Abstract
Objective
The global COVID-19 pandemic has changed healthcare across the world. Efforts have concentrated on managing this crisis, with impact on cancer care unclear. We investigated the impact on endoscopy services and gastrointestinal (GI) cancer diagnosis in the UK.
Design
Analysis of endoscopy procedures and cancer diagnosis at a UK Major General Hospital. Procedure rates and diagnosis of GI malignancy were examined over 8-week periods in spring, summer and autumn 2019 before the start of the crisis and were compared with rates since onset of national lockdown and restrictions on elective endoscopy. The number of CT scans performed and malignancies diagnosed in the two corresponding periods in 2019 and 2020 were also evaluated.
Results
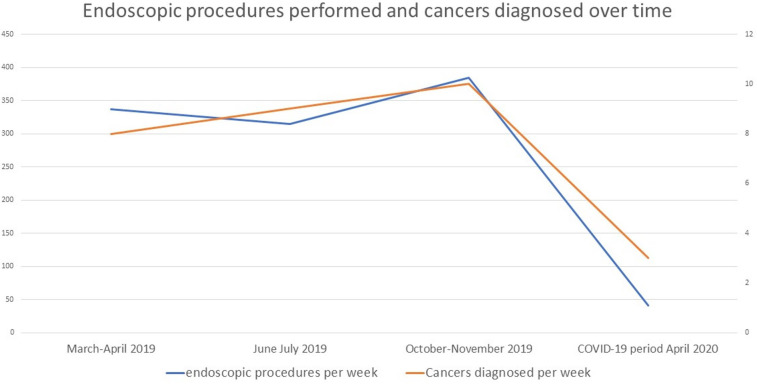
2 698 2516 and 3074 endoscopic procedures were performed in 2019, diagnosing 64, 73 and 78 cancers, respectively, the majority being in patients with alarm symptoms and fecal immunochemical test+ve bowel cancer screening population. Following initiation of new guidelines for management of endoscopy services 245 procedures were performed in a 6 week duration, diagnosing 18 cancers. This equates to potentially delayed diagnosis of 37 cancers per million population per month. Clinician triage improved, resulting in 13.6 procedures performed to diagnose one cancer.
Conclusions
Our data demonstrate an 88% reduction in procedures during the first 6 weeks of COVID-19 crisis, resulting in 66% fewer GI cancer diagnoses. Triage changes reduced the number of procedures required to diagnose cancer. Our data can help healthcare planning to manage the extra workload on endoscopy departments during the recovery period from COVID-19.
Keywords: colorectal cancer, endoscopic procedures, endoscopy, gastric cancer, oesophageal cancer
Key messages.
What is already known about this subject?
The global COVID-19 pandemic has resulted in the restructuring of healthcare services to facilitate treatment and to prevent health services from becoming overwhelmed. This has resulted in many services being restricted, including gastrointestinal (GI) endoscopy. GI malignancies are a major cause of cancer-related mortality. Much of this is treatable but is dependent on the stage of presentation. Endoscopy is essential for the diagnosis, and it is currently unclear what impact endoscopy restrictions are having on cancer diagnosis.
What are the new findings?
On an average, 38 endoscopic procedures are performed to diagnose one cancer. Most cancers are diagnosed in those with alarm symptoms.
Current measures have cut endoscopy capacity by 88%, resulting in 66% fewer GI cancers being diagnosed during the 6 weeks of COVID-19 crisis. However, physician-led triage of referrals improved as it only took 13.6 procedures to diagnose one cancer.
Key messages.
How might it impact on clinical practice in the foreseeable future?
