Abstract
Purpose
To provide an updated comparison between modern arthroscopic and mini-open repairs for treating rotator cuff tears.
Methods
Multiple online databases were searched from 2010 to October 1st, 2020. A meta-analysis was conducted for patient-reported outcomes and complications.
Results
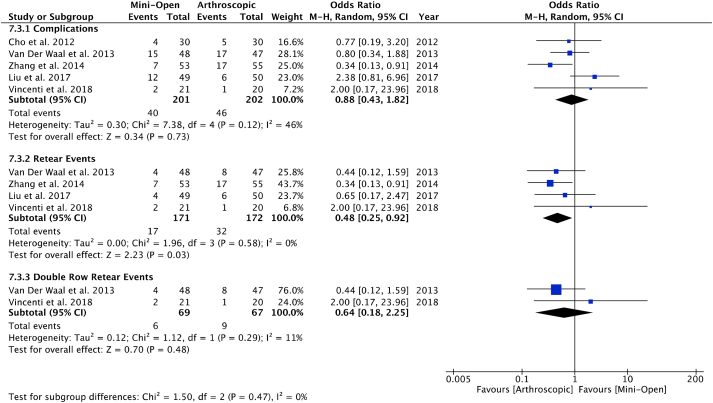
Eleven studies were included. Majority of patients underwent mini-open repair (MOR) compared to arthroscopic repair (AR) (57.4% vs 42.6%). A meta-analysis found statistically significant differences (p < 0.05) in patient-reported outcomes favouring AR. While retear rates were higher in AR (p = 0.03) analysis of retear rates for arthroscopic double row and mini-open repairs, yielded no differences between groups (p = 0.48).
Conclusion
Patients undergoing AR for rotator cuff tears had improved post-operative clinical outcomes in some functional outcomes compared to MOR. Modern arthroscopic double row repair result in similar failure rates to open repair techniques.
Level of evidence
Level III, Systematic Review of Level I-III studies.
Keywords: Rotator cuff repair, Arthroscopy, Mini-open, Double-row, Single-row, Rotator cuff
1. Introduction
Rotator cuff tears are common and result in pain, weakness and limited function.1, 2, 3 It is expected that 20.7% of the general population (age range 18–87) will develop either a traumatic or degenerative tear of the rotator cuff with increasing incidence with age.4 When conservative treatment is exhausted, various surgical approaches are available for repair of the rotator cuff. These include mini-open techniques, arthroscopic-assisted mini-open and all-arthroscopic rotator cuff repair.5, 6, 7, 8 Arthroscopic repairs are considered standard of care and have been more commonly performed with prevalence increasing by six fold over the past 20 years, while open repairs have increased by 34%.9 Although mini-open repairs result in good outcomes, concerns remain regarding potentially increased early postoperative pain, injury to the deltoid resulting in detachment and/or weakness as well as risk of arthrofibrosis.5,6,10,11 Advances in operative techniques and instrumentation over the past decade have now shifted surgeons’ preferences towards an all-arthroscopic approach.5,8 Although studies have shown that an arthroscopic approach is just as effective as the mini-open repair while being more cosmetically appealing for patients, concerns still exist regarding the strength of bone-tendon fixation and increased costs.
While early arthroscopic repair techniques involved single row repair, there has been an increasing trend towards using double row repair techniques in order to improve the contact surface of the rotator cuff footprint as well as biomechanical strength at time zero.12 While clinical outcomes between single and double row techniques have been equivocal, some studies suggest decreased failure rates with double row repairs particularly in large rotator cuff tears patterns.12, 13, 14
Although previous reviews have demonstrated similar outcomes between mini-open and arthroscopic techniques, they consisted of studies with heterogeneous populations (i.e. surgical techniques) and a limited focus on post-operative retear rates.15,16 The aim of this review is to provide an updated comparison between modern arthroscopic and mini-open repairs for treating rotator cuff tears.
2. Materials and methods
This systematic review was performed according the methods outlined in the Cochrane Handbook and reported according to the PRISMA Guidelines.17
2.1. Search strategy
A systematic literature search was conducted in PUBMED, EMBASE and MEDLINE, and Cochrane (CENTRAL) databases for literature comparing arthroscopic and mini-open rotator cuff repair from 2010 to October 1st, 2020. Medical Subject Headings (MeSH) terms were utilized in various combinations to increase search sensitivity. The terms consisted of “rotator cuff tear repair”, “mini-open”, “arthroscopic” and similar phrases (Appendix I).
A manual search of these terms was entered onto Google Scholar to ensure that additional potentially eligible articles were not missed and ClinicalTrials.gov was searched for recently completed trials. The research question and inclusion/exclusion criteria were established a priori.
Inclusion criteria were: (1) rotator cuff tears (2) arthroscopic and mini-open repair (3) human studies; and (4) English language (5) studies published within the last 10 years. This timeframe was utilized to ensure the latest and most modern arthroscopic and mini-open suture techniques were compared.
The exclusion criteria were: (1) non-comparative studies (2) other major shoulder surgery or bony procedures (e.g., open Bankart, Latarjet, modified Bristow, etc.); (4) review articles, letters to editorials, opinion pieces and conference proceedings (5) cadaver/non-human studies; and (6) case reports (7) not published within the last 10 years.
2.2. Study screening
Screening was performed independently and in duplicate and data was recorded in a Microsoft Excel spreadsheet (Version 2016; Microsoft Corp, USA). Any discrepancies between reviewers were discussed and resolved with input by a third reviewer. The references of included studies were also systematically screened to capture any additional relevant articles.
