Abstract
The 2020 SARS-CoV-2 pandemic posed significant challenges to the health service. Many services cancelled all routine appointments and surgery, which allowed them to redirect care towards large numbers of infected patients requiring respiratory and other support. Maternity services are relatively unique in that most of the care is time sensitive and cannot be rescheduled. Assessment such as routine bloods need to be taken in early pregnancy, anatomic surveys are best conducted at 20–22 weeks' gestation, and births continue regardless of a pandemic. In this paper we describe how National Maternity Hospital Dublin, with an annual delivery rate of 8000 births, reorganised services to continue to care for our mothers and babies. This included the development of a ‘hospital within a hospital’ approach, and separate physical and care pathways for positive cases. The delivery of virtual outpatient appointments and a comprehensive online patient education portal have proved successful.
Keywords: Covid 19, Obstetrics, Gynecology, Pregnancy services, Reconfiguration
Introduction
The first SARS-CoV-2 positive case in Ireland was recorded on 29th February 2020. Since then, like other maternity services, rapid transformation and adaptation of healthcare services has been necessary to respond to this pandemic [1,2]. Cognisant of the scenes of overwhelmed health services being reported around the world and, in particular, in Italy, the National Maternity Hospital (NMH) management commenced a proactive operational programme in early February 2020, to protect patients and staff. Here, we describe the NMH journey and, in particular, the reorganisation of our services to allow us to continue to provide safe care to our women and babies.
Background
The NMH is a standalone tertiary referral perinatal centre and university teaching hospital for both obstetrics and gynaecology, delivering more than 8000 babies annually. It is the leading hospital for women's health in the Ireland East Hospital Group. It was established in 1894 and today all its clinical activity occurs in the original building. The infrastructural inadequacies and challenges of such a building, which have been well recognised, became even more obvious with the C19 pandemic. These challenges are similar to those experienced in younger co-located maternity hospitals and the solutions that worked for us have relevance and learning for other maternity services.
In 2019, the caesarean section rate was 30.3% with 31% of women undergoing induction of labour. The antenatal outpatient department saw 31,384 attendances, with the community midwifery team caring for a further 14,768 women through community clinics, satellite hospital clinics and antenatal and postnatal home visits throughout both counties Dublin and Wicklow. The fetal medicine unit performed 35,745 pregnancy ultrasound scans.
A total of 1579 babies were admitted to the Neonatal Unit, with 116 less than 1500 g and/or 29 week's gestation.
A total of 3443 babies attended the neonatal outpatient service. The neonatology department is an
Active participant in the National Neonatal Transport Programme (NNTP) along with the.
Other two Dublin maternity hospitals
The Department of Gynaecology had 15,662 outpatient attendances and 2459 gynaecological surgical procedures were performed in theatre. The operating theatres are shared with obstetrics, where lists are often disrupted by emergency caesarean sections. Gynaecological cancer surgery is performed in a nearby large general hospital.
The NMH uses an Electronic Health Record (EHR) for all patients.
As the core business of maternity care and baby deliveries is time sensitive and continues regardless of the COVID-19 pandemic, it was therefore critical that the planning of service provision commenced at an early stage. The NMH executive management team embraced this and proactively set about protecting both patients and staff prior to the first case being recorded in Ireland. The core features of this programme involved:
Governance.
Patient Services.
Patient Flows.
Infrastructural Adaptations.
Hygiene services.
Visitor policies.
Thus, the NMH has continued the delivery of safe services to patients and staff throughout this ongoing pandemic.
Governance
The existing organisational structure and governance of the NMH continues with the Master (Consultant Obstetrician/Gynaecologist and CEO), Director of Midwifery, Secretary Manager and Clinical Director (Consultant Anaesthetist) forming the Executive Management Team (EMT).
