Abstract
Background
Recently the performance rate of one anastomosis gastric bypass (OAGB) bariatric surgery has increased. Bile reflux is on of common considered complication of OAGB challenging surgeon.
Methods
We searched English full text with keyword “bile reflux” AND “OAGB” OR “one anastomosis gastric bypass” OR “SAGB” OR “single anastomosis gastric bypass” that published from January 1st, 2000 to December 31st, 2020 in PubMed, EMBASE, Google scholar and Cochrane Library. We included prospective or retrospective systematic review, review, clinical, and meta-analysis human article that its full text was available and focused on bile reflux after OAGB/SAGB as the fundamental performed bariatric surgery.
Results
A total of 1259 articles were analyzed, of which 5 were included. Analysis of number articles by year revealed that 2019 and 2020 was the highest number of published articles (n = 232; 68%). Study type analysis revealed that review studies and clinical research (n = 62; 18.2%) were the most frequent study types. Reported data on bile reflux after OAGB had diversity. Implicitly, postoperative incidence of bile reflux differed from 7.8 to 55.5%. General consensus was not existed among authors to consider the OAGB as the first suspect leading to postoperative bile reflux among other bariatric surgery types.
Conclusion
Although surgeons prefer to conduct OAGB procedure because of its easier surgical approach needing just one anastomosis formation it is not virtually clear that is the procedure costly benefitted regarding bile reflux outcomes.
Keywords: Bile reflux, Bariatric surgery, Gastric bypass, OAGB, One anastomosis
Highlights
-
•
Review of the literature shows bile reflux is a not well understood complication after OAGB.
-
•
Regarding current data incidence of bile reflux after OAGB varied from 8 to over 55%.
-
•
It seems current surgical technique is not influenced on incidence of bile reflux after OAGB.
1. Introduction
Obesity is a hazardous public health concern due to its vigorous well known metabolic side effects [1]. Obesity refers to a body mass index (BMI) greater than or equal to 30 kg/m2 [2]. Nowadays near 1.7 billion people around the world, specifically in modern countries, suffer from obesity with BMI ≥30 kg/m2 [3]. Metabolic syndrome, type 2 diabetes mellitus, premature osteoarthritis, obstructive sleep apnea, and also cardiovascular diseases which could lead to mortality are commonly seen among obese patient [4]. Therefore, any patient with a calculated BMI ≥30 kg/m2 is a candidate to have regular exercise, life style modification, and dietary consult to lose weight. Medical treatment was not satisfying. According to increased risk of fatal complication in patient whether with 35≤ BMI< 40 kg/m2 and concurrent obesity related symptoms or BMI ≥40 kg/m2 surgery is preserved to decrease weight [5]. Bariatric surgery is a relatively novel interventional approach that its efficacy was implied to reduce appropriate weight, metabolic disturbances, obesity complication, and disease expense in combination with increasing in overall survival, social and psychosomatic function [6]. Since bariatric surgeries generally conduct via laparoscopic approach, therefore, better intra-operative view with lesser organ injuries in addition to shorter postoperative recovery time is expected if those are performed by an experienced laparoscopic surgeon. Currently laparoscopic bariatric surgeries are increasingly conducted worldwide because weight change, improvement of obesity and metabolic symptoms, and recovery time all are satisfying for either the patient or the surgeon in compared with medical treatment [7]. Bariatric surgeries lead to weight loss through both reducing primary food intake and following alimentary absorption [8]. Considering surgical technique to perform bariatric surgery it should be mentioned to most common current approaches including Roux-en-Y gastric bypass (RYGB), Sleeve gastrectomy (SG), and one anastomosis gastric bypass (OAGB). Although these surgical approaches have been improved gradually through the time no one is absolutely preferred for all patients yet, additionally complication events always are probable for any selected technique [9]. Among all above bariatric surgeries the OAGB has been increasingly performed recently in comparison with others. Namely it placed third following SG and RYGB in 2016 with 4.8% of prevalence rate of conduction [10]. Surgery authors have welcomed to OAGB since last 20 years and the result is many studies concentrated on OAGB safety and details of technique consideration [11,12]. The mostly prominent complication after OAGB is bile reflux which finalize to esophageal cancer if does not diagnose and treat in time. This complication was sufficient enough for many surgeons to avoid them selecting OAGB as their routine technique for patients [13,14]. Although available data shows that esophageal dysplasia due to bile reflux following OAGB is very rare, worsening preoperative and resulting in de novo gastroesophageal reflux is seen yet relatively common [12]. If postoperative bile reflux following OAGB is detected the next step would be change the OAGB to RYGB through the surgery. Despite bile reflux, since easier surgical technique to perform OAGB than the RYGB is needed many surgeons advocate and also recommend the OAGB [15] but ever it seems comprehensive idea about bile reflux after OAGB is lacking. To find an evidence based answer of the question that asks is at last recommendation and widely performance of laparoscopic gastric bypass with one anastomosis approach is costly benefited while considering incidence of postoperative bile reflux, we have reviewed previously published work concentrated on bile reflux after OAGB to prepare a panel for comparing current data and also to find the answer for study question.
