Abstract
Objective
The aim of this study was to evaluate the associations between insomnia, sleep duration and self-reported academic performance/failure in a large sample of Norwegian college and university students.
Methods
This cross-sectional survey comprised 50,054 full-time students (69% women) aged 18–35 years (mean age 23.2, standard deviation (SD) = 3.3), with a response rate of 31%. Binary logistic regression analyses were conducted to examine the associations between the independent variables, an approximation of the insomnia disorder and sleep duration, and the dependent variables, failed examinations and delayed study progress.
Results
The results showed that insomnia was associated with a higher risk of failed examinations (adjusted for background variables, odds ratio (ORadjusted) = 1.31, 95% confidence interval (CI) 1.25–1.37, p < 0.001) and delayed study progress (ORadjusted = 1.32, 95% CI: 1.22–1.42, p < 0.001). A curvilinear relationship between sleep duration and risk of academic failure was demonstrated, where both sleeping less than 5 h, and 10 h or more, were associated with higher odds of failed study examinations, compared to with sleeping 7–9 h (ORadjusted = 1.46, 95% CI: 1.33–1.63, p < 0.001 and ORadjusted = 1.53, 95% CI: 1.33–1.75, p < 0.001, respectively). Insomnia and deviations from an optimal sleep duration may have notable consequences for academic success in higher education.
Keywords: Insomnia, Sleep duration, Student, Academic performance
Highlights
-
•
Insomnia complaints were associated with students reporting failed examinations.
-
•
Insomnia complaints were associated with students reporting delayed study progress.
-
•
Both short and long sleep durations were associated with failed study examinations.
-
•
Long sleep duration was associated with students reporting delayed study progress.
1. Introduction
Sleep is essential for the maintenance of cognitive functions related to academic success in higher education, including learning and memory consolidation, decision making, and critical thinking [1], [2]. Optimal functioning in these areas will often be impaired in the absence of sufficient sleep [3]. A considerable number of college/university students report obtaining insufficient sleep [4], [5], [6], [7], [8], [9]. The recommended sleep duration for young adults is between 7 and 9 h [10]. However, one survey of more than 1000 American college students found that 25% slept less than 6.5 h, and only 29% slept for 8 h or more [5]. A recent national survey from Norway that included more than 50,000 college/university students showed that the mean sleep duration on weekdays was just above 7.5 h among healthy sleepers, whereas students who were considered to have insomnia according to an approximation of the DSM-5 criteria for insomnia on average slept less than 7.0 h [7]. In that study, 22% of men and 34% of women met the criteria for insomnia, and the proportion of students reporting difficulties initiating and/or maintaining sleep had increased from 23% in 2010 to 31% in 2018 [7].
It is well established that shortened or disturbed sleep quality reduces students' learning capacity and academic performance, and interventions that restrict or facilitate students' sleep have been associated with impaired and improved, respectively, neurocognitive functioning and academic performance (eg, Curcio et al., [3]; Gilbert & Weaver [11]). However, most studies on the relationship between sleep and cognitive functions and its implications for academic success have been conducted on younger cohorts. For example, one large population-based study of Norwegian adolescents (16–19 years old) found that a sleep deficit and short sleep duration were independently associated with a higher risk of poor grade point average (GPA) [12] and school non-attendance [13]. Similar results have been found in the relationship between insomnia and academic performance. For example, one study showed that American college students with insomnia had a more than six-fold odds of attaining a low GPA [14].
Students' GPA is perhaps the most commonly used measurement of academic performance. However, other measures of educational success have also been examined, such as failed examinations and delayed study progress. These outcomes are relevant not only for the students and their career prospects, but from a socioeconomic perspective failed exams and delayed study progress leads to a direct economic loss to society [15]. A large population-based study that included more than 13,000 college/university students in Norway demonstrated a dose–response relationship between difficulties initiating and maintaining sleep (DIMS) and delayed study progress and having failed several examinations [16]. To the best of our knowledge, no previous study has examined a more stringent evaluation of disturbed sleep based on an approximation of the DSM-5 criteria for insomnia among college students, and how this relates to the risk of delayed study progress and having failed examinations. Recent laboratory studies suggest that those who have a subtype of insomnia characterized by short sleep duration (<6 h) may experience more pronounced neurocognitive deficit than insomnia sufferers with normal sleep duration and healthy controls [17], [18]. However, no previous studies have researched how an approximation of this subtype of insomnia with short sleep duration relates to scholastic parameters such as delayed study progress and having failed examinations.
There can be some overlap between chronic insomnia and delayed sleep–wake phase disorder (DSPD) [19]. Given that the reported prevalence of DSPD in teenagers and young adults range between 7% and 16%, it has been emphasized that the possibility of this alternate or comorbid diagnosis should be considered when evaluating individuals presenting sleep onset insomnia complaints [19]. However, no previous studies on insomnia and academic performance have attempted to rule out the potential effects of DSPD. Insomnia is also closely intertwined with other mental health complaints such as anxiety and depression [20], [21], which, based on the same line of reasoning as above, should be taken into consideration when evaluating the relationship between insomnia and academic performance. Furthermore, both the presentation of sleep problems and academic performance can be influenced by a range of sociodemographic characteristics such as sex, age, marital status, childcare responsibilities, financial situation, alcohol consumption, and physical activity [22], [23], [24], [25], [26], [27]. We therefore argue that these characteristics should be controlled for in models that examine the associations between sleep parameters and academic performance.
The purpose of the present study was to investigate how academic failure is associated with insomnia and sleep duration, while controlling for a range of background variables, DSPD, and symptoms of anxiety and depression (ie, psychological distress). Based on the findings from previous studies, we hypothesize that insomnia and short sleep duration is associated with a higher risk of delayed study progress and having failed examinations.
