Abstract
Colorectal cancer (CRC) is the third most diagnosed form of cancer and second most deadly cancer worldwide. Introduction of better screening has improved both incidence and mortality. However, as the coronavirus disease 2019 (COVID-19) pandemic began, healthcare resources were shunted away from cancer screening services resulting in a sharp decrease in CRC screening and a backlog of patients awaiting screening tests. This may have significant effects on CRC cancer mortality, as delayed screening may lead to advanced cancer at diagnosis. Strategies to overcome COVID-19 related disruption include utilizing stool-based cancer tests, developing screening protocols based on individual risk factors, expanding telehealth, and increasing open access colonoscopies. In this review, we will summarize the effects of COVID-19 on CRC screening, the potential long-outcomes, and ways to adapt CRC screening during this global pandemic.
Keywords: Colorectal cancer, COVID-19, Colonoscopy, Early detection of cancer, Diagnostic screening programs, Mass screening
Core Tip: Coronavirus disease 2019 (COVID-19) has resulted in a major decrease in colorectal cancer (CRC) screening and will likely have significant long-term effects on CRC incidence and mortality. This review discusses the effects of COVID-19 on CRC screening and the outcomes that will likely result. We then review different options to ensure safe and convenient resumption of CRC screening in the midst of this pandemic.
INTRODUCTION
Colorectal cancer (CRC), comprising of cancer of the colon and rectum, is the third most diagnosed form of cancer globally. It encompasses over 10% of all cancer diagnoses, for an estimated 1.9 million CRC diagnoses in 2020[1-3]. In terms of mortality, CRC ranks second for most deadly cancer worldwide[1,2]. It accounts for over 900000 deaths annually, often due to diagnosis at advanced clinical stages[3,4]. In the United States specifically, there were a projected 147950 CRC diagnoses for the year 2020, with 53200 CRC deaths[5]. Studies show significant regional variation in incidence best explained by behavioral and lifestyle differences and disparities in access to screening[1]. Racial and socioeconomic disparities in CRC also exist, with highest incidence and mortality rates in non-Hispanic blacks (NHBs) and American Indians/Alaskan Natives (AI/ANs), and a higher likelihood of CRC diagnosis in those with low socioeconomic status (SES)[5]. Regarding economic burden, 2007-2012 Surveillance, Epidemiology, and End Results Program-Medicare data shows an average of $63063 spending per patient for CRC. More advanced stage at diagnosis was associated with higher annual spending[6].
The introduction of better screening has been a major driver for greater survival[1,7]. Efforts for early detection and removal of polyps allow for diagnosis of previously unknown disease; this diagnosis at an early stage and removal of pre-cancerous and/or un-metastasized polyps has led to a long-term reduction in mortality[8]. In the United States, Surveillance, Epidemiology, and End Results Program data from 1991-2011 shows a 35% reduction in incidence rate with a 37% reduction in mortality rate related to the beginning of the screening programs[3,9,10]. A cost effectiveness study showed that if screening rates were increased to 80%, 3-fold more CRC deaths could be avoided at one third of the current costs[11].
The coronavirus disease 2019 (COVID-19) began in late 2019; by March 30th 2020, it had spread to 203 countries and was officially declared a global pandemic[12-14]. As of May 1, 2021, there was a total of 84474195 confirmed cases with 1848704 confirmed deaths globally. 222 different countries, areas, or territories were affected with cases[13]. The original effects due to COVID-19 were severe due to both the infective spread and lack of preparedness and proper anticipation. In the United States, there was a rapid mobilization and distribution of existing health care resources and an effort to social distance[15]. The trend in many affected countries, such as Italy, France, United Kingdom, Germany, and Spain, was an initial outbreak in March 2020, followed by a decline in case count after May 2020. There was then a new surge of COVID-19 cases around November 2020, resulting in the “second wave”[13,16].
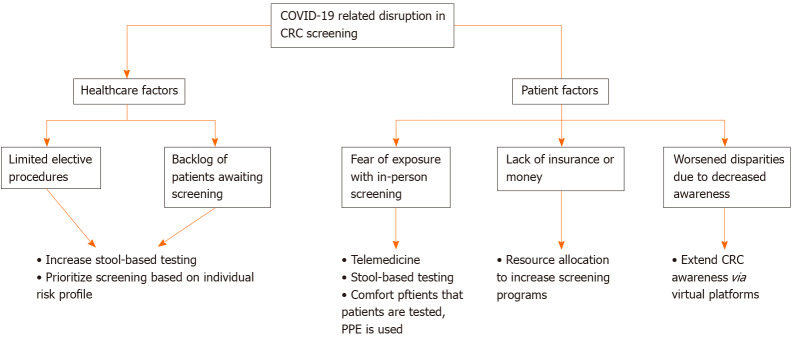
The COVID-19 pandemic has been ongoing from March 2020 to present day, and the consequences must be considered. During this time, patients were recommended to avoid unnecessary hospital and emergency department visits. Nonurgent office visits as well as elective procedures and surgeries were cancelled. The changes in healthcare utilization during this time may result in serious long-term effects[15]. Specifically, new challenges have arisen regarding cancer prevention and treatment, as cancer screenings and surgeries were cancelled, and therapeutic plans were disrupted[17]. This raises many barriers to CRC screening that must be addressed, as summarized in Figure 1.
Figure 1.
Summary of the disruption of coronavirus disease 2019 on the standard of care for colorectal cancer screening as well as possible solutions to these problems. COVID-19: Coronavirus disease 2019; CRC: Colorectal cancer.
This article will review current issues in CRC screening due to COVID-19. First, we will provide an overview of the barriers to CRC screening and the long-term outcomes of such a disruption. We will then discuss ways to manage this disruption, including adapting current screening methods, developing a more organized system for screening, and utilizing open access colonoscopies. Then, we will consider how COVID-19 may exacerbate CRC inequities in medically underserved populations. We will conclude with some opportunities for innovation as we adapt to CRC screening during this pandemic.
BARRIERS TO CRC SCREENING DUE TO COVID-19
COVID-19 has caused a major disruption in healthcare utilization as patients were encouraged to avoid hospitals and were forced to reschedule nonurgent office visits and elective procedures[15]. To conserve health care resources and redirect them towards efforts against COVID-19, cancer screening services for patients were brought to a halt. As of March 12, 2020, The American Cancer Society recommended postponing of cancer screening plans[17,18]. Endoscopy units were recommended to prioritize necessary procedures and strongly consider postponing non-urgent procedures[17,19,20]. This significant decrease in endoscopic procedures greatly affects volume of CRC screening and may have a long term of effect on these diagnoses[20]. In the United States, between January 20, 2020 and April 21, 2020, CRC screening rates are estimated to have dropped by 85%. By June 16, 2020, rates remained 36% below pre-COVID-19 Levels. This equates to 95000 missed screenings just within this time frame, which is 64% less than expected based on historical data[17,21].
