Abstract
BACKGROUND
The perinatal period is a challenging time of substantial emotional, physiological, social, and relational changes. Depression, anxiety, and stress symptoms are common, and co-exist in the perinatal period. Digital technology continues to grow at an unprecedented pace with wide application, including psychotherapeutic intervention. A growing number of meta-analyses supported the application of digital psychotherapeutic intervention across different populations, but relatively few meta- and meta-regression analyses have concentrated on perinatal women.
AIM
To evaluate the effectiveness of digital psychotherapeutic intervention on improving psychological outcomes among perinatal women and identify its essential features.
METHODS
Randomized controlled trials (RCTs) were obtained from eight databases, including Cumulative Index to Nursing and Allied Health Literature, Cochrane Library, Embase, Scopus, PsycINFO, PubMed, Web of Science, and ProQuest Dissertation and Theses from inception up until November 24, 2020. Comprehensive Meta-analysis 3.0 software was used to conduct meta- and meta-regression analyses. The Cochrane risk-of-bias tool and the Grading of the Recommendation, Assessment, Development, and Evaluation system were adopted to assess the individual and overall qualities of the evidence, respectively.
RESULTS
A total of 25 RCTs that included 3239 women were identified. Meta-analyses revealed that intervention significantly improved depression (Hedges’s g = 0.49), anxiety (g = 0.25), and stress (g = 0.47) symptoms compared to the control. Subgroup analyses demonstrated that a website platform with ≥ eight therapist-guided sessions using the theoretical principle of cognitive behavioral therapy was more effective than other treatments in improving depression symptoms in postnatal women. Meta-regression analyses observed that the age of perinatal women and the type of psychotherapy also had statistically significant effects on depression symptoms. Egger’s regression asymmetry tests suggested that no publication biases occurred, but the overall quality of the evidence was very low.
CONCLUSION
This review suggests that digital psychotherapeutic intervention may be a potential solution to reduce psychological problems in perinatal women. Further high-quality RCTs with large sample sizes are needed.
Keywords: Digital psychotherapeutic intervention, Perinatal women, Meta-analysis, Meta-regression
Core Tip: This systematic review identified and analyzed the findings of 25 randomized controlled trials, and the results indicated that digital psychotherapeutic intervention could significantly reduce depression, anxiety, and stress symptoms among perinatal women. The essential features of this intervention were a website platform with ≥ eight therapist-guided sessions using the cognitive behavioral therapy theoretical principle. This intervention was also effective in reducing depression symptoms when treating young postnatal women. The overall evidence grade of outcomes was very low according to the Grading of Recommendations, Assessment, Development, and Evaluation criteria. Thus, future trials need to include a high-quality design and a large sample size.
INTRODUCTION
Perinatal period is a challenging time of substantial emotional, physiological, social, familial, and role changes[1,2]. These changes may affect psychological and physical resources, resulting in increased susceptibility of psychological problems, including depression, anxiety, and stress[3]. A systematic review observed that depression, anxiety, and stress symptoms co-existed in the perinatal period[4]. The prevalence in the perinatal period was estimated to be 7.4%-12.8% for depressive disorders[5], 3%-6% for anxiety disorders[6], and 3.3%-4.0% for posttraumatic stress disorders[7]. Perinatal mental disorders during pregnancy and postpartum period are associated with considerable maternal, infant, and child morbidity and mortality[8-10]. In addition, they lead to huge economic burden on health and social care[3]. Therefore, effective intervention is imperative. Psychotherapeutic intervention is considered a highly effective intervention for depression, anxiety, and stress[11].
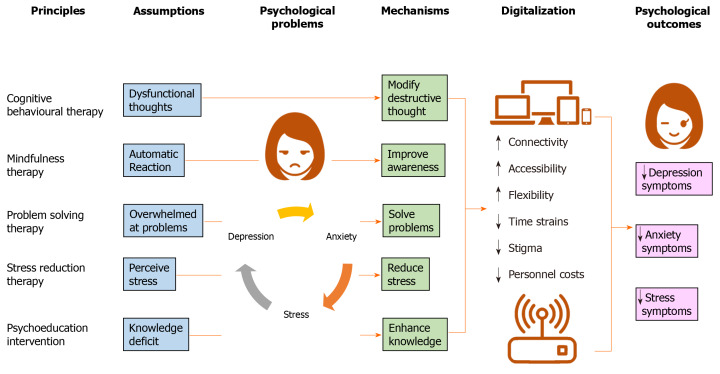
Psychotherapeutic interventions are based on several principles, including cognitive behavioral therapy (CBT)[12], mindfulness therapy[13], problem-solving therapy[14], stress-reduction therapy[15], psychoeducation intervention[16], or their combination. The assumption of CBT is that dysfunctional cognitive patterns result in emotional distress and subsequent maladaptive behavior[12]. CBT aims to improve psychological outcomes by helping women learn how to recognize and modify destructive thought patterns[12]. Mindfulness therapy suggests that negative psychological outcomes are due to automatic reaction[13]. It works by training women to react to things differently, and it involves the awareness of existing thoughts, emotions, and sensations to cultivate acceptance of every moment[13].
The core assumption of problem-solving therapy is that psychological symptoms are generated when women become overwhelmed by practical problems they face in their daily lives[14]. This type of therapy aims to help perinatal women by teaching structured means to solve their problems, which in turn alleviate their psychological outcomes[14]. Stress-reduction therapy focuses on stress management that helps women develop skills to manage, cope with, and reduce stress to promote well-being[15]. Psychoeducation intervention integrates and synergizes psychotherapeutic and educational components to help women deal with problems[16]. Psychoeducational techniques are used to improve awareness of cognitive distortions, communication, and problem-solving skills by providing information in a proactive fashion[16].
Empirical evidence suggests that CBT[17], mindfulness therapy[18], problem-solving therapy[19], stress-reduction therapy[20], and psychoeducation intervention[21] using face-to-face approach is effective in improving psychological outcomes among perinatal women. However, traditional face-to-face psychotherapeutic interventions may reduce effectiveness due to structural and psychological barriers[22-24]. Structural barriers include insufficient mental health professionals, difficulties booking appointments, and transportation problems[24,25]. Psychological barriers could arise due to the lack of motivation and self-stigmatization to seek treatment or overestimated barriers to seek treatment[26,27].
Digital technology continues to grow at an unprecedented pace with wide application, including psychotherapeutic intervention[28,29]. Psychotherapeutic intervention is considered as digital when technology, such as website, mobile application, email, or text messaging services, is used in its delivery[28]. Given that 80% of the population own mobile phones and 50% have access to the Internet[30], the use of digital technology in psychotherapeutic interventions has increased rapidly over the past several years[28]. Digital psychotherapeutic interventions essentially allow for improved connectivity, accessibility, and availability of support[31]. With the interventions being delivered online, a potential exists for a larger audience to receive these interventions because they could likely be accessed regardless of geographical location[31]. The option of implementing online programs helps mitigate the problem of insufficient healthcare professionals and reduce waiting times[22]. Thus, digital psychotherapeutic interventions could be comparatively more cost effective than other interventions[32]. Another important benefit is that digital psychotherapeutic interventions may be more attractive to individuals who may not feel comfortable with being out in public places or are reluctant to seek treatment due to social stigma[33].
Digital psychotherapeutic intervention aims at alleviating psychological symptoms with different assumptions and mechanisms in accordance with the different principles of psychotherapy. Figure 1 illustrates the possible mechanisms by which digital psychotherapeutic intervention could improve depression, anxiety, and stress symptoms in perinatal women. These mechanisms were proposed by extracting the frameworks of CBT[12], mindfulness therapy[13], problem-solving therapy[14], stress-reduction therapy[15], and psychoeducation intervention[16]. Perinatal women experienced psychological problems due to dysfunctional thoughts[12], automatic reaction[13], being overwhelmed by problems[14], perceived stress[15], and knowledge deficit[16]. They may learn how to modify destructive thought patterns[12], improve awareness[13], solve problems[14], reduce stress[15], and enhance their knowledge[16]. The use of digital technology could improve the connectivity, accessibility, and flexibility of psychotherapeutic intervention in accordance with a wide array of functions of digital platform[28,29,31]. Besides, the digitalization of psychotherapy could reduce time strain, stigma, and personnel costs[22,32,33]. Consequently, perinatal women may alleviate their depression, anxiety, and stress symptoms.
Figure 1.
Potential mechanisms of digital psychotherapeutic intervention in improving psychological outcomes.
A growing number of systematic reviews[28,34,35] have supported the effectiveness of digital psychotherapeutic intervention among college students[35], patients with serious mental illness[34], and young adults[28]. However, relatively little is known about its effectiveness in the perinatal population. Previous reviews[36-38] have investigated the potential effect of digital psychotherapeutic intervention among perinatal women. However, these reviews were limited to few selected trials[37,38], a mixture of different research designs[36-38], few databases[37], and only narrative synthesis[37]. None of these reviews investigated the preferred features and the overall evidence. In addition, none of them used meta-regression analysis to assess the influence of covariates on their effect size. Thus, the effectiveness and essential features of digital psychotherapeutic intervention among perinatal women remain unclear.
In light of the abovementioned limitations of the existing systematic reviews[36-38], the present review aims to synthesize the best evidence to (1) assess the effectiveness of digital psychotherapeutic intervention in reducing depression, anxiety, and stress symptoms; (2) evaluate the preferred design features of the intervention.