If the current restrictions are sustained, there is a risk that cancers will be diagnosed late, resulting in a worse outlook for patients. The backlog of procedures could grow very rapidly, and the ability to catch up will be challenging if urgent measures are not taken to improve endoscopy capacity. An urgent uplift in endoscopy capacity and better triage will be required during the recovery phase to rapidly catch up with the work load and minimise the delay in cancer diagnosis.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was first reported from China in December 2019. Subsequently, the disease caused by SARS-Cov-2 was labelled as COVID-19 and WHO declared a global pandemic of COVID-19 on 11 March 2020.1 2 This has had significant impact on healthcare services around the world. Hospital services have been reconfigured to manage the crisis, and traditional targets for cancer diagnosis and treatment have been in the short term suspended to prevent services becoming overwhelmed by this new infection. Furthermore, there is evidence to suggest that patients are concerned about presenting for investigation of symptoms which could represent malignancy, for fear of catching a virus which could kill them. It is broadly acknowledged that SARS-CoV-2 is mainly spread via droplets and contacts. It is also known that airborne spread is possible during aerosol-generating procedures (AGPs).3 Endoscopy is considered as an AGP resulting in an increased risk of viral transmission. Like all the other national societies, the British Society of Gastroenterology (BSG) issued a guidance to reduce the risk of spread of SARS-CoV-19 viral transmission during endoscopy. This is important as it has been suggested that healthcare workers exposed to such procedures could be 4.66 times more likely to become infected compared with non-exposed healthcare workers,4 and it has been demonstrated that microbial contamination can occur up to 6 ft away during endoscopy.5 The key recommendation was to reduce any non-essential exposure to the COVID-19 virus and to take all reasonable measures to limit its spread; the BSG recommended3 that all endoscopy procedures except emergency and essential procedures should stop immediately.
The BSG and other national society guidance divided endoscopic activity into three categories: emergency procedures (should continue during the pandemic), elective procedures (defer until further notice) and procedures which should require case-by-case discussion about the timing of the procedure. This has resulted in dramatic reduction of endoscopy activity due to suspension of all elective procedures, including colon cancer screening.
The impact of these changes is currently unclear. In the UK, the national policy of social isolation appears to have prevented the National Health Service from becoming overwhelmed by COVID-19 cases, and complete shutdown of all elective procedures in hospitals has released the healthcare professionals to look after the COVID-19 patients.
However, this drastic reduction in elective healthcare activity will have a huge impact on the diagnosis and treatment of serious disease like cancers. Furthermore, it is unclear as to how long the pandemic and related restrictions are likely to continue, with some experts predicting some form of restrictions for over a year. With these uncertainties, the planning of health services, and in particular cancer pathways, is challenging. Increasingly the impact on cancer outcomes is being questioned in the media, with some sources suggesting almost 50 000 additional deaths due to cancer in the UK if this extends for 6 months.6
This study aimed to evaluate the impact of COVID-19 crisis on endoscopy services in general but more specifically on the endoscopic diagnosis of gastrointestinal (GI) malignancy.
Methods
This is a service evaluation exercise so it was exempted from UK ethics approval. As such, patients or the public were not involved in the design conduct or reporting of this. Endoscopy reporting software was interrogated with specific keywords to identify all procedures performed during specified periods. Data were downloaded from the hospital’s endoscopy reporting database (Hospital Information Clinical Support System (HICSS)) for histology-proven cases of oesophageal, gastric and colorectal cancers diagnosed over 8-week periods in spring 2019, summer 2019, autumn 2019 and the first 6 weeks of the recent COVID-19 crisis. The number and breakdown of procedures were recorded, along with the number of cancer diagnosis. The procedures were then classified by the indications of endoscopy. These indications broadly fell under three categories: colon cancer screening (fecal immunochemical test-positive colonoscopy and bowel scope flexible sigmoidoscopy), elective or symptomatic group, and urgent referrals for patients with alarm symptoms. The urgent group included ‘2-week wait’ cancer pathway referrals from primary care and urgent cancer wait target referrals from secondary care. It is worth noting that UK has a national pathway for referring patients with alarm symptoms (2-week pathway). This essentially comprises any patient with dysphagia or patients >55 years of age with any one of the symptoms of dyspepsia, reflux or abdominal pain who would qualify for an urgent 2-week referral for gastroscopy. Similarly, for lower gastrointestinal (LGI) cancer, this includes age-dependent symptoms like weight loss, abdominal pain, abdominal mass, rectal bleeding, change in bowel habit and iron deficiency anaemia.7
The restrictions related to COVID-19 were introduced in our department on 27 March. We have therefore looked at 6 weeks of activity from this date until 7 May 2020 during the COVID-19 crisis. After this date, clinical pathways in our unit changed substantially. During the crisis, endoscopy activity was restricted to only emergencies (GI bleed and cholangitis) and urgent cases with alarm symptoms considered to be highly suggestive of cancer. This was based on the guidance issued by BSG.3 Triage criterion involved consultant review of each referral. Patients only qualified for endoscopy if they had weight loss on top of an additional GI symptom or sign, that is, anaemia, dysphagia, diarrhoea or abdominal pain. Any symptom in isolation did not qualify for investigation. Statistical comparisons were calculated using a Pearson uncorrected χ2 test.
