Abstract
Background
Severe radiocapitellar pathologies represent a unique problem in the pediatric population, as radial head excision can lead to substantial long-term complications. We present a case series of four pediatric patients treated by a novel technique—radial head excision followed by Achilles allograft interposition arthroplasty.
Methods
Four children (ages 12–15 years) are described. Their clinical and radiographic outcomes were assessed by a visual analog scale, the Mayo Elbow Performance Score, the Disabilities of the Arm, Shoulder and Hand questionnaire, grip strength, and range of motion.
Results
At a mean follow-up of two years, the average flexion-extension arc of motion improved from 107° to 131°, and the rotation arc improved from 100° to 154°. The average visual analog scale, Mayo Elbow Performance Score, and Disabilities of the Arm, Shoulder and Hand scores were 2, 92.5, and 11.5, respectively. Two patients required subsequent additional procedures—manipulation under anesthesia and ulnar shortening osteotomy. Proximal migration of the radius was observed in three out of the four patients.
Discussion
Combined radial head excision and Achilles allograft interposition arthroplasty represents a viable option for the treatment of chronic pediatric radiocapitellar pathologies, with good results in terms of clinical and functional outcomes as well as patient satisfaction in the short-medium term.
Keywords: radial head excision, radial head resection, radiocapitellar joint, Achilles interposition, congenital radial head dislocation
Introduction
The radiocapitellar joint is known for its susceptibility to trauma or chondropathies involving its articular surface, which may eventually lead to limited function, reduced range of motion (ROM), and pain.1,2 The quest for the most suitable treatment for radiocapitellar pathologies is ongoing. The classic surgical solution is radial head excision, which results in pain reduction in most cases, but impaired elbow stability. It is a suitable solution when there are no associated ligamentous injuries causing elbow instability,3 otherwise it may cause impingement of the lateral collateral ligament,4 rotatory instability,5 movement restriction,6 future arthritis possibly due to increased load on the coronoid,7 and proximal migration of the radius leading to wrist pain and limited elbow and wrist ROM, such as in an Essex-Lopresti lesion.8,9
To address these problems, Morrey and Schneeberger introduced the anconeus interposition arthroplasty technique.10 Ozsoy et al. described the use of that technique combined with repair of the medial and lateral structures for the treatment of acute elbow trauma with unreconstructed radial head fractures.11 Radial head excision followed by interposition of the anconeus muscle was shown to have the ability to alleviate pain and improve clinical function,10,12,13 but with the limitations of not providing much stability against valgus stress or proximal migration of the radius, and a substantial rate of re-operations.12
Radial head arthroplasty following radial head excision is another viable option, which has been shown to have acceptable results.14 However, the use of arthroplasty in patients with damaged capitellar articular surface, marked proximal radius bone loss, or inability to obtain adequate tracking of the implant over the capitellum at the time of surgery might be problematic and is contraindicated in some cases.12 Radiocapitellar prosthetic arthroplasty, which involves radial head arthroplasty with a polyethylene articulating surface, combined with metallic capitellar resurfacing arthroplasty attempts to address some of these problems, while restoring elbow kinematics.15 A recent study showed good midterm outcome in 15 adults,16 but clinical data are still scarce,17 and both the revision and re-operation rates were quite high.16
There is paucity of data on the ways to deal with similar issues in the pediatric population. The use of radial head excision is usually avoided in this group due to concerns regarding the development of early joint arthrosis, cubitus valgus, limited rotation, and wrist deformity.18,19 There are only few published articles reporting results of radial head excision in the pediatric population, and the most recent ones usually used some sort of interposition to reduce possible late sequel—Hresko et al. sutured the capsule over the proximal radial stump as an interposition graft;20 and Wegmann et al. used anconeus muscle interposition.21
The use of radial head prostheses in children is somewhat more problematic since erroneous estimations of the size of an implant might require further surgeries, as emphasized by Duckworth et al.22 Moreover, there are no “off-the-shelf” radial head products that fit the pediatric population and that provide future solutions for the growing child. To our knowledge, there is no published data on radial head replacement or radiocapitellar prosthetic arthroplasty in children.
The complexity of treatment and the outcomes in this setting motivated the search for “outside-the-box” therapeutic methods in an attempt to address the radio capitellar space, following radial head excision. Ramazanian et al. recently described a technique of radiocapitellar Achilles allograft disc arthroplasty following radial head excision, which has been shown to reduce the contact pressure in the lateral coronoid in vitro.7
Following the limited success of the anconeus interposition and in search for alternative solutions intended for the pediatric population, we have been implementing the surgical technique of radial head excision followed by an interposition arthroplasty with an Achilles allograft interposition arthroplasty (AAIA). In this case series, we present the outcomes of a cohort of four pediatric patients treated with this technique.