The drop in endoscopic procedures is also mirrored by a drop in face-to-face office visits. A cross-sectional study analyzing health insurance claims for patients across the United States showed a 68% decrease in office visits when comparing April 2020 to April 2019. During this time, there was an increase in telemedicine visits by 40.81%. While the relative increase of telemedicine is significant, the absolute increase does not offset the reduction in office visits, suggesting many healthcare needs may be going unmet[22]. This could indicate that patients with nonspecific cancer symptoms such as fatigue, weight loss, or change in bowel habits choose not to present to their physicians[23,24]. Those that present via video or telephone consultation may have missed diagnoses due to lack of physical exam and inability for physician to use their intuition[23]. Patients may also feel more embarrassed and uncomfortable expressing concerns about alarming symptoms in a telemedicine format[25]. When patients do present with cancer symptoms that are caught during their visit, their further management is still likely to be delayed. If only emergency endoscopy is being performed, patients with symptoms suggestive of CRC will still have prolonged diagnosis[23].
The impact of the COVID-19 pandemic also exacerbates patients’ barriers to receiving care. The effects of the pandemic add significant psychological stress on patients and may affect their desire to seek preventative cancer care[17]. In the United States, as unemployment rates rise, many workers and their dependents are at risk of losing their employer-based insurance, which would further decrease accessibility to these preventative healthcare services[17]. Even those that do have health insurance may be discouraged from seeking services due to fear of exposure of COVID-19. Additionally, those without ability to utilize telehealth options are further limited in access to care[17]. Patients residing in lower-income zip codes or in minority populated areas have lower rates of telemedicine use[22]. Older adults and those living in rural areas may also lack the technology needed to access telemedicine[25]. Poverty has long been a barrier to CRC screening, especially in countries with limited resources. Patients are unlikely to seek out preventative services when they are unable to fulfill their basic needs[26]. The effects of the pandemic are likely to worsen these barriers and result in further decreases in screening in these populations.
LONG-TERM OUTCOMES
With COVID-19, the halt in CRC screening has led to a major backlog of patients awaiting screening tests. As the pandemic still affects many major countries in the world, it is also unlikely that screening activities will resume at full capacity in the near future. The buildup of backlog coupled with the inability to resume screenings completely will likely have significant consequences[27]. CRC screening allows for early detection, which both decreases mortality and improves quality of life scores. In the long-term, it also allows for significant healthcare savings, as lifetime costs of managing colon cancer increase exponentially with later staging at time of diagnosis[28]. This suggests that there may be increased mortality, healthcare spending, and psychological burden of CRC due to the pause in screening[28].
In the United States, CRC screening is approached mostly via screening colonoscopy, while in Europe, most countries screen via fecal immunochemical test (FIT); both have been on hold since the start of the pandemic[27]. In Europe, a positive FIT is recommended to be followed up by colonoscopy within the next 1 mo[29]. One study based on the European FIT-based screening program showed that a 9 mo delay following a positive FIT is associated with poorer outcomes in terms of risk of CRC and CRC progression[30]. Another study using data from the Taiwan Nationwide CRC Screening Program shows that delays for colonoscopy after positive FIT past 6 mo are associated with higher risk and significant progression of disease[31]. Estimates of the effects of COVID-19 on CRC suggest that a moderate 7-12 mo screening delay will cause a significant increase in advanced cancers at detection (from 26% to 29%). This worsens after a 12 mo delay up to 33%[27]. These estimates suggest a delay past 6 mo will result in a shift towards advanced stages in detection, and a delay past 12 mo will result in an increase in mortality rates. These effects will increase both disease burden and costs of disease[27]. Similarly, early population-based modeling data in the United Kingdom suggests a substantial increase in avoidable cancer deaths due to COVID-19, with up to a 16.6% increase in deaths due to CRC in the 5 years after diagnosis[32].
ADAPTING CRC SCREENING METHODS
CRC screening tests offered are generally divided into either direct visualization screening methods like colonoscopies or stool-based screening methods like FIT, mt-sDNA (Cologuard in the United States), or Fecal Occult Blood Test (FOBT)[33]. A reduction in elective procedures due to the pandemic has resulted in a significant drop in screening colonoscopies, the mainstay of CRC screening in the United States. Such volume has not recovered to pre-pandemic levels[34,35]. As additional practices are put into place to protect and educate both patients and healthcare workers, the process of getting a colonoscopy has become more complex and operating capacity of endoscopy centers will continue to be affected[36]. The additional measures being taken include pre-procedure screenings for COVID-19 infection, increasing levels of hygiene measures, and social distancing throughout the waiting rooms and recovery rooms[37]. These measures will both increase the amount of time required per procedure and limit the number of people that can be accommodated in the endoscopy unit[37]. The implementation of these practices will continue to affect the operating capacity of endoscopy units[37]. Hospitals and providers are responding to the major upheaval in CRC screening practices in various ways. There have been calls to increase the utilization of FIT to triage and reduce the backlog of patients who need to be screened[34]. Since FIT is a non-invasive procedure, this may be a way to reach patients who are hesitant of hospital procedures due to a perceived increased risk of contracting COVID-19[36]. FIT also has a high negative predictive value, making it an appropriate test to triage symptomatic patients. Those with positive tests can continue to be worked up while patients with negative tests can be reassured that their symptoms are most likely not due to CRC[38]. Considerations in performing colonoscopy vs FIT screening in the wake of the pandemic are summarized on Table 1. An area of focus should be ensuring individuals at higher risk, particularly if there may be an increase in stool-based testing, are prioritized for timely access to follow-up or surveillance colonoscopies[39]. One study based on the Galician CRC screening program showed that upon resumption of colonoscopies, over 3000 colonoscopies were conducted with no cases of COVID-19 infection reported[40]. This suggests that resuming colonoscopy screening for those at highest risk may pose a very limited risk for infection. Patients can therefore by reassured and encouraged to proceed with colonoscopy as needed.
Table 1.
Comparison of colorectal cancer screening tests during the coronavirus disease 2019 pandemic
|
Colonoscopy
|
Stool based testing
|
| Advantages | |
| Prioritization “risk stratification” of patient population can ensure those at highest risk for developing CRC can still have timely access to tests[39] | Widespread use of FIT may lower CRC mortality rates[49], some models indicate similar benefit to colonoscopy[85] |
| Allows longer interval between colonoscopies[33] | Cheaper and less invasive compared to colonoscopy[36] |
| Visualization and, if needed, polypectomy can be completed within the same procedure[33] | Reduces scheduling of colonoscopies, lessening patient exposures[34] |
| Can be completed at home and sent back to the laboratory[33] | |
| Disadvantages | |
| Needs pre-procedure visits[36] | Short interval between tests[33] |
| Loss of health insurance may limit patient ability to pay for procedures[36] | Positive individuals still need to undergo colonoscopy, which may be subject to out-of-pocket costs[33] |
| Little consensus on optimal threshold cutoff value[86] | |
| Implementing on a larger scale requires establishment systems in place[34] | |
FIT: Fecal immunochemical test; CRC: Colorectal cancer.
Another approach is considering increased use of other stool-based options such as mt-sDNA. Mt-sDNA may be conducted at 3-year intervals as compared to the 1-year interval of FIT[41], which may be preferable to patients and reduce hospital burden as the backlog of patients needing screening increases. Another advantage of mt-sDNA is the presence of a patient navigation service that ships kits to patients’ homes and returns them directly for processing[42]. The screening test is done entirely from home with no special preparation or time off from work, a very convenient service in the wake of the pandemic[42]. Studies show that mt-sDNA has increased sensitivity for detection of CRC and precancerous lesions as compared to FIT, but with a lower specificity[43]. Since mt-sDNA has a high false positive rate, the chances a patient would need to return to the hospital for a follow-up colonoscopy are increased[44]. Given that the CRC screening field is trying to reduce excess colonoscopies in the COVID-19 pandemic, the high false positive rate is an important limitation to the test. Still, mt-sDNA remains a potential option to increase access to CRC stool-based screening within the confines of the current COVID-19 reality.
