Abstract
Background
The primary aim of this study is to determine the accuracy of CT scanning when evaluating non-union of the clavicle.
Methods
A retrospective review was performed of all CT scans undertaken for suspected nonunion of midshaft clavicle fractures over a 10-year period. The influence of scan timing, callus and patient characteristics was evaluated.
Results
One hundred eighty-four CT scans were analysed. No patient was incorrectly diagnosed with union (n = 85). Ninety-nine scans were reported as non-union with inadequate bridging callus, 19 of which were united at operation or on repeat CT imaging and represented delayed unions. Atrophic callus was found in 57 patients and all of which had a confirmed non-union (positive predictive value 100%). A hypertrophic callus was found in 42 patients, all of the delayed unions were found in this group (positive predictive value for non-union 55%, p < 0.001). CT compared to radiographs showed greater inter-observer agreement for union (weighted kappa 0.75 vs. 0.50 respectively). Overall, CT is 100% sensitive and 81.7% specific for non-union diagnosis.
Discussion
CT has excellent accuracy to determine clavicle union but approximately one in five suspected non-unions went onto unite. Hypertrophic callus finding resulted in a delayed union in approximately half of the cases in our study.
Keywords: Clavicle, CT, non-union
Background
Displaced midshaft clavicle fractures result in non-union in approximately 15% of cases following non-operative management and this is thought to significantly impair patient outcome.1–5 In these recent clinical trials, non-union of the clavicle is generally accepted as lack of radiological and clinical union at six months post-injury.1–5 Conversely a delayed union can be considered as fracture union that occurs beyond six months. Diagnosis of a clavicle non-union is based on ongoing pain in the presence of clinical features such as fracture mobility, tenderness on palpation and absent bridging callus on radiograph.6
Pain following a clavicle fracture may be caused by neurogenic plexus irritation or concurrent shoulder pathology, such as adhesive capsulitis, and may be falsely attributed to a non-union without due consideration on clinical examination.7,8 Judgement of radiological union requires interpretation of bridging callus on radiograph which can be subjective between observers. For most fractures this can be improved with orthogonal views for callus evaluation (e.g. tibia9) but this is challenging with the clavicle.
CT scanning provides high resolution multi-planar imaging of fractures which can be used to determine union by evidence of bridging callus. Although the popularity of CT for fracture healing evaluation has increased, the advantage over radiographs for decision making is contested and there is a risk of overdiagnosis of non-union.10 When used to evaluate tibia union following intramedullary fixation, it was estimated to have a non-union sensitivity of 100% but a specificity of 62%. Although no cases of non-union were missed, the lack of specificity resulted in over diagnosis of non-union and unnecessary operations for perceived inadequate healing.11
The use of CT scanning for the evaluation of midshaft clavicle fracture non-union has not been previously investigated. It would be useful to know if CT scans improve decision making over radiographs with regards to non-union diagnosis and if there are patient or scan factors that influence the accuracy.
The primary aim of this study is to determine the accuracy of CT scanning when evaluating non-union of the clavicle. The secondary aim is to evaluate whether CT scans compared to plain radiographs result in better agreement between blinded observers for fracture healing decision making.
Materials and methods
A consecutive series of patients who underwent CT scanning of a midshaft clavicle fracture to confirm or refute non-union were retrospectively reviewed. These were identified from a locally held radiological database (2007 to 2017). Inclusion criteria were all midshaft displaced Robinson type 2 fractures12 (AO/OTA 15.2) that underwent a CT scan to confirm the clinical suspicion of non-union following conservative management or post-fixation. Exclusion criteria were lateral end clavicle fractures or those without follow-up post CT scan to determine outcome.
CT scans following conservative management were undertaken in patients with pain, examination findings in keeping with non-union and equivocal radiographs for bridging callus. Post-fixation CT scans were exclusively following open reduction and plate fixation for acute fractures, intra-medullary devices were not used in the study centre. Non-union suspicion following fixation was based on ongoing pain at fracture site with a persistent fracture line on radiograph without clear bridging callus. At the time of operative intervention for a perceived non-union, all patients were over six months from injury, or initial acute fixation.