Materials and methods
After obtaining the approval of our institutional review board, the medical charts, operative notes, and radiographic records of four pediatric patients who underwent AAIA for symptomatic elbow pain and dysfunction related to radiocapitellar pathologies at our tertiary care referral center were reviewed. Only patients who failed conservative treatment were offered an AAIA procedure.
The mechanism for radiocapitellar pathology in our patients was post traumatic in three and congenital in one:
Patient #1 (Table 1) presented with chronic posterior dislocation of the radial head, limiting elbow ROM. Elbow radiographs showed 40° angular deformity at the radial neck (Figure 1). He had a rheumatologic workup for a possible inflammatory process, and the results failed to show any pathological findings.
Table 1.
Patient demographics and outcome following AAIA.
| Case | Sex, Age (y) | Pre-operative diagnosis | Side | Dominant hand | Open radial head physis | Time between injury and treatment (mo) | Follow-up (mo) | Subsequent intervention | Postoperative proximal migration of the radius |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M, 12 | Congenital radial head subluxation | R | Yes | Yes | - | 25 | -MUA | No |
| 2 | F, 12 | Prior Monteggia fracture | R | Yes | Yes | 60 | 25 | Ulnar- shortening osteotomy | Yes |
| 3 | M, 14 | Prior supracondylar fracture | L | No | Yes | 114 | 23 | Yes | |
| 4 | M, 15 | Prior Monteggia fracture | R | Yes | No | 13 | 20 | Yes |
AAIA: Achilles allograft interposition arthroplasty; M: male; F: female; R: right; L: left; MUA: manipulation under general anesthesia; Ext: extension; Flex: flexion; Pron: pronation; Sup: supination; VAS: visual analog scale; MEPS: the Mayo Elbow Performance Score; DASH: the Disabilities of the Arm, Shoulder and Hand questionnaire.
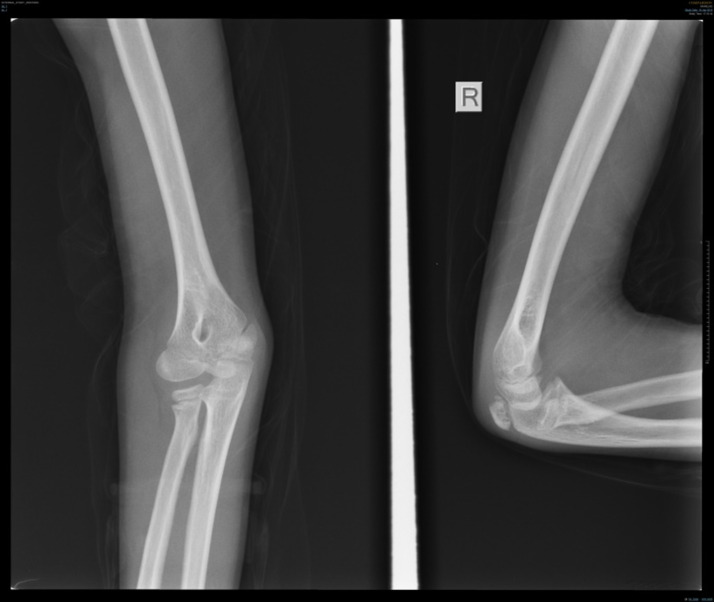
Figure 1.
Anteroposterior and lateral views of the right elbow (patient #1) showing radial head angulation of 40°, posterior dislocation of the radial head, and partial obliteration of the proximal radius growth plate.
Patients #2 and #4 were originally treated for olecranon fractures, which eventually turned out to be misdiagnosed Monteggia fracture dislocations: Patient #2 was originally treated conservatively with a splint, but was later found to have had a 20° angulated radial neck fracture and a non-displaced coronoid fracture. She presented to our clinic 4.5 years after the injury due to gradually increasing elbow pain. Patient #4 had an open reduction and internal fixation of an olecranon fracture by means of a tension band wiring technique. He presented four months later complaining of gross clicking during elbow motion, and physical and radiographic examination revealed anterior subluxation of the radial head during pronation.
Patient #3 presented eight years following a supracondylar elbow fracture that was treated surgically by closed reduction and percutaneous pinning. He complained of elbow pain, clicking and locking which happened on a daily basis.
The patients were interviewed and clinically assessed by an independent reviewer (SF). Grip strength was measured by the Jamar hydraulic hand dynamometer,23 and ROM was measured by a goniometer.24 Pre-operative and follow-up radiographs were reviewed for the assessment of degenerative changes and heterotopic ossification.25 Proximal migration of the radius was assessed comparing radiographs of both wrists at final follow-up.
