Abstract
Background
It has been observed that subjects with comorbidities related to metabolic syndrome (MetS) as hypertension, obesity, cardiovascular disease (CVD), and diabetes mellitus (DM2) show severe cases and a higher mortality by COVID-19. To date, there is little information available on the impact of the interaction between these comorbidities in the risk of death by COVID-19.
Aim of the Study
To evaluate the impact of the combinations of MetS components in overall survival (OS) and risk of death among COVID-19 patients.
Methods
Using public data of the Ministry of Health, suspected, and confirmed COVID-19 cases from February 25–June 6, 2020 was analyzed. Mortality odds ratio (OR) was calculated with a univariate analysis (95% CI) and attributable risk. Interactions between components and survival curves were analyzed and a multivariate logistics regression analysis was conducted.
Results
The analysis included 528,651 cases out of which 202,951 were confirmed for COVID-19. Probabilities of OS among confirmed patients were 0.93, 0.89, 0.87, 0.86, and 0.83 while the OR of multivariate analysis was 1.83 (1.77–1.89), 2.58 (2.48–2.69), 2.83 (2.66–3.01), and 3.36 (2.83–3.99) for zero, one, two, three, and four MetS components, respectively. The combination with the highest risk was DM2 + hypertension at 2.22 (2.15–2.28), and the attributable risk for any component was 9.35% (9.21–9.49). Only the combination obesity + CVD showed no significant interaction.
Conclusion
The presence of one MetS component doubles the risk of death by COVID-19, which was higher among patients with DM2 + hypertension. Only obesity and CVD do not interact significantly.
Keywords: COVID-19, SARS-CoV-2, obesity, DM2, hypertension, cardiovascular disease
Introduction
In December 2019, a group of patients in Wuhan, China showed pneumonia compatible with severe acute respiratory syndrome (SARS) due to a new zoonotic virus called SARS-CoV-2 causing the COronaVirusDisease-19 (COVID-19) (1). SARS-CoV-2 is easily transmitted and has suddenly spread so that the World Health Organization (WHO) declared a pandemic by SARS-CoV-2 on March 11, 2020. By February 2021, there were around 100 million confirmed cases and 2 million deaths by COVID-19 have been reported (2).
Currently, over 50% of the total cases and deaths by COVID-19 are found in The Americas. The cases reported in Mexico account for around 2% of those worldwide and 4.5% of the cases in The Americas. In Mexico, the lethality of COVID-19 recorded in 2020 in confirmed patients was 10.5% approximately and it lowered to 8.5% by 2021. This value is among the highest according to international records. WHO states that the mortality rate of COVID-19 is 139.14 deaths per 100,000 inhabitants, only below that of Italy (157.51 per 100,000) and the United States (147.84 per 100,000) (2,3).
The COVID-19 pandemic coexists with another one caused by metabolic alterations such as obesity and diabetes mellitus (DM2). In 2016, WHO reported 650 million people with obesity (4). Furthermore, the International Federation of Diabetes (IFD) indicated that 463 million adults lived with diabetes in 2019 (5). In Mexico, the most recent National Health and Nutrition survey (ENSANUT) found that, in 2018, the prevalence of DM2, obesity, and hypertension among Mexicans over 20 years of age was 10.3, 36.1, and 18.4%, respectively, representing at least 50 million people (6).
Metabolic syndrome (MetS) is a clinical entity that increases the risk of developing cardiovascular diseases (CVD) and DM2. It is characterized by metabolic, inflammatory, and prothrombotic abnormalities that clinically manifest as abdominal obesity, hypertension, and dyslipidemia. There are different criteria to identify MetS, such as ATP-III and those by WHO and IDF, that evaluate the presence of abdominal obesity (according to waist circumference), dyslipidemia (triglycerides and HDL levels), hypertension, and alterations in glucose metabolism (fasting glucose level or presence of DM2) (7,8). MetS is a progressive disease and has four stages of development: A, in which people show certain risk factors (overweight, low physical activity, and racial susceptibility) of developing MetS; B, in which one or two MetS components are present; C, in which the diagnosis criteria for MetS are met; C, when the diagnosis criteria for MetS are met according to WHO, IDF, or ATP III but there is no damage in target organs; and finally, in stage D patients with MetS show damage in target organs, so MetS components are expressed in diseases as obesity, DM2, hypertension, CVD, fatty liver, and sleep apnea, among other comorbidities (9).
A high proportion of individuals can show combinations of MetS comorbidities, leading to a high prevalence of this condition among the Mexican population. An interval from 13 (according to WHO criteria) to 56% (according to IDF criteria) is reported for the general population and, worryingly, it is 20% among children and adolescents (10).
Around the world, these comorbidities have not only been highly prevalent in COVID-19 patients but are also factors of a worse prognosis (11). Obese patients with COVID-19 show an increased risk of needing ICU care, invasive mechanical ventilation, and mortality (12,13). Additionally, the presence of hypertension and DM2 is linked to a significant increase in the relative risk (RR) of severe disease (14). In the Mexican population, the mortality odds ratio (OR) reported for severe COVID-19 is 1.87, 1.77, and 1.43 in the presence of DM2, hypertension, and obesity, respectively, while the risk increases to 1.67 in obese subjects over 50 years old (15). These studies do not analyze RR of mortality by the combination of MetS components.
