Abstract
Background:
Over 180,000 coronary artery bypass grafting (CABG) procedures are performed annually, accounting for $7–10 billion in episode expenditures. Assessing tradeoffs between spending and quality contributing to value during 90-day episodes has not been conducted, but is essential for success in bundled reimbursement models. We therefore identified determinants of variability in hospital 90-day episode value for CABG.
Methods/Results:
Medicare and private payor admissions for isolated CABG from 2014–2016 were retrospectively linked to clinical registry data for 33 non-federal hospitals in Michigan. Hospital composite risk-adjusted complication rates (≥1 National Quality Forum-endorsed, Society of Thoracic Surgeons measure: deep sternal wound infection, renal failure, prolonged ventilation >24 hours, stroke, re-exploration, and operative mortality) and 90-day risk-adjusted, price-standardized episode payments were used to categorize hospitals by value by defining the intersection between complications and spending. Among 2573 total patients, those at low- vs. high-value hospitals had a higher percentage of prolonged length of stay >14 days (9.3% vs. 2.4%, p=0.006), prolonged ventilation (17.6% vs. 4.8%, p<0.001), and operative mortality (4.8% vs. 0.6%, p=0.001). Mean total episode payments were $51,509 at low- compared with $45,526 at high-value hospitals (p<0.001), driven by higher readmission ($3675 vs. $2177, p=0.005), professional ($7462 vs. $6090, p<0.001), post-acute care ($7315 vs. $5947, p=0.031), and index hospitalization payments ($33,474 vs. $30,800, p<0.001). Among patients not experiencing a complication or 30-day readmission (1923/2573, 74.7%), low-value hospitals had higher inpatient evaluation and management (E&M) payments ($1405 vs. $752, p<0.001) and higher utilization of inpatient rehabilitation (7% vs. 2%, p<0.001), but lower utilization of home health (66% vs. 73%, p=0.016) and emergency department services (13% vs. 17%, p=0.034).
Conclusions:
To succeed in emerging bundled reimbursement programs for CABG, hospitals and physicians should identify strategies to minimize complications while optimizing inpatient E&M spending and use of inpatient rehabilitation, home health, and emergency department services.
INTRODUCTION
Approximately 300,000 adults undergo cardiac surgery annually, and over half include coronary artery bypass grafting (CABG), accounting for approximately $7–10 billion in episode expenditures.1–3 As a result, CABG is one of the most widely studied inpatient surgical procedures and has become a target for bundled payment models. Extensive work has been performed describing hospital variation in the quality of CABG care,4–9 prompting the establishment of quality measures through the Society of Thoracic Surgeons (STS) and National Quality Forum (NQF).10 Despite these efforts, less attention has been paid to the relationship between quality and spending.
The Bundled Payments for Care Improvement-Advanced (BPCI-A) program was initiated on October 1, 2018 by the Center for Medicare & Medicaid Services (CMS) to implement voluntary episode payment models11 and hold providers accountable for the quality and expenditures throughout an episode of care. A number of investigators have identified hospital variation in clinical outcomes after CABG, including mortality,4,12 complications,5–7,12 and failure to rescue,4,8,9,12 but have not assessed spending. Other investigators have reported wide hospital variation in episode payments after cardiac surgery, but have not assessed clinical outcomes.3,13 While healthcare reform efforts such as the BPCI have focused on optimizing value (defined as quality divided by expenditures), few studies have examined the relationship between clinical outcomes and episode payments to identify how high-value hospitals achieve their performance, whether through increasing quality and/or decreasing payments. The few studies that have characterized “value” in performing CABG have either been performed at a single center,14 limited to one outcome (pneumonia),2 or used hospital costs and charge-to-cost ratios, which may not accurately reflect real-world spending.14–16 In contrast, an analysis linking established measures of clinical outcomes (e.g., complications and mortality) with episode payments could help hospitals identify targets to increase value and succeed in the BPCI or other similar programs.
To help hospitals, payors, and providers better navigate value-based reimbursement models, clinical outcomes data were linked to 90-day episode payments housed within two statewide quality improvement collaboratives. These data were used to assess determinants of high-value episodes for CABG surgery.
METHODS
The University of Michigan Institutional Review Board deemed this study to be exempt from review. These data cannot be made available due to data use restrictions. Additional details pertaining to analytic methods are available from the corresponding author upon reasonable request.
Data Sources
Episode payments were collected from the Michigan Value Collaborative (MVC), a group of 87 Michigan acute care hospitals and 31 physician organizations that seeks to achieve the best possible patient outcomes at the lowest reasonable cost. The MVC Coordinating Center uses Medicare fee-for-service claims data and Blue Cross Blue Shield of Michigan (BCBSM) preferred provider organization claims to create a validated registry of comprehensive 90-day episodes of care among Michigan patients.17
Clinical data were collected through the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative (MSTCVS-QC), developed in 2001 as a cardiac surgeon-led quality collaborative embedded in the MSTCVS. In 2005, the MSTCVS-QC became partially funded by the Blue Cross/Blue Shield of Michigan insurance company. The collaborative meets quarterly to review hospital-specific processes and outcomes, and to facilitate and evaluate quality improvement studies to improve the outcomes of cardiac and general thoracic surgical patients in Michigan. The MSTCVS-QC gathers data from all 33 non-federal hospitals in Michigan that provide cardiac surgery. On a quarterly basis, each of the 33 non-federal adult cardiac surgical hospitals in Michigan send the MSTCVS-QC data coordinating center a copy of their STS national harvest file through a certified STS vendor.
