Abstract
Background
COVID-19 has posed an enormous threat to public health around the world. Some severe and critical cases have bad prognoses and high case fatality rates, unraveling risk factors for severe COVID-19 are of significance for predicting and preventing illness progression, and reducing case fatality rates. Our study focused on analyzing characteristics of COVID-19 cases and exploring risk factors for developing severe COVID-19.
Methods
The data for this study was disease surveillance data on symptomatic cases of COVID-19 reported from 30 provinces in China between January 19 and March 9, 2020, which included demographics, dates of symptom onset, clinical manifestations at the time of diagnosis, laboratory findings, radiographic findings, underlying disease history, and exposure history. We grouped mild and moderate cases together as non-severe cases and categorized severe and critical cases together as severe cases. We compared characteristics of severe cases and non-severe cases of COVID-19 and explored risk factors for severity.
Results
The total number of cases were 12 647 with age from less than 1 year old to 99 years old. The severe cases were 1662 (13.1%), the median age of severe cases was 57 years [Inter-quartile range(IQR): 46–68] and the median age of non-severe cases was 43 years (IQR: 32–54). The risk factors for severe COVID-19 were being male [adjusted odds ratio (aOR) = 1.3, 95% CI: 1.2–1.5]; fever (aOR = 2.3, 95% CI: 2.0–2.7), cough (aOR = 1.4, 95% CI: 1.2–1.6), fatigue (aOR = 1.3, 95% CI: 1.2–1.5), and chronic kidney disease (aOR = 2.5, 95% CI: 1.4–4.6), hypertension (aOR = 1.5, 95% CI: 1.2–1.8) and diabetes (aOR = 1.96, 95% CI: 1.6–2.4). With the increase of age, risk for the severity was gradually higher [20–39 years (aOR = 3.9, 95% CI: 1.8–8.4), 40–59 years (aOR = 7.6, 95% CI: 3.6–16.3), ≥ 60 years (aOR = 20.4, 95% CI: 9.5–43.7)], and longer time from symtem onset to diagnosis [3–5 days (aOR = 1.4, 95% CI: 1.2–1.7), 6–8 days (aOR = 1.8, 95% CI: 1.5–2.1), ≥ 9 days(aOR = 1.9, 95% CI: 1.6–2.3)].
Conclusions
Our study showed the risk factors for developing severe COVID-19 with large sample size, which included being male, older age, fever, cough, fatigue, delayed diagnosis, hypertension, diabetes, chronic kidney diasease, early case identification and prompt medical care. Based on these factors, the severity of COVID-19 cases can be predicted. So cases with these risk factors should be paid more attention to prevent severity.
Keywords: COVID-19, Severe case, Non-severe case, Risk factor
Background
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and is transmitted by respiratory droplets and contacts. Sources of infection are cases and asymptomatic infections, infectivity starts from the incubation period and becomes relatively strong within five days after symptom onset, the populations are generally susceptible to infection [1]. The contagiousness of SARS-CoV-2 is higher than severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV), and the scale of morbidity and mortality of COVID-19 are far greater than Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) [2–4]. The World Health Organization (WHO) declared COVID-19 a public health emergency of international concern on January 30, 2020 [5]. COVID-19 has brought great burden on the public health worldwide; as of December 27, 2020, more than 210 countries and regions worldwide have reported 79.2 million cases and more than 1.7 million deaths [6]. The National Health Commission of the People’s Republic of China made COVID-19 a Class B notifiable infectious diseases, but managed COVID-19 as a Class A infectious disease [7, 8].
COVID-19 causes lots of symptoms, including fever, cough, fatigue, and the clinical spectrum of COVID-19 pneumonia ranges from mild to critical. More than 80% infected individuals are asymptomatic or develop mild upper respiratory tract symptoms were reported [9], and parts of cases have severe courses that can include dyspnea, hypoxemia, Acute Respiratory Distress Syndrome (ARDS), shock, and even death. Mild and moderate cases can recover after symptomatic treatment, but severe and critical patients require early intervention, respiratory support and sometimes intensive care unit (ICU) care [10]. The case fatality rates of severe and critical cases are relatively high, critical patients witness significantly higher mortality which is up to 49.0%, by contrast with 2.3% for overall COVID-19 patients [9, 11]. Due to the higher mortality of severe cases, there is a need to explore the risk factors for severity, prevent developing severe cases, followed by reducing the case fatality rate.
Most studies on exploring risk factors for COVID-19 severity in China were with limited sample size and most focused on influence of clinical characteristics and treatments on severity [12–14]. Whereas comparisons of severe and non-severe cases and the influences of early symptoms on predicating progression of COVID-19 need to be further explored.
Wuhan reached the highest peak of the COVID-19 outbreak around February 12, 2020, diagnosis and treatment may have been delayed because the medical resources for COVID-19 were limited at that time [15]. During early stage, the COVID-19 case fatality rate in Hubei Province was higher than other provinces in mainland China [16, 17]. Severity of COVID-19 cases can be affected by availability of medical resources, as too many cases at one point can overwhelm the health care system, leading to increasing risks of adverse outcome and death [18, 19]. This study was mainly focued on analyzing characteristics of COVID-19 cases and identifying the risk factors for severe COVID-19 cases in order to prevent poor prognosis.
Methods
Setting, subjects, and data availability
The study setting was in 30 provinces outside Hubei Province in the mainland of China. Geographic classification into regions (eastern, central, and western) were based on socioeconomic level which were in accordance with the National Bureau of Statistics of China [20].