Clinical data relating to the injury, index procedure and subsequent follow-up was collected electronically using the study centres electronic TRAK Care™ (InterSystems Corp, Cambridge, MA) system. Radiographs were reviewed using Carestream Picture Archiving and Communication System (PACS) system (Carestream Health, USA) for fixation strategy and classification by the primary author.
Definition of non-union and delayed union
A suspected non-union was diagnosed on CT by the absence of bridging callus of 50% cortical diameter across the fracture. It was deemed atrophic if there was sclerosis, minimal callus formation and/or re-absorption of the fracture site. Hypertrophic non-union was based on new bone formation extending out with the cortical surface but with a persistent fracture line without bridging (Figure 1). In patients diagnosed with a non-union, this was assumed to be correct if a mobile non-union was confirmed at time of operation or if they declined operative fixation with no further radiographic evidence of union, i.e. a presumed fibrous non-union. Incorrect diagnosis of non-union was defined as cases where the fracture was found to be united at time of operation or if patients declined operative fixation and the fracture was later found to be united on subsequent CT imaging. This suggested a false positive diagnosis of non-union on the initial CT and therefore more likely represented a delayed union.
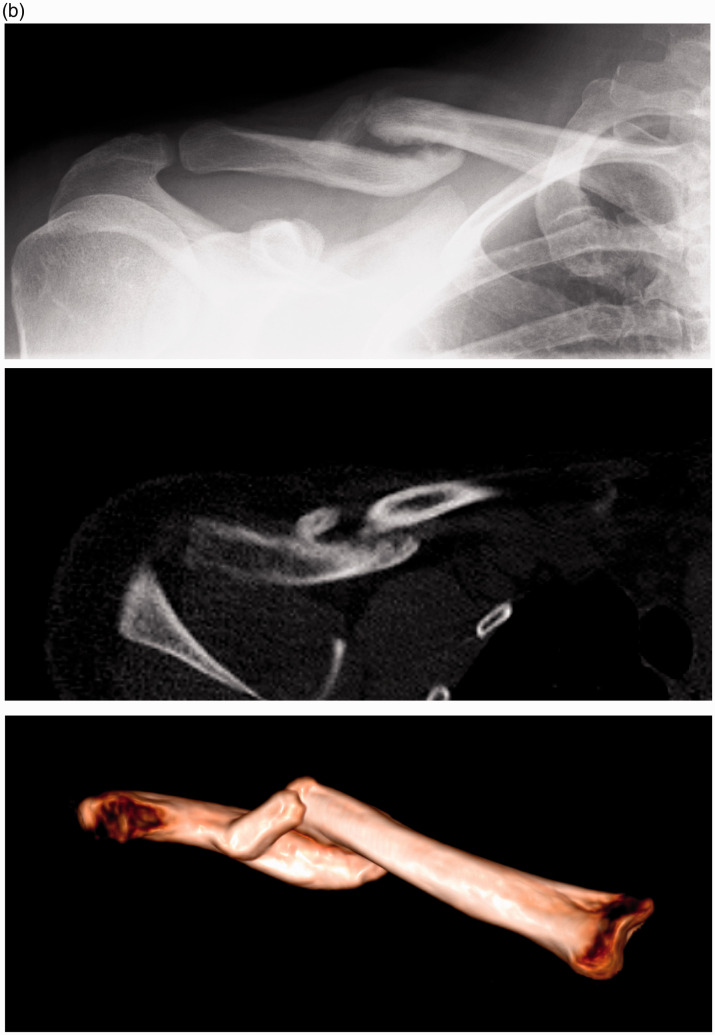
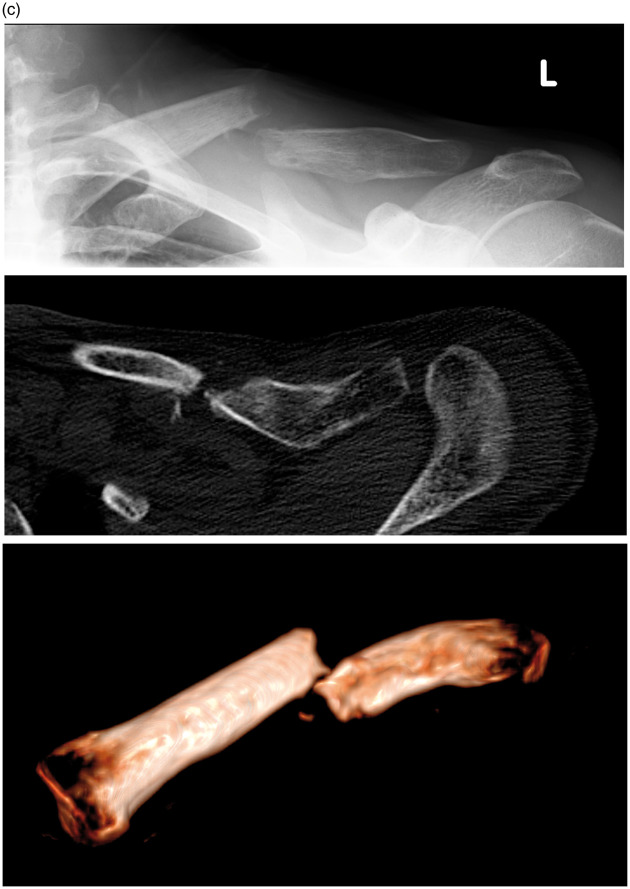
Figure 1.
Examples of callus grading from three patients following non-operative management at six months post-injury. Radiograph, axial CT and 3D reconstruction CT taken within one month. (a) Bridging callus formation and union. (b) Hypertrophic non-union. (c) Atrophic non-union.
A correct union diagnosis was assumed if they were discharged following scan with resolution of symptoms, did not represent at a later date with an incorrect diagnosis or undergo further imaging within our national PACS imaging system.