MATERIALS AND METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines was followed[39]. This review was registered in the PROSPERO database at the Centre of Reviews and Dissemination in the United Kingdom (CRD42021226534).
Eligibility criteria
All types of randomized controlled trials (RCTs) were included because of the strongest empirical evidence of the intervention’s effectiveness[40]. Published and unpublished trials in the English language without restriction to publication year were included to maximize the search scope. A description of the eligibility criteria is summarized in Supplementary Table 1. The RCTs were selected on the basis of their fulfilment of the Participants, Interventions, Comparisons, Outcomes, and Study design framework[39]. The population involved perinatal women aged 18 years and older from the start of pregnancy to first-year postpartum. The psychotherapeutic interventions were included if the content design was based on the CBT theoretical principle[12], mindfulness therapy[13], problem-solving therapy[14], stress-reduction therapy[15], psychoeducation intervention, or their combination and if they were delivered via website or/and mobile application[28]. The comparators or counterparts consisted of treatment as usual, waitlist control, or placebo control. Outcomes were depression, anxiety, and stress symptoms.
Searching strategies
A scoping search was conducted in the Cochrane Central Register of Controlled Trials, Joanne Briggs Institute Evidence Synthesis, and PROSPERO databases to prevent duplication of similar systematic reviews. A senior librarian was consulted regarding the search strategy. A comprehensive three-step search strategy was conducted in congruence with the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions[41]. First, a search of published literature up until November 24, 2020 was conducted using keyword and index terms in eight electronic databases as follows: Cumulative Index to Nursing and Allied Health Literature, Cochrane Library, Embase, Scopus, PsycINFO, PubMed, Web of Science, and ProQuest Dissertation and Theses, as shown in Supplementary Table 2. Next, ongoing trials from various clinical trial registries (ClinicalTrials.gov, World Health Organization International Clinical Trials Registry Platform, and ISRCTN Registry) were explored. Lastly, the bibliographies of RCTs and systematic reviews were hand-searched using snowballing. In addition, specific journals and different grey literature resources (Google Scholar and GreySource) were checked to ensure the comprehensiveness of the search[42].
Study selection
Study selection was conducted in accordance with the PRISMA flow diagram[39]. EndNote X9 (version 9.3.3) software[43] was used to import all identified citations and remove duplicates. After records from the databases were identified, two independent reviewers (JYC and KYY) screened the titles and abstracts for relevance. Full-text articles of eligible studies were retrieved and examined by the two reviewers independently on the basis of eligibility criteria. Differing responses were discussed and referred to a third reviewer (YL). Reasons for excluding trials in the full-text screening stage were recorded. A Kappa statistic (κ) larger than 0.6 was computed to determine an acceptable inter-rater agreement[44].
Data extraction
A standardized data extraction form was developed and piloted in accordance with the Cochrane Handbook for Systematic Reviews of Intervention[41]. The items extracted in relation to the characteristics of the trials included study setting, city/country, study design, sample size, participants’ age (mean and standard deviation), sample size, intervention (name), comparator, outcome (measure), attrition rate, grant support, intention to treat (ITT), missing data management, published protocol, and registration. The items involving digital psychotherapeutic intervention included aim, types, component, platform, regime (length, number of sessions, frequency, duration, and follow-up), guidance (from therapist/self), and theoretical basis. Dichotomous or continuous psychological outcomes, such as depression, anxiety, and stress symptoms at post-intervention, were extracted. The authors of the selected trials were contacted to obtain unpublished data or clarify questionable information.
Quality assessment
The Cochrane Collaboration risk-of-bias tool[45] was adopted to individually evaluate the quality of the trials. Two reviewers (JYC and KYY) conducted the assessments independently to minimize errors[41]. Selection, performance, detection, attrition, and reporting biases were assessed using the following six domains: (1) Random sequence generation; (2) Allocation concealment; (3) Participant and personnel blinding; (4) Outcome assessment blinding; (5) Incomplete outcome data; and (6) Selective reporting. The risk for each author was graded as low, high, or unclear. The attrition rate, ITT, missing data management, published protocol, and registration of selected trials were investigated to further assess the quality of evidence.
The Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) checklist[46] was adopted to judge the overall quality and strength of the recommendations by using GRADEpro 3.6 software[47]. The overall evidence was graded as high, moderate, low, or very low in accordance with five aspects: Methodological limitations, inconsistency, indirectness, imprecision, and publication bias[48]. Publication bias was evaluated through visual inspection of the funnel plot asymmetry[49] and Egger’s test[50] when each outcome included 10 or more trials.
Statistical analysis
Comprehensive Meta-Analysis software (version 3)[51] was used for meta-analyses. The random-effect model was also used because it accounts for the statistical assumption of variation in the estimation of mean across all trials[52]. The overall effect was computed using Z-statistics at a significance level of P < 0.05. The pooled mean effect sizes of psychological outcomes were estimated using Hedges’ g, which provides an accurate estimation of the overall effect size when the included trials have small sample sizes[53]. The effect size was interpreted as small (0.2), medium (0.5), large (0.8), and very large (1.2)[54].
The inverse-variance statistical method was utilized to compute continuous outcomes[41]. Heterogeneity was evaluated on the basis of the Cochran Q test, in which P < 0.10 indicates the presence of significant statistical heterogeneity[41]. The I2statistic was used to quantify the degree of heterogeneity, in which I2 indicates the variation percentage[55], such as 0%-40% (may not be important), 30%-60% (moderately important), 50%-90% (substantially important), and 75%-100% (considerably important)[56].
Additional analysis
Sensitivity analyses were conducted to identify heterogeneous trials that were removed to maintain overall homogeneity[57]. Subgroup analyses were also performed to reduce the overall heterogeneity across studies (I2 > 40%)[58] and compare the effects among various populations, settings, and features of intervention[59]. The predefined subgroups included population nature, theoretical principle, digital platform, aim of intervention, guidance, and number of sessions.
Meta-regression analysis was conducted to explain whether the heterogeneity between trials could be attributed to covariates[60]. A random-effect meta-regression model was used to assess if the year of publication, mean age, sample size, type of psychotherapy, number of sessions, and duration influenced the effect size of digital psychotherapeutic intervention. A significance level of P < 0.05 was used for the random-effect meta-regression analysis. Narrative synthesis of outcomes was performed when meta-analysis could not be conducted on the data.
RESULTS
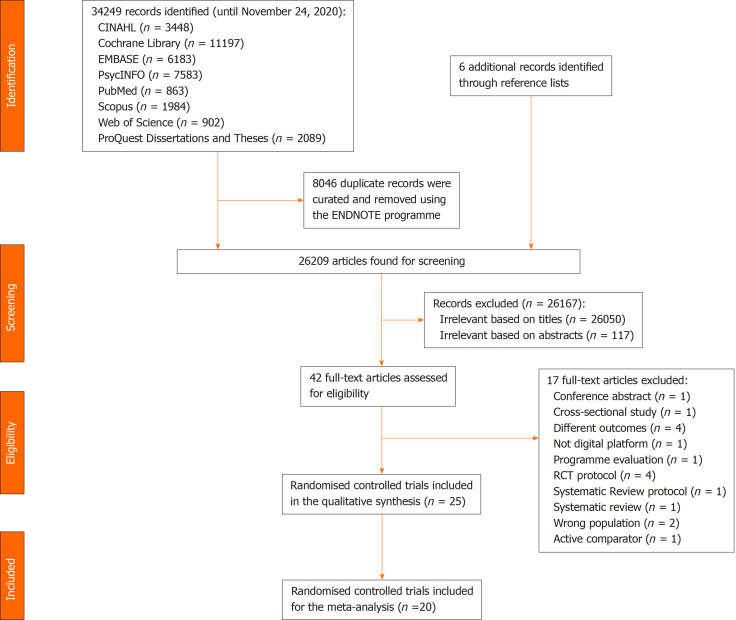
Study selection
Figure 2 illustrates a PRIMSA flowchart of the selection of trials. A total of 34249 articles were identified from eight databases, and 8046 duplicates were removed using Endnote. Six additional records obtained from snowballing were included. After screening was conducted by two independent reviewers (JYC and KYY), 26167 articles were excluded in accordance with their titles and abstracts, and 42 full-test articles were selected for eligibility. Twenty-five RCTs were eventually selected. Among them, 24 were international peer-reviewed articles[61-84] and one was an unpublished doctoral dissertation[85]. Moderate agreement was reached between the dyad raters (κ = 0.78).
Figure 2.
Study selection.
Characteristics of included randomized controlled trials
Table 1 summarizes the characteristics of 3239 perinatal women in the 25 included RCTs from 2009[85] to 2020[77] in Australia[73,75], Canada[81], China[84], Germany[70,71], Iran[67], Netherlands[66,76,76], Portugal[64], Scotland[72], Singapore[68], Sweden[65,74,78], Switzerland[82,83], the United States of America[62,63,69,85], the United Kingdom[79,80], and 23 countries[61]. The RCTs were two armed (k = 22) or three armed (k = 3)[67,68,74]. They were conducted in hospital (k = 2)[68,84] or in the community (k = 23). The populations studied included healthy antenatal[61,62,74,76,77] and postnatal[68,85] women and women who experienced psychological problems[64-67,73,75,77-81,84], insomnia[63,69], preterm labor[82,83], miscarriage[72], or pregnancy loss[70,71]. The sample size ranged from 25[62] to 910[80]. The mean age was between 27.7[67] and 34.6[78] years.
Table 1.