Subjects were symptomatic COVID-19 cases reported to the Chinese Center for Disease Control and Prevention (China CDC) COVID-19 online reporting system. The National Health Commission’s Protocol for Prevention and Control of COVID-19 issued by National Health Commission of the People’s Republic of China specified that county (district) level disease control and prevention agencies must complete an initial epidemiological investigation within 24 h upon receiving a report of a COVID-19 case and should submit investigation questionnaires to COVID-19 online reporting system. Epidemiological investigations include basic demographic data, initial symptoms at the time of diagnosis, laboratory findings and imaging features on admission, health-care-seeking behaviors and epidemiological history [21].
We included data of symptomatic cases of COVID-19 reported from January 19 to March 9, 2020. We matched information of cases in the COVID-19 online reporting system with their information in the National Notifiable Diseases Reporting System (NNDRS) based on national ID card number. Then we linked demographic data, date of symptom onset, date of diagnosis, and final clinical severity with epidemiological history, clinical manifestations, laboratory findings, radiographic features, and underlying diseases in the online reporting system. We then created a de-identified and unified dataset for all analyses.
The information in our study were from NNDRS and COVID-19 case reporting system. Analyses of these data are routine work, which are involved with relative divisions in China CDC.
Definitions
Case definitions were based on Guidelines on Diagnosis and Treatment of Patients with COVID-19, which classifies cases as mild, moderate, severe, and critical [22]. Mild cases have mild symptoms without radiographic findings of pneumonia. Moderate cases have fever or cough with radiographic findings of pneumonia. Severe cases were those with shortness of breath, respiratory rate (RR) over 30/min, resting blood oxygen saturation less than 93%, and PaO2/FiO2 less than 300 mm Hg. Cases with radiographic findings of pneumonia progressing more than 50% in 24–28 h were considered severe cases. Critical cases had dyspnea with need for mechanical ventilation, shock, multiple organ failure, and required ICU care. The clinical severity classification in NNDRS is dynamic, which is revised by clinical doctors based on the progression of the cases, and being the most severe situation of cases finally. We categorized mild and moderate cases as non-severe cases, and categorized severe and critical cases as severe cases. Date of symptom onset was the onset date of fever, cough, or other symptoms of COVID-19, and was self-reported. Date of diagnosis was when the individual was diagnosed with COVID-19. All cases were laboratory confirmed by Real-Time reverse transcriptase Polymerase Chain Reaction (RT-PCR) assay. Early abnormal imaging included multiple small speckled shadows and interstitial changes with an obvious peripheral distribution, and bilateral multilobar ground-glass opacification and infiltration [22]. Laboratory tests and chest radiograph or Computed Tomography (CT) on admission were not mandatory in the case epidemiology investigation questionnaire, thus some data of laboratory findings and imaging features were unavailable.
Exposure history was determined by epidemiology history, travel or living in Wuhan or other areas with cases reported, contact history with symptomatic individuals from Wuhan and its surrounding areas or other communities reporting cases, contact history with a confirmed case or asymptomatic infected person, history of treatment, and presence of clustered cases in family, workplace, kindergartens, or schools.
Statistical methods
This study used descriptive statistics to analyze median [interquartile range (IQR)], frequencies and proportions. We used univariate logistic regression analyses to determine association of variables with severity of COVID-19. Variables with P-values < 0.05 in the univariate logistic analyses were included in multivariable logistic regression. We used forward selection of variables in the logistic regression model and determined adjusted odds ratios (aORs) and their 95% confidence intervals (CIs). A two-sided α of less than 0.05 (P < 0.05) was considered statistically significant. Statistical analyses were made with SPSS (Version 22.0).
Results
Sociodemographic and epidemiologic characteristics
The objects for this study were12 647 confirmed cases of COVID-19 reported in 30 provinces outside Hubei Province in mainland China between January 19, 2020 and March 9, 2020. The median age of all cases was 45 years (IQR: 33–56 years); the median age of severe cases was 57 years (IQR: 46–68 years) and the median age of non-severe cases was 43 years (IQR: 32–54 years). There were more cases among males (52.0%) than females (48.0%), and 23.6% cases had at least one underlying chronic diseases, 8.0% had an exposure history (Table 1).
Table 1.
The characteristics of COVID-19 cases based on surveillanc data from January 19 to March 19 in 2020 in China
| Variables | All cases, n (%) | Severe cases, n (%) |
|---|---|---|
| Sex | ||
| Male | 6581 (52.0) | 965 (58.1) |
| Female | 6066 (48.0) | 697 (41.9) |
| Age group, years | ||
| 0–19 | 826 (6.5) | 6 (0.4) |
| 20–39 | 4132 (32.7) | 253 (15.2) |
| 40–59 | 5241 (41.4) | 686 (41.3) |
| ≥ 60 | 2448 (19.4) | 717 (43.1) |
| Living area | ||
| Urban | 6923 (54.7) | 959 (57.7) |
| Rural | 5724 (45.3) | 703 (42.3) |
| Regions | ||
| East | 4860 (38.4) | 590 (35.5) |
| Central | 5351 (42.3) | 730 (44.0) |
| West | 2436 (19.3) | 342 (20.6) |
| From symptom onset to diagnosis, days | ||
| 0–2 | 3811 (30.1) | 272 (16.4) |
| 3–5 | 3610 (28.5) | 447 (26.9) |
| 6–8 | 2583 (20.4) | 451 (27.1) |
| ≥ 9 | 2643 (20.9) | 492 (29.6) |
| Underlying disease | ||
| No | 9664 (76.4) | 927 (55.8) |
| Yes | 2983 (23.6) | 735 (44.2) |
| Exposure history | ||
| No | 1009 (8.0) | 215 (12.9) |
| Yes | 11 638 (92.0) | 1447 (87.1) |
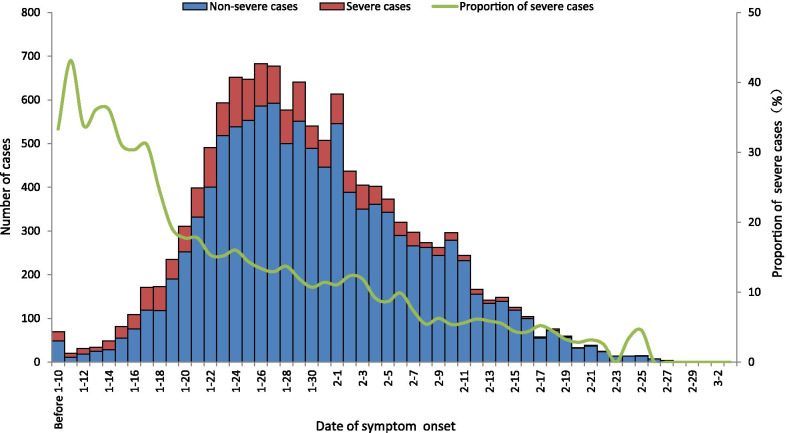
According to the definition of clinical classification of COVID-19, the 12 647 cases were categorized into 3788 (30.0%)mild cases, 7197 (56.9%) moderate cases, 1280 (10.1%)severe cases and 382 (3.0%)critical cases; 966 (58.1%) severe cases were male, 717 (43.1%) were ≥ 60 years, 6923 (54.7%) lived in urban area (Fig. 1).
