Abstract
Mucosal fenestration is a rare entity wherein apex of the tooth is exposed in the oral cavity due to breakdown of the overlying bone and mucosa. This leads to accumulation of plaque and if left untreated can hamper the further prognosis of the tooth. Although there are few evidences regarding mucosal fenestrations in posterior region of maxilla, treatment of the same have been challenging for the clinicians. This case report describes the management of mucosal fenestrations in the posterior maxilla by regenerative periodontal flap surgical approach using xenograft (Osseograft) and platelet-rich fibrin membrane.
Keywords: Apicoectomy, mucosal fenestration, platelet-rich fibrin, regenerative therapy
INTRODUCTION
Alveolar dehiscence is the denuded area extending through the marginal bone while fenestration is the isolated area in which the root surfaces are denuded of bone and the root surface is covered only by periosteum and overlying gingiva.[1] Another defect encountered is a mucosal fenestration, wherein apex of the tooth is exposed in the oral cavity due to breakdown of the overlying bone and mucosa. Although this is a rare phenomenon, very few evidences have been reported and treatment of the same have been challenging for the clinicians.
Etiology for this type of defects are attributed to occlusal trauma, root-bone angulation, root prominences, inadequate soft tissue thickness, pulpal–periradicular diseases, abnormal frenum attachment, or orthodontic tooth movement.[2,3,4] Literature search has reported mostly the management of mucosal fenestration in anterior region, only one case report in posterior region.[3]
Hence, this case report describes the management of mucosal fenestrations in the posterior maxilla by regenerative approach using xenograft (Osseograft) and platelet-rich fibrin (PRF) membrane.
CASE REPORT
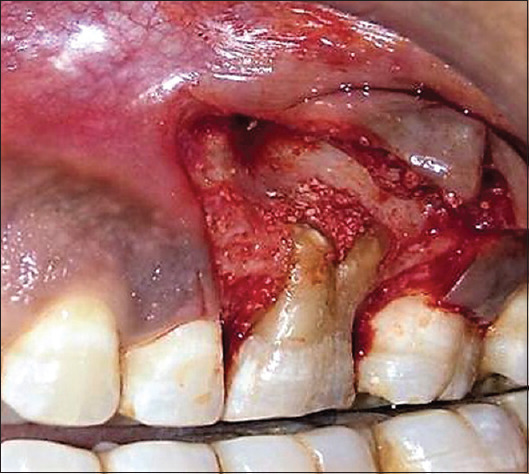
A 27-year-old male patient presented with chief complaint of food lodgment in the upper left posterior teeth region with no history of pain. On clinical examination, 26 had deep occlusal caries and were asymptomatic to horizontal and vertical percussion. Clinically, there was Miller's Class I gingival recession on the buccal surface and two widely apart placed mucosal fenestration measuring about 3mm exposing the apical one-third of mesiobuccal and distobuccal roots in the vestibule [Figure 1]. No evident probing depth, no furcation involvement, and mobility was found. An intraoral radiograph revealed periapical radiolucency and bone loss with palatal root; pulp test showed tooth to be nonvital [Figure 2] suggestive of apical periodontitis with pulpal necrosis and no periodontal involvement. Hence, the diagnosis was primary endodontic lesion according to classification given by Simon et al.[5] and mucosal fenestration with 26. Histobacteriological analysis of root apices exposed to oral cavity through mucosal fenestration revealed extensive resorptive defects on root apices filled with thick bacterial biofilm, irregular detachment of the cementum layers with consequent infection of underlying spaces, and heavy infection in the apical foramina; soft tissue specimen exhibited no or minimal inflammation.[6] Treatment plan for managing these mucosal fenestration was to carry out root canal therapy, periodontal flap surgery, and apicoectomy of mesiobuccal and distobuccal roots with MTA sealing of the apices and not the palatal root as it is not exposed to oral cavity then followed by regenerative procedure using bone graft and PRF membrane.
Figure 1.