2.3. Quality assessment
The methodological quality of non-randomized comparative studies was evaluated using the methodological index for nonrandomized studies (MINORS).18 A score of 0, 1 or 2 is given for each of the 12 items on the MINORS checklist with a maximum score of 24 as all studies were comparative studies. Methodological quality was categorized a priori as follows: a score of 0–12 was considered poor quality, 13–18 was considered fair quality, and 19–24 was considered excellent quality, for non-comparative and comparative studies, respectively. Additionally, the level of evidence (I to IV) for each study was assessed.19
2.4. Data abstraction
Data was extracted in duplicate and independently from the eligible articles and recorded onto a Microsoft Excel spreadsheet (Version 2016; Microsoft Corp, USA). Disagreements were resolved either by consensus or through discussion with a third reviewer. Demographic data included author, year of publication, sample size, study design, level of evidence and patient demographics (e.g., gender, age, etc.). Information regarding rehabilitation protocols and post-operative outcomes (surgical and radiographic) and complications were documented.
2.5. Statistical analysis
Descriptive statistics such as mean, range and measures of variance (e.g., standard deviations, 95% confidence intervals [CI]) are presented where applicable. The intraclass correlation coefficient (ICC) was used to evaluate inter-reviewer agreement for assessing study quality. A kappa (κ) statistic was used to evaluate inter-reviewer agreement at all screening stages. Agreement was categorized a priori as follows: κ of 0.81–0.99 was considered as nearly perfect agreement; κ value of 0.61–0.80 was substantial agreement; κ value of 0.41–0.60 was moderate agreement; 0.21 to 0.40 fair agreement and a κ value of 0.20 or less was considered slight agreement.20 Review Manager 5.4 (The Cochrane Collaboration, 2020) was used to perform the meta-analysis. Continuous data were presented as mean differences with a 95% confidence interval (CI). Dichotomous data were presented as odds ratios (OR) with a 95% CI. The χ2 and I2 statistics were used to measure the heterogeneity of results within the included studies. A p < 0.05 was considered significant for the χ2 test. The I2 test was categorized as follows: 0.0%–24.9% to indicate no heterogeneity, 25.0%–49.9% to indicate low heterogeneity; 50.0%–74.9% to indicate moderate heterogeneity; 75.0%–100.0% to indicate high heterogeneity. Additionally, the random-effects model was used due to expected clinical heterogeneity.
3. Results
3.1. Study characteristics
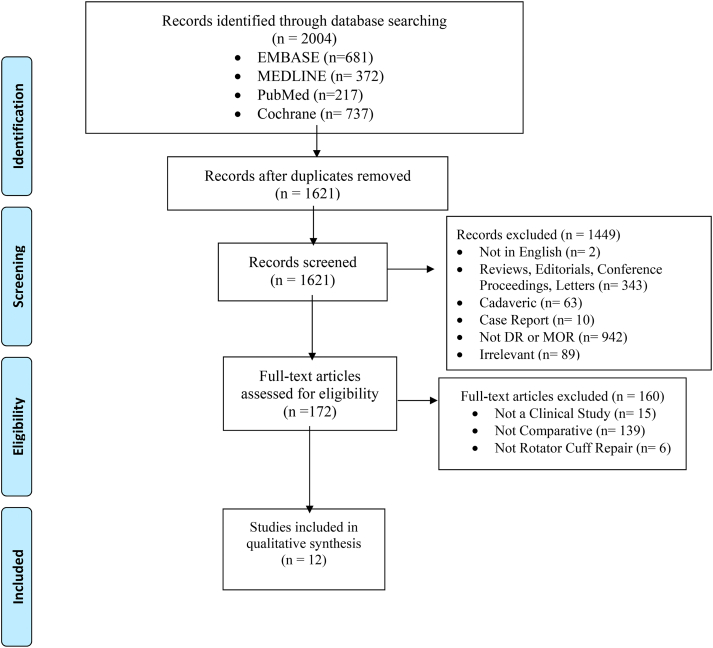
The initial search yielded a total of 2004 articles. After excluding 383 duplicates, 1621 articles were screened by title and abstract, leaving a total of 172 studies eligible for full text review. Following full text review, a total of 11 articles met the inclusion criteria for this review (Fig. 1). Of the 11 included studies published between 2010 and 2020, there were five retrospective cohort studies, one prospective, and five randomized controlled trials. From the studies included the majority (63.6%; 7/11) of these papers were published 2017 and onwards. The included studies were conducted in Asia (36.3%; n = 4), the Middle East (i.e., Turkey) (18.2%; n = 2), Europe (27.3%; n = 3), North America (9.1%; n = 1), and Oceania (9.1%; n = 1).
Fig. 1.
Prisma flow diagram.
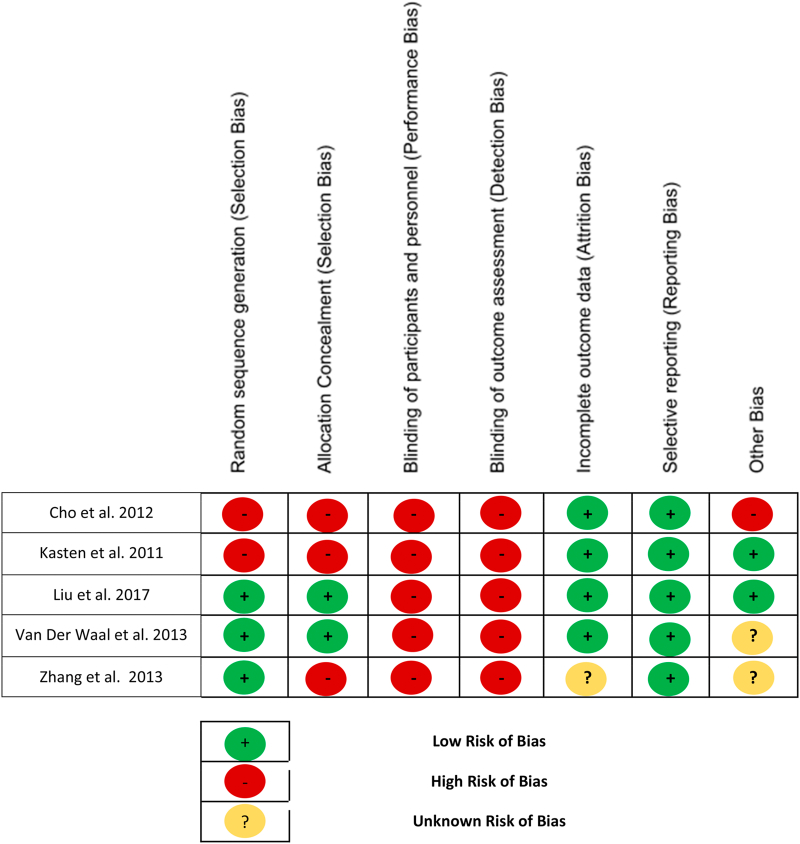
3.2. Study quality
Of the 11 studies included in this review, five were level 1 evidence (45.5%),5,21, 22, 23, 24 one was level 2 (9.1%),25 and five were level 3 evidence (45.5%).26, 27, 28, 29, 30 There was substantial agreement between reviewers at the title and abstract screening stage (κ = 0.76; 95% CI, 0.70 to 0.82) and excellent agreement at the full text screening stage (κ = 0.89; 95% CI, 0.75 to 1.0). There was excellent level of agreement for quality assessment scores based on the MINORS criteria (ICC = 0.93; 95% CI 0.53–0.99). The non-randomized comparative studies had a mean MINORS score of 15.7 ± 1.0, indicating fair quality of evidence, while the RCTs had a moderate risk of bias (Table I) (Fig. 2).