CT reporting was performed by a musculoskeletal consultant radiologist at the time of the investigation and was retrospectively reviewed. The type of callus was taken from the radiology report and cross checked by the main author who is a senior Orthopaedic registrar and reviewed all of the CT scans for accuracy. Any discrepancies between the radiology report and main author were reviewed by the senior author who is a consultant upper limb trauma surgeon.
Reviewer agreement of CT versus radiograph to determine union
To determine if CT has an advantage over radiographs for decision making with regard to clavicle fracture healing, a series of 40 patient scans were evaluated. Two of the authors who are both senior Orthopaedic registrars reviewed 40 patient scans. Radiographs and CT scans that were performed within 30 days of each other were identified from the database and a random selection was chosen. The reviewers were not involved in any of the patients’ routine medical care. Reviewers were blinded to the diagnosis, previous reports and subsequent clinical course. Radiographs and CTs were viewed independently of each other to avoid bias of comparison between images. Bridging callus evaluation was based principally on the axial imaging of the fracture, but other image orientations or 3D reconstructions were permitted if equivocal. Weighted kappa was used to determine the inter-observer agreement between radiographs and CT. Strength of association was considered as 1.0–0.8 very strong, 0.8–0.6 strong and 0.6–0.4 fair.13
Statistical analysis
Statistical analysis was performed using SPSS version 24 (Chicago, IL). Data was tested for normal distribution with the D’Agostino and Pearson test. Linear variables were assessed using the Student t test for parametric data or the Mann–Whitney U test for nonparametric data. Differences between dichotomous data were assessed using the chi-square test and odds ratio (OR). Multiple risk factor covariates for adverse outcomes were analysed with binary logistic regression to determine the relationship and interaction. A p value of < 0.05 was defined as statistically significant.
Ethics and source of funding
Access to patient notes was acquired through the local Caldicott guardian and registration with musculoskeletal audit department. Formal ethical approval was not required after seeking advice from our local ethics committee.