Given the high lethality by COVID-19 in the Mexican population and the high prevalence of comorbidities, as MetS components, this work identified the probability of overall survival (OS), OR attributable risk and component interaction in the mortality of patients with COVID-19 associated to obesity, hypertension, DM2, and CVD, individually or in combination. The aim is to provide information on the effect of these comorbidities in the outcome of the infection by SARS-CoV-2 in the Mexican population.
Materials and Methods
Study Design, Data Collection, and Definitions
This is a retrospective, observational, and multicentric study including 582,651 subjects who showed viral respiratory disease between February 28 and June 25, 2020 as recorded in the public database of the epidemiological surveillance system (Sistema de Vigilancia Epidemiológica de Enfermedades Respiratorias, SISVER) at Dirección General de Epidemiología de la Secretaría de Salud de México (http://www.gob.mx/salud/documentos/datos-abiertos-152127) (16). This is a free-access database updated daily with all suspected COVID-19 cases. In Mexico, during data collection, the operational definition of suspected COVID-19 case included people of any age showing at least two of the following symptoms: cough, fever, and headache. In addition, they should present at least one of the following: dyspnea, arthralgia, myalgia, odynophagia, rhinorrhea, conjunctivitis, and chest pain. Then, the diagnosis of COVID-19 was confirmed by a polymerase chain reaction (PCR) test for SARS-CoV-2 performed by the institute of epidemiological diagnosis and reference (Instituto de Diagnóstico y Referencia Epidemiológicos, InDRE) or any laboratory of the national network of public health laboratories (Red Nacional de Laboratorios de Salud Pública, RNLSP).
Comorbidity records on the SISVER online platform are determined by the patient's self-report when receiving medical attention and classified as present or absent. There is no record of disease duration nor active treatments at the time of registration. In consequence, the platform provides no records of parameters as triglyceride and HDL levels, fasting glucose, or abdominal circumference. This study defines the presence of MetS according to the classification of stage D proposed by Sperling (9) in the presence of clinical entities affecting organs (DM2 and CVD) or components (obesity and hypertension).
Statistical Analysis
A frequency and percentage descriptive analysis of the categorical variables was carried out; median and interquartile range of age were also reported. Mortality risk was evaluated by calculating OR (exposed/non-exposed incidences), 95% confidence intervals (CI), and a univariate analysis that considered adult age group with the least mortality, and absence of MetS components as reference groups. We calculated OR for total cases and confirmed COVID-19 patients.
A univariate analysis of RR and attributable risk was carried out per MetS component, along with an analysis of interaction between comorbidities. We assessed the impact of the number of MetS components on OS, according to the Kaplan–Meier method and a log-rank test. Finally, a multivariate logistic regression analysis adjusted to age and sex was conducted for the total number of cases and the group of confirmed patients. In all cases, p <0.05 was considered statistically significant. Data were analyzed using SPSS version 23.
Results
This study included 528,651 total cases that met the operational definition of viral respiratory disease; 202,951 (38.4%) tested positive and 262,117 (49.6%) were negative to PCR test for SARS-CoV-2. No confirmatory test was obtained for 12% of the cases (63,583), which were considered suspicious. The distribution of sex ratio in the confirmed COVID-19 group was 54.8% male and 45.2% female, while the median age was 45 years (interquartile range 34–57 years) and lethality was 12.3%. The prevalence of DM2, hypertension, obesity, and CVD were 16.6, 20.2, 19.7, and 2.4%, respectively. In this same group, 59.7% of the subjects showed no components, but 25, 11.2, 3.3, and 0.3% showed one, two, three, and four MetS components, respectively. These frequencies were higher with respect to the groups of the total, negative, and suspicious cases (Table 1 ).
Table 1.
Demographic characteristics and prevalence of comorbidities
| Characteristic | Total (n = 528 651) | Confirmed cases (n = 202 951) | Negative cases (n = 262 117) | Suspected cases (n = 63 583) |
|---|---|---|---|---|
| Female n (%) | 260 477 (49.3) | 91 652 (45.2) | 137 730 (52.5) | 31 095 (48.9) |
| Male n (%) | 268 174 (50.7) | 111 299 (54.8) | 124 387 (47.5) | 32 488 (51.1) |
| Age, years median (RIQ) | 41 (31, 53) | 45 (34, 57) | 39 (29, 50) | 41 (31, 54) |
| Death n (%) | 33 596 (6.4) | 25 060 (12.3) | 6 570 (2.5) | 1 966 (3.1) |
| DM2 n (%) | 66 047 (12.5) | 33 492 (16.6) | 24 740 (9.5) | 7 815 (12.4) |
| Hypertension n (%) | 86 251 (16.4) | 40 814 (20.2) | 35 057 (13.4) | 10 380 (16.4) |
| Obesity n (%) | 86 339 (16.4) | 39 873 (19.7) | 36 461 (13.9) | 10 005 (15.8) |
| CVD n (%) | 12 047 (2.3) | 4 802 (2.4) | 5 977 (2.3) | 1 268 (2.0) |
| CKD n (%) | 10 605 (2.0) | 4 434 (2.2) | 4 974 (1.9) | 1 197 (1.9) |
| Smoking n (%) | 45 043 (8.5) | 15 877 (7.9) | 24 388 (9.3) | 4 778 (7.6) |
| COPD n (%) | 8 667 (1.6) | 3 607 (1.8) | 4 214 (1.6) | 846 (1.3) |
| Asthma n (%) | 17 025 (3.2) | 5 610 (2.8) | 9689 (3.7) | 1 726 (2.7) |
| MetS components Prevalences | ||||
| Cero, n (%) | 352 902 (66.8) | 121 176 (59.7) | 188 852 (72) | 42 874 (67.4) |
| One, n (%) | 112 743 (21.3) | 50 673 (25.0) | 48 978 (18.7) | 13 092 (20.6) |
| Two, n (%) | 45 867 (8.7) | 22 679 (11.2) | 17 673 (6.7) | 5 515 (8.7) |
| Three, n (%) | 13 289 (2.5) | 6667 (3.3) | 5 064 (1.9) | 1 558 (2.5) |
| Four, n (%) | 1 414 (0.3) | 641 (0.3) | 621 (0.2) | 152 (0.2) |
DM2: diabetes mellitus 2; CVD: cardiovascular disease; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; MetS: metabolic syndrome. RIQ: Interquartile Range.