Table 1.
Study quality.
| Study Quality | |
|---|---|
| Prospective cohort | 1 (9.1%) |
| Retrospective cohort | 5 (45.5%) |
| RCT | 5 (45.5%) |
| Level 1 | 5 (45.5%) |
| Level 2 | 1 (9.1%) |
| Level 3 | 5 (45.5%) |
| MINORS | 15.7 ± 1.0 |
| Cochrane Risk of Bias | Moderate Risk |
Fig. 2.
Cochrane risk of bias summary.
3.3. Patient characteristics
Of the 2352 patients eligible for surgical intervention, a total of 2314 patients (61.5% male) were included in this review; (38 patients were lost prior to surgical intervention). The total mean sample size was 210.4 (range, 34–1374) in this review. Within the MOR group the mean sample size was 120.7 (range, 17–956), while it was 89.6 (range, 17–418) in the AR group. Of included patients, the mean age was 57.2 ± 4.4 years and their mean follow up time was 15.9 ± 8.1 months. Moreover, 57.4% (n = 1328; mean age 56.5 ± 4.8) of patients underwent mini-open repair (MOR), while 42.6% (n = 986; mean age 58.2 ± 3.8) of patients underwent arthroscopic repair (AR). Three studies did not stratify mean age for each group24, 25, 26 and the majority of studies did not stratify mean follow up period for each group (Table II).21, 22, 23, 24, 25, 26, 27, 28, 29, 30 Of the 18.4% (n = 432) patients lost to follow up after the surgical intervention, 23.2% (n = 308) of the patients were lost from the MOR group and 11.6% (n = 114) of the patients were lost from the AR group. One of the studies did not stratify the 10 patients that were lost from their study.26
Table 2.
Study characteristics.
| Patient Characteristics | Total | Mini-Open | Arthroscopic |
|---|---|---|---|
| Shoulders eligible (analyzed) | 2352 (2314) | 1328 (57.4%) | 986 (42.6%) |
| Males | 1447 (61.5%) | 870 (65.5%) | 561 (56.9%) |
| Age (years) | 57.2 ± 4.4 | 56.5 ± 4.8 | 58.2 ± 3.8 |
| Lost to Follow Up | 432 (18.4%)a | 308 (23.2%) | 114 (11.6%) |
| Follow up (months) | 15.87 ± 8.1 | N/A | N/A |
| Single Row Fixation | 683 (29.5%) | 449 (33.8%) | 234 (23.7%) |
| Double Row Fixation | 1014 (43.8%) | 632 (47.6%) | 382 (38.7%) |
| Both Double/Single Row | 325 (14.0%) | 127 (9.6%) | 198 (20.1%) |
| Unspecified | 292 (12.6%) | 120 (9.0%) | 172 (17.4%) |
3.4. Surgical techniques
MOR and AR techniques were utilized in each of the studies for rotator cuff repair (RCR). Suture fixation techniques for MOR included suture anchors (69.8%; n = 927), bone tunnels (13.5%; n = 179), a combination of anchors and tunnels (13.0%; n = 173), and an unspecified fixation method (3.7%; n = 49). Repair techniques for AR included double row repair (38.7%; n = 382), single row repair (23.7%; n = 234), either a single or double row repair (20.1%; n = 198), and an unspecified fixation method (17.4%; n = 172). Of all patients that had double row repair, 5.8% (95/1646) of them were suture bridge constructs.24 All suture techniques for AR patients were fixated using suture anchors.