Results
Procedure numbers (excluding endoscopic retrograde cholangiopancreatography and endoscopic ultrasound) and cancer diagnosis during different time periods in 2019
In spring 2019, 2698 endoscopies were performed and diagnosed 64 GI cancers in 8 weeks. In summer 2019, 2516 endoscopies were performed and diagnosed 73 GI cancers in 8 weeks, whereas in autumn 2019, 3074 endoscopies were performed, diagnosing 78 GI cancers in 8 weeks. The breakdown of these are shown in table 1A, B and 2A–2C. This resulted in an average of 345 procedures and 9 cancer diagnoses per week. This equates to 38 endoscopic procedures/week to detect one GI cancer. There was a very close split between upper gastrointestinal (UGI) and LGI cancers. This equates to an average of 4.9 UGI cancers (Ca)/week and 4.1 LGI Ca/week, resulting in 31 procedures/week to detect 1 UGI cancer and 47 procedures/week to detect one LGI cancer.
Table 1A.
Procedure numbers during different seasons in 2019 prior to the pandemic
| Colon | Flexible sigmoidoscopy | Gastroscopy | ERCP | ||
| March–April 2019 | Urgent | 245 | 121 | 608 | 31 |
| Routine | 203 | 137 | 558 | 23 | |
| Screening | 116 | 673 | NA | NA | |
| June–July 2019 | Urgent | 361 | 116 | 650 | 45 |
| Routine | 199 | 105 | 535 | 27 | |
| Screening | 111 | 439 | NA | NA | |
| October–November 2019 | Urgent | 370 | 157 | 602 | 39 |
| Routine | 247 | 154 | 678 | 25 | |
| Screening | 166 | 700 | NA | NA | |
| Total | 2018 | 2602 | 3631 | 190 | |
| Average per week | 84 | 108 | 151 | 8 |
ERCP, endoscopic retrograde cholangiopancreatography; NA, not applicable.
Table 1B.
Average weekly activity and average weekly cancer detection
| Average weekly capacity | Average weekly cancer detected | ||
| Colonoscopy | Urgent | 40.7 | 1.8 |
| Routine | 27.0 | 0.42 | |
| Screening | 16.4 | 0.71 | |
| Flexible sigmoidoscopy | Urgent | 16.4 | 1 |
| Routine | 16.5 | 0.29 | |
| Screening | 75.5 | 0.08 | |
| Gastroscopy | Urgent | 77.5 | 3.75 |
| Routine | 73.8 | 1 |
Table 2A.
1 March–30 April 2019: procedure numbers and cancers stratified by indications
| Urgent | Routine elective | Colon cancer screening | Total | |
| Colonoscopy | 9/282 (3.2%) |
5/203 (2.5%) |
5/116 (4.3%) |
19/601 (3.2%) |
| P value | 0.636 | |||
| Flexible sigmoidoscopy | 6/121 (5.0%) |
4/137 (2.9%) |
0/673 (0%) |
8/931 (0.9%) |
| P value | 0.397 | |||
| Gastroscopy | 25/393 (6.4%) |
9/796 (1.1%) |
27/1166 (3.2%) |
|
| P value | 0.000 | |||
Table 2B.