Hospital characteristics were collected through the American Hospital Association Annual Survey and included the following reported variables: number of beds, teaching status, and urban designation.
Patient Population
Isolated CABG 90-day episodes were identified within the MVC based on admission date ranges (June 1, 2014 through June 1, 2016) for BCBSM and Medicare beneficiaries residing in Michigan (n=2782). Procedures from both data warehouses were successfully probabilistically matched (match rate 92.5%, n=2573) using an algorithm that included: hospital, surgeon, patient date of birth, gender, admit date, and discharge date (eAppendix in the Supplement).
Defining Hospital Value
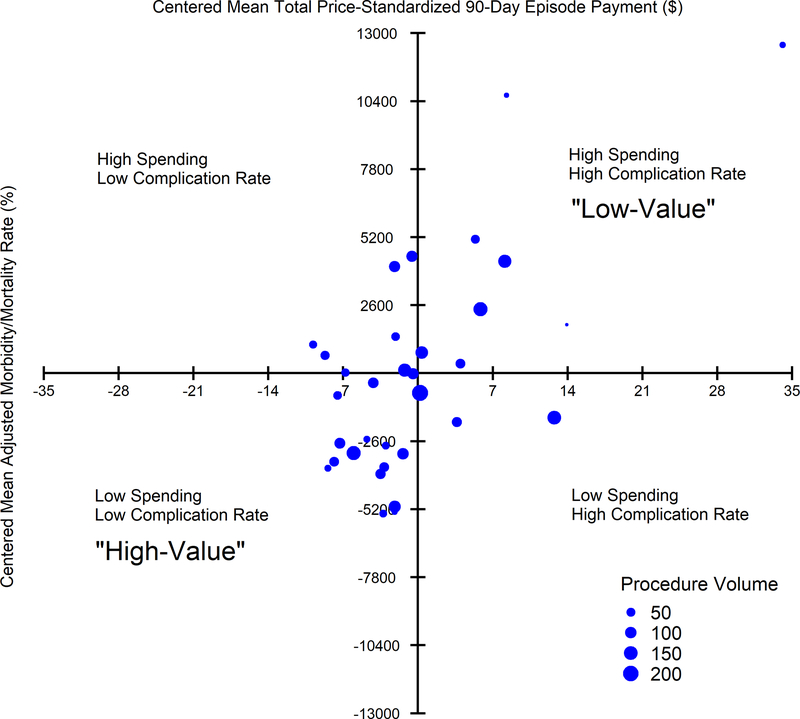
A centered mean complication rate and centered mean total episode payment was defined empirically for each of the 33 hospitals. For clinical risk-adjustment, observed/expected (O/E) ratios were created by dividing the patient-level observed complication rate by the expected morbidity and operative mortality according to the NQF-endorsed STS CABG composite measure risk-adjustment model.10 The O/E ratio for each hospital was then multiplied by the crude complication rate to form a risk-adjusted mean complication rate. Each hospital was added to a scatter plot of risk-adjusted centered means, with each dot representing one hospital and weighted in size by its overall isolated CABG volume (Figure 1). Hospitals were subsequently defined as “low” or “high” value based on their risk-adjusted complication rates and spending as compared to the centered means. While analyses were primarily focused on the comparison between low- versus high-value hospitals (Tables 1–3), a more complete analysis of all hospital value strata was also conducted (eTables 1 and 2).
Figure 1.
Deviation from centered mean in complication rate (x-axis) and total episode payments (y-axis). Plotted dots are weighted by hospital volume of isolated coronary artery bypass grafting procedures. Quadrants are labeled as “high” or “low” spending and complication rates. Complications included any of the following: deep sternal wound infection, renal failure, prolonged ventilation (>24 hours), stroke, surgical re-exploration, and operative mortality. Centers in the high spending and high complication rate quadrant are considered “low-value,” while those in the low spending and low complication rate quadrant are considered “high-value.” Pearson-weighted correlation coefficient=0.51.
Table 1.
Hospital characteristics stratified by “low-value” and “high-value” hospitals defined by spending and complication rate category.
| Overall | High spending & high complication rate “Low-value” | Low spending & low complication rate “High-value” | P-value | |
|---|---|---|---|---|
| Hospitals, n | 33 | 8 | 15 | |
| Total patients, n | 2573 | 587 | 1027 | |
| Percent Medicare CABG Patients, mean % per hospital | 77 | 76 | 78 | 0.52 |
| Hospital Structure | ||||
| Mean beds, n (std) | 464 (241) | 460 (266) | 411 (219) | 0.52 |
| Teaching, % | 97 | 88 | 100 | 0.36 |
| Urban, % | 90 | 100 | 86 | 0.52 |
| Hospital processes, % compliance | ||||
| Compliance with all processes | 93.5 | 93.3 | 93.9 | 0.70 |
| Aspirin at discharge | 99.2 | 99.9 | 98.8 | 0.21 |
| Beta blockers at discharge | 99.6 | 99.9 | 99.4 | 0.21 |
| Lipid-lowering statin at discharge | 98.7 | 99.6 | 98.6 | 0.24 |
| Preoperative beta blockers | 97.3 | 95.8 | 97.8 | 0.42 |
| Use of internal mammary artery | 99.1 | 99.5 | 99.4 | 0.62 |
| Appropriate antibiotic selection | 99.9 | 100 | 100 | 1.00 |
| Appropriate antibiotic discontinuation | 99.5 | 99.5 | 99.4 | 0.50 |
| Clinical Characteristics | ||||
| Mean HCCs, n (std) | 4.9 (0.9) | 5.7 (1.2) | 4.6 (0.6) | 0.012 |
| Mean admission to discharge LOS, d (std) | 9.6 (2.1) | 11.6 (3.4) | 8.6 (0.9) | 0.006 |
| Mean surgery to discharge LOS, d (std) | 7.2 (1.8) | 8.9 (2.8) | 6.4 (0.8) | 0.002 |
| Mean ICU LOS, h (std) | 80 (49) | 123 (78) | 63 (20) | 0.008 |
| Emergency department visit, % | 19.3 | 16.9 | 18.8 | 0.35 |
| Unplanned readmission rate, % | 17.2 | 20.6 | 13.4 | 0.005 |
| Overall complication rate, % | 11.1 | 20.8 | 6.7 | <0.001 |
| Surgery status, % | ||||
| Elective | 50.0 | 45.3 | 54.3 | 0.11 |
| Emergent | 1.7 | 2.0 | 1.8 | 0.57 |
| Emergent Salvage | 0.2 | 0.9 | 0.0 | 0.13 |
| Urgent | 48.1 | 51.9 | 43.9 | 0.19 |
CABG, coronary artery bypass grafting; HCC, hierarchical condition category; ICU, intensive care unit; LOS, length of stay; std, standard deviation.
