Abstract
Pyogenic granuloma is a commonly occurring inflammatory hyperplasia involving the oral cavity. Surgical resection of the lesion is the mainstay treatment of pyogenic granuloma. However, intraoperative bleeding, postoperative infection, and recurrence chances are more with the surgical technique. Therefore, sclerotherapy has evolved as an effective alternative approach, which is simple, noninvasive, with minimal discomfort to the patient and having little recurrences and few complications. This case report is an attempt to highlight the usefulness of sclerotherapy procedure in the management of orogingival pyogenic granuloma, particularly involving the anterior esthetic zone of the oral cavity.
Keywords: Gingiva, gingival diseases, granuloma, mouth mucosa, polidocanol, pyogenic granuloma, sclerotherapy, sodium tetradecyl sulfate
INTRODUCTION
Pyogenic granuloma is a common, benign lesion of vascular origin.[1,2] This lesion is neither associated with pus nor histologically resembles a granuloma.[3] They occur at any age and are often stimulated by foreign objects such as calculus or a sharp margin of a restoration.[3,4]
Conservative surgical resection or laser surgical excision of the lesion is the mainstay treatment of pyogenic granuloma, but it often results in recurrence, as they are reactive hyperplasias. In cases where pyogenic granuloma is large or occurs in a surgically difficult area, choosing an appropriate treatment modality can be difficult.[5] Therefore, sclerotherapy was considered as an alternative and effective treatment modality, as it is a simple and noninvasive procedure with a better safety profile, repeatability, and low cost of treatment even when multiple sessions are needed with low recurrence rate.[1,6] Sclerotherapy with 3% sodium tetradecyl sulfate has been proved to be effective as a conservative approach in the treatment of oral pyogenic granuloma.[1]
This case report is an attempt to emphasize the effectiveness of sclerotherapy (3% of sodium tetradecyl sulfate) in the management of oro-gingival pyogenic granuloma, particularly when the lesion is large and occurs in the anterior esthetic zone of the oral cavity.
CASE REPORT
An 18-year-old female patient reported with a complaint of swelling over the gums in the lower front tooth region that had developed over several months, which caused discomfort while eating. Detailed history revealed that the swelling was painless and initially small in size, which gradually increased to the present size. The patient also stopped brushing in the area due to excessive bleeding from that region while brushing. No relevant drug, dental, medical, and family history was present.
An extraoral examination showed no significant findings. Intraoral examination revealed a large sessile lobulated gingival overgrowth, appeared irregular in shape, measuring approximately 18 mm × 12 mm in dimensions, extending on buccal surfaces of 41, 42, 31, 32, and 33. It was reddish pink in color, having a smooth overlying surface with no ulcerations. The oral hygiene of the patient was poor, with large plaque deposits on the buccal surfaces of the involved teeth [Figure 1]. On palpating the lesion, it was firm, nontender, and bleeds on manipulation. Based on the above clinical findings, a provisional diagnosis of gingival pyogenic granuloma was considered. Teeth associated with it showed grade I mobility. Radiographic evaluation was also done to rule out any bony involvement, which showed no significant findings, except for the mild amount of bone loss associated with both central incisors. Complete blood count was found to be within the normal limits.
Figure 1.

Pretreatment intraoral picture of the patient showing extensive lobulated gingival overgrowth, involving the buccal surfaces of mandibular anterior teeth with large calculus deposits
As the lesion was large and develops in an esthetic zone, it is difficult to choose an appropriate treatment modality. Surgical excisions of the lesion can apparently have relatively high chances of recurrence, and also there were chances of losing the anterior teeth; treatment with a laser was also inappropriate, as the lesion was thick. The patient has been informed about the various treatment options and their pros and cons. However, the patient was not willing to go for surgical treatment due to esthetic concern. Therefore, with patient consent, we chose sclerotherapy as a management approach in this case. The patient first underwent oral hygiene instructions and motivated to ensure optimal plaque control. At first, complete oral prophylaxis was done to remove the causative local factors, followed by local application of ornidazole (1.0%w/w) and chlorhexidine gluconate (0.25% w/w) gel [Ointment Ornigreat Gel; Mankind Pharma Ltd.] and metronidazole gel (1% w/w) (Ointment Metrohex Gel; Dr. Reddy's Lab. Ltd.) on an alternate basis twice a day [Figure 2]. Improvement in gingival health was noted during the reassessment [Figure 3]. After 2 weeks, the sclerotherapy procedure was planned. At first, surface local anesthesia was applied over the lesion. Then, 0.2–0.5 mL of 3% sodium tetradecyl sulfate (Setrol) [Figure 4] was slowly injected into the base of the lesion by insulin syringe (0.3 mm × 8 mm size, 31G) until the solution gets leaked out from the surface of the lesion [Figure 5]. Patients were examined at weekly intervals up to 1 month to evaluate the response until the lesions reduced in size, and accordingly, the second, third, and fourth injections were planned and given at weekly intervals [Figure 6]. After 4 weeks of follow-up, the lesion was significantly regressed in size and extent [Figure 7].
Figure 2.
(a) Complete oral prophylaxis procedure to remove the local irritants, (b) immediately after prophylaxis, (c) thorough irrigation with betadiene
Figure 3.