2. Methods
2.1. Subjects and procedure
Data for this study were derived from the Student's Health and Wellbeing Study (SHoT2018), a national student survey for higher education in Norway, initiated by the three largest student welfare organizations [Sammen (Bergen and surrounding area), Sit (Trondheim and surrounding area) and SiO (Oslo and Akershus)]. Data collection for the SHoT surveys are carried out every fourth year, starting from 2010. Details of the SHoT study have been published elsewhere [28]. The present study comprises data from the 2018 data collection only, which took place between February 6 and April 5, 2018, and included all full-time Norwegian students enrolled in higher education (both in Norway and abroad). Participating institutions set off-time during lectures to allow students to complete the questionnaires electronically in class through a web-based platform. The total number of students qualified to participate in the SHoT2018 study was 162,512, of whom 50,054 students completed the questionnaires. This represented a response rate of 30.8%.
The SHoT2018 study was approved by the Regional Committee for Medical and Health Research Ethics in Western Norway (no. 2017/1176). Electronic informed consent was obtained from all participants.
2.2. Questionnaire
2.2.1. Academic performance
Self-reported academic performance/failure was assessed with the following two questions: (1) ‘Are you following your normed study progression (30 + credits per semester) on the study programme you are taking now?’ with the response options ‘yes’ (= 0) and ‘no’ (= 1); and (2) ‘Have you failed an exam after you started studying at your college/university?’ with the response options ‘no’ (= 0) and ‘yes’ (= 1). A normed study progression for a full-time student in Norway means obtaining 30 credits per semester. Those who, for various reasons, obtain less than 30 credits per semester have a delayed study progress and risk having to spend an extra semester (or a whole school year) to complete their degree. Passed exams give study credits and a failed exam can result in delayed study progress. Some courses offer the option to re-take the exam shortly after failing an examination, which prevents delayed study progress for those who pass the re-take exam. The number of exams per semester can vary greatly across study programs. Information about the number of exams the students had per semester were not available in this study.
2.2.2. Sleep measures
Participants were asked to indicate whether they currently experienced difficulties initiating sleep (DIS), difficulties maintaining sleep (DMS), suffered early morning awakenings (EMA), suffered daytime sleepiness, and/or suffered daytime tiredness. The recognition of these symptoms was followed up with questions regarding how many days per week they experience each of the specific symptoms (1–7 days). In addition, the recognition of any of the symptoms was followed up with a question regarding how long they had been suffering from such sleep problems (‘less than 1 month’, ‘1–2 months’, ‘3–6 months’, ‘7–11 months’, ‘1–3 years’, ‘more than 3 years’). In line with the DSM-5 criteria, insomnia in this paper was operationalized as experiencing at least one nocturnal symptom (ie, DIS, DSM, or EMA), daytime sleepiness, and daytime tiredness minimum three days per week for three months or longer. This is only an approximation of the insomnia disorder, because we were not able to distinguish insomnia from other sleep–wake disorders (eg, narcolepsy, breathing-related sleep disorder, circadian rhythm sleep–wake disorder (other than the approximation of the DSPD), parasomnia), or whether the complaint of insomnia was predominately explained by a coexisting mental disorder or a medical condition, or whether the insomnia was attributable to the physiological effects of a substance (eg, a drug of abuse, a medication) [29].
Participants were asked to indicate, separately for weekdays and weekends, when they usually go to sleep at night (bedtime, hh:mm), when they usually get up in the morning (rise time, hh:mm), how long it usually takes them to fall asleep (sleep onset latency (SOL), hh:mm), and how long they are awake during the night (wake after sleep onset (WASO), hh:mm). Time in bed (TIB) was calculated as the difference between bedtime and rise time. Sleep duration (total sleep time, TST) was calculated as TIB-SOL-WASO.
Furthermore, we identified students who displayed symptoms in line with the diagnostic criteria for DSPD. Following the operationalization of DSPD described by Johnson et al., [30]; reporting: (1) a minimum of 1-h shift in sleep-onset and wake times from the weekdays to the weekends; (2) frequent difficulty falling asleep (≥3 days per week); (3) little or no difficulty maintaining sleep (≤1 day per week); (4) frequent difficulty awakening (oversleep ‘sometimes’ or more often); and (5) obtaining at least 7 h of sleep per night on the weekends, were classified as DSPD. In the present study, the DSPD variable was only used as a control variable in the analyses of insomnia and academic performance.
2.2.3. Demographic and lifestyle information
All participants answered questions about their sex, age, relationship status (‘married/registered partner’, ‘cohabitant’, ‘romantic partner, but lives alone’, ‘single’), whether they had care for children (‘yes’, ‘no’), and immigrant status (‘Were you, or at least one of your parents, born abroad?’ yes/no). In addition, they answered questions pertaining to financial difficulties (‘never/seldom’, ‘sometimes’, ‘often’), study programme (‘one year, ‘lower grade’, ‘higher grade’, ‘other’), and average weekly physical exercise (‘0 or <1 day’, ‘1–3 days’, ‘≥4 days’).
2.2.4. Alcohol use
All participants completed the Alcohol Use Disorders Identification Test (AUDIT) [31]. The AUDIT comprises 10 items designed to assess alcohol consumption, alcohol harm, and symptoms of alcohol dependency. The period of reference is one year (except for two items which also assess lifetime incidences). The composite AUDIT-score range between 0 and 40. The recommended cut-off value to identify hazardous alcohol use is eight [31]. Reliability analyses yielded a Cronbach's alpha of 0.76 in the current sample.
2.2.5. Psychological distress
Psychological distress was assessed using the Hopkins Symptoms Checklist, HSCL-25 [32], derived from the 90-item Symptom Checklist (SCL-90), a screening tool designed to detect symptoms of anxiety and depression. The HSCL-25 is composed of a 10-item subscale for anxiety and a 15-item subscale for depression, with each item scored on a Likert scale from 1 (‘not at all’) to 4 (‘extremely’). The period of reference is two weeks. One item on DIMS was omitted from the composite score and replaced with the mean of the remaining items, thereby preserving the recommended total score to enable comparison with other studies. Reliability analyses of HSCL-25 (without the sleep item) yielded a Cronbach's alpha of 0.93, which is comparable to previous psychometric assessments of this modified scale [16].