Subjective outcomes were assessed by self-report scales, including the Disabilities of the Arm, Shoulder and Hand (DASH: best possible score = 0 points, worst possible score = 100 points) Questionnaire for upper-extremity disability, and a visual analogue scale (VAS score, range 0–10) for pain.26,27 An elbow impairment and functional index, the Mayo Elbow Performance Score (MEPS: range 0–100) was calculated as well.28
Surgical technique
After undergoing general anesthesia, the patients were placed supine on the operating table, prophylactic intravenous antibiotics were administered, and a sterile tourniquet was applied on the operated arm. A midline posterior elbow incision was made just lateral to the tip of the olecranon, and a full-thickness lateral fasciocutaneous flap was elevated on the deep fascia. Deep dissection to expose the radial head was carried out by means of an extensor digitorum communis splitting approach.29,30 Care was taken to keep the forearm pronated, to protect the posterior interosseous nerve, and to ensure that the dissection remained anterior to the lateral ulnar collateral ligament in order to prevent iatrogenic posterolateral rotatory instability.31 The humeral origin of the radial collateral ligament and the overlying extensor muscles were elevated anteriorly off the lateral epicondyle.
Following exposure, the senior surgeon assessed the congruency of the radiocapitellar and proximal radio-ulnar joints, and the quality of the cartilage covering the articular surface, to determine whether the radial head could be salvaged. In cases where the radial head was unsalvageable (Figure 2), it was excised as proximally as possible, usually at the radial head and neck junction. Debridement of synovitis and loose bodies removal from the elbow, as well as contracture release were performed as needed.
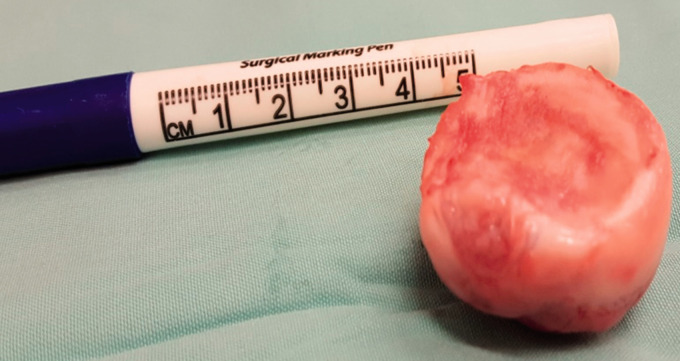
Figure 2.
A deformed dysplastic radial head (patient #2) demonstrating significant cartilage loss on all articular surfaces.
An Achilles allograft interposition was carried out according to the technique described by Ramazanian et al.7 Briefly, a portion of an Achilles tendon allograft was folded upon itself and contoured to a pocket-shaped piece of tissue (Figure 3). A suture anchor was placed at the equator of the distal border of the lesser sigmoid notch (LSN) of the ulna. Two #0 Vicryl sutures were placed at either side of the attachments of the annular ligament to the LSN and prepared for later use. The two suture limbs of the suture anchor were passed through the base of the pocket-shaped allograft, and the latter was shuttled to its position in the LSN by means of a sliding knot technique. The allograft was then secured by #0 Vicryl sutures such that it could serve as an unlinked spacer between the radial neck and capitellum (Figure 4).
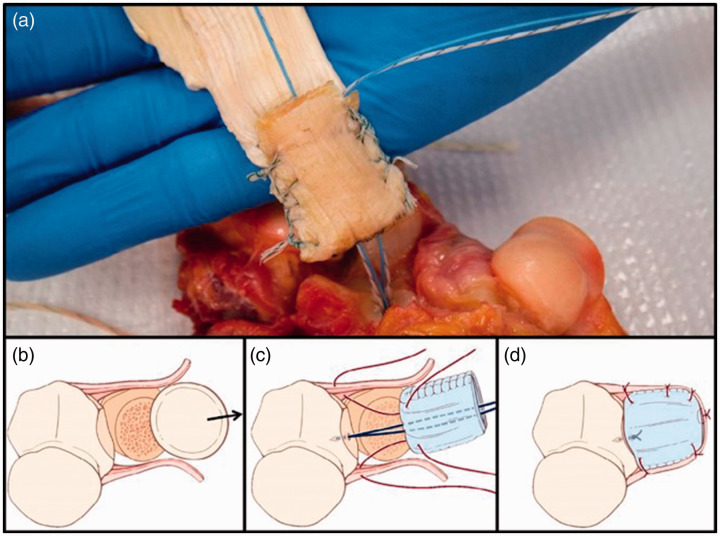
Figure 3.
Preparation of the Achilles tendon graft, and illustration of the axial views of the Achilles allograft interposition arthroplasty surgical technique. (a) The thick distal portion of the tendon was folded on itself and sutured along both sides, creating a pocket-shaped tissue “disc”. (b) After the annular ligament was cut and the radial head was excised, a 4.5-mm anchor was placed into the middle of the radial notch of the ulna. (c) A No. 2 FiberWire (Arthrex) suture was passed through the folded edged of the graft, and the graft was pulled down into position and tied into place. (d) The graft was sutured to the anterior and posterior annular ligament, and the annular ligament was repaired. From Ramazanian et al.7 Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved.