Adapting to the new reality of COVID-19 will also require consideration of other potential approaches that may improve patient compliance and screening rates. One such approach is embracing telehealth to reduce unnecessary office appointments, including pre-procedure colonoscopy visits[45]. Many outpatient visits already transitioned to telehealth during the pandemic[46]. Electronic medical records can be queried to identify patients not up to date with screening, a method that would transition well to organized screening practices[45]. Individuals can be contacted for follow-up of positive stool-based tests with automated phone calls, or notes from patient messaging platforms[45]. This will allow for convenient pre-procedure and follow up visits and may help improve patient compliance[45].
The pandemic presents a unique opportunity for the United States to transition from its current largely opportunistic screening approach, defined as screening offered by a provider, to a more organized programmatic approach[34]. Models for organized screening already exist, where screening is extended to an eligible population with a pre-determined approach[47], and have been studied in different community settings. An Italian study instituted programmatic FIT outreach in staggered timelines across the country and found a 22% decrease in subsequent CRC mortality as compared to no screening[48]. This is consistent with other organized outreach studies that show a reduction in CRC incidence and mortality, as well as a significant increase in screening uptake[49,50]. Instituting organized outreach in one large healthcare system where the previous approach had been mostly opportunistic screening saw screening rates improve from 40% to over 80%[50]. This type of population-based management is cost-effective[51], and may reduce over-screening in the long term[34]. Since the United States healthcare system exists in the form of fractured silos, a significant effort and collaboration is needed between hospitals, the government, and applicable organizations to set up the funding and systems in place[34]. While the initial work may be labor-intensive, organized screening can serve as an excellent way to address the pandemic-driven screening crisis by way of increasing the group of patients taking part in screening, and identifying individuals at higher risk for developing CRC[36].
Risk stratification for CRC screening
While a programmatic approach will be useful in increasing screening, an individualized approach for CRC screening can help focus resources on those with highest risk. Studies have shown known risk factors for CRC such as age, male sex, family history of CRC, obesity, diabetes, consumption of red and processed meats, smoking, and excessive alcohol intake[52], but there has been difficulty establishing a model that accurately identifies high risk CRC patients. A systematic review of 52 models incorporating 87 different risk factors showed that half the models had acceptable-to-good discrimination[53], and only 21 of the 52 models have been externally validated[54]. Another systematic review focused specifically on 17 CRC risk models derived from asymptomatic patients undergoing colonoscopy. This showed that the risk prediction models had a median of five risk factors, with age, sex, family history in 1st degree relative, Body mass index, and smoking history being the most common factors[55]. The summary of risk factors based on these studies that can be easily applied by clinicians is summarized in Table 2. While different models have been suggested in the past, the need to implement an effective risk-based screening approach is increased more than ever in the wake of the pandemic.
Table 2.
Risk factors to consider for risk stratification model of colorectal cancer based on recent studies[52,53,55]
|
Demographic characteristics
|
Older age, obesity, male sex, family history of CRC, race/ethnicity
|
| Personal medical history | Hypertension, diabetes |
| Lifestyle | Smoking, alcohol, sedentary lifestyle |
| Diet | Red meat consumption, processed meat consumption, low fiber diet |
CRC: Colorectal cancer.
A recent study using data from two international consortia of 9748 CRC cases and 10590 controls from 1992 to 2005 tested more individualized screening, incorporating environmental factors (E-score) and genetics based on CRC-associated single-nucleotide polymorphisms (G-score). The scores determined CRC risk more accurately than family history alone. These results may encourage clinicians to recommend more intense screening to high-risk patients while creating reluctance to intensely screen those with lower scores; however, further research is needed[56,57]. Incorporating FIT into these risk models may be helpful to determine which patients to prioritize for screening. A study of 34658 patients with no family history of CRC were evaluated for risk of advanced neoplasia based on a scoring system for certain risk factors (male sex, obesity, smoking status). Utilizing the scoring system showed a higher advanced neoplasia prevalence in patients as their risk score increased. The risk of advanced neoplasia increased even more significantly in FIT positive patients[58]. This scoring system may be used to determine which screening tools to use. Colonoscopy may be recommended for patients with high clinical risk while FIT can be used initially for lower risk patients[58]. Instead of using FIT as a dichotomous positive and negative value, studies show that measuring the fecal hemoglobin (f-Hb) concentration is also useful for CRC detection[59,60]. Retrospective analysis of 3733 asymptomatic patients over 50 years of age in Korea demonstrated that scoring models combining f-Hb concentrations and clinical risk factors (age, smoking status, and diabetes) were more effective than binary FIT results[60].
COVID-19 may present the opportunity to refine risk stratification models and help clinicians individualize screening for CRC. Studying risk factors such as those listed in Table 2 can help pave the way towards a validated risk score that can be widely applicable to the population. More investigation of single-nucleotide polymorphisms related to CRC may further individualize CRC risk assessment. The risk assessment can be combined with f-Hb concentrations based on FIT to help identify those at highest risk for CRC. This individualized model will be especially important for ensuring patients at highest risk are screened appropriately amid this global pandemic.
OPEN ACCESS COLONOSCOPY
Open access colonoscopy (OAC) is a service that allows patients to schedule colonoscopies without a pre-procedure evaluation by a gastroenterologist. To provide this service, a healthcare center needs an infrastructure in place for patients to directly schedule their colonoscopies without consulting a gastroenterologist. Hospital systems coordinate OACs through various systems such as patient navigators or primary care physicians, who manage the referral and pre-procedure preparation[61-63]. OACs appear to be a viable solution for addressing the delay in colonoscopy screening, as they show promise in increasing screening, decreasing healthcare costs, and navigating the reallocation of gastrointestinal services in the setting of COVID-19[63]. The advantages and disadvantages of OAC are outlined in Table 3.
Table 3.
Advantages and disadvantages of open access colonoscopies
|
Advantages
|
Disadvantages
|
|||
| No pre-colonoscopy consultations | Promotes development of an electronic risk-assessment system | Increased rates of inappropriate surveillance guidelines | Dependent on hospital infrastructure to facilitate OAC | High rates of no-shows and cancellations |
| Decreased healthcare expenditure | Shared medical records amongst patient’s care team | May take away from limited available resources | Loss of appointment spots needed to make up for COVID-19 backlog | |
| Patients save time and money | Identifies high risk individuals | |||
| Decreased patient load on gastroenterologists | Recommends screening based on most recent CRC guidelines | |||
CRC: Colorectal cancer; OAC: Open access colonoscopy; COVID-19: Coronavirus disease 2019.
Studies show that open access providers ordered screening colonoscopies with similar efficacy as gastroenterologists, with both healthcare professionals appropriately ordering screening colonoscopies over 90% of the time[64,65]. Patients who underwent OACs compared to those who had a pre-procedural evaluation by a gastroenterologist (NOAC) had similar pre-procedural outcomes and clinical outcomes[65]. Regarding CRC prevention, OAC and NOAC adenoma detection rate was 39.7% and 38.6%, respectively[64].
