Abstract
Background:
Preservation of the tibial stump during anterior cruciate ligament reconstruction (ACLR) is controversial. While proposed benefits include enhanced graft revascularization, improved proprioception, and decreased graft rupture rates, a potential complication is the development of a symptomatic cyclops lesion. It is therefore important to determine whether any benefits outweigh potential complications.
Purpose:
To determine whether greater preservation of the tibial stump remnant would be associated with a decreased graft rupture rate without a concomitant increase in the rate of surgery for symptomatic cyclops lesions at 2 years after ACLR.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A cohort of 658 patients in whom the amount of tibial stump preserved was classified as no stump (n = 228), <50% (n = 342), or >50% (n = 88) was followed up for 2 years, with graft ruptures and surgical treatment for cyclops lesions recorded. Contingency and Kaplan-Meier survival analyses were used to determine trends among the 3 remnant preservation groups in terms of graft rupture rates and surgery for cyclops lesions. Subgroup analysis was also conducted to examine sex-based differences.
Results:
There was no significant association between graft rupture rates and remnant preservation. There was a significant trend for fewer operations for symptomatic cyclops lesions with greater remnant preservation when the entire cohort was analyzed (P = .04) and also when only female patients were analyzed (P = .04).
Conclusion:
Although preservation of the tibial stump remnant was not associated with a reduced graft rupture rate, it was also not associated with increased rates of surgery for symptomatic cyclops lesions.
Keywords: ACL injury, remnant preservation, stump retention, reinjury, graft failure, cyclops lesion
Anterior cruciate ligament (ACL) reconstruction (ACLR) is a commonly performed surgical procedure to restore knee stability and allow a return to sporting activities after ACL injury. Despite good to excellent clinical outcomes, graft failure is still an issue, and there are many causes for failure.2,26–28 Histologic studies have confirmed the presence of a vascular network and viable mechanoreceptors within the ACL remnants, and preservation of this may promote cell proliferation and the recovery of proprioceptive function, as well as revascularization of the graft and its synovial coverage after surgery.11,18 Preservation of the ACL remnant has therefore remained a topic of interest.
While some studies have shown superior knee stability and clinical outcomes with remnant preservation,3,9,10 results have been mixed, with other studies showing no additional benefit.15 Initial systematic reviews concluded that there was little evidence to support the routine practice of remnant preservation.8,13,17,19 The most recent reviews have not really changed this conclusion.21,24 Although some studies have shown lower rates of graft ruptures or revision surgeries,7,12,16,20 these have not been statistically significant findings mostly because of the small patient numbers in the studies. Follow-up length has also been insufficient in providing meaningful graft rupture data, and most of the studies have focused primarily on clinical outcomes.
One of the risks of ACLR is the development of a cyclops lesion, which has a reported incidence ranging from 2% to 47%.10 These lesions are characterized by the development of fibrovascular tissue anterior to the ACL graft.4,6 The majority of these lesions are asymptomatic, but some do result in a symptomatic loss of full extension due to the impingement of the cyclops lesion in the intercondylar notch.14,22,25 Although preservation of ACL remnants might be expected to increase the risk of development of a cyclops lesion, a recent review that combined data from 4 studies and 223 patients showed no significant association between remnant preservation and the presence of a cyclops lesion.23 However, the relatively small patient numbers limited the strength of this result.
Therefore, the purpose of the current study was to determine whether greater preservation of the tibial stump remnant would be associated with a decrease in the graft rupture rate without a concomitant increase in the rate of surgery for symptomatic cyclops lesions at 2 years after ACLR.
Methods
Study Design
This was a longitudinal study with classification of tibial stump remnant preservation (no stump, <50%, >50%) made at the completion of the ACLR surgery and subsequent 2-year follow-up. The study analyses were retrospectively made for this prospectively collected data. Procedures were approved by an institutional ethics committee and patients consented to their medical data being used for reserach purposes.