Table 3.
Mean (standard error) risk-adjusted, price-standardized 90-day total and component episode payments in low-value (high spending and high complication rate) and high-value (low spending and low complication rate) hospitals. Conditional-on-use payments only include patients alive at discharge (Overall: 2542/2573, 98.8%; Low-value: 568/587, 96.8%; High-value: 1023/1027, 99.6%) who used readmission and/or post-acute care payments. E&M, evaluation and management.
| Overall | Low-value | High-value | P-value | |
|---|---|---|---|---|
| Hospitals, n | 33 | 8 | 15 | |
| Total patients, n | 2573 | 587 | 1027 | |
| Patients, mean n (std) per hospital | 78 (51) | 73 (59) | 68 (38) | 0.85 |
| Total payments, $ | 48,099 (375) | 51,509 (1024) | 45,526 (402) | <0.001 |
| Index hospitalization, $ | 31,928 (186) | 33,474 (546) | 30,800 (213) | <0.001 |
| Professional services, $ | 6511 (56) | 7462 (157) | 6090 (67) | <0.001 |
| Surgical procedures | 3244 (22) | 3273 (50) | 3195 (30) | 0.25 |
| Inpatient E&M services | 1372 (33) | 2109 (96) | 1004 (35) | <0.001 |
| Outpatient E&M services | 248 (4) | 286 (8) | 238 (5) | 0.010 |
| E&M consult (inpatient and outpatient) | 115 (7) | 161 (18) | 107 (11) | 0.027 |
| Anesthesia | 925 (7) | 980 (15) | 935 (11) | 0.43 |
| Imaging | 274 (4) | 330 (10) | 269 (6) | 0.038 |
| Labs and tests | 93 (3) | 118 (7) | 86 (5) | 0.017 |
| Other professional | 231 (14) | 266 (32) | 181 (17) | 0.003 |
| Overall readmission, $ | 3115 (213) | 3675 (485) | 2177 (246) | 0.005 |
| n patients with any $ | 471 [19%] | 116 [20%] | 149 [15%] | 0.006 |
| $, when present | 23,746 (1285) | 25,955 (2671) | 20,939 (1763) | 0.07 |
| Overall post-acute care, $ | 6614 (194) | 7315 (539) | 5947 (216) | 0.031 |
| n patients with any $ | 2457 [97%] | 546 [93%] | 983 [96%] | 0.020 |
| $, when present | 6964 (202) | 7908 (576) | 6247 (223) | 0.013 |
| Inpatient rehabilitation | 927 (97) | 1419 (230) | 489 (94) | 0.005 |
| n patients with any $ | 163 [6%] | 61 [10%] | 40 [4%] | <0.001 |
| $, when present | 29,109 (2093) | 28,874 (2929) | 24,982 (2900) | 0.65 |
| Outpatient rehabilitation | 489 (19) | 466 (31) | 496 (26) | 0.67 |
| n patients with any $ | 1396 [55%] | 300 [51%] | 571 [56%] | 0.08 |
| $, when present | 938 (33) | 847 (49) | 929 (41) | 0.86 |
| Skilled nursing facility | 1585 (115) | 1862 (278) | 1668 (184) | 0.58 |
| n patients with any $ | 433 [17%] | 113 [19%] | 181 [18%] | 0.42 |
| $, when present | 16,860 (974) | 22,666 (2132) | 16,939 (1485) | 0.88 |
| Home health | 2373 (40) | 2100 (97) | 2368 (65) | 0.25 |
| n patients with any $ | 1947 [77%] | 386 [66%] | 755 [74%] | 0.001 |
| $, when present | 3199 (41) | 3258 (114) | 3286 (66) | 0.89 |
| Facility emergency department | 316 (20) | 205 (28) | 276 (24) | 0.021 |
| n patients with any $ | 510 [20%] | 88 [15%] | 200 [19%] | 0.024 |
| $, when present | 1788 (85) | 1537 (151) | 1590 (92) | 0.77 |
| Other outpatient facility | 698 (48) | 834 (144) | 706 (71) | 0.33 |
| n patients with any $ | 2007 [79%] | 383 [65%] | 855 [83%] | <0.001 |
| $, when present | 912 (62) | 1302 (222) | 864 (86) | 0.033 |
To distinguish between the quality and spending determinants of hospital value, a subset analysis was additionally performed among patients who did not experience a complication or 30-day readmission (n=1923/2573, 74.7%). This analysis focused on identifying differences in episode payments between low- and high-value hospitals for uncomplicated isolated CABG.