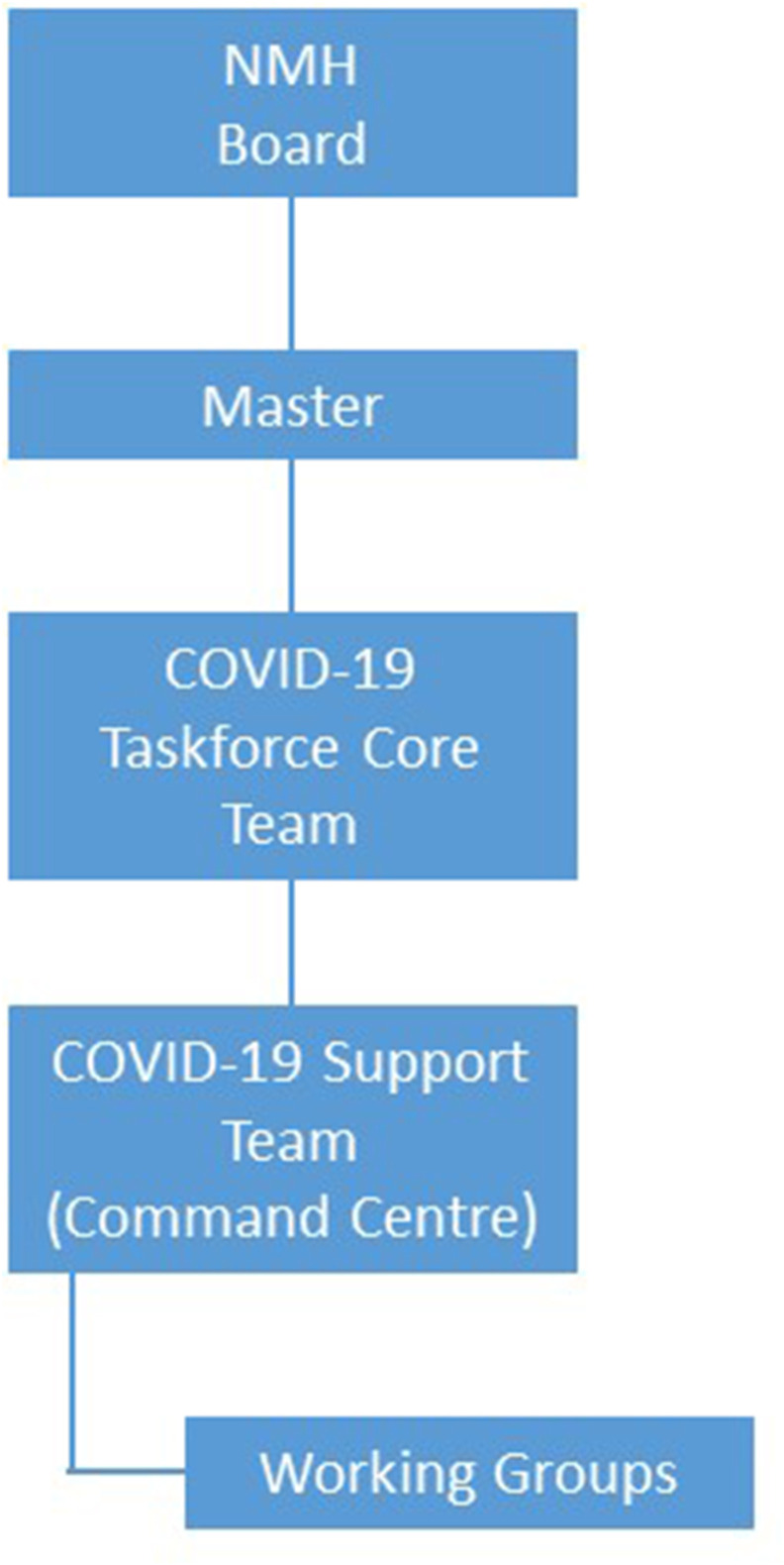
A COVID-19 Taskforce Core Group (CTCG) was set up. This is a multidisciplinary group who have overall responsibility for key decisions related to COVID-19 within the NMH. It is supported by various working groups from all areas with each having specific roles, as outlined in Table 1 .
Table 1.
