Abstract
Background
Video consultation (VC) has been scaled up at our academic centre attempting to facilitate and accommodate patient-provider interaction in times of social distancing during the recent and ongoing COVID-19 pandemic.
Objectives
This study evaluates qualitative outcomes with data insights from the electronic health record, to contrast satisfaction outcomes with the actual use of VC.
Methods
Healthcare providers and patients using VC during the COVID-19 pandemic at a large academic centre in the Netherlands were surveyed for user satisfaction and experiences with VC. In addition, quantitative technical assessment was performed using data related to VC from the EHR record.
Results
In total, 1,027/4,443 patients and 87/166 healthcare providers completed their online questionnaire. Users rated the use of VC during a pandemic with an average score of 8.3/10 and 7.6/10 respectively. Both groups believed the use of VC was a good solution to continue the provision of healthcare during this pandemic. The use of VC increased from 92 in March 2020 to 837 in April 2020.
Conclusion
This study strongly signals that VC is an important modality in futureproofing outpatient care during and beyond pandemic times. Further development in end-user technology is needed for EHR integrated VC solutions. Guidelines needs to be developed advising both patients and healthcare providers. Such guidelines should not solely focus on technical implementation and troubleshooting, but must also consider important aspects such as digital health literacy, patient and provider authentication, privacy and ethics.
Abbreviations: VC, video consultation; EHR, electronic health record; PCA, Principal Components Analysis
Keywords: Telemedicine, Video consultation, Virtual visit, COVID-19, Electronic health record, Patient records
1. Introduction
Since the outbreak of COVID-19 (coronavirus disease-19) caused by the coronavirus SARS CoV-2 late 2019, over 10 million detected cases of illness and over 500.000 confirmed deaths worldwide are reported [1]. On 11 March 2020, COVID-19 was declared a pandemic by the World Health Organization [2]. With no vaccine available yet, lockdown regimens, use of face masks in public areas and ‘social distancing’ have become–and still are–the most important strategies used for prevention [3,4]. Many countries have instigated rules enforcing person-to-person interactions to take place at a presumably safe distance [[4], [5], [6]]. In an attempt to prevent human-to-human transmission of the virus, whilst facilitating human interaction, lockdown restrictions are alleviated when this is deemed possible [[6], [7], [8]]. In this ongoing pandemic, strategies to prevent viral contamination to both prevent and cope with a possible second wave in healthcare are of great importance [[9], [10], [11], [12]].
During this pandemic, hospitals face multiple challenges. First, they have to cope with the increasing demands on hospital capacity, resources, and staff resulting from great numbers of patients infected with SARS CoV-2 [13]. Simultaneous, hospitals need to ensure proper care for non-COVID-19 patients in need of urgent medical attention. During the pandemic, taking care for COVID-19 patients needing Intensive Care Unit attention has become the primary focus of many institutions. Care for non-COVID-19 patients suffering from a variety of diseases and conditions including cancer is thus at risk of being compromised [14,15]. To avoid excessive backlogs impacting current and future healthcare, the challenge remains how to provide continuous high-quality healthcare in outpatient clinics during the pandemic, whilst limiting the chances of spreading the virus [16].
Replacing outpatient physical appointments with virtual care using video consultations (VC) provides a solution to this challenge. VC prevents the risk of spreading the virus, as vulnerable patients and their supporting relatives do not have to travel nor visit the hospital [17]. The use of a real-time video connection preserves important aspects of communication that cannot be accommodated over the telephone, such as visual interaction and non-verbal cues [18]. Indeed, several hospitals describe the value of using VC [[19], [20], [21], [22], [23]]. An important prerequisite for larger scale-up of VC is not only the availability of the solution to both provider and patient, but also to research the sustainability of this contact modality [24]. This in order to safeguard use and facilitate best implementation of VC in healthcare across settings as a fully accepted, normal contact modality.
The aim of this mixed methods study is to evaluate satisfaction of VC among patients and providers whilst investigating the actual use, by a quantitative technical implementation study using data from the electronic health record (EHR).