2.3. Statistical analyses
All analyses were performed using IBM SPSS Statistics for Macintosh, Version 25.0 (IBM Corp., Armonk, NY, USA). Binary logistic regression analyses were used to examine the association between insomnia and sleep duration as independent variables, and academic performance/failure (ie, failed examinations and delayed study progress) as dependent variables.
For the analyses on insomnia and academic performance/failure, four models were examined: (1) Model 1: crude, (2) Model 2: adjusting for background variables including age, sex, relationship status, care for children, immigrant status, financial difficulties, study programme, physical exercise, and AUDIT classification, (3) Model 3: Model 2 + adjusting for delayed sleep phase disorder (DSPD), and (4) Model 4: Model 3 + additional adjustment for psychological distress (HSCL-25). Furthermore, subgroups of people with and without insomnia were created based on three categories of sleep duration: short sleep duration (<6 h), normal sleep duration (6–8 h), and long sleep duration (>8 h). Logistic regression analyses were run to examine the association between the six groups created based on insomnia/no insomnia at various sleep durations and academic failure as outcome (Models 1–4 as described above). Normal sleepers (no insomnia) with normal sleep duration (6–8 h) were set as the reference category. In order to be able to compare insomnia sufferers with short sleep duration to non-insomniacs with short sleep duration, an additional analysis was run with the latter group set as the reference category.
Binary logistic regression analyses were used to examine the relationship between sleep duration and academic performance/failure (failed study examinations and delayed study progress). Three models were examined: (1) Model 1: crude, (2) Model 2: adjusting for background variables as described above, and (3) Model 3: Model 2 + additional adjustment for psychological distress (HSCL-25). Furthermore, sleep duration was categorized into six groups: ‘Less than 5 h’, ‘5–6 h’, ‘6–7 h’, ‘7–9 h’, ‘9–10 h’, and ‘10 h or more’. With a sleep duration of 7–9 h as the reference category, logistic regression analyses were employed to examine the effects of the various sleep durations on the risk of having failed study examinations and delayed study progress.
The association between the independent and dependent variables were presented as odds ratios (ORs) with 95% confidence intervals. All tests were set at a conventional two-tailed with p < 0.05 as the threshold for significance.
3. Results
3.1. Sample characteristics
The background characteristics of the present sample, including total values and stratified by sex, are summarized in Table 1. Table 2 provides a descriptive summary of the sleep characteristics of the sample, stratified by sex. The proportion of women vs men in the sample (69% vs 31%) was larger than the proportion of women vs men in the population of invited students [58% (N = 93,267) vs 42% (N = 67,558)]. The mean age of the students was 23.2 years (standard deviation (SD) = 3.3) and the age distribution – presented in Table 1 – closely resembled that of all invited students [invited students: 18–20 years (18%, N = 28,996), 21–22 years (31%, N = 49,731), 23–25 years (32%, N = 51,714), 26–28 years (12%, N = 19,901) and 29–35 years (7%, N = 10,216)]. As previously reported [7], the overall prevalence of insomnia based on an approximation of the DSM-5 criteria was 30.5%, with significantly higher prevalence among female (34.2%) than among male (22.2%) students.
Table 1.
Demographical and clinical characteristics among the students in the SHoT-2018 study.
| Women |
Men |
Total |
||||
|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | |
| Demographic characteristics | ||||||
| Age group | ||||||
| 18–20 years | 6490 | (19.1) | 2287 | (15.2) | 8811 | (17.9) |
| 21–22 years | 10,980 | (32.3) | 4402 | (29.2) | 15,434 | (31.3) |
| 23–25 years | 10,607 | (31.2) | 5212 | (34.6) | 15,871 | (32.2) |
| 26–28 years | 3658 | (10.8) | 2009 | (13.3) | 5696 | (11.6) |
| 29–35 years | 2240 | (6.6) | 1166 | (7.7) | 3421 | (6.9) |
| Relationship status | ||||||
| Single | 16,194 | (47.2) | 8585 | (56.0) | 24,890 | (49.9) |
| Romantic partner, but lives alone | 8251 | (24.0) | 3575 | (23.3) | 11,863 | (23.8) |
| Cohabitant | 8630 | (25.1) | 2713 | (17.7) | 11,380 | (22.8) |
| Married/registered partner | 1255 | (3.7) | 454 | (3.0) | 1713 | (3.4) |
| Has children | ||||||
| Yes | 1943 | (5.7) | 509 | (3.3) | 2463 | (4.9) |
| No | 32,339 | (94.3) | 14,792 | (96.7) | 47,307 | (95.1) |
| Immigrant status | ||||||
| Yes | 5180 | (15.0) | 2555 | (16.6) | 7778 | (15.5) |
| No | 29,158 | (84.7) | 12,791 | (83.1) | 42,095 | (84.1) |
| Variables related to socioeconomic status | ||||||
| Financial difficulties | ||||||
| Never/seldom | 23,311 | (68.0) | 11,599 | (75.7) | 35,035 | (70.3) |
| Sometimes | 8063 | (23.5) | 2762 | (18.0) | 10,868 | (21.8) |
| Often | 2919 | (8.5) | 967 | (6.3) | 3910 | (7.8) |
| Study programme | ||||||
| One year | 1982 | (5.8) | 776 | (5.1) | 2773 | (5.6) |
| Lower grade | 21,011 | (61.3) | 8922 | (58.3) | 30,064 | (60.4) |
| Higher grade | 10,786 | (31.5) | 5438 | (35.5) | 16,268 | (32.7) |
| Other | 508 | (1.5) | 166 | (1.1) | 680 | (1.4) |
| Physical exercise (days/week) | ||||||
| 0 or <1 days | 5334 | (15.6) | 2984 | (19.5) | 8363 | (16.8) |
| 1–3 days | 21,297 | (62.2) | 8227 | (53.9) | 29,631 | (59.6) |
| ≥4 days | 7635 | (22.3) | 4059 | (26.6) | 11,735 | (23.6) |
| Alcohol Use Disorder Identification Test classification | ||||||
| Normal | 14,210 | (41.3) | 7331 | (47.7) | 21.756 | (43.6) |
| Hazardous | 20,164 | (58.7) | 8023 | (52.3) | 28,187 | (56.4) |
| Psychological distress | ||||||
| Hopkins Symptom Checklist (>2 points) | 10,598 | (30.8) | 2268 | (14.8) | 12,951 | (25.9) |
| Mean | (SD) | Mean | (SD) | Mean | (SD) | |
| Hopkins Symptom Checklist total score, mean (SD) | 1.81 | (0.55) | 1.52 | (0.47) | 1.72 | (0.55) |
SD, standard deviation.