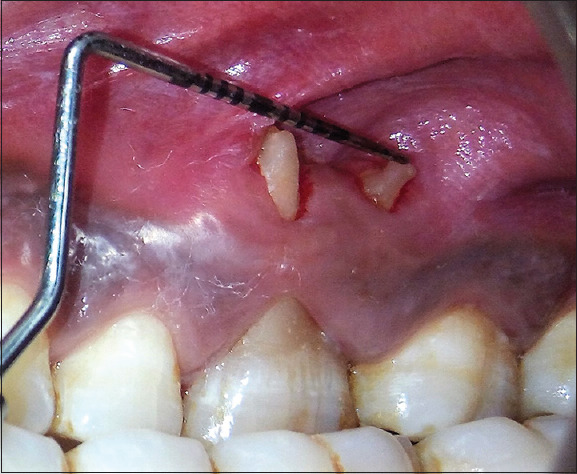
Preoperative clinical photograph of mucosal fenestration with 26
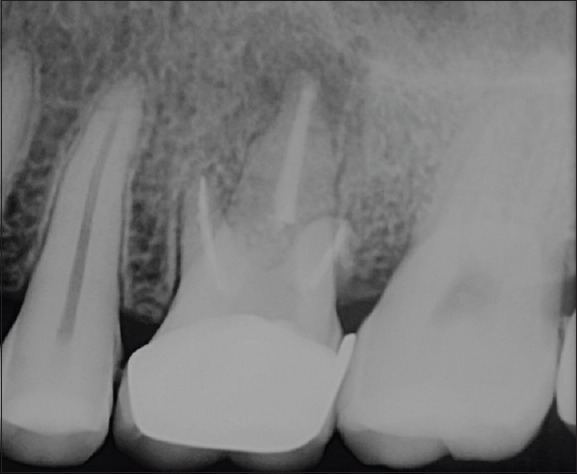
Figure 2.
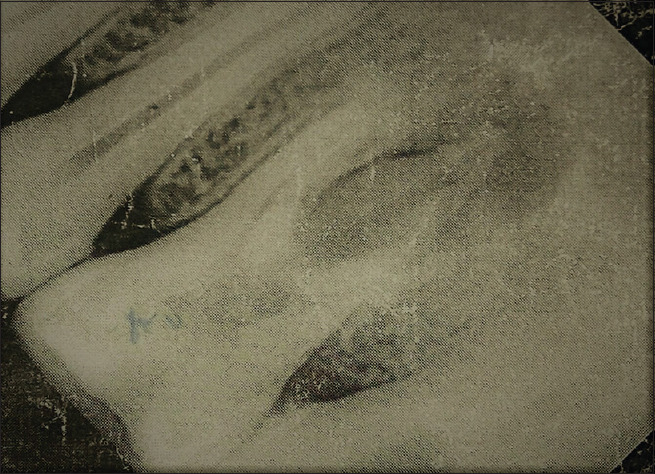
Preoperative radiograph of 26 showing interradicular bone loss
The patient's written consent was obtained and root canal treatment (RCT) was carried out under 2% lignocaine (LIGNOX 2% A, INDOCO REMEDIES LTD) , access opening and biomechanical preparation was done with protaper gold system, intermittent irrigation was performed using 3%NaOCl and saline. Calcium hydroxide was placed as intracanal medicament for 7 days , followed by obturation of canals with gutta-percha by lateral compaction technique. Coronal cavity was restored with resin based composite material.
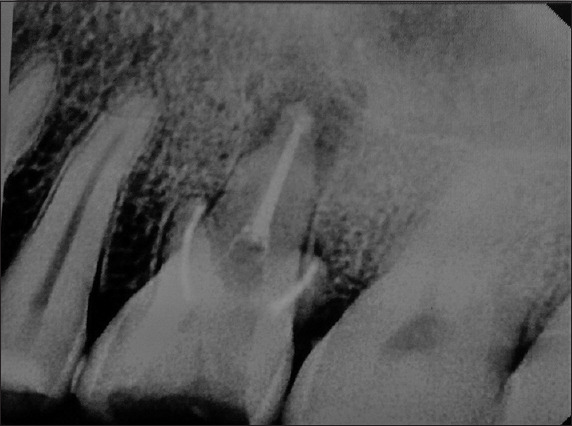
Complex apical intraradicular infection and extraradicular mineralized biofilms can the cause of wet canals and endodontic treatment failure. None of these cases had deep periodontal pockets reaching the apex, and most of them were associated with sinus tracts.[7] In the present case the root apices of mesiobuccal and distobuccal roots were exposed to oral cavity, hence apicoectomy of these two roots were decided and did not wait for three months of healing phase after the RCT [Figure 3].