Participants
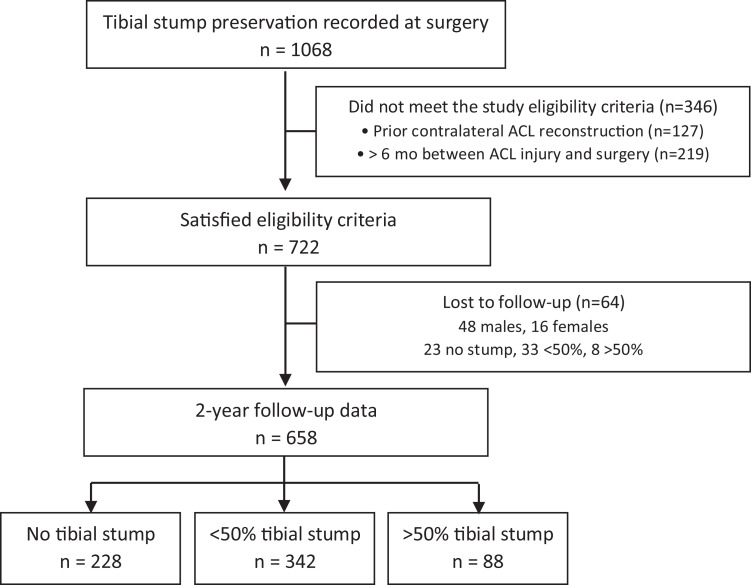
Between July 1, 2013, and June 30, 2016, the percentage of tibial stump remnant preservation at the completion of primary ACLR was recorded in 1068 patients. The procedures were carried out by 1 of 2 surgeons. Patients who had previous contralateral ACLR (n = 127) or who did not have surgery within the first 6 months after ACL injury (n = 219) were excluded, leaving a cohort of 722 eligible patients. A total of 64 patients were lost to follow-up, leaving a final cohort of 658 patients (91% follow-up) as the study participants. A flowchart of the study patients is shown in Figure 1.
Figure 1.
Flowchart of study patients. ACL, anterior cruciate ligament.
Surgical and Rehabilitation Details
For all participants, the ACLR was performed arthroscopically by 1 of 2 surgeons (J.A.F., T.S.W.), using a hamstring tendon autograft. Both surgeons were highly experienced and performed large numbers of ACLRs, each performing at least 200 per year. Both the semitendinosus and the gracilis tendons were harvested and doubled. If the graft diameter was less than 7.5 mm and there was adequate length of the semitendinosus, then this tendon was tripled. During the initial arthroscopy, the morphologic status of the remnant tissue was observed, and, if it was well-vascularized and of good quality, as much of the remnant as possible was preserved.
The femoral tunnel was drilled via the anteromedial portal to the same diameter as that of the proximal portion of the graft. While arthroscopically viewing the tibial attachment of the ACL, a 2.4-mm guide pin was inserted into the central portion of the remnant. Care was taken to minimize damage to the ACL remnant. The tibial bone tunnel was drilled over the guide pin to the same diameter as that of the distal portion of the graft. During tunnel creation, the reamer was carefully advanced to minimize damage to the remnant. Bony debris was removed from both tunnels, and a suture loop was passed through both tunnels to facilitate graft passage. Suspensory fixation was used for femoral graft fixation, and an interference screw was used for tibial graft fixation. The interference screw was inserted with the knee in 0° of extension. The absence of impingement of the graft/remnant in the intercondylar notch with the knee in full extension was confirmed arthroscopically.
The percentage of stump preservation was determined by the extent of coverage of the native ACL along the length of the ACL graft after passage and final debridement. This was categorized into 1 of 3 groups: no stump, less than 50%, and more than 50%. A finding of no stump was recorded when the full circumference of the intra-articular tibial aperture was visible arthroscopically adjacent to the anteromedial aspect of the anterior horn of the lateral meniscus with minimal insertional ACL stump fibers remaining. Satisfactory tunnel position was confirmed on a routine postoperative radiograph.
Postoperatively, all patients followed the same rehabilitation protocol, which encouraged immediate full active knee extension and the restoration of quadriceps function as soon as possible. Weightbearing was allowed as tolerated from the first postoperative day. No braces or splints were used. Progression was guided by the presence and degree of pain and swelling.