Fig. 1.
Clinical categories of different sociodemographic characteristics of COVID-19 cases. The data in this figure was surveillance data from January 19 to March 9 in 2020, from the NNDRS and COVID-19 online reporting system in China CDC
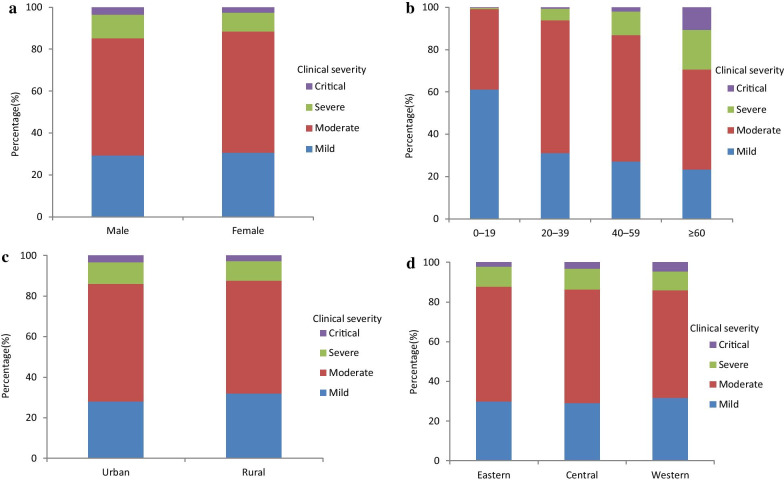
Characteristic of time from symptom onset to diagnosis
The median time from symptom onset to diagnosis was 4 days (IQR: 2–8 days) for the total cases, 6 days (IQR: 4–9) for severe cases, 5 days (IQR: 2–8) for non-severe cases. Regardless of gender, age group, region and residency, the proportion of severe cases increased with increasing time from symptom onset to diagnosis (Fig. 2).
Fig. 2.
Severity of different characteristics of COVID-19 cases with different time from symptom onset to diagnosis. Data in this figure were surveillance data from January 19 to March 9 in 2020 from the NNDRS and COVID-19 online reporting system in China CDC
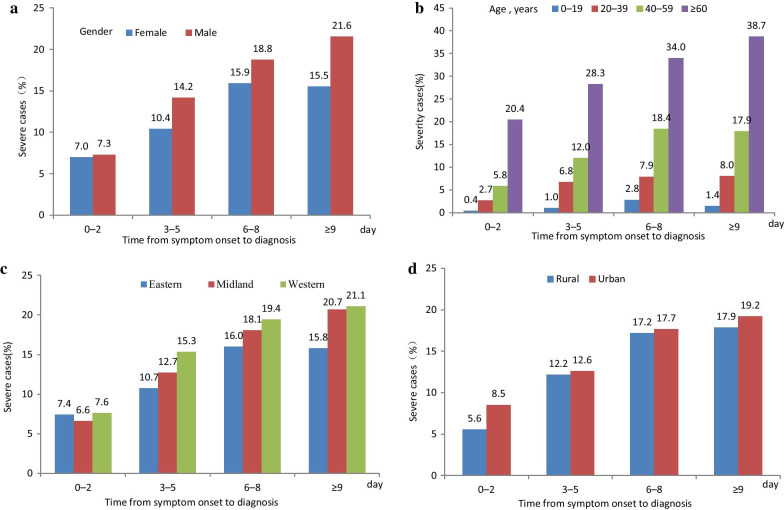
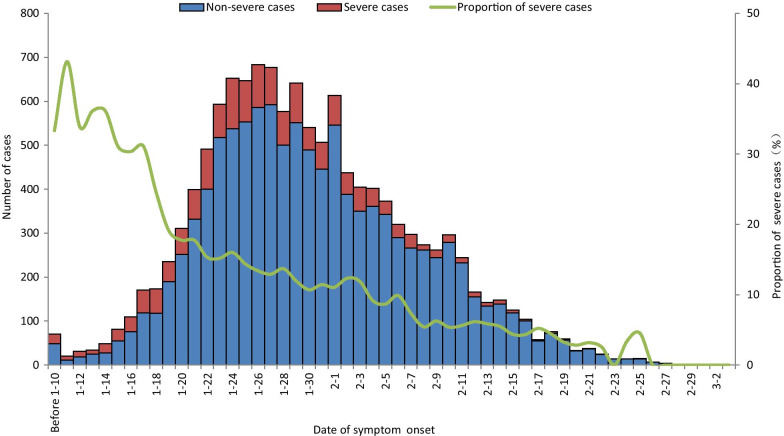
Proportion of severe COVID-19 cases progression
The proportion of severe cases decreased from 23.3% before January 23, 2020 to 6.5% after February 5, 2020 (Fig. 3).