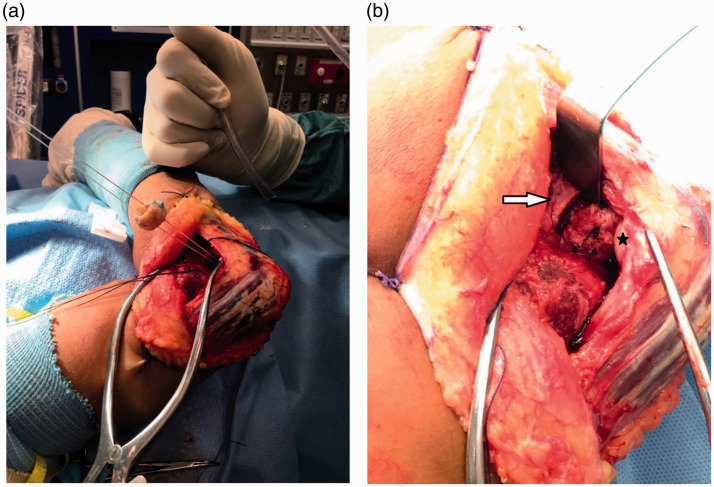
Figure 4.
Two suture limbs of the suture anchor were passed through the base of the pocket-shaped allograft (a), and the latter was shuttled to its position in the lesser sigmoid notch by means of a sliding knot technique. The allograft serves as an unlinked spacer between the radial neck (white arrow) and the capitellum (black asterisk) (b).
At the end of the procedure, the annular ligament was repaired, and the muscle interval that was used for exposure was closed. Elbow stability was assessed both visually and under image intensifier. Active motion was initiated on the first postoperative day, and a static progressive extension splint was constructed for nighttime use. Strengthening and stretching exercises were usually initiated around 6–12 weeks postoperatively. Two of the four patients were given indomethacin 75 mg for three weeks to prevent heterotopic ossification.
Results
None of the patients was lost to follow-up. There were three males and one female with a mean age of 13 years (range 12 to 15 years) at the time of surgery. Three of the patients had an open radial head physis at the time of surgery. The dominant arm was involved in three of the patients. The AAIA was performed at 13, 60, and 114 months following the original injury in the three post traumatic cases. All the patients reported pain, crepitus, limited ROM, and limb weakness prior to surgery. The patients were reviewed after an average of 23 months following the procedure (range 20 to 25 months).
Pre-operative ROM of the injured elbows averaged 118° of flexion (range 90°–135°), fixed flexion deformity of 12° (range 0°–20° of extension), pronation of 57° (range 0°–80°), and supination of 50° (range 0°–70°). Postoperative ROM of the injured elbows averaged 136° of flextion (range 130°–140°), fixed flexion deformity of 5° (range 0°–15°), pronation of 83° (range 80°–90°), and supination of 42.5° (range 30°–70°). The flexion-extension arc of motion improved by 24° on average, and the rotatory arc of motion improved by 54°. At final follow-up, the average DASH score was 11.5 points (range 0–44.6); the average MEPS score was 92.5 points (range 70–100); and the average VAS score was 2 (range 0–7). Patient demographics and outcome following the AAIA, as well as differences between the affected and unaffected elbows at final follow-up, are presented in Tables 1 and 2, respectively.
Table 2.
Differences between the affected and unaffected elbows at the final follow-up.
| Case 1 | Case 2 | Case 3 | Case 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Movement | Affected | Unaffected | Affected | Unaffected | Affected | Unaffected | Affected | Unaffected |
| Extension (°) | 5.0 | 0.0 | 0.0 | 0.0 | 15.0 | 0.0 | 5.0 | 5.0 |
| Flexion (°) | 140.0 | 140.0 | 140.0 | 140.0 | 130.0 | 140.0 | 145.0 | 135.0 |
| Supination (°) | 70.0 | 70.0 | 30.0 | 85.0 | 80.0 | 80.0 | 70.0 | 85.0 |
| Pronation (°) | 90.0 | 90.0 | 85.0 | 85.0 | 80.0 | 80.0 | 80.0 | 80.0 |
| Pinch strength (kg) | 7.0 | 7.0 | 13.0 | 13.0 | 17.0 | 22.0 | 16.0 | 17.0 |
| Grip strength (kg) | 30.0 | 20.0 | 23.0 | 14.0 | 28.0 | 40.0 | 25.0 | 32.0 |
X-rays taken at the final follow-up showed evidence of proximal migration of the radius in three of four patients (Table 1). None of the elbows developed heterotopic ossification. Only one patient (patient #3) had medial and lateral osteophytes which were present prior to the AAIA and did not change. No signs of elbow arthrosis were found in the other patients.