Follow-up
The study cohort was followed for 2 years from the date of surgery, and any subsequent graft ruptures or surgery for symptomatic cyclops lesions were recorded. All patients were followed up via a clinical examination at 3 weeks as well as at 3, 6, and 12 months. Specifically, at either the 3-month or the 6-month review, the presence of an otherwise unexplained effusion or loss of symmetrical passive extension was noted. In addition, the symptoms of swelling, an inability to fully straighten the knee, or pain with extension was noted. If any or all of the above were present, a provisional diagnosis of a symptomatic cyclops lesion was made and investigated using a magnetic resonance imaging scan. Once the diagnosis was confirmed, these patients were offered an arthroscopic debridement of the cyclops lesion if their symptoms were severe enough to warrant surgical intervention. For graft rupture, the date of the injury was recorded (further surgery was not required for inclusion), and for cyclops lesions, the date of arthroscopic surgery was recorded. This information was gathered via several different processes including examination of the medical records, completion of regular follow-up surveys by the clinic, and direct telephone contact with the patient. At the 12-month follow-up, further clinical and patient self-report measures including flexion and extension deficits, anterior tibial translation (measured with a KT-1000 arthrometer), single and triple crossover hops for distance, International Knee Documentation Committee subjective knee form, and the Marx activity scale were recorded. Return to sports status, as yes or no, was also recorded at 12 months and again at 2 years.
Data and Statistical Analysis
Contingency analysis and Kaplan-Meier survival analysis were used to determine trends in graft rupture rates and treatment for cyclops lesions between the 3 remnant preservation groups (no stump, <50%, or >50%). For contingency analysis, the Cochrane-Armitage (CA) test for trend was calculated, as this has greater power than does the chi-square test of association if there is a trend in ordinal categories (ie, amount of tibial stump preservation). The CA test statistic was calculated from the linear-by-linear association test (LLA) using the following formula: LLA value by N/(N – 1), where N is the number of participants. Data were initially analyzed for all patients and then subsequently analyzed by subgroup according to patient sex. To determine if the available patient cohort was of an appropriate size to achieve sufficient statistical power for the CA test, the probability of response was estimated to be between 2% and 8% with differences of 3% between groups and equally spaced levels of the independent variable (remnant preservation). This required a total sample of 486 patients (162 per group) to achieve 80% power with an alpha level of .05. All data were analyzed using SPSS Version 25 (IBM Corp) software. A P value ≤ .05 was used to indicate statistical significance.
Results
There was no difference in age, sex, or the proportion of patients that returned to sports among the 3 remnant preservation groups (Table 1). Femoral (P = .02) and tibial (P < .0001) bone tunnel diameters were smaller with remnant preservation.
Table 1.
Descriptive Data for the 3 Remnant Preservation Groupsa
| No Stump (n = 228) | <50% (n = 342) | >50% (n = 88) | P Value | |
|---|---|---|---|---|
| Age, y | 26.3 ± 10 | 26.0 ± 9 | 26.0 ± 9 | .9 |
| Sex, M:F | 152:76 | 205:137 | 48:40 | .09 |
| Time from injury to surgery, mo | 2.2 ± 1.5 | 2.3 ± 1.4 | 2.2 ± 1.2 | .8 |
| Femoral tunnel diameter, mm | 8.0 ± 0.7 | 7.9 ± 0.7 | 7.9 ± 0.7 | .02 |
| Tibial tunnel diameter, mm | 8.5 ± 0.8 | 8.1 ± 0.8 | 7.9 ± 0.6 | <.0001 |
| Returned to sports, n | 175/222b | 257/338 | 64/88 | .5 |
aData are reported as mean ± SD unless otherwise indicated. Bolded P values indicate statistically significant differences among the groups. F, female; M, male.
bReturn to sport data was not available for all patients.
At 12 months postoperatively, 95% of the cohort were reviewed, and equivalence among the 3 tibial stump group categorizations was shown for a variety of clinical and patient-reported outcomes, which are detailed in Table 2.
Table 2.