1 June–30 July 2019: procedure numbers and cancers stratified by indications
| Urgent | Routine elective | Colon cancer screening | Total | |
| Colonoscopy | 15/361 (4.2%) |
2/199 (1.0%) |
09/111 (8.1%) |
26/671 (3.9%) |
| P value | 0.038 | |||
| Flexible sigmoidoscopy | 5/116 (4.3%) |
1/105 (0.95%) |
2/439 (0.46%) |
8/660 (1.2%) |
| P value | 0.125 | |||
| Gastroscopy | 35/650 (5.4%) |
4/535 (0.75%) |
39/1185 (3.3%) |
|
| P value | 0.000 | |||
Table 2C.
1 October–30 November 2019: procedure numbers and cancers stratified by indications
| Urgent | Routine elective | Colon cancer screening | Total | |
| Colonoscopy | 19/370 (5.1%) |
3/247 (1.2%) |
3/166 (1.8%) |
25/783 (3.2%) |
| P value | 0.050 | |||
| Flexible sigmoidoscopy | 13/157 (8.3%) |
2/154 (1.3%) |
0/700 (0%) |
12/1011 (0.12%) |
| P value | 0.004 | |||
| Gastroscopy | 30/602 (5.0%) |
11/678 (1.6%) |
41/1280 (3.2%) |
|
| P value | 0.001 | |||
Table 2D.
Total activity of 6 weeks during COVID-19 restriction (cancer/total procedures)
| Urgent | Planned | Colon cancer screening | Total | |
| Colonoscopy | 7/59 (11.9%) |
0/5 (0%) |
0/7 (0%) |
7/71 (9.9%) |
| Flexible sigmoidoscopy | 4/37 (10.8%) |
0/24 (0%) |
0/0 (0%) |
4/61 (6.6%) |
| UGI | 7/82 (8.5%) |
0/31 (0%) |
7/113 (6.2%) |
UGI, upper gastrointestinal.
The highest numbers of cancers were found in patients referred with alarm symptoms (UGI 3.75 Ca/week, LGI 2.8 Ca/week) and in those undergoing bowel cancer screening colonoscopy (LGI 0.7 Ca/week). Another way of expressing this result would be that 76.5% (3.75/4.9) of all UGI cancers were detected in patients undergoing gastroscopy for urgent indications due to alarm symptoms. Similarly, 73% (3.5/4.1) of all LGI cancers were detected in those with urgent indications (alarm symptoms) or bowel cancer screening. Routine and planned procedures had a very low cancer detection rate, along with bowel scope flexible sigmoidoscopy. This difference was statistically significant.
Procedure numbers and cancer diagnosis during the COVID-19 pandemic
Data were analysed following the initiation of social isolation measures and the new BSG guidelines for management of endoscopy services during the COVID-19 pandemic. The results are summarised in table 2D. In total, 245 procedures were performed in 6 weeks (41 procedures/week), resulting in the diagnosis of 18 cancers in 6 weeks (3 Ca/week). This equates to 13.6 procedures required to detect one cancer. This demonstrates an 88% reduction in the volume of endoscopy being performed, resulting in 66% reduction in the number of cancers being diagnosed on a weekly basis. However, the number of procedures performed to diagnose one cancer has significantly improved from 38.6 to 13.6. See table 2D and figure 1.
Figure 1.
Change in endoscopic procedure rate per week and cancers diagnosed with time.
Impact of this per million population
Our centre caters to 650 000 population. Based on our data, we can extrapolate an average of 531 endoscopies performed per 1 000 000 population per week in UK. This should result in diagnosis of 13.85 GI cancers per 1 000 000 population per week in UK. During the COVID-19 pandemic, we are currently performing 63 endoscopies per 1 000 000 population per week, diagnosing 4.62 cancers per 1 000 000 population per week. The population that our centre caters to is almost 1% of UK population, and if we accept that endoscopic activity in our unit is reflective of national practice in the UK, then the number of procedures being deferred due to COVID-19 restrictions and the number of cancer diagnosis being delayed can be extrapolated from our data. The actual numbers will be dependent on the duration and severity of restrictions. Table 3 gives an estimate based on the current level of restrictions lasting for different durations.