Groups and roles.
| Group | Chair | Role |
|---|---|---|
| COVID-19 Taskforce Core | Master of the NMH | Overall responsibility for key decisions relating to COVID-19 within the NMH. COVID-19 taskforce provided weekly briefs to the NMH board. |
| COVID-19 Support (Control Centre) | Secretary Manager | Provided daily administrative support to the Taskforce as required and aided in coordinating on all aspects of COVID-19. |
| Infection Control | NMH Consultant Microbiologist | Overall responsibility on all aspects relating to COVID-19 infection control within the NMH |
| Occupational Health | NMH Director of Midwifery and Nursing | Overall responsibility for the management of all aspects of staff related COVID-19 issues. Included: staff testing, follow up of positive COVID-19 staff and contact tracing within the NMH. |
| Patient Helpline | Clinical Practice Development Coordinator/Assistant Director of Midwifery (ADOM) | Responsible for providing information to NMH patients related to COVID-19. |
| Rostering | Compliance Manager of the NMH | Responsible for establishing and maintaining a database of staff rosters (midwifery, medical, administration and allied health), redeployment lists, list of staff required on health grounds to remain at home and staff working from home. Each staff group had a Lead Representative/ Coordinator. |
| Accommodation | Chaired by members of the COVID-19 support team | Responsible for arranging temporary accommodation for NMH staff, if required. Temporary accommodation under remit of national Health Service Executive. |
| Facilities | NMH Facilities Manager | Responsible for coordinating all necessary engineering activities in relation to infrastructural alterations for COVID-19 requirements and the NMH building. |
| Communications Subcommittee | NMH Director of Midwifery and Nursing | The role of the COVID-19 Communications Subcommittee group was to oversee, advise and co-ordinate all communications in relation to COVID-19 to patients and staff. Communications required approval process through the NMH COVID-19 Taskforce and sign off by EMT. |
| NMH Digital Learning | Consultant Obstetrician/ Gynaecologist | The role of this group was to provide patients with information on pregnancy, labour, post-delivery and COVID-19. The information was delivered online through the NMH website/ ‘virtual classroom’. The multidisciplinary team developed a series of education modules for patients. |
| Procurement | NMH Secretary Manager | Responsible for ordering and maintaining stock requirements in relation to COVID-19 within the NMH. |
| Recruitment/ HR | NMH Secretary Manager | This group was responsible for the recruitment functions required for additional staff during this pandemic within the NMH. They were responsible for identifying staff required on health grounds to remain at home and redeployment. |
| Hygiene Services | Hygiene Manager | This group was responsible for all hygiene requirements for COVID-19 in the NMH. |
From early March 2020 daily CTCG meetings were convened, seven days a week, with the working groups informing as appropriate. The CTCG also engaged in daily teleconferences with the Ireland East Health Group where local and national information and guidance was shared [[3], [4], ∗[5], ∗[6]]. International experience and guidance were closely followed and embraced as was pertinent to our needs [∗[7], ∗[8], ∗[9], ∗[10], ∗[11]]. Thus, informed decisions were made as to appropriate reorganisation of our services to protect all involved and allowed for flexibility within the management structure to accommodate the changing landscape as SARS-CoV-2 positive cases increased. (See Fig. 1 )
Fig. 1.
The reporting structure of the COVID-19 taskforce and its constituent groups.
Weekly staff information sessions were convened using various platforms. This ensured all groups understood what was happening and its rationale. They provided an opportunity for staff engagement and questions. The feedback received was that staff felt supported and informed in what was a challenging and very uncertain time for all.
Patient services
All patient services were reviewed and altered in accordance with national and international guidance. The following changes were made:
Elective Gynaecology and colposcopy outpatients and elective gynaecology surgery were cancelled from March 13th to June 30th, 2020.
Maternity outpatient clinics were prioritised, with patients telephoned prior to their planned appointment. Visits were reduced to essential, face to face, timed visits. Clinician discretion was maintained. Early pregnancy assessment and histories were conducted by telephone and face to face antenatal visits were reduced to three times in pregnancy (20 weeks, 28 weeks, and 36 weeks) with virtual consultations in between.