Advantages of OAC
OAC is convenient for the patient, gastroenterologist, and hospital as it allows patients to bypass a pre-procedural specialist office visit. Patients no longer must miss work for a pre-procedural consultation, saving the patients time and money. It is estimated that direct referral for colonoscopy decreased the number of pre-procedural gastroenterologist consultations by 9558 and decreased healthcare expenditures by $850000 in Israel[66]. OAC may also reduce the time delay between initial consultation and colonoscopy and result in higher diagnostic yield, which may be vital for symptomatic patients[67]. In the wake of the COVID-19-related postponement of screening and surveillance colonoscopies, gastroenterologists will be overwhelmed by the backlog of patients awaiting colonoscopies. The anticipated increase in demand for colonoscopies may be mitigated by decreasing the number of pre-procedural consultations that gastroenterologists must perform.
With the increased availability of OAC services, healthcare organizations will need to reform and remodel their electronic health records to promote integrated care, such that medical records can be easily distributed among a patient’s care team. The building of these uniform electronic medical records (EMR) presents an opportunity for hospitals to encode automatic risk assessments into their systems[68]. A study showed that the implementation of the Electronic Health Records-Based Risk-Assessment System (which incorporated the risk CRC assessment tool developed by Kastrinos et al[69]) resulted in increased identification of high-risk individuals as patients scheduled their screening colonoscopies[68,69].
Barriers to OAC
A major challenge that exists with OAC includes a significantly increased rate of inappropriate surveillance colonoscopies when compared to NOAC[64]. Based on 2012 consensus guidelines, surveillance colonoscopies were inappropriately recommended by open access providers in 32.6% of cases, while gastroenterologists recommended inappropriate surveillance colonoscopies in 26.4% of cases[64]. The majority of the inappropriate surveillance colonoscopies were deemed improper because they were performed too early as opposed to too late[64]. Over the course of the years, the surveillance guidelines have become even more liberal with longer recommended intervals between normal colonoscopies. Application of the newest guidelines would likely result in even higher percentages of inappropriate surveillance due to early surveillance[70]. As hospital systems attempt to recover from the setbacks of the pandemic, early inappropriate surveillance may take away the limited available spots from more vulnerable patients who are at higher risk for CRC.
Furthermore, OAC success appears to be highly dependent on the hospital infrastructure available to facilitate the service. In spite of the established OAC services, as of 2016, “approximately 30% of colonoscopies for colon cancer screening and polyp surveillance were preceded by a gastroenterology office visit”[71]. Therefore, even if OAC systems are available, they are being bypassed by patients. Lastly, OACs have high rates of no-shows (13.5%) and cancellations (31.5%)[65]. Given that colonoscopies require time for adequate pre-procedural prep, filling in for last-minute cancellations is difficult and results in a loss of time that is desperately needed to make up for the backlog due to COVID-19.
Addressing barriers to OAC
Options for addressing the high rates of inappropriate surveillance include utilizing quality checks built into the system to reevaluate the patients who are most in need of colonoscopies and automating EMRs to recommend appropriate guidelines. A recent study suggested that by strictly following the United States Multi-Society Task Force guidelines when reviewing patients who were referred for OAC, there could be a 33%-39% estimated decrease in the burden of surveillance of colonoscopy[70]. EMRs should be automated to suggest appropriate follow-up upon required completion of risk-assessment surveys to allow convenient application of CRC screening and surveillance guidelines[64,70]. Programming these structures into the EMR will decrease the workload for physicians and likely decrease the burden of screening and surveillance colonoscopies. After determining which patients are high risk, use of a mediator such as patient navigators can improve colonoscopy completion rates. Use of patient navigators is associated with low no-show rates (2.9%) and adequate bowel preparation (89%)[61]. In the long-term, to change misinformed perceptions of published screening and surveillance guidelines, educational sessions for both primary care providers and gastroenterologists are needed[70]. These meetings can strengthen working relationship among the teams and facilitate discussion for feedback and improvement[63].
EXACERBATIONS OF CRC INEQUITIES DUE TO COVID-19
Prior to COVID-19, there were known disparities in CRC metrics among racial and ethnic groups as well as patients of low SES in the United States. Rates of CRC are highest among NHBs and AIs/ANs[5]. From 2012 to 2016, the age adjusted incidence rate for CRC was highest in NHBs at 45.7 and AIs/ANs at 43.3 per 100000 people[5]. The difference in CRC mortality in NHBs compared to other racial and ethnic groups is more striking. Between 2013 and 2017, NHBs had a 40% higher death rate than non-Hispanic whites, with a death rate of 19.0 in NHBs compared to 13.8 in non-Hispanic whites. The death rate in NHBs was twice higher than that of Asian Americans/Pacific Islanders, who had a death rate of 9.5 per 100000 in Americans/Pacific Islanders[5]. Patients of low SES are affected by CRC disparities as well. Prospective analysis of the National Institutes of Health-American Association of Retired Persons Diet and Health Study data from 1995 to 1996 of over half a million adults found that the overall incidence of CRC was significantly higher in those with low educational level or patients that lived in low SES neighborhoods[72]. This association remained after accounting for individual CRC risk factors such as sex, age, race and ethnicity, state of residence, and history of CRC in a first degree relative. Adults with less than 12 years of education had a 42% higher risk of incidence of CRC and those who resided in the poorest neighborhoods had a 31% higher CRC risk[72]. When comparing rural and urban neighborhoods, rural populations also have both increased incidence and mortality from CRC[73].
The basis for these disparities is complex and multifactorial. Further analysis of data from the National Institutes of Health-American Association of Retired Persons Diet and Health Study found that 44% of the association between education and 36% of the association between low SES neighborhoods in CRC incidence was due to a combination of health behaviors (diet, physical activity, and smoking) and Body mass index[74]. Other barriers to CRC screening that contribute to disparities include lack of health insurance, inability to take off of work to have a colonoscopy, expense, lack of provider recommendation, unpleasantness of CRC screening tests (fecal sampling and storage and bowel preparation for colonoscopy), and lack of options given for screening tests with only being offered a colonoscopy[75,76]. Among NHBs, there is a lack of knowledge regarding CRC and mistrust in the medical community. In one study, only 38% of NHBs thought that CRC is usually fatal, 40% did not feel the disease was preventable, and 43% did not think there was a cause for CRC[77].
COVID-19 may exacerbate these inequities. Medically underserved populations had limited access to preventive health services prior to the pandemic[78] and there was an estimated 86% drop in colon cancer screening between January 20, 2020 and April 21, 2020[17]. In the United States, federally qualified health centers are community health centers (CHCs) funded by the federal government. Federally qualified health centers provide preventive services to over 22 million Americans that are low-income, uninsured, and/or underinsured[78]. There has been a sharp reduction in clinical visits and the ability to provide endoscopic services to these patients. Also, clinics that provided FIT/FOBT pick-up and return have halted CRC screening due to social distancing policies[78]. In the United States, there were also lower rates of telemedicine use among patients residing in lower-income zip codes or in minority populated areas, which may indicate further limitations in access to health care services[22].
Adapting to exacerbations of CRC inequities
The disruptions to health services due to COVID-19 may cause further strain in medically underserved populations that had limited access to preventive health services even prior to the pandemic[78]. There are several suggestions proposed to counteract the decline in CRC screening to these patients.