Table 3.
Effect of a prolonged restriction on endoscopy services on the UK population
| Length of restrictions | 1 month | 3 months | 6 months | 1 year |
| Undiagnosed cancers (UK population) | 2400 | 7200 | 14 400 | 28 800 |
| Undiagnosed cancers per million population | 37 | 111 | 222 | 443 |
| Procedural backlog (UK population) | 121 700 | 365 100 | 730 200 | 1 460 400 |
| Procedural backlog per million population | 1872 | 5616 | 11 233 | 22 468 |
CT during the COVID-19 pandemic
We examined the number of CT scans performed between 27 March and 7 May 2019 and compared this with those performed during the COVID-19 pandemic. In March–May 2019, a total of 5938 CT scans were performed, diagnosing 81 new cancers (excluding the staging scans for diagnosed cancers). This included 10 UGI cancers and 25 colorectal cancers with the remainder representing pancreatic cancer, lymphomas, and hepatobiliary and small bowel malignancies. This equates to an average of 990 scans per week and 13.5 cancers diagnosed per week (1.7 UGI and 4.2 LGI per week). In total, 73 CT scans were required to diagnose one cancer. During the 27 March–7 May 2020 COVID-19 pandemic, 3690 CT scans were performed, diagnosing 55 cancers. This included seven UGI cancers and 24 colorectal cancers. This equates to an average of 615 scans per week and 9.2 cancers diagnosed per week (1.2 UGI and 4 LGI per week). In total, 67 CT scans were required to diagnose one cancer. There was no statistically significant difference in the number of GI cancers diagnosed by imaging. There was a small improvement in the number needed to diagnose one cancer.
Discussion
While it was undeniable that the COVID-19 world pandemic would have an impact on cancer care, our results demonstrate the potential scale of the impact on cancer care, as well as overall activity of endoscopy departments. The longer the restrictions last, the bigger will be the impact.
Our data demonstrate that, despite our best efforts, endoscopic activity went down by 88% and cancer detection rate fell by 66% during the COVID-19 pandemic. With capacity cut by 88%, it is unsurprising that we are currently diagnosing less than 33% of the previous GI cancer burden. It demonstrates that while every effort is being taken to be selective in optimising our caseload, clinicians cannot triage cases to the degree of accuracy necessary to pick anywhere near all of the previously diagnosed cases based on current capacity, and even in this current situation, the cancer detection rate at endoscopy is only 7%. This reflects a fundamental problem with GI pathology; symptoms are not a reliable guide to pathology, and often the only way to exclude malignancy is with an objective test.
An important question relates to what impact a delayed diagnosis has on clinical outcome, and the picture is not certain. There has been some evidence to suggest that a limited healthcare-related delay in diagnosis of colorectal cancer does not impact on outcome.8 This was a retrospective study and concentrated on stage IV disease. It was not designed to investigate the impact of changes in stage of less advanced disease. However, a recent study calculated the impact of a hypothetical suspension of elective colonoscopy for 6 months and predicted a delayed diagnosis of over 2800 colorectal cancers and 22 000 high-grade adenomatous polyps with malignant potential.9 The 6-month mortality rate for those eventually diagnosed with colorectal cancer would increase by 6.5%.10
Previous data from the UK have shown that the OR of death at 12 months rapidly increases with increasing stage of colorectal cancer. The OR for death at 12 months for Duke’s A was reported at 1, Duke’s B as 1.46, Duke’s C as 3.92 and for stage with distant metastasis at 14.6.11 The suspension of endoscopic activity due to the COVID-19 pandemic is certainly going to delay the diagnosis of these cancers, potentially resulting in a possible progression of the stage of cancer with potential worsening of outcome. There are growing data to suggest that delays in diagnosis are associated with a more advanced stage of presentation,12 and it is well established that prognosis is stage dependent. Indeed, it is an underpinning principle of bowel cancer screening programmes that early diagnosis results in a better outcome. For oesophageal cancer, it has been suggested that a delay results in worse short-term outcomes.13 It is believed that doubling times are shorter for oesophageal cancer compared with colorectal cancer, so delays may be more significant in this group.