Characteristics of selected 25 randomised controlled trials
|
Ref.
|
Country/setting
|
Design
|
Population (nature)
|
Age (mean ± SD)
|
Intervention (name)
|
Comparator
|
Sample size
|
Outcome (Measures)
|
Attrition rate (%)
|
ITT/MDM
|
Protocol/registry
|
Grant
|
| Barrera et al[61], 2015 | 23 countries/Community | 2-arm RCT | Antenatal (mixed trimesters) | 30.2 ± 5.6 | Mood management internet intervention (Curso Internet de Mamás y Bebés) | Placebo (Information only) | I: 57; C: 54 | Depression symptoms (CES-D) | 66.1% | No/No | No/No | Yes |
| Duffecy et al[62], 2019 | United States/Community | 2-arm RCT | Antenatal (20–28 wk) | 30.5 ± 4.1 | Share (group) condition (Sunnyside) | Placebo (individual) condition | I: 18; C: 7 | Depression symptoms (PHQ-8 and HDRS) | 28% | No/No | No/Yes | Yes |
| Felder et al[63], 2020 | United States/Community | 2-arm RCT | Antenatal (≤ 28 wk, insomnia by SCI, EPDS ≥ 15) | 33.6 ± 3.7 | Digital cognitive behavioural therapy for insomnia (Sleepio) | Treatment as usual | I: 105; C: 103 | Depression symptoms (EPDS), Anxiety symptoms (GAD-7) | 11.1 % | Yes/No | No/Yes | Yes |
| Fonseca et al[64], 2019 | Portugal /Community | 2-arm RCT | Postnatal women (PDPI-R ≥ 5.5 or EPDS > 9 | 32.6 ± NR | Web-based intervention (Be a Mom) | Waitlist | I: 98; C: 96 | Depression symptoms (EPDS) | 24.2 % | Yes/Yes | No/Yes | Yes |
| Forsell et al[65], 2017 | Sweden/Community | 2-arm RCT | Antenatal (10-28 wk, major depression by SCID; MADRS-S: 15-35) | 31.0 ± NR | Internet-delivered cognitive behaviour therapy (ICBT) | Treatment as usual | I: 22; C: 20 | Depression symptoms (EPDS and MADRS-S), Anxiety symptoms (GAD-7) | 7.1 % | Yes/Yes | No/Yes | Yes |
| Heller et al[66], 2020 | Netherlands /Community | 2-arm RCT | Antenatal (< 30 wk with CES-D ≥ 16, HADS-A ≥ 8) | 32.0 ± NR | Internet- based problem-solving treatment (MamaKits Online) | Treatment as usual | I: 79; C: 80 | Depression symptoms (EPDS and CES-D), Anxiety symptoms (HADS-A) | 17.6% | Yes/Yes | Yes/Yes | Yes |
| Jannati et al[67], 2020 | Iran/Community | 3-arm RCT | Postnatal (≤ 6 mo, EPDS ≥ 13 and MINI) | 27.7 ± 4.2 | App-based cognitive behavioural therapy (Happy Mom) | Treatment as usual | I: 39; C: 39 | Depression symptoms (EPDS) | 3.9% | No/No | No/Yes | Yes |
| Jiao et al[68], 2019 | Singapore/Hospital | 3-arm RCT | Postnatal (first time mother < 6 wk) | 30.7 ± NR | Web-based psychoeducational intervention (NR) | Treatment as usual | I: 68; C: 68 | Depression symptoms (EPDS) | 6.9% | Yes/Yes | Yes/Yes | Yes |
| Kalmbach et al[69], 2020 | United States/Community | 2-arm RCT | Antenatal (27.76 ± 0.87 wk with insomnia using ISI ≥ 10 and EPDS ≥ 19) | 29.0 ± 4.2 | Digital cognitive behavioural therapy for insomnia (Sleepio) | Placebo (Digital sleep education) | I: 46; C: 45 | Depression symptoms (EPDS) | 1.1% | Yes/Yes | No/Yes | Yes |
| Kersting et al[71], 2011 | Germany/Community | 2-arm RCT | Postnatal (loss of child with 5-43 wk) | 34.3 ± 5.3 | Internet-based cognitive behavioural treatment programme (NR) | Waitlist | I: 45; C: 33 | Depression symptoms (GSI-D), Anxiety symptoms (GSI-A) Stress symptoms (IES) | 22.9% | Yes/Yes | No/No | Yes |
| Kersting et al[70], 2013 | Germany/Community | 2-arm RCT | Postnatal (loss of child with 2-40 wk) | 34.2 ± 5.2 | Internet-based cognitive behavioural treatment programme (NR) | Waitlist | I: 115; C: 113 | Depression symptoms (GSI-D) Anxiety symptoms (GSI-A) Stress symptoms (IES-R) | 12.7% | Yes/No | No/No | Yes |
| King et al[85], 2009 | United States/Community | 2-arm RCT | Postnatal (≤ 12 mo) | 32.5 ± NR | Internet-based stress management program (LivingSmart) | Face- to-Face control group | I: 28; C: 29 | Depression symptoms (BDI-II), Anxiety symptoms (STAI) Stress symptoms (PSS) | 33.1% | No/No | No/No | Yes |
| Klein et al[72], 2012 | Scotland/Community | 2-arm RCT | Postnatal (Miscarriage with < 24 wk) | 33.0 ± 6.3 | Web-based intervention (Miscarriage matters) | Treatment as usual | I: 33; C: 34 | Depression symptoms (HADS-D), Anxiety symptoms (HADS-A) | 35.8% | Yes/Yes | No/No | Yes |
| Loughnan et al[73], 2019 | Australia/Community | 2-arm RCT | Antenatal (13-30 wk, GAD-7 > 9 and/or PHQ-9 > 9) | 31.6 ± 4.0 | Internet-delivered cognitive behavioural therapy program (MUMentum Pregnancy) | Treatment as usual | I: 43; C: 44 | Depression symptoms (EPDS), Anxiety symptoms (GAD-7) Stress symptoms (K-10) | 11.5% | Yes/Yes | Yes/Yes | Yes |
| Matvienko-Sikar et al[74], 2017 | Sweden/Community | 3-arm RCTs | Antenatal (10-22) wk | 33.8 ± 3.0 | Novel positive psychological intervention (BodyScan and Reflection) | Treatment as usual | I: 32; C: 14 | Depression symptoms (EPDS) Stress symptoms (PDQ) | 6.5% | No/No | No/No | No |
| Milgrom et al[75], 2016 | Australia/Community | 2-arm RCT | Postnatal (< 12 mo, EPDS 11-23) | 31.6 ± NR | Internet cognitive behavioural therapy (MumMoodBooster) | Treatment as usual | I: 21; C: 22 | Depression symptoms (BDI-II), Anxiety symptoms (DASS-21-A), Stress symptoms (DASS-21-S) | 6.9% | Yes/Yes | No/Yes | Yes |
| Missler et al[76], 2020 | Netherlands/Community | 2-arm RCT | Antenatal (26-34 wk) | 32.5 ± NR | Psycho-educational Intervention (NR) | Waitlist | I: 68; C: 69 | Depression symptoms (EPDS), Anxiety symptoms (HADS-A), Stress symptoms (PSI) | 11.7% | Yes/Yes | Yes/Yes | Yes |
| Molenaar et al[77], 2020 | Netherlands/Community | 2-arm RCT | Antenatal (12-16 wk, depression history) | 32.2 ± 4.9 | Discontinuation of anti-depressants with Preventive Cognitive Therapy (STOP) | Treatment as usual | I: 24; C: 20 | Depression symptoms (EPDS and HDRS), Anxiety symptoms(STAI) | 13.6% | No/No | Yes/Yes | Yes |
| Nieminen et al[78], 2016 | Sweden/Community | 2-arm RCT | Postnatal (≥ 3 mo, TES ≥ 30) | 34.6 ± 4.8 | Internet-based trauma-focused cognitive behaviour therapy (TF-ICBT) | Waitlist | I: 28; C: 28 | Depression symptoms (BDI-II and PHQ-9), Anxiety symptoms (BAI), Stress symptoms (IER-R) | 9.8% | Yes/Yes | No/No | Yes |
| O'Mahen et al[80], 2013 | United Kingdom/Community | 2-arm RCT | Postnatal (< 12 mo, EPDS > 12) | 32.3 ± NR | Internet-based behavioral activation (Netmums) | Treatment as usual | I: 462;C: 448 | Depression symptoms (EPDS) | 61% | Yes/No | No/No | Yes |
| O'Mahen et al[79], 2014 | United Kingdom/Community | 2-arm RCT | Postnatal (< 12 mo, EPDS > 12) | 32.3 ± NR | Internet behavioral activation treatment (NetmumsHWD) | Treatment as usual | I: 41; C: 42 | Depression symptoms (EPDS), Anxiety symptoms (GAD-7) | 13.2% | Yes/Yes | No/No | Yes |
| Pugh et al[81], 2016 | Canada/Community | 2-arm RCT | Postnatal (< 12 mo, EPDS ≥ 10) | ≥ 18 ± NR | Therapist assisted, Internet-delivered cognitive behavior therapy (TA-ICBT) | Waitlist | I: 25; C: 25 | Depression symptoms (DASS-21-D), Anxiety symptoms (DASS-21-A), Stress symptoms (DASS-21-S) | 18% | Yes/Yes | No/Yes | Yes |
| Scherer et al[82], 2016 | Switzerland/Community | 2-arm RCT | Postnatal (preterm labour with 18-32 wk) | 32.7 ± 3.0 | Internet-based cognitive behavioral stress management (IB-CBSM) | Placebo (Limited support) | I: 51; C: 42 | Anxiety symptoms (STAI-S), Stress symptoms (PSS) | 37.6% | No/No | No/Yes | Yes |