Patient Outcomes Recorded at 12 Months After Anterior Cruciate Ligament Reconstruction for the 3 Remnant Preservation Groupsa
| No Stump (n = 185) | <50% (n = 281) | >50% (n = 75) | P Value | |
|---|---|---|---|---|
| Active flexion deficit, deg | 4.0 ± 6 | 4.2 ± 6 | 5.7 ± 66 | .1 |
| Passive flexion deficit, deg | 4.0 ± 6 | 3.3 ± 6 | 4.2 ± 6 | .4 |
| Extension deficit, deg | 1.2 ± 3 | 1.1 ± 3 | 0.7 ± 4 | .4 |
| KT-1000 side to side difference (67 N) | 0.7 ± 2 | 0.6 ± 2 | 0.6 ± 2 | .9 |
| KT-1000 side to side difference (134 N) | 1.4 ± 3 | 1.5 ± 3 | 1.7 ± 2 | .5 |
| Single hop for distance LSI | 95.0 ± 12 | 95.1 ± 18 | 96.1 ± 13 | .9 |
| Triple crossover hop for distance LSI | 95.1 ± 13 | 95.9 ± 11 | 97.3 ± 11 | .6 |
| IKDC subjective knee score | 83.2 ± 16 | 83.4 ± 16 | 83.4 ± 16 | >.99 |
| Marx activity score | 9.8 ± 5 | 9.1 ± 5 | 8.9 ± 5 | .2 |
aData are reported as mean ± SD. IKDC, International Knee Documentation Committee; LSI, limb symmetry index.
There was no significant association between graft rupture rates and remnant preservation (Table 3). There was a significant trend for fewer operations for symptomatic cyclops lesions with greater remnant preservation when all patients were included in the analysis (P = .04) and also when female patients were analyzed as a subgroup (P = .04) (Table 3). The cumulative incidence of cyclops lesions over time in the 3 remnant preservation groups is shown in Figure 2. Independent of remnant preservation group, there was no difference in femoral (7.9 vs 8.1 mm; P = .07) or tibial tunnel diameter (8.2 vs 8.4 mm; P = .07) between patients who sustained a graft rupture and those who did not. Patients who had cyclops lesions had significantly larger femoral (7.9 vs 8.4 mm; P = .02) and tibial tunnels (8.2 vs 8.8 mm; P = .04).
Table 3.
Graft Rupture Rate and Rate of Surgery for Symptomatic Cyclops Lesions Within 2 Years of Anterior Cruciate Ligament Reconstruction Surgery Stratified According to the Degree of Tibial Stump Remnant Preservationa
| Tibial Stump Remnant Preservation | ||||
|---|---|---|---|---|
| No Stump | <50% | >50% | P Value | |
| Graft rupture | 20/228 (8.8) | 20/342 (5.8) | 3/88 (3.4) | .06 |
| Female | 6/76 (7.9) | 2/137 (1.5) | 1/40 (2.5) | .06 |
| Male | 14/152 (9.2) | 18/205 (8.8) | 2/48 (4.2) | .37 |
| Cyclops lesion | 12/228 (5.3) | 9/342 (2.6) | 1/88 (1.1) | .04 |
| Female | 6/76 (7.9) | 5/137 (3.6) | 0/40 (0) | .04 |
| Male | 6/152 (3.9) | 4/205 (2.0) | 1/48 (2.1) | .31 |
aData are reported as n/total (%). There were 253 female patients and 405 male patients in each group. Bolded P values indicate statistically significant differences among the groups.
Figure 2.
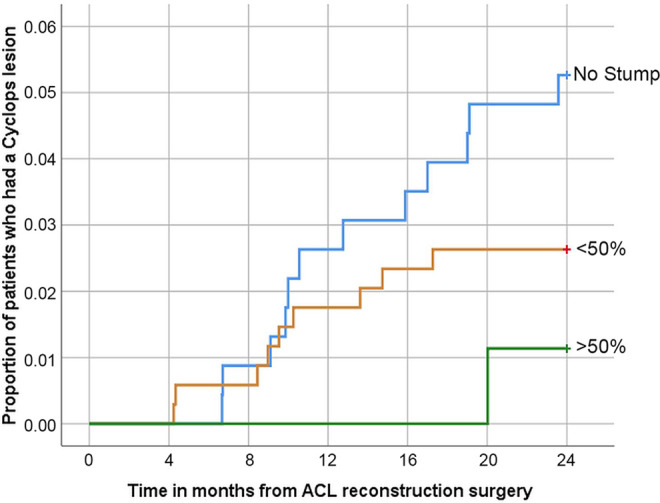
Cumulative incidence of surgery for symptomatic cyclops lesions among the 3 remnant preservation groups over time (up to 24-month follow-up). ACL, anterior cruciate ligament.