2. Methods
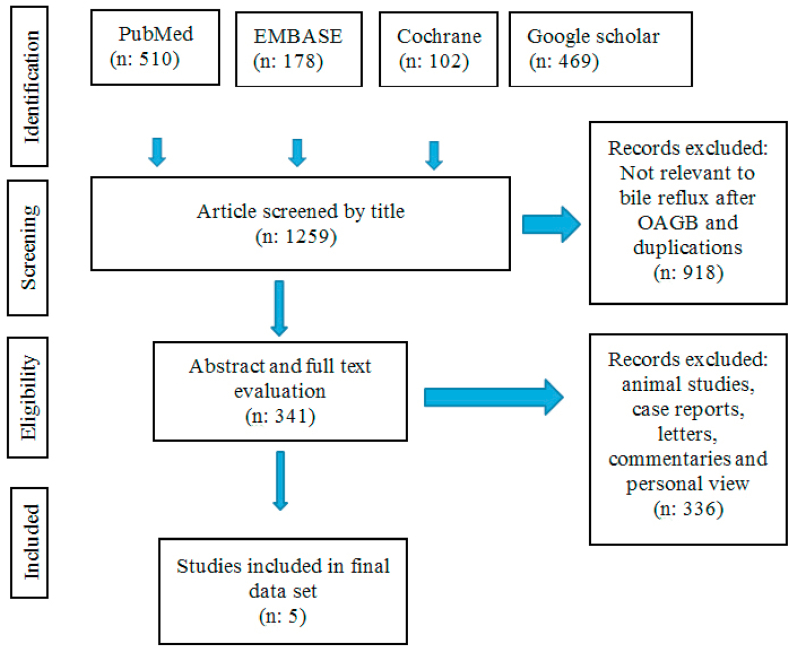
We search in Pubmed, EMBASE, Google scholar and Cochrane Library using keyword “bile reflux” AND “OAGB” OR “one anastomosis gastric bypass” OR “SAGB” OR “single anastomosis gastric bypass”. We added English full text and 20 years publications in filter searching engine. The search resulted in a total of 1259 articles from January 1st, 2000 until December 31st, 2020. We included the articles that discussed about bile reflux following OAGB/SAGB. All original human articles including clinical study, systematic review, review articles, and meta-analysis that published in selected 20 years were included. We excluded the book sections, conference presentations, guidelines, commentaries, animal studies or personal review. The PRISMA guidelines [16] for conducting the review were followed (Fig. 1).
Fig. 1.
PRISMA flow chart of the article selection process.
All abstract were screened independently by two reviewers to determine whether it met eligibility criteria. The full articles of eligible studies were reviewed and included into the study for further data extraction and analysis. Extracted data from included studies was visualized in table.
3. Results
A total of 1259 articles which published in a 20 years interval were analyzed, of that 5 were included. Analysis of number articles by year revealed that the highest number of publication namely authors’ attention to the bile reflux following OAGB surgery was in 2019 and 2020. Of all relative studies 232(68%) articles have been published in mentioned years. Among all type of studies reviews and clinical researches (n = 62; 18.2%) were mostly frequent and involved 18.2% (62) of all. Considering eligible 5 studies to review all were designed as cohort clinical research. Table 1 shows extracted data from reviewed articles. As Table 1 manifests incidence of bile reflux after an OAGB procedure differs from 7.8 to 55.5% which is relatively frequent complication.