Mailed FIT and FOBT kits and initiating safe protocols to pick up and return these kits has been recommended[78,79]. Patients that have an abnormal FIT/FOBT or those that develop CRC associated interval symptoms should be prioritized for follow up and colonoscopy[78]. Telehealth visits can be used to follow up on these patients. At the start of the pandemic, the Centers for Medicare and Medicaid Services expanded coverage and payment for telehealth services[25]. This can significantly increase access to care, as telemedicine allows patients to have more flexibility with their appointments, limit their time away from work, and cut down on travel times and expenses[25]. A study of four large CHCs in Southern California showed success in telehealth services with 80%-85% of their clinical consultations shifting to telehealth since March of 2020 with few missed appointments[79]. Regarding colonoscopies for these patients, grassroot advocacy programs are encouraged to generate a list of community gastroenterologists to provide colonoscopies to CHC patients[79]. A qualitative study from Mexico shows that implementation of screening programs that offer FIT and colonoscopy at no cost would greatly increase CRC screening participation[26]. To alleviate knowledge gaps in patients, existing platforms should provide information about COVID-19 and extend CRC awareness throughout the year[78]. Advocacy and policy campaigns for underserved communities should utilize virtual platforms to continue their efforts amidst COVID-19[78]. Although these changes are already difficult to organize in a COVID-19 free time, implementing them now can help address these disparities and prevent their exacerbation. Making FIT and FOBT kits more accessible through mail, increasing the convenience of telehealth, and disseminating information virtually in an increasingly online world would greatly benefit these patient populations.
EFFECTS OF NEW SCREENING GUIDELINES ON RECOVERY EFFORTS
In October 2020, the United States Preventive Services Task Force drafted a recommendation to start colon cancer screening at age 45 instead of at 50, as was previously recommended[80,81]. This new recommendation is consistent with that of American Cancer Society, which lowered its recommended age for screening from 50 to 45 in June 2018[33]. According to United States Preventive Services Task Force, CRC screening for people between ages 45-49 is a grade B recommendation, meaning that there is strong evidence that there is net moderate benefit or moderate evidence that there is substantial benefit. Meanwhile, screening for people between ages 50-75 is a grade A recommendation, meaning that there is high certainty that there is substantial benefit[82].
This new recommendation would make over 20 million Americans, between the ages of 45-50, newly eligible for screening. This adds 20 million more people waiting for CRC screening in addition to the backlog of patients from COVID-19-related pauses in screening[83]. This further raises a need for a new public health strategy to ensure those at highest risk for CRC are prioritized for screening. If resources are not distributed appropriately, there is a risk of diverting healthcare resources away from those with high risk factors and alarming symptoms. This problem can potentially be addressed by making use of noninvasive stool-based screening tests and stratifying patient risk based on personal risk factors and presence of alarming symptoms[84].
CONCLUSION
While the COVID-19 pandemic has been a major disturbance to CRC screening, this disruption may result in some beneficial changes to the current screening strategies. There may be a resulting shift from current CRC screening and surveillance practices towards the development of an individualized approach based on risk factors. This will allow allocation of resources to people with high risk and prevent inappropriate use of healthcare resources for those with low risk[84]. Screening methods may also transition from direct visualization methods to stool-based screening, like FIT. Stool-based screening is relatively inexpensive compared to colonoscopies while also less invasive. If scaled appropriately, this can reduce the need for colonoscopy by up to 80%, which would allow significant healthcare savings[84-86]. Less colonoscopy load will also allow for better management of backlog and less patient exposures[45,51]. The use of telehealth can help carry out stool-based screening on a large scale, as it allows for organized outreach and increased accessibility. Telehealth implementation can increase screening rates by recognizing patients that need screening and have more convenient follow-up through phone calls and text messages[45]. Open access colonoscopies may also be adopted to help recover from COVID-19 related backlog. This could facilitate the rescheduling of colonoscopies to high-risk patients and those with positive FIT results while reducing healthcare spending by avoiding pre-procedure consultations[66,70]. Although this pandemic was a major disruption to CRC screening, adapting to this disruption may result in positive changes with individualized screening strategies, more accessible and convenient options, and better patient compliance.
Footnotes
Conflict-of-interest statement: The authors disclose no conflicts of interest or external funding for this publication.
Manuscript source: Invited manuscript
Peer-review started: January 21, 2021
First decision: March 8, 2021
Article in press: March 25, 2021
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bogach J S-Editor: Zhang L L-Editor: A P-Editor: Wu YXJ
Contributor Information
Anusri Kadakuntla, Albany Medical College, Albany Medical College, Albany, NY 12208, United States.
Tiffany Wang, Albany Medical College, Albany Medical College, Albany, NY 12208, United States.
Karen Medgyesy, Albany Medical College, Albany Medical College, Albany, NY 12208, United States.
Enxhi Rrapi, Albany Medical College, Albany Medical College, Albany, NY 12208, United States.
James Litynski, Division of Gastroenterology, Albany Medical Center, Albany, NY 12208, United States.
Gillian Adynski, National Clinician Scholars Program, Duke University School of Nursing, Durham, NC 27710, United States.
Micheal Tadros, Division of Gastroenterology, Albany Medical Center, Albany, NY 12208, United States. tadrosm1@amc.edu.
References
- 1.Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14:89–103. doi: 10.5114/pg.2018.81072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Colorectal Cancer. In: Global Cancer Observatory. 2020 [cited 22 March 2021]. Available from: https://gco.iarc.fr/today/data/factsheets/cancers/10_8_9-Colorectum-fact-sheet.pdf.
- 4.Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16:713–732. doi: 10.1038/s41575-019-0189-8. [DOI] [PubMed] [Google Scholar]
- 5.Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70:145–164. doi: 10.3322/caac.21601. [DOI] [PubMed] [Google Scholar]
- 6.Chen CT, Li L, Brooks G, Hassett M, Schrag D. Medicare Spending for Breast, Prostate, Lung, and Colorectal Cancer Patients in the Year of Diagnosis and Year of Death. Health Serv Res. 2018;53:2118–2132. doi: 10.1111/1475-6773.12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN, Jemal A, Schymura MJ, Lansdorp-Vogelaar I, Seeff LC, van Ballegooijen M, Goede SL, Ries LA. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544–573. doi: 10.1002/cncr.24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–691. doi: 10.1136/gutjnl-2015-310912. [DOI] [PubMed] [Google Scholar]
- 9.Issa IA, Noureddine M. Colorectal cancer screening: An updated review of the available options. World J Gastroenterol. 2017;23:5086–5096. doi: 10.3748/wjg.v23.i28.5086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rockey DC, Paulson E, Niedzwiecki D, Davis W, Bosworth HB, Sanders L, Yee J, Henderson J, Hatten P, Burdick S, Sanyal A, Rubin DT, Sterling M, Akerkar G, Bhutani MS, Binmoeller K, Garvie J, Bini EJ, McQuaid K, Foster WL, Thompson WM, Dachman A, Halvorsen R. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet. 2005;365:305–311. doi: 10.1016/S0140-6736(05)17784-8. [DOI] [PubMed] [Google Scholar]
- 11.Ladabaum U, Mannalithara A, Meester RGS, Gupta S, Schoen RE. Cost-Effectiveness and National Effects of Initiating Colorectal Cancer Screening for Average-Risk Persons at Age 45 Years Instead of 50 Years. Gastroenterology. 2019;157:137–148. doi: 10.1053/j.gastro.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu S, Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395:1321–1322. doi: 10.1016/S0140-6736(20)30845-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johns Hopkins University & Medicine. New Cases of COVID-19 in World Countries 2021 [cited 22 March 2021]. Available from: https://coronavirus.jhu.edu/data/new-cases.
