end point determined as death was 94.9% (95% CI 94.87 to 94.925, SE 0.013). This is expressed as a Kaplan-Meier Curve (Fig. 5). No control for gender, co-morbidity, gender or age occurred.
Fig. 5.
Kaplan-Meier estimate of patient survival in months from index procedure.
3.5. Other complications
One patient sustained a tibial fracture following low energy trauma. This occurred in an 88 year old lady, 2 years and 4 months after index surgery. The sagittal plane fracture was minimally displaced, originating at the medial tibia spine, extending into the metaphysis to the medial cortex. Implant had subsided with a varus overall knee alignment. This was definitively managed conservatively in a non-weight bearing cast followed by a hinged knee brace with evidence of union at the 3 month check radiographs (Fig. 6 and Fig. 7).
Fig. 6.
AP X-Ray of left knee at time of injury with a medial tibial plateau fracture.
Fig. 7.
AP X-Ray of left knee 3 months following injury.
4. Discussion
The five-year revision rates for the oxford uni-compartmental knee replacement are estimated to be below 2.9% by Pandit et al. .14 This figure is in keeping with data published by Beveland et al. with a revision rate of 2.7%.15 Our study expands current evidence, supporting the use of the cementless UKR to treat patients with anteromedial knee arthritis. In this dual centre study of 289 cementless UKR’s six patients underwent further revision surgery at five-years, with a revision rate of 2.2%. These five-year implant survivorship rates are comparable with previously published literature.
The risk of bearing dislocation or subluxation when using the phase 3 Oxford UKR is 0.73%. 16 Most dislocations occur in the early post-operative period. In our series mean time for bearing subluxation was 14.8 months following surgery (range, 12–19 months). Primary dislocation usually occurs following distraction of the joint and bearing impingement. Secondary dislocations occur due to loss of entrapment and loosening or subsidence of the metal components. In our series five revisions occurred due to primary bearing dislocation or subluxation. Of these, two bearing dislocations occurred due to trauma. Upsizing of the bearing occurred in two cases and like for like exchange in two cases. In one case due to recurrent spacer subluxation a total knee replacement was performed. Incidence of spacer dislocation in our study was 1.7%, higher than previously reported. Intraoperatively there were no concerns regarding sizing of the polyethylene bearing. The senior author felt one patient’s post-operative radiographs suggest oversized bearing. This was not the case in the other patients suffering a dislocation and no evidence of impingement. Bearing dislocation is a risk, and can be managed successfully with a single stage bearing exchange which may need to be larger.
According to the UK national joint registry the five-year revision rate for unicompartmental knee replacements is 5.95% compared with 2.19% for total knee arthroplasty. Revision for unexplained pain occurs in 0.6% of cases. Perceived ease of revision by surgeons of converting a UKR to TKR may explain higher NJR revision rates. Literature published by Murray et al. recognises a revision risk due to progression of arthritis to be 0.74% and asceptic loosening to be 0.42% following UKR. Our study had one revision due to progressive arthritis (0.35%). These are comparable revision rates for a consecutive series incorporating learning curve, by a high-volume surgeon (mean 45 cases per year) who was fellowship trained. The most commonly implanted number of UKR by a surgeon according to joint registries is one followed by two. These surgeons have a reported revision rates of 40% at 10 years whereas those surgeons that perform over 30 a year had a revision rate which was not statistically different from revision rates of total knee replacements.17.
The low revision figures are also helped by the senior author’s meticulous follow-up program, supported by a specialist nurse practitioner. Perhaps negating the decision-making effect of other surgeons having a lower threshold to revise UKR during follow-up in patients with persistent knee pain, an observation that was made in early survival studies.18 No revisions occurred due to radiographic evidence of asceptic loosening of tibial or femoral components.
Periprosthetic tibial plateau fractures are a serious complication in unicompartmental knee arthroplasty. These can occur due to extended sagittal tibial bone cuts or during impaction of the uncemented implant. The load required to fracture the tibia with uncemented implants is lower than cemented implants.19 Beverland et al. found low rates of intra-operative fracture (0.004%)and 8.9% of radiographs had a partial tibial lucency, which were not clinically relevant.7 No intraoperative tibial fractures occurred in our study and no revisions occurred due to tibial subsidence or radiographic lucencies. A single tibial fracture occurred following traumatic injury which was managed conservatively. Our study further supports that radiographic lucencies are not a correlation to patient outcome nor are they an indication for further revision surgery.
This study has shown a five-year patient survival following index surgery of 94.9%. Thirteen deaths occurred in five years. Beveland et al. have reported five-year survival to be 93.3% for patients undergoing cementless OUKR.20 Our results are comparable to current evidence; however, this is all cause mortality that was not stratified by co-morbidity. The five-year patient survival rates for TKA according to UK registry data is 91.2% and UKR is 95.9%.
The average age for UKR in the UK joint registry is 64 years compared to 69 years for a TKA. Our results are comparable to registry data. The mean age and ASA of our cohort is 66 years and ASA 2.
In our study population the mean oxford knee score was 40.1 at a mean six years and three months from index surgery. Researchers have questioned the efficacy of uncemented prothesis in older patients, however functional outcomes did not vary by age groups.
The study must be considered in line with its limitations. There was loss to follow-up, although we regard 14 patients in this sample size to be small. We lack pre-operative oxford knee scores and cannot quantify the degree of improvement at one-year following surgery. When calculating patient death rates at five-years we did not control for co-morbidity or investigate the cause of death. Thus, we cannot accurately quantify the impact surgery had on our patients. Post-operative radiographs were not evaluated for evidence of subsidence or tibial lucencies as this has been investigated and reported on. Thus, particular focus was placed on clinical parameters rather than radiological findings.