Table 1.
Characteristics of studies focused on bile reflux after one anastomosis gastric bypass surgery.
| Author | Number | Report Year |
Study design | Preoperative BMI(kg/m2) | EWL1 | Bile reflux incidence | Follow up interval (m) | Diagnostic method | Operation characteristic | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Saarinen | 40 | 2020 | cohort | 45.2 (35.4–62) | N/A | 12 (31.6%) | 6 | bile reflux scintigraphy EGD2 gastric pouch biopsy |
gastric tube: 15 cm antecolic biliopancreatic limb: 210 cm stapler: 45 mm |
postoperative bile reflux in the gastric pouch after OAGB4 is a common finding in scintigraphy and endoscopy |
| Lasheen | 40 | 2019 | cohort | 44.31 | 81.2% | 8 (20%) | 12 | EGD histopathological examination gastric juice aspiration |
gastric tube: 18 cm antecolic biliopancreatic limb: 200 cm from DJF stapler: 40 mm |
20% of patients under OAGB suffered from biliary reflux |
| Keleidari | 122 | 2019 | cohort | 41.7 ± 2.6 | 16.86 ± 1.98 Kg |
5 (7.8%) | 12 | the Sydney scoring system for bile reflux EGD gastric pouch biopsy |
gastric tube:18–22 cm antecolic biliopancreatic limb: 150–200 cm stapler: 45 mm |
OAGB and RYGB5 are similar in creating biliary reflux |
| Saarinen | 9 | 2017 | cohort | 43.1 (34.2–54.6) | 83.9% (49.5–128.3) | 5 (55.5%) | 12 | hepatobiliary scintigraphy reflux symptom questionnaire(GerdQ) EGD gastric pouch biopsy |
gastric tube:15 cm antecolic biliary limb: 250–275 cm stapler: 40 mm |
one patient with positive scintigraphy in the gastric tube required re-operation |
| Shenouda | 20 | 2017 | cohort (pilot) | 47 (38–61) | 74% (60–84) | 6 (30%) | 6 | EGD histopathological examination gastric juice aspiration |
gastric tube: 18 cm or slightly more antecolic gastrojejunostomy: 200 cm from DJF stapler: 30 mm |
biliary gastritis presented in 30% of patients and significant relationship between bilirubin level and severity of inflammation was existed |
1 Estimated weight loss, 2 esophagogastrodeudenoscopy, 3 duodenojujenal flexure, 4 one anastomosis gastric bypass, 5 roux-en-y gastric bypass.
4. Discussion
Bile reflux is generally a rare complication while considering all types of bariatric surgeries. Since bile reflux could lead to esophageal cancer any sign and/or symptoms after bariatric surgeries should be paid attention to reduce the risk of esophageal malignant changes. Therefore, reoperation is preserved for patient suffering from bile reflux after bariatric surgery. Since bile reflux is relatively a common complication after OAGB procedure, revision to RYGB is optimal approach when bile reflux presents following previously performed OAGB [[13], [14], [15]]. Although pathophysiologic clues to clearly describe bile reflux mechanism isn't sufficient for different types of bariatric surgeries in case of OAGB development of whether a gastrogastric fistula or any gastric punch is introduced. Since probability for generation of these two latter operative related disorders are relatively higher in OAGB than to the other types of bariatric surgeries, therefore, authors have attributed the higher incidence of bile reflux following OAGB to gastric punch or fistula [15,[17], [18], [19], [20]]. Diagnosis of bile reflux occurs by scintigraphy, esophagogastroduodenoscopy (EGD), histopathologic examination on tissue biopsy, and biochemistric evaluation of bilirubin level in aspirated gastric juice. Whenever the diagnosis of bile reflux is confirmed because of its treatable nature patient is then indicated for surgery; namely revision of OAGB to RYGB [15]. The latter approach is also clinically effective if previously performed Braun's jejunojejunostomy has failed to prevent bile reflux [15]. Despite higher incidence of Postoperative bile reflux in OAGB trends to select of this procedure is not also declined but has increased recently. Reasons for the latter include easier surgical technique, needing one anastomosis, shorter time of surgery, fast postoperative recovery, and having treatment if bile reflux appears [[17], [18], [19]].