Results
During the study period 1079 displaced midshaft clavicle fractures presented to our unit. Two hundred eighty-three CT scans were undertaken to confirm or refute the clinical suspicion of clavicle non-union met the inclusion criteria. Ninety-nine scans were undertaken for lateral end fractures (Robinson 3) and were excluded.
One hundred eighty-four CT scans were analysed, most were following conservative management (n = 139) and the remainder following acute plate fixation (n = 45). CT scans were undertaken at a median of 174 days following injury (or operation date; range 96–322 days). Approximately half were performed prior to six months (n = 103; Figure 2). There were 130 males (70.7%), 44 smokers (23.9%) and the mean age was 44.5 years (SD 22, range 17–87 years).
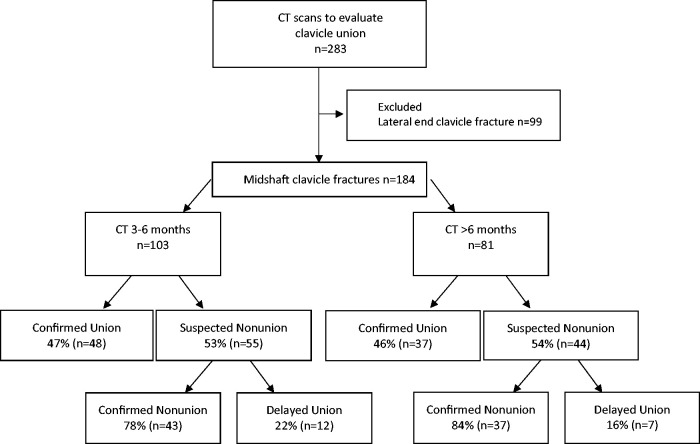
Figure 2.
Flow diagram of patients included in study and outcome.
There were 85 unions and 99 non-unions diagnosed on CT. Scans performed between three and six months were not found to result in a higher proportion of non-union diagnosis compared to those performed after six months (55/103 vs. 44/81 respectively, p = 0.9).
Of the 99 suspected non-unions, 67 had operative intervention at a median time of 292 days (range 192–491 days). Fifty-nine were following failed conservative management. Post-operatively, there was one deep infection associated with a septic non-union and five revision fixations required for metalwork failure for ongoing non-union. The remaining eight were revisions for non-union following acute plate fixation and no complications occurred.
CT accuracy for non-union diagnosis
No patient with union diagnosed on CT re-presented with evidence of an incorrect diagnosis. Out of 99 patients with suspected non-union on CT (conservative n = 84, post-ORIF n = 15), 80 were thought to be correctly identified. Of which 60 were confirmed at time of operation and 20 patients declined fixation with no further evidence of radiographic union, i.e. presumed fibrous non-union.
The remaining 19 patients were found to be united at the time of operation (n = 7) or on repeat CT imaging after declining fixation (n = 12). The time delay to CT did not affect the incorrect diagnosis of non-union (Table 1). This finding was not altered when patients who declined fixation were excluded (p = 0.44). Delay to surgery following CT scan was also not significantly different with confirmed non-unions at 113 days versus incorrect diagnosis at 126 days (p = 0.98). For those patients who united on repeat CT scanning, imaging occurred at a median of 402 days (range 251–440 days) following initial injury. Age, comminution, gender, smoking, or the presence of a plate following acute fixation did not affect the accuracy of diagnosis on univariate analysis (Table 1).
Table 1.
