Abstract
The circadian clock exerts significance influence on the immune system and disruption of circadian rhythms has been linked to inflammatory pathologies. Shift workers often experience circadian misalignment as their irregular work schedules disrupt the natural light-dark cycle, which in turn can cause serious health problems associated with alterations in genetic expressions of clock genes. In particular, shift work is associated with impairment in immune function, and those alterations are sex-specific. The goal of this study is to better understand the mechanisms that explain the weakened immune system in shift workers. To achieve that goal, we have constructed a mathematical model of the mammalian pulmonary circadian clock coupled to an acute inflammation model in the male and female rats. Shift work was simulated by an 8h-phase advance of the circadian system with sex-specific modulation of clock genes. The model reproduces the clock gene expression in the lung and the immune response to various doses of lipopolysaccharide (LPS). Under normal conditions, our model predicts that a host is more sensitive to LPS at circadian time (CT) CT12 versus CT0 due to a dynamic change of Interleukin 10 (IL-10), an anti-inflammatory cytokine. We identify REV-ERB as a key modulator of IL-10 activity throughout the circadian day. The model also predicts a reversal of the times of lowest and highest sensitivity to LPS, with males and females exhibiting an exaggerated response to LPS at CT0, which is countered by a blunted immune response at CT12. Overall, females produce fewer pro-inflammatory cytokines than males, but the extent of sequelae experienced by males and females varies across the circadian day. This model can serve as an essential component in an integrative model that will yield mechanistic understanding of how shift work-mediated circadian disruptions affect the inflammatory and other physiological responses.
Author summary
Shift work has a negative impact on health and can lead to chronic diseases and illnesses. Under regular work schedules, rest is a night time activity and work a daytime activity. Shift work relies on irregular work schedules which disrupt the natural sleep-wake cycle. This can in turn disrupt our biological clock, called the circadian clock, a network of molecular interactions generating biochemical oscillations with a near 24-hour period. Clock genes regulate cytokines before and during infection and immune agents can also impact the clock function. We provide a mathematical model of the circadian clock in the rat lung coupled to an acute inflammation model to study how the disruptive effect of shift work manifests itself in males and females during inflammation. Our results show that the extent of sequelae experienced by male and female rats depends on the time of infection. The goal of this study is to provide a mechanistic insight of the dynamics involved in the interplay between these two systems.
Introduction
Most organisms from bacteria to humans are equipped with an internal biological clock, known as a circadian clock—a network of molecular interactions generating biochemical oscillations with a near 24-hour period [1]. In mammals, the circadian timing system consists of almost as many clocks as there are cells, as most cells house self-sustained and autonomous circadian oscillators [1]. This coordination of rhythms with the diurnal cycle is under the control of a central synchronizer, the suprachiasmatic nucleus (SCN), located in the ventral hypothalamus [2]. The SCN receives direct photic input from the retina, produces rhythmic outputs and orchestrates local clocks in the brain and peripheral clocks throughout the body [3].
Peripheral clocks can be coordinated by systemic cues emanating from the SCN [1], and they can be synchronized also by external cues such as temperature, feeding schedules and light [3]. In particular, the circadian circuitry in the lungs is exquisitely sensitive to environmental factors and exposomes [4], including air pollutants [5], cigarette smoke [6, 7], shift work [8–10], jet lag [11, 12], pathogens [13, 14] and much more. Of particular interest is the impact of circadian disruption on immune cell function, host defense and inflammation. The emerging picture is that the strength of the immune response varies throughout the day and that dysregulation of clock genes can lead to inflammatory disease or immunodeficiency [15].
Over the past decades, our societies have experienced rapid growth in the need for work in recurring periods other than traditional daytime periods. Research shows that shift work disrupts the natural sleep-wake cycle and feeding patterns [16], which may in turn cause serious health problems [17]. Here, we use mathematical modeling to study the effects of shift work, also known as chronic jet lag (CJL), on the lung circadian clock and consequently the immune response to inflammation. We address important questions: How do interactions between clock genes affect the strength of the inflammatory response at CT0 compared to CT12? Does the disruptive effect of shift work manifest itself differently in males and females? If so, what are the clock genes responsible for the sex-specific responses? Existing mathematical models of the circadian clock that focus on immunity can be classified into two categories: 1) models of the interplay between circadian rhythms and the immune system via neuroendocrine players (e.g. melatonin, cortisol) [18–20]; 2) models for the NF-κB network modulated by the circadian clock [21]. The former do not model the core clock machinery, but rather use rhythmic hormones such as cortisol to drive the circadian variations in the system. The latter include the core clock system but with unidirectional coupling from the clock to the immune system. It is now known that the immune system can affect the circadian clock in a reciprocal manner [15, 22]. Given this observation, we have developed a model of the core circadian clock genes and proteins and their reciprocal interactions with the immune system under acute inflammation. Our mathematical model was extended to include the effect of shift work, represented as an 8h-advance of the circadian phase with sex-specific alterations in the expression of clock genes and proteins (see Fig 1).
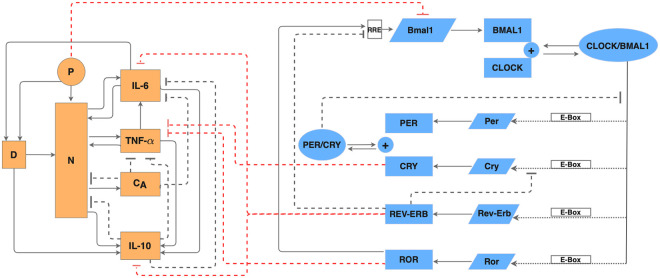
Fig 1. Regulatory network of the coupled immune system and circadian clock.