Fig. 3.
Distribution of severe and non-severe cases of COVID-19 with date of symptom onset. This figure shows the time course of the epidemic. The number and proportion of severe cases decreased after the epidemic peaked. Before January 23, 23.3% of cases were severe or critical, compared with 6.5% after February 5. Information in this figure was surveillance data from NNDRS and COVID-19 online reporting system
The risk factors of severe COVID-19 cases
The risk factors for developing severe COVID-19 were being male (aOR = 1.3, 95% CI: 1.2–1.5); fever (aOR = 2.3, 95% CI: 2.0–2.7), fatigue (aOR = 1.4, 95% CI: 1.2–1.6), cough (aOR = 1.3, 95% CI: 1.2–1.5), diabetes (aOR = 1.5, 95% CI: 1.2–1.8), hypertension (aOR = 1.5, 95% CI: 1.2–1.8) and chronic kidney disease (aOR = 2.5, 95% CI: 1.4–4.6); abnormal CT imaging (aOR = 1.6, 95% CI: 1.2–2.1), lymphocyte count decrease (aOR = 1.3, 95% CI: 1.1–1.5). With the increase of age, the risk for severity was gradually higher, < 20 years (aOR = 1), 20–39 years (aOR = 3.9, 95% CI: 1.8–8.4), 40–59 years (aOR = 7.6, 95% CI: 3.6–16.3), ≥ 60 years (aOR = 20.4, 95% CI: 9.5–43.7). With the increase of time from symptom onset to diagnosis, the risk of severity was gradually higher, 0–2 days (aOR = 1), 3–5 days (aOR = 1.4, 95% CI: 1.2–1.7), 6–8 days (aOR = 1.8, 95% CI: 1.5–2.1), ≥ 9 days (aOR = 1.9, 95% CI: 1.6–2.3) (Table 2).
Table 2.
The risk factors for developing severe COVID–19 cases based on surveillance data from January 19 to March 9 in 2020 in China
| Variable | Severe cases (n)/all cases (N) (%) | Crude OR (95% CI) | P value | aOR (95% CI) |
|---|---|---|---|---|
| Gender | ||||
| Female | 697/6066 (11.5) | 1 | 1 | |
| Male | 965/6581 (14.7) | 1.33 (1.2–1.5) | 0.000 | 1.34 (1.2–1.5) |
| Age group, years | ||||
| 0–19 | 6/826 (0.8) | 1 | 1 | |
| 20–39 | 253/4132 (6.1) | 7.63 (3.6–16.2) | 0.000 | 3.90 (1.8–8.4) |
| 40–59 | 686/5241 (13.1) | 17.62 (8.3–37.2) | 0.000 | 7.63 (3.6–16.3) |
| ≥ 60 | 717/2448 (29.3) | 48.46 (22.9–102.5) | 0.000 | 20.42 (9.5–43.7) |
| Living area | ||||
| Rural | 703/5724 (12.3) | 1 | 1 | |
| Urban | 959/6923 (13.9) | 1.15 (1.0–1.3) | 0.010 | 0.94 (0.8–1.1) |
| Region | ||||
| East | 590/4860 (12.1) | 1 | 1 | |
| Central | 730/5351 (13.7) | 1.14 (1.0–1.3) | 0.022 | 1.12 (1.0–1.3) |
| West | 342/2436 (14.0) | 1.18 (1.0–1.4) | 0.022 | 1.40 (1.2–1.6) |
| The symptom onset to diagnosis, days | ||||
| 0–2 | 272/3811 (7.1) | 1 | 1 | |
| 3–5 | 447/3610 (12.4) | 1.84 (1.6–2.2) | 0.000 | 1.41 (1.2–1.7) |
| 6–8 | 451/2583 (17.5) | 2.75 (2.4–3.2) | 0.000 | 1.79(1.5–2.1) |
| ≥ 9 | 492/2643 (18.6) | 2.98 (2.5–3.5) | 0.000 | 1.91(1.6–2.3) |
| Fever | ||||
| No | 265/4376 (6.1) | 1 | 1 | |
| Yes | 1397/8271 (16.9) | 3.14 (2.7–3.6) | 0.000 | 2.30(2.0–2.7) |
| Fatigue, joint or muscle soreness | ||||
| No | 1034/9397 (11.0) | 1 | 1 | |
| Yes | 628/3250 (19.3) | 1.94 (1.7–2.2) | 0.000 | 1.33(1.2–1.5) |
| Cough or respiratory symptoms | ||||
| No | 520/5597 (9.3) | 1 | 1 | |
| Yes | 1142/7050 (16.2) | 1.75 (1.6–1.9) | 0.000 | 1.40(1.2–1.6) |
| Gastrointestinal symptoms | ||||
| No | 1495/11712 (12.8) | 1 | 1 | |
| Yes | 167/935 (17.9) | 1.48 (1.3–1.8) | 0.000 | 1.09(0.9–1.3) |
| Headache | ||||
| No | 1446/11308 (12.8) | 1 | 1 | |
| Yes | 216/1339 (16.1) | 1.31 (1.1–1.5) | 0.001 | 1.15(1.0–1.4) |
| Conjunctival congestion | ||||
| No | 1658/12625 (13.1) | 1 | ||
| Yes | 4/22 (18.2) | 1.47 (0.5–4.4) | 0.487 | |
| White blood cell count (109/L)a | ||||
| 4–10 | 1088/7981 (13.6) | 1.0 | 1 | |