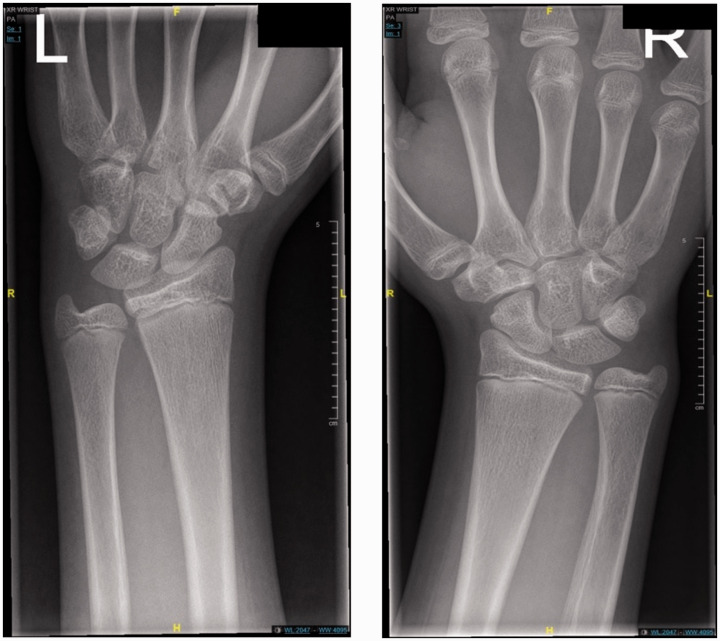
One patient (patient #1) showed only minimal and slow postoperative improvement in ROM despite intensive therapy program, and eventually underwent a closed manipulation under general anesthesia six weeks following the AAIA, with excellent final results. Another patient (patient #2) had persistent and increasing wrist pain following the AAIA, with radiographic evidence of proximal migration of the radius (Figure 5). She underwent diagnostic wrist arthroscopy followed by ulnar shortening osteotomy 12 months after the AAIA. At the final follow-up, she showed fair functional results and persistent wrist pain.
Figure 5.
Posteroanterior X-ray views of the left (a) and right (b) wrists of patient #2 at one year following an AAIA. Note the proximal migration of the radius on the right with a positive ulnar variance.
Discussion
In this study, we present a case series of four pediatric patients with chronic radiocapitellar pathologies who underwent surgical treatment by a novel technique: excision of the radial head followed by Achilles allograft interposition arthroplasty. After two years of follow-up, three of the four patients displayed excellent clinical outcome with improved ROM, pain, and strength. One patient needed an additional surgical procedure. Of concern, three of the four patients showed radiographic proximal migration of the radius following the procedure, making them prone to future wrist pain.
Elbow pain, weakness, and loss of motion due to radiocapitellar pathologies are difficult to manage. Restoration of the exact anatomy of the proximal radius and its anatomical relations with the capitellum and proximal ulna is still challenging. The literature regarding radial head excision in the pediatric population includes exclusively small case series, with heterogeneity in ages, physial status, and duration of follow-up, limiting the ability to compare the outcomes of different surgical procedures. Currently, there is no consistently reliable solution for the treatment of chronic radiocapitellar joint pathology in the pediatric population.
Most publications regarding radial head excision for the treatment of congenital radial head dislocation demonstrated improvement in pain and cosmetics, but only limited improvement in ROM, mainly rotatory:
Bell et al. presented 12 cases of radial head excision in 10 patients. Most of them were skeletally mature (ages 12–24, average 16). Most of the patients had improved pain and cosmetics following surgery, with no consistent change in ROM;32 Mardam-Bey and Ger presented seven cases (only one was skeletally immature), with improved pain and cosmetics following radial head excision but no improvement in ROM;33 Bengard et al. showed mild improvement (19°) in the rotatory arc of motion of 15 elbows (10 patients, ages 12–18) 10 years following excision of congenitally dislocated radial head;34 Campbell et al., on the other hand, showed significant improvement of 53° in the rotatory arc of motion of eight elbows (6 patients aged 10 to 15.5 years) treated with the same procedure for the same pathology.35 In our series, there was only one patient with congenital radial head dislocation (patient #1), whose ROM significantly improved following AAIA both in flexion-extension (65°) as well as rotation (160°). This was probably related to his severely deformed radial head, which caused significant pre-operative elbow stiffness.
Reports about radial head excision for the treatment of post traumatic changes in the pediatric population are even rarer. Tibone and Stoltz published the results of pediatric patients treated for radial head fracture. Tree patients, aged 11, 12, and 14, underwent late radial head excision, one of them following attempted ORIF. All three patients had poor final results.36 Our series include three post traumatic cases (patients #2–4) whose ROM almost normalized following surgery.