Schematic diagram of the acute immune response model (orange shapes) and the circadian clock (blue shapes) in the lung of a rat. In the circadian clock model, slanted boxes denote mRNAs; blue rectangles denote proteins; ovals denote protein complexes. Dotted arrows represent transactivation; blunt dashed arrows represent inhibition. In the acute inflammation model, P denotes endotoxin; D, damage marker; N, activated phagocytic cells; CA, slow-acting anti-inflammatory cytokines.
The immune system is under control of the circadian clock. A primary means of circadian control over the immune system is through direct interactions of clock proteins with components of key inflammatory pathways such as members of the NF-κB protein family [22]. This regulation is independent of transcription and allows the immune system to also reciprocally exert control over the function of the circadian clock [22]. Our model, which is composed of core clock genes (Bmal1, Per, Cry, Rev-Erb and Ror) and their related proteins as well as the regulatory mechanism of pro- and anti-inflammatory mediators (e.g. IL-6, TNF-α and IL-10), predicts temporal profiles of clock gene expression and cytokine expression during inflammation. This allows us to study how immune parameters respond to shift work-mediated circadian disruption. Moreover, we compare how the disruptive effect of shift work manifests itself differently in males and females.
Materials and methods
We developed a mathematical model for simulating the circadian clock in the lung of a rat, the immune system under acute inflammation, and the interactions between the two systems. A schematic diagram that depicts the regulatory network is shown in Fig 1. Model equations and parameters can be found in Tables A-J in S1 File.
Circadian clock in the lung
The mammalian clock consists of interlocked transcriptional-translational feedback loops that drive the circadian oscillations of core clock components [23]. Both the master and peripheral clocks share essentially the same molecular architecture [24]. The activators CLOCK and BMAL1 dimerize to induce the transcription of target genes, including the Period genes (Per1, 2, 3), Cryptochrome genes (Cry1, 2), retinoic acid-related orphan receptor (Rora, Rorb, Rorc) and Rev-Erb nuclear orphan receptor (Rev-Erbα, Rev-Erbβ) to activate their transcription [1]. PERs and CRYs then heterodimerize and enter the nucleus to inhibit their own transcription by acting on the CLOCK-BMAL1 protein complex, and thus form the main feedback loop [1, 25, 26]. In the secondary loop, the nuclear receptors REV-ERBα, β and RORa, b, c compete for ROR regulatory element (RRE) binding sites in the promoter region of Bmal1 and respectively repress and activate its transcription. The REV-ERBs, which also repress Cry1 transcription [27], are essential for robust oscillations [28–30]. See the clock network in Fig 1, and refer to Refs. [3, 26, 28] for a detailed overview of the molecular clock architecture.
The present lung circadian clock model, inspired by Ref. [31], describes the time evolution of mRNA and corresponding protein concentrations of Per, Cry, Rev-Erb, Ror, and Bmal1, and their modulation of proximal tubule epithelial transport [32]. Following the model assumptions in Ref. [31], we grouped the three Period homologs (Per1-3) as a single Per gene and the two cryptochromes (Cry1,2) as a single Cry gene. Similarly, the two isoforms Rev-Erbα and Rev-Erbβ and three isoforms Rora, Rorb and Rorc are represented by single variables Rev-Erb and Ror, respectively. It was assumed that the CLOCK protein is constitutively expressed. We did not include post-translational protein modifications, considering that transport between the cytoplasm and the nucleus is rapid on a circadian timescale [33]. The time evolution of the core clock genes and proteins is described by Eqs. 1–12 in Table B in S1 File.
Acute immune response
The acute immune response model, inspired by Refs. [34] and [35] with some modifications, consists of eight variables: endotoxin concentration (P); the total number of activated phagocytic cells (N, which includes activated immune response cells such as neutrophils and monocytes); a non-accessible tissue damage marker (D); concentrations of pro- and anti-inflammatory cytokines, namely IL-6, TNF-α and IL-10; a tissue driven non-accessible IL-10 promoter (YIL10); and a state representing the level of slow acting anti-inflammatory mediators (CA), which comprises slow-acting anti-inflammatory agents such as cortisol and TGF-β1. Model assumptions can be found in Refs. [34] and [35].
The introduction of bacterial insult in the system activates the phagocytic cells, N, and inflicts direct tissue damage, D [36]. This is different from the work of Roy et al. [34] in which endotoxin only activates phagocytic cells. The activated cells up-regulate the production of inflammatory agents (TNF-α, IL-6, IL-10, and CA) [37]. The pro-inflammatory cytokines TNF-α and IL-6 exert a positive feedback on the system by further activating N, as well as up-regulating other cytokines [37, 38]. The anti-inflammatory cytokines IL-10 and CA, on the other hand, have a negative feedback on the system. They inhibit the activation of N and other cytokines [39, 40]. The model also incorporates tissue damage, represented by a non-accessible damage marker, D. Tissue damage further up-regulates activation of N [41] and also contributes to up-regulation of IL-10 [42, 43]. In our model, D is up-regulated by IL-6 because it has been shown that IL-6 is associated with the development of sepsis [44–46]. This differs from Ref. [34] in which damage is up-regulated by N. Note also that D should not be interpreted directly as a cell type in the model. The acute inflammatory response is described by Eqs. 13–20 in Table B in S1 File; see also Fig 1.