3.5. Rehabilitation protocol
The postoperative rehabilitation was the same for both surgical interventions in nine (81.8%) of the included studies.5,21, 22, 23, 24,26, 27, 28, 29 In six of the studies an abduction sling/brace/pillow was utilized postoperatively.5,21,22,26, 27, 28 Two studies had an immobilization period ranging from 3 to 6 weeks after the surgery. Passive range of motion (ROM) exercises were done in five studies ranging from 1 week to 6 weeks postoperatively.5,21, 22, 23, 24 Following passive ROM, in five studies active ROM exercises ranged between 3 and 6 weeks long.21,23,24,26,29 Strengthening exercises ranged from 6 to 12 weeks in five studies.21,23,26,28,29 Heavy labour and overhead physical activities were allowed in three studies at a range of 4–6 months.5,21,23
3.6. Outcomes
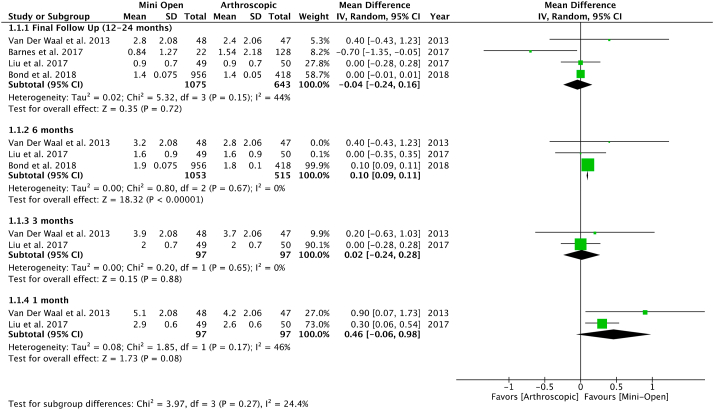
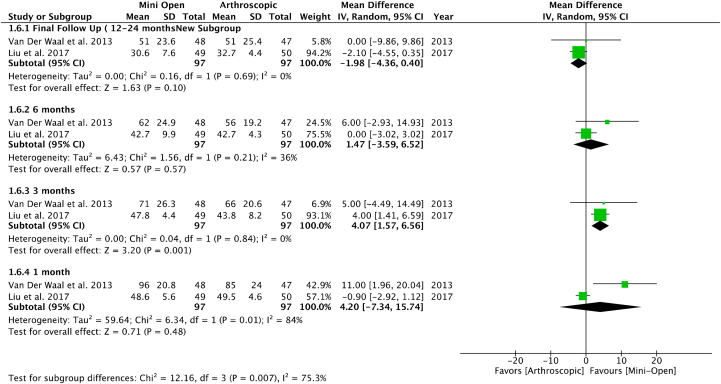
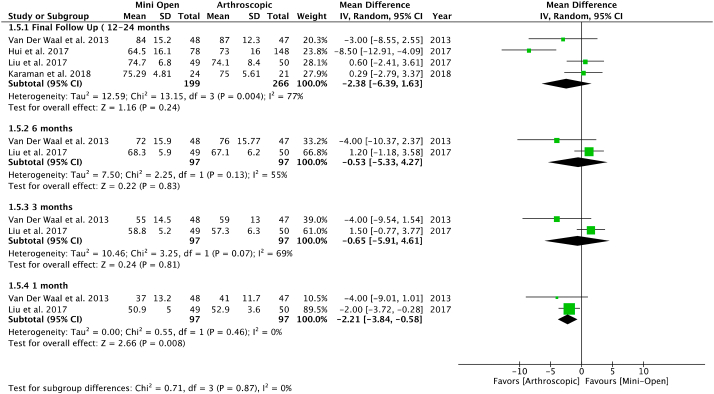
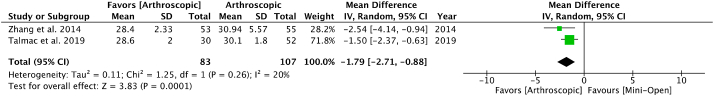
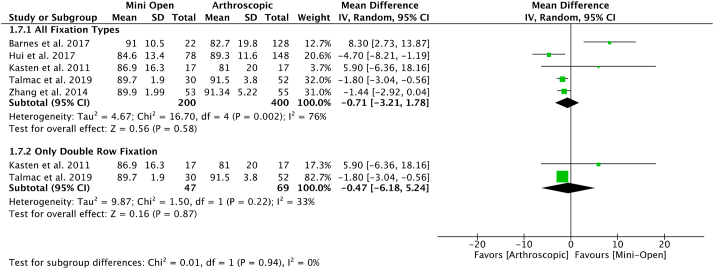
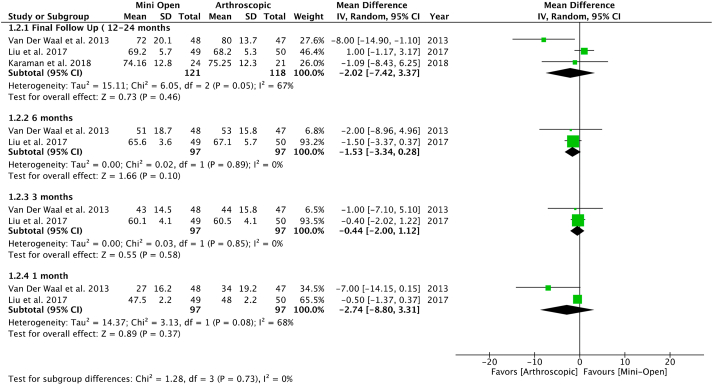
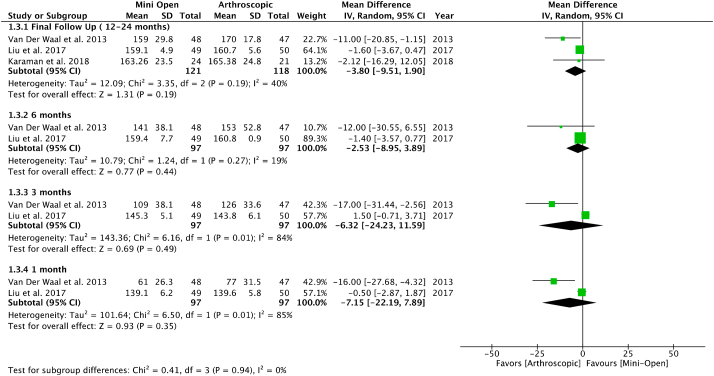
Pooled outcomes of three studies reporting VAS pain scores at 6 months found significantly lower VAS scores for patients undergoing AR (mean difference [MD], 0.10; 95% CI, 0.09 to 0.11 points, I2 = 0%; P < 0.00001) (Fig. 3).23, 24, 25 Two studies that reported DASH scores at 3 months were included in the meta-analysis.23,24 The findings illustrated that MOR DASH scores are significantly higher than AR DASH scores at 3 months (MD, 4.07; 95% CI, 1.57 to 6.56 points, I2 = 0%; p = 0.001) (Fig. 4). Using the same studies, another analysis was conducted for the Constant scores at 1 month postoperatively. It was found that AR had significantly higher Constant scores than MOR at this time period (MD, −2.21; 95% CI, −3.84 to −0.58 points, I2 = 0%; p = 0.008) (Fig. 5).23,24 Lastly, two different studies that reported UCLA scores were also used to conduct an analysis at the final follow-up (12–24 months).5,29 The meta-analysis results show that AR has significantly greater UCLA scores in comparison to MOR (MD, −1.79; 95% CI, −2.71 to −0.88 points, I2 = 20%; p = 0.0001) (Fig. 6). All other postoperative periods yielded an insignificant difference between the two procedures for functional outcomes (e.g., VAS, Constant, UCLA, DASH, ASES) (Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7) and range of motion (e.g., External Rotation and Forward Flexion) (Fig. 8, Fig. 9) (p > 0.05).