Clinical Data
All processes of care and clinical outcomes measures were selected based on their inclusion in either the STS CABG performance measures10 or as part of the Merit-Based Incentive Payment System (MIPS) under CMS.18
Processes of care measures included preoperative beta blocker, appropriate antibiotic selection and discontinuation, use of internal mammary artery, and aspirin, beta blockers, and lipid-lowering statins at discharge. In accordance with the STS and the NQF,10 the composite postoperative outcomes measure included any of the following: deep sternal wound infection, renal failure, prolonged ventilation (>24 hours), stroke, surgical re-exploration, and operative mortality. Prolonged length of stay was defined as greater than 14 days. Operative mortality was defined as death during hospitalization in which CABG was performed or within 30 days after surgery. Risk-adjusted 30-day readmission was derived from an STS model of Medicare fee-for-service beneficiaries only10 and thus could not be included in the composite complication rate O/E ratio calculation. Instead, a regression of unadjusted 30-day readmission with morbidity and operative mortality was conducted to determine a risk-adjusted readmission rate. The distribution of hospitals by centered mean readmission rate and 90-day episode payments is displayed in eFigure 1.
Ninety-Day Price-Standardized Episode Payments
The primary outcome was total 90-day price-standardized episode payments. Payments were quantified for 90-day episodes of care and were disaggregated into index hospitalization, professional, readmission, and post-acute care components and further subcomponents.19 Patient clinical demographic data for these episodes were collected using International Classification of Diseases 9 (ICD-9) codes. Payments were price-standardized using average Medicare payments in the state of Michigan to account for payer-type, inflation, regional variation, and contractual differences.20 Price standardization ensures that variation in payments reflects differences in healthcare utilization rather than differences in geographic reimbursement.
Readmission and post-acute care payments were reported as mean component payments and as “conditional on use,” which restricted payments to patients who were readmitted and/or received post-acute care. Post-discharge payments were restricted to patients known to be alive at hospital discharge (low-value hospitals: 568/587, 96.8% and high-value hospitals: 1023/1027, 99.6%).
Statistical Analyses
Total and component payments were risk-adjusted using a two-step regression model, adjusting for patient characteristics, comorbidities, and payments in the 6 months prior to the index procedure. Risk adjustment was performed using observed/expected (O/E) ratios as previously described.13 Among component and subcomponent payments, percent attributed to the total difference in payments between groups was reported. Since total and component episode payments were risk-adjusted separately, component percentages attributed to the total difference may not equal 100%. A sensitivity analysis was performed to compare mean inpatient evaluation and management (E&M) payments indexed per hospital day between low- vs. high-value hospitals in both the primary and subset analyses to evaluate differences not attributed to the number of days spent in the hospital. Hospital days used to index these payments consisted of the total length of stay during the 90-day episode, including any readmissions.
A Pearson’s weighted product-moment correlation coefficient was calculated for Figure 1 and eFigure 1 to incorporate hospital procedural volume. Categorical variables were presented as percentages, continuous variables as mean (standard deviation), and payments as mean (standard error). Mann-Whitney U or Kruskal-Wallis tests were used to test continuous hospital-level variables and aggregated patient-level characteristics among low- vs. high-value and all 4 hospital categories, respectively. Chi-squared tests were used for hospital-level variables. Payment data were tested using a generalized estimating equation treating hospital as a cluster unit.
P-values of less than 0.05 (2-tailed) were considered statistically significant. All analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Hospital Value Distribution
Eight hospitals (n=587) had high spending and a high complication rate (“low-value” hospitals), 15 hospitals (n=1027) had low spending and a low complication rate (“high-value” hospitals), 3 hospitals (n=448) had low spending and a high complication rate, and 7 hospitals (n=511) had high spending and a low complication rate (Figure 1).
Hospital Structure and Processes
The distribution of Medicare patients, hospital structural characteristics, and compliance with performance processes did not differ between high- and low-value hospitals (Table 1). Patients in low-value hospitals had a higher mean number of hierarchical condition categories (5.7 [1.2] vs. 4.6 [0.6], p=0.012), longer mean intensive care unit length of stay (123 [78] vs. 63 [20] hours, p=0.008) and overall postoperative length of stay (8.9 [2.8] vs. 6.4 [0.8] days, p=0.002), and a higher rate of unplanned readmission within 30 days (20.6% vs. 13.4%, p=0.005).
Risk-Adjusted Clinical Outcomes
Risk-adjusted rates of prolonged hospital length of stay (low-value: 9.3% vs. high-value: 2.4%, p=0.006), prolonged ventilation (low-value: 17.6% vs. high-value: 4.8%, p<0.001), and operative mortality (low-value: 4.8% vs. high-value: 0.6%, p<0.001) were higher at low- compared to high-value hospitals, while adjusted rates of deep sternal wound infection, renal failure, stroke, surgical re-exploration, and 30-day readmission did not statistically differ (Table 2).
Table 2.