| < 4 | 356/2477 (14.4) | 1.06 (0.9–1.2) | 0.351 | 1.03(0.9–1.2) |
| > 10 | 87/400 (21.8) | 1.76 (1.4–2.3) | 0.000 | 1.47(1.1–2.0) |
| Unavailable | 131/1789 (7.4) | 0.51 (0.4–0.6) | 0.000 | 0.54(0.2–1.5) |
| Lymphocyte count (109/L)b | ||||
| 0.8–3.5 | 1029/8632 (11.9) | 1 | 1 | |
| < 0.8 | 431/1752 (24.6) | 2.41 (2.1–2.7) | 0.000 | 1.28 (1.1–1.5) |
| > 3.5 | 62/444 (14.0) | 1.20 (0.9–1.6) | 0.197 | 1.22 (0.9–1.7) |
| Unavailable | 140/1819 (7.8) | 0.62 (0.5–0.8) | 0.000 | 1.72 (0.8–3.6) |
| Lymphocyte percentage(%)c | ||||
| 20–40 | 690/6084 (11.3) | 1 | 1 | |
| < 20 | 739/3441 (21.5) | 2.14 (1.9–2.4) | 0.000 | 1.19 (1.0–1.4) |
| > 40 | 100/1333 (7.5) | 0.63 (0.5–0.8) | 0.000 | 0.77 (0.60–1.0) |
| Unavailable | 133/1789 (7.5) | 0.63 (0.5–0.8) | 0.000 | 1.22 (0.4–3.8) |
| Neutrophil percentage (%)d | ||||
| 40–75 | 914/7928 (11.5) | 1 | 1 | |
| < 40 | 117/944 (12.4) | 1.09 (0.9–1.3) | 0.433 | 1.27 (1.0–1.6) |
| > 75 | 498/1984 (25.1) | 2.57 (2.3–2.9) | 0.000 | 1.55 (1.3–1.9) |
| Unavailable | 133/1791 (7.5) | 0.62 (0.5–0.8) | 0.000 | 0.98 (0.3–2.8) |
| Abnormal X-ray | ||||
| No | 326/2576 (12.7) | 1 | 1 | |
| Yes | 239/1319 (18.1) | 1.53 (1.3–1.8) | 0.000 | 1.29 (1.1–1.6) |
| Unavailable | 1097/8752 (12.5) | 0.99 (0.9–1.1) | 0.883 | 0.96 (0.8–1.1) |
| Abnormal CT imaging | ||||
| No | 326/2576 (12.7) | 1 | 1 | |
| Yes | 239/1319 (18.1) | 3.21 (2.4–4.3) | 0.000 | 1.57(1.2–2.1) |
| Unavailable | 1097/8752 (12.5) | 2.14 (1.6–2.9) | 0.000 | 1.53(1.1–2.2) |
| Underlying diseases | ||||
| No | 927/9664 (9.6) | 1 | 1 | |
| Yes | 735/2983 (24.6) | 3.08 (2.8–3.4) | 0.000 | 0.88 (0.7–1.1) |
| Diabetes | ||||
| No | 1447/12 098 (12.0) | 1 | 1 | |
| Yes | 215/549 (39.2) | 4.73(4.0–5. 7) | 0.000 | 1.96 (1.6–2.4) |
| Hypertension and other cardiovascular and cerebrovascular diseases | ||||
| No | 1195/11126 (10.7) | 1 | 1 | |
| Yes | 467/1521 (30.7) | 3.68 (3.3–4.2) | 0.000 | 1.46 (1.2–1.8) |
| Lung diseases | ||||
| No | 1574/12350 (12.8) | 1 | 1 | |
| Yes | 88/297 (29.6) | 2.88 (2.2–3.7) | 0.000 | 1.42 (1.1–1.9) |
| Chronic liver diseases | ||||
| No | 1648/12 550 (13.1) | 1 | ||
| Yes | 14/97 (14.4) | 1.12 (0.6–2.0) | 0.707 | |
| Chronic kidney diseases | ||||
| No | 1637/12 594 (13.0) | 1 | 1 | |
| Yes | 25/53 (47.2) | 5.97 (3.5–10.3) | 0.000 | 2.50 (1.4–4.6) |
| Exposure history | ||||
| No | 215/1009 (21.3) | 1 | 1 | |
| Yes | 1447/11 638 (12.4) | 0.53 (0.5–0.6) | 0.000 | 0.63 (0.5–0.8) |
a The normal range of the white blood cell count is 4 × 109/L to 10 × 109/L
b The lymphocyte count normal range is 0.8 × 109/L to 3.5 × 109/L
c The lymphocyte percentage normal range is 20% to 40%
d The normal range of percent neutrophils is 40% to 75% [23]
Discussion
COVID-19 are bringing huge burden on public health globally, and decreasing the severity of cases would reduce the medical resources and case fatality. This study found risk factors included being male, older age, symptoms including fever, cough and fatigue at the time of diagnosis, lymphopenia, abnormal CT imaging at the time of diagnosis, hypertension, diabetes, and chronic kidney disease, which were consistent with some reports [4, 12, 15, 19, 24]. Meanwhile, our study found that having exposure history and timely diagnosis decreased the risks for developing severe cases. These findings are helpful for predicting and preventing the poor prognosis of COVID-19 cases, moreover providing evidence for further making strategy for controlling COVID-19.