Follow-up visit after 1 week postprophylaxis showing improvement in the gingival condition
Figure 4.

Three percent sodium tetradecyl sulfate (Setrol)
Figure 5.
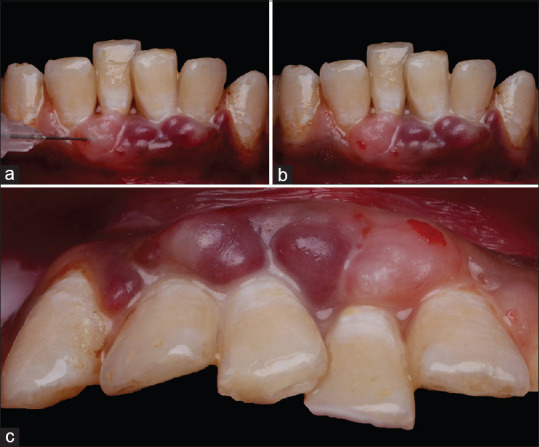
Sclerotherapy procedure (a) Slow injection of 0.2–0.5 mL of 3% sodium tetradecyl sulfate solution into the base of the lesion by insulin syringe, (b) Note the multiple sites of injection administration, (c) Occlusal view showing leaking of solution from the surface of the lesion
Figure 6.
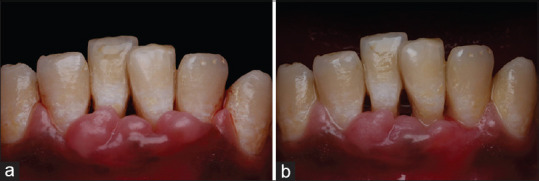
Follow-up visit postsclerotherapy (a) after 1 week; (b) after 3 weeks, showing progressive improvement in the gingival health condition
Figure 7.

Follow-up visit postsclerotherapy after 4th week. Significant reduction in size and extent of the lesion noted
The patient was recalled every 3rd month for maintenance and to check for possible recurrence. This case was followed up for a period of 1 year, and there has been no recurrence so far [Figure 8].
Figure 8.