Discussion
In the current study, no statistical association was found between stump preservation and graft rupture rate within the first 2 postoperative years. In addition, stump preservation did not increase the rate of surgery for symptomatic cyclops lesions. In fact, stump preservation was associated with a lower incidence of surgery for symptomatic cyclops lesions, particularly for female patients.
There are few comparative studies with respect to graft rupture and retention of the tibial stump. Ouanezar et al16 reviewed 128 patients at a minimum of 24 months after surgery and reported no statistical difference in the rates of graft failure between those with a small amount (<50%) of remnant preservation (7.4%) and those with a large amount (>50%, 3.3%). These results are similar to those of the current study. Takazawa el al20 reviewed 183 patients, also with a 24-month minimum follow-up, and reported a significant difference in graft rupture rate depending on whether or not remnant preservation was possible. Patients who had their stump preserved had a lower graft rupture rate (1.2% vs 7.1%). In their study, the degree and quality of the remnant stump was critical. The stump was preserved only if it was covered with synovial tissue; was well-vascularized; and the amount of stump remaining was greater than 75% along the length of the graft from its tibial attachment, with a remnant bridge between the femur and tibia. Such strict criteria were not employed in the current study, although the quality and utility of the remnant tissue was carefully assessed and managed.
Although there has been concern that remnant preservation may lead to an increase in the occurrence of cyclops lesions after ACLR surgery,14,22 the current study did not demonstrate an increase in reoperation rate for symptomatic cyclops lesions with increasing stump preservation. This is consistent with the findings of several studies that demonstrated either no difference in reoperation rates or, in fact, a reduced reoperation rate with increasing amounts of stump retention.24 Ahn et al,1 in a magnetic resonance imaging study, reported no difference in the prevalence of a cyclops lesion after single-bundle ACLR between the remnant-preserving and remnant-resecting procedures (12.2% and 15%, respectively). Kondo et al10 similarly found no difference in the preservation group versus the resection group (14% vs 17.4%). Kim et al9 reported a cyclops lesion rate of 40% in patients in whom the stump was not able to be preserved compared with only 8% of patients in whom it was; the cyclops lesions were detected at second-look arthroscopy and were not symptomatic. Based on these findings, one might deduce that stump preservation has a protective effect on the development of cyclops lesions. However, a recent study by Delaloye et al,5 which reported on 3633 patients, found no relationship between reoperation for cyclops lesions and the amount of stump preservation. The authors determined that the most important risk factor for reoperation for a symptomatic cyclops lesion was an extension deficit in the early postoperative period.
The cohort in the current study consisted of a group of patients undergoing acute (within 6 months of injury) primary ACLR. The results showed a significant trend for higher rates of operative treatment of symptomatic cyclops lesion in patients with less remnant preservation. These findings highlight the complex cause of cyclops lesions, and although redundant ACL stump tissue may play an important role, clearly other tissue must be involved as well. One possible explanation may be the development of hypervascular scar tissue, which may be more prevalent in situations where the stump was completely debrided. In these situations, increased bleeding—and subsequent scar tissue formation—may occur from the stump insertion site, the fat pad, and the tibial tunnel aperture. A surgical technique focusing on stump retention may be associated with less overall tissue debridement and bleeding. This study demonstrated that with appropriate patient selection and surgical technique, the tibial stump may be safely retained without increasing the risk of developing a symptomatic cyclops lesion that requires subsequent surgery.
Although the follow-up rate of 91% was high, this study was not randomized, creating the potential for a selection bias. The groups were nonetheless well matched in terms of demographic variables as well as clinical and patient-reported outcome measures at 12 months. It should be noted that a selection bias may in fact be useful in appropriately managing this patient cohort, as selecting appropriate stump material to retain may be important in preventing the development of a cyclops lesion. The association between tunnel diameter and remnant preservation should also be considered a potential confounder, and future work should be done to determine whether this was a chance association.