Table 2.
Sleep characteristics among the students in the SHoT-2018 study.
| Women |
Men |
Total |
||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Insomnia and sleep duration | ||||||
| No insomnia and normal sleep (6–8 h) | 11,928 | (36.0) | 6695 | (45.1) | 18,687 | (37.3) |
| No insomnia and short sleep (<6 h) | 1541 | (4.7) | 937 | (6.3) | 2491 | (5.0) |
| No insomnia and long sleep (>8 h) | 8251 | (24.9) | 3924 | (26.4) | 12,206 | (24.4) |
| Insomnia and normal sleep (6–8 h) | 6442 | (19.4) | 1882 | (12.7) | 8365 | (16.7) |
| Insomnia and short sleep (<6 h) | 2629 | (7.9) | 821 | (5.5) | 3476 | (6.9) |
| Insomnia and long sleep (>8 h) | 2330 | (7.0) | 600 | (4.0) | 1.72 | (0.55) |
| Sleep duration (six categories) | ||||||
| Less than 5 h | 1608 | (4.9) | 682 | (4.7) | 2309 | (4.9) |
| 5–6 h | 2090 | (6.4) | 838 | (5.7) | 2945 | (6.2) |
| 6–7 h | 6094 | (18.7) | 2729 | (18.7) | 8868 | (18.7) |
| 7–9 h | 19,256 | (59.0) | 8922 | (61.0) | 28,262 | (59.6) |
| 9–10 h | 2868 | (8.8) | 1197 | (8.2) | 4075 | (8.6) |
| 10 h or more | 733 | (2.2) | 253 | (1.7) | 991 | (2.1) |
3.2. Insomnia and academic performance
Table 3 present the results from the binary logistic regression analyses on the association between an approximation of the insomnia disorder and academic performance/failure. Insomnia was significantly associated with higher odds of failing study examinations and delayed study progress. This finding was robust across the four models.
Table 3.
Results from the binary logistic regression analyses: an approximation of the insomnia disorder (DSM-5) and academic performance/failure.
| Failed study examinations (reference category: no failed examinations, OR = 1) |
Delayed study progression (reference category: no delay, OR = 1) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 (crude) |
Model 2 (adjusted for backgrounda) |
Model 3 (adjusted for backgrounda + DSPD) |
Model 4 (adjusted for backgrounda + DSPD + psychological distressb) |
Model 1 (crude) |
Model 2 (adjusted for backgrounda) |
Model 3 (adjusted for backgrounda + DSPD) |
Model 4 (adjusted for backgrounda + DSPD + psychological distressb) |
|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Insomnia (reference category: no insomnia) | 1.42 (1.36–1.48)*** | 1.31 (1.25–1.37)*** | 1.30 (1.25–1.36)*** | 1.15 (1.10–1.20)*** | 1.44 (1.34–1.55)*** | 1.32 (1.22–1.42)*** | 1.31 (1.22–1.42)*** | 1.09 (1.01–1.18)* |
| Insomnia and sleep duration (reference category: no insomnia and normal sleep duration) | ||||||||
| No insomnia and short sleep | 1.56 (1.43–1.71)*** | 1.41 (1.29–1.54)*** | 1.41 (1.29–1.54)*** | 1.34 (1.23–1.47)*** | 1.38 (1.18–1.62)*** | 1.24 (1.06–1.46)** | 1.24 (1.06–1.46)** | 1.15 (0.98–1.35) |
| No insomnia and long sleep | 0.96 (0.92–1.01) | 1.02 (0.97–1.08) | 1.02 (0.97–1.08) | 1.04 (0.98–1.09) | 1.01 (0.92–1.11) | 1.11 (1.01–1.22)* | 1.11 (1.01–1.22)* | 1.13 (1.03–1.24)* |
| Insomnia and normal sleep | 1.36 (1.29–1.44)*** | 1.30 (1.22–1.37)*** | 1.29 (1.22–1.36)*** | 1.15 (1.09–1.23)*** | 1.40 (1.27–1.55)*** | 1.32 (1.20–1.46)*** | 1.32 (1.19–1.46)*** | 1.11 (1.00–1.23) |
| Insomnia and short sleep | 1.64 (1.52–1.78)*** | 1.45 (1.34–1.57)*** | 1.44 (1.33–1.56)*** | 1.23 (1.13–1.34)*** | 1.45 (1.27–1.67)*** | 1.26 (1.10–1.45)** | 1.26 (1.09–1.45)** | 0.98 (0.85–1.13) |
| Insomnia and long sleep | 1.49 (1.38–1.62)*** | 1.47 (1.35–1.60)*** | 1.46 (1.34–1.59)*** | 1.31 (1.20–1.43)*** | 1.72 (1.51–1.97)*** | 1.73 (1.51–1.98)*** | 1.72 (1.50–1.98)*** | 1.45 (1.26–1.67)*** |
∗p < 0.05, ∗∗p < 0.01, ∗∗∗p < 0.001.