In the largest series published thus far, Hresko et al.20 presented the results of 27 excised radial heads in 25 patients aged 4.6–18 years (average 14). The indications for surgery were congenital\developmental in 13 patients, and post traumatic in 12. The surgical technique included suturing of the capsule over the radial stump as an interposition graft. After an average follow-up of seven years, the developmental group had improved ROM both for flexion-extension (15°) and rotation (29°). The post-traumatic group showed similar improvement (17° and 35°, respectively).
Recently, Wegmann et al.21 published the results of radial head excision with anconeus interposition in seven skeletally immature patients (average age 11). The indication for surgery was congenital in two cases and post traumatic in five. After a mean follow-up of four years, there was a significant improvement only in the rotatory arc of motion of about 100°. We could not find other articles reporting the results of anconeus interposition following excision of the radial head in the pediatric population.
Proximal migration of the radius (or change in wrist ulnar variance) is a serious sequel following radial head excision, leading to wrist pain and deformity. Bell et al. reported an average proximal migration of 3.4 mm in 10 out of 12 elbows seven years following the procedure;32 Bengard et al. reported an average proximal migration of 5.3 mm after 10 years;34 and Campbell et al. did not specify the magnitude of proximal migration, but noted that all their patients developed post-operative wrist pain.35 Using capsular interposition, Hresko et al. showed similar results: an average of 4.4 mm proximal migration in skeletally immature patients, and 4.1 mm in skeletally mature patients, with only 33% of patients without significant change in ulnar varience.20 Wegmann et al., using anconeus interposition, reported an average proximal migration of 3 mm after four years, while one of his young patients already developed wrist joint arthrosis.21 In our series, all three post traumatic cases showed proximal migration of the radius following the AAIA, but only one of them was clinically significant. One year after the surgery, she underwent wrist arthroscopy, which failed to show any pathological findings, combined with an ulnar shortening osteotomy. At the final follow-up, she only had partial improvement of her wrist pain, with no radiographic signs of wrist arthrosis. None of the other patients had wrist pain or gross deformity at the final follow-up, but that would have to be re-assessed at a longer term follow-up.
Another possible sequel of radial head excision is early elbow arthrosis. Only few articles reported longer term radiographic follow-up regarding this issue: Bell et al. reported 2 out of 12 (17%) cases who developed clinically significant degenerative elbow arthritis after an average of seven years, one of them already had mild arthritic changes at the time of surgery.32 Using capsule interposition, Hresko et al. reported that after a mean follow-up of 7.8 years, radiographic medial degenerative changes of the elbow were present in 18 out of 27 patients (67%), of which 44% were minimal, 19% moderate, and 4% severe.20 Wegmann et al., using anconeus interposition, reported that after a mean follow-up of four years, two out of seven patients (29%) had radiographic signs of elbow joint arthrosis.21
Achilles allograft interposition arthroplasty was designed in an attempt to address these dreaded sequels. In this procedure, the Achilles tendon allograft serves as an unlinked spacer between the radial neck and the capitellum. Given the characteristics of the tendon, it was expected to prevent proximal migration of the radius and impingement against the capitellum, postpone capitellar cartilage wear as well as elbow and wrist arthrosis. Although some proximal migration of the radius was noted in three out of the four patients in our series, it was relatively mild, with only one case of clinical significance after two years. Ramazanian et al. demonstrated in an in vitro biomechanical study that radial head excision increases the contact pressure on the coronoid, and that Achilles interposition arthroplasty improves contact pressures, bringing them to an almost normal level.7 We hope that this normalization of joint pressures will also occur in vivo, and will eventually prevent or postpone the development of early degenerative changes. That would have to be assessed in a longer term follow-up studies.
One of the major issues with radial head excision in the pediatric population is the inconsistency of outcomes, demonstrated by a double digit rate of re-operations, due to osteophytes,32 radial head re-formation,35 and proximal migration of the radius causing wrist pain and deformity.34 The use of capsular interposition failed to show better outcome, with 32% of re-operations.20 For anconeus interposition, Wegmann et al. reported no re-operations in a cohort of seven patients after four years,21 but larger studies on adult patients reported 24%12 and 22%37 re-operation rate. A larger number of cases would be needed in order to assess whether AAIA will provide better outcome.
This study is a case series of four pediatric patients who underwent an AAIA following excision of the radial head for the treatment of chronic radiocapitellar pathologies. The results in our small series were excellent in three patients and fair in one patient, in terms of clinical and functional outcome as well as patient satisfaction. At the final follow-up, three out of the four patients reported no pain, and one patient reported moderate pain. Moreover, the postoperative ROM improved in all four patients. One patient underwent a closed manipulation under general anesthesia38 six weeks following the AAIA due to slow improvement, and eventually had excellent results. Another patient had a subsequent ulnar shortening osteotomy one year following the AAIA due to proximal migration of the radius and increasing wrist pain, with only fair results at the final follow-up.