Our data also demonstrate an 88% reduction in endoscopy volume, and this will affect not only cancer care but also a lot of other conditions like variceal haemorrhage due to disruption of variceal banding cycles, as well as delay in diagnosis of new patients with varices. Data from USA has shown that delay in detection and treatment of varices could potentially lead to almost 1500 patients suffering from a terminal variceal bleed that may have been otherwise prevented by endoscopic surveillance.14 15 There are of course other strategies to managing varices, and it may be that a medical approach could be substituted as an alternative strategy. Such approaches, where safe, should be adopted. Oesophageal varices are just an example of a range of benign conditions which are diagnosed and managed by endoscopy. The pandemic-related suspension of endoscopy services will have an impact on the management of all such conditions.
The current restrictions have just gone past 6 weeks, and extrapolation from our data suggests that nationally in the UK, we would have deferred an average of 121 700 gastroscopy and colonoscopy procedures. This equates to 1872 endoscopy procedures per million population. It is important to bear in mind the possibility that not all units might have followed the same approach as us and there may be variations across the UK. However, it is probable that all UK endoscopy units based their approach on the BSG guidelines, so variations in practice, if any, will be minor, and these findings reflect the anxiety that have been raised publicly by cancer specialists.6 An analysis of the National Endoscopy Database would be one way to examine this and a good area for future research.
A valid question would also be how many cancers were diagnosed through other routes, for example, CT imaging. We analysed imaging during both the COVID-19 period and 1 year previously and did not identify any evidence of shift in pathway from endoscopy to CT scanning with no increase in the number of CT scans performed during the pandemic. The total number of CT scans performed went down, suggesting an improvement in referrals, but this was modest. We therefore believe that a proportion of GI cancers still remain undiagnosed due to suspension of endoscopy services during the COVID-19 crisis.
We will have to find new ways to catch up with this lost work. One of the ways to cope with this extra work load would be to increase the capacity of endoscopy departments. However, most units in the UK operate at 90% capacity, and the loss of 10% is mainly due to sickness and holidays, so it is not easy to expand capacity during normal working hours. However, the physical capacity of endoscopy departments in the evenings and weekends can be used if additional work force becomes available. The other ways would be to improve our endoscopy pathways by fast-tracking high-risk patients and finding alternative tests for low-risk patients. Our data demonstrate that our triage system during the pandemic was significantly better for detection of cancers as we were only performing 13.6 procedures to find one cancer as compared with prepandemic figures when almost 39 procedures were being performed to detect one GI cancer. We can learn from this experience and improve our endoscopy pathway
It may be possible to improve triage further through a combination of symptoms to triage risk. Furthermore, new national guidelines in the UK have cut down the requirements for endoscopic follow-up, and it is our contention that we will need to rethink our current approach to endoscopy if we are to ensure that cancers are diagnosed within the constraints that are likely to be in place in the near future. Our prepandemic data show that significantly more cancers are found in patients presenting with alarm symptoms (detailed in the Methods section) and those undergoing screening colonoscopy as compared with elective endoscopy and screening sigmoidoscopy. Going forward in the postpandemic era, this information should help us better triage/prioritise endoscopy services for patients at higher risk. It is also important to understand that in the postpandemic era, endoscopy practice will not return back to normal as we will have to take additional measures with screening of patients, personal protective equipment and even redesigning of units to maintain appropriate social distancing and patient flow.