Shenouda et al. published a cohort (pilot) study among 20 patients with preoperative BMI 47(38–61) kg/m2. They made OAGB by constructing 18 cm gastric pouch and an antecolic gastrojejunostomy with 30 mm stapler while biliopancreatic limb length was considered 200 cm from duodenojejunal flexure. After 6 months of OAGB operation patients underwent surveillance diagnostic EGD, gastric biopsy, histopathologic examination, and biochemical examination of bile in aspirated gastric juice. Of all 30%(6) had bile reflux. They also represented that bilirubin level in aspirated gastric juice was significantly elevated in bile reflux. Details of the study regarded also a significant relationship between bilirubin level of aspirated gastric juice and the degree of inflammation in 18(90%) patients. However, while 2(10%) patients had moderate to severe gastritis the measured bilirubin level in aspirated gastric juice was normal for them. The author described that bilirubin level of aspirated gastric juice above than 20 mg/dL could be associated with severe esophagitis, erosive gastritis, or gastroesophageal metaplastic changes [21].
Saarinen et al. presented a cohort study in 2017 among 9 patients. Subjects had preoperative BMI 43.1(34.2–54.6) kg/m2. The OAGB was accomplished through making 15 cm gastric tube followed by an anastomosis formation with 40 mm stapler and an antecolic 250–270 cm biliary limb construction. To diagnose postoperative bile reflux after 12 months they applied hepatobiliary scintigraphy, EGD, gastric pouch biopsy examination, in addition to filling reflux symptom questionnaire (GerdQ). The result was presence of bile reflux among 55.5%(5) of all. Eventually one subject due to severe symptoms of bile reflux underwent reoperation [20].
Three years later, in 2020, again in a cohort study Saarinen et al. evaluated 40 patients with preoperative BMI 45.2(35.4–62) kg/m2 who underwent OAGB. This time, surgical technique changed except for gastric tube length. They constructed the anastomosis by using 45 mm stapler and an antecolic 210 cm biliopancreatic limb. Incidence of bile reflux after 6 months of operation reached to 31.6%(12) by using scintigraphy test, EGD, and gastric pouch biopsy pathologic study. Details of the study manifested that gastric puncture was the reason for bile reflux among all investigated subjects. The author was finally convinced that bile reflux after OAGB surgery is a common complication [22].
Lasheen et al. conducted a cohort study in 2019, to investigate postoperative bile reflux after OAGB. They involved 40 patients with preoperative BMI 44.3 kg/m2. Intraoperative technique proceeded by making 18 cm gastric pouch following an antecolic 200 cm biliopancreatic limb from duodenojejunal flexure and using 40 mm stapler for anastomosis construction. Diagnostic EGD and histopathologic study on gastric tissue in addition to biochemical examination of bilirubin in aspirated gastric juice was performed 12 months after operation. The incidence of bile reflux was reported 20%(8) [18].
Keleidari et al. performed another cohort study on 122 patients in 2019. They tried to compare incidence rate of bile reflux between OAGB and RYGB. Of all 64(52.4%) underwent OAGB, that shows author's trend to perform OAGB was a bit higher than to do RYGB. Preoperative BMI among OAGB candidates was measured 41.7 ± 2.6 kg/m2. In operating room for OAGB they made a gastric pouch with 18–22 cm in length which followed by constructing an anastomosis by 45 mm stapler and an antecolic 250–275 cm biliary limb. The Sydney scoring system for bile reflux, EGD, and gastric tissue examination were included for diagnosis of postoperative bile reflux. Bile reflux incidence rate was 7.8%(5) after 12 months of OAGB surgery while it was 3.4%(2) after RYGB. Finally author concluded that there was no significant difference for presence of bile reflux whether considering OAGB or RYGB [19].