Fig. 3.
Meta-analysis of VAS pain scores in months 1, 3, 6, and 12–24 respectively.
Fig. 4.
Meta-analysis of DASH Scores in months 1, 3, 6, and 12–24 respectively.
Fig. 5.
Meta-analysis of Constant Scores in months 1, 3, 6, and 12–24 respectively.
Fig. 6.
Meta-analysis of UCLA scores at a final follow up of 12–24 months.
Fig. 7.
Meta-analysis of ASES score at final follow up with subgroup analysis of only Double row repair.
Fig. 8.
Meta-analysis of External Rotation (deg) in months 1, 3, 6, and 12–24 respectively.
Fig. 9.
Meta-analysis of Forward Flexion (deg) in months 1, 3, 6, and 12–24 respectively.
3.7. Complications
Complications were reported in a total of five studies (n = 343 RCR).5,23,24,27 The overall complication rate was 21.3% (86/403). An analysis of these four studies reported no significant difference in complication events between the two surgical interventions (odds ratio [OR], 0.88; 95% CI, 0.43–1.82, I2 = 46%; p = 0.73) (Fig. 10). The most common complication was rotator cuff retear (12.2%; 49/403) followed by adhesive capsulitis (4.7%; 19/403). Of the studies that reported retears, 9.9% (17/171) of patients that underwent MOR got a retear, while 18.6% (32/172) of patients that underwent AR suffered from a retear. A meta-analysis of the number of retear events reported significantly higher retear rates in AR than MOR (OR, 0.48; 95% CI, 0.25–0.92, I2 = 0%; p = 0.03) (Fig. 10). Within the MOR group we found 4.1% (7/171) of retears for the single row repair technique, 3.5% (6/171) for the double row repair technique, and 2.3% (4/171) wasn't specified. Within the AR group we found 9.9% (17/172) of retears for the single row repair technique, 5.2% (9/172) for the double row repair technique, and 3.5% (6/172) wasn't specified. A subgroup meta-analysis of two studies that utilized double row repair for the two procedures showed that there is an insignificant difference in retears when using this repair technique (OR, 0.64; 95% CI, 0.64–2.25, I2 = 11%; p = 0.48) (Fig. 10).24,27 Due to the limited quantity of the available literature, a single row meta-analysis was precluded.
Fig. 10.
Meta-analysis of complications with subgroup analysis of retear complications and retear complications in only double row repairs.
4. Discussion
The most significant finding of this systematic review was that patients undergoing AR had significantly improved post-operative outcomes (e.g., VAS, DASH, Constant, UCLA) compared to MOR at all postoperative intervals (1-month, 3- month, 6-month and final follow up [i.e., 12–24 months]). While the arthroscopic approach had a significantly higher retear rate in comparison to the MOR approach (18.6% vs 9.9%; p = 0.03), a subgroup analysis of retear rates for arthroscopic double row repair and all mini-open repairs, yielded no differences between groups (p = 0.48). Furthermore, the retear rate of arthroscopic single row within the population was 9.9% whereas the retear rate for arthroscopic double row was 5.2% for this review.
Although both MOR and AR provide significant improvements from the preoperative state, the contrast in how the shoulder is approached may determine preferences for surgeons and patients.5,23,24 The MOR approach has some advantages such as decreased learning curve as well as potential cost benefits.23,31 However, there is a significant risk of postoperative shoulder stiffness as well as other complications specific to the deltoid muscle.23,32 Arthroscopic approach provides a cosmetic appeal for patients, and potentially decreased risk of soft tissue injury. It is due to minimally invasive nature of arthroscopic repair that significant differences were likely seen in various functional scores (e.g., DASH, VAS, etc.) that favour the arthroscopic group within this current study. Specifically, pooled analysis of VAS scores at 6 months found significantly lower scores in the AR group (p < 0.00001) compared to the MOR group. In addition to this, there was significantly lower DASH scores at 3 months (p = 0.001), significantly higher 1-month Constant scores (p = 0.008), and significantly greater UCLA scores at a final follow-up (12–24 months) for the AR approach (p = 0.0001). However, all other outcomes yielded insignificant differences, especially after at a 12–24 month follow up period as AR and MOR had similar outcomes. These results contrast a review by Huang et al. published in 2016, in which only MOR Constant scores (no specified postoperative time) were increased in comparison to AR outcomes.16 A systematic review of Level I studies by Nazari et al. published in 2019 identified there was no significant differences reported between the techniques for functional score or range of motion at any postoperative interval.15 However, there was a general trend that favours beneficial functional outcomes and ROM outcomes for AR, similar to the findings of the current review. These differences across these reviews can be attributed to the literature included. Past reviews such as in Nazari et al. included studies with a smaller sample size, of which 80% (4 out of 5 included studies) were published prior to 2015. Another systematic review by Huang et al. had 72% of included studies published prior to 2010. The current review includes many studies primarily published after 2017 (63.6%; n = 7) with a mean sample size of 210.4 (34–1374), thus allowing for a more complete assessment of the literature. Additionally, as time has progressed, repair techniques advanced to become biomechanically stronger and secure. Thus, it is possible that future studies of higher quality, and large sample sizes may find postoperative and complications favouring AR.