In the univariate analysis, mortality OR by age range and sex for age groups under 18, between 40 and 65, and over 65 were 1.41 (1.27–1.57), 7.18 (6.88–7.50), and 31.74 (30.34–33.19) in the group of total patients. The OR was 0.77 (0.62–0.95), 6.76 (6.51–7.12), and 25.16 in the group of total patients and confirmed cases, respectively. Mortality risk for men considering total cases was 1.88 (1.83–1.91) and 1.71 (1.66–1.76) for women in confirmed cases. Regarding MetS components, mortality risk for the total cases was 3.18 (3.05–3.27), 6.38 (6.19–6.58), 7.34 (7.00–7.69), and 9.19 (8.12–10.41) for one, two, three and four comorbidities respectively, but always lower for confirmed cases at 2.69 (2.60–2.78), 5.05 (4.87–5.24), 5.69 (5.37–6.03), and 7.24 (6.14–8.53). In the total cases, the mortality for identified MetS components were DM2 4.79 (4.68–4.91), hypertension 4.25 (4.15–4.35), obesity 1.62 (1.58–1.67), and CVD 3.22 (3.07–3.38). The same value in confirmed cases was DM2 3.74 (3.63–3.85), hypertension 3.55 (3.45–3.65), obesity 1.43 (1.39–1.48), and CVD 2.48 (2.67–3.03). Since the presence of combined MetS components was frequent, we calculated the mortality risk for the different comorbidity combinations as follows for total and confirmed cases respectively: DM2 and hypertension 5.02 (4.88–5.17), 3.98 (3.85–4.12); DM2 and obesity 3.32 (3.19–3.45), 2.61 (2.49–2.74); DM2 and CVD 4.46 (4.16–4.79), 3.86 (3.51–4.24); obesity and hypertension 2.86 (2.76–2.97), 2.44 (2.33–2.54); hypertension and CVD 4.13 (3.89–4.38), 3.59 (3.33–3.38); and obesity and CVD 3.42 (3.15–3.72), 3.01 (2.70–3.35). When the combination included three components, representing diagnosed MetS, results were: DM2, hypertension, and obesity 3.82 (3.64–4.01), 3.02 (2.85–3.21); DM2, hypertension, and CVD 4.68 (4.32–5.06), 4.01 (3.61–4.46); obesity, hypertension, and CVD 3.80 (3.63–3.99), 3.02 (2.84–3.19), and obesity, DM2, and CVD 4.25 (3.79–4.77), 3.54 (3.05–4.12). Finally, when the four components were combined, OR were 4.55 (4.03–5.15) and 3.76 (3.19–4.43) (Table 2 ). Multivariate analysis adjusted by age and sex were also confirmatory of this trend both in all suspected cases and in those confirmed by PCR (Table 3 ).
Table 2.
Univariate OR in total and confirmed cases
| Total cases | Confirmed cases | |
|---|---|---|
| Age group | ||
| <18 years | 1.41 (1.27,1.57) | 0.77 (0.62,0.95) |
| 18–39 years (reference) | Reference | Reference |
| 40–65 years | 7.18 (6.88,7.50) | 6.76 (6.51,7.12) |
| More 65 years | 31.74 (30.34,33.19) | 25.16 |
| Sex | ||
| Female | Reference | Reference |
| Male | 1.88 (1.83,1.91) | 1.71 (1.66,1.76) |
| Components number of MetS | ||
| 0 | Reference | |
| 1 | 3.18 (3.09,3.27) | 2.69 (2.60,2.78) |
| 2 | 6.38 (6.19,6.58) | 5.05 (4.87,5.24) |
| 3 | 7.34 (7.00,7.69) | 5.69 (5.37,6.03) |
| 4 | 9.19 (8.12,10.41) | 7.24 (6.14,8.53) |
| Componet MetS | ||
| DM2 | 4.79 (4.68–4.91) | 3.74 (3.63–3.85) |
| Hypertension | 4.25 (4.15–4.35) | 3.55 (3.45–3.65) |
| Obesity | 1.62 (1.58–1.67) | 1.43 (1.39–1.48) |
| CVD | 3.22 (3.07–3.38) | 2.84 (2.67–3.03) |
| DM2+HAS | 5.02 (4.88–5.17) | 3.98 (3.85,4.12) |
| DM2+Obesity | 3.32 (3.19–3.45) | 2.61 (2.49–2.74) |
| DM2+CVD | 4.46 (4.16–4.79) | 3.86 (3.51–4.24) |
| Obesity+Hypertension | 2.86 (2.76–2.97) | 2.44 (2.33–2.54) |
| Hypertension+CVD | 4.13 (3.89–4.38) | 3.59 (3.33–3.38) |
| Obesity+CVD | 3.42 (3.15–3.72) | 3.01 (2.70–3.35) |
| DM2+Hypertension+ Obesity | 3.82 (3.64–4.01) | 3.02 (2.85–3.21) |
| DM2+Hypertension+ CVD | 4.68 (4.32–5.06) | 4.01 (3.61–4.46) |
| Obesity+Hypertension+ CVD | 3.80 (3.63–3.99) | 3.02 (2.84–3.19) |
| Obesity+DM2+CVD | 4.25 (3.79–4.77) | 3.54 (3.05,4.12) |
| Obesity+DM2+ hypertension+CVD | 4.55 (4.03–5.15) | 3.76 (3.19–4.43) |
Table 3.