Demographics and clinical information of confirmed non-union versus delayed union following initial diagnosis of suspected non-union on CT.
| Confirmed non-union n = 80 | Delayed union n = 19 | Significance | |
|---|---|---|---|
| Age – years | 48.4 (CI 45.1–51.6) | 45.9 (CI 39.1–52.7) | 0.51 |
| Male/Female | 51/29 | 12/7 | 0.96 |
| Smoker | 29 (36.3%) | 4 (21.1%) | 0.21 |
| Post plate fixation (n = 15) | 12 (15.0%) | 3 (15.8%) | 0.93 |
| Time to CT – days | 168.5 (IQR 116.5–239.8) | 146 (IQR 95.0–193.0) | 0.12 |
| <180 days | 43 | 12 | 0.46 |
| >180 days | 37 | 7 | |
| Time from CT to operation Days | 113 (IQR 74.3–117.3) | 126 (IQR 78.0–215.0) | 0.98 |
| Overall time to operation Days | 288.5 (IQR 222.5–447.0) | 333.0 (IQR 261.0–430.0) | 0.45 |
| Comminution (Robinson 2B2) | 41 (51.3%) | 11 (57.9%) | 0.60 |
| Callus hypertrophic | 23 (28.8%) | 19 (100%) | <0.001* |
| High energy | 37 (46.3%) | 8 (42.1%) | 0.74 |
Mean and 95% confidence interval (CI) given in brackets. Median and interquartile range (IQR) 25th–75th centile in brackets.
*Significance < 0.05.
Callus findings
The majority of the non-union callus findings were atrophic (57/99) with the remainder hypertrophic (42/99). Correct non-union diagnosis was most likely found with atrophic callus (atrophic 71.3% vs. hypertrophic 28.8%, p < 0.001) whereas all of the delayed unions were hypertrophic. Early CT scans prior to six months were not more likely to diagnose atrophic callus (p = 0.28). Smoking was more likely to result in an atrophic non-union (smoker 28/33 vs. non-smoker 29/66, p < 0.001, OR 4.1). No other patient demographic (sex or age) or fracture characteristics (comminution or post-fixation) affected the appearance of the fracture callus formation.
Overall accuracy of CT for non-union prediction
The accuracy of CT to determine non-union has an 80.8% positive predictive value (PPV) and a 100% negative predictive value. Alternatively, it was 100% sensitive and 81.7% specific for the diagnosis of non-union. If a hypertrophic non-union was present, this had a 54.8% PPV for a correct diagnosis of non-union whereas atrophic non-union had a 100% PPV.
Kappa agreement between CT and radiographs
CT had greater inter-observer agreement over radiographs for the evaluation of bridging callus and fracture union (weighted kappa 0.75 vs. 0.50 respectively). The independent evaluation of each reviewer against the final diagnosis showed greater agreement on CT (Table 2). Reviewer agreement was not affected by the presence of plate fixation or comminution at the fracture site.
Table 2.
Weighted Kappa agreement.
| Imaging modality | Kappa | CI 95% | Significance |
|---|---|---|---|
| Radiograph | |||
| Inter-observer agreement | 0.50 | 0.25–0.75 | 0.001* |
| Reviewer 1 vs. Final diagnosis | 0.50 | 0.23–0.77 | 0.002* |
| Reviewer 2 vs. Final diagnosis | 0.50 | 0.25–0.75 | 0.001* |
| CT | |||
| Inter-Observer agreement | 0.75 | 0.55–0.95 | <0.001* |
| Reviewer 1 vs. Final diagnosis | 0.90 | 0.77–1.04 | <0.001* |
| Reviewer 2 vs. Final diagnosis | 0.85 | 0.69–1.01 | <0.001* |
CI: confidence interval.
*Significance < 0.05.
Discussion
CT evaluation of clavicle fractures has excellent accuracy to diagnose union but results in an overdiagnosis of non-union in approximately 20% of cases. This could be the result of CT not detecting unconsolidated bridging callus or simply because of a small number of clavicle fractures that develop a delayed union after six months. Timing of the scan does not appear to influence the accuracy with early scanning after three months showing comparable findings beyond six months. A hypertrophic fracture appearance had the greatest risk of incorrect non-union diagnosis with a delayed union found in approximately half of all cases. Blinded reviewer assessment showed greater agreement and diagnostic accuracy with CT when compared to radiographs. To our knowledge there has been no previous evaluation of clavicle CT scans to determine the accuracy, optimal timing or callus findings.