We feel that it is vital that endoscopy capacity is addressed as a matter of urgency. Our data demonstrate the amount of work that has been deferred and the impact that this will have on cancer diagnosis and treatment. However, endoscopy procedures are not performed for just cancer diagnosis but are essential in the management of a lot of serious but benign conditions, and the impact of this building backlog of endoscopy procedures in a system that normally operates at full capacity will be enormous. It is our contention that harm can be largely mitigated in the short term, but this situation could very rapidly grow into a problem which becomes impossible to manage unless urgent measures are implemented to cope with this extra workload. This calls for all national societies to join hands and develop consensus about the appropriate use of endoscopy resources and to develop some new pathways for diagnosis and management of common GI conditions.
Footnotes
Contributors: (1) Substantial contributions to the conception or design of the work and the acquisition, analysis, and interpretation of data in the work; (2) drafting the work for important intellectual content; (3) final approval of the version to be published; (4) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. Data available from point of publication upon reasonable request via email.
References
- 1. WHO . Coronavirus disease (COVID-2019) situation report 84. Geneva, Switzerland: WHO, 2020. [Google Scholar]
- 2. WHO . Coronavirus disease (COVID-2019) situation report 51. Geneva, Switzerland: WHO, 2020. [Google Scholar]
- 3. Endoscopy activity and COVID-19: Bsg and JAG guidance. Available: https://www.bsg.org.uk/covid-19-advice/endoscopy-activity-and-covid-19-bsg-and-jag-guidance/ [Accessed 24 Apr 2020].
- 4. Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One 2012;7:e35797. 10.1371/journal.pone.0035797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Johnston ER, Habib-Bein N, Dueker JM, et al. Risk of bacterial exposure to the endoscopist's face during endoscopy. Gastrointest Endosc 2019;89:818–24. 10.1016/j.gie.2018.10.034 [DOI] [PubMed] [Google Scholar]
- 6. If this goes on for six months, 50,000 more people could die of cancer, writes consultant oncologist KAROL SIKORA. Available: https://www.dailymail.co.uk/debate/article-8247141/If-goes-six-months-50-000-people-die-cancer.html [Accessed 24 Apr 2020].
- 7. NICE (2015)Suspected cancer: recognition and referral (NG12) . National Institute for health and care excellence. Available: www.nice.org.uk%5BFreeFull-text%5D [PubMed]
- 8. Fernández-de Castro JD, Baiocchi Ureta F, Fernández González R, et al. The effect of diagnostic delay attributable to the healthcare system on the prognosis of colorectal cancer. Gastroenterol Hepatol 2019;42:527–33. 10.1016/j.gastrohep.2019.03.012 [DOI] [PubMed] [Google Scholar]
- 9. Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology 2019;156:254–72. 10.1053/j.gastro.2018.08.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pita-Fernández S, González-Sáez L, López-Calviño B, et al. Effect of diagnostic delay on survival in patients with colorectal cancer: a retrospective cohort study. BMC Cancer 2016;16:664. 10.1186/s12885-016-2717-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Downing A, Aravani A, Macleod U, et al. Early mortality from colorectal cancer in England: a retrospective observational study of the factors associated with death in the first year after diagnosis. Br J Cancer 2013;108:681–5. 10.1038/bjc.2012.585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tørring ML, Murchie P, Hamilton W, et al. Evidence of advanced stage colorectal cancer with longer diagnostic intervals: a pooled analysis of seven primary care cohorts comprising 11 720 patients in five countries. Br J Cancer 2017;117:888–97. 10.1038/bjc.2017.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grotenhuis BA, van Hagen P, Wijnhoven BPL, et al. Delay in diagnostic workup and treatment of esophageal cancer. J Gastrointest Surg 2010;14:476–83. 10.1007/s11605-009-1109-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lay CS, Tsai YT, Teg CY, et al. Endoscopic variceal ligation in prophylaxis of first variceal bleeding in cirrhotic patients with high-risk esophageal varices. Hepatology 1997;25:1346–50. 10.1002/hep.510250608 [DOI] [PubMed] [Google Scholar]
- 15. North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices . Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med 1988;319:983–9. 10.1056/NEJM198810133191505 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. Data available from point of publication upon reasonable request via email.