A potential weakness of this study is the reliability of categorizing the amount of stump retained. This was recorded by the 2 treating surgeons on their own patients at the time of surgery, and we did not assess inter- or intrarater reliability. Despite the large overall sample size, remnant preservation group sizes were unequal with the fewest number of patients in the >50% remnant preservation group. This may indicate that substantial preservation of only viable, robust, and potentially useful tibial stump is difficult to achieve but necessary in order to maximize the chance of future incorporation and minimize the risk of remnant atrophy and subsequent cyclops formation. In addition, this study only reported on symptomatic cyclops lesions that were surgically managed. The true incidence of cyclops lesions in this cohort is not known, as asymptomatic lesions and symptomatic lesions not undergoing surgical management were not reported. It is also possible that a patient may have quit sports due to persistent laxity and therefore had an undocumented rupture that was not included in the current study. Apart from tunnel size, the surgical technique and, in particular, tunnel position were not evaluated. This is a potential limitation, as stump retention has been reported to potentially adversely affect surgical exposure and subsequent tunnel positioning. However, routine arthroscopic assessment of the position of the graft-stump complex in relation to the intercondylar notch in full extension was made and deemed to be free of impingement in all cases.
Conclusion
Although the graft rupture rate was not reduced via greater tibial ACL stump remnant preservation, stump preservation was also not associated with an increased reoperation rate for symptomatic cyclops lesions. The highest reoperation rate for symptomatic cyclops lesions was in the group with no remaining tibial stump, which may indicate that cyclops lesions, in addition to sometimes being caused by the ACL remnant, may have another cause, which is likely to be multifactorial.
Footnotes
Final revision submitted October 8, 2020; accepted November 24, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.A.F. is a paid associate editor for The Orthopaedic Journal of Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from La Trobe University (reference No. S16/220).
References
- 1. Ahn JH, Lee SH, Choi SH, Lim TK. Magnetic resonance imaging evaluation of anterior cruciate ligament reconstruction using quadrupled hamstring tendon autografts: comparison of remnant bundle preservation and standard technique. Am J Sports Med. 2010;38(9):1768–1777. [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Lee YS, Ha HC. Comparison of revision surgery with primary anterior cruciate ligament reconstruction and outcome of revision surgery between different graft materials. Am J Sports Med. 2008;36(10):1889–1895. [DOI] [PubMed] [Google Scholar]
- 3. Andonovski A, Topuzovska S, Samardziski M, et al. The influence of anterior cruciate ligament remnant on postoperative clinical results in patients with remnant preserving anterior cruciate ligament reconstruction. Open Access Maced J Med Sci. 2017;5(5):624–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cha J, Choi SH, Kwon JW, Lee SH, Ahn JH. Analysis of cyclops lesions after different anterior cruciate ligament reconstructions: a comparison of the single-bundle and remnant bundle preservation techniques. Skeletal Radiol. 2012;41(8):997–1002. [DOI] [PubMed] [Google Scholar]
- 5. Delaloye JR, Murar J, Vieira TD, et al. Knee extension deficit in the early postoperative period predisposes to cyclops syndrome after anterior cruciate ligament reconstruction: a risk factor analysis in 3633 patients from the SANTI Study Group Database. Am J Sports Med. 2020;48(3):565–572. [DOI] [PubMed] [Google Scholar]
- 6. George MS, Dunn WR, Spindler KP. Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34(12):2026–2037. [DOI] [PubMed] [Google Scholar]
- 7. Guo L, Chen H, Luo JM, et al. An arthroscopic second-look study on the effect of remnant preservation on synovialization of bone--patellar tendon—bone allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2016;32(5):868–877. [DOI] [PubMed] [Google Scholar]
- 8. Hu J, Qu J, Xu D, et al. Clinical outcomes of remnant preserving augmentation in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):1976–1985. [DOI] [PubMed] [Google Scholar]