Coupling between the circadian clock and the immune system
Most studies on circadian-immune interactions have focused on Bmal1, since inactivation of this gene is a convenient way to abrogate clock function [13, 47, 48]. Thus, care should be taken in distinguishing Bmal1-specific effects from downstream effects because other clock components act as intermediaries. The inhibitory effects that the circadian clock and the inflammatory response have on each other are shown in Fig 1. Specifically:
CRY proteins. Cry1−/−Cry2−/− mice exhibit an elevated number of T cells in the spleen with increased TNF-α levels [22, 49]. Other studies showed that Cry1 and Cry2 double KO in fibroblasts and bone-marrow-derived macrophages (BMDMs) leads to increased Il6 and Tnf-α mRNA and an hypersensitivity to lipopolysaccharide (LPS) infection [15, 50]. Furthermore, the NF-κB signaling pathway was shown to be constitutively activated in Cry1−/−Cry2−/− BMDMs [50]. Due to the ensuing higher constitutive inflammatory state, Cry1−/−Cry2−/− mice exhibit increased infiltration of leukocytes in lungs and kidneys [51]. Therefore, CRYs play an important anti-inflammatory role by downregulating inflammatory cytokines. Because IL-6 is inducible with TNF-α, effects on IL-6 in CRY double KO experiments are primarily mediated by TNF-α [50]. In our model, CRY directly inhibits the production of TNF-α, hence indirectly inhibits the TNF-α-induced IL-6 production (Eq. 17 in Table B in S1 File).
ROR proteins. Similarly to the CRY proteins, experiments have shown that Rora−/− mice, also known as the staggerer mutant, exhibit higher levels of IL-6 in bronchoalveolar lavage fluid, which renders them more susceptible to LPS lethality [52]. Interestingly, staggerer mutant mice have an increased production of IL-6 and TNF-α in mast cells and macrophages after LPS stimulation [53, 54]. Furthermore, overexpression of RORa in human primary smooth muscle cells inhibits TNF-α-induced expression of IL-6 [55]. The present model assumes that ROR downregulates TNF-α, thus indirectly downregulates IL-6 (Eq. 17, Table B in S1 File). Recall that the model does not distinguish between the three isoforms Rora, Rorb and Rorc.
REV-ERB proteins. There is compelling evidence for a role for REV-ERBα in the control of the immune system. REV-ERBα is encoded by Nr1d1 and in vivo challenge of Nr1d1−/− mice with LPS leads to IL-6 upregulation in serum in comparison to wildtype animals [56]. REV-ERBα represses Il6 expression not only indirectly through an NF-κB binding motif but also directly through a REV-ERBα binding motif in the murine Il6 promoter region [57]. A more recent study showed that the dual mutation of REV-ERBα and its paralog REV-ERBβ in bronchial epithelial cells further augmented inflammatory responses and chemokine activation [58]. REV-ERBα also negatively affects the expression of anti-inflammatory cytokine IL-10. Rev-ErbαmRNA binds to the IL-10 proximal promoter and represses expression in human macrophages [59]. Together, these studies reveal the role of REV-ERBα as an equilibrist. In our model, REV-ERB directly inhibits the production of IL-6 and IL-10 (Eqs. 16 and 18 in Table B in S1 File, respectively). We note that the two isoforms Rev-Erbα and Rev-Erbβ are represented by a single model variable Rev-Erb.
Inflammation. In a reciprocal manner, inflammation induced by agents such as LPS, TNF-α, and IFN-γ [60–64] or acute bacterial infection [65] can affect the circadian clock. In particular, rodent studies indicate that LPS transiently suppresses clock gene expression and oscillations in the SCN and peripheral tissues [33, 64, 66, 67]; notably, a number studies show significant suppression of Bmal1 [15, 66, 68]. The inhibition of the circadian mechanism during endotoxemia lasts for at least 24 h [64, 68]. To represent the sustained effect of a bacterial infection on the circadian clock, we introduced a filter function for LPS (Eq. 21 in Table B in S1 File), which acts on the clock through its inhibition of Bmal1 (Eq. 5 in Table B in S1 File). The filter function decays linearly over 24h and causes circadian disruption for at least this amount of time. We assume that the effects of cytokines such as TNF-α are incorporated in the net effect of LPS on clock genes, and so we do not include direct links from cytokines to clock genes and proteins.
Model parameters
Most of the model parameters are not well characterized, and were estimated by fitting model dynamics to experimental data. Due to the transient nature of acute inflammation, this is done in a two-step process: we first fit the circadian clock model in isolation, in an infection-free state. In the absence of infection, the acute inflammation model is idle and therefore has no influence on the expression of clock genes. Likewise, clock genes have no effect on inflammation variables whose initial conditions are zero. The fitting of the clock model is done using data on the expression of circadian genes in the mouse lung (CircaDB:http://circadb.hogeneschlab.org). Animals were entrained to a 12h light:12h dark schedule for one week, then released into constant darkness. Clock gene expression was recorded starting at CT18 postrelease [69]. It is noteworthy that the present model is based on the rat, whereas the parameters for the circadian clock were based on mouse data. However, while species differences exist, core clock gene expressions of the mouse and rat lungs exhibit substantial similarities [70]. Our model inherits the period of the data which is 24 h.
In a second step, we fit the acute inflammation model together with the clock-inflammation coupling, without changing the circadian clock parameters. This is done by simultaneously fitting experimental measurements of the cytokines IL-6, TNF-α, and IL-10 in rat following the administration of endotoxin at 3 mg/kg and also at 12 mg/kg [34, 35]. In other words, we fit the time profiles for all variables (P, D, N, CA, IL-6, IL-10, TNF-α) using measured data on IL-6, IL-10 and TNF-α only. This fitting was conducted with the coupling with the clock model taken into account. Some parameters in the model were specified. The clearance rate of endotoxin, P, captured by the parameter dP in Eq. 13 was obtained from the literature [71, 72]. Parameters sIL10 and sCA from Eqs. 18 and 20 were extracted directly from the experimental data, respectively [34]. Model parameters are shown in Tables C–J in S1 File.