Finally, considering available data, bile reflux incidence after OAGB operation varies from 7.8 to 55.5%. This relatively wide span of postoperative bile reflux after OAGB may due to different reasons including sample size, subjects’ demographic characteristics, preoperative BMI, applying surgical technique, size of gastric pouch, diameter of anastomosis site, length of biliopancreatic limb, time of surgery, time of follow up and condition of other concurrent metabolic disorders at the time of surgery [[23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38]]. Hence, it is highly recommended to design studies with greater sample size and more isolated consideration specifically for surgical technique characteristics to have more precise decision while bile reflux after OAGB is considered.
It should be noted as limiting point of the study that data was extracted from some medical literature sources but not all of them were discovered, therefore some of related reports may be missed. Although available data about laparoscopic gastric bypass is expanded finding studies with specific concentration on an issue is not easy and methods are not necessarily identical which makes difficulty comparing the results. Considering the latter we had to omit any study which was not specifically performed for bile reflux after OAGB.
5. Conclusion
Bile reflux after OAGB surgery is a relatively common complication which if untreated makes proximal tissue to anastomosis site, esophagus in particular, susceptible to malignant degeneration. Although RYGB is preserved for such condition varied incidence rate of bile reflux in literature implies on that there are conditions in which decrease the possibility of the event. Investigation of these conditions through further studies should prepare more safety after OAGB surgery which has been welcomed recently.
Provenance and peer review
Not commissioned, externally peer reviewed.
Ethics approval and consent to participate
This study was performed under supervision of Isfahan University of Medical Sciences.
Consent for publication
Not applicable.
Availability of data and material
The data used to support findings of this study is available in medical literature.
Funding
This study was conducted under order and supervision of Isfahan University of Medical Sciences and all advantages referred back to this university.
Author contribution
Behrouz Keleidari: study design, data collection, interpret results.
Mohsen Mahmoudieh Dehkordi: study design, supervision, data collection, interpret results.
Masoud Sayadi Shahraki: study design, supervision, interpret results.
Hossein Taheri Nasaj: study design, data collection, data analysis.
Mahmoud Heidari: study design, data collection, data analysis.
Zeinab Sadat Ahmadi: study design, data collection.
Abbas Hajian: Study design, interpret results, article draft.
Registration of research studies
This study was conducted under supervision of the Isfahan University of Medical Sciences.
Guarantor
Abbas Hajian.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgment
We present our great thanks to departments of general and laparoscopic surgery of the School of Medicine in Isfahan University of Medical Sciences, Isfahan, Iran.
Contributor Information
Behrouz Keleidari, Email: Alago83@yahoo.com.
Mohsen Mahmoudieh Dehkordi, Email: Mahmoudieh46@gmail.com.
Masoud Sayadi Shahraki, Email: Drsayadi@yahoo.com.
Zeinab Sadat Ahmadi, Email: Drzahmadi@yahoo.com.
Mahmoud Heidari, Email: Dr.m.heydari1365@gmail.com.
Abbas Hajian, Email: Abbashajian@ymail.com.
Hossein Taheri Nasaj, Email: Dr.taherinasaj@gmail.com.