- 14.World Health Organization. Rolling Updates on COVID-19 2020 [cited 22 March 2021]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
- 15.Argulian E. Anticipating the "Second Wave" of Health Care Strain in the COVID-19 Pandemic. JACC Case Rep. 2020;2:845–846. doi: 10.1016/j.jaccas.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diaz RS, Vergara TRC. The COVID-19 s wave: A perspective to be explored. Braz J Infect Dis. :2020: 101537. doi: 10.1016/j.bjid.2020.101537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cancino RS, Su Z, Mesa R, Tomlinson GE, Wang J. The Impact of COVID-19 on Cancer Screening: Challenges and Opportunities. JMIR Cancer. 2020;6:e21697. doi: 10.2196/21697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Cancer Society. Cancer Screening during the COVID-19 Pandemic 2020 [cited 22 March 2021]. Available from: https://www.cancer.org/healthy/find-cancer-early/cancer-screening-guidelines/cancer-screening-during-covid-19-pandemic.html.
- 19.Gralnek IM, Hassan C, Beilenhoff U, Antonelli G, Ebigbo A, Pellisé M, Arvanitakis M, Bhandari P, Bisschops R, Van Hooft JE, Kaminski MF, Triantafyllou K, Webster G, Voiosu AM, Pohl H, Dunkley I, Fehrke B, Gazic M, Gjergek T, Maasen S, Waagenes W, de Pater M, Ponchon T, Siersema PD, Messmann H, Dinis-Ribeiro M. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and COVID-19: An update on guidance during the post-lockdown phase and selected results from a membership survey. Endoscopy. 2020;52:891–898. doi: 10.1055/a-1213-5761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gralnek IM, Hassan C, Dinis-Ribeiro M. COVID-19 and endoscopy: implications for healthcare and digestive cancer screening. Nat Rev Gastroenterol Hepatol. 2020;17:444–446. doi: 10.1038/s41575-020-0312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mast CMA. Delayed Cancer Screenings-A Second Look. In: Epic Health Research Network 2020 [cited 22 March 2021]. Available from: https://ehrn.org/articles/delayed-cancer-screenings-a-second-look/
- 22.Whaley CM, Pera MF, Cantor J, Chang J, Velasco J, Hagg HK, Sood N, Bravata DM. Changes in Health Services Use Among Commercially Insured US Populations During the COVID-19 Pandemic. JAMA Netw Open. 2020;3:e2024984. doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care. Lancet Oncol. 2020;21:748–750. doi: 10.1016/S1470-2045(20)30242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitaker KL, Scott SE, Winstanley K, Macleod U, Wardle J. Attributions of cancer 'alarm' symptoms in a community sample. PLoS One. 2014;9:e114028. doi: 10.1371/journal.pone.0114028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hunt TL 2nd, Hooten WM. The Effects of COVID-19 on Telemedicine Could Outlive the Virus. Mayo Clin Proc Innov Qual Outcomes. 2020;4:583–585. doi: 10.1016/j.mayocpiqo.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unger-Saldaña K, Saldaña-Tellez M, Potter MB, Van Loon K, Allen-Leigh B, Lajous M. Barriers and facilitators for colorectal cancer screening in a low-income urban community in Mexico City. Implement Sci Commun. 2020;1:64. doi: 10.1186/s43058-020-00055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ricciardiello L, Ferrari C, Cameletti M, Gaianill F, Buttitta F, Bazzoli F, Luigi de'Angelis G, Malesci A, Laghi L. Impact of SARS-CoV-2 Pandemic on Colorectal Cancer Screening Delay: Effect on Stage Shift and Increased Mortality. Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan KK, Lau J. Cessation of cancer screening: An unseen cost of the COVID-19 pandemic? Eur J Surg Oncol. 2020;46:2154–2155. doi: 10.1016/j.ejso.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moss S, Ancelle-Park R, Brenner H International Agency for Research on Cancer. European guidelines for quality assurance in colorectal cancer screening and diagnosis. First Edition--Evaluation and interpretation of screening outcomes. Endoscopy. 2012;44 Suppl 3:SE49–SE64. doi: 10.1055/s-0032-1309788. [DOI] [PubMed] [Google Scholar]
- 30.Zorzi M, Hassan C, Capodaglio G, Baracco M, Antonelli G, Bovo E, Rugge M. Colonoscopy later than 270 days in a fecal immunochemical test-based population screening program is associated with higher prevalence of colorectal cancer. Endoscopy. 2020;52:871–876. doi: 10.1055/a-1159-0644. [DOI] [PubMed] [Google Scholar]
- 31.Lee YC, Fann JC, Chiang TH, Chuang SL, Chen SL, Chiu HM, Yen AM, Chiu SY, Hsu CY, Hsu WF, Wu MS, Chen HH. Time to Colonoscopy and Risk of Colorectal Cancer in Patients With Positive Results From Fecal Immunochemical Tests. Clin Gastroenterol Hepatol 2019; 17: 1332-1340. :e3. doi: 10.1016/j.cgh.2018.10.041. [DOI] [PubMed] [Google Scholar]
- 32.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, Rachet B, Aggarwal A. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte SJ, Etzioni R, McKenna MT, Oeffinger KC, Shih YT, Walter LC, Andrews KS, Brawley OW, Brooks D, Fedewa SA, Manassaram-Baptiste D, Siegel RL, Wender RC, Smith RA. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250–281. doi: 10.3322/caac.21457. [DOI] [PubMed] [Google Scholar]
- 34.Shaukat A, Church T. Colorectal cancer screening in the USA in the wake of COVID-19. Lancet Gastroenterol Hepatol. 2020;5:726–727. doi: 10.1016/S2468-1253(20)30191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mehrotra A, Linetsky D, Hatch H, Cutler D, Schneider EC. The Impact of the COVID-19 Pandemic on Outpatient Visits: Changing Patterns of Care in the Newest COVID-19 Hot Spots Commonwealth Fund. 2020. [Google Scholar]
- 36.Gupta S, Lieberman D. Screening and Surveillance Colonoscopy and COVID-19: Avoiding More Casualties. Gastroenterology. 2020;159:1205–1208. doi: 10.1053/j.gastro.2020.06.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marín-Gabriel JC, Santiago ER en representación de la Asociación Española de Gastroenterología y la Sociedad Española de Endoscopia Digestiva. AEG-SEED position paper for the resumption of endoscopic activity after the peak phase of the COVID-19 pandemic. Gastroenterol Hepatol. 2020;43:389–407. doi: 10.1016/j.gastrohep.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D'Souza N, Georgiou Delisle T, Chen M, Benton S, Abulafi M NICE FIT Steering Group. Faecal immunochemical test is superior to symptoms in predicting pathology in patients with suspected colorectal cancer symptoms referred on a 2WW pathway: a diagnostic accuracy study. Gut. 2020 doi: 10.1136/gutjnl-2020-321956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roundtable National Colorectal Cancer. Reigniting Colorectal Cancer Screening as Communities Face and Respond to the COVID-19 Pandemic: A Playbook 2020 [cited 22 March 2021]. Available from: https://nccrt.org/resource/a-playbook-for-reigniting-colorectal-cancer-screening-as-communities-respond-to-the-covid-19-pandemic/
- 40.Peña-Rey I, Almazán R, Rodríguez-Camacho E, Cubiella J. Resumption of endoscopy in the Galician colorectal cancer screening programme after the COVID-19 Lock down: patient safety results. Rev Esp Enferm Dig. 2021;113:119–121. doi: 10.17235/reed.2020.7647/2020. [DOI] [PubMed] [Google Scholar]
- 41.US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, García FAR, Gillman MW, Harper DM, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Owens DK, Phillips WR, Phipps MG, Pignone MP, Siu AL. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315:2564–2575. doi: 10.1001/jama.2016.5989. [DOI] [PubMed] [Google Scholar]
- 42.Colon Cancer Screening Resources and Support. Cologuard [cited 22 March 2021]. Available from: https://www.cologuardtest.com/colon-cancer-screening-support-resources.