Parameter estimation technique
Parameter identification for the coupled system was carried out with a nonlinear least-squares method with a normalized residual, which minimizes the error between the computed model output and the experimental data. To this end, we defined:
| (1) |
Here, yi, is the measured data at time ti. The model prediction is given by y(ti, θ), where θ represent model parameters. Q is the total number of data points. Experimental error bars were not taken into account. The cost function that we minimize is given by:
| (2) |
The subscripts 3 and 12 refer to the injected dose of endotoxin (mg/kg). As proposed in Ref. [73], the cost function has been minimized by using an optimization function in MATLAB known as fminsearch to search for the parameter estimated values which give the best fit of the model to the experimental data. Still, obtaining our final result required a series of educated guesses, manually correcting the most obvious difference before restarting the optimization. We have found that the parameter values are not uniquely determined, as different sets of parameters provide almost the same goodness of fit. In order to assess the relative influence of each parameter on the outcomes, we performed a sensitivity analysis using the Sobol’ method (S1 File).
Sexual dimorphism in clock gene alterations under circadian disruption
In their 2012 study, Hadden et al. reported sexual dimorphism in clock gene expression in the lungs of mice exposed to chronic jet lag [12]. Male and female mice were assigned to either remain in a LD12:12 regimen or to undergo experimental chronic jet lag (CJL). Under the CJL regimen, mice were subjected to serial 8-h advances of the light/dark cycle every 2 days for 4 weeks. Then using quantitative Polymerase chain reaction (PCR) to measure the relative amount of clock gene mRNAs, Hadden et al. observed that Rev-Erbα gene expression is upregulated in CJL males and downregulated in CJL females by 98% and 70% on average, respectively. Bmal1 is downregulated in CJL females only by 43% on average, while Clock, which forms a heterodimer with Bmal1 (CLOCK:BMAL1) [69], is downregulated in males only by 26%. The repressors Per2 and Cry2 are both upregulated when compared with same-sex control animals, although Cry2 upregulation was not significant for CJL males. In particular, Per2 and Cry2 increased by 497% and 69%, respectively in CJL female mice, while Per2 increased by 230% in CJL male mice. The authors did not test the effects of chronic jet lag on Ror gene expression. This could be explained by the fact that Ror is not directly related to the shift work phenotype. Indeed, the association between Ror and shift work disorder has been shown to be weak at best [74].
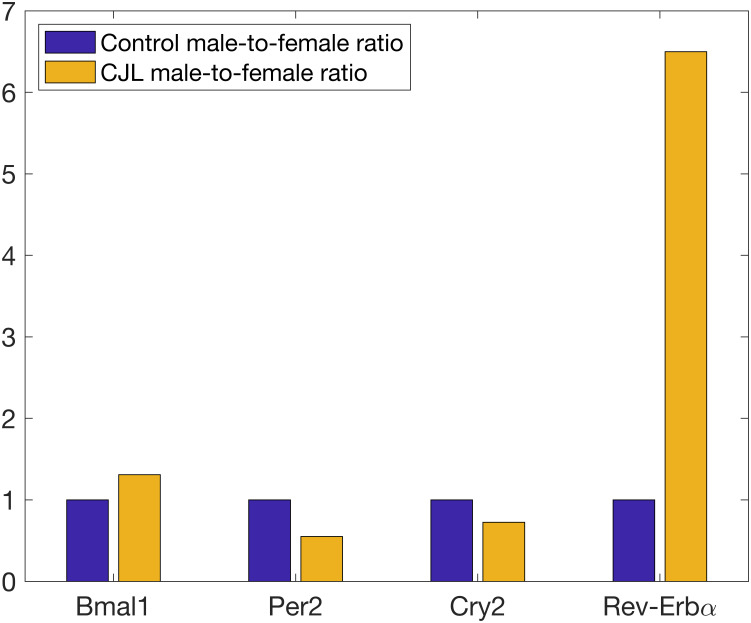
We used this information to create separate mathematical models of the lung circadian clock for males and females undergoing CJL. The decrease in Clock mRNA for CJL males is not taken into account because we do not model this gene explicitly and only constitutively represent the associated CLOCK protein. In addition, NPAS2, a paralog of CLOCK, has been shown to compensate for the loss of CLOCK in peripheral circadian oscillators [75, 76]. We note also that the baseline immune system likely differs between the sexes, but due to insufficient quantitative data, we were only able to construct one baseline model. Fig 2 shows the male-to-female relative abundance of mRNAs for controls and shifters, as reported by Hadden et al., normalized by control male-to-female ratios.
Fig 2. Male-to-female relative abundance of mRNAs for controls and shifters, normalized by control male-to-female ratios.
A method similar to that of the baseline system was used for the calibration of the CJL male and CJL female models. Hadden et al. did not measure clock gene expression over a 24-hour period, which would have allowed identification of rhythm differences, i.e. mesor, amplitude and phase expression of these genes, but rather reported the average expression level of clock genes. We have therefore modified the cost function, Eqs 1 and 2, to minimize the error between the average gene concentration in our models and the experimental data. A comparison between the change in mean gene expression between our models and experimental data is available in Table L in S1 File.