2. Methods
2.1. Study design
This study uses a mixed-methods approach, combining a qualitative survey study with a quantitative observational implementation study in a large academic hospital. Mixed methods were used to generate a set of evidence in order to elucidate if high satisfaction rates will in fact lead to increased usage of VC [25]. Three departments (surgery, anaesthesiology and reproductive medicine) had VC opportunities prior to this pandemic. Patient- and healthcare provider satisfaction using VC in the outpatient setting was surveyed. Simultaneously, VC implementation was quantitatively assessed using data from the EHR, evaluating the number of VC’s, duration of the consultations and technical aspects such as down-time of connection and number of successful- and failed connections.
2.2. Participants and setting
As per hospital policy, all non-urgent outpatient clinic visits were initially postponed. Starting up, healthcare providers from all departments were asked to select either telephone consultation (TC) or VC for patient interaction as alternative means for urgent outpatient clinic appointments that were initially scheduled as a physical contact. All patients and healthcare providers choosing to use VC as alternative means for physical contact were invited to complete our study questionnaire, evaluating their experiences with VC. The technical framework and VC-integration into the EHR is described elsewhere [19].
2.3. Data collection and analysis
Prior to sending out the satisfaction questionnaire to patients and healthcare providers, a Privacy Impact Assessment (PIA) was performed by the hospital’s Data Protection Officer (DPO). Patients were invited to complete the questionnaire via a message through their own patient portal of the EHR of the hospital, named MyChart™ (Epic Hyperspace 2017, Verona, USA), directly after their VC. Healthcare providers were invited to complete a questionnaire after having performed at least five VC scheduled, to allow for a representative opinion towards their clinical value. Questionnaires were digitally distributed using LimeSurvey© survey software (LimeSurvey GmbH, Hamburg, Germany). Data was collected anonymously to ensure that patients’ and providers’ privacy was optimally protected, and was stored on the hospital’s local server, following the European General Data Protection Regulation (GDPR). The patient questionnaire contained 11 statements with response options rated on a visual analogue scale (VAS). In addition, 3 open questions were added to provide the opportunity for motivation of responses. The questionnaire for healthcare providers contained 19 statements to be rated using a VAS with 6 open-ended questions to elaborate accordingly.
2.3.1. The use of VC during the COVID-19 pandemic
To monitor the use during the scale-up, the total number of scheduled VC of the outpatient clinic was assessed from 17 March 2020 – when physical outpatient visits were retricted- up to and including 15 May 2020. After this time, restrictions for visiting the outpatient clinic in person were partially alleviated, allowing a limited number of patients (those requiring physical interaction with the provider for various reasons according to their providers) to visit the clinic in person. The following data was obtained from the Electronic Health Records (EHR) of our hospital (Epic Hyperspace 2017, Verona, USA): number of VC scheduled for each department, waiting time for the healthcare provider to establish a video-connection, average duration of the consultation specified per department, the number of attempts to start a video connection and the number of successful video-connections.
2.4. Data analysis
Survey responses were summarized using descriptive statistics. Continuous, normally distributed variables were expressed as means and standard deviations; continuous, non-normally distributed and ordinal variables as medians and 25th–75th percentiles; categorical variables were represented as counts and percentages. Missing items were excluded from analysis. Answers to open questions were coded using standardized text analysis in combination with manual coding.
An explanatory factor analysis was performed on the 7 items that measured patient satisfaction. The Kaiser-Meyer-Olkin measure of sampling adequacy verified the sampling adequacy for the analysis (KMO = 0.866), meaning that the items were sufficiently comparable to allow for a factor analysis. The outcome of Bartlett’s test of sphericity was 12,472, p < 0.001. This indicated that correlations between items were sufficiently large for Principal Components Analysis (PCA). The PCA revealed one factor component with an Eigenvalue above 1. Internal consistency was established as the questionnaire showed a high reliability with a Cronbach’s alpha of 0.818.
A two-sided p-value ≤0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS; version 25.