- 43.Imperiale TF, Ransohoff DF, Itzkowitz SH, Levin TR, Lavin P, Lidgard GP, Ahlquist DA, Berger BM. Multitarget stool DNA testing for colorectal-cancer screening. N Engl J Med. 2014;370:1287–1297. doi: 10.1056/NEJMoa1311194. [DOI] [PubMed] [Google Scholar]
- 44.Ebner DW, Kisiel JB. Stool-Based Tests for Colorectal Cancer Screening: Performance Benchmarks Lead to High Expected Efficacy. Curr Gastroenterol Rep. 2020;22:32. doi: 10.1007/s11894-020-00770-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patel S, Issaka RB, Chen E, Somsouk M. Colorectal Cancer Screening and COVID-19. Am J Gastroenterol. 2021;116:433–434. doi: 10.14309/ajg.0000000000000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mehrotra A, Linetsky D, Hatch H, Cutler D. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges 2020 [cited 22 March 2021]. Available from: https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits.
- 47.Geneve N, Kairys D, Bean B, Provost T, Mathew R, Taheri N. Colorectal Cancer Screening. Prim Care. 2019;46:135–148. doi: 10.1016/j.pop.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 48.Zorzi M, Fedeli U, Schievano E, Bovo E, Guzzinati S, Baracco S, Fedato C, Saugo M, Dei Tos AP. Impact on colorectal cancer mortality of screening programmes based on the faecal immunochemical test. Gut. 2015;64:784–790. doi: 10.1136/gutjnl-2014-307508. [DOI] [PubMed] [Google Scholar]
- 49.Chiu HM, Chen SL, Yen AM, Chiu SY, Fann JC, Lee YC, Pan SL, Wu MS, Liao CS, Chen HH, Koong SL, Chiou ST. Effectiveness of fecal immunochemical testing in reducing colorectal cancer mortality from the One Million Taiwanese Screening Program. Cancer. 2015;121:3221–3229. doi: 10.1002/cncr.29462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Levin TR, Corley DA, Jensen CD, Schottinger JE, Quinn VP, Zauber AG, Lee JK, Zhao WK, Udaltsova N, Ghai NR, Lee AT, Quesenberry CP, Fireman BH, Doubeni CA. Effects of Organized Colorectal Cancer Screening on Cancer Incidence and Mortality in a Large Community-Based Population. Gastroenterology 2018; 155: 1383-1391. :e5. doi: 10.1053/j.gastro.2018.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Somsouk M, Rachocki C, Mannalithara A, Garcia D, Laleau V, Grimes B, Issaka RB, Chen E, Vittinghoff E, Shapiro JA, Ladabaum U. Effectiveness and Cost of Organized Outreach for Colorectal Cancer Screening: A Randomized, Controlled Trial. J Natl Cancer Inst. 2020;112:305–313. doi: 10.1093/jnci/djz110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet. 2014;383:1490–1502. doi: 10.1016/S0140-6736(13)61649-9. [DOI] [PubMed] [Google Scholar]
- 53.Usher-Smith JA, Walter FM, Emery JD, Win AK, Griffin SJ. Risk Prediction Models for Colorectal Cancer: A Systematic Review. Cancer Prev Res (Phila) 2016;9:13–26. doi: 10.1158/1940-6207.CAPR-15-0274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hull MA, Rees CJ, Sharp L, Koo S. A risk-stratified approach to colorectal cancer prevention and diagnosis. Nat Rev Gastroenterol Hepatol. 2020;17:773–780. doi: 10.1038/s41575-020-00368-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peng L, Weigl K, Boakye D, Brenner H. Risk Scores for Predicting Advanced Colorectal Neoplasia in the Average-risk Population: A Systematic Review and Meta-analysis. Am J Gastroenterol. 2018;113:1788–1800. doi: 10.1038/s41395-018-0209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kuipers EJ, Spaander MC. Personalized screening for colorectal cancer. Nat Rev Gastroenterol Hepatol. 2018;15:391–392. doi: 10.1038/s41575-018-0015-8. [DOI] [PubMed] [Google Scholar]
- 57.Jeon J, Du M, Schoen RE, Hoffmeister M, Newcomb PA, Berndt SI, Caan B, Campbell PT, Chan AT, Chang-Claude J, Giles GG, Gong J, Harrison TA, Huyghe JR, Jacobs EJ, Li L, Lin Y, Le Marchand L, Potter JD, Qu C, Bien SA, Zubair N, Macinnis RJ, Buchanan DD, Hopper JL, Cao Y, Nishihara R, Rennert G, Slattery ML, Thomas DC, Woods MO, Prentice RL, Gruber SB, Zheng Y, Brenner H, Hayes RB, White E, Peters U, Hsu L Colorectal Transdisciplinary Study and Genetics and Epidemiology of Colorectal Cancer Consortium. Determining Risk of Colorectal Cancer and Starting Age of Screening Based on Lifestyle, Environmental, and Genetic Factors. Gastroenterology 2018; 154: 2152-2164. :e19. doi: 10.1053/j.gastro.2018.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Park CH, Kim NH, Park JH, Park DI, Sohn CI, Jung YS. Individualized colorectal cancer screening based on the clinical risk factors: beyond family history of colorectal cancer. Gastrointest Endosc. 2018;88:128–135. doi: 10.1016/j.gie.2018.02.041. [DOI] [PubMed] [Google Scholar]
- 59.Kuipers EJ, Grobbee EJ. Personalised screening for colorectal cancer, ready for take-off. Gut. 2020;69:403–404. doi: 10.1136/gutjnl-2019-319677. [DOI] [PubMed] [Google Scholar]
- 60.Park CH, Jung YS, Kim NH, Park JH, Park DI, Sohn CI. Usefulness of risk stratification models for colorectal cancer based on fecal hemoglobin concentration and clinical risk factors. Gastrointest Endosc 2019; 89: 1204-1211. :e1. doi: 10.1016/j.gie.2019.02.023. [DOI] [PubMed] [Google Scholar]
- 61.Eberth JM, Thibault A, Caldwell R, Josey MJ, Qiang B, Peña E, LaFrance D, Berger FG. A statewide program providing colorectal cancer screening to the uninsured of South Carolina. Cancer. 2018;124:1912–1920. doi: 10.1002/cncr.31250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lamanna A, Sheaffer H, Guerra C, Kochman M. Colorectal Cancer Screening Navigation for the Underserved: Experience of an Urban Program. Gastroenterol Hepatol (N Y) 2016;12:547–551. [PMC free article] [PubMed] [Google Scholar]
- 63.Niv Y, Dickman R, Levi Z, Neumann G, Ehrlich D, Bitterman H, Dreiher J, Cohen A, Comaneshter D, Halpern E. Establishing an integrated gastroenterology service between a medical center and the community. World J Gastroenterol. 2015;21:2152–2158. doi: 10.3748/wjg.v21.i7.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kapila N, Singh H, Kandragunta K, Castro FJ. Open Access Colonoscopy for Colorectal Cancer Prevention: An Evaluation of Appropriateness and Quality. Dig Dis Sci. 2019;64:2798–2805. doi: 10.1007/s10620-019-05612-8. [DOI] [PubMed] [Google Scholar]