Attributable Risks for one, two, three, four or any components of metabolic syndrome
| Number of components of MetS | Relative Risk (CI 95%) | Attributable risk (CI 95%) | Number needed to be exposed |
|---|---|---|---|
| One | 2.97 (2.94,2.99) | 6.36% (6.21,6.50) | 16 |
| Two | 5.43 (5.41,5.46) | 14.32% (14.11,14.53) | 7 |
| Three | 6.09 (6.06,6.13) | 16.46% (16.12,16.79) | 6 |
| Four | 7.27 (7.17,7.37) | 20.25% (19.32,21.18) | 5 |
| Any | 3.90 (3.87,3.92) | 9.35% (9.21,9.49) | 11 |
Within the univariate analysis, we calculated the contribution of the number of MetS components to COVID-19 lethality. The RR and attributable risks for one component were 2.97 (2.94–2.99) and 6.36% (6.21–6.50); for two components, 5.43 (5.41–5.46) and 14.32% (14.11–14.53); for three components, 6.09 (6.06–6.13) and 16.46% (16.12–16.79); for four components, 7.27 (7.17–7.37) and 20.25% (19.32–21.18); and for any component, 3.90 (3.87–3.92) and 9.35% (9.21–9.49), respectively (Table 4 ).
Table 4.
MetS components Interaction analysis
| OR (95% CI) | p | p for interaction | |
|---|---|---|---|
| OBESITY | |||
| Obesity by DM2 | <0.001 | ||
| No DM2 | 1.61 (1.54,1.68) | <0.001 | |
| DM2 | 1.00 (0.94,1.05) | 0.881 | |
| Obesity by hypertension | <0.001 | ||
| No hypertension | 1.99 (1.91,2.07) | <0.001 | |
| Hypertension | 1.06 (1.01,1.12) | 0.016 | |
| Obesity by CVD | 0.226 | ||
| No CVD | 1.47 (1.42,1.51) | <0.001 | |
| CVD | 1.29 (1.12,1.48) | <0.001 | |
| DM2 | |||
| DM2 by obesity | <0.001 | ||
| No obesity | 2.24 (2.16,2.32) | <0.001 | |
| Obesity | 1.64 (1.55,1.75) | <0.001 | |
| DM2 by hypertension | <0.001 | ||
| No hypertension | 2.15 (2.05,2.25) | <0.001 | |
| Hypertension | 1.57 (1.50,1.64) | <0.001 | |
| DM2 by CVD | 0.015 | ||
| No CVD | 2.14 (2.07,2.21) | <0.001 | |
| CVD | 1.49 (1.31,1.71) | <0.001 | |
| HYPERTENSION | |||
| Hypertension by Obesity | <0.001 | ||
| No obesity | 1.82 (1.76,1.89) | <0.001 | |
| Obesity | 1.52 (1.43,1.61) | <0.001 | |
| Hypertension by DM2 | <0.001 | ||
| No DM2 | 1.62 (1.56,1.69) | <0.001 | |
| DM2 | 1.32 (1.25,1.39) | <0.001 | |
| Hypertension by CVD | 0.009 | ||
| No CVD | 1.80 (1.74,1.86) | <0.001 | |
| CVD | 1.42 (1.23,1.65) | <0.001 | |
| CVD | |||
| CVD by Obesity | 0.226 | ||
| No Obesity | 1.36 (1.25,1.49) | <0.001 | |
| Obesity | 1.42 (1.26,1.60) | <0.001 | |
| CVD by DM2 | 0.015 | ||
| No DM2 | 1.42 (1.29,1.56) | <0.001 | |
| DM2 | 1.17 (1.06,1.29) | <0.001 | |
| CVD by Hypertension | 0.009 | ||
| No Hypertension | 1.40 (1.24,1.59) | <0.001 | |
| Hypertension | 1.17 (1.08,1.28) | <0.001 |
Age and gender adjusted OR.
Nearly all of the interactions between MetS components were significant: obesity and DM2, p <0.001; obesity and hypertension, p <0.001; DM2 and hypertension, p <0.001; DM2 and CVD, p <0.015; hypertension and CVD, p <0.009; and only the combination obesity and CVD showed no significant interaction (p = 0.226) (Table 5).