Only a few parameters changed drastically from the nominal values in the baseline model. Thus, we fixed the parameters that had not changed much, and repeated the calibration with a reduced set of free parameters for the CJL models: 6 parameters for the male CJL model and 10 parameters for the female CJL model. CJL model parameters can be found in Table K in S1 File. This process resulted in a change in the average concentration of clock genes in CJL models to the levels specified by the data. Consequently, the amplitude of the oscillations increased or decreased depending on the direction of the change. A previous study using the same experimental protocol has recorded sustained alterations to the average gene concentration as well as the amplitude of clock genes in the SCN and peripheral tissues [77].
At the time of this study, [12] is the only work known to us that reports quantitative data on the sexual dimorphism of clock gene expression in the lungs of mice exposed to CJL. However, other studies involving only male rats or mice have recorded changes similar to CJL males [77, 78].
Results
Expression of clock genes in lungs is accurately reproduced by the model
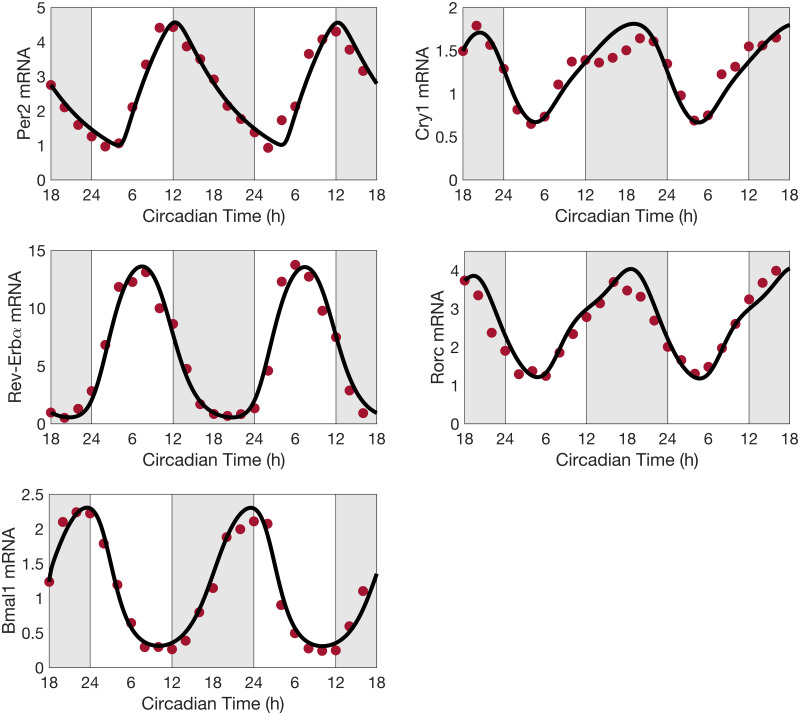
Using the baseline model parameters (Tables C-J in S1 File), the circadian clock model predicts limit-cycle oscillations in the expression levels of all clock components with a system period of 24 h. Fig 3 compares the predicted time profiles of Bmal1, Per, Cry, Rev-Erb and Ror with experimental observations for Bmal1, Per2, Cry1, Rev-Erbα and Rorc. We refer to the onset of the rest phase of night-active organisms as CT0 and to the onset of activity as CT12 [79]. These two times correspond to the onset of the light and dark phases, respectively. Good agreement can be observed between the predicted and experimental temporal profiles. Note that the parameter estimation procedure above concerns the baseline model and does not involve CJL. Thus, all CJL results are model predictions.
Fig 3. Predicted clock gene time profiles.
Comparison of predicted time profiles (solid lines) for Per, Cry, Rev-Erb, Ror and Bmal1, with experimental data (circles) for Per2, Cry1, Rev-Erbα, Rorc, and Bmal1 mRNA expression levels obtained in mouse lungs in constant darkness. Gray shading and white regions correspond to activity and restcycles, respectively.
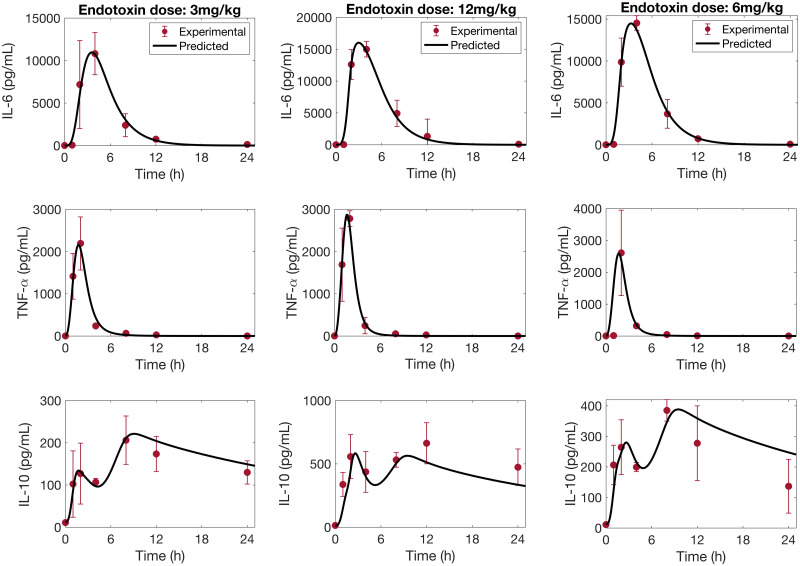
Cytokine dynamics during endotoxemia are accurately reproduced by the model
We estimated the parameter values for the acute inflammation model by simultaneously fitting experimental measurements of the cytokines IL-6, TNF-α, and IL-10 at endotoxin doses 3mg/kg and 12mg/kg. The predicted time profiles are shown in Fig 4, left and center columns. The model performs similarly well for all three cytokines, and is able to capture the second peak in IL-10 expression. We note that the predicted IL-10 concentrations at 1 h and after 10 h are slightly underestimated compared to the value recorded experimentally for the endotoxin dose 12mg/kg.