Risk-adjusted composite and individual outcomes stratified by low-value (high spending and high complication rate) and high-value (low spending and low complication rate) hospitals.
| Overall | Low-value | High-value | P-value | |
|---|---|---|---|---|
| Hospitals, n | 33 | 8 | 15 | |
| Total patients, n | 2573 | 587 | 1027 | |
| Risk-adjusted composite major morbidity and mortality, % | 11.0 | 21.0 | 6.6 | <0.001 |
| Prolonged length of hospital stay (>14 days) | 4.4 | 9.3 | 2.4 | 0.006 |
| Deep sternal wound infection | 0.2 | 0.1 | 0.2 | 0.63 |
| Postoperative renal failure | 1.5 | 2.2 | 1.0 | 0.16 |
| Prolonged intubation/ventilation | 8.5 | 17.6 | 4.8 | <0.001 |
| Stroke/cerebrovascular accident | 1.3 | 1.1 | 1.7 | 0.88 |
| Operative Mortality | 1.8 | 4.8 | 0.6 | <0.001 |
| Surgical re-exploration | 2.5 | 4.5 | 1.3 | 0.26 |
| 30-day risk-adjusted readmission rate | 11.3 | 11.7 | 10.8 | 0.25 |
Ninety-Day Price-Standardized Episode Payments
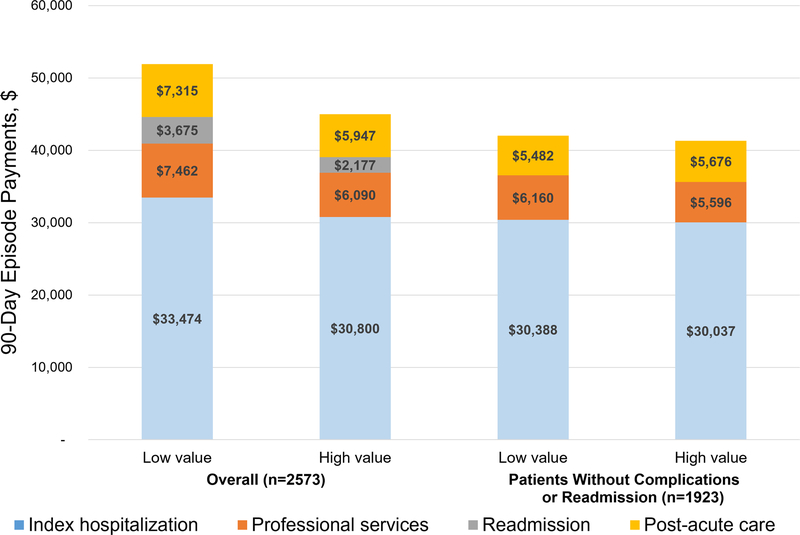
Mean total episode payments were higher at low-value hospitals ($51,509 [$1024] vs. $45,526 [$402], p<0.001). Nearly half (45%, $2674) of the difference in spending between low- and high-value hospitals was accounted for by higher index hospitalization spending (Figure 2).
Figure 2.
Variation in total and component 90-day episode payments after coronary artery bypass grafting in low- and high-value hospitals among the overall population (n=2573) and only patients who did not experience a complication or get readmitted within 30 days (n=1923). Complications included any of the following: deep sternal wound infection, renal failure, prolonged ventilation (>24 hours), stroke, surgical re-exploration, and operative mortality. Post-acute care payments include inpatient and outpatient rehabilitation, home health, skilled nursing facility, emergency department, and other outpatient facility payments.
Eighty-one percent of the difference in professional payments at low- and high-value hospitals were driven by inpatient E&M payments (low: $2109 [$96] vs. high: $1004 [$35], p<0.001). Inpatient E&M payments remained higher at low- compared to high-value hospitals when indexed by hospital days ($183 [$5] vs. $108 [$4] per hospital day, p=0.002). Sixty-eight percent of the difference in post-acute care payments was driven by inpatient rehabilitation payments (low: $1419 [$230] vs. $489 [$94], p=0.005). A higher proportion of patients at low-value hospitals were readmitted (20% vs. 15%, p=0.006) and used post-discharge inpatient rehabilitation (10% vs. 4%, p<0.001), while a smaller proportion used home health (66% vs. 74%, p=0.001) and emergency department services (15% vs. 19%, p=0.024). Patients in the low complications/high spending hospital group had similar mean inpatient E&M payments ($1727 [$79]) as low-value hospitals ($2109 [$96]), but had a similar proportion of patients using emergency department services (20%) as high-value hospitals (19%) [eTable 3]. Among patients with any payments, overall post-acute care payments were higher at low-value hospitals ($7908 [$576] vs. $6247 [$223], p=0.013) [Table 3].
Payment Variation Among Patients Without Complications
Among patients who did not experience a complication or readmission (n=1923/2573, 74.7%), total episode payments no longer statistically differed between low-value vs. high-value hospitals ($42,489 [$552] vs. $41,380 [$325], p=0.11). Low-value hospitals had higher professional payments ($6160 [$88] vs. $5596 [$57], p<0.001), especially higher inpatient E&M payments ($1405 vs. $752, p<0.001), which remained higher at low- compared to high-value hospitals when indexed by hospital days ($171 [$6] vs. $95 [$4] per hospital day, p=0.002). In contrast, index hospitalization and post-acute care payments were not statistically different between low- and high-value hospitals. In addition, a higher proportion of patients at low-value hospitals used inpatient rehabilitation (7% vs. 2%, p<0.001), while a smaller proportion used home health (66% vs. 73%, p=0.016) and the emergency department (13% vs. 17%, p=0.034) [eTable 4].
DISCUSSION
In this large, multi-center, statewide experience, variability existed both in healthcare quality and spending across hospitals in a 90-day episode following isolated CABG. Specifically, low-value hospitals had higher rates of prolonged hospital stay (9.3% vs. 2.4%), more patients with prolonged ventilation (17.6% vs. 4.8%), and a higher operative mortality (4.8% vs. 0.6%). Additionally, low-value hospitals had higher total and component 90-day episode payments. Patients not experiencing a complication or rehospitalization at low- compared to high-value hospitals had higher professional payments and a higher rate of inpatient rehabilitation utilization, but lower rates of home health and emergency department utilization.