CT scanning for fracture non-union diagnosis was first advocated in 1988 and it was proposed that lack of bridging bone at the fracture could be visualised in multiple planes to provide a more detailed assessment of union.14 Additionally, this appeared to be of value when fracture site visualisation was difficult due to trauma implants such as intramedullary nails or plate and screws constructs.15–17 It has been shown that CT scanning can detect callus sooner than radiographs for distal radius and tibia fractures.18 The main benefit of CT compared to radiographs in fracture healing is the increased sensitivity for the detection of union.18,19
Bhattacharyya et al. found superior inter-class correlation agreement and greater sensitivity of CT for the diagnosis of union over radiographs (100% vs. 54% respectively) for tibia fractures post intramedullary nailing.11 However, it did not improve specificity for non-union accuracy which was comparable to radiographs at 62%. Other research groups have suggested that CT does not increase user agreement over plain radiographs alone with regards to management decisions, diagnosis of union, bridging callus and persistent fracture line detection.10 However, the authors of that study included a variety of fractures and fixation techniques which may have resulted in a too heterogenous clinical question.10
Radiation dose of a shoulder CT for clavicle evaluation is approximately 2.9 millisieverts (mSv).20 Given the close location of radiosensitive tissue in the neck and chest, this is much higher dose than a peripheral limb CT (e.g. ankle/wrist 0.8 mSv) or radiograph (0.01 mSv).21 A shoulder CT dose is comparable to a 1 in 8000 life-time fatal cancer risk or 14 months of background radiation.20 This is smaller when compared to other common CT indications such as abdomen and pelvis (14 mSv)21 but still represents a significant radiation dose of which surgeons should be mindful. It is difficult to counsel the patient on the theoretical life time risk of radiation and perhaps the main emphasis is that any CT should be essential to guide management when radiographs are equivocal for union. The use of CT with regard to clavicle fractures to date has largely been concerned with the evaluation of fracture displacement and measurement of clavicle shortening.22–24 Accuracy for fracture healing has not been explored.
The ability to predict non-union of the clavicle is of increasing importance given the evidence that conservative management results in equivalent function to acute fixation at one year if union occurs.1–5 Clavicle acute fixation is thought to be on the increase,25,26 despite evidence that approximately seven acute fixations are required to prevent one non-union.2 Selective early fixation of those at high risk of non-union maybe an effective strategy which has not been explored in recent controlled trials. Identifying patients with poor clinical recovery at six weeks27 could be a useful screening tool for selective CT scanning in patients where bridging callus is difficult to interpret on radiograph alone at three months. The detection of bridging callus on CT was 100% predictive of union and appeared to be equally accurate with early scanning before six months. Bridging callus on radiograph following tibia and femoral fractures beyond four months also appears to be a critical finding for union prediction.28–30
The patients in this study had radiographs that were difficult to interpret, and CT scanning was used to confirm the diagnosis prior to potential operative intervention. CT does not appear to distinguish between delayed unions and persistent non-unions. Given the over diagnosis of non-union our study does highlight the importance of correlation with the clinical picture and decision to proceed with surgery should not be based on CT result alone. Therefore, rather than recommending routine use of CTs, we would advocate the use of CT in a symptomatic patient where radiographs are difficult to judge clear bridging callus beyond three months. Furthermore, patients with hypertrophic callus finding and resolving pain at six months require careful clinical correlation prior to proceeding to surgery given we found half of these had a delayed union.
The cohort was relatively uniform as all CT scans were performed to confirm or refute union of midshaft clavicle fractures. Timings of the CT scans varied but this reflects clinical practice and all patients were a minimum of 12 weeks from injury and were beyond 24 weeks at time of surgery. Although this is the first large CT series to date to explore clavicle fracture union we recognise that there is a degree of selection bias in those patients who underwent CT scanning. Kappa agreements were not performed of callus type and fracture classification. However, judgement was based on a musculoskeletal radiologist report and retrospective review of the imaging, any discrepancies were discussed with the senior author who is an experienced consultant upper limb trauma surgeon.