References
- 1.Lee P.C., Dixon J. Medical devices for the treatment of obesity. Nat. Rev. Gastroenterol. Hepatol. 2017;14(9):553–564. doi: 10.1038/nrgastro.2017.80. [DOI] [PubMed] [Google Scholar]
- 2.Mechanick J.I., Youdim A., Jones D.B., Garvey W.T., Hurley D.L., McMahon M.M. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity. 2013;21(S1) doi: 10.1002/oby.20461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buchwald H., Avidor Y., Braunwald E., Jensen M.D., Pories W., Fahrbach K. Bariatric surgery: a systematic review and meta-analysis. Jama. 2004;292(14):1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 4.Coblijn U.K., Goucham A.B., Lagarde S.M., Kuiken S.D., van Wagensveld B.A. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes. Surg. 2014;24(2):299–309. doi: 10.1007/s11695-013-1118-5. [DOI] [PubMed] [Google Scholar]
- 5.Elrazek A.E.M.A.A., Elbanna A.E.M., Bilasy S.E. Medical management of patients after bariatric surgery: principles and guidelines. World J. Gastrointest. Surg. 2014;6(11):220. doi: 10.4240/wjgs.v6.i11.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vegel A.J., Shah N., Lidor A.O., Greenberg J.A., Shan Y., Wang X. Patient-reported quality of life after bariatric surgery: a single institution analysis. J. Surg. Res. 2017;218:117–123. doi: 10.1016/j.jss.2017.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thereaux J., Lesuffleur T., Païta M., Czernichow S., Basdevant A., Msika S. Long‐term follow‐up after bariatric surgery in a national cohort. Br. J. Surg. 2017;104(10):1362–1371. doi: 10.1002/bjs.10557. [DOI] [PubMed] [Google Scholar]
- 8.Concors S.J., Ecker B.L., Maduka R., Furukawa A., Raper S.E., Dempsey D.D. Complications and surveillance after bariatric surgery. Curr. Treat. Options Neurol. 2016;18(1):5. doi: 10.1007/s11940-015-0383-0. [DOI] [PubMed] [Google Scholar]
- 9.Adams T.D., Davidson L.E., Litwin S.E., Kim J., Kolotkin R.L., Nanjee M.N. Weight and metabolic outcomes 12 years after gastric bypass. N. Engl. J. Med. 2017;377(12):1143–1155. doi: 10.1056/NEJMoa1700459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angrisani L., Santonicola A., Iovino P. IFSO Worldwide Survey 2016: primary, endoluminal and revisional procedures. Obes. Surg. 2018;28(3):3783–3794. doi: 10.1007/s11695-018-3450-2. [DOI] [PubMed] [Google Scholar]
- 11.Rutledge R. The mini-gastric bypass: experience with the first 1, 274 cases. Obes. Surg. 2001 Jun;11(3):276–280. doi: 10.1381/096089201321336584. [DOI] [PubMed] [Google Scholar]
- 12.Parmar C.D., Mahawar K.K. One anastomosis (mini) gastric bypass is now an established bariatric procedure: a systematic review of 12, 807 patients. Obes. Surg. 2018 Sep;28(9):2956–2967. doi: 10.1007/s11695-018-3382-x. [DOI] [PubMed] [Google Scholar]
- 13.Lee W.J., Almalki O.M., Ser K.H. Randomized controlled trial of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity: comparison of the YOMEGA and Taiwan studies. Obes. Surg. 2019 Sep;29(9):3047–3053. doi: 10.1007/s11695-019-04065-2. [DOI] [PubMed] [Google Scholar]
- 14.Mahawar K.K., Borg C.M., Kular K.S. Understanding objections to one anastomosis (mini) gastric bypass: a survey of 417 surgeons not performing this procedure. Obes. Surg. 2017;27(9):2222–2228. doi: 10.1007/s11695-017-2663-0. [DOI] [PubMed] [Google Scholar]
- 15.Nimeri A., Al Shaban T., Maasher A. Conversion of one anastomosis gastric bypass/mini gastric bypass to Roux-en-Y gastric bypass for bile reflux gastritis after failed Braun jejunojejunostomy. Surg. Obes. Relat. Dis. 2017 Feb 1;13(2):361–363. doi: 10.1016/j.soard.2016.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haddad A., Bashir A., Nimeri A. Gastrogastric fistula: an unusual cause for severe bile reflux following conversion of Sleeve gastrectomy to one anastomosis gastric bypass. 2018. [DOI] [PubMed]