This study has several limitations. First, while representing the predominant healthcare payors in Michigan (Medicare, BCBSM), the MVC does not capture other important payors (e.g., Medicaid) and the distribution of payors may differ by hospital. Second, although the present study represents the experience of all 33 non-federal hospitals performing cardiac surgery in Michigan, these findings may not be generalizable outside of Michigan or to procedures other than isolated CABG. Third, while the results from this study were risk-adjusted and price-standardized, all important confounding factors may not be accounted for. Last, while the MVC collects the majority of expenses reimbursed during a 90-day episode, not all relevant expenditures may be captured from both a payor (e.g., pharmaceutical) and patient (e.g., out of pocket expenses) standpoint.
These data indicate that high-value hospitals succeeded in part by minimizing complications, but also had lower professional services spending and differences in component post-acute care utilization among patients without postoperative complications or readmissions. Hospitals engaged in bundled care models may succeed by investing in home health and emergency department services in efforts to avoid readmissions and inpatient rehabilitation. Although not statistically significant (p=0.19), low-value hospitals had a higher proportion of non-elective operations. While this difference may reflect differences in disease severity, clinical risk-adjustment was performed and it may alternatively indicate better patient selection and preoperative optimization at high-value hospitals. Succeeding in preoperative preparation and appropriate patient selection may not only result in decreased rates of prolonged hospital stay, prolonged ventilation, and operative mortality, but could also decrease spending for inpatient E&M through fewer postoperative consultations. Additionally, low-value hospitals may have higher E&M payments due likely in part to poor care coordination21 or evaluating patients on a more frequent basis, as has been reported with increased laboratory testing at low- compared to high-ranked medical centers.22
Prior investigators have evaluated value for cardiac surgical patients. The Virginia Cardiac Services Quality Initiative (VCSQI) leveraged clinical data along with risk-adjusted cost-to-charge ratios to identify targets for advancing value. The authors reported a strong positive correlation between risk-adjusted quality (e.g., morbidity and mortality) and risk-adjusted length of stay, but not between risk-adjusted quality and cost measures.15 Similarly, the current study found a higher incidence of prolonged length of stay at low-value hospitals and a mean 2.5-day longer length of stay compared to high-value hospitals. In contrast to the VCSQI analysis, the current study includes specific NQF-defined quality metrics included as part of STS national CABG hospital performance ratings. Additionally, the VCSQI authors did not find a significant association between quality and cost, potentially because they reported cost-to-charge ratios rather than spending. Authors of another recent study used a proprietary accounting tool in conjunction with 10 clinical outcome metrics used to define “perfect care.”14 Similar to the current study, the authors used STS performance metrics, as well as additional metrics deemed more closely tied to cost. However, the analysis was limited to a single center, with uncertain application at other hospitals, whereas the current data were collected from 33 diverse hospitals and as episode payments are more generalizable in assessing reimbursement. In further contrast to the current analysis and similar to the VCSQI analysis15, the authors quantified actual costs to the hospital.14 While cost-to-charge ratios and other measures of hospital cost are informative for hospital operations, incorporating spending by payors is essential to be competitive in value-based bundled reimbursement models, since measures from the BPCI-A and similar models are based on payments received.
Avedis Donabedian defined a hospital’s performance as the byproduct of processes of care, outcomes, and a hospital’s structure.23 Since metrics of process and structure are conceptually important,23 but largely unmeasured,7 most prior assessments of hospital performance have consisted of measuring variation in outcomes,5,7,8 finances (e.g., charges, hospital costs, payments),3,13,24 or both (e.g. “value”).2,14–16,25 In this study, existing metrics reflecting both hospital structure (from the AHA survey) and processes of care (from the STS) were largely similar across categories of hospital value (Table 1), but may inadequately capture these aspects of quality. Important differences were identified in outcomes, with higher rates of prolonged hospital stay, prolonged intubation, and operative mortality at low-value hospitals. In the context of bundled payment models, traditional conceptual models for assessing institutional quality should be broadened to capture the application of learning health system principles to quality improvement cycles in routine practice.26–28 While Donabedian provides a commonly-cited framework for quality, efforts focusing on value will require modifications to Donabedian’s model to include spending. Accordingly, the current study also included analyses of risk-adjusted, price-standardized episode payments rather than hospital charges, cost-to-charge ratios, or other estimates of cost.15,16,24 Episode payments are a better reflection of payers’ and society’s perspective on cost, since they reflect the actual realized cost of the episode of care and are thus more relevant to bundled payments and value-based reimbursement.
Given the importance of spending, one prior analysis of MVC data assessed reimbursement by evaluating variation in episode payments after isolated CABG.3 Sources of variation between the highest and lowest hospital payment quartiles were readmission (35.1% higher), professional (33.9% higher), and post-acute care (29.6%) payments. Subcomponent drivers of payment differences included diagnosis related group distribution, inpatient E&M services, higher utilization of inpatient rehabilitation, and patients with multiple readmissions.3 Similarly, the current study identified inpatient E&M professional payments and post-discharge inpatient rehabilitation payments to be the main drivers of payment variation between hospitals. Importantly, inpatient E&M payments are driven by the duration of a patient’s hospital stay, while inpatient rehabilitation payments are driven by utilization (yes vs. no), since the latter’s payments are based on diagnosis-related group pricing rather than care intensity. However, when indexed by hospital day, inpatient E&M payments were still higher at low-value hospitals both overall and among patients avoiding complications or readmission. These findings may suggest that high-value hospitals are more protocoled in standard care resulting in lower inpatient E&M payments, independent of time spent in the hospital. The present analysis further advances these prior findings by incorporating risk-adjusted clinical outcomes to evaluate value and defining specific targets for succeeding in bundled care reimbursement models, especially among patients without complication or readmission.
