In their response to our article (1), Rabb et al. (2) present results from a survey experiment testing the effect of community- or family-based appeals on participants’ interest in reading a COVID-19 vaccination plan. The authors report a null finding and argue that “evidence suggests, counterintuitively, that common-good appeals have limited utility.” In our view, Rabb et al.’s results and the interpretation thereof should be put into perspective.
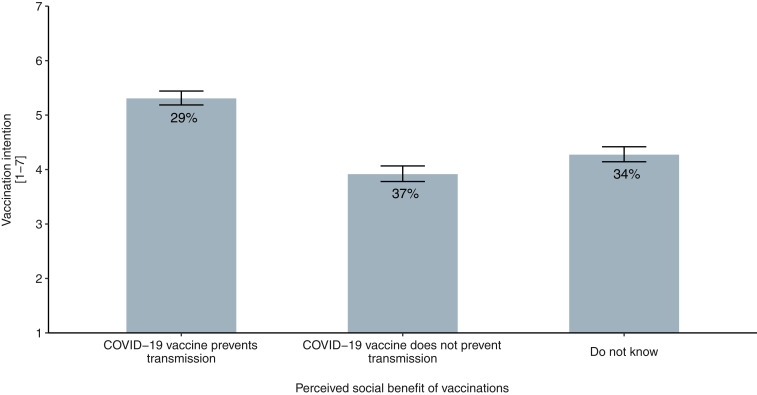
First, both appeals emphasize the social benefit of vaccination through indirect protection (herd or community immunity). The experiment did not test whether common-good appeals (vs. no such appeals) lead to higher vaccination interest but rather whether interest differs when different target groups profit from vaccination. Previous research, however, has tested the effectiveness of such appeals using appropriate (nonintervention) control groups. A recent systematic review by Hakim et al. (3) summarized 32 studies comparing common-good appeals with alternative strategies. It concluded that stressing the social benefit of vaccination has an overall positive effect on knowledge, attitudes, and vaccination intentions. The social aspects of vaccination also seem to play a role in individuals' COVID-19 vaccination decision (4). Data from the biweekly COVID-19 Snapshot MOnitoring (COSMO) in Germany, for example, indicate that individuals who believe that the COVID-19 vaccine prevents pathogen transmission have greater intentions to vaccinate, compared to individuals who do not think so or are unsure (Fig. 1).
Fig. 1.
Vaccination intentions as a function of the belief, or lack thereof, that COVID-19 vaccines prevent transmission. The percentages in the bars represent the proportions of respondents per belief. Most respondents did not know or did not assume that vaccination would curb transmission (i.e., lead to community immunity). When respondents believed that vaccination prevents transmission, vaccination intentions were higher than in the two other cases (F[2, 2,983] = 99.18, P < 0.001, = 0.062). Data were collected as part of the cross-sectional COVID-19 Snapshot MOnitoring (COSMO; ethical clearance from University of Erfurt’s institutional review board no. 20200302/20200501) study series between 15 and 29 December 2020; n = 2,986.
Second, and related to the above-mentioned evidence, Rabb et al. (2) intentionally or unintentionally used the weakest form of communicating community immunity, i.e., a text-based appeal of the vaccination’s social benefit. Purely text-based interventions have been shown to be less (if at all) effective—particularly when the perceived costs, including potential risks through side effects of vaccination, are high (5–7). This is important given that currently, in the United States, vaccination against COVID-19 is likely to be perceived as costly due to the vaccines’ fast-track emergency approval and people’s associated safety concerns (8). In this situation, common-good appeals are likely to be insufficient to increasing vaccination intentions. Thus, in addition to addressing safety concerns, successful communication strategies should use more effective means of communicating social benefits, including visualizations that clarify the concept of community immunity (6). Combining common-good appeals with inspiring empathy for those most vulnerable to an infection can further amplify vaccination intentions (9).
In sum, common-good appeals are not a panacea to low vaccination intentions. The aforementioned boundary conditions are well known. Further, vaccines need to provide community immunity in the first place. This important detail is still under scientific debate for COVID-19 vaccines, a debate mirrored by people’s beliefs (Fig. 1). We therefore conclude that common-good appeals are a promising building block for an evidence-based communication strategy—at least when based on the available evidence regarding the most effective communication formats. However, building upon common-good appeals may be too early in the case of COVID-19, as trust in the safety of vaccines and knowledge about sterile immunity must be established first.
Footnotes
The authors declare no competing interest.
Data Availability
Data and script of analysis are available at Open Science Framework (OSF) (https://osf.io/nrqhs/) (10).
References
- 1.Korn L., Böhm R., Meier N. W., Betsch C., Vaccination as a social contract. Proc. Natl. Acad. Sci. U.S.A. 117, 14890–14899 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rabb N., Glick D., Houston A., Bowers J., Yokum D., No evidence that collective-good appeals best promote COVID-related health behaviors. Proc. Natl. Acad. Sci. U.S.A., 10.1073/pnas.2100662118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hakim H., et al., Interventions to help people understand community immunity: A systematic review. Vaccine 37, 235–247 (2019). [DOI] [PubMed] [Google Scholar]
- 4.Head K. J., Kasting M. L., Sturm L. A., Hartsock J. A., Zimet G. D., A national survey assessing SARS-CoV-2 vaccination intentions: Implications for future public health communication efforts. Sci. Commun. 42, 698–723 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Betsch C., Böhm R., Moral values do not affect prosocial vaccination. Nat. Hum. Behav. 2, 881–882 (2018). [DOI] [PubMed] [Google Scholar]
- 6.Betsch C., Böhm R., Korn L., Holtmann C., On the benefits of explaining herd immunity in vaccine advocacy. Nat. Hum. Behav. 1, 0056 (2017). [Google Scholar]
- 7.Betsch C., Böhm R., Korn L., Inviting free-riders or appealing to prosocial behavior? Game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychol. 32, 978–985 (2013). [DOI] [PubMed] [Google Scholar]
- 8.Shmerling R. H., “COVID-19 vaccines: Safety, side effects –– and coincidence” Harvard Health Publishing (2021). https://www.health.harvard.edu/blog/covid-19-vaccines-safety-side-effects-and-coincidence-2021020821906. Accessed 10 February 2021.
- 9.Pfattheicher S., Petersen M. B., Böhm R., Information about herd immunity through vaccination and empathy promote COVID-19 vaccination intentions. PsyArXiv [Preprint] (2020). https://psyarxiv.com/wzu6k/. Accessed 10 February 2021. [DOI] [PubMed]
- 10.Korn L., Betsch C., Böhm R., Reply to Rabb et al.: Why promoting COVID-19 vaccines with community immunity is not a good strategy (yet). Open Science Framework. https://osf.io/nrqhs/. Deposited 12 February 2021. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and script of analysis are available at Open Science Framework (OSF) (https://osf.io/nrqhs/) (10).