3. Results
3.1. Patient and provider responses
In total, 1,027/4,443 patients (response rate: 23 %), and 87/166 healthcare providers (response rate: 53 %) completed their online questionnaire. Demographic details concerning their role at the hospital is provided in Table 1 .
Table 1.
Demographics of respondents amongst providers.
| Respondents | Completed survey (n) | % of total |
|---|---|---|
| Medical specialist | 42 | 53 % |
| Paramedic | 20 | 25 % |
| Psychosocial worker | 11 | 14 % |
| Resident | 4 | 5 % |
| Specialized nurse | 3 | 4 % |
Overall, patients and providers were highly satisfied with the use of VC during this pandemic. However, patients were significantly more satisfied with the care provided over a video connection, when compared to providers. Moreover, when stated that VC has the same value as a physical appointment at the hospital, patients tend to agree more with this statement than healthcare providers (mean 78, SD: ±25 versus mean 58 SD: ±27, p < 0.001). Users rated the use of VC during a pandemic with an average score of 8.3/10 and 7.6/10 respectively. The outcome of responses are illustrated in Table 2, Table 3 .
Table 2.
Patient- and provider responses to questionnaire items by using Visual Analogue Scale (VAS). Items were measured on a scale from 0-100 mm.* p-value ≤0.05.
| Questionnaire item | Patients (VAS Mean ± SD (n) (score 0−100) | Providers (VAS Mean ± SD (n) (score 0−100) |
p-value (Mann Whitney U test) |
|---|---|---|---|
| “I have discussed everything I needed to discuss during the video consultation”. | 91 ± 17 (749) | 78 ± 19 (87) | <0.001* |
| “I think this video consultation had the same value as if I had an physical appointment at the hospital”. | 78 ± 25 (732) | 58 ± 27 (87) | <0.001* |
| “I think video consultation is a good solution to continue the provision of healthcare during this pandemic”. | 90 ± 17 (741) | 86 ± 13 (87) | <0.001* |
| “Even when this pandemic is over, I would like to use a video consult with my healthcare provider in the future”. | 71 ± 29 (740) | 82 ± 20 (87) | <0.001* |
| “I would recommend a video consult to other patients/providers (who provider care to patients) who are not able or not allowed to attend a physical appointment at the hospital”. | 90 ± 19 (741) | 84 ± 18 (87) | <0.001* |
| “I am satisfied with the care I received during the video consult”. | 91 ± 18 (741) | 77 ± 20 (87) | <0.001* |
Table 3.
Healthcare providers’ responses to questionnaire items by using the Visual Analogue Scale (VAS). Items were measured on a scale from 0-100.
| Questionnaire item | Providers (VAS Mean (SD) score 0−100) |
|---|---|
| “The equipment I needed to use a VC was available”. | 77 (±27) |
| “If I would have needed technical support, then I knew where and how I could ask for it”. | 69 (±25) |
| “In general, I am satisfied with the quality of the video connection”. | 68 (±26) |
| “The use of VC fits the current workflow at the outpatient clinic”. | 65 (±23) |
| “I think it is easy to use a VC”. | 79 (±19) |
| “I think patients are able to use a VC”. | 57 (±23) |
| “In general, I was able to assess the healthcare condition of my patients over a video connection”. | 66 (±19) |
| “In general, I was able to assess the state of mind of my patients over a video connection”. | 71 (±19) |
When asked for their consultation preference as an alternative to a physical appointment at the outpatient clinic, 551/756 (73 %) patients and 56/80 (70 %) providers preferred a VC over a telephone consultation (TC). Other answers given by participants included having a preference for TC (50/756 (6%) of patients and 5/80 (6%) of providers), no preference (135/756 (18 %) of patients), or stated their preference to be highly dependent on the reason for the consultation (17/80 (21 %) of providers). Open text answers stated a telephone consultation was preferred over a VC by both patients and healthcare providers in case of a short follow-up call.