Changes were made to clinical care as appropriate, for example, the diabetes service moved to using HbA1c and fasting glucose for diagnosis of gestational diabetes, as did many units in the UK [12]. Gestational Diabetes Virtual Care was introduced; this was a smart phone application platform into which patients entered blood sugar values, supported by weekly telephone contact from the diabetes midwifery service. This transformed the multidisciplinary delivery of this service from frequent hospital attendances to care primarily in the woman's own home [13].
Pregnancy ultrasound scans continued for essential scans. The scanning time was restricted to 15 min. If further time was required, a second appointment was arranged.
Neonatal clinic appointments were reduced to essential visits only.
Allied health services. Non-essential face to face consultations were cancelled. Virtual or telephone consultations were provided where possible.
Community midwifery services were increased with more ‘early transfer home’ visits facilitated within 24 h of birth. The home birth service continued and the community midwives performed many of the postnatal visits by telephone.
Scheduled individual and group education services were replaced by virtual sessions. A new digital education platform was developed within 1 month of national lockdown where all components of antenatal, intrapartum and postnatal education were delivered through our hospital website patient portal.
COVID-19 testing facilities for patients and staff were provided on site and in house, including a ‘drive thru’ facility.
A pre-assessment clinic for elective admissions was commenced and included screening for COVID-19.
Visiting policies were adapted and reviewed as required by local and national circumstances.
The reorganisation of the services as outlined above, allowed the NMH to continue to provide essential, safe services to patients. The postponement of gynaecological clinics and elective gynaecological surgery facilitated the use of staff and space to create a ‘hospital within a hospital’. This allowed the patients to be cohorted, with the suspected or confirmed COVID-19 positive patients managed separately to all others, while ensuring the full range of clinical and other supports were available to these and to all our patients.
Patient flows
Two clear patient flow pathways were developed:
Non-SARS-CoV-2 positive patients.
Suspected or confirmed SARS-CoV-2 positive patients.
Each group was cohorted and had clearly identified physical entry and exit points, and routes and accommodation within the hospital.
The non-SARS-CoV-2 patient flows facilitated ongoing care with essential face to face or virtual appointments continuing, as necessary. All patients were contacted by phone in advance of their appointment and prioritised for attendance and/or advice.
The suspected or confirmed SARS-CoV-2 positive patient flows allowed these patients to be cared for in the appropriate environment with staff protected with personal protective equipment (PPE). The suspected or confirmed SARS-CoV-2 patients were requested to inform the NMH in advance of their attendance. The environment of a ‘hospital within a hospital’ was created. This will be explained further in the ‘Infrastructural Adaptations’ section below.
All staff were educated in these flows and the appropriate procedures necessary, e.g. PPE use and its specific requirements for different situations.
Infrastructural adaptations
The NMH building is 130 years old and has been modernised internally in many areas. Nonetheless, its basic structure makes any infrastructural adaptations complicated, which is a challenge common to many maternity units. This posed several challenges in the presence of a pandemic where social distancing and isolation facilities are an integral part of patient care and staff management. Several areas required urgent adaptation to facilitate keeping patients and staff safe during this time.
As stated above, the reduction in some clinical services freed up space to allow our onsite facilities department make alterations as required. The CTCG identified and prioritised several key clinical and non-clinical areas for adaptation. The key clinical areas adapted are outlined in Table 2 . This created the ‘hospital within a hospital’.
Table 2.
Infrastructural adaptations made to key clinical areas.
| Location |
|
|---|---|
| ‘Hospital within a Hospital’ Iveagh Ward (Gynaecology Ward) Theatre/ HDU |
|
| Fitzwilliam Wing (Postnatal Ward) |
|
| Delivery Ward |
|
| Emergency Room (ER) |
|
In summary, the main adaptations were the provision of:
-
•
negative pressure ventilation single rooms
-
•
dedicated donning and doffing areas
-
•
designated storage facilities
-
•
clear signage for entry, exit and PPE requirements.
New patient flows were developed in these areas. Staff were allocated specific patient cohorts to reduce the possibility of close contact exposure.
Other clinical areas in the hospital needed less work. For example, the Neonatal Unit had been more recently redeveloped and already included an isolation wing and single rooms with heating, ventilation, and air conditioning (HVAC). One area of the Special Care Baby Unit (SCBU) had negative pressure ventilation installed.