The ‘gold standard’ was operative exploration of the fracture site to determine union, we decided to include those who declined operative intervention but had further evidence of union on CT evaluation on repeat imaging as delayed union. Additionally, those patients who declined operative intervention and had no further evidence of union were treated as fibrous non-unions. Potentially these patients may have gone onto unite or had delayed treatment out with the treatment centre but review of our national PACS system did not reveal this. When looking at only those patients who had operative exploration it did not change the overall estimations of CT sensitivity and specificity.
Conclusions
CT scanning of midshaft clavicle fractures has excellent accuracy to determine union but approximately one in five suspected non-unions went onto unite. Hypertrophic non-unions resulted in a delayed union in approximately half of the cases in our study. Early CT scanning from three months had comparable accuracy to delayed scanning beyond six months. Compared to radiographs it has superior reviewer agreement and maybe a useful investigation where union is clinically in doubt.
Acknowledgements
This article was presented as a podium presentation at BESS 2019.
Footnotes
Declaration of Conflicting Interest: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: CMR reports personal consultancy fees and institutional funding received from Acumed, not related to this study.
Ethical approval: Not required.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Virtanen KJ, Remes V, Pajarinen J, et al. Sling compared with plate osteosynthesis for treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am 2012; 94: 1546–1553. [DOI] [PubMed] [Google Scholar]
- 2.Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures. J Bone Joint Surg Am 2013; 95: 1576–1584. [DOI] [PubMed] [Google Scholar]
- 3.Woltz S, Stegeman SA, Krijnen P, et al. Plate fixation compared with nonoperative treatment for displaced midshaft clavicular fractures: a multicenter randomized controlled trial. J Bone Joint Surg Am 2017; 99: 106–112. [DOI] [PubMed] [Google Scholar]
- 4.Ahrens PM, Garlick NI, Barber J, et al. Clavicle Trial Collaborative Group. The Clavicle Trial: a multicenter randomized controlled trial comparing operative with nonoperative treatment of displaced midshaft clavicle fractures. J Bone Joint Surg Am 2017; 99: 1345–1354. [DOI] [PubMed] [Google Scholar]
- 5.Qvist AH, Væsel MT, Jensen CM, et al. Plate fixation compared with nonoperative treatment of displaced midshaft clavicular fractures: a randomized clinical trial. Bone Joint J 2018; 100-B: 1385–1391. [DOI] [PubMed] [Google Scholar]
- 6.Robinson CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004; 86: 1359–1365. [DOI] [PubMed] [Google Scholar]
- 7.Kitsis CK, Marino AJ, Krikler SJ, et al. Late complications following clavicular fractures and their operative management. Injury 2003; 34: 69–74. [DOI] [PubMed] [Google Scholar]
- 8.Beliaev AM, Fougere C. Thoracic outlet syndrome secondary to a mid-clavicle malunion. BMJ Case Rep 2015; 2015: bcr2015209583–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leow JM, Clement ND, Tawonsawatruk T, et al. The radiographic union scale in tibial (RUST) fractures: reliability of the outcome measure at an independent centre. Bone Joint Res 2016; 5: 116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kleinlugtenbelt YV, Scholtes VAB, Toor J, et al. Does computed tomography change our observation and management of fracture non-unions? Arch Bone Jt Surg 2016; 4: 337–342. [PMC free article] [PubMed] [Google Scholar]
- 11.Bhattacharyya T, Bouchard KA, Phadke A, et al. The accuracy of computed tomography for the diagnosis of tibial nonunion. J Bone Joint Surg Am 2006; 88: 692–697. [DOI] [PubMed] [Google Scholar]