Table 5.
Multivariate OR in total cases and confirmed cases
| Components number of MetS | Total Cases | Confirmed Cases |
|---|---|---|
| 0 | Reference | |
| 1 | 1.99 (1.93,2.05) | 1.83 (1.77,1.89) |
| 2 | 2.83 (2.74,2.92) | 2.58 (2.48,2.69) |
| 3 | 3.09 (2.94,3.25) | 2.83 (2.66,3.01) |
| 4 | 3.51 (3.09,4.00) | 3.36 (2.83,3.99) |
| Componet MetS | ||
| DM2 | 2.32 (3.02,3.13) | 2.09 (2.03,2.16) |
| Hypertension | 1.92 (1.87,1.97) | 1.82 (1.77,1.89) |
| Obesity | 1.51 (1.46,1.55) | 1.43 (1.38,1.48) |
| CVD | 1.47 (1.40,1.55) | 1.49 (1.39,1.60) |
| DM2+HAS | 2.069 (1.99,2.15) | 2.22 (2.15,2.28) |
| DM2+Obesity | 2.00 (1.92,2.09) | 1.82 (1.73,1.91) |
| DM2+CVD | 1.70 (1.58,1.84) | 1.82 (1.72,1.91) |
| Obesity+Hypertension | 1.73 (1.66,1.79) | 1.66 (1.58,1.73) |
| Hypertension+CVD | 1.55 (1.46,1.65) | 1.63 (1.50,1.77) |
| Obesity+CVD | 1.75 (1.61,1.92) | 1.79 (1.59,2.01) |
| DM2+Hypertension+ Obesity | 2.06 (1.96,2.16) | 1.90 (1.78,2.02) |
| DM2+Hypertension+ CVD | 1.73 (1.59,1.88) | 1.84 (1.64,2.06) |
| Obesity+Hypertension+ CVD | 1.84 (1.66,2.03) | 1.88 (1.65,2.14) |
| Obesity+DM2+CVD | 1.95 (1.73,2.20) | 1.97 (1.68,2.32) |
| Obesity+DM2+ hypertension+CVD | 2.05 (1.80,2.33) | 2.07 (1.74,2.46) |
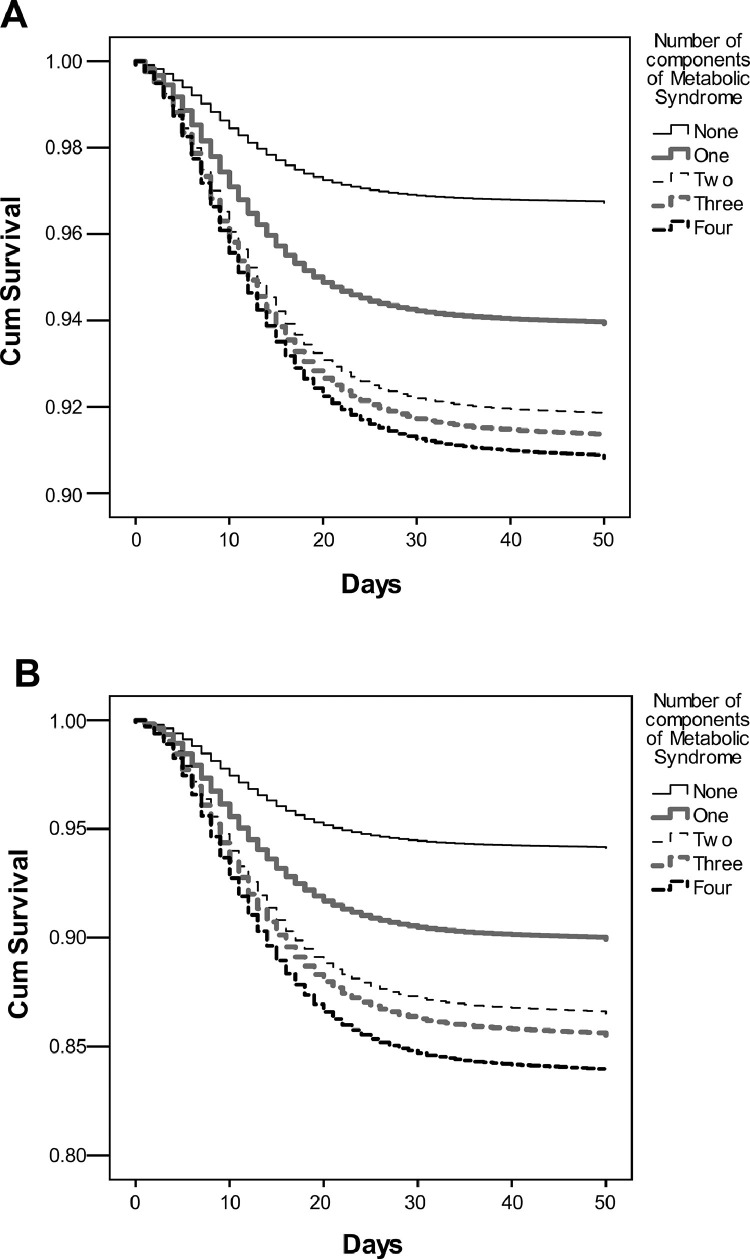
Subsequently, survival probability was calculated at 50 d, the period contemplating a wide range for death from the beginning of symptoms (17,18) for all patients and confirmed COVID-19 cases and based on the number of MetS components. In the group of total patients showing zero, one, two, three, and four MetS components, probability was 0.97, 0.95, 0.935, 0.927, and 0.92, respectively. These same probabilities were 0.937, 0.89, 0.87, 0.86, and 0.84 in the confirmed COVID-19 cases (Figure 1 ).