Figure 3.
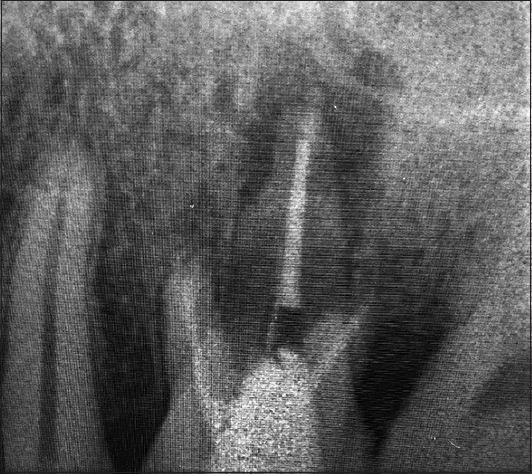
Completed root canal treatment radiograph
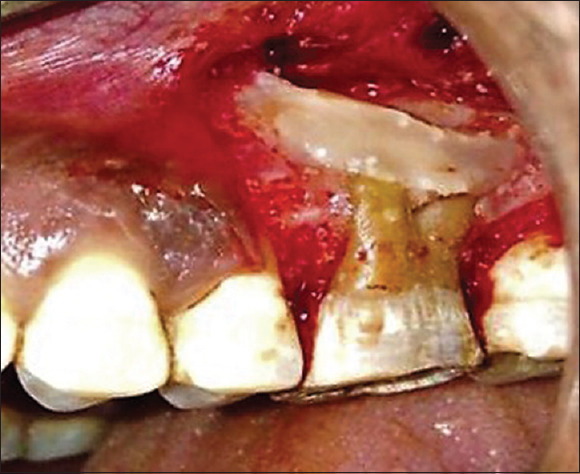
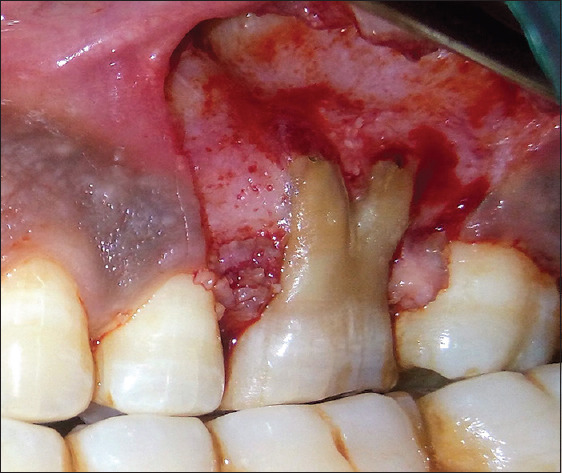
After phase I therapy, surgery was performed under local anesthesia using 2% lignocaine. (Lignox 2% A, Indoco Remedies Ltd). A full-thickness mucoperiosteal flap was reflected beyond mucogingival junction using vertical releasing incisions with number 15 blade [Figure 4]. After flap reflection, loss of cortical plate was evident exposing mesiobuccal, distobuccal roots, and interradicular area with 26. Apicoectomy was performed with both the roots till the healthy surrounding bone was appreciated [Figure 5]. Following this, all the granulation tissue was debrided from the defect. Gutta-percha from both mesiobuccal and distobuccal roots was then removed using H-file and root preparation was carried using K-file. Whole root length was sealed using root repair cement mineral trioxide aggregate (MTA). MTA is biocompatible, capable of stimulating healing, osteogenesis, hydrophilic, and has been shown in dye and bacterial leakage studies to be superior to that of amalgam and zinc oxide cement reinforced with ethoxy benzoic acid (Super-EBA). A xenogenic bone graft (Osseograft, Advance Biotech Products (P) Ltd) was then placed in the defect [Figure 6].