Though healthcare providers’ incentive was to use VC both during and after the pandemic, they reported the necessity to improve the current technology and workflow. To optimize the use of VC, 60/80 (75 %) of healthcare providers would like to have the possibility to inform the patient of any possible delays in scheduled appointments. An additional 52/80 (65 %) would like to be able to share their computer screen with patients, and 45/80 (56 %) would like to conduct a VC with multiple caregivers at the same time. Other reported wishes were; being able to record the VC, invite an interpreter, or to be able to use a laptop, personal computer, or an Android device for VC purposes.
3.2. Thematic analysis of open questions answers by patients
Patients reported that VC can be a valuable supplement to care, but the value was dependent on the reason for consultation. Some patients feared that VC would be considered a replacement rather than a substitute to care. Related concerns included the inability to perform physical examination and the impact on the patient-healthcare provider relationship by the lack of physical contact.
Twenty-two patients mentioned the inability of elderly people to use a VC and the dependence on an appropriate internet connection. Patients express their concerns that the use of VC might be difficult for specific patient groups such as patients with low digital literacy, the elderly, patients with low socio-economic status and non-native speakers.
Although the use of VC is often considered as comforting because patients are in their own environment, when using VC for psycho-social purposes, such as psychiatric care, it should first be considered if the home environment can be considered a safe place for patients. An overview of topics and items are presented in Supplementary Table 1.
3.3. Thematic analysis of open question answers by healthcare providers
Especially considering the additional value of visual cues and the ability to use inspection and read emotions, healthcare providers are satisfied with the use of VC. They underline the benefits for the patients when receiving care from their own home in terms of patient related expenditure, inconveniences and logistics.
Considering the use of technology, the usability is considered high. The absence of wanted functionalities such as a virtual waiting room or a chat function leads to challenges in the workflow. Thirteen healthcare providers preferred to use bigger screens than their smartphone. Residents specifically reported wanting the option for supervisors to dial-in to allow direct supervision during the VC. The most frequently mentioned concerns were the lack of digital literacy in patients and lack of physical contact.
3.4. The adoption of VC during the pandemic
3.4.1. The total number of VC
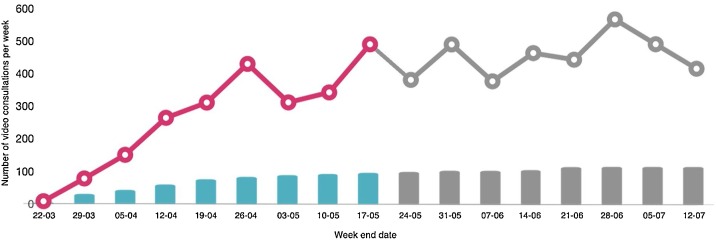
During the study period, a total of 1.546 VC were scheduled by 65 departments. The use of VC’s increased from 92 in March to 837 in April. An overview of the weekly number of VC’s are presented in Fig. 1 .
Fig. 1.
An overview of the number of VC’s used during the study period (until week 20) and the number of participating departments using VC’s. After week 20 restrictions in physical appointments at the outpatient clinic in person were alleviated, allowing a limited number of patients to be present in the outpatient clinic.
3.4.2. Waiting time and consultation duration
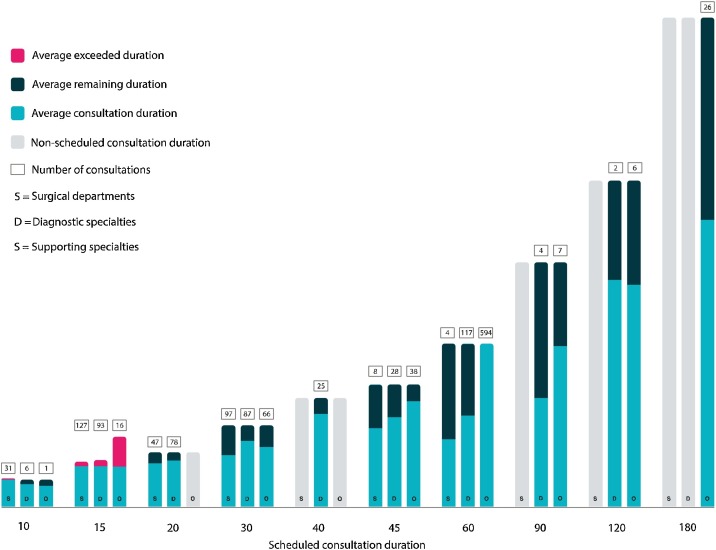
When using a VC, patients had the shortest waiting time (6.6 min, SD 9.4) when scheduled for an appointment with one of the supporting specialties or the psychosocial department, followed by the diagnostic specialties (9.1 min, SD 13.4). Patients scheduled for an appointment at one of the surgical outpatient clinics had the longest waiting time (11.3 min, SD 14.7).