- 12.Robinson CM. Fractures of the clavicle in the adult. epidemiology and classification. J Bone Joint Surg Br 1998; 80: 476–484. [DOI] [PubMed] [Google Scholar]
- 13.Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions, Hoboken, NJ: John Wiley & Sons, Inc, 2003. [Google Scholar]
- 14.Kuhlman JE, Fishman EK, Magid D, et al. Fracture nonunion: CT assessment with multiplanar reconstruction. Radiology 1988; 167: 483–488. [DOI] [PubMed] [Google Scholar]
- 15.Schnarkowski P, Rédei J, Peterfy CG, et al. Tibial shaft fractures: assessment of fracture healing with computed tomography. J Comput Assist Tomogr 1995; 19: 777–781. [PubMed] [Google Scholar]
- 16.Costelloe CM, Dickson K, Cody DD, et al. Computed tomography reformation in evaluation of fracture healing with metallic fixation: correlation with clinical outcome. J Trauma 2008; 65: 1421–1424. [DOI] [PubMed] [Google Scholar]
- 17.Ohashi K, El-Khoury GY, Bennett DL et al. Orthopedic hardware complications diagnosed with multi-detector row CT. Radiology 2005 N; 237: 570-577. [DOI] [PubMed]
- 18.Grigoryan M, Lynch JA, Fierlinger AL, et al. Quantitative and qualitative assessment of closed fracture healing using computed tomography and conventional radiography. Acad Radiol 2003; 10: 1267–1273. [DOI] [PubMed] [Google Scholar]
- 19.Krestan CR, Noske H, Vasilevska V, et al. MDCT versus digital radiography in the evaluation of bone healing in orthopedic patients. Am J Roentgenol 2006; 186: 1754–1760. [DOI] [PubMed] [Google Scholar]
- 20.Yi JW, Park HJ, Lee SY, et al. Radiation dose reduction in multidetector CT in fracture evaluation. Br J Radiol 2017; 90: 20170240–20170240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N Engl J Med 2007; 357: 2277–2284. [DOI] [PubMed] [Google Scholar]
- 22.Omid R, Kidd C, Yi A, et al. Measurement of clavicle fracture shortening using computed tomography and chest radiography. Clin Orthop Surg 2016; 8: 367–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goudie EB, Clement ND, Murray IR, et al. The influence of shortening on clinical outcome in healed displaced midshaft clavicular fractures after nonoperative treatment. J Bone Joint Surg Am 2017; 99: 1166–1172. [DOI] [PubMed] [Google Scholar]
- 24.Oki S, Matsumura N, Kiriyama Y, et al. Three-dimensional deformities of nonoperative midshaft clavicle fractures: a surface matching analysis. J Orthop Traum 2017; 31: e385–389. [DOI] [PubMed] [Google Scholar]
- 25.Huttunen TT, Launonen AP, Berg HE, et al. Trends in the incidence of clavicle fractures and surgical repair in Sweden. J Bone Joint Surg Am 2016; 98: 1837–1842. [DOI] [PubMed] [Google Scholar]
- 26.Navarro RA, Gelber JD, Harrast JJ, et al. Frequency and complications after operative fixation of clavicle fractures. J Shoulder Elbow Surg 2013; 22: e36–37. [DOI] [PubMed] [Google Scholar]
- 27.Clement ND, Goudie EB, Brooksbank AJ, et al. Smoking status and the disabilities of the arm shoulder and hand score are early predictors of symptomatic nonunion of displaced midshaft fractures of the clavicle. Bone Joint J 2016; 98-B: 125–130. [DOI] [PubMed] [Google Scholar]
- 28.Lack WD, Starman JS, Seymour R, et al. Any cortical bridging predicts healing of tibial shaft fractures. J Bone Joint Surg Am 2014; 96: 1066–1072. [DOI] [PubMed] [Google Scholar]
- 29.Strotman PK, Karunakar MA, Seymour R, et al. Any cortical bridging predicts healing of supracondylar femur fractures after treatment with locked plating. J Orthop Traum 2017; 31: 538–544. [DOI] [PubMed] [Google Scholar]
- 30.DiSilvio F, Jr, Foyil S, Schiffman B, et al. Long bone union accurately predicted by cortical bridging within 4 months. JBJS Open Access 2018; 3: e0012–e0012. [DOI] [PMC free article] [PubMed] [Google Scholar]