Regarding the gender in our study, males had higher risk of developing severe COVID-19 than females, which is consistent with some reports [4, 24]. The differences between different gender may be related to underlying biological differences, diversity of immune responses, sex hormones and a combination of behavioral or lifestyle risk factors [25–27]. Furthermore, several comorbidities, which disproportionally occur in men, likely contribute to worse COVID-19 outcomes [28]. The clinical situation of COVID-19 cases varied by age. We found that the elderly tended to have severe illness, while younger individuals had less severe cases. This might due to the lower immunity and higher prevalence rate of comorbidities in elderly people [29]. In contrast with adults, young generation less than 20 years that mainly include school students and children were less frequently exposed to the main sources of virus transmission, as their movement was limited by interventions such as closure of schools [11, 30]. And some reported that most infected children were less likely to be symptomatic or develop severe symptoms, as well as the percentage of patients who were treated in the ICU or received invasive mechanical ventilation was increased for the elderly [31, 32].
Similar to SARS-CoV and MERS-CoV infections, the most common symptoms of COVID-19 were fever and cough, but the absence of fever in Covid-19 was more frequent than SARS-CoV and MERS-CoV infection [34, 35, 36]. Fever is a reaction activated by the immune systems to resist pathogens, and cough might indicate the defense against invaders [4]. Consitent with some reports, hyperpyrexia more often appeared in older patients than that in young and middle age patients with COVID-19 [37]. Also the hyperpyrexia associated with adverse outcomes in patients with COVID-19, which might be caused by SARS-CoV-2 related brain injury, exuberant immune response, and thrombus formation reported by relative study [38].
Laboratory examinations can provide essential assistance to predict severity of COVID-19 [39]. The most common laboratory test abnormality was lymphopenia. [28, 40] which associated with final COVID-19 severity [1, 10]. Chest imaging played a key role in the early evaluation by allowing rapid triage of dyspneic patients [41]. Early in the progression of this disease, CT imaging findings in approximately 15% of individuals and chest radiograph findings in approximately 40% of individuals can be normal [42]. Similar to our result, previous study demonstrated that initial chest CT abnormalities would indicate a poor prognosis [41].
As for COVID-19, the average time from exposure to symptom onset is 5 days, and 97.5% of people who develop symptoms do so within 11.5 days [42, 43]. Early diagnosis and prompt medical care help relieve symptoms and signs, prevent illness aggravation and lessen severity [32, 33]. A study indicated that presymptomatic transmission is a major contributor to the spread of SARS-CoV-2, early identification and diagnosis of cases could prevent more infections [44], moreover, can prevent the poor prognosis.
Our study showed that underlying diseases were associated with increasing risks of severity of COVID-19, and that 55.8% of severe cases had at least one chronic disease, a lower percentage than that the 68% found in a study of critical patients infected with SARS-CoV-2 admitted to ICU [45]. SARS-CoV-2 infection can affect the cardiovascular system and can cause acute kidney failure [46, 47]. Meanwhile, chronic underlying conditions can cause metabolic disorders and weaken immune systems, all of these factors place patients with hypertension and chronic kidney failure at greater risk of severe SARs-CoV-2 infection [48, 49]. The Guidelines on Diagnosis and Treatment of Patients with COVID-19 also indicates that people with these underlying diseases are at high risk of severity [1].
A history of travel to epidemic area was important for early case finding and management. According to the Protocol for Prevention and Control of COVID-19, persons with travel history to Wuhan or other high risk communities were paid more attention to be screened as a high-risk population and strictly followed up, medical workers should to increase awareness of people with exposure histories [50, 51]. In the early phase of the epidemic (before January 23), 23.3% were severe, and most cases reported from other provinces outside Hubei were from Hubei [52]. To control the epidemic, provinces outside Hubei fortified quarantine and management of people from Hubei, and ensuring home-medical-observation for 14 days and admission to designated hospitals with related symptoms arise [53, 54]. These control and prevention measures were instrumental in shortening time from symptom onset to diagnosis, allowing people with exposure histories to receive early detection and early medical care, which could be explanations for our finding that having exposure histories reduced the risks of developing severe COVID-19 cases.
There are several limitations in our study. One is that data in our study were from January to March in 2020, the epidemiological and clinical characteristics might be different as for the mutation of the virus. Besides, the symptoms at the time of diagnosis and date of symptom onset were based on self-report, there might be recall bias. Third, the laboratory and imaging testing were not mandatory in admission, so some data were unavailable. Finally, we did not have hospitalised treatment records which might also influence the progression of illness.
Conclusions
Our study with large sample size explored the risk factors for developing severe cases of COVID-19. Our study found early diagnosis and having exposure history reduced the risks of COVID-19 severity. Meanwhile, the risk factors of developing severe COVID-19 including male, older age, fever, fatigue, cough, hypertension, diabetes, and chronic kidney, which are very helpful to predict and prevent developing severe cases of COVID-19. Therefore, we should pay more attention to cases with these risk factors, and avert poor prognosis.
Acknowledgements
We thank Lance Rodewald, senior advisor to China CDC’s National Immunization Program, for English language editing. We thank all healthcare workers at different levels and investigators for their contribution.
Abbreviations
- COVID-19
Coronavirus Disease 2019
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- MERS-CoV
Middle East Respiratory Syndrome Coronavirus
- SARS-CoV
Severe Acute Respiratory Syndrome Coronavirus
- MERS
Middle East Respiratory Syndrome
- SARS
Severe Acute Respiratory Syndrome
- ICU
Intensive Care Unit
- WHO
World Health Organization
- China CDC
Chinese Center for Disease Control and prevention
- NNDRS
National Notifiable Diseases Reporting System
- RR
Respiratory Rate
- CT
Computed Tomography
- RT-PCR
Real-time reverse transcriptase Polymerase Chain Reaction
- aOR
adjusted Odds Ratio
- CI
Confidence Interval
Authors' contributions
M-JG designed and implemented the study, managed and analyzed the data, interpreted the data and wrote, reviewed and edited the manuscript. G-XH and Z-JL designed the study, interpreted the data, wrote and edited the manuscript. L-PW, XR and J-XY convinced the idea, review and revised the manuscript. Z-RC, C-JZ, Z-JA, YL, X-KY and H-TZ provided support in study design and revised the manuscript. Z-JF wrote, review and edited the manuscript. All authors read and approved the final manuscript.