CI, confidence interval; DSPD, an approximation of the delayed sleep phase disorder; OR, odds ratio.
Background variables include age, sex, relationship status, care for children, immigrant status, income, financial difficulties, study length and programme, physical exercise, smoking, AUDIT classification, and BMI classification.
Psychological distress refers to the score on HSCL-25, where the sleep item on the depression subscale had been taken out.
Additional logistic regression analyses were run on subgroups of students with and without insomnia based on three categories of sleep duration: insomnia sufferers with short (<6 h), normal (6–8 h) and long sleep duration (>8 h) and non-insomniacs with short (<6 h), normal (6–8 h) and long sleep duration (>8 h). Non-insomniacs with normal sleep duration was set as the reference group. The results are presented in Table 3. In order to be able to compare insomnia sufferers with short sleep duration to non-insomniacs with short sleep duration, an additional logistic regression analysis was run with the latter group set as the reference category. The results from these analyses showed no significant difference between insomnia sufferers with short sleep duration and non-insomniacs with short sleep duration on failed study examinations and delayed study progress (results not reported in table).
3.3. Sleep duration and academic performance
Binary logistic regression analyses were employed to investigate the association between sleep duration (as a continuous variable) and academic performance/failure. The results showed that a short sleep duration was associated with higher odds of students failing study examinations in the crude model (Model 1: p < 0.001, OR = 0.92, 95% CI: 0.91–0.93), and this result was robust when controlling for background variables (Model 2: p < 0.001, OR = 0.96, 95% CI: 0.94–0.97) and psychological distress (Model 3: p = 0.014, OR = 0.98, 95% CI: 0.97–1.00). In terms of delayed study progress as outcome, the results from the crude model suggested a shorter sleep duration was associated with higher odds of delayed study progress (Model 1: p = 0.005, OR = 0.97, 95% CI: 0.94–0.99). This association was no longer significant when background variables were controlled for (Model 2: p = 0.294, OR = 1.14, 95% CI: 0.98–1.04), and when psychological distress was controlled for the results indicated the inverse relationship, with longer sleep duration being associated with higher odds of students reporting delayed study progress (Model 3: p < 0.001, OR = 1.05, 95% CI: 1.02–1.08).
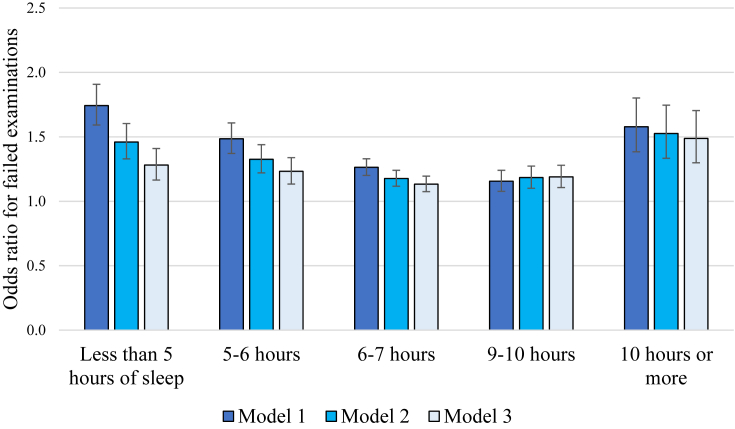
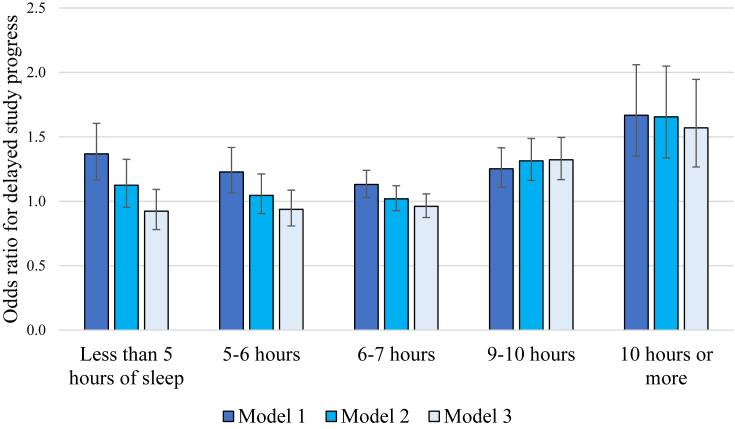
In order to further elucidate a potential curvilinear relationship between sleep duration and academic performance/failure, sleep duration was categorized into six groups: ‘less than 5 h’, ‘5–6 h’, ‘6–7 h’, ‘7–9 h’, ‘9–10 h’, and ‘10 h or more’. Sleep duration of 7–9 h was set as the reference category. The results from the logistic regression analyses for failed examinations and delayed study progress are presented in Fig. 1, Fig. 2, respectively. A curvilinear relationship was indicated between the various sleep durations and academic performance/failure. Sleeping less than 7 h and longer than 9 h appeared both to be associated with higher odds of students reporting failed examinations with a significance level of p < 0.001 (in the crude model and when adjusting for background variables and psychological distress). For example, when adjusting for background variables (Model 2), the OR for failed study examinations when sleeping less than 5 h was 1.46 (95% CI: 1.33–1.60) and when sleeping 10 h or more it was 1.53 (95% CI: 1.33–1.75), compared to sleeping 7–9 h (Fig. 1). This pattern of results was also indicated with delayed study progress as outcome, but only in the crude model (Fig. 2). When background variables were controlled for (Model 2) and when psychological distress was controlled for (Model 3), sleeping less than 7 h was not associated with higher odds of delayed study progress. However, sleeping longer than 9 h was associated with higher odds of delayed study progress in all models with a significance level of p < 0.001. For example, when adjusting for background variables (Model 2), the OR for delayed study progress when sleeping 9–10 h was 1.31 (95% CI: 1.16–1.49), and when sleeping 10 h or more it was 1.66 (95% CI: 1.34–2.05), compared to sleeping 7–9 h (Fig. 2).