Follow-up visit after 1 year showing healthy gingiva with no recurrence of the lesion
DISCUSSION
Pyogenic granuloma is a common, nonneoplastic reactive lesion of the oral cavity. Its incidence has been reported as 26.8%–32% of all reactive lesions with age ranging from 11 to 40 years. Females are predominantly affected with a predilection of 3:2 over males.[1,4] Clinically, pyogenic granuloma presents as a red-purple nodule usually found arising from the interdental gingiva.[1] The young lesions are highly vascular, often elevated and ulcerated, and bleed easily, whereas older lesions tend to be more collagenized and pink in appearance.[7] In our case also, the patient was an 18-year-old female having lesion involving the mandibular anterior gingiva for a long period of time that becomes more reddish pink and thicker in appearance with no associated pain or any altered sensation.
Local irritants, such as calculus, poor oral hygiene, certain drugs, and hormonal factors, are considered as probable factors in causation.[8] In the present case also, poor oral hygiene with a huge calculus deposit was the major irritant factor in causing such lesions.
The management of pyogenic granuloma depends on the clinical scenario. For smaller lesions, removal of the causative irritants, keen clinical observation, and regular follow-up may be considered as a suggestive treatment.[9] However, larger lesions can be managed by conservative surgical resection or laser excision, but invasive resection of the extensive lesion may sometimes involve the removal of the seriously loose tooth,[10] while laser excision is apparently inappropriate for a thicker lesion.[6] Several recent studies showed that the sclerotherapy should be considered as an effective alternative treatment approach for surgery in case of oral pyogenic granuloma, especially when the lesion was large in dimension, thicker in nature, and develops in a surgically difficult/inaccessible area. Samatha et al.,[4] in their study, presented a case series on oral pyogenic granulomas wherein four cases showed complete resolution and one fibrosed on treating with a sclerosing agent. Khaitan et al.,[1] also in their study, successfully treated 40 cases of pyogenic granuloma after 1–4 consecutive shots of a sclerosing agent in a weekly interval. Further study by Shah and Ranghani[6] on 15 clinically diagnosed cases of oral pyogenic granuloma (8 cases) and mucocele (7 Cases) showed complete regression of the lesion after 1–3 consecutive injections of a sclerosing agent (0.5–1 mL of polidocanol) in a weekly interval. It was important to note that none of the studies mentioned its indication in the anterior esthetic zone of the oral cavity. In our case, we had chosen sclerotherapy as a mode of treatment, because the lesion was large in size and also involves an anterior esthetic zone of the oral cavity.
Sclerotherapy is defined as the targeted elimination of small vessels and vascular anomalies by the injection of a sclerosant.[6] These are tissue irritants causing vascular thrombosis and permanent damage to the endothelial vessels resulting in endofibrosis and vascular obliteration when injected into or adjacent to blood vessels.[11] The most commonly used sclerosants are polidocanol, sodium tetradecyl sulfate, sodium morrhuate, sodium sylliate, pingyangmycin, OK-432, ethanolamine oleate, and ethanol. Sodium tetradecyl sulfate composed of sodium 1-isobutyl-4-echyloctyl sulfate plus benzoyl alcohol 2% (as an anesthetic agent). It is a synthetic, surface-active substance which is phosphate buffered to pH 7.6. It is a long-chain fatty acid salt of an alkaline metal with properties of soap. The solution is clear and nonviscous with low surface tension and is readily miscible with blood.[12] About 3% of sodium tetradecyl sulfate (60 mg/2 mL), an anionic surfactant, was used as a sclerosant in this case study, which has been proved very effective.
The advantages of sclerotherapy are that it is a simple, safe, effective, minimally invasive procedure, with little discomfort to the patient and few complications, compared to surgery. There are negligible blood loss and no requirement for any postoperative dressing or specific care.[1,13] In this case study also, no postoperative complications were observed, except for local discomfort and mild bleeding which resolved within an hour.
CONCLUSION
In summary, it appears reasonable to conclude that an appropriate management protocol should be followed in a patient with pyogenic granuloma to prevent further bone loss and to maintain the structural integrity of the dento-alveolo-mucosal structure. Sclerotherapy is proven to be a valid treatment option with significant clinical benefits in a patient with oral pyogenic granuloma. The present clinical case report is an attempt to speculate sclerotherapy as an effective alternative treatment approach for surgery, especially when the lesion was involving an anterior esthetic zone of the oral cavity, and thereby, widen the spectrum of indication of sclerotherapy for managing oral pyogenic granuloma. We hope that this clinical case study may serve as a guide for further future case studies with a larger representative sample to confirm our findings and to justify an evidence-based management protocol.
Consent
Written informed consent was obtained from the patient for publication of this case report.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Khaitan T, Sinha R, Sarkar S, Kabiraj A, Ramani D, Sharma M. Conservative approach in the management of oral pyogenic granuloma by sclerotherapy. J Indian Acad Oral Med Radiol. 2018;30:46–51. [Google Scholar]
- 2.Hamdoun R, Ennibi OK, Amine C. Pyogenic granuloma of the gingiva: A case report. Int J Cont Med Res. 2018;5:K1–3. [Google Scholar]
- 3.Eversole LR, Greenberg MS, Glick M, editors. Burket's Oral Medicine: Diagnosis and Treatment. 10th ed. Hamilton, Ontario: BC Decker Inc; 2003. Benign tumours of the oral cavity; pp. 141–2. [Google Scholar]
- 4.Samatha Y, Reddy TH, Jyothirrmai K, Ravikiran A, Sankar AJ. Management of oral pyogenic granuloma with sodium tetra decyl sulphate.a case series. N Y State Dent J. 2013;79:55–7. [PubMed] [Google Scholar]
- 5.Rahman H, Hadiuzzaman M. Pyogenic granuloma successfully cured by sclerotherapy: a case report. J Pak Assoc Dermatol. 2014;24:361–4. [Google Scholar]
- 6.Shah JS, Ranghani AF. Sclerotherapy in pyogenic granuloma and mucocele. J Indian Acad Oral Med Radiol. 2018;30:230–4. [Google Scholar]
- 7.Kashyap B, Reddy PS, Nalini P. Reactive lesions of oral cavity: A survey of 100 cases in Eluru, West Godavari district. Contemp Clin Dent. 2012;3:294–7. doi: 10.4103/0976-237X.103621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gomes SR, Shakir QJ, Thaker PV, Tavadia JK. Pyogenic granuloma of the gingiva: A misnomer.-A case report and review of literature? J Indian Soc Periodontol. 2013;17:514–9. doi: 10.4103/0972-124X.118327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cai Y, Sun R, He KF, Zhao YF, Zhao JH. Sclerotherapy for the recurrent granulomatous epulis with pingyangmycin. Med Oral Patol Oral Cir Bucal. 2017;22:e214–18. doi: 10.4317/medoral.21422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: A review. J Oral Sci. 2006;48:167–75. doi: 10.2334/josnusd.48.167. [DOI] [PubMed] [Google Scholar]
- 11.Croffie J, Somogyi L, Chuttani R, DiSario J, Liu J, et al. Technology Assessment Committee. Sclerosing agents for use in GI endoscopy. Gastrointest Endosc. 2007;66:1–6. doi: 10.1016/j.gie.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 12.Leach BC, Goldman MP. Comparative trial between sodium tetradecyl sulphate and glycerin in the treatment of telangiectatic leg veins. Dermatologic Surg. 2003;29:612–5. doi: 10.1046/j.1524-4725.2003.29148.x. [DOI] [PubMed] [Google Scholar]
- 13.Reddy GS, Reddy GV, Reddy KS, Priyadarshini BS, Sree PK. Intralesional sclerotherapy-A novel approach for the treatment of intraoral haemangiomas. J Clin Diagn Res. 2016;10:ZD13–4. doi: 10.7860/JCDR/2016/17568.7137. [DOI] [PMC free article] [PubMed] [Google Scholar]