Figure 4.

Root end resected and presence of bone defect with 26
Figure 5.
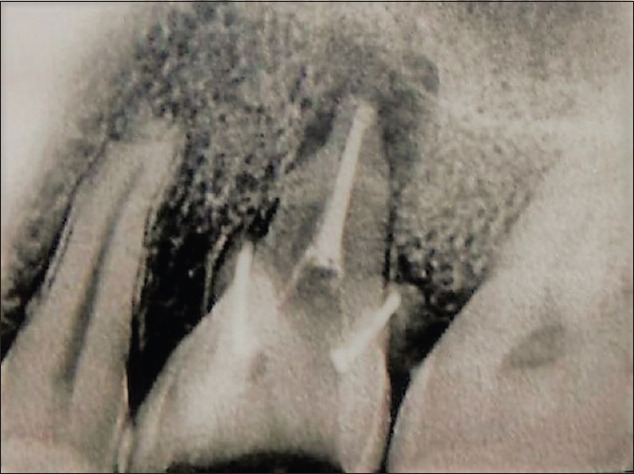
Radiograph after root-end resection and periapical lesion with palatal root of 26
Figure 6.
Xenograft (Osseograft) placed in the defect with 26
A biological PRF was prepared by collecting 10 ml of the blood sample into a vacutainers. This was prepared by centrifugation at 3000 rpm for 10 min, removed, and then squeezed in-between sterile gauze pieces to form a membrane and adapted over the bone graft [Figure 7]. The surgical flap was sutured with sling suture using 4-0 Mersilk (Johnson and Johnson Pvt. Ltd) and the vertical releasing incisions by simple interrupted sutures [Figure 8]. A periodontal dressing (Coe-pack; GC America, USA) was placed, and antibiotics and analgesics (amoxicillin 500 mg thrice a day for 5 days and diclofenac sodium twice a day for 3 days) were prescribed to the patient for less postoperative discomfort and infection. Furthermore, instructions were given for the use of 0.2% chlorhexidine mouth (Hexidine, ICPA Health Products Ltd) for 2 weeks, twice daily for oral hygiene maintenance followed by another one week after suture removal. Sutures were removed 2 weeks postoperatively and wound healing was uneventful. The patient was instructed to maintain proper oral hygiene and was followed at 3 and 6 months [Figure 9]. At the 6-month follow-up visit, radiograph showed bone fill, increase in recession as compared to preoperatively and clinically complete resolution of mucosal fenestration [Figures 10 and 11]. First phase of treatment was aimed only to treat mucosal fenestration and regeneration of endodontic defect; so, at the second phase of treatment, decision was taken for an attempt for complete root coverage using PRF membrane with coronally advanced flap with patient's consent. Interradicular defect fill was seen during root coverage procedure [Figure 11]. Following this, attempt was made for the complete root coverage using PRF membrane, although corrections of root prominences were carried out before flap advancement [Figure 12]. There was no complete root coverage at the end of 3 months of root coverage procedure, but there was increase in gingival tissue thickness [Figure 13]. At 9-month follow-up, 26 was restored with porcelain fused to metal crown [Figure 14]. The patient was further recalled till 14 months for follow-up to evaluate resolution of palatal root lesion with 26 [Figure 15].
Figure 7.
Platelet rich fibrin membrane placed over bone graft with 26
Figure 8.

Clinical photograph after suturing
Figure 9.
Radiograph of 26 at 6 months postoperative
Figure 10.

Postoperative photograph at 6 months showing complete resolution of mucosal fenestrations
Figure 11.
Interradicular defect fill seen during root coverage procedure
Figure 12.

Coronally advanced flap with sutures in place
Figure 13.