Appointments that were scheduled to last 15 min, exceeded the scheduled duration on average by 1.6 min for surgical departments, 2.2 min for diagnostic specialties, and 9.1 min for supporting specialties, respectively. The time exceeding the scheduled time of a consultation, increases when the planned consultation duration increases. The scheduled duration and mean actual consultation duration for each time slot and type of speciality are illustrated in Fig. 2 .
Fig. 2.
An overview of scheduled consultation duration versus average consultation duration.
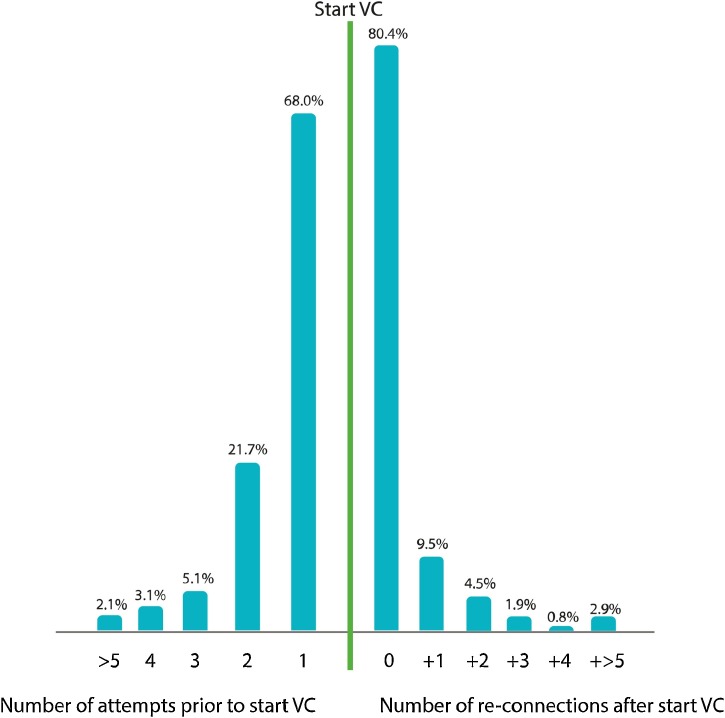
3.4.3. Number of attempts needed to establish a successful video connection
In order to start a VC, 1,052/1,546 (68 %) patients needed a single attempt only to start the VC. For 336/1,546 (21.7 %) patients, two attempts were needed to establish a successful video connection. Out of all cases, 158/1,546 (10.2 %) patients used three or more attempts to establish a connection. Once a successful connection was established, no re-connections were necessary in 81.4 % of the cases (Fig. 3 ). If, after the start of a VC re-connection attempts were made, in most cases a PC or laptop was used which are not supported by the VC software of the hospital.
Fig. 3.
Number of attempts patients made to establish a successful video connection and the number of additional re-connections after a video-connection was established.
3.4.4. Overview used devices for VC
In 44 % of cases, healthcare providers used their personal iPhone to use VC. Patients used an iPhone or an Android device in a similar amount of the VC. In 4 % of VC, patients used a PC or laptop to start a video connection.