Figure 1.
Kaplan-Meier survival curves at 50 d for each Metabolic Syndrome component. A. All cases included. B. COVID-19 confirmed cases. Patients were stratified by the presence of cero, one, two, three and four MetS components. Different scales in Y axis were used.
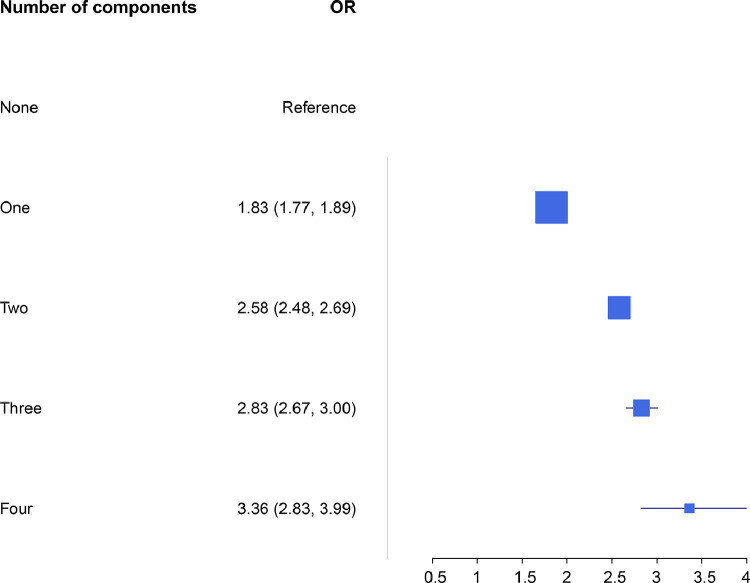
Finally, given that these comorbidities are frequent in older people, a multivariate analysis adjusted according to age and sex was carried out. Mortality OR for one, two, three, and four components regarding the reference value for total cases were 1.99 (1.93–2.05), 2.83 (2.74–2.92), 3.09 (2.94–3.25), and 3.51 (3.09–4.00). For confirmed COVID-19 cases, they were 1.83 (1.77–1.89), 2.58 (2.48–2.69), 2.83 (2.66–3.01), and 3.36 (2.83–3.99); for identified components in all cases they were DM2 2.32 (3.02–3.13), hypertension 1.92 (1.87–1.97), obesity 1.51 (1.46–1.55), and CVD 1.47 (1.40–1.55); and for confirmed cases they were DM2 2.09 (2.03–2.16), hypertension 1.82 (1.77–1.89), obesity 1.43 (1.38–1.48), and CVD 1.49 (1.39–1.60). When comorbidities were combined, OR for total and confirmed cases were DM2 and hypertension 2.07 (1.99–2.15) and 2.22 (2.15–2.28); DM2 and obesity 2.00 (1.92–2.09) and 1.82 (1.73–1.91); DM2 and CVD 1.70 (1.58–1.84) and 1.82 (1.72–1.91); obesity and hypertension 1.73 (1.66–1.79) and 1.66 (1.58–1.73); hypertension and CVD 1.55 (1.46–1.65) and 1.63 (1.50–1.77); obesity and CVD 1.75 (1.61–1.92) and 1.79 (1.59–2.01) When three components were combined, integrating a MetS diagnosis, results were DM2, hypertension, and obesity 2.06 (1.96–2.16) and 1.90 (1.78–2.02); DM2, hypertension, and CVD 1.73 (1.59–1.88) and 1.84 (1.34–2.06); obesity, hypertension, and CVD 1.84 (1.66–2.03) and 1.88 (1.65–2.14); obesity, DM2, and CVD 1.95 (1.73–2.20) and 1.97 (1.68–2.32); finally, results of four components combined were 2.05 (1.80–2.33) and 2.07 (1.74–2.46) (Table 4 and Figure 2 ).
Figure 2.
Floret's plot of probability of death in confirmed cases for COVID-19 according to the number of components of MetS. OR (CI 95%) for number of components of metabolic syndrome in patients with COVID-19 confirmed. Age and sex adjusted Multivariate analyses.
Discussion
The devastation caused by COVID-19 in humankind has evidenced key factors to prioritize in public health. Among them are actions leading to achieving an adequate metabolic and nutritional state in the population, leaving out the normalization of overweight and obesity. Mexico is an example of the degree of vulnerability that MetS and its components confer against the infection by SARS-CoV-2.
The results in this study prove that one MetS component in COVID-19 patients nearly doubles the risk of death, as compared against patients without MetS components. The combination of DM2 and hypertension increases this risk the most, regardless of age and sex. Furthermore, this study provides information on the contribution to risk of lethality by COVID-19 based on the number of MetS components patients show. We proved that the combination of obesity, DM2, hypertension, and CVD account for up to 60% of lethality.