Differences in the technicalities of the single row and double row repair can influence post-operative outcomes in AR as well. While double row repair has increased costs, its advantages include improved mechanical strength at time zero, increased tendon to bone contact, better restoration of the anatomical footprint and decreased gap formation.33, 34, 35, 36, 37, 38 Due to the improved biomechanics it is more resistant to perturbing movements that can cause a retear event in the early post-operative phase and double row repair reduces the risk of failure due to suture loosening.33,39 In a review published in 2011, it was found that double row repairs have a significantly higher tendon healing rate and a greater range of motion for external rotation than single row repairs.40 However, no significant differences were found in functional scores between the two repair techniques (p > 0.05).40 Additionally, a meta-analysis of five studies published in 2014 found that the retear incidence of both full and partial retears was significantly lower in double row repairs in comparison to single row (p = 0.05).41 Considering that the double row technique and its variations such as the suture bridge technique are more modern suture techniques than the single row, subgroup analyses of double row AR and MOR provide greater insight into how the latest arthroscopic techniques compare to MOR.12 In the current review, there were no significant differences (p = 0.48) in retear rates between arthroscopic double row repair and MOR. An analysis between arthroscopic single row repair and MOR could not be made due to a lack of comparative studies. Thus, future studies should determine the influence of repair technique (i.e., single or double row) on postoperative outcomes and complications in comparison to MOR.
Variables other than surgical and suture techniques can play a pivotal role in the success and outcomes of an RCR. Adjunct procedures performed during RCR, such as microfracture at the footprint is simple, inexpensive and effective in reducing short term pain and retear rates, as well as improving tendon-to-bond healing within patients.42 Exploring this option could improve tendon to bone healing and may likely reduce the VAS pain outcomes after a RCR.42 Other technical differences such as the use of vented anchors as opposed to solid anchors have shown no difference in healing outcomes.43 Meanwhile, the RCR is most vulnerable to retears within the first 6 months after the surgery, a time frame known as the “critical period”. Patients undergoing large RCRs require more caution within the critical period as they are more likely to experience a retear.44 Additional risk factors such as age, inflammatory arthritis, operative time, number of anchors, critical shoulder angle and fatty degeneration can also contribute to a retear event.45,46 Surgeons should therefore consider the use of procedures such as an anterolateral acromioplasty/resection during RCR, in order to reduce the CSA and the risk of retear.46 However, as none of the included studies in the current review reported radiographic parameters such as the CSA, it is difficult to ascertain its influence on outcomes and retear rates.
4.1. Limitations
The limitations of this review stem from the limited quantity and quality of evidence of the available literature. Due to a lack of robust studies with large sample sizes and long-term follow-up, a widespread investigation of whether double row suture techniques make AR a superior technique to MOR is still inconclusive. Furthermore, poor documentation of data (e.g., surgical techniques and outcomes) for the population of interest, limited our ability to establish a comprehensive difference between AR and MOR and the influence of suture type. Another limitation was the quality of the included studies as a moderate amount of risk was found within the RCTs due to lack of randomization and blinding of participants.
4.2. Future directions
Future studies using a robust RCT design or large cohorts should investigate the effects of suture types in AR such as double row and single row repair compared to MOR repair. Furthermore, these studies should have a widespread population with an appropriate follow-up length to allow for more accurate complication and retear rates. Adequate documentation of patient data, surgical techniques, rehabilitation (e.g., mobilization period) and outcomes will enable a thorough analysis of AR and MOR. Additionally, reducing the amount of bias within the studies through proper randomization is essential.
5. Conclusions
Patients undergoing AR for rotator cuff tears had better post-operative outcomes and higher retear rates compared to MOR for some functional outcomes and follow up periods. However, subgroup analysis of arthroscopic double row repair and MOR for retear rates revealed no significant differences. The influence of surgical technique and suture method on retear rates remains elusive and requires further investigation. Future studies using a robust RCT or large cohort design are required to ascertain these results.
Funding
No funding was received for the implementation of this study.
Ethical approval
This review did not involve primary data collection from patients.
Informed consent
N/A.
Category
Review.
Authors’ contribution
All authors contributed substantially to conception and design, or acquisition of data, or analysis and interpretation of data; drafted the article or revised it critically for important intellectual content; provided the final approval of the version to be published; and agreed to act as guarantor of the work (ensuring that questions related to any part of the work are appropriately investigated and resolved).
Declaration of competing interest
N/A.
Acknowledgements
None.
List of Abbreviations
- R AMSTAR
Revised assessment of multiple systematic reviews
- JBJS
Journal of bone and joint surgery
- MINORS
Methodological Index for Non-Randomized
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- ICC
Intraclass correlation coefficient
- RCR
Rotator cuff repair
- MOR
Mini-open repair
- AR
Arthroscopic repair
- ROM
Range of motion
- CI
Confidence interval
- OR
Odds ratio
- CSA
Critical stability angle
APPENDICES.
Appendix I.
Search strategy
| MEDLINE: 372 studies |
EMBASE: 681 studies |
PUBMED: 217 studies |
COCHRANE: 734 studies |
|---|---|---|---|
Strategy:
|
Strategy:
|
Strategy: ((((all arthroscopic or all-arthroscopic) OR (rotator cuff repair)) OR (mini open or mini-open)) OR (double row or double-row)) AND ((glenohumeral) OR (rotator cuff)) Filters: in the last 1 year, Humans, English |
Strategy: ((((all arthroscopic or all-arthroscopic) OR (rotator cuff repair)) OR (mini open or mini-open)) OR (double row or double-row)) AND ((glenohumeral) OR (rotator cuff))" with Cochrane Library publication date Between Jan 2010 and Sep 2020 |
1-3 - anatomical terms.