| Urech et al[83], 2018 | Switzerland/Community | 2-arm RCT | Postnatal (preterm labour with 18-32 wk) | 32.6 ± 3.7 | Internet-based cognitive behavioral stress management (IB-CBSM) | Placebo (Generic information) | I: 50; C: 43 | Depression symptoms (EPDS), Anxiety symptoms(STAI-S and PRA), Stress symptoms (PSS) | 44.1% | No/Yes | No/No | Yes |
| Yang et al[84], 2019 | China/Hospital | 2-arm RCT | Antenatal (24-30 wk, GAD-7 > 4 or PHQ-9 > 4) | 30.9 ± NR | Online mindfulness intervention (NR) | Placebo (Wechat) | I: 62; C: 61 | Depression symptoms (PHQ-9), Anxiety symptoms (GAD-7) | 13.8% | Yes/Yes | No/No | Yes |
BAI: Beck anxiety inventory; BDI-II: Beck depression inventory-II; C: Control; CES-D: Center for epidemiological studies depression; CES-D: Centre for epidemiologic studies-depression scale; DASS-21-A: Depression, anxiety and stress scales-21- anxiety subscale; DASS-21-D: Depression, anxiety and stress scales-21- depression subscale; DASS-21-S: Depression, anxiety and stress scales-21- stress subscale; EPDS: Edinburgh postnatal depression scale; GAD-7: Generalized anxiety disorder scale; GSI-A: Global severity index-anxiety subscale; GSI-D: Global severity index-depression subscale; HADS-A: Hospital anxiety and depression scale-anxiety subscale; HADS-A: Hospital anxiety and depression scale-anxiety subscale; HADS-D: Hospital anxiety and depression scale-depression subscale; HDRS: Hamilton depression rating scale; I: Intervention; IES: Impact of event scale; IES-R: Impact of event scale-revised; ISI: Insomnia severity index; ITT: Intention-to-treat analysis; K-10: Kessler psychological distress 10-item scale; MADRS-S: Montgomery-Asberg depression rating scale self-report version; MDM: Missing data management; MINI: International neuropsychiatric interview; NR: Not reported; PDPI-R: Postpartum depression predictors inventory-revised; PDQ: Prenatal distress scale; PHQ-8: Patient health questionnaire-8; PRA: The pregnancy related anxiety test; PSI: Parenting stress index; PSS: Perceived stress scale; RCT: Randomised controlled trial; SCI: Sleep condition indicator; SCI-I: Structural clinical interview for DSM Axis I disorders; STAI: State trait anxiety inventory; STAI-S: Spielberger state trait anxiety inventory; TES: Traumatic event scale.
Risk of bias
A risk-of-bias summary is shown in Supplementary Figure 1 with moderate inter-rater agreement (κ = 0.72). Among the 25 included RCTs, 53.33% had low risk of bias across six domains. More than half (56%) had unclear allocation concealment. The participants and personnel in the majority of trials were not blinded (92%). Assessment of the outcomes was also not blinded in most trials (72%). Eleven RCTs[61,70-72,74,78-80,84,85] did not have published protocols nor were registered in any clinical trial registry. Therefore, 44% of the reported bias was unclear. The attrition rates ranged from 1.1%[69] to 66.1%[61]. The majority of trials used ITT analysis (68%) and mentioned missing data management (60%).
Digital psychotherapeutic intervention
A detailed description of digital psychotherapeutic intervention for the 25 trials is presented in Supplementary Table 3. The aims of intervention were divided into prevention and treatment using CBT principles, mindfulness therapy, problem-solving therapy, stress-reduction therapy, psychoeducation intervention, or the combined version. The interventions were mainly delivered via website (k = 22) or mobile application (k = 4)[63,67,77,84], and some of them were supplemented with email, phone call, short messaging service, or home visit. The elements consisted of counselling, education, advice, assignment, feedback, reminder, forum, support, self-monitoring, questions, and answers. The interventions lasted between 10[62] and 90[61] min and ranged from three sessions[73] to 12 sessions[79] for 3[74]-15[80] wk. They were either self-guided (k = 7)[61,64,65,67,73,83,85] or therapist-guided (k = 18). The majority of them reported follow-up assessment (k = 19) a using theoretical basis (k = 23).
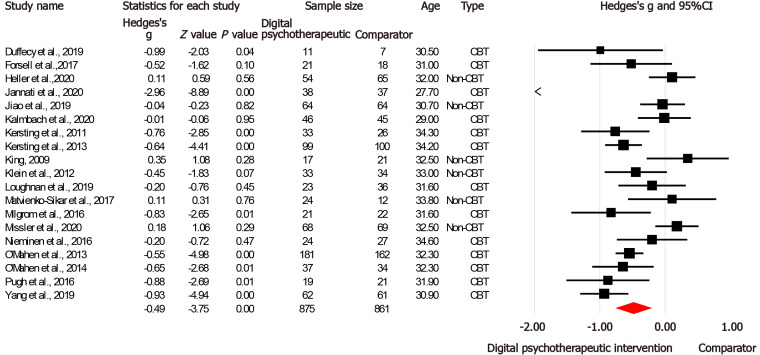
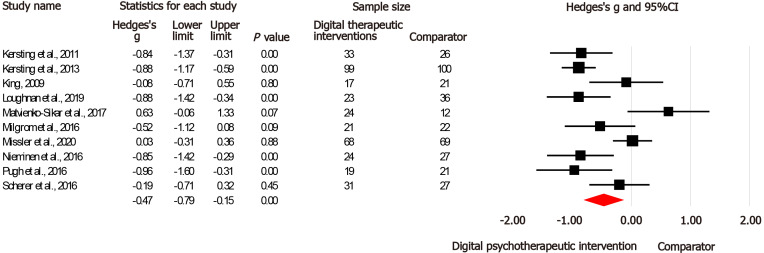
Depression symptoms
A total of 19 RCTs[62,65-76,78-81,84,85] considered depression symptoms as the outcome among 1736 perinatal women by using various measures. Meta-analysis results observed that digital psychotherapeutic intervention had a medium effect size (g = 0.49) in alleviating depression symptoms significantly (Z = -3.75, P < 0.001) compared with the control. Figure 3 illustrates the pooled results of meta-analysis using the random-effect model. Sensitivity and subgroup analyses were conducted given the considerable heterogeneity (I2 = 84.41). However, the heterogeneity remained unexplained.
Figure 3.
Forest plot of Hedges’s g (95% confidence interval) in depression symptoms for digital psychotherapeutic intervention and comparators.
Subgroup analyses
A series of subgroup analyses was conducted (Table 2) on the basis of population nature, theoretical principle, digital platform, aim of intervention, guidance, and number of sessions. The effect sizes were greater and significant among postnatal women (g = 0.67) than antenatal women (g = 0.24). Subgroup analyses demonstrated that the essential features of the intervention, that is, the use of CBT principle only (g = 0.56) via a website platform (g = 0.32) for the purpose of treatment (g = 0.71) were significant. Therapist-guided intervention (g = 0.40) and ≥ eight sessions were more effective than their counterparts. However, no significant subgroup differences (P = 0.09–0.54) were found.
Table 2.
Subgroup analyses of digital psychotherapeutic intervention on depression symptoms
|
Deign
|
Subgroups
|
No of trials
|
Sample size
|
g
|
P
value
|
Subgroup differences, P value
|
| Population nature | Antenatal women | 8[62,65,66,69,73,74,76,84] | 622 | -0.24 | 0.16 | Q = 2.95, P = 0.09 |
| Postnatal women | 11[67,68,70-72,75,78-81,85] | 1114 | -0.67 | < 0.001c | ||
| Theoretical principle | Cognitive behavioural therapy and others | 3[67,73,78] | 185 | -1.11 | 0.19 | Q = 4.13, P = 0.13 |
| Cognitive behavioural therapy only | 8[62,65,69-71,79-81] | 447 | -0.56 | < 0.001c | ||
| Other psychotherapy | 8[66,68,72,74-76,84,85] | 691 | -0.19 | 0.26 | ||
| Digital platform | Website | 17[64-66,68-76,78-81,85] | 1538 | -0.32 | < 0.001c | Q = 2.49, P = 0.11 |
| Mobile application | 2[67,84] | 198 | -1.93 | 0.06 | ||
| Aim | Prevention | 9[62,68,70-74,76,85] | 741 | -0.25 | 0.09 | Q = 3.31, P = 0.07 |
| Treatment | 10[65-67,69,75,78-81,84] | 995 | -0.71 | < 0.001c | ||
| Guidance | Self-guided | 4[65,67,73,85] | 211 | -0.83 | 0.23 | Q = 0.37, P = 0.54 |
| Therapist-guided | 15[62,66,68-72,74-76,78-81,84] | 1525 | -0.40 | < 0.001c | ||
| Number of sessions | < 8 sessions | 8[66,69,73,75,76,81,84,85] | 650 | -0.26 | 0.15 | Q = 2.47, P = 0.12 |
| ≥ 8 sessions | 11[62,65,67,68,70-72,74,78-80] | 1086 | -0.66 | < 0.001c |
Hedges’s g: Effect size; Q: Cochran’s statistic; Z: z-statistics.