As in other small case series, this study has obvious limitations, predominantly (1) the small number of patients; (2) the relatively short follow-up; and (3) the lack of comparison with other treatment options such as radial head excision alone. Unfortunately, these limitations are inherent to the study of rare medical conditions such as this. A larger patient group and a longer follow-up would be beneficial to further assess the outcome, function, and possible complications of this promising procedure in the pediatric population.
In conclusions, the findings of the current case series suggest that radial head excision followed by AAIA is a viable and safe treatment option for children with painful restricted elbows originating from radiocapitellar pathologies where the radial head is unsalvageable.
Footnotes
Contributorship: SF wrote the first draft of the manuscript. DR helped with obtaining patient data and patient examination, and wrote the revision. RA helped with obtaining patient data. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: IRB aproval 0585-18-TLV.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patients for their anonymized information to be published in this article
ORCID iD: Dani Rotman https://orcid.org/0000-0003-4013-0152
References
- 1.Kaas L, van Riet RP, Vroemen JP, et al. The incidence of associated fractures of the upper limb in fractures of the radial head. Strategies Trauma Limb Reconstr 2008; 3: 71–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nalbantoglu U, Gereli A, Kocaoglu B, et al. Capitellar cartilage injuries concomitant with radial head fractures. J Hand Surg Am 2008; 33: 1602–1607. [DOI] [PubMed] [Google Scholar]
- 3.Lopiz Y, Gonzalez A, Garcia-Fernandez C, et al. Comminuted fractures of the radial head: resection or prosthesis? Injury 2016; 47: S29–S34. [DOI] [PubMed] [Google Scholar]
- 4.Johnson JA, Beingessner DM, Gordon KD, et al. Kinematics and stability of the fractured and implant-reconstructed radial head. J Shoulder Elbow Surg 2005; 14: 195S–201S. [DOI] [PubMed] [Google Scholar]
- 5.Hall JA, McKee MD. Posterolateral rotatory instability of the elbow following radial head resection. J Bone Joint Surg Am 2005; 87: 1571–1579. [DOI] [PubMed] [Google Scholar]
- 6.Ikeda M, Sugiyama K, Kang C, et al. Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Joint Surg Am 2005; 87: 76–84. [DOI] [PubMed] [Google Scholar]
- 7.Ramazanian T, Muller-Lebschi JA, Chuang MY, et al. Effect of radiocapitellar Achilles disc arthroplasty on coronoid and capitellar contact pressures after radial head excision. J Shoulder Elbow Surg 2018; 27: 1785–1791. [DOI] [PubMed] [Google Scholar]
- 8.Hergenroeder PT, Gelberman RH. Distal radioulnar joint subluxation secondary to excision of the radial head. Orthopedics 1980; 3: 649–650. [DOI] [PubMed] [Google Scholar]
- 9.Mikic ZD, Vukadinovic SM. Late results in fractures of the radial head treated by excision. Clin Orthop Relat Res 1983; 181: 220–228. [PubMed] [Google Scholar]
- 10.Morrey BF, Schneeberger AG. Anconeus arthroplasty: a new technique for reconstruction of the radiocapitellar and/or proximal radioulnar joint. J Bone Joint Surg Am 2002; 84: 1960–1969. [PubMed] [Google Scholar]
- 11.Ozsoy MH, Isik M, Sakaogullari A, et al. Anconeus interposition arthroplasty in acute multiligamentous elbow injuries with irreparable radial head fractures: a novel approach. Acta Orthop Traumatol Turc 2016; 50: 303–308. [DOI] [PubMed] [Google Scholar]
- 12.Baghdadi YM, Morrey BF, Sanchez-Sotelo J. Anconeus interposition arthroplasty: mid- to long-term results. Clin Orthop Relat Res 2014; 472: 2151–2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishida K, Iwasaki N, Funakoshi T, et al. Prevention of instability of the proximal end of the radius after radial head resection using an anconeus muscle flap. Hand Surg 2012; 17: 25–31. [DOI] [PubMed] [Google Scholar]
- 14.Monica JT, Mudgal CS. Radial head arthroplasty. Hand Clin 2010; 26: 403–410, vii. [DOI] [PubMed] [Google Scholar]
- 15.Sabo MT, Shannon H, De Luce S, et al. Elbow kinematics after radiocapitellar arthroplasty. J Hand Surg Am 2012; 37: 1024–1032. [DOI] [PubMed] [Google Scholar]