Fig 4. Predicted cytokine time profiles.
Comparison of predicted time-courses of IL-6, TNF-α and IL-10 (solid line), against experimental data (circle) (mean ± SD), in response to endotoxin challenge at dosages of 3 mg/kg, 12mg/kg and 6mg/kg.
Model predictions were validated by comparing model simulations with available cytokine data at a 6 mg/kg endotoxin challenge level. These data were not used in the parameter fitting. The results are shown in Fig 4, right column. In general, model predictions of the measured cytokines are in good agreement with the experimental data. We observe that TNF-α concentration is overestimated at 1 h. This discrepancy may be explained by the apparent inconsistency between the data collected at 1 h with samples collected at the same time point for endotoxin dose levels of 3 and 12 mg/kg. A similar model behavior was observed in the initiating article [34]. We note also that the model over-predicts IL-10 concentration after 12 h.
Effect of infection timing on immune response
It is well established that the survival of rodents after endotoxemic shock varies with the time of administration of bacterial insult. Studies have shown an increased lethality towards the end of the resting phase in controlled light-dark experiments [56, 80, 81]. Since an organism’s ability to fight off an infection depends in part on having a sufficiently large population of cytokines, we investigate how the timing of infection affects cytokine dynamics. Interestingly, a discrepancy can be discerned in post-infection IL-10 dynamics: some studies reported a single peak [82], whereas others reported two peaks [34]. We hypothesize that this discrepancy can be explained by the different infection timing (unfortunately infection timing was not reported in those studies).
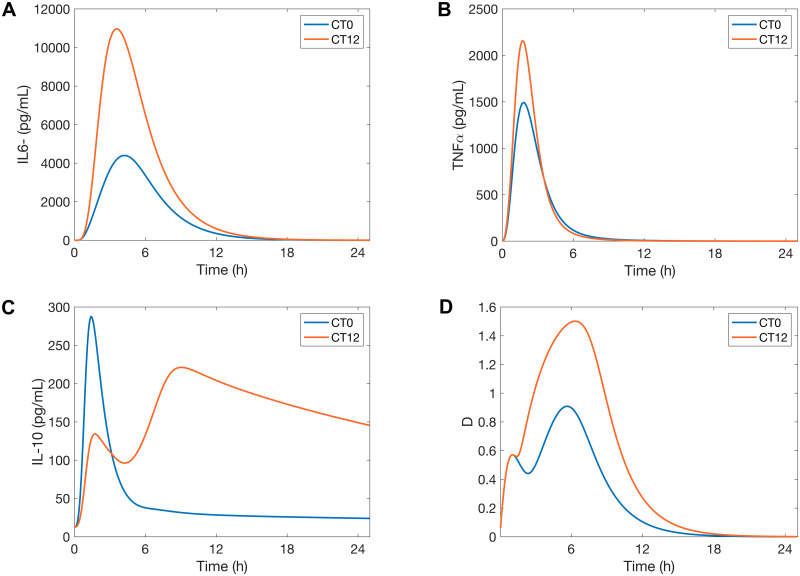
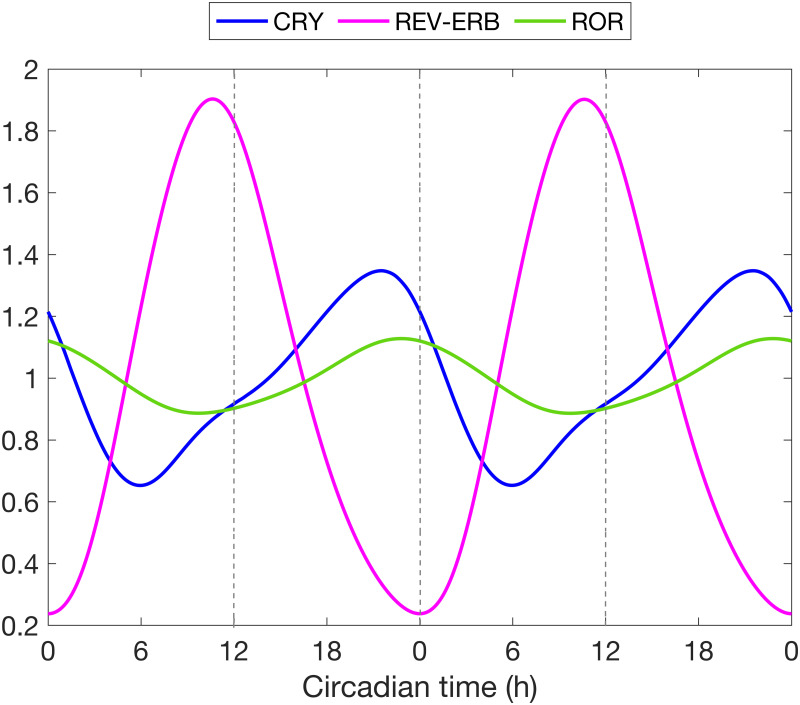
We first seek to explain how the time of infection affects its lethality. Model simulations predict more tissue damage results from an infection administered at CT12 compared to CT0 (Fig 5D). This difference can be explained in terms of the organism’s sensitivity to LPS, which is predicted to be highest at CT12, consistent with the observed phenotype of increased cytokine release [15, 56]. This increased sensitivity to LPS can be explained by a mismatch in the acrophases of REV-ERB and ROR in particular. Fig 6 shows the phase relations between CRY, REV-ERB and ROR. REV-ERB crests while ROR attains its minimum at CT12. Thus ROR inhibition of TNF-α and IL-6 is considerably reduced, hence allowing for a greater production of the cytokines. At the same time, the inhibition of IL-6 and IL-10 by REV-ERB is maximized, but since IL-10 also inihibits IL-6, its inhibition by REV-ERB repeals its action on IL-6, leading IL-6 to more than double (Fig 5A). We note that TNF-α increases less than IL-6 due to the inhibitory action of CRY which increases as REV-ERB decreases (see Figs 1 and 6). The larger increase in cytokine populations following a CT12 infection results in more tissue damage, compared to a CT0 infection (Fig 5).