After initially introducing mandatory bundled payment models in 2016, CMS announced the voluntary BPCI-A model and enrolled its first cohort in October of 2018.11 Michigan quality improvement collaboratives are uniquely situated to evaluate the BPCI-A in future analyses by linking MSTCVS-QC risk-adjusted clinical data to MVC 90-day episode payments to compare the performance of BPCI-A participants to non-participants. While Michigan includes a diverse set of geographies and practice environments to analyze, a similar nationwide analysis of Medicare patients could be performed by linking STS clinical data to Medicare claims. These future data could further highlight specific strategies for success in BPCI-A and other value-based payment models.
CONCLUSIONS
In conclusion, high-value hospitals’ performance was driven by avoiding prolonged length of stay, prolonged intubation, and operative mortality, in conjunction with achieving lower episode spending in all areas. Among patients who avoided complications or readmissions at high-value hospitals, lower spending was driven by professional payments, but not index hospitalization, post-acute care, or readmission payments. These findings may reflect a higher proportion of elective operations performed at high-value centers, with improved postoperative care leading to fewer complications and lower spending. These data identify specific clinical outcomes and sources of modifiable payment variation which may inform approaches to bundled payments and value-based reimbursement for hospitals and payors.
Supplementary Material
What is Known:
Extensive variation in the quality of CABG care has prompted the establishment of quality measures through the Society of Thoracic Surgeons and National Quality Forum.
Sources of variation in 90-day episode payments for isolated coronary artery bypass grafting (CABG) include readmission, professional, and post-acute care payments.
What the Study Adds:
This study adds specific targets for succeeding in bundled care reimbursement models by incorporating both risk-adjusted clinical outcomes and risk-adjusted, price-standardized 90-day episode payments to assess value (i.e., quality/spending).
High-value hospitals’ performance in Michigan was driven by avoiding prolonged length of stay, prolonged intubation, and operative mortality, in conjunction with achieving lower episode spending in all areas.
Patients who avoided complications or readmissions at high-value hospitals had lower inpatient evaluation and management spending and lower utilization of inpatient rehabilitation, but higher utilization of home health and emergency department services.
Acknowledgments
SOURCES OF FUNDING
AAB is supported by the National Research Service Award postdoctoral fellowship (No. 5T32HL076123). Support for the Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative (MSTCVS-QC) and the Michigan Value Collaborative (MVC) is provided by the BCBSM and Blue Care Network as part of the BCBSM Value Partnerships program. Although BCBSM works collaboratively with MSTCVS-QC and MVC, the opinions, beliefs and viewpoints expressed by the author do not necessarily reflect the opinions, beliefs and viewpoints of BCBSM or any of its employees.
DISCLOSURES
DSL, ECN, JDS, MPT, and SER receive partial salary support from Blue Cross Blue Shield of Michigan (BCBSM). Data from the MVC was obtained through data use agreement RSCH-2014-26142.
DSL receives research funding from the Agency for Healthcare Research and Quality (R01HS026003 AHRQ) and National Institutes of Health (1R01HL146619-01A1 REVISED) and serves as a consultant for the American Society of Extracorporeal Technology. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health or the Agency for Healthcare Research and Quality.
REFERENCES
- 1.D’Agostino RS, Jacobs JP, Badhwar V, Fernandez FG, Paone G, Wormuth DW, Shahian DM. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2019 Update on Outcomes and Quality. Ann Thorac Surg. 2019;107:24–32. [DOI] [PubMed] [Google Scholar]
- 2.Thompson MP, Cabrera L, Strobel RJ, Harrington SD, Zhang M, Wu X, Prager RL, Likosky DS. Association Between Postoperative Pneumonia and 90-Day Episode Payments and Outcomes Among Medicare Beneficiaries Undergoing Cardiac Surgery. Circ Cardiovasc Qual Outcomes. 2018;11:e004818. [DOI] [PubMed] [Google Scholar]
- 3.Guduguntla V, Syrjamaki JD, Ellimoottil C, Miller DC, Prager RL, Norton EC, Theurer P, Likosky DS, Dupree JM. Drivers of Payment Variation in 90-Day Coronary Artery Bypass Grafting Episodes. JAMA Surg. 2018;153:14–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368–1375. [DOI] [PubMed] [Google Scholar]
- 5.Shih T, Zhang M, Kommareddi M, Boeve TJ, Harrington SD, Holmes RJ, Roth G, Theurer PF, Prager RL, Likosky DS; Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative. Center-Level Variation in Infection Rates After Coronary Artery Bypass Grafting. Circ Cardiovasc Qual Outcomes. 2014;7:567–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Likosky DS, Wallace AS, Prager RL, Jacobs JP, Zhang M, Harrington SD, Saha-Chaudhuri P, Theurer PF, Fishstrom A, Dokholyan RS, Shahian DM, Rankin JS; Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative. Sources of Variation in Hospital-Level Infection Rates After Coronary Artery Bypass Grafting: An Analysis of The Society of Thoracic Surgeons Adult Heart Surgery Database. Ann Thorac Surg. 2015;100:1570–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brescia AA, Rankin JS, Cur DD, Jacobs JP, Prager RL, Zhang M, Matsouaka RA, Harrington SD, Dokholyan RS, Bolling SF, Fishstrom A, Pasquali SK, Shahian DM, Likosky DS; Michigan Society of Thoracic and Cardiovascular Surgeons Quality Collaborative. Determinants of Variation in Pneumonia Rates After Coronary Artery Bypass Grafting. Ann Thorac Surg. 2018;105:513–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez AA, Dimick JB, Birkmeyer JD, Ghaferi AA. Understanding the volume-outcome effect in cardiovascular surgery: the role of failure to rescue. JAMA Surg. 2014;149:119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edwards FH, Ferraris VA, Kurlansky PA, Lobdell KW, He X, O’Brien SM, Furnary AP, Rankin JS, Vassileva CM, Fazzalari FL, Magee MJ, Badhwar V, Xian Y, Jacobs JP, Wyler von Ballmoos MC, Shahian DM. Failure to Rescue Rates After Coronary Artery Bypass Grafting: An Analysis From The Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg. 2016;102:458–464. [DOI] [PubMed] [Google Scholar]
- 10.Performance Measure Descriptions | STS. https://www.sts.org/quality-safety/performance-measures/descriptions. Accessed August 22, 2019.