The Antenatal Outpatient department remains one of the original areas of our old building. It was not possible to adapt this area in such a short timeframe. Hence, the focus here was on care pathways to ensure maximum adherence to social distancing and limitation of footfall with reduced clinic attendances and timed appointments.
Patient check-in and waiting areas were assessed. Clear signage, screens and reduction of seating capacity was prioritised. An additional modular building was erected in the car park as a waiting area. The focus was also on timed appointments to limit exposure risk.
Office areas were reviewed to maintain social distancing and reduce occupancy. Screens, signage, and reduced seating were facilitated. New work practices, including split shifts, extended day working and working from home, were introduced.
Further attention was given to ‘front desk’ management of patient entrance and egress.
Clear signage was erected throughout the hospital for both patients and staff. These were both directional and informative regarding mask wearing, social distancing, hand hygiene and cough etiquette.
Additional hand washing stations and alcohol gel dispensers were installed throughout the hospital. Extra storage space for PPE was provided in all departments. An additional testing platform was acquired and fitted in the laboratory
The Staff Canteen capacity was reduced and additional staff eating areas provided in vacated areas.
An area of the car park was adapted to provide a ‘drive thru’ SARS-CoV-2 swabbing facility for both patients and staff.
Hygiene Services
Hygiene service provision was expanded to enhance a clean, safe hospital environment. Additional resources were allocated. A COVID-19 theatre/COVID-19 Response cleaning team was established with staff given extra training in the cleaning requirements for high-risk areas. Standard operating procedures were adopted and Infection Prevention and Control training introduced across all areas. Waste management policies and procedures were reviewed and modified as necessary to meet demands and apply best practice.
Visiting policies
In accordance with national guidance our visiting policy required alteration. The attendance of partners/accompanying persons was reviewed.
It was necessary to restrict attending partners to labour and delivery only, including caesarean section.
During the first lockdown (March to June 2020) no partners were permitted to attend for clinic visits or pregnancy ultrasound unless there were special or compassionate circumstances or for counselling and support for women experiencing pregnancy complications.
Partners were not permitted in the antenatal ward as the majority of antenatal women are accommodated in shared wards with very limited availability of single rooms.
Over time, as SARS-CoV-2 positive cases decreased, partners were allowed to visit for 2 h daily in the postnatal period and thereafter permitted to attend routine second trimester anatomy ultrasound scans.
Initially no partners were permitted in the neonatal unit. ‘CommunNICU’ was introduced to allow parents to keep in touch with their baby's progress using Angel Eye (a camera that keeps parents connected with their newborn in the NICU) along with video calls and recordings. Baby journals were introduced to record the infant's progress. As the number of cases decreased parents were allowed to visit freely according to the Neonatal Unit practice.
These policies are under regular review and visiting capacity will increase as soon as it is safe to do so from a public health perspective.
We are very grateful to our women and their families who have stoically accepted the need for such restrictions with little objection.
Other considerations
The COVID-19 pandemic has been difficult for everyone. We have endeavoured to protect our patients and staff as much as possible. While needing to reorganise many of our services, we have striven to continue to provide excellence in care and compassion.
We have not changed our labour or breastfeeding management. Our home birth service continues.
We have been fortunate that we have had relatively few cases of COVID-19 amongst our women, and to date, all have recovered well [2]. The pregnant women in our care have been proactive in caring for themselves and by adhering to public health guidelines.
Following the first lockdown, in July 2020 we have reintroduced all gynaecology services. This was possible with the introduction of new work practices such as extended clinic days and the incorporation of virtual and telephone consultations. The entire backlog of deferred clinic appointments and surgical procedures has been cleared.
Organisational positives
The COVID-19 crisis has brought many positive features of the NMH to the fore. The most evident of these is the hospital's teamworking culture. All departments rowed in to help our patients and one another. The EMT led the strategy and its management.
Several work practices have been embraced such as establishing efficient timed outpatient appointments which is working well. The Gestational Diabetes Virtual Care service will continue. Working from home has been facilitated where possible.