Funding
China Ministry of Science and Technology (Grant No. 2018ZX10713001), National Natural Science Foundation of China (NSFC) (No. 91846302).
Availability of data and materials
According to the requirement of the NNDRS in China CDC, original data can be used only by our researchers and cannot be provided to others.
Declarations
Ethics approval and consent to participate
The information in our study were from NNDRS and COVID-19 case reporting system. Analyses of these data are routine work, which are involved with relative divisions in China CDC.
Consent for publication
Written informed consent was obtained from the participants for the publication of this paper.
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Zhong-Jie Li, Email: lizj@chinacdc.cn.
Guang-Xue He, Email: hegx@chinacdc.cn.
Zi-Jian Feng, Email: fengzj@chinacdc.cn.
References
- 1.China NHCotPsRo. Guidelines on the diagnosis and treatment of patients with COVID-19 (Edition 8). http://www.nhc.gov.cn/xcs/zhengcwj/202008/0a7bdf12bd4b46e5bd28ca7f9a7f5e5a/files/a449a3e2e2c94d9a856d5faea2ff0f94.pdf. Accessed 19 Aug 2020.
- 2.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kakodkar P, Kaka N, Baig MN. A Comprehensive Literature Review on the Clinical Presentation, and Management of the Pandemic Coronavirus Disease 2019 (COVID-19) Cureus. 2020;12(4):e7560. doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang SY, Lian JS, Hu JH, Zhang XL, Lu YF, Cai H, et al. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID-19 in Zhejiang, China. Infect Dis Poverty. 2020;9(1):85. doi: 10.1186/s40249-020-00710-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. IHR Emergency Committee on Novel Coronavirus (2019-nCoV). https://www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov). Accessed 30 Jan 2020.
- 6.WHO. Weekly epidemiological update - 29 December 2020. https://www.who.int/publications/m/item/weekly-epidemiological-update---29-december-2020. Accessed 29 Dec 2020.
- 7.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.China NHCotPsRo. Notice of National Health Commission of the People’s Republic of China. http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml . Accessed 20 Jan 2020. [DOI] [PMC free article] [PubMed]
- 9.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen FF, Zhong M, Liu Y, Zhang Y, Zhang K, Su DZ, et al. The characteristics and outcomes of 681 severe cases with COVID-19 in China. J Crit Care. 2020;8(60):32–37. doi: 10.1016/j.jcrc.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 12.Liu D, Cui P, Zeng S, Wang S, Feng X, Xu S, Li R, et al. Risk factors for developing into critical COVID-19 patients in Wuhan, China: A multicenter, retrospective, cohort study. Clin Med. 2020;25:100471. doi: 10.1016/j.eclinm.2020.100471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xi C, Jin T, Xiang Jianhua Hu, Jingjing. Retrospective study on the epidemiological characteristics of 139 patients with COVID-19 on the effects of severity. Chongqing Med. 2020;49(17):2802–2806. [Google Scholar]
- 14.Zhao C, Xu Y, Zhang X, Zhong Y, Long L, Zhan W, et al. Public health initiatives from hospitalized patients with COVID-19 China. J Infect Public Health. 2020;13(9):1229–1236. doi: 10.1016/j.jiph.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li X, Xu S, Yu M, Wang K, Tao Y, Zhou Y, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peng Y, Xu B, Sun B, Han G, Zhou YH. Importance of timely management of patients in reducing fatality rate of coronavirus disease 2019. J Infect Public Health. 2020;13(6):890–892. doi: 10.1016/j.jiph.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang J, Chen X, Deng X, Chen Z, Gong H, Yan H, et al. Disease burden and clinical severity of the first pandemic wave of COVID-19 in Wuhan, China. Nat Commun. 2020;11(1):5411. doi: 10.1038/s41467-020-19238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Critical Care Medicine of Chinese Medical Association Chinese Medical Doctors Association Critical Care Medicine Branch, Chinese Pathophysiological Society of Committee of Critical Care Medicine. Chin J Crit Care Intensive Care Med. 2020;6(1):1–11. [Google Scholar]
- 19.Sun Y, Sun W, Ye J, Yu WL, Chen H, Shan N, et al. Analysis of the clinical characteristics of novel coronavirus pneumonia and the influencing factors of severe disease progress. Chin J Emerg Med. 2020;29(7):901–7. [Google Scholar]
- 20.National Bureau of Statistics. Fifteenth in a series of reports on China's achievements in economic and social development in the 70th anniversary of the founding of China. http://www.stats.gov.cn/tjsj/zxfb/201908/t20190812_1690526.html. Accessed 12 Aug 2019.
- 21.China NHCotPsRo. Protocol for Prevention and Control of COVID-19 (Edition 6). http://www.nhc.gov.cn/xcs/zhengcwj/202003/4856d5b0458141fa9f376853224d41d7/files/4132bf035bc242478a6eaf157eb0d979.pdf. Accessed 7 Mar 2020. [DOI] [PMC free article] [PubMed]
- 22.China NHCotPsRo. Guidelines on the diagnosis and treatment of patients with COVID-19 (Edition 7). http://www.nhc.gov.cn/xcs/zhengcwj/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf. Accessed 3 Mar 2020.
- 23.Chen W, Pan X. Diagnostics. 6th ed. 271. Beijing. People’s Medical Publishing House Corporation. 2004.