4. Discussion
This study evaluates the use of VC based on patient reported qualitative outcomes with data insights from the electronic health record. Patients and healthcare providers considered VC a promising solution to continue the provision of healthcare during the pandemic when physical consultations were restricted according to hospital policy. Consequently, there was a significant increase in the number of scheduled VC during this period. In comparison with other hospitals in the Netherlands, our usage of VC is considered high [26]. Although the average consultation duration was shorter than the scheduled consultation duration, both patients and healthcare providers felt they could discuss everything they needed to discuss during the consultation. Moreover, patients and healthcare providers were highly satisfied and would recommend a VC to other patients and colleagues respectively. Both patients and healthcare providers alike stated they would prefer the continued use and further implementation of VC, also after this pandemic. However, when restrictions for patients visiting the outpatient clinics were alleviated, the increase of scheduled VC stagnated.
There are a few reasons that may explain for this stagnation. First, the period of strict regulations might have been insufficient to convince late adopters (healthcare providers who need to be convinced of the advantage of VC by peers or the actual laggards). Studies show, that first-hand experience is vital to experience the benefits of VC [27]. Especially to convince hesitant healthcare providers that the use of VC offers more benefits than the convenience of a telephone consultation. In scaling up VC as a regular contact modality, It may help to stress to the provider that VC is associated with a higher patient satisfaction and -understanding when compared to telephone consultation due to the presence of visual cues and non-verbal communication [28].
But more likely, when restrictions are alleviated doctors once again started to do what they became doctor for, what they enjoyed and were used to do: schedule face-to-face consultations with their patients. Doctors were not trained nor did they choose to interact with patients primarily via VC. It is thus of utmost importance in futureproofing digital care, much appreciated by patients, to train doctors and show them the benefits of VC as they are the key in scheduling appointments.
When interpreting the results of this study, some limitations are to be considered. First, because the survey was sent from the EHR, we could not gather demographic details of the respondents due to privacy legislation and to ensure anonymity. In addition, only healthcare provider and patients with VC experience were asked to participate in this study, which might have skewed the results in favour of VC. However, it is known that early adopters heaving positive experiences are vital in organisations trying to implement innovation in routine work processes. Their beliefs may help other healthcare providers with initial hesitations to support and adopt VC into their clinical practice. Second, the contextual effect of surveying respondents during a pandemic might have resulted in higher satisfaction rates because physical appointments at the hospital were restricted. Furthermore, the response rate was lower than expected. Unfortunately the new privacy regulations prevent sending out reminders on a personal basis. Yet, still almost 1 out 4 patients completed the survey. In comparison to other studies the sample size and response rate in this study remains above the average lower limit [29].
Future studies should focus on in-depth analysis of patient-provider communication over a video-connection in order to understand if and how VC alters the clinician-patient dynamic. Also, it needs to be evaluated if there is a risk on missing clinical cues that may impact patient outcomes, especially when it comes to a shorter consultation duration. Above all, equity in providing care at distance should be addressed, by first identifying vulnerable populations. For once identified, we can develop solutions to ensure equity for all patients, including disparities, those with limited health literacy or limited digital literacy [30].
5. Conclusion
This study shows that the replacement of outpatient care appointments by VC is feasible, and accepted by patients as well as providers without a detriment to the quality of care provided.
To ensure that VC can truly support in future provision of healthcare, implementation guidelines are much needed. Such guidelines should not solely focus on technical implementation and troubleshooting, but must also consider important aspects such as digital health literacy, patient and provider authentication, privacy and ethics. It is also important to acknowledge that VC is not a panacea for every consultation, nor for every patient or provider. That being said, it does offer important benefits over a telephone consultation and cannot be overlooked futureproofing healthcare. VC should thus not be regarded as a substitute for standard healthcare during a pandemic, yet should be implemented into the regular healthcare arsenal for patient follow-up and consultations. To gain best results, health care professionals need to be educated on the correct selection of consultations fit for VC and reciprocal benefits. Furthermore, there should be equity when it comes to offering care at distance within similar patients, which fits in the current climate of self-efficacy and patient empowerment [31]. The challenge for stakeholders and policy makers is to utilize the lessons learned from this pandemic to provide clear health policy guidance and to secure the use of VC during a possible second outbreak of the corona virus and to use VC in standard clinical practice in the future.