This study analyzed OS and risk of death, both in confirmed cases of COVID-19 and the total number of patients. This prevents the exclusion of false negatives and patients who met the operational definition of viral respiratory disease and whose samples were not taken or did not meet the conditions for processing.
According to data from ENSANUT 2018, the prevalence of DM2 and hypertension in people over 20 years of age is 10.3 and 18.4%, respectively, representing around 24 million Mexicans (6). The data in our study show that any of the two comorbidities doubles the risk of mortality by COVID-19 with respect to the population without them. When these comorbidities are combined, the OR for the fatal outcome reaches 2.2 (2.15–2.28). Therefore, many adults are exposed to the highest risk of lethality.
We compared the results in this study against the work by Alamdari NH, et al. who also conducted a multivariate analysis to calculate the risk of mortality in 157 Iranian patients with COVID-19 admitted to the ICU and classified as not having and having MetS, including the number of components shown. The authors found that the presence of one and two MetS components conferred protection against death by COVID-19 with OR of 0.52 (0.21–1.29) and 0.53 (0.20–1.43) for one and two MetS components, respectively (19). In contrast, the OR we obtained for the same number of MetS components were 1.83 (1.77–1.89) and 2.58 (2.66–3.01). This contrast in results is mostly explained by the fact that Alamdari NH, et al. calculated OR based on the presence of three MetS components while our work was the absence of MetS components. In fact, the OR reported by the authors in the presence of three and four components were 1.95 (0.99–3.82) and 5.70 (2.02–16.08) while the OR in our population were 2.83 (2.66–3.01) and 2.36 (2.83–3.99), respectively. In addition to the reference used in the calculation of OR, Alamdari NH, et al. used the ATP III criteria to diagnose MetS, but we used stage D in Sperling's classification. Other factors that might create differences in OR are the difference in sample sizes, those in the combined prevalence of comorbidities, and, obviously, the interindividual biological differences of the population. However, we consider the difference in the comparison group makes the studies different. Furthermore, Alamdari NH, et al. might be biased when dismissing the contribution of the risk of mortality in the presence of one or two MetS components. In contrast, our work proves that one or two MetS components can double the risk in COVID-19 patients.
Additionally, Maddaloni E, et al. calculated the OR of different outcomes in a CoViDiab261 study of Italian population as follows: need for mechanical ventilation and admission to ICU or death in 354 COVID-19 patients with DM2 and in the presence of another cardiometabolic comorbidity (hypertension, dyslipidemia, CVD, COPS, or tumoral disease. They also used a logistic regression model adjusted according to age and sex. The study reported an OR of mortality in COVID-19 patients of 1.3 (0.5–3.10) and 2.8 (1–7.5) in the presence of DM2 and hypertension, respectively (20). Contrastingly, the OR in the present work were 2.09 (2.303–2.16) and 1.82 (1.77–1.89) for the same comorbidities. In both studies, comparisons were done against confirmed COVID-19 cases and zero comorbidities. In this case, the presence of DM2 posed a higher risk of death for the Mexican population than for Italians, but the opposite was true in the case of hypertension. To explain these differences, further details would be necessary on glycemic and blood pressure control in both works. It has been proven that fasting glucose levels and glycemic control in patients at the time of hospital admission are key in the outcome of COVID-19 patients. Higher glycemia levels and a lower glycemic control are linked to longer hospital stays and a higher mortality (21,22,23).
On the other hand, the study by Kammar-García A, et al. using Mexican population considered the presence of individual and grouped comorbidities (24). The authors observed a survival of 96.6% in the absence of comorbidities, 88.5% with one comorbidity, 81.8% with two comorbidities, and 73.7% in the presence of over three comorbidities. The survival reported was lower than that in our results. This could be the answer to the effect of other comorbidities (COPS, asthma, CKD, use of immunosuppressive therapy) considered along with MetS components. Among the MetS components linked to a higher risk of mortality, they observed HR of 1.9 (1.8–2.2) for DM, 1.8 (1.6–2.1) for obesity, 1.6 (1.5–1.8) for hypertension, and 1.3 (1.01–1.6) for CVD. These results were lower than those obtained in our analysis, likely due to the regression given that our study does not consider proportionality in time. In the analysis of combined comorbidities, they obtained a higher risk for all the combinations, except those related to CVD. This could be because the multivariate model was further adjusted to the presence of tobacco use and the time from onset of symptoms to medical attention. In contrast, we did not analyze the interaction with the combination of three MetS components.
In another study by Bello-Chavolla OY, et al. conducted using Mexican population, the authors observed that DM and obesity are two factors of risk of death, as observed in this work (25). This is especially important since these two diseases are chronic and highly prevalent among Mexicans. This study had some limitations regarding possible non-differential classification since it originates from a secondary source of information, obtained by self-reports. Since the information was obtained from a secondary source, we were unable to obtain the BMI and establish a diagnosis of obesity. On the other hand, it should be noted that, given the type of epidemiological surveillance for COVID-19, the most severe cases with the worst prognosis might be overrepresented. Still, this study also shows strengths, as having a large sample that allowed for extracting association measures with precise intervals, which agree with others observed in Mexicans. In addition, we analyzed the interactions established between MetS components, a phenomenon scarcely studied until now. In our analysis we also dealt with risk attributable to the presence of MetS components and their increase when they are present in COVID-19 patients.