- 18.Lasheen M., Mahfouz M., Salama T., Salem H.E. 2019. Biliary reflux gastritis after mini gastric bypass: the effect of bilirubin level. [Google Scholar]
- 19.Keleidari B., Mahmoudieh M., Jazi A.H., Melali H., Esfahani F.N., Minakari M., Mokhtari M. Comparison of the bile reflux frequency in one anastomosis gastric bypass and roux-en-Y gastric bypass: a cohort study. Obes. Surg. 2019 Jun 15;29(6):1721–1725. doi: 10.1007/s11695-018-03683-6. [DOI] [PubMed] [Google Scholar]
- 20.Saarinen T., Pietiläinen K.H., Loimaala A., Ihalainen T., Sammalkorpi H., Penttilä A., Juuti A. Bile reflux is a common finding in the gastric pouch after one anastomosis gastric bypass. Obes. Surg. 2020 Mar;30(3):875–881. doi: 10.1007/s11695-019-04353-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shenouda M.M., Harb S.E., Mikhail S.A., Mokhtar S.M., Osman A.M., Wassef A.T., Rizkallah N.N., Milad N.M., Anis S.E., Nabil T.M., Zaki N.S. Bile gastritis following laparoscopic single anastomosis gastric bypass: pilot study to assess significance of bilirubin level in gastric aspirate. Obes. Surg. 2018;28(2):389–395. doi: 10.1007/s11695-017-2885-1. [DOI] [PubMed] [Google Scholar]
- 22.Saarinen T., Pietiläinen K.H., Loimaala A., Ihalainen T., Sammalkorpi H., Penttilä A., Juuti A. Bile reflux is a common finding in the gastric pouch after one anastomosis gastric bypass. Obes. Surg. 2020 Mar;30(3):875–881. doi: 10.1007/s11695-019-04353-x. PMID: 31853864; PMCID: PMC7347680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee W.J., Lin Y.H. Single-anastomosis gastric bypass (SAGB): appraisal of clinical evidence. Obes. Surg. 2014 Oct;24(10):1749–1756. doi: 10.1007/s11695-014-1369-9. PMID: 25056233. [DOI] [PubMed] [Google Scholar]
- 24.Bruzzi M., Duboc H., Gronnier C., Rainteau D., Couvelard A., Le Gall M., Bado A., Chevallier J.M. Long-term evaluation of biliary reflux after experimental one-anastomosis gastric bypass in rats. Obes. Surg. 2017;27(4):1119–1122. doi: 10.1007/s11695-017-2577-x. [DOI] [PubMed] [Google Scholar]
- 25.Csendes A. Bile reflux after one anastomosis gastric bypass. Obes Surg. 2020 Jul;30(7):2802–2803. doi: 10.1007/s11695-020-04567-4. PMID: 32277329. [DOI] [PubMed] [Google Scholar]
- 26.Facchiano E., Leuratti L., Veltri M., Lucchese M. Laparoscopic conversion of One anastomosis gastric bypass to roux-en-Y gastric bypass for chronic bile reflux. Obes. Surg. 2016 Mar;26(3):701–703. doi: 10.1007/s11695-015-2017-8. PMID: 26746224. [DOI] [PubMed] [Google Scholar]
- 27.Nimeri A., Al Shaban T., Maasher A. Laparoscopic conversion of one anastomosisgastric bypass/mini gastric bypass to Roux-en-Y gastric bypass for bile refluxgastritis. Surg. Obes. Relat. Dis. 2017 Jan;13(1):119–121. doi: 10.1016/j.soard.2016.09.033. Epub 2016 Sep 29. PMID: 27825579. [DOI] [PubMed] [Google Scholar]
- 28.Braghetto I., Csendes A. Single anastomosis gastric bypass (one anastomosisgastric bypass or mini gastric bypass): the experience with billroth ii must be considered and is a challenge for the next years. Arq Bras Cir Dig. 2017 Oct-Dec;30(4):267–271. doi: 10.1590/0102-6720201700040010. PMID: 29340552; PMCID:PMC5793146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kassir R., Petrucciani N., Debs T., Juglard G., Martini F., Liagre A. Conversion of one anastomosis gastric bypass (OAGB) to roux-en-Y gastric bypass (RYGB) for biliary reflux resistant to medical treatment: lessons learned from a retrospective series of 2780 consecutive patients undergoing OAGB. Obes. Surg. 2020 Jun;30(6):2093–2098. doi: 10.1007/s11695-020-04460-0. PMID: 32052289. [DOI] [PubMed] [Google Scholar]