- 24.Yingtao Z, Deng Aiping Hu, Ting CX, Yali Z, et al. Clinical outcomes of COVID-19 cases and influencing factors in Guangdong province. Chin J Epidemiol. 2020;41(12):1999–2004. doi: 10.3760/cma.j.cn112338-20200318-00378. [DOI] [PubMed] [Google Scholar]
- 25.Kelada M, Anto A, Dave K, Saleh SN. The role of sex in the risk of mortality from COVID-19 amongst adult patients: a systematic review. Cureus. 2020;12(8):e10114. doi: 10.7759/cureus.10114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–638. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 27.Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588(7837):315–320. doi: 10.1038/s41586-020-2700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haitao T, Vermunt JV, Abeykoon J, Ghamrawi R, Gunaratne M, Jayachandran M, et al. COVID-19 and sex differences: mechanisms and biomarkers. Mayo Clin Proc. 2020;95(10):2189–2203. doi: 10.1016/j.mayocp.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dhochak N, Singhal T, Kabra SK, Lodha R. Pathophysiology of COVID-19: why children fare better than adults? Indian J Pediatr. 2020;87(7):537–546. doi: 10.1007/s12098-020-03322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naja M, Wedderburn L, Ciurtin C. COVID-19 infection in children and adolescents. Br J Hosp Med (Lond) 2020;81(8):1–10. doi: 10.12968/hmed.2020.0321. [DOI] [PubMed] [Google Scholar]
- 31.Zimmermann P, Curtis N. Coronavirus Infections in Children Including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39(5):355–368. doi: 10.1097/INF.0000000000002660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet. 2015;386(9997):995–1007. doi: 10.1016/S0140-6736(15)60454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gu J, Gong E, Zhang B, Zheng J, Gao Z, Zhong Y, et al. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005;202(3):415–424. doi: 10.1084/jem.20050828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chu H, Zhou J, Wong BH, Li C, Chan JF, Cheng ZS, et al. Middle east respiratory syndrome coronavirus efficiently infects human primary T lymphocytes and activates the extrinsic and intrinsic apoptosis pathways. J Infect Dis. 2016;213(6):904–914. doi: 10.1093/infdis/jiv380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harrison AG, Lin T, Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunol. 2020;41(12):1100–1115. doi: 10.1016/j.it.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suwanwongse K, Shabarek N. Hyperpyrexia in patients with COVID-19. J Med Virol. 2020;92(11):2857–2862. doi: 10.1002/jmv.26154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta. 2020;510:475–482. doi: 10.1016/j.cca.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang YQ, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5(1):33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jalaber C, Lapotre T, Morcet-Delattre T, Ribet F, Jouneau S, Lederlin M. Chest CT in COVID-19 pneumonia: A review of current knowledge. Diagn Interv Imaging. 2020;101(7–8):431–437. doi: 10.1016/j.diii.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324(8):782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 43.McAloon C, Collins Á, Hunt K, Barber A, Byrne AW, Butler F, et al. Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open. 2020;10(8):e039652. doi: 10.1136/bmjopen-2020-039652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang J, Litvinova M, Wang W, Wang Y, Deng X, Chen X, et al. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study. Lancet Infect Dis. 2020;20(7):793–802. doi: 10.1016/S1473-3099(20)30230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lotfi M, Hamblin MR, Rezaei N. COVID-19: Transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254–266. doi: 10.1016/j.cca.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chaturvedi S, Gorelick P. The interplay between COVID 19 and non-communicable diseases. J Stroke Cerebrovasc Dis. 2020;29(9):105104. doi: 10.1016/j.jstrokecerebrovasdis.2020.105104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ma CM, Liu Q, Li ML, Ji MJ, Zhang JD, Zhang BH, Yin FZ. The Effects of Type 2 diabetes and postoperative pneumonia on the mortality in inpatients with surgery. Diabetes Metab Syndr Obes. 2019;29(12):2507–2513. doi: 10.2147/DMSO.S232039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.China NHCotPsRo. Protocol for Prevention and Control of COVID-19(Edition 3). http://www.nhc.gov.cn/xcs/zhengcwj/202001/470b128513fe46f086d79667db9f76a5/files/8faa1b85841f42e8a0febbea3d8b9cb2.pdf. Accessed 28 Jan 2020. [DOI] [PMC free article] [PubMed]
- 51.China NHCotPsRo. Protocol for Prevention and Control of COVID-19(Edition 4). http://www.nhc.gov.cn/xcs/zhengcwj/202002/573340613ab243b3a7f61df260551dd4/files/c791e5a7ea5149f680fdcb34dac0f54e.pdf. Accessed 6 Feb 2020. [DOI] [PMC free article] [PubMed]
- 52.Hu JX, He GH, Liu T, Xiao JP, Rong ZH, Guo LC, et al. Risk assessment of exported risk of COVID-19 from Hubei Province. Chin J Prev Med. 2020;54(4):362–366. doi: 10.3760/cma.j.cn112150-20200219-00142. [DOI] [PubMed] [Google Scholar]
- 53.Chen W, Wang Q, Li YQ, Yu HL, Xia YY, Zhang ML, et al. Early containment strategies and core measures for prevention and control of novel coronavirus pneumonia in China. Chin J Prev Med. 2020;54(3):239–244. doi: 10.3760/cma.j.issn.0253-9624.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 54.China NHCotPsRo. Notice on strengthening the prevention and control work of community of Novel Coronavirus Pneumonia. http://www.nhc.gov.cn/xcs/zhengcwj/202001/dd1e502534004a8d88b6a10f329a3369.shtml.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
According to the requirement of the NNDRS in China CDC, original data can be used only by our researchers and cannot be provided to others.