P < 0.05.
P < 0.01.
P < 0.001.
Meta-regression analyses
Univariate and multivariate random-effect regression was performed to examine whether the effect size magnitude was related to covariates (year of trials, age, sample size, number of sessions, type of psychotherapy, and duration of intervention), as shown in Table 3. The results of univariate and multivariate random-effect regression analyses showed that age (β = 0.18, P = 0.02; β = 0.14, P = 0.04, respectively) and the use of CBT (β = 0.07, P < 0.001; β = 0.07, P < 0.001, respectively) had significant effects on depression symptoms. The Q-value for the multivariate random-effect regression model was 68.76, with df = 16 and P < 0.001. Thus, the null hypothesis was rejected, and the effect size was related to covariates. The explained variance (R2 = 0.364) was calculated using the regression model, and it revealed that 36.40% of the variance in true effects could be explained by these two covariates. Two bubble plots of depression symptoms on age and types of psychotherapy are presented in Supplementary Figure 2. The multivariate meta-regression model suggested that younger perinatal women who received CBT showed a larger effect size in terms of improving depression symptoms than older perinatal women who received other psychotherapies. However, covariates such as year of trial, sample size, number of sessions, and duration of intervention had no effect on these symptoms.
Table 3.
Random-effects univariate and multivariate meta-regression analyses of covariates on depression symptoms
| Covariates |
Univariate meta-regression
|
Multivariate meta-regression
|
||||||
|
β
|
SE
|
95%CI
|
P
value
|
β
|
SE
|
95%CI
|
P
value
|
|
| Age | 0.18 | 0.08 | 0.03, 0.33 | 0.02b | 0.14 | 0.07 | 0.01, 0.27 | 0.04a |
| Cognitive behavioral therapy1 | -0.077 | 0.23 | -1.23, 0.31 | < 0.001c | -0.070 | 0.24 | -1.16, -0.23 | < 0.001c |
| Year of trials | -0.02 | 0.04 | -0.10, 0.06 | 0.66 | - | - | - | - |
| Sample size | < 0.001 | < 0.001 | -0.00, 0.00 | 0.94 | - | - | - | - |
| Numbers of session | -0.05 | 0.04 | -0.13, 0.03 | 0.20 | - | - | - | - |
| Duration of intervention (wk) | -0.07 | 0.05 | -0.16, 0.02 | 0.13 | - | - | - | - |
Reference group: Non-cognitive behavioral therapy.
P < 0.05.
P < 0.01.
P < 0.001.
β: Coefficient; SE: Standard error; CI: Confident interval.
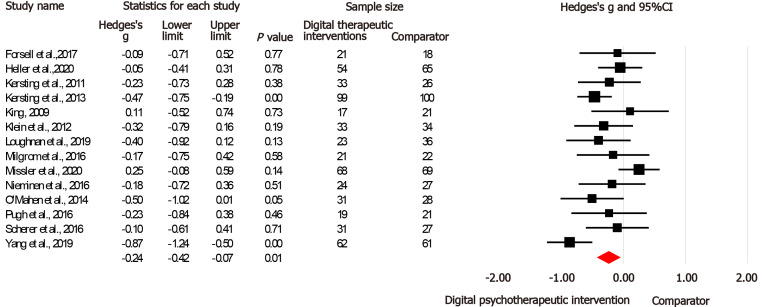
Anxiety and stress symptoms
Fourteen RCTs[65,66,70-73,75,76,78,79,81,82,84,85] assessed the effectiveness of digital psychotherap-eutic intervention in 1091 perinatal women by using anxiety as an outcome. Meta-analysis results indicated that digital psychotherapeutic intervention exerted a significant effect on improving anxiety symptoms (Z = -5.72, P = 0.007), with a small effect size (g = 0.25), as shown Figure 4. Moderate heterogeneity (I2 = 50.70%) was also found. Another 10 RCTs[70,71,73-76,78,81,82,85] used stress as an outcome in 720 perinatal women. Meta-analysis results demonstrated that stress symptoms were significantly reduced (Z = -2.90, P < 0.001) in the intervention group with a medium effect size (g = 0.47) compared with the comparator (Figure 5). Considerable heterogeneity (I2 = 75.34%) was also revealed. Sensitivity and subgroup analyses were conducted to decrease the I2 in both outcomes, but the heterogeneity did not improve.
Figure 4.
Forest plot of Hedges’s g (95% confidence interval) in anxiety symptoms for digital psychotherapeutic intervention and comparators.
Figure 5.
Forest plot of Hedges’s g (95% confidence interval) in stress symptoms for digital psychotherapeutic intervention and comparators.
Narrative synthesis
Given that five trials[61,63,64,77,83] did not report inadequate data for pooling of data in the present meta-analysis, the authors were contacted three times to ask for supplementary data on the psychological outcomes. Unfortunately, the team did not receive any reply. Thus, narrative synthesis was conducted. One trial[63] showed that digital CBT considerably reduced depression and anxiety symptoms. However, one trial[62] did not clearly report psychological outcomes after intervention, and another three[61,77,83] suggested that the intervention did not significantly improve the psychological outcomes. These inconsistencies indicated the need for further investigation.
Overall evidence
In accordance with the GRADE criteria, the overall quality of evidence was graded as very low (Supplementary Figure 2). For the outcome measures of depression, anxiety, and stress symptoms, methodological limitations were downgraded because of performance, selection, and detection biases. Inconsistency was downgraded because of moderate to considerable heterogeneities (50.70%–84.41%). Indirectness was downgraded due to the variation in digital psychotherapeutic interventions. Imprecision was downgraded because of small sample size with wide confidence intervals. Publication bias was not detected for trials that reported depression, anxiety, and stress scores, as observed from the symmetrical distribution of the included trials on the funnel plots (Supplementary Table 4). The P value of Egger’s regression asymmetry tests ranged from 0.24 to 0.33, thereby suggesting no evidence of publication bias.
DISCUSSION
This review revealed statistically significantly lower depression, anxiety, and stress symptom scores with small to medium effect in digital psychotherapeutic intervention than in the comparators. Subgroup analyses identified that the essential features of the intervention, that is a website platform with ≥ eight therapist-guided sessions using CBT principle for treatment among postnatal women appeared to be more effective in improving depression symptoms than their counterparts. Meta-regression analyses observed that the age of perinatal women and the type of psychotherapy had statistically significant effects on depression symptoms.
The findings revealed that digital psychotherapeutic interventions were effective in improving depression, anxiety, and stress symptoms among perinatal women. These results are consistent with those of previous reviews[36-38]. They could explain the proposed mechanistic pathways linking digital psychotherapeutic intervention to psychological outcomes (Figure 1). Digital psychotherapeutic interventions aid perinatal women to modify their dysfunctional thoughts[12], ameliorate their level of awareness[13], enhance their problem-solving skills[14], deal with stress[15], and acquire further knowledge[16]. Such principles of psychotherapy help build resilience, as women are able to learn and strengthen their cognitive flexibility[86]. Digital platform allows for improving connectivity, accessibility, and availability[31]. Moreover, it could reduce the time constraint, social stigma, and cost[22,32,33]. The components of digital psychotherapeutic interventions involve reminders, forums, and self-monitoring; they help enhance the ability of women to actively adapt to their circumstances and improve their abilities to cope with stressful perinatal situations[87]. As a result, perinatal women may improve their depression, anxiety and stress symptoms.
Subgroup and meta-regression analyses highlighted that the use of the CBT principle, therapist support, and ≥ eight sessions using website platform for treatment among postnatal young women could optimize the intervention effect. Efficacious intervention adopted the CBT principle, possibly because CBT is a patient-centered and personalized therapy that uses collaborative psychological approach[12]. The core components of cognitive restructuring and behavioral activation assist perinatal women to understand their own special beliefs and behavior patterns via counselling, education, advice, and assignment and finding an enhanced method to modify their dysfunctional thoughts, thus bringing about emotional and behavioral changes and improving their psychological problems[12]. Therapist support involved increased levels of customized human support to provide feedback, support, questions, and answers in a flexible manner for clarifications that could intensify the effect of intervention and improve depression symptoms[88]. In addition, ≥ eight sessions was suggested to be the appropriate number for intervention. This finding seems to be a possible explanation of a dose-response effect from the cumulative intervention intensity[89].
The interventions are effective for the purpose of treatment, and they are targeted at complicated perinatal women, such as those who experienced psychological problems[65-67,73,75,78-81,84], insomnia[69], miscarriage[72], or pregnancy loss[70,71]. This finding is consistent with that of a previous review[36], which showed that preventive digital psychotherapy may not be as effective as when targeted at high-risk perinatal women. High-risk women are possibly more willing to seek help and be actively involved in psychotherapy because they felt depressed, anxious, or stressed for a long period than low-risk women[3,24].
Young women are particularly at high risk of having perinatal mental disorders because they may not access antenatal care or mental health services in a timely manner[3]. Similar to the findings of a previous review[87], interventions implemented during the postnatal period were more effective than those implemented during the antenatal period. Postnatal period is a time of adaptation to parenthood, and postnatal women need to adjust to the new role of motherhood and familial relationships[90]. Therefore, interventions were found to be more effective in postnatal women. Website was found to be the preferred platform among perinatal women. This case may be linked to perinatal women expressing interest in the use of web-based resources and their increased engagement in e-mental health[91]. One study suggested that mobile applications are an important source of support during childbearing[92]. Low statistical power in small sample size was possible because only two trials were conducted in 198 perinatal women by using mobile applications in subgroup analysis. Further investigation is necessary.