- 11.BPCI Advance | Center for Medicare & Medicaid Innovation. https://innovation.cms.gov/initiatives/bpci-advanced. Accessed August 19, 2019.
- 12.Fry BT, Smith ME, Thumma JR, Ghaferi AA, Dimick JB. Ten-year Trends in Surgical Mortality, Complications, and Failure to Rescue in Medicare Beneficiaries. Ann Surg. 2020;271:855–861. [DOI] [PubMed] [Google Scholar]
- 13.Brescia AA, Syrjamaki JD, Regenbogen SE, Paone G, Pruitt AL, Shannon FL, Boeve TJ, Patel HJ, Thompson MP, Theurer PF, Dupree JM, Kim KM, Prager RL, Likosky DS. Transcatheter Versus Surgical Aortic Valve Replacement Episode Payments and Relationship to Case Volume. Ann Thorac Surg. 2018;106:1735–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glotzbach JP, Sharma V, Tonna JE, Pettit JC, McKellar SH, Eckhauser AW, Varghese TK Jr, Selzman CH. Value-driven cardiac surgery: Achieving “perfect care” after coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2018;156:1436–1448.e2. [DOI] [PubMed] [Google Scholar]
- 15.Osnabrugge RL, Speir AM, Head SJ, Jones PG, Ailawadi G, Fonner CE, Fonner E Jr, Kappetein AP, Rich JB. Cost, quality, and value in coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2014;148:2729–2735.e1. [DOI] [PubMed] [Google Scholar]
- 16.Yount KW, Isbell JM, Lichtendahl C, Dietch Z, Ailawadi G, Kron IL, Kern JA, Lau CL. Bundled Payments in Cardiac Surgery: Is Risk Adjustment Sufficient to Make It Feasible? Ann Thorac Surg. 2015;100:1646–1652; discussion 1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ellimoottil C, Syrjamaki JD, Voit B, Guduguntla V, Miller DC, Dupree JM. Validation of a claims-based algorithm to characterize episodes of care. Am J Manag Care. 2017;23:e382–e386. [PubMed] [Google Scholar]
- 18.Merit-Based Incentive Payment System Reporting | STS. https://www.sts.org/registries-research-center/sts-national-database/mips-reporting. Accessed August 22, 2019.
- 19.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010;45:1783–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices Don’t Drive Regional Medicare Spending Variations. Health Aff (Millwood). 2010;29:537–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baicker K and Chandra A. The Productivity of Physician Specialization: Evidence from the Medicare Program. American Economic Review. 2004;94:357–361. [DOI] [PubMed] [Google Scholar]
- 22.Doyle JJ, Ewer SM, Wagner WH. Returns to physician human capital: evidence from patients randomized to physician teams. J Health Econ. 2010;29:866–82. [DOI] [PubMed] [Google Scholar]
- 23.Donabedian A The Quality of Care: How Can It Be Assessed? JAMA. 1988;260:1743–1748. [DOI] [PubMed] [Google Scholar]
- 24.Kilic A, Shah AS, Conte JV, Mandal K, Baumgartner WA, Cameron DE, Whitman GJ. Understanding variability in hospital-specific costs of coronary artery bypass grafting represents an opportunity for standardizing care and improving resource use. J Thorac Cardiovasc Surg. 2014;147:109–115. [DOI] [PubMed] [Google Scholar]
- 25.Mehaffey JH, Hawkins RB, Byler M, Charles EJ, Fonner C, Kron I, Quader M, Speir A, Rich J, Ailawadi G; Virginia Cardiac Services Quality Initiative. Cost of individual complications following coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2018;155:875–882.e1. [DOI] [PubMed] [Google Scholar]
- 26.Learning Health Systems. Accessed May 15, 2020. Agency for Healthcare Research and Quality, Rockville, MD. Available at: https://www.ahrq.gov/learning-health-systems/index.html. [Google Scholar]
- 27.Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector; Board on Health Sciences Policy; Board on the Health of Select Populations; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine, Berwick D, Downey A, Cornett E. A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. Mil Med. 2017;182:1563–1565.29087893 [Google Scholar]
- 28.SCOAP Collaborative, Writing Group for the SCOAP Collaborative, Kwon S, Florence M, Grigas P, Horton M, Horvath K, Johnsson M, Jurkovich G, Klamp W, Peterson K, Quigley T, Raum W, Rogers T, Thirlby R, Farrokhi ET, Flum DR. Creating a learning healthcare system in surgery: Washington State’s Surgical Care and Outcomes Assessment Program (SCOAP) at 5 years. Surgery. 2012;151:146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.