- 16.Spross C, Jak W, van Riet RP. Radiocapitellar arthroplasty: a consecutive case series with 2 to 6 years' follow-up. J Shoulder Elbow Surg 2019; 28: 131–136. [DOI] [PubMed] [Google Scholar]
- 17.Heijink A, Morrey BF, Eygendaal D. Radiocapitellar prosthetic arthroplasty: a report of 6 cases and review of the literature. J Shoulder Elbow Surg 2014; 23: 843–849. [DOI] [PubMed] [Google Scholar]
- 18.Ibrahim S. Tachdjian's pediatric orthopaedics: from the Texas Scottish Rite Hospital for Children. Malays Orthop J 2015; 9: 53–53. [Google Scholar]
- 19.Herndon JH, Williams JJ, Weidman CD. Radial growth and function of the forearm after excision of the radial head. A study of growing macaque monkeys. J Bone Joint Surg Am 1990; 72: 736–741. [PubMed] [Google Scholar]
- 20.Hresko MT, Rosenberg BN, Pappas AM. Excision of the radial head in patients younger than 18 years. J Pediatr Orthop 1999; 19: 106–113. [PubMed] [Google Scholar]
- 21.Wegmann H, Heider S, Novak M, et al. Outcome following excision of the radial head in children with open physes for impaired elbow motion. J Shoulder Elbow Surg 2019; 28: 525–529. [DOI] [PubMed] [Google Scholar]
- 22.Duckworth AD, Wickramasinghe NR, Clement ND, et al. Radial head replacement for acute complex fractures: what are the rate and risks factors for revision or removal? Clin Orthop Relat Res 2014; 472: 2136–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mathiowetz V, Weber K, Volland G, et al. Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am 1984; 9: 222–226. [DOI] [PubMed] [Google Scholar]
- 24.Chapleau J, Canet F, Petit Y, et al. Validity of goniometric elbow measurements: comparative study with a radiographic method. Clin Orthop Relat Res 2011; 469: 3134–3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petscavage JM, Ha AS, Chew FS. Radiologic review of total elbow, radial head, and capitellar resurfacing arthroplasty. Radiographics 2012; 32: 129–149. [DOI] [PubMed] [Google Scholar]
- 26.Beaton DE, Katz JN, Fossel AH, et al. Measuring the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther 2001; 14: 128–146. [PubMed] [Google Scholar]
- 27.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain 1986; 27: 117–126. [DOI] [PubMed] [Google Scholar]
- 28.Morrey BF, Sanchez-Sotelo J and Morrey ME. Morrey's the elbow and its disorders. 5th ed. Philadelphia, PA: Elsevier, 2018.
- 29.Desloges W, Louati H, Papp SR, et al. Objective analysis of lateral elbow exposure with the extensor digitorum communis split compared with the Kocher interval. J Bone Joint Surg Am 2014; 96: 387–393. [DOI] [PubMed] [Google Scholar]
- 30.Wolfe SW, Hotchkiss RN, Pederson WC, et al. Green's operative hand surgery. In: ClinicalKey. 7th ed. Philadelphia, PA: Elsevier, 2017, p. 1.
- 31.Schimizzi A, MacLennan A, Meier KM, et al. Defining a safe zone of dissection during the extensor digitorum communis splitting approach to the proximal radius and forearm: an anatomic study. J Hand Surg Am 2009; 34: 1252–1255. [DOI] [PubMed] [Google Scholar]
- 32.Bell SN, Morrey BF, Bianco AJ, Jr. Chronic posterior subluxation and dislocation of the radial head. J Bone Joint Surg Am 1991; 73: 392–396. [PubMed] [Google Scholar]
- 33.Mardam-Bey T, Ger E. Congenital radial head dislocation. J Hand Surg Am 1979; 4: 316–320. [DOI] [PubMed] [Google Scholar]
- 34.Bengard MJ, Calfee RP, Steffen JA, et al. Intermediate-term to long-term outcome of surgically and nonsurgically treated congenital, isolated radial head dislocation. J Hand Surg Am 2012; 37: 2495–2501. [DOI] [PubMed] [Google Scholar]
- 35.Campbell CC, Waters PM, Emans JB. Excision of the radial head for congenital dislocation. J Bone Joint Surg Am 1992; 74: 726–733. [PubMed] [Google Scholar]
- 36.Tibone JE, Stoltz M. Fractures of the radial head and neck in children. J Bone Joint Surg Am 1981; 63: 100–106. [PubMed] [Google Scholar]
- 37.Rahmi H, Neumann JA, Klein C, et al. Clinical outcomes of anconeus interposition arthroplasty after radial head resection in native and prosthetic radial heads. J Shoulder Elbow Surg 2018; 27: S29–S34. [DOI] [PubMed] [Google Scholar]
- 38.Rotman D, Factor S, Schermann H, et al. Manipulation under anesthesia for the postsurgical stiff elbow: a case series and review of literature. Eur J Orthop Surg Traumatol 2019; 29: 1679–1685. [DOI] [PubMed] [Google Scholar]