This review demonstrates that digital psychotherapeutic intervention may be a potential solution to reduce psychological problems in perinatal women. The poor quality of existing evidence reduced certainty in implementing digital psychotherapeutic intervention at this phase. However, the subgroup and meta-regression analysis results could provide a future direction in designing interventions effectively. Future designs should consider therapist-guided treatment among young postnatal women.
This systematic review has several strengths. It is the first systematic review to investigate the essential features, covariates, and quality of the overall evidence. A total of 25 RCTs were selected, and the PRISMA criteria were strictly followed, with a robust three-step search strategy throughout eight databases. RCTs were selected from over 23 countries using published and unpublished resources. Hedges’s g was adopted to accurately estimate the overall effect size because of the small sample size in most of the included RCTs. However, this review also has some limitations. First, the restriction to trials in English and self-selected samples from media recruitment may have limited the generalization of the findings. Second, the high heterogeneities in the meta-analyses could have resulted from the low accuracy of pooled estimates. Third, self-report measures may have led to overestimation or underestimation of the effect size. Fourth, very low overall evidence could have diminished the internal validity of the findings. Lastly, this review only pooled post-intervention outcomes; thus, the sustainability of digital psychotherapeutic intervention remains uncertain.
This review highlighted a number of directions for future trials. Further well-designed RCTs are needed, particularly allocation concealment, participant and personnel blinding, and outcome assessment blinding. Future RCTs should stick to the consolidated standards of reporting trial statements[93]. Future trials should also consider a large sample size to provide a more precise estimate of the effect size and generalize the results. Considering that CBTs using website platform have dominated the existing literature, upcoming research should focus on different types of psychotherapy using other digital platforms for fair comparison. Future trials are warranted to assess the long-term effect and cost-effectiveness of digital psychotherapeutic intervention among perinatal women.
CONCLUSION
Meta-analyses found a small to medium and significant group difference favoring digital psychotherapeutic interventions over the comparators in regard to depression, anxiety, and stress outcomes. This systematic review provides evidence for the effectiveness of digital psychotherapeutic intervention in reducing psychological problems during the perinatal period. Future designs should consider the use of CBT principle, therapist support, and ≥ eight sessions using website platform for the treatment of postnatal young women. Further high-quality RCTs with large sample sizes are required to evaluate the sustainability of the intervention.
ARTICLE HIGHLIGHTS
Research background
Perinatal women are at increased susceptibility of psychological problems, including depression, anxiety, and stress. Perinatal psychological problems are associated with considerable adverse effects on women, offspring, family, and healthcare services.
Research motivation
Previous reviews were limited to few selected trials, a mixture of different research designs, few databases, and only narrative synthesis. None of the previous reviews investigated the preferred features of digital psychotherapeutic intervention and the influence of covariates on study effect size.
Research objectives
This review aimed to synthesize the best evidence to (1) assess the effectiveness of digital psychotherapeutic intervention in reducing depression, anxiety, and stress symptoms; and (2) evaluate the preferred design features of the intervention.
Research methods
A comprehensive three-step search strategy was conducted in congruence with the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions from eight databases. Comprehensive Meta-analysis 3.0 software was used to conduct meta- and meta-regression analyses. The individual and overall quality of the evidence were evaluated using the Cochrane risk-of-bias tool and the Grading of Recommendations, Assessment, Development, and Evaluation criteria.
Research results
A total of 25 randomized controlled trials that included 3239 perinatal women were identified. Meta-analyses revealed that digital psychotherapeutic intervention significantly improved the depression (g = 0.49), anxiety (g = 0.25), and stress (g = 0.47) symptoms of perinatal women compared to the control. Subgroup analyses demonstrated that a website platform with ≥ eight therapist-guided sessions using the cognitive behavioral therapy theoretical principle was more effective than other treatments in postnatal women. Meta-regression analyses observed that the age of perinatal women and the type of psychotherapy had statistically significant effects on depression symptoms. Egger’s regression asymmetry tests found no publication biases, but the overall quality of evidence was very low.
Research conclusions
This systematic review provides evidence for the effectiveness of digital psychotherapeutic intervention in reducing psychological problems during the perinatal period, particularly depression, anxiety, and stress symptoms. Future designs should consider the use of the cognitive behavioral therapy principle, therapist support, and ≥ eight sessions using a website platform for the treatment of postnatal young women.
Research perspectives
Given that the poor quality of the existing evidence reduced certainty in implementing digital psychotherapeutic intervention at this phase, further high-quality randomized controlled trials with large sample sizes are required to evaluate the sustainability of the intervention.
ACKNOWLEDGEMENTS
The authors would like to thank authors of the randomized controlled trials considered for sharing their additional data for use in our meta-analysis.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Invited manuscript
Peer-review started: December 30, 2020
First decision: January 11, 2021
Article in press: March 10, 2021
Specialty type: Obstetrics and gynecology
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Feng QS, Lee PN S-Editor: Zhang L L-Editor: A P-Editor: Li JH
Contributor Information
Ying Lau, Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore 117597, Singapore. nurly@nus.edu.sg.
Jing-Ying Cheng, Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore 117597, Singapore.
Sai-Ho Wong, Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore 117597, Singapore.
Kai-Yoong Yen, Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Singapore 117597, Singapore.
Ling-Jie Cheng, Nursing Research Unit, Department of Nursing, Khoo Teck Puat Hospital, Yishun Health Campus, National Healthcare Group, Singapore 768828, Singapore.
References
- 1.Garcia ER, Yim IS. A systematic review of concepts related to women's empowerment in the perinatal period and their associations with perinatal depressive symptoms and premature birth. BMC Pregnancy Childbirth. 2017;17:347. doi: 10.1186/s12884-017-1495-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lederman RP, Weis KL. Psychosocial anxiety, stress, and adaptation in pregnancy: assessment of seven dimensions of maternal development. Psychosocial adaptation to pregnancy: seven dimensions of maternal development. Cham: Springer International Publishing, 2020: 1-50. [Google Scholar]
- 3.Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19:313–327. doi: 10.1002/wps.20769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agius A, Xuereb RB, Carrick-Sen D, Sultana R, Rankin J. The co-existence of depression, anxiety and post-traumatic stress symptoms in the perinatal period: A systematic review. Midwifery. 2016;36:70–79. doi: 10.1016/j.midw.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Howdeshell KL, Ornoy A. Depression and Its Treatment During Pregnancy: Overview and Highlights. Birth Defects Res. 2017;109:877–878. doi: 10.1002/bdr2.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viswasam K, Eslick GD, Starcevic V. Prevalence, onset and course of anxiety disorders during pregnancy: A systematic review and meta-analysis. J Affect Disord. 2019;255:27–40. doi: 10.1016/j.jad.2019.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J Affect Disord. 2017;208:634–645. doi: 10.1016/j.jad.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 8.Pais M, Pai MV. Stress among pregnant women: a systematic review. J Clin Diagn. 2018;12:LE01–LE04. [Google Scholar]
- 9.Goodman JH. Perinatal depression and infant mental health. Arch Psychiatr Nurs. 2019;33:217–224. doi: 10.1016/j.apnu.2019.01.010. [DOI] [PubMed] [Google Scholar]
- 10.Rees S, Channon S, Waters CS. The impact of maternal prenatal and postnatal anxiety on children's emotional problems: a systematic review. Eur Child Adolesc Psychiatry. 2019;28:257–280. doi: 10.1007/s00787-018-1173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nillni YI, Mehralizade A, Mayer L, Milanovic S. Treatment of depression, anxiety, and trauma-related disorders during the perinatal period: A systematic review. Clin Psychol Rev. 2018;66:136–148. doi: 10.1016/j.cpr.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beck AT. Cognitive behavior therapy: Basic and beyond. 3rd ed. New York: The Guilford Press, 2021. [Google Scholar]
- 13.Creswell JD. Mindfulness Interventions. Annu Rev Psychol. 2017;68:491–516. doi: 10.1146/annurev-psych-042716-051139. [DOI] [PubMed] [Google Scholar]
- 14.Nezu AM, Nezu CM, D'Zurilla TJ. Problem-solving therapy: A treatment manual. New York: Springer, 2013. [Google Scholar]
- 15.Bochenek K, LeGrave A, Ausderau K. Stress reduction interventions for pregnant women: A scoping review. Am J Occup Ther. 2017;71:7111515214p1. [Google Scholar]
- 16.Walsh JF. Psychoeducation in mental health. Chicago, IL: Lyceum Books, 2010. [Google Scholar]
- 17.Van Lieshout RJ, Yang L, Haber E, Ferro MA. Evaluating the effectiveness of a brief group cognitive behavioural therapy intervention for perinatal depression. Arch Womens Ment Health. 2017;20:225–228. doi: 10.1007/s00737-016-0666-9. [DOI] [PubMed] [Google Scholar]
- 18.Luberto CM, Park ER, Goodman JH. Postpartum Outcomes and Formal Mindfulness Practice in Mindfulness-Based Cognitive Therapy for Perinatal Women. Mindfulness (N Y) 2018;9:850–859. doi: 10.1007/s12671-017-0825-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sampson M, Villarreal Y, Rubin A. A problem-solving therapy intervention for low-income, pregnant women at risk for postpartum depression. Res Soc Work Pract. 2014;26:236. [Google Scholar]
- 20.Urizar GG Jr, Caliboso M, Gearhart C, Yim IS, Dunkel Schetter C. Process Evaluation of a Stress Management Program for Low-Income Pregnant Women: The SMART Moms/Mamás LÍSTAS Project. Health Educ Behav. 2019;46:930–941. doi: 10.1177/1090198119860559. [DOI] [PubMed] [Google Scholar]
- 21.Kariuki EW, Kuria MW, Were FN, Ndetei DM. Effectiveness of a brief psychoeducational intervention on postnatal depression in the slums, Nairobi: a longitudinal study. Arch Womens Ment Health. 2020 doi: 10.1007/s00737-020-01085-1. [DOI] [PubMed] [Google Scholar]
- 22.Tal A, Torous J. The digital mental health revolution: Opportunities and risks. Psychiatr Rehabil J. 2017;40:263–265. doi: 10.1037/prj0000285. [DOI] [PubMed] [Google Scholar]
- 23.Renn BN, Hoeft TJ, Lee HS, Bauer AM, Areán PA. Preference for in-person psychotherapy vs digital psychotherapy options for depression: survey of adults in the U.S. NPJ Digit Med. 2019;2:6. doi: 10.1038/s41746-019-0077-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sambrook Smith M, Lawrence V, Sadler E, Easter A. Barriers to accessing mental health services for women with perinatal mental illness: systematic review and meta-synthesis of qualitative studies in the UK. BMJ Open. 2019;9:e024803. doi: 10.1136/bmjopen-2018-024803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baker N, Gillman L, Coxon K. Assessing mental health during pregnancy: An exploratory qualitative study of midwives' perceptions. Midwifery. 2020;86:102690. doi: 10.1016/j.midw.2020.102690. [DOI] [PubMed] [Google Scholar]
- 26.Chan SYY, Ho GWK, Bressington D. Experiences of self-stigmatization and parenting in Chinese mothers with severe mental illness. Int J Ment Health Nurs. 2019;28:527–537. doi: 10.1111/inm.12558. [DOI] [PubMed] [Google Scholar]
- 27.Husain W. Barriers in Seeking Psychological Help: Public Perception in Pakistan. Community Ment Health J. 2020;56:75–78. doi: 10.1007/s10597-019-00464-y. [DOI] [PubMed] [Google Scholar]
- 28.Fu Z, Burger H, Arjadi R, Bockting CLH. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7:851–864. doi: 10.1016/S2215-0366(20)30256-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garrido S, Millington C, Cheers D, Boydell K, Schubert E, Meade T, Nguyen QV. What Works and What Doesn't Work? Front Psychiatry. 2019;10:759. doi: 10.3389/fpsyt.2019.00759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The World Bank Group. World development report 2016: Digital dividends. [cited 30 December 2020]. Available from: https://www.worldbank.org/en/publication/wdr2016 .