Fig. 1.
Odds ratio for failed study examinations with five categories of sleep duration as compared to sleeping 7–9 h per night. Model 1: crude model. Model 2: adjusted for background variables (age, sex, relationship status, care for children, immigrant status, financial difficulties, study programme, physical exercise, and AUDIT classification). Model 3: adjusted for Model 2 + psychological distress (HSCL-25).
Fig. 2.
Odds ratio for delayed study progress with five categories of sleep duration as compared to sleeping 7–9 h per night. Model 1: crude model. Model 2: adjusted for background variables (age, sex, relationship status, care for children, immigrant status, financial difficulties, study programme, physical exercise, and AUDIT classification). Model 3: adjusted for Model 2 + psychological distress (HSCL-25).
4. Discussion
The present paper demonstrates an association between an approximation of the insomnia disorder and failed study examinations, which was independent of a range of background and lifestyle factors, an approximation of the DSPD and psychological distress. Similarly, those who had insomnia also had higher odds of reporting delayed study progress. A curvilinear relationship was demonstrated between sleep duration and failed study examinations, where both short and long sleep duration was associated with higher odds of failed study examinations. These findings should be replicated in studies that can employ an objective assessment of sleep duration.
The finding that insomnia was associated with failed study examinations are in line with those of the previous SHoT survey from 2014, where a single item measuring DIMS was associated with failing several examinations [16]. The present study support and further expand on these findings, and provides additional specificity with regards to an approximation of the DSM-5 insomnia disorder. Furthermore, these updated data indicate that an approximation of the DSPD does not adequately account for these findings. It is important to rule out DSPD because this is prevalent among young people and can be characterized by complaints that overlap with the insomnia disorder [19], [33].
The association between insomnia and failed examinations may be mediated through cognitive function, and the results are thus in line with those of laboratory studies on insomnia and cognitive impairments. For example, a meta-analysis showed that insomnia was associated with mild to moderate impairments on more complex cognitive functioning, such as working memory and executive control, whereas performance on areas such as alertness, sustained attention and vigilance were not affected compared to normal sleepers [34]. Recent advancements in this field suggest that these impairments might be more pronounced among those who have the subtype of insomnia characterized by short sleep duration [17], [18]. Indeed, our findings indicate that those with insomnia and a short sleep duration (<6 h) had the highest risk of reporting more failed exams relative to the other categories when no other variables were controlled for. However, the present study did not find any significant differences between insomnia sufferers with short sleep duration and non-insomniacs with short sleep duration in terms of failed examinations, which contrasts laboratory findings where insomniacs with short sleep duration have been found to have greater cognitive impairments compared to non-insomniacs with short sleep duration (eg, Fernandez-Mendoza [35]). Thus, the current results suggest that short sleep duration is associated with more failed study examinations irrespective of whether the individuals have insomnia or not.
In the present study, those who were suffering from insomnia had higher odds of reporting delayed study progress. This is in line with most previous studies on sleep and academic performance, which tend to indicate an association between insufficient sleep or sleep quality and academic failure [13], [36], [37]. Furthermore, insomnia sufferers, regardless of their sleep duration, had higher odds of delayed study progress than non-insomniacs with normal sleep duration, when adjusting for background variables and an approximation of the DSPD. However, insomnia sufferers with short sleep duration had lower odds of delayed study progress than those with normal and long sleep duration. These results might be considered to contradict those of previous laboratory studies on the added detriments of having insomnia with short sleep duration on neurocognitive morbidity [35]. However, these previous studies tend to identify this particular subtype of insomnia based on objective assessments of sleep duration. Insomnia sufferers with objectively normal sleep duration are known to underestimate their total sleep time [36]. It can thus be argued that the subjective assessment of sleep duration used in the present study provides an imprecise classification of this particular subtype of insomnia with short sleep duration. Our results should therefore be replicated in studies that can employ an objective assessment of sleep duration.
Short sleep duration was associated with a higher risk of students reporting failed examinations in the present study. This finding was independent of a range of lifestyle factors and psychological distress, and the results are in line with previous field and laboratory studies [13], [17], [18], [37], [38]. The relationship between sleep duration and failed examinations was further elucidated in some additional regression analyses that were conducted, where we distinguished between six categories of sleep duration. These analyses illustrated a curvilinear relationship between sleep duration and the risk of students reporting failed study examinations, where both short and long sleep duration appear to be associated with a higher risk of failed study examinations compared to sleeping 7–9 h. A similar pattern of results was obtained with delayed study progress as outcome, although these analyses indicated a more dubious link between short sleep duration and risk of academic failure. Taken together, these results might suggest there is an optimal sleep duration for academic performance, and to the best of our knowledge, the present study is the first to suggest this for academic performance as an outcome. Optimal sleep duration has been demonstrated in previous studies on health-related outcomes. For example, both short and long sleep duration have been associated with negative outcomes such as body weight and fat gain [39], diabetes, hypertension, and cardiovascular disease in adults [40]. Deviations from the average sleep duration can reflect other underlying health problems or the sleep pattern of an individual whose circadian phase is misaligned with their day–night schedule, both of which can conceivably contribute to academic failure.
4.1. Limitations and strengths
Limitations of the present study include the cross-sectional design, which precludes inferences about directionality. Another limitation pertains to the fact that all measures are self-reported. Nevertheless, it is worth noting that self-reported measures of sleep can often be recommended for the characterization of sleep parameters in both clinical and population-based research [41]. However, academic failure could preferably have been based on objective records, because students may have provided inaccurate reports of failed examinations and delayed study progress due to a recall bias, or they may have intentionally refrained from telling the truth. There might be other confounders or pathways between sleep and study progress that were not assessed in the current study. For example, school absence is known to account for some of the associations between sleep and academic outcomes in younger cohorts [12].