Postoperative photograph at 3 months after coronal flap advancement
Figure 14.

At 9-month follow-up with final prosthesis
Figure 15.
Radiograph at 14-month follow-up showing complete resolution of the palatal root lesion with 26
DISCUSSION
Mucosal fenestration is a rare pathologic condition usually seen during daily clinical practice. If these conditions are left untreated, it can affect the prognosis of the involved tooth. In this condition, the root apex is exposed to the oral environment making it more prone for plaque accumulation and can result in the inflammation of the surrounding tissue and bone destruction.
The literature review has shown that the prevalence of apical fenestration is between 7.5% and 20% and highest in the maxillary than in the mandibular teeth.[8] It is found to be most evident in the anterior teeth, i.e., central, lateral incisors and in the prominent teeth like cuspids than that of posterior teeth. In the abovediscussed case report, the fenestration was evident with first molar in the maxillary left posterior region.
For the treatment of same, a clinician should delineate the cause and accordingly treat the condition. Although mucosal fenestrations are very less prevalent, various treatment modalities have been suggested in the literature. These procedures include lateral pedicle flap, mucogingival envelope flap technique along with guided tissue regeneration and membranes, use of subepithelial connective tissue, free gingival graft, and apicoectomy with the endodontic surgical procedures with successful treatment outcomes.[2,4]
No mobility was seen with 26, therefore the decision was to treat mucosal fenestration instead of extraction of the tooth and implant placement. In the present case, treatment was carried out by reflecting a full thickness mucoperiosteal flap along with resection of root ends to contain the roots into the alveolar housing and orthograde filling with MTA to seal root canal system. Bone graft and a biological PRF membrane were placed to regenerate the furcation defect and for healing of mucosal fenestrations.
PRF membrane was used because of its ability for hard and soft tissue regeneration which was due to release of various growth factors such as platelet-derived factor, transforming growth factor-b, vascular endothelial growth factor, and epidermal growth factor and cytokines.[9,10]
In 1983, Sawes and Barnes got successful results at 6 weeks postoperatively for the buccal fenestrations in the maxillary right first molar by performing apicoectomy using full-thickness mucoperiosteal flap.[3] In the present case, the healing mucosal fenestrations was seen at 2 weeks; this may be because of accelerated soft tissue healing by PRF. Whereas, Chen et al. in 2009 managed two cases with similar type of defects by performing apicoectomy and covering with the use of subepithelial connective tissue graft with successful treatment outcome 1 year postoperatively.[2] Singh et al. in 2013 managed the case of mucosal fenestration in the maxillary central incisor with the use of autogenousfree gingival graft with successful outcome 6 months postoperatively [Figure 4].[4] Treatment of mucosal fenestration with connective tissue graft or free gingival graft need second surgical site for the grafts where there is a certain degree of discomfort, and an increased risk of postoperative complications, such as pain and hemorrhage, limited availability of graft material from donor site, in contrast treatment with PRF is minimally invasive.[11] Jha et al. in 2018 got successful results by managing their case with the use of PRF and tetracycline fibers for the complete healing of the bone defects. In the present case, the results were similar with the use of PRF.[12]
26 had furcation lesion without marginal periodontium and can be classified as Class IIIa lesion according to Classification of membrane application in endodontic surgery by von Arx and Cochran.[13] Based on the clinical success of guided tissue regeneration (GTR) and guided bone regeneration, it became obvious to use the same principle in endodontic surgery, where the ultimate goal is regeneration of periradicular tissues including cementum, periodontal ligament, and alveolar bone. The objectives of membrane application in endodontic surgery resemble those in periodontology and implantology: (1) facilitate tissue regeneration by creating an optimum environment (stable and protected wound); and (2) exclude nondesired fast-proliferating cells that interfere with desired tissue regeneration.[13] PRF has a great potential for bone and soft tissue regeneration, because of growth factors it accelerates the process of angiogenesis and stimulation to proliferate and differentiate osteoblasts. Though the normal PRF has rapid degradability (1-2 weeks),[7] It can serve as GTR membrane in initial period of wound healing. It can serve as GTR membrane in initial period of wound healing. PRF as GTR was employed in the present case for the abovementioned objectives. Effect of PRF on healing of the endodontic defect was appreciated,[14] also on mucosal fenestration healing.