In conclusion, the proportion of patients requiring revision at five-years is lower than that generally reported for UKR. Patient survival is in keeping with data reported by the inventor centre. These findings add support for the use of the cementless Oxford UKR outside the design centre in a safe and effective manner.
Author contributions
R. Nandra: Collected and analysed data, wrote manuscript
H.D. Rajgor: Wrote manuscript
C. Winkworth: Collected data. Edited the manuscript
N. Aslam: Initiated project, Edited manuscript
References
- 1.Burn E., Liddle A., Hamilton T. Choosing between unicompartmental and total knee replacement: what can economic evaluation tell us? A systematic review. Pharmacoecon. 2017;4:241–253. doi: 10.1007/s41669-017-0017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beard D.J., Price A.J., Cook J. Total or partial knee replacement for medial osteoarthritis? Early results from the TOPKAT trial. Arthroscopy. 2017;33:e91. doi: 10.1016/j.arthro.2017.08.091. 2. [DOI] [Google Scholar]
- 3.Liddle A., Judge A., Pandit H., Murray Adverse outcomes after total and unicompartmental knee replacement in 1010330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384(9952):1437–1445. doi: 10.1016/S0140-6736(14)60419-0. [DOI] [PubMed] [Google Scholar]
- 4.Murray D., Liddle D., Dodd C., Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty? Bone Joint Lett J. 2015;97-B(10 Suppl A):3–8. doi: 10.1302/0301-620X.97B10.36542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.No authors listed National Joint Registry: 16th Annual Report. 2019. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf [PubMed]
- 6.Wilson H.A., Middleton R., Abram S.G.F. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ. 2019 Feb 21;364:l352. doi: 10.1136/bmj.l352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liddle A., Pandit H., O’brien S., Doran E. Cementless fixation in oxford unicompartmental knee replacement. A multicentre study of 1000 knees. Bone Joint Lett J. 2013;95-B doi: 10.1302/0301-620X.95B2.30411. [DOI] [PubMed] [Google Scholar]
- 8.Mohammad H., Matharu G., Judge A., Murray D. Comparison of 10 year outcomes of cemented and cementless unicompartmental knee replacements: data from the National Joint registry for England, Wales, Northern Ireland and Isle of Man. Acta Orthop. 2020:91. doi: 10.1080/17453674.2019.1680924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray D., Mohammad H., Matharu G. 100 B. 2018. A comparison of the outcomes of cemented and cementless oxford unicompartmental knee arthroplasty: a propensity matched cohort study of 10 836.https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.2018.12.001 (Orthopaedic Proceedings). 12. 29 September 2019. [Google Scholar]
- 10.Pandit H., Campi S., Hamilton T., Dada O. Five-year experience of cementless Oxford unicompartmental knee replacement. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):694–702. doi: 10.1007/s00167-015-3879-y. [DOI] [PubMed] [Google Scholar]
- 11.No authors listed National Joint Registry: 16th Annual Report. 2019. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf [PubMed]
- 12.Aldinger P.R., Clarius M., Murray D.W., Goodfellow J.W. Medial unicompartmental knee replacement using the "Oxford Uni" meniscal bearing knee. Orthopä. 2004;33(11):1277–1283. doi: 10.1007/s00132-004-0712-6. [DOI] [PubMed] [Google Scholar]
- 13.Hamilton T., Pandit H., Lombardi A. Radiological Decision Aid to determine suitability for medial unicompartmental knee arthroplasty. development and preliminary validation. Bone Joint Lett J. 2016 Oct;98:3–10. doi: 10.1302/0301-620X.98B10.BJJ-2016-0432.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pandit H., Campi S., Hamilton T., Dada O. Five-year experience of cementless Oxford unicompartmental knee replacement. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):694–702. doi: 10.1007/s00167-015-3879-y. [DOI] [PubMed] [Google Scholar]
- 15.Blaney J., Harty H., Doran E. Five-year clinical and radiological outcomes in 257 Oxford medial unicompartmental knee arthroplasties. The bone and joint journal. 2017;4 doi: 10.1302/0301-620X.99B5.BJJ-2016-0760.R1. [DOI] [PubMed] [Google Scholar]
- 16.Takahashi T., Pandit H.G. Unicompartmental Knee Replacement. Journal of Arthroscopy and Joint Surgery. 2017;4(2):55–60. [Google Scholar]
- 17.Murray D., Liddle D., Dodd C., Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty? Bone Joint Lett J. 2015;97-B(10 Suppl A):3–8. doi: 10.1302/0301-620X.97B10.36542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lombardi A., Kolich M., Berend K., Morris M., Crawford D., Adams J. Revision of unicompartmental knee arthroplasty to total knee arthroplasty: is it as good as a primary result? J Arthroplasty. 2018 Jul;33(7S):S105–S108. doi: 10.1016/j.arth.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 19.Seeger J.B., Haas D., Jager S., Rohner E. Extended sagittal saw cut significantly reduces fracture load in cementless unicompartmental knee arthroplasty compared to cemented tibia plateaus: an experimental cadaver study. Knee Surg Sports Traumatol Arthrosc. 2015;20:1087–1091. doi: 10.1007/s00167-011-1698-3. [DOI] [PubMed] [Google Scholar]
- 20.Liddle A., Pandit H., O’brien S., Doran E. Cementless fixation in oxford unicompartmental knee replacement. A multicentre study of 1000 knees. Bone Joint Lett J. 2013;95-B doi: 10.1302/0301-620X.95B2.30411. [DOI] [PubMed] [Google Scholar]