Another limitation of the study is the response rate of 31%, which is less than the preferred minimum of 50–60% response rate, and implies a higher risk for non-response bias [42]. The use of a web-based survey approach may have contributed to the moderate response rate, because web-based platforms typically yield lower response rates compared to traditional mail approaches [43]. It should be noted that 69% of the participants in this survey were women, which may limit the generalizability of the results. It is possible that the female preponderance created a bias in the sample, because women generally report worse sleep across most parameters compared to men. However, about 70% of the student population in Norwegian colleges/universities are women, at least up to bachelor's degree. The female preponderance in the present study should therefore not represent a substantial bias.
A major strength of the present study pertains to the large sample size. Furthermore, the detailed assessments of sleep parameters allowed for an approximation of the insomnia disorder according to the DSM-5 criteria. It should nevertheless be noted that we were not able to distinguish between the insomnia disorder and other sleep–wake disorder (eg, narcolepsy, a breathing-related sleep disorder, a circadian rhythm sleep–wake disorder (other than the approximation of the DSPD), a parasomnia), or whether the complaint of insomnia was predominantly explained by a coexisting mental disorder or a medical condition, or whether the insomnia was attributable to the physiological effects of a substance (eg, a drug of abuse, a medication) [29]. This may have contributed to a high prevalence of insomnia in the present study, which should be replicated in studies that can use a clinical assessment of the insomnia disorder according to the DSM-5 criteria.
4.2. Conclusion and practical implications
Insomnia disorder has notable consequences for aspects of learning ability and academic success in higher education. In this population-based sample of Norwegian higher education/university students, we found that insomnia was associated with a higher risk of students reporting failed examinations and experiencing delayed study progress. This study also demonstrates a curvilinear relationship between sleep duration and the risk of academic failure – both short and long sleep was associated with failed study examinations, and long sleep was especially associated with delayed study progress. Failed examinations and delayed study progress can have major personal and financial consequences for the students, which can negatively affect their career prospects and other aspects of their lives. Students who are delayed in their study progress or need to re-take exams will often contribute to overcrowded lecture halls and drain resources from the educational institutions, which in turn may impair the learning environment for other students. In this respect, failed examinations and delayed study progress come with both direct and indirect financial costs for society, especially in countries where higher education is subsidized by the state [15]. This calls for low-threshold and efficacious treatments for insomnia that should be implemented in student populations. For example, it has been demonstrated that unguided internet-based cognitive behavioural therapy for insomnia may be effective in improving sleep for students and adults with chronic insomnia, both in the short and the long term ([44], [45], [46]).
Acknowledgements
The authors wish to thank all of the students who participated in the study, as well as the three largest student-welfare organizations in Norway (SiO, Sammen, and SiT), who initiated and designed the SHoT study. SHoT2018 received funding from the Norwegian Ministry of Education and Research (2017) and the Norwegian Ministry of Health and Care Services (2016).
Footnotes
The authors have no competing interests to declare.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleepx.2019.100005.
Conflict of interest
The following is the supplementary data to this article:
Multimedia component 1
References
- 1.Harrison Y., Horne J. The impact of sleep deprivation on decision making: a review. J Exp Psychol Appl. 2000;6:236–249. doi: 10.1037//1076-898x.6.3.236. [DOI] [PubMed] [Google Scholar]
- 2.Pilcher J., Walters A. How sleep deprivation affects psychological variables related to college students' cognitive performance. J Am Coll Health. 1997;46:121–126. doi: 10.1080/07448489709595597. [DOI] [PubMed] [Google Scholar]
- 3.Curcio G., Ferrara M., De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10:323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Hershner S.D., Chervin R.D. Causes and consequences of sleepiness among college students. Nat Sci Sleep. 2014;6:73. doi: 10.2147/NSS.S62907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lund H.G., Reider B.D., Whiting A.B. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Medeiros A.L.D., Mendes D.B.F., Lima P.F. The relationships between sleep-wake cycle and academic performance in medical students. Biol Rhythm Res. 2001;32:263–270. [Google Scholar]
- 7.Sivertsen B., Vedaa Ø., Harvey A.G. Sleep patterns and insomnia in young adults: a National survey of Norwegian university students. J Sleep Res. 2018 doi: 10.1111/jsr.12790. [DOI] [PubMed] [Google Scholar]
- 8.Taylor D.J., Bramoweth A.D. Patterns and consequences of inadequate sleep in college students: substance use and motor vehicle accidents. J Adolesc Health. 2010;46:610–612. doi: 10.1016/j.jadohealth.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Tsai L.-L., Li S.-P. Sleep patterns in college students: gender and grade differences. J Psychosom Res. 2004;56:231–237. doi: 10.1016/S0022-3999(03)00507-5. [DOI] [PubMed] [Google Scholar]
- 10.Hirshkowitz M., Whiton K., Albert S.M. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Gilbert S.P., Weaver C.C. Sleep quality and academic performance in university students: a wake-up call for college psychologists. J Coll Stud Psychother. 2010;24:295–306. [Google Scholar]
- 12.Hysing M., Harvey A.G., Linton S.J. Sleep and academic performance in later adolescence: results from a large population-based study. J Sleep Res. 2016;25:318–324. doi: 10.1111/jsr.12373. [DOI] [PubMed] [Google Scholar]
- 13.Hysing M., Haugland S., Stormark K.M. Sleep and school attendance in adolescence: results from a large population-based study. Scand J Publ Health. 2015;43:2–9. doi: 10.1177/1403494814556647. [DOI] [PubMed] [Google Scholar]