CONCLUSION
Mucosal fenestration in the posterior region is rare; such type of defect can be effectively managed with apicoectomy combined with regenerative approach using PRF and bone graft for long-term prognosis of the tooth.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Carranza FA, Bernard GW, Newman MG, Takei HH, Carranza FA, editors. Carranza's Clinical Periodontology. Philadelphia: W.B. Saunders Co.; 2002. The tooth supporting structures; pp. 36–57. [Google Scholar]
- 2.Chen G, Fang CT, Tong C. The management of mucosal fenestration: A report of two cases. Int Endod J. 2009;42:156–64. doi: 10.1111/j.1365-2591.2008.01463.x. [DOI] [PubMed] [Google Scholar]
- 3.Sawes WL, Barnes IE. The surgical treatment of fenestrated buccal roots of an upper molar: A case report. Int Endod J. 1983;16:82–6. doi: 10.1111/j.1365-2591.1983.tb01301.x. [DOI] [PubMed] [Google Scholar]
- 4.Singh S, Panwar M, Arora V. Management of mucosal fenestration by multidisciplinary approach: A rare case report. Med J Armed Forces India. 2013;69:86–9. doi: 10.1016/j.mjafi.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simon JH, Glick DH, Frank AL. The relationship of endodontic-periodontic lesions. J Periodontol. 1972;43:202–8. doi: 10.1902/jop.1972.43.4.202. [DOI] [PubMed] [Google Scholar]
- 6.Ricucci D, Siqueira JF, Jr, Loghin S, Grosso A, Valois EM, Leal AS, et al. Management and histobacteriological findings of mucosal fenestration: A report of 2 cases. J Endod. 2018;44:1583–92. doi: 10.1016/j.joen.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Ricucci D, Candeiro GT, Bugea C, Siqueira JF., Jr Complex apical intraradicular infection and extraradicular mineralized biofilms as the cause of wet canals and treatment failure: Report of 2 cases. J Endod. 2016;42:509–15. doi: 10.1016/j.joen.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 8.Carranza FA, Camargo PM, Takei HH, Newman M, Takei H, Klokkevold P, Carranza F, editors. Carranza's Clinical Periodontology. 11th ed. St. Louis, MO: Elsevier Saunders; 2012. Bone loss and patterns of bone destruction; pp. 140–50. [Google Scholar]
- 9.Preeja C, Arun S. Platelet-rich fibrin: Its role in periodontal regeneration. Saudi J Dent Res. 2014;5:117–22. [Google Scholar]
- 10.Agrawal M, Agrawal V. Platelet rich fibrin and its applications in dentistry – A review article. Natl J Med Dent Res. 2014;2:51–8. [Google Scholar]
- 11.Mufti S, Dadawala SM, Patel P, Shah M, Dave DH. Comparative evaluation of platelet-rich fibrin with connective tissue grafts in the treatment of Miller's class I gingival recessions. Contemp Clin Dent. 2017;8:531–7. doi: 10.4103/ccd.ccd_325_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jha A, Singh A, Sarmah S, Adinarayana R. Management of mucosal fenestration using PRF and tetracycline fibres: A case report. Int J Innov Res Adv Stud. 2018;5:95–9. [Google Scholar]
- 13.von Arx T, Cochran DL. Rationale for the application of the GTR principle using a barrier membrane in endodontic surgery: A proposal of classification and literature review. Int J Periodontics Restorative Dent. 2001;21:127–39. [PubMed] [Google Scholar]
- 14.Metlerska J, Fagogeni I, Nowicka A. Efficacy of autologous platelet concentrates in regenerative endodontic treatment: A systematic review of human studies. J Endod. (e1) 2019;45:20–30. doi: 10.1016/j.joen.2018.09.003. [DOI] [PubMed] [Google Scholar]