Transparency declaration
The lead author Prof. dr. Schijven affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Author’s contributors
EZB, HM, WAB and MPS conceptualised the study. HM and JB contributed to data acquisition, data analysis, interpretation of the findings and drafting the manuscript. HM, HM, JB and MJS helped to interpret the results and contributed to drafting the manuscript. WAB and MPS critically reviewed the analysis and final version of the manuscript. All authors made a thorough review of the final draft. All authors read and approved the final manuscript for publication.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Data sharing statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Summary points.
WHAT IS ALREADY KNOWN ON THIS TOPIC
-
•
Introducing video consultations in long established processes and routine clinical practices is often complex.
-
•
The rapid spread of covid-19 has focused attention on using VC to avoid physical contact between healthcare provider and patient.
-
•
VC is associated with higher patient satisfaction and patient understanding when compared to telephone consultation due to the presence of visual cues and non-verbal communication.
WHAT THIS STUDY ADDS
-
•
This study shows that the replacement of outpatient care appointments by VC is feasible, without a detriment to the quality of care provided even with shorter consultation durations.
-
•
Even within optimal conditions, the adoption of VC by healthcare providers is highly dependent on personal beliefs towards digital solutions. To overcome unnecessary variation due the willingness – or unwillingness – to use VC by a single healthcare provider or group of providers, the use of VC should be integrated in standardized guidelines.
Transparency document
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
The authors wish to thank all those who have contributed to, and were part of, the implementation of video consultation.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijmedinf.2021.104463.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Wiersinga W.J., Rhodes A., Cheng A.C., et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324(8):782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 2.Organization W.H. 2020. Coronavirus Disease 2019 (COVID-19) Situation Report -66.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200326-sitrep-66-covid-19.pdf?sfvrsn=9e5b8b48_2 Available from: [Google Scholar]
- 3.Koh W.C., Alikhan M.F., Koh D., et al. Containing COVID-19: implementation of early and moderately stringent social distancing measures can prevent the need for large-scale lockdowns. Ann. Glob. Health. 2020;86(1):88. doi: 10.5334/aogh.2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sen-Crowe B., McKenney M., Elkbuli A. Social distancing during the COVID-19 pandemic: staying home save lives. Am. J. Emerg. Med. 2020;38(7):1519–1520. doi: 10.1016/j.ajem.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahase E. Covid-19: UK starts social distancing after new model points to 260 000 potential deaths. BMJ-Br. Med. J. 2020;368 doi: 10.1136/bmj.m1089. [DOI] [PubMed] [Google Scholar]
- 6.Lewnard J.A., Lo N.C. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect. Dis. 2020;20(6):631–633. doi: 10.1016/S1473-3099(20)30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Killeen G. Containment strategies for the 2019 Novel Coronavirus: flatten the curve or crush it? Eur. J. Epidemiol. 2020;35(8):789–790. doi: 10.1007/s10654-020-00656-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matrajt L., Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg. Infect. Dis. 2020;26(8) doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Brouwer R., van Veldhuisen D.J., de Boer R.A. Surviving the first COVID-19 wave and learning lessons for the second. Eur. J. Heart Fail. 2020;22(6):975–977. doi: 10.1002/ejhf.1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahase E. Covid-19: medical leaders call for rapid review to prepare for second wave. BMJ. 2020;369:m2529. doi: 10.1136/bmj.m2529. [DOI] [PubMed] [Google Scholar]
- 11.Xu S., Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395(10233):1321–1322. doi: 10.1016/S0140-6736(20)30845-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kissler S.M., Tedijanto C., Goldstein E., et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368(6493):860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li R., Rivers C., Tan Q., et al. The demand for inpatient and ICU beds for COVID-19 in the US: lessons from Chinese cities. medRxiv. 2020 [Google Scholar]