A new Digital patient education programme has been introduced and has been very well received.
Communication with patients and staff is regular and is frequently updated using various platforms, hospital website, staff intranet, newsletters, memos, and social media.
In our experience, this health crisis has strengthened our focus and drive to continue to do our best for the women and families who attend us, and for the staff who care for them.
Practice points.
Over a short period of time the following adaptations to our obstetric services allowed us to continue to care safely for 8000 mothers and their babies:
-
1.
Development of a ‘hospital within a hospital’
-
2.
Separate physical and care pathways for suspected and positive cases of SARS-CoV-2
-
3.
Development of robust virtual care pathways for antenatal care.
-
4.
Development of a virtual patient education platform.
Research agenda lessons learned for future pandemics?
Analysis of impact of infrastructural changes and virtual care pathways on clinical outcomes for mother and baby.
Consideration of future pandemics in the development of our maternity services.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of competing interest
The authors have no conflict of interest to declare.
Acknowledgements
The women who attend and the staff of the National Maternity Hospital, Dublin.
References
- Ryan G.A., Purandare N.C., McAuliffe F.M., Hod M., Purandare C.N. Clinical update on COVID-19 in pregnancy: a review article. J Obstet Gynaecol Res. 2020;46(8):1235–1245. doi: 10.1111/jog.14321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanella F., Hannes S., Keating N., Martyn F., Browne I., Briet J., et al. COVID-19 infection during the third trimester of pregnancy: current clinical dilemmas. Eur J Obstet Gynecol Reprod Biol. 2020;251:268–271. doi: 10.1016/j.ejogrb.2020.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.HSE. COVID-19 operations reports and policies Dublin, Ireland. Health Service Executive; 2020. https://www.hse.ie/eng/services/news/newsfeatures/covid19-updates/covid19-updates.html Available from: [Google Scholar]
- 4.HPSC. New and updated guidance Dublin, Ireland. Health Protection Surveillance Centre; 2020. https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/guidance/newupdatedguidance/ Available from: [Google Scholar]
- HPSC. Guidance for healthcare workers Dublin, Ireland. Health Protection Surveillance Centre; 2020. https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/guidance/guidanceforhealthcareworkers/ Available from: [Google Scholar]
- RCPI. Clinical . Royal College of Physicians of Ireland; 2020. Guidance for doctors Dublin, Ireland.https://www.rcpi.ie/covid19/clinical-guidance-for-doctors/ Available from: [Google Scholar]
- Ross-Davie M., Lambert J., Brigante L., Livingstone C., Crowe S., Pandya P., et al. Royal College of Obstetricians and Gynecologists; 2020. Guidance for antenatal and postnatal services in the evolving coronavirus (COVID-19) pandemic. 10/07/2020. [Google Scholar]
- WHO. Country & technical guidance - coronavirus disease (COVID-19) World Health Organization; 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications [Available from: [Google Scholar]
- ECDC . European Centre for Disease Prevention and Control; Stockholm: 2020. Infection prevention and control and preparedness for COVID-19 in healthcare settings – fifth update. 6th October 2020. [Google Scholar]
- ECDC . European Centre for Disease Prevention and Control; Stockholm: 2020. Use of gloves in healthcare and non-healthcare settings in the context of the COVID-19 pandemic. [Google Scholar]
- Knight M., Bunch K., Cairns A., Cantwell R., Cox P., Kenyon S., et al. University of Oxford; Oxford MBRRACE-UK: 2020. Saving lives, improving mothers' care rapid report: learning from SARS-CoV-2-related and associated maternal deaths in the UK. March - May 2020. [Google Scholar]
- Thangaratinam S., Cooray S., Sukumar N., Huda M., Devlieger R., Benhalima K., et al. Endocrinology IN the time OF COVID-19: diagnosis and management of gestational diabetes mellitus. Eur J Endocrinol. 2020;183(2):G49–G56. doi: 10.1530/EJE-20-0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coveney C., Rooney H., Byrne S., Rutter E. 2020. Gestational diabetes vritual care. [Google Scholar]