5-10 - surgical terms.
References
- 1.Piper C.C., Hughes A.J., Ma Y., Wang H., Neviaser A.S. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2018;27(3):572–576. doi: 10.1016/j.jse.2017.09.032. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell C., Adebajo A., Hay E., Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331(7525):1124–1128. doi: 10.1136/bmj.331.7525.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rees J.L. The pathogenesis and surgical treatment of tears of the rotator cuff. J Bone Joint Surg Br. 2008;90(7):827–832. doi: 10.1302/0301-620X.90B7.19874. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto A., Takagishi K., Osawa T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Zhang Z., Gu B., Zhu W., Zhu L., Li Q. Arthroscopic versus mini-open rotator cuff repair: a prospective, randomized study with 24-month follow-up. Eur J Orthop Surg Traumatol. 2014;24(6):845–850. doi: 10.1007/s00590-013-1263-5. [DOI] [PubMed] [Google Scholar]
- 6.Vastamäki M., Lohman M., Borgmästars N. Rotator cuff integrity correlates with clinical and functional results at a minimum 16 Years after open repair. Clin Orthop. 2013;471(2):554–561. doi: 10.1007/s11999-012-2494-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bell S., Lim Y.-J., Coghlan J. Vol. 95. 2013. pp. 151–157. (Long-term longitudinal follow-up of mini-open rotator cuff repair: J Bone Jt Surg-Am). 2. [DOI] [PubMed] [Google Scholar]
- 8.Ames J.B., Horan M.P., Van der Meijden O.A.J., Leake M.J., Millett P.J. Association between acromial index and outcomes following arthroscopic repair of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2012;94(20):1862–1869. doi: 10.2106/JBJS.K.01500. [DOI] [PubMed] [Google Scholar]
- 9.Colvin A.C., Egorova N., Harrison A.K., Moskowitz A., Flatow E.L. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227–233. doi: 10.2106/JBJS.J.00739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mall N.A., Chahal J., Heard W.M. Outcomes of arthroscopic and open surgical repair of isolated subscapularis tendon tears. Arthrosc J Arthrosc Relat Surg. 2012;28(9):1306–1314. doi: 10.1016/j.arthro.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 11.Bartl C., Scheibel M., Magosch P., Lichtenberg S., Habermeyer P. Open repair of isolated traumatic subscapularis tendon tears. Am J Sports Med. 2011;39(3):490–496. doi: 10.1177/0363546510388166. [DOI] [PubMed] [Google Scholar]
- 12.Randelli P., Cucchi D., Ragone V., de Girolamo L., Cabitza P., Randelli M. History of rotator cuff surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):344–362. doi: 10.1007/s00167-014-3445-z. [DOI] [PubMed] [Google Scholar]
- 13.Noticewala M.S., Ahmad C.S. Double-row rotator cuff repair: the new gold standard. Tech Shoulder Elbow Surg. 2015;16(1):6–9. doi: 10.1097/BTE.0000000000000038. [DOI] [Google Scholar]
- 14.Chen M., Xu W., Dong Q., Huang Q., Xie Z., Mao Y. Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2013;29(8):1437–1449. doi: 10.1016/j.arthro.2013.03.076. [DOI] [PubMed] [Google Scholar]
- 15.Nazari G., MacDermid J.C., Bryant D., Dewan N., Athwal G.S. Effects of arthroscopic vs. mini-open rotator cuff repair on function, pain & range of motion. A systematic review and meta-analysis. PloS One. 2019;14(10) doi: 10.1371/journal.pone.0222953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang R., Wang S., Wang Y., Qin X., Sun Y. Systematic review of all-arthroscopic versus mini-open repair of rotator cuff tears: a meta-analysis. Sci Rep. 2016;6 doi: 10.1038/srep22857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D., Shamseer L., Clarke M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 19.Wright J.G., Swiontkowski M.F., Heckman J.D. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]
- 20.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 21.Cho C.-H., Song K.-S., Jung G.-H., Lee Y.-K., Shin H.-K. Early postoperative outcomes between arthroscopic and mini-open repair for rotator cuff tears. Orthopedics. 2012;35(9):e1347–1352. doi: 10.3928/01477447-20120822-20. [DOI] [PubMed] [Google Scholar]
- 22.Kasten P., Keil C., Grieser T., Raiss P., Streich N., Loew M. Prospective randomised comparison of arthroscopic versus mini-open rotator cuff repair of the supraspinatus tendon. Int Orthop. 2011;35(11):1663–1670. doi: 10.1007/s00264-011-1262-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu J., Fan L., Zhu Y., Yu H., Xu T., Li G. Comparison of clinical outcomes in all-arthroscopic versus mini-open repair of rotator cuff tears: a randomized clinical trial. Medicine (Baltim) 2017;96(11) doi: 10.1097/MD.0000000000006322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Zwaal P., Thomassen B.J.W., Nieuwenhuijse M.J., Lindenburg R., Swen J.-W.A., van Arkel E.R.A. Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small to medium-sized tears: a randomized controlled trial in 100 patients with 1-year follow-up. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2013;29(2):266–273. doi: 10.1016/j.arthro.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 25.Bond E.C., Hunt L., Brick M.J. Arthroscopic, open and mini-open approach for rotator cuff repair: no difference in pain or function at 24 months. ANZ J Surg. 2018;88(1-2):50–55. doi: 10.1111/ans.14176. [DOI] [PubMed] [Google Scholar]