- 14.Vogler S.A., Lightner A.L. Rethinking how we care for our patients in a time of social distancing during the COVID-19 pandemic. Br. J. Surg. 2020;107(8):937–939. doi: 10.1002/bjs.11636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smrke A., Younger E., Wilson R., et al. Telemedicine during the COVID-19 pandemic: impact on care for rare cancers. JCO Glob. Oncol. 2020;6:1046–1051. doi: 10.1200/GO.20.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. N. Engl. J. Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 17.Elkbuli A., Ehrlich H., McKenney M. The effective use of telemedicine to save lives and maintain structure in a healthcare system: current response to COVID-19. Am. J. Emerg. Med. 2020 doi: 10.1016/j.ajem.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenhalgh T., Koh G.C.H., Car J. Covid-19: a remote assessment in primary care. BMJ. 2020;368:m1182. doi: 10.1136/bmj.m1182. [DOI] [PubMed] [Google Scholar]
- 19.Barsom E.Z., Feenstra T., Bemelman W.A., Bonjer J.H., Schijven M.P. Coping with COVID-19: scaling up virtual care to standard practice. Nat. Med. 2020;26(5):632–634. doi: 10.1038/s41591-020-0845-0. [DOI] [PubMed] [Google Scholar]
- 20.Lonergan P.E., Washington Iii S.L., Branagan L., et al. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19. J. Med. Internet Res. 2020;22(7):e19322. doi: 10.2196/19322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greenhalgh T., Wherton J., Shaw S., et al. Video consultations for covid-19. BMJ. 2020;368:m998. doi: 10.1136/bmj.m998. [DOI] [PubMed] [Google Scholar]
- 22.Trethewey S.P., Beck K.J., Symonds R.F. Video consultations in UK primary care in response to the COVID-19 pandemic. Br. J. Gen. Pract. 2020;70(694):228–229. doi: 10.3399/bjgp20X709505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehrota A., R.K, Brockmeyer D.M., Barnett M.L., Bender J.A. Rapidly converting to “Virtual practices”: outpatient care in the era of Covid-19. NEJM Catalist. 2020 [Google Scholar]
- 24.Kauw Dirkjan, Huisma Piter R., Medlock Stephanie K., Koole Maarten A.C., Wierda Eric, Abu-Hanna Ameen, Schijven Marlies P., Mulder Barbara J.M., Bouma Berto J., Winter Michiel M., Schuuring Mark J. Mobile health in cardiac patients: an overview on experiences and challenges of stakeholders involved in daily use and development. BMJ Innov. 2020;0:1–8. [Google Scholar]
- 25.Regnault A., Willgoss T., Barbic S. Towards the use of mixed methods inquiry as best practice in health outcomes research. J. Patient Rep. Outcomes. 2018;2(19) doi: 10.1186/s41687-018-0043-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Twillert M. 2020. Meer ziekenhuizen gebruiken videoconsulting.https://www.medischcontact.nl/nieuws/laatste-nieuws/nieuwsartikel/meer-ziekenhuizen-gebruiken-videoconsulting-.htm [cited 2021 25-03]; Available from: [Google Scholar]
- 27.Bashshur R., Doarn C.R., Frenk J.M., et al. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed. J E Health. 2020;26(5):571–573. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 28.Lion K.C., Brown J.C., Ebel B.E., et al. Effect of telephone vs video interpretation on parent comprehension, communication, and utilization in the pediatric emergency department: a randomized clinical trial. JAMA Pediatr. 2015;169(12):1117–1125. doi: 10.1001/jamapediatrics.2015.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park H.Y., Kwon Y.M., Jun H.R., et al. Satisfaction survey of patients and medical staff for telephone-based telemedicine during hospital closing due to COVID-19 transmission. Telemed J E Health. 2020 doi: 10.1089/tmj.2020.0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nouri S., K.E.C, Lyles C.R., Karliner L. Adressing equity in telemedicine for chronic disease management during the covid-19 pandemic. NEJM Catalist. 2020 [Google Scholar]
- 31.Hinman R.S., Nelligan R.K., Bennell K.L., et al. “Sounds a bit crazy, but it was almost more personal:” a qualitative study of patient and clinician experiences of physical therapist-prescribed exercise for knee osteoarthritis via skype. Arthritis Care Res. (Hoboken) 2017;69(12):1834–1844. doi: 10.1002/acr.23218. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.