- 14.Gaultney J.F. The prevalence of sleep disorders in college students: impact on academic performance. J Am Coll Health. 2010;59:91–97. doi: 10.1080/07448481.2010.483708. [DOI] [PubMed] [Google Scholar]
- 15.O'Neill L.D., Wallstedt B., Eika B. Factors associated with dropout in medical education: a literature review. Med Educ. 2011;45:440–454. doi: 10.1111/j.1365-2923.2010.03898.x. [DOI] [PubMed] [Google Scholar]
- 16.Hayley A.C., Sivertsen B., Hysing M. Sleep difficulties and academic performance in Norwegian higher education students. Br J Educ Psychol. 2017;87:722–737. doi: 10.1111/bjep.12180. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez-Mendoza J., Calhoun S., Bixler E.O. Insomnia with objective short sleep duration is associated with deficits in neuropsychological performance: a general population study. Sleep. 2010;33:459–465. doi: 10.1093/sleep/33.4.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khassawneh B.Y., Bathgate C.J., Tsai S.C. Neurocognitive performance in insomnia disorder: the impact of hyperarousal and short sleep duration. J Sleep Res. 2018;27 doi: 10.1111/jsr.12747. [DOI] [PubMed] [Google Scholar]
- 19.American Academy of Sleep Medicine . 3rd ed. American Academy of Sleep Medicine; Darien, IL: 2014. International classification of sleep disorders. [Google Scholar]
- 20.Sivertsen B., Salo P., Mykletun A. The bidirectional association between depression and insomnia: the HUNT study. Psychosom Med. 2012;74:758–765. doi: 10.1097/PSY.0b013e3182648619. [DOI] [PubMed] [Google Scholar]
- 21.Taylor D.J., Lichstein K.L., Durrence H.H. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–1464. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 22.Grandner M.A., Patel N.P., Gehrman P.R. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hale L. Who has time to sleep? J Public Health. 2005;27:205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 24.Hartmann M.E., Prichard J.R. Calculating the contribution of sleep problems to undergraduates' academic success. Sleep Health. 2018;4(5):463–471. doi: 10.1016/j.sleh.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Marques A., Santos D.A., Hillman C.H. How does academic achievement relate to cardiorespiratory fitness, self-reported physical activity and objectively reported physical activity: a systematic review in children and adolescents aged 6–18 years. Br J Sports Med. 2018;52:1039. doi: 10.1136/bjsports-2016-097361. [DOI] [PubMed] [Google Scholar]
- 26.Sheard M. Hardiness commitment, gender, and age differentiate university academic performance. Br J Educ Psychol. 2009;79:189–204. doi: 10.1348/000709908X304406. [DOI] [PubMed] [Google Scholar]
- 27.Zhang B., Wing Y.-K. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 28.Sivertsen B., Råkil H., Munkvik E. Cohort profile: the SHoT-study, a national health and well-being survey of Norwegian university students. BMJ Open. 2019 doi: 10.1136/bmjopen-2018-025200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Psychiatric Association . American Psychiatric Pub; 2013. Diagnostic and statistical manual of mental disorders (DSM-5®) [Google Scholar]
- 30.Johnson E.O., Roth T., Schultz L. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:e247–e256. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 31.Saunders J.B., Aasland O.G., Babor T.F. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 32.Derogatis L.R., Lipman R.S., Rickels K. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 33.Sivertsen B., Pallesen S., Stormark K.M. Delayed sleep phase syndrome in adolescents: prevalence and correlates in a large population based study. BMC Public Health. 2013;13:1163. doi: 10.1186/1471-2458-13-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fortier-Brochu É., Beaulieu-Bonneau S., Ivers H. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev. 2012;16:83–94. doi: 10.1016/j.smrv.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 35.Fernandez-Mendoza J. The insomnia with short sleep duration phenotype: an update on it's importance for health and prevention. Curr Opin Psychiatr. 2017;30:56–63. doi: 10.1097/YCO.0000000000000292. [DOI] [PubMed] [Google Scholar]
- 36.Fernandez-Mendoza J., Calhoun S.L., Bixler E.O. Sleep misperception and chronic insomnia in the general population: the role of objective sleep duration and psychological profiles. Psychosom Med. 2011;73:88. doi: 10.1097/PSY.0b013e3181fe365a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dewald J.F., Meijer A.M., Oort F.J. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14:179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 38.Taylor D.J., Vatthauer K.E., Bramoweth A.D. The role of sleep in predicting college academic performance: is it a unique predictor? Behav Sleep Med. 2013;11:159–172. doi: 10.1080/15402002.2011.602776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chaput J.-P., Després J.-P., Bouchard C. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec family study. Sleep. 2008;31:517–523. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buxton O.M., Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 41.Zinkhan M., Berger K., Hense S. Agreement of different methods for assessing sleep characteristics: a comparison of two actigraphs, wrist and hip placement, and self-report with polysomnography. Sleep Med. 2014;15:1107–1114. doi: 10.1016/j.sleep.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 42.Kerlinger F.N. CBS Publishing; New York: 1986. Foundations of behavioral research. [Google Scholar]
- 43.Sheehan K.B. E-mail survey response rates: a review. J Computer-Mediated Commun. 2001;6 doi: 10.1111/j.1083-6101.2001.tb00117.x. [DOI] [Google Scholar]
- 44.Hagatun S., Vedaa Ø., Nordgreen T. The short-term efficacy of an unguided internet-based cognitive-behavioral therapy for insomnia: a randomized controlled trial with a six-month nonrandomized follow-up. Behav Sleep Med. 2019;17(2):137–155. doi: 10.1080/15402002.2017.1301941. [DOI] [PubMed] [Google Scholar]
- 45.Freeman D., Sheaves B., Goodwin G.M. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 2017;4:749–758. doi: 10.1016/S2215-0366(17)30328-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vedaa Ø., Hagatun S., Kallestad H. Long-term effects of an unguided online cognitive behavioral therapy for chronic insomnia. J Clin Sleep Med. 2019;15:101–110. doi: 10.5664/jcsm.7580. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1