- 9. Kim MK, Lee SR, Ha JK, et al. Comparison of second-look arthroscopic findings and clinical results according to the amount of preserved remnant in anterior cruciate ligament reconstruction. Knee. 2014;21(3):774–778. [DOI] [PubMed] [Google Scholar]
- 10. Kondo E, Yasuda K, Onodera J, Kawaguchi Y, Kitamura N. Effects of remnant tissue preservation on clinical and arthroscopic results after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(8):1882–1892. [DOI] [PubMed] [Google Scholar]
- 11. Lee BI, Kim BM, Kho DH, et al. Does the tibial remnant of the anterior cruciate ligament promote ligamentization? Knee. 2016;23(6):1133–1142. [DOI] [PubMed] [Google Scholar]
- 12. Lu W, Wang D, Zhu W, et al. Placement of double tunnels in ACL reconstruction using bony landmarks versus existing footprint remnant: a prospective clinical study with 2-year follow-up. Am J Sports Med. 2015;43(5):1206–1214. [DOI] [PubMed] [Google Scholar]
- 13. Ma T, Zeng C, Pan J, et al. Remnant preservation in anterior cruciate ligament reconstruction versus standard techniques: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57(7-8):1014–1022. [DOI] [PubMed] [Google Scholar]
- 14. McMahon PJ, Dettling JR, Yocum LA, Glousman RE. The cyclops lesion: a cause of diminished knee extension after rupture of the anterior cruciate ligament. Arthroscopy. 1999;15(7):757–761. [DOI] [PubMed] [Google Scholar]
- 15. Naraoka T, Kimura Y, Tsuda E, Yamamoto Y, Ishibashi Y. Is remnant preservation truly beneficial to anterior cruciate ligament reconstruction healing? Clinical and magnetic resonance imaging evaluations of remnant-preserved reconstruction. Am J Sports Med. 2017;45(5):1049–1058. [DOI] [PubMed] [Google Scholar]
- 16. Ouanezar H, Blakeney WG, Fernandes LR, et al. Clinical outcomes of single anteromedial bundle biologic augmentation technique for anterior cruciate ligament reconstruction with consideration of tibial remnant size. Arthroscopy. 2018;34(3):714–722. [DOI] [PubMed] [Google Scholar]
- 17. Papalia R, Franceschi F, Vasta S, et al. Sparing the anterior cruciate ligament remnant: is it worth the hassle? Br Med Bull. 2012;104:91–111. [DOI] [PubMed] [Google Scholar]
- 18. Sha L, Xie G, Zhao S, Zhao J. A morphologic and quantitative comparison of mechanoreceptors in the tibial remnants of the ruptured human anterior cruciate ligament. Medicine. 2017;96(5):e6081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Song GY, Zhang H, Zhang J, et al. The anterior cruciate ligament remnant: to leave it or not? Arthroscopy. 2013;29(7):1253–1262. [DOI] [PubMed] [Google Scholar]
- 20. Takazawa Y, Ikeda H, Kawasaki T, et al. ACL reconstruction preserving the ACL remnant achieves good clinical outcomes and can reduce subsequent graft rupture. Orthop J Sports Med. 2013;1(4):2325967113505076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tie K, Chen L, Hu D, Wang H. The difference in clinical outcome of single-bundle anterior cruciate ligament reconstructions with and without remnant preservation: a meta-analysis. Knee. 2016;23(4):566–574. [DOI] [PubMed] [Google Scholar]
- 22. Tonin M, Saciri V, Veselko M, Rotter A. Progressive loss of knee extension after injury: cyclops syndrome due to a lesion of the anterior cruciate ligament. Am J Sports Med. 2001;29(5):545–549. [DOI] [PubMed] [Google Scholar]
- 23. Wang H, Liu Z, Li Y, et al. Is remnant preservation in anterior cruciate ligament reconstruction superior to the standard technique? A systematic review and meta-analysis. Biomed Res Int. 2019;2019:1652901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang HD, Wang FS, Gao SJ, Zhang YZ. Remnant preservation technique versus standard technique for anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2018;13(1):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang J, Ao Y. Analysis of different kinds of cyclops lesions with or without extension loss. Arthroscopy. 2009;25(6):626–631. [DOI] [PubMed] [Google Scholar]
- 26. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–647. [DOI] [PubMed] [Google Scholar]
- 27. Wright R, Gill C, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am 2012;94(6):531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wright RW, Huston LJ, Spindler KP, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]