Conclusion
Among the Mexican population, the presence of one component of MetS reduces the probability of survival by doubling the risk of death by COVID-19. The risk is even higher in patients who showed DM2 and hypertension while almost all combinations of components interact significantly. All the actions leading to an improvement of the population's metabolic state will greatly contribute to limiting the impact of COVID-19 in public health.
Acknowledgements
ORC and RFM acknowledge supports SIP20180722 and SIP20778.
References
- 1.Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Heatlh Organization. Coronavirus disease (COVID-19). https://covid19.who.int/. (Accessed February 20, 2021).
- 3.Richie H, Ortiz-Ospina E, Beltekian D, et al. Coronavirus Pandemic (COVID-19). 2021. https://ourworldindata.org/coronavirus. (Accessed February 8, 2021).
- 4.World Heatlh Organization. Health-topics/obesity. 2021. https://www.who.int/health-topics/obesity#tab=tab_1. (Accessed February 20, 2021).
- 5.International Diabetes Federation. 2021. https://idf.org/. (Accessed February 8, 2021).
- 6.Instituto Nacional de Salud Pública . Instituto Nacional de Salud Pública; México: 2018. Encuesta Nacional de Salud y Nutrición (ENSANUT) 2018. [DOI] [PubMed] [Google Scholar]
- 7.Grundy SM, Cleeman JI, Daniels SR, et al. An American Heart Association/National Heart Lung and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 8.Grundy SM. Metabolic syndrome pandemic. Artherioscler Thromb Vasc Biol. 2008;28:629–636. doi: 10.1161/ATVBAHA.107.151092. [DOI] [PubMed] [Google Scholar]
- 9.Sperling LS, Mechanick JI, Neeland IJ, et al. The CardioMetabolic Health Alliance: Working Toward a New Care Model for the Metabolic Syndrome. J Am Coll Cardiol. 2015;66:1050–1067. doi: 10.1016/j.jacc.2015.06.1328. PMID: 26314534. [DOI] [PubMed] [Google Scholar]
- 10.Wacher-Rodarte N., II Epidemiología del síndrome metabólico. Gac Med Mex. 2009;145:384–391. [PubMed] [Google Scholar]
- 11.Khan MMA, Khan MN, Mustagir MG, et al. Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: A systematic review and meta-analysis. J Glob Health. 2020;10 doi: 10.7189/jogh.10.020503. 020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Popkin BM, Du S, Green WD, et al. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020;21:1–17. doi: 10.1111/obr.13128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tamara A, Tahapary DL. Obesity as a predictor for a poor prognosis of COVID-19: A systematic review. Diabetes Metab Syndr. 2020;14:655–659. doi: 10.1016/j.dsx.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denova-Gutiérrez E, Lopez-Gatell H, Alomia-Zegarra JL, et al. The association of Obesity, Type 2 Diabetes, and Hypertension with Severe Coronavirus Disease 2019 on Admission Among Mexican Patients. Obesity. 2020;28:1826–1832. doi: 10.1002/oby.22946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Datos Abiertos Dirección General de Epidemiología. 2021. https://www.gob.mx/salud/documentos/datos-abiertos-152127 (Accessed June 25, 2020).
- 17.Sousa GJB, Garces TS, Cestari VRF, et al. Mortality and survival of COVID-19. Epidemiol Infect. 2020;148:e123. doi: 10.1017/S0950268820001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grasselli G, Greco M, Zanella A, et al. COVID-19 Lombardy ICU Network. Risk Factors Associated With Mortality Among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern Med. 2020;180:1345–1355. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alamdari NM, Rahimi FS, Afaghi S, et al. The impact of metabolic syndrome on morbidity and mortality among intensive care unit admitted COVID-19 patient. Diabetes Metab Syndr. 2020;14:1979–1985. doi: 10.1016/j.dsx.2020.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maddaloni E, DÓnofrio L, Alessandri F, et al. Cardiometabolic multimorbidity is associated with a worse Covid-19 prognosis than individual cardiometabolic risk factors a multicentre retrospective study (CoViDiab II) Cardiovasc Diabetol. 2020;19:164. doi: 10.1186/s12933-020-01140-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhu L, She ZG, Cheng X, et al. Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Matabolism. 2020;31:1068–1077. doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bode B, Garrett V, Messler J, et al. Glycemic Characteristics and Clinical Outcome of COVID-19 Patients Hospitalized in the United States. J Diabetes Sci Technol. 2020;14:813–821. doi: 10.1177/1932296820924469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang S, Ma P, Zhang S, et al. Diabetologia. 2020;63:2102–2111. doi: 10.1007/s00125-020-05209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kammar-García A, Vidal-Mayo JJ, Vera-Zertruche JA, et al. Impact of comorbidities in Mexican SARS-CoV2-Positive Patientes: A retrospective Analyses in a national cohort. Rev Invest Clin 202072:151–158. [DOI] [PubMed]
- 25.Bello-Chavolla OY, Bahena-López JP, NE Antonio-Villa, et al. Predicting Mortality Due to SARS-CoV-2: A Mechanistic Score Relating Obesity and Diabetes to COVID-19 Outcomes in Mexico. J Clin Endocrinol Metab. 2020;105:1–10. doi: 10.1210/clinem/dgaa346. [DOI] [PMC free article] [PubMed] [Google Scholar]