Fig 5. Inflammatory response after infection at CT0 and CT12.
Model simulations of the time course of IL-6, TNF-α, IL-10 and the damage marker for the control model in response to endotoxin dose 3mg/kg administered at CT0 and CT12.
Fig 6. Phase relations between CRY, REV-ERB and ROR.
Baseline model simulation of the main clock genes involved in the inflammatory response. Normalized temporal expression profiles of CRY, REV-ERB and ROR proteins, relative to their respective mean value.
It is noteworthy that our model predicts a single peak in the expression of the anti-inflammatory cytokine IL-10 when the host is infected at CT0 versus two peaks when the infection occurs at CT12 (Fig 5C). This behavior persists across different doses of endotoxin (results not shown), which indicates that the immune response might be different at CT0 compared to CT12 regardless of the extent of the infection. We hypothesize that the different timing of infection may explain the single peak versus two peaks in IL-10 time profiles in previous studies [34, 82]
A closer look at the dynamics of REV-ERB revealed the following: at CT0 and without infection, REV-ERB is close to its minimum. An attack by pathogens inhibits Bmal1, causing REV-ERB to drop below its nadir. This is followed by an almost complete loss of IL-10 inhibition by REV-ERB, and thus leads to a single IL-10 spike. The high levels of circulating IL-10 limit the production of proinflammatory cytokines (Fig 5A and 5B). On the contrary, REV-ERB is close to its maximum at CT12, and while an attack by pathogens inhibits its production, REV-ERB concentration remains sufficiently high for the first few hours. Therefore, REV-ERB still inhibits IL-10 during the early stages of inflammation and only a weak peak in IL-10 emerges. This inhibitory action is later counteracted by the accumulation of circulating IL-6 and TNF-α which upregulate IL-10 production, hence explaining the rise of a second peak in IL-10 when the infection occurs at CT12. About ten hours after the onset of inflammation, REV-ERB finally drops below its normal minimum levels. This is similar to the case at CT0, and leads to sustained elevated levels of IL-10 for a few hours after the elimination of IL-6 and TNF-α. We hypothesize that the lower production of pro-inflammatory cytokines at CT0 is due to high levels of IL-10, which spikes earlier during endotoxemia due to the loss of REV-ERB. The second peak in IL-10 production can be an indicator of a stronger inflammatory response as can be seen at CT12.
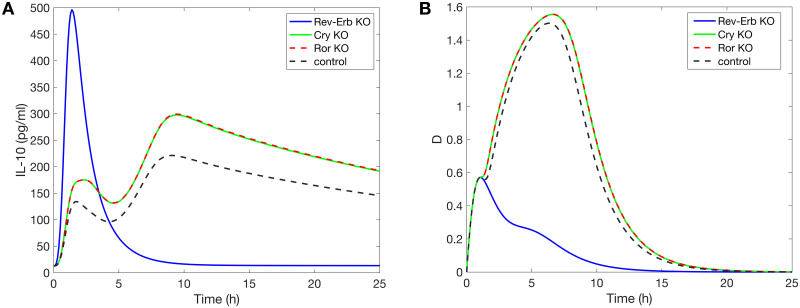
To test our hypothesis, we simulate acute inflammation under three scenarios at CT12: Rev-Erb KO, Cry KO and Ror KO. Fig 7A shows that the loss of Rev-Erb leads to a loss of the second peak of IL-10, while the absence of Cry or Ror does not give rise to qualitatively different dynamics. As expected, a CT12 infection following Rev-Erb KO produces results similar to a CT0 infection (see Fig 5) because in both cases the concentration of the REV-ERB is at a minimum or even zero. Additionally, the damage marker is greatly reduced by the loss of Rev-Erb (Fig 7B). This is due to the increased inhibition of D by IL-6 following the sharp increase in the anti-inflammatory cytokine IL-10. In this case, the damage marker indicates an inadequate immune response because not enough inflammatory cytokines are produced to fight the infection. In conclusion, the different timing of infection may indeed explain the single peak versus two peaks in the IL-10 temporal profiles.
Fig 7. Knockout experiment at CT12.
Model simulations of the time course of IL-10 (A) and the damage marker (B) in response to endotoxin dose 3mg/kg administered CT12. Three scenarios are simulated: Rev-Erb KO, Cry KO and Ror KO.
Circadian disruption alters host immune response
It has been reported that a challenge of LPS in rodents with a disrupted circadian clock leads to a stronger inflammatory response and increased mortality [83, 84]. Particularly, Castanon-Cervantes et al. observed a sustained reduction in Bmal1 transcript following CJL [84]. This is similar to findings by Hadden et al. for female mice [12]. Below we conduct simulations to illustrate that how circadian disruption alters immune response depends on (i) the time of infection, and (ii) the sex of the organism.