- 26.Karaman O., Karakus O., Saygi B. A comparison of full arthroscopic and arthroscopic-assisted mini-open repair methods in rotator cuff tears 1–3 cm in size. J Orthop. 2018;15(3):894–898. doi: 10.1016/j.jor.2018.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vicenti G., Moretti L., Carrozzo M., Pesce V., Solarino G., Moretti B. Evaluation of long-term postoperative outcomes between mini-open and arthroscopic repair for isolated supraspinatus tears: a retrospective analysis. Musculoskelet Surg. 2018;102(Suppl 1):21–27. doi: 10.1007/s12306-018-0549-5. [DOI] [PubMed] [Google Scholar]
- 28.Hui Y.J., Teo A.Q.A., Sharma S., Tan B.H.M., Kumar V.P. Immediate costs of mini-open versus arthroscopic rotator cuff repair in an Asian population. J Orthop Surg Hong Kong. 2017;25(1) doi: 10.1177/2309499016684496. 2309499016684496. [DOI] [PubMed] [Google Scholar]
- 29.Talmaç M.A., Görgel M.A., Bozca M.A., Arya A., Sönmez M.M., Özdemir H.M. Mini-open versus arthroscopic rotator cuff repair: a comparison of clinical results and Re-tear rates by magnetic resonance arthrogram. Med Bull Haseki. 2019;57(3):274–278. doi: 10.4274/haseki.galenos.2019.5245. [DOI] [Google Scholar]
- 30.Barnes L.A.F., Kim H.M., Caldwell J.-M. Satisfaction, function and repair integrity after arthroscopic versus mini-open rotator cuff repair. Bone Jt J. 2017;99-B(2):245–249. doi: 10.1302/0301-620X.99B2.BJJ-2016-0055.R1. [DOI] [PubMed] [Google Scholar]
- 31.Norberg F.B., Field L.D., Savoie F.H. Repair of the rotator cuff. Mini-open and arthroscopic repairs. Clin Sports Med. 2000;19(1):77–99. doi: 10.1016/s0278-5919(05)70297-0. [DOI] [PubMed] [Google Scholar]
- 32.Mormino M.A., Gross R.M., McCarthy J.A. Captured shoulder: a complication of rotator cuff surgery. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 1996;12(4):457–461. doi: 10.1016/s0749-8063(96)90040-7. [DOI] [PubMed] [Google Scholar]
- 33.Wall L.B., Keener J.D., Brophy R.H. Double-row vs single-row rotator cuff repair: a review of the biomechanical evidence. J Shoulder Elbow Surg. 2009;18(6):933–941. doi: 10.1016/j.jse.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 34.Meier S.W., Meier J.D. Rotator cuff repair: the effect of double-row fixation on three-dimensional repair site. J Shoulder Elbow Surg. 2006;15(6):691–696. doi: 10.1016/j.jse.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 35.Milano G., Grasso A., Zarelli D., Deriu L., Cillo M., Fabbriciani C. Comparison between single-row and double-row rotator cuff repair: a biomechanical study. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2008;16(1):75–80. doi: 10.1007/s00167-007-0382-0. [DOI] [PubMed] [Google Scholar]
- 36.Brady P.C., Arrigoni P., Burkhart S.S. Evaluation of residual rotator cuff defects after in vivo single- versus double-row rotator cuff repairs. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2006;22(10):1070–1075. doi: 10.1016/j.arthro.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 37.Aydin N., Karaismailoglu B., Gurcan M., Ozsahin M.K. Arthroscopic double-row rotator cuff repair: a comprehensive review of the literature. SICOT-J. 2018;4:57. doi: 10.1051/sicotj/2018048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bisson L., Zivaljevic N., Sanders S., Pula D. A cost analysis of single-row versus double-row and suture bridge rotator cuff repair methods. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2015;23(2):487–493. doi: 10.1007/s00167-012-2338-2. [DOI] [PubMed] [Google Scholar]
- 39.Ma C.B., Comerford L., Wilson J., Puttlitz C.M. Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg Am. 2006;88(2):403–410. doi: 10.2106/JBJS.D.02887. [DOI] [PubMed] [Google Scholar]
- 40.Prasathaporn N., Kuptniratsaikul S., Kongrukgreatiyos K. Single-row repair versus double-row repair of full-thickness rotator cuff tears. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2011;27(7):978–985. doi: 10.1016/j.arthro.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 41.Shen C., Tang Z.-H., Hu J.-Z., Zou G.-Y., Xiao R.-C. Incidence of retear with double-row versus single-row rotator cuff repair. Orthopedics. 2014;37(11):e1006–1013. doi: 10.3928/01477447-20141023-58. [DOI] [PubMed] [Google Scholar]
- 42.Osti L., Del Buono A., Maffulli N. Microfractures at the rotator cuff footprint: a randomised controlled study. Int Orthop. 2013;37(11):2165–2171. doi: 10.1007/s00264-013-1952-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sarmento MC, Cartucho AE, Monteiro JM. Short-term results (1 year) of vented versus solid polyetheretherketone anchors in treatment of rotator cuff tears. SICOT-J. 5. doi:10.1051/sicotj/2019026. [DOI] [PMC free article] [PubMed]
- 44.Barth J., Andrieu K., Fotiadis E., Hannink G., Barthelemy R., Saffarini M. Critical period and risk factors for retear following arthroscopic repair of the rotator cuff. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2017;25(7):2196–2204. doi: 10.1007/s00167-016-4276-x. [DOI] [PubMed] [Google Scholar]
- 45.Lee Y.S., Jeong J.Y., Park C.-D., Kang S.G., Yoo J.C. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017;45(8):1755–1761. doi: 10.1177/0363546517695234. [DOI] [PubMed] [Google Scholar]
- 46.Kuper G., Shanmugaraj A., Horner N.S. Critical shoulder angle is an effective radiographic parameter that is associated with rotator cuff tears and osteoarthritis: a systematic review. J ISAKOS Jt Disord Orthop Sports Med. 2019;4(2):113–120. doi: 10.1136/jisakos-2018-000255. [DOI] [Google Scholar]