- 31.Graham AK, Lattie EG, Powell BJ, Lyon AR, Smith JD, Schueller SM, Stadnick NA, Brown CH, Mohr DC. Implementation strategies for digital mental health interventions in health care settings. Am Psychol. 2020;75:1080–1092. doi: 10.1037/amp0000686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kraepelien M, Mattsson S, Hedman-Lagerlöf E, Petersson IF, Forsell Y, Lindefors N, Kaldo V. Cost-effectiveness of internet-based cognitive-behavioural therapy and physical exercise for depression. BJPsych Open. 2018;4:265–273. doi: 10.1192/bjo.2018.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rogers MA, Lemmen K, Kramer R, Mann J, Chopra V. Internet-Delivered Health Interventions That Work: Systematic Review of Meta-Analyses and Evaluation of Website Availability. J Med Internet Res. 2017;19:e90. doi: 10.2196/jmir.7111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Batra S, Baker RA, Wang T, Forma F, DiBiasi F, Peters-Strickland T. Digital health technology for use in patients with serious mental illness: a systematic review of the literature. Med Devices (Auckl) 2017;10:237–251. doi: 10.2147/MDER.S144158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lattie EG, Adkins EC, Winquist N, Stiles-Shields C, Wafford QE, Graham AK. Digital Mental Health Interventions for Depression, Anxiety, and Enhancement of Psychological Well-Being Among College Students: Systematic Review. J Med Internet Res. 2019;21:e12869. doi: 10.2196/12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ashford MT, Olander EK, Ayers S. Computer- or web-based interventions for perinatal mental health: A systematic review. J Affect Disord. 2016;197:134–146. doi: 10.1016/j.jad.2016.02.057. [DOI] [PubMed] [Google Scholar]
- 37.Lee EW, Denison FC, Hor K, Reynolds RM. Web-based interventions for prevention and treatment of perinatal mood disorders: a systematic review. BMC Pregnancy Childbirth. 2016;16:38. doi: 10.1186/s12884-016-0831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Loughnan SA, Joubert AE, Grierson A, Andrews G, Newby JM. Internet-delivered psychological interventions for clinical anxiety and depression in perinatal women: a systematic review and meta-analysis. Arch Womens Ment Health. 2019;22:737–750. doi: 10.1007/s00737-019-00961-9. [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hariton E, Locascio JJ. Randomised controlled trials - the gold standard for effectiveness research: Study design: randomised controlled trials. BJOG. 2018;125:1716. doi: 10.1111/1471-0528.15199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors) Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester (UK): John Wiley & Sons, 2019. [Google Scholar]
- 42.Paez A. Gray literature: An important resource in systematic reviews. J Evid Based Med. 2017;10:233–240. doi: 10.1111/jebm.12266. [DOI] [PubMed] [Google Scholar]
- 43.Clarivate Analytics. EndNote X9 [Computer Program]. Philadelphia: Clarivate Analytics, 2019. [cited 30 December 2020]. Available from: https://clarivate.libguides.com/endnote_training/users/enx9 .
- 44.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22:276–282. [PMC free article] [PubMed] [Google Scholar]
- 45.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O'Connell D, Oxman AD, Phillips B, Schünemann HJ, Edejer T, Varonen H, Vist GE, Williams JW Jr, Zaza S GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.GRADEpro GDT. Guideline Development Tool [Software]. [cited 30 December 2020]. McMaster University, 2020 (developed by Evidence Prime, Inc.). Available from: https://gradepro.org/
- 48.Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations, 2013. [cited 30 December 2020]. Available from: https://gdt.gradepro.org/app/handbook/handbook.html .
- 49.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, Harbord RM, Schmid CH, Tetzlaff J, Deeks JJ, Peters J, Macaskill P, Schwarzer G, Duval S, Altman DG, Moher D, Higgins JP. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- 50.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive Meta-Analysis Version 3. Englewood, NJ: Biostat, 2013. [Google Scholar]
- 52.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 53.Rosenthal R. Parametric measures of effect size. In: Cooper H, Hedges L. The handbook of research synthesis. New York: Russell Sage Foundation, 1994: 231-244. [Google Scholar]
- 54.Hedges LV, Olkin I. Statistical methods for meta-analysis: Academic press, 2014. [Google Scholar]
- 55.Sedgwick P. Meta-analyses: heterogeneity and subgroup analysis. BMJ . 2013;346:f4040. doi: 10.1136/bmj.h1435. [DOI] [PubMed] [Google Scholar]
- 56.Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta-analyses. 2nd ed. Chichester (UK): John Wiley & Sons, 2019. [Google Scholar]
- 57.Saltelli A, Tarantola S, Campolongo F, Ratto M. Sensitivity analysis in practice: A guide to assessing scientific models. Ispra, Italy: John Wiley & Sons, 2004: 1-29. [Google Scholar]
- 58.Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin Epidemiol Glob Health. 2019;7:192. [Google Scholar]
- 59.Borenstein M, Higgins JP. Meta-analysis and subgroups. Prev Sci. 2013;14:134–143. doi: 10.1007/s11121-013-0377-7. [DOI] [PubMed] [Google Scholar]
- 60.Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to meta-analysis. John Wiley & Sons, 2011. [Google Scholar]
- 61.Barrera AZ, Wickham RE, Muñoz RF. Online prevention of postpartum depression for Spanish- and English-speaking pregnant women: A pilot randomized controlled trial. Internet Interv. 2015;2:257–265. doi: 10.1016/j.invent.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Duffecy J, Grekin R, Hinkel H, Gallivan N, Nelson G, O'Hara MW. A Group-Based Online Intervention to Prevent Postpartum Depression (Sunnyside): Feasibility Randomized Controlled Trial. JMIR Ment Health. 2019;6:e10778. doi: 10.2196/10778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Felder JN, Epel ES, Neuhaus J, Krystal AD, Prather AA. Efficacy of Digital Cognitive Behavioral Therapy for the Treatment of Insomnia Symptoms Among Pregnant Women: A Randomized Clinical Trial. JAMA Psychiatry. 2020;77:484–492. doi: 10.1001/jamapsychiatry.2019.4491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fonseca A, Monteiro F, Alves S, Gorayeb R, Canavarro MC. Be a Mom, a Web-Based Intervention to Prevent Postpartum Depression: The Enhancement of Self-Regulatory Skills and Its Association with Postpartum Depressive Symptoms. Front Psychol. 2019;10:265. doi: 10.3389/fpsyg.2019.00265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Forsell E, Bendix M, Holländare F, Szymanska von Schultz B, Nasiell J, Blomdahl-Wetterholm M, Eriksson C, Kvarned S, Lindau van der Linden J, Söderberg E, Jokinen J, Wide K, Kaldo V. Internet delivered cognitive behavior therapy for antenatal depression: A randomised controlled trial. J Affect Disord. 2017;221:56–64. doi: 10.1016/j.jad.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 66.Heller HM, Hoogendoorn AW, Honig A, Broekman BFP, van Straten A. The Effectiveness of a Guided Internet-Based Tool for the Treatment of Depression and Anxiety in Pregnancy (MamaKits Online): Randomized Controlled Trial. J Med Internet Res. 2020;22:e15172. doi: 10.2196/15172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jannati N, Mazhari S, Ahmadian L, Mirzaee M. Effectiveness of an app-based cognitive behavioral therapy program for postpartum depression in primary care: A randomized controlled trial. Int J Med Inform. 2020;141:104145. doi: 10.1016/j.ijmedinf.2020.104145. [DOI] [PubMed] [Google Scholar]
- 68.Jiao N, Zhu L, Chong YS, Chan WS, Luo N, Wang W, Hu R, Chan YH, He HG. Web-based vs home-based postnatal psychoeducational interventions for first-time mothers: A randomised controlled trial. Int J Nurs Stud. 2019;99:103385. doi: 10.1016/j.ijnurstu.2019.07.002. [DOI] [PubMed] [Google Scholar]