- 30.Bashah M., Aleter A., Baazaoui J., El-Menyar A., Torres A., Salama A. Single anastomosis duodeno-ileostomy (SADI-S) versus one anastomosis gastric bypass (OAGB-MGB) as revisional procedures for patients with weight recidivism after Sleeve gastrectomy: a comparative analysis of efficacy and outcomes. Obes. Surg. 2020 Dec;30(12):4715–4723. doi: 10.1007/s11695-020-04933-2. Epub 2020 Aug 26. PMID: 32845477; PMCID: PMC7719107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sheikh L., Pearless L.A., Booth M.W. Laparoscopic silastic ring mini-gastric bypass (SR-MGBP): up to 11-year results from a single centre. Obes. Surg. 2017 Sep;27(9):2229–2234. doi: 10.1007/s11695-017-2659-9. PMID: 28378207. [DOI] [PubMed] [Google Scholar]
- 32.Perez Galaz F., Moedano Rico K., Lopez-Acosta M.E., Raffoul Cohen I., Cervantes Gutierrez O., Cuevas Bustos R., Perez Tristan F.A., Jafif Cojab M. Conversion from mini bypass to laparoscopic Roux en Y gastric bypass in an emergency setting: case report and literature review. Int J Surg Case Rep. 2020;75:32–36. doi: 10.1016/j.ijscr.2020.08.032. Epub 2020 Aug 31. PMID: 32901216; PMCID:PMC7457964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahawar K.K., Borg C.M., Kular K.S., Courtney M.J., Sillah K., Carr W.R.J., Jennings N., Madhok B., Singhal R., Small P.K. Understanding objections to one anastomosis (mini) gastric bypass: a survey of 417 surgeons not performing this procedure. Obes. Surg. 2017 Sep;27(9):2222–2228. doi: 10.1007/s11695-017-2663-0. PMID:28361493. [DOI] [PubMed] [Google Scholar]
- 34.Kassir R., Giudicelli X., Lointier P., Breton C., Blanc P. Omega loop gastroileal bypass (OLGIBP/SAGI) versus one anastomosis gastric bypass (OAGB): medium-term results. Obes. Surg. 2021 Jan 7 doi: 10.1007/s11695-020-05165-0. Epub ahead of print. PMID: 33409980. [DOI] [PubMed] [Google Scholar]
- 35.Surve A., Cottam D., Sanchez-Pernaute A., Torres A., Roller J., Kwon Y., Mourot J., Schniederjan B., Neichoy B., Enochs P., Tyner M., Bruce J., Bovard S., Roslin M., Jawad M., Teixeira A., Srikanth M., Free J., Zaveri H., Pilati D., Bull J., Belnap L., Richards C., Medlin W., Moon R., Cottam A., Sabrudin S., Cottam S., Dhorepatil A. The incidence of complications associated with loop duodeno-ileostomy after single- anastomosis duodenal switch procedures among 1328 patients: a multicenter experience. Surg. Obes. Relat. Dis. 2018 May;14(5):594–601. doi: 10.1016/j.soard.2018.01.020. Epub 2018 Feb 2. PMID: 29530597. [DOI] [PubMed] [Google Scholar]
- 36.Bindal V., Sudan R. Has mini gastric bypass come of age? Surg. Obes. Relat. Dis. 2015 Mar-Apr;11(2):326–327. doi: 10.1016/j.soard.2014.10.001. Epub 2014 Oct 7.PMID: 25620434. [DOI] [PubMed] [Google Scholar]
- 37.Karcz W.K., Kuesters S., Marjanovic G., Grueneberger J.M. Duodeno-enteral omega switches - more physiological techniques in metabolic surgery. Wideochir Inne Tech Maloinwazyjne. 2013 Dec;8(4):273–279. doi: 10.5114/wiitm.2013.39647. Epub 2013 Dec 22. PMID: 24501596; PMCID: PMC3908648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shim J.H., Oh S.I., Yoo H.M., Jeon H.M., Park C.H., Song K.Y. Roux-en-Y gastrojejunostomy after totally laparoscopic distal gastrectomy: comparison with Billorth II reconstruction. Surg. Laparosc. Endosc. Percutaneous Tech. 2014 Oct;24(5):448–451. doi: 10.1097/SLE.0b013e31829014ea. PMID: 24710243. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support findings of this study is available in medical literature.