- 65.Ghaoui R, Ramdass S, Friderici J, Desilets DJ. Open access colonoscopy: Critical appraisal of indications, quality metrics and outcomes. Dig Liver Dis. 2016;48:940–944. doi: 10.1016/j.dld.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 66.Gingold-Belfer R, Niv Y, Horev N, Gross S, Sahar N, Dickman R. [The Failure Modes And Effects Analysis Facilitates A Safe, Time And Money Saving Open Access Colonoscopy Service] Harefuah. 2017;156:230–233. [PubMed] [Google Scholar]
- 67.Vega-Villaamil P, Salve-Bouzo M, Cubiella J, Valentín-Gómez F, Sánchez-Hernández E, Gómez-Fernández I, Fernández-Seara J. Evaluation of the implementation of Galician Health Service indications and priority levels for colonoscopy in symptomatic patients: prospective, cross-sectional study. Rev Esp Enferm Dig. 2013;105:600–608. doi: 10.4321/s1130-01082013001000005. [DOI] [PubMed] [Google Scholar]
- 68.Gunaratnam NT, Akce M, Al Natour R, Bartley AN, Fioritto AF, Hanson K, Ladabaum U. Screening for Cancer Genetic Syndromes With a Simple Risk-Assessment Tool in a Community-Based Open-Access Colonoscopy Practice. Am J Gastroenterol. 2016;111:589–593. doi: 10.1038/ajg.2016.84. [DOI] [PubMed] [Google Scholar]
- 69.Kastrinos F, Allen JI, Stockwell DH, Stoffel EM, Cook EF, Mutinga ML, Balmaña J, Syngal S. Development and validation of a colon cancer risk assessment tool for patients undergoing colonoscopy. Am J Gastroenterol. 2009;104:1508–1518. doi: 10.1038/ajg.2009.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xiao AH, Chang SY, Stevoff CG, Komanduri S, Pandolfino JE, Keswani RN. Adoption of Multi-society Guidelines Facilitates Value-Based Reduction in Screening and Surveillance Colonoscopy Volume During COVID-19 Pandemic. Dig Dis Sci. 2020 doi: 10.1007/s10620-020-06539-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Riggs KR, Segal JB, Shin EJ, Pollack CE. Prevalence and Cost of Office Visits Prior to Colonoscopy for Colon Cancer Screening. JAMA. 2016;315:514–515. doi: 10.1001/jama.2015.15278. [DOI] [PubMed] [Google Scholar]
- 72.Doubeni CA, Laiyemo AO, Major JM, Schootman M, Lian M, Park Y, Graubard BI, Hollenbeck AR, Sinha R. Socioeconomic status and the risk of colorectal cancer: an analysis of more than a half million adults in the National Institutes of Health-AARP Diet and Health Study. Cancer. 2012;118:3636–3644. doi: 10.1002/cncr.26677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Carmichael H, Cowan M, McIntyre R, Velopulos C. Disparities in colorectal cancer mortality for rural populations in the United States: Does screening matter? Am J Surg. 2020;219:988–992. doi: 10.1016/j.amjsurg.2019.09.027. [DOI] [PubMed] [Google Scholar]
- 74.Doubeni CA, Major JM, Laiyemo AO, Schootman M, Zauber AG, Hollenbeck AR, Sinha R, Allison J. Contribution of behavioral risk factors and obesity to socioeconomic differences in colorectal cancer incidence. J Natl Cancer Inst. 2012;104:1353–1362. doi: 10.1093/jnci/djs346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hall IJ, Tangka FKL, Sabatino SA, Thompson TD, Graubard BI, Breen N. Patterns and Trends in Cancer Screening in the United States. Prev Chronic Dis. 2018;15:E97. doi: 10.5888/pcd15.170465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Joseph DA, King JB, Dowling NF, Thomas CC, Richardson LC. Vital Signs: Colorectal Cancer Screening Test Use - United States, 2018. MMWR Morb Mortal Wkly Rep. 2020;69:253–259. doi: 10.15585/mmwr.mm6910a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.White PM, Itzkowitz SH. Barriers Driving Racial Disparities in Colorectal Cancer Screening in African Americans. Curr Gastroenterol Rep. 2020;22:41. doi: 10.1007/s11894-020-00776-0. [DOI] [PubMed] [Google Scholar]
- 78.Balzora S, Issaka RB, Anyane-Yeboa A, Gray DM 2nd, May FP. Impact of COVID-19 on colorectal cancer disparities and the way forward. Gastrointest Endosc. 2020;92:946–950. doi: 10.1016/j.gie.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nodora JN, Gupta S, Howard N, Motadel K, Propst T, Rodriguez J, Schultz J, Velasquez S, Castañeda SF, Rabin B, Martínez ME. The COVID-19 Pandemic: Identifying Adaptive Solutions for Colorectal Cancer Screening in Underserved Communities. J Natl Cancer Inst. 2020 doi: 10.1093/jnci/djaa117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.US Preventative Services Task Force. Colorectal Cancer: Screening 2020 [cited 22 March 2021]. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/colorectal-cancer-screening3.
- 81.US Preventative Services Task Force. Colorectal Cancer: Screening 2016 [cited 22 March 2021]. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening.
- 82.US Preventive Services Task Force. Grade Definitions after July 2012 [cited 22 March 2021]. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/grade-definitions.
- 83.Statista Resident Population of the United States by Sex and Age as of July 1, 2019 [cited 22 March 2021]. Available from: https://www.statista.com/statistics/241488/population-of-the-us-by-sex-and-age/
- 84.Nunoo-Mensah JW, Giordano P, Chung-Faye G. COVID-19: An Opportunity to Reimagine Colorectal Cancer Diagnostic Testing-A New Paradigm Shift. Clin Colorectal Cancer. 2020;19:227–230. doi: 10.1016/j.clcc.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Knudsen AB, Zauber AG, Rutter CM, Naber SK, Doria-Rose VP, Pabiniak C, Johanson C, Fischer SE, Lansdorp-Vogelaar I, Kuntz KM. Estimation of Benefits, Burden, and Harms of Colorectal Cancer Screening Strategies: Modeling Study for the US Preventive Services Task Force. JAMA. 2016;315:2595–2609. doi: 10.1001/jama.2016.6828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lee JK, Liles EG, Bent S, Levin TR, Corley DA. Accuracy of fecal immunochemical tests for colorectal cancer: systematic review and meta-analysis. Ann Intern Med. 2014;160:171. doi: 10.7326/M13-1484. [DOI] [PMC free article] [PubMed] [Google Scholar]