- 69.Kalmbach DA, Cheng P, O'Brien LM, Swanson LM, Sangha R, Sen S, Guille C, Cuamatzi-Castelan A, Henry AL, Roth T, Drake CL. A randomized controlled trial of digital cognitive behavioral therapy for insomnia in pregnant women. Sleep Med. 2020;72:82–92. doi: 10.1016/j.sleep.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kersting A, Dölemeyer R, Steinig J, Walter F, Kroker K, Baust K, Wagner B. Brief Internet-based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: a randomized controlled trial. Psychother Psychosom. 2013;82:372–381. doi: 10.1159/000348713. [DOI] [PubMed] [Google Scholar]
- 71.Kersting A, Kroker K, Schlicht S, Baust K, Wagner B. Efficacy of cognitive behavioral internet-based therapy in parents after the loss of a child during pregnancy: pilot data from a randomized controlled trial. Arch Womens Ment Health. 2011;14:465–477. doi: 10.1007/s00737-011-0240-4. [DOI] [PubMed] [Google Scholar]
- 72.Klein S, Cumming GP, Lee AJ, Alexander DA, Bolsover D. Evaluating the effectiveness of a web-based intervention to promote mental wellbeing in women and partners following miscarriage, using a modified patient preference trial design: an external pilot. BJOG. 2012;119:762–767. doi: 10.1111/j.1471-0528.2012.03302.x. [DOI] [PubMed] [Google Scholar]
- 73.Loughnan SA, Sie A, Hobbs MJ, Joubert AE, Smith J, Haskelberg H, Mahoney AEJ, Kladnitski N, Holt CJ, Milgrom J, Austin MP, Andrews G, Newby JM. A randomized controlled trial of 'MUMentum Pregnancy': Internet-delivered cognitive behavioral therapy program for antenatal anxiety and depression. J Affect Disord. 2019;243:381–390. doi: 10.1016/j.jad.2018.09.057. [DOI] [PubMed] [Google Scholar]
- 74.Matvienko-Sikar K, Dockray S. Effects of a novel positive psychological intervention on prenatal stress and well-being: A pilot randomised controlled trial. Women Birth. 2017;30:e111–e118. doi: 10.1016/j.wombi.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 75.Milgrom J, Danaher BG, Gemmill AW, Holt C, Holt CJ, Seeley JR, Tyler MS, Ross J, Ericksen J. Internet Cognitive Behavioral Therapy for Women with Postnatal Depression: A Randomized Controlled Trial of MumMoodBooster. J Med Internet Res. 2016;18:e54. doi: 10.2196/jmir.4993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Missler M, van Straten A, Denissen J, Donker T, Beijers R. Effectiveness of a psycho-educational intervention for expecting parents to prevent postpartum parenting stress, depression and anxiety: a randomized controlled trial. BMC Pregnancy Childbirth. 2020;20:658. doi: 10.1186/s12884-020-03341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Molenaar NM, Brouwer ME, Burger H, Kamperman AM, Bergink V, Hoogendijk WJG, Williams AD, Bockting CLH, Lambregtse-van den Berg MP. Preventive Cognitive Therapy with Antidepressant Discontinuation during Pregnancy: Results from a Randomized Controlled Trial. J Clin Psychiatry. 2020;81 doi: 10.4088/JCP.19l13099. [DOI] [PubMed] [Google Scholar]
- 78.Nieminen K, Berg I, Frankenstein K, Viita L, Larsson K, Persson U, Spånberger L, Wretman A, Silfvernagel K, Andersson G, Wijma K. Internet-provided cognitive behaviour therapy of posttraumatic stress symptoms following childbirth-a randomized controlled trial. Cogn Behav Ther. 2016;45:287–306. doi: 10.1080/16506073.2016.1169626. [DOI] [PubMed] [Google Scholar]
- 79.O'Mahen HA, Richards DA, Woodford J, Wilkinson E, McGinley J, Taylor RS, Warren FC. Netmums: a phase II randomized controlled trial of a guided Internet behavioural activation treatment for postpartum depression. Psychol Med. 2014;44:1675–1689. doi: 10.1017/S0033291713002092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.O'Mahen HA, Woodford J, McGinley J, Warren FC, Richards DA, Lynch TR, Taylor RS. Internet-based behavioral activation--treatment for postnatal depression (Netmums): a randomized controlled trial. J Affect Disord. 2013;150:814–822. doi: 10.1016/j.jad.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 81.Pugh NE, Hadjistavropoulos HD, Dirkse D. A Randomised Controlled Trial of Therapist-Assisted, Internet-Delivered Cognitive Behavior Therapy for Women with Maternal Depression. PLoS One. 2016;11:e0149186. doi: 10.1371/journal.pone.0149186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Scherer S, Alder J, Gaab J, Berger T, Ihde K, Urech C. Patient satisfaction and psychological well-being after internet-based cognitive behavioral stress management (IB-CBSM) for women with preterm labor: A randomized controlled trial. J Psychosom Res. 2016;80:37–43. doi: 10.1016/j.jpsychores.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 83.Urech C, Scherer S, Emmenegger M, Gaab J, Tschudin S, Hoesli I, Berger T, Alder J. Efficacy of an internet-based cognitive behavioral stress management training in women with idiopathic preterm labor: A randomized controlled intervention study. J Psychosom Res. 2017;103:140–146. doi: 10.1016/j.jpsychores.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 84.Yang M, Jia G, Sun S, Ye C, Zhang R, Yu X. Effects of an Online Mindfulness Intervention Focusing on Attention Monitoring and Acceptance in Pregnant Women: A Randomized Controlled Trial. J Midwifery Womens Health. 2019;64:68–77. doi: 10.1111/jmwh.12944. [DOI] [PubMed] [Google Scholar]
- 85.King E. The effectiveness of an Internet-based stress management program in the prevention of postpartum stress, anxiety and depression for new mothers. Dissertations & Theses - Gradworks, 2009 [cited 30 December 2020]. Available from: https://xueshu.baidu.com/usercenter/paper/show?paperid=73cb128bc68565f0d391427d0a7c30cc&site=xueshu_se .
- 86.Nagata S, Seki Y, Shibuya T, Yokoo M, Murata T, Hiramatsu Y, Yamada F, Ibuki H, Minamitani N, Yoshinaga N, Kusunoki M, Inada Y, Kawasoe N, Adachi S, Oshiro K, Matsuzawa D, Hirano Y, Yoshimura K, Nakazato M, Iyo M, Nakagawa A, Shimizu E. Does cognitive behavioral therapy alter mental defeat and cognitive flexibility in patients with panic disorder? BMC Res Notes. 2018;11:23. doi: 10.1186/s13104-018-3130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sockol LE. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. J Affect Disord. 2015;177:7–21. doi: 10.1016/j.jad.2015.01.052. [DOI] [PubMed] [Google Scholar]
- 88.Lau Y, Htun TP, Wong SN, Tam WSW, Klainin-Yobas P. Therapist-Supported Internet-Based Cognitive Behavior Therapy for Stress, Anxiety, and Depressive Symptoms Among Postpartum Women: A Systematic Review and Meta-Analysis. J Med Internet Res. 2017;19:e138. doi: 10.2196/jmir.6712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Robinson L, Delgadillo J, Kellett S. The dose-response effect in routinely delivered psychological therapies: A systematic review. Psychother Res. 2020;30:79–96. doi: 10.1080/10503307.2019.1566676. [DOI] [PubMed] [Google Scholar]
- 90.Finlayson K, Crossland N, Bonet M, Downe S. What matters to women in the postnatal period: A meta-synthesis of qualitative studies. PLoS One. 2020;15:e0231415. doi: 10.1371/journal.pone.0231415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fonseca A, Gorayeb R, Canavarro MC. Women's use of online resources and acceptance of e-mental health tools during the perinatal period. Int J Med Inform. 2016;94:228–236. doi: 10.1016/j.ijmedinf.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 92.Connor K, Wambach K, Baird MB. Descriptive, Qualitative Study of Women Who Use Mobile Health Applications to Obtain Perinatal Health Information. J Obstet Gynecol Neonatal Nurs. 2018;47:728–737. doi: 10.1016/j.jogn.2018.04.138. [DOI] [PubMed] [Google Scholar]
- 93.Moher D, Schulz KF, Altman D CONSORT Group (Consolidated Standards of Reporting Trials) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–1991. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]