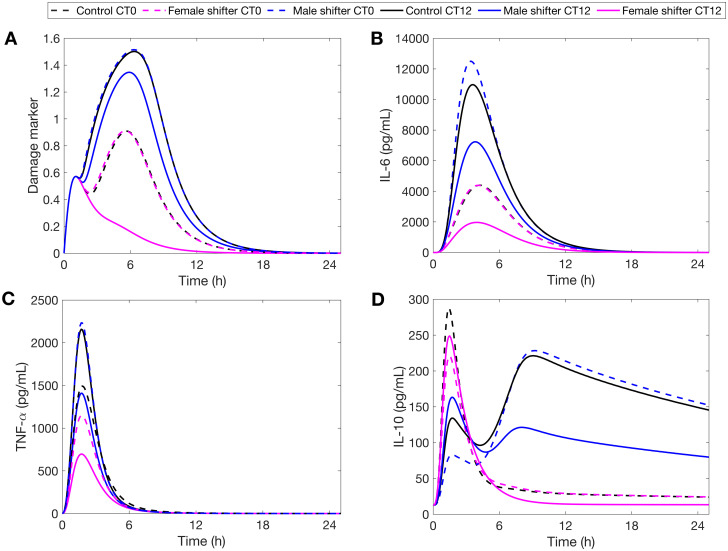
When endotoxin is administered at the onset of the rest phase (CT0), our model predicts an increased production of IL-6 and TNF-α in CJL males compared to controls (Fig 8B and 8C). Similar results were shown in experiments on CJL male mice [85] and CJL male rats [86] where the animals were injected with LPS during the early rest period. This stronger response is also observed in CJL females, and is due to the 8h-advance circadian disruption which resets their clock to the middle of the active phase. In contrary, CJL females remained relatively close to baseline compared to their male counterparts (Fig 8). Unlike males, the upregulation of CRY in CJL females decreases TNF-α and IL-6 production, while the downregulation of REV-ERB leads to increased levels of IL-10 and therefore more IL-10-induced IL-6 inhibition. In sum, CJL rats suffer more tissue damage from LPS administered at CT0, with CJL males more so than females (Fig 8A).
Fig 8. Sex-specific response to infection during CJL at CT0 and CT12.
Model simulations of the time course of IL-6, TNF-α, IL-10 and the damage marker for controls (black) against CJL males (blue) and CJL females (pink) in response to endotoxin challenge of 3mg/kg administered at CT0 and CT12.
The trend is reversed at CT12. Fig 8 shows that CJL rats have blunted IL-6 and TNF-α responses. We recall that REV-ERB is upregulated in CJL males compared to CJL females and controls (Fig 2D). Higher levels of REV-ERB further inhibit the production of IL-10, which then releases its inhibitory action on pro-inflammatory cytokines. This explains why CJL males, while having a blunted immune response, still produce more cytokines than CJL females. The downregulation of IL-6 following CJL has also been observed in all-male mice experiments [87–89]. Moreover, the weaker immune response in both CJL males and females is explained by their internal circadian disruption (8-h phase advance) which puts them at a circadian phase similar to CT4 in control rats. The reduced production of cytokine is represented by a lower damage marker and could indicate an inadequate and disrupted immune response (Fig 8A), particularly for CJL females. We note that the damage marker for CJL females (Fig 8A) is similar to that of the Rev-Erb KO experiment (Fig 7A). This highlights the role of REV-ERB in promoting an adequate immune response. Our model predictions at CT12 are consistent with experimental reports that the immune system in females is detrimentally affected more than that of males during CJL [90].
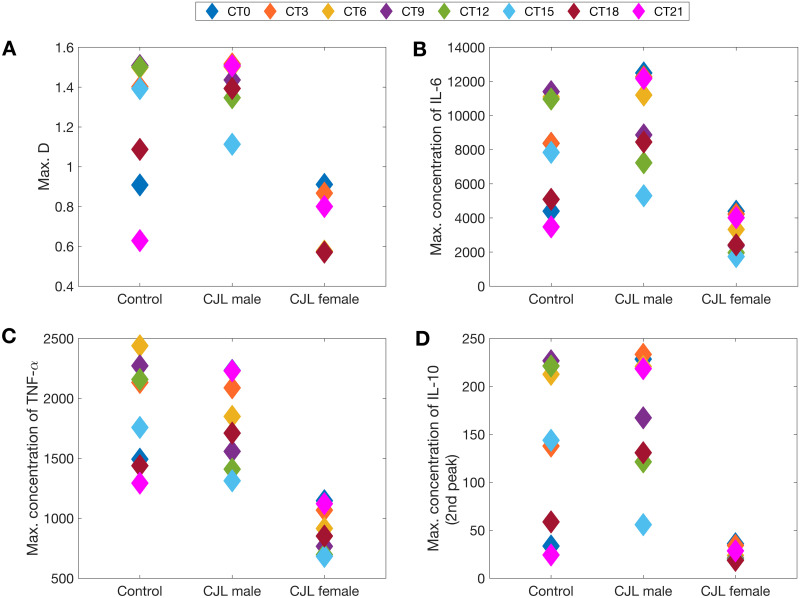
Effect of infection timing on immune response: Beyond CT0 and CT12
Previous studies have shown, in the absence of CJL, increased lethality towards the end of the resting phase, approximately 2 h before the onset of activity [80, 81]. We tested our baseline (no CJL) model predictions for different time points of infection, and indeed our results show higher sensitivity to LPS infection at CT9, followed closely by CT12 (see Fig 9).
Fig 9. Simulated acute inflammation across different circadian times.
IL-6 (A), TNF-α (B), IL-10 (C), Damage marker (D). The endotoxin dose is 3mg/kg. Left column, no CJL; middle column, CJL females; right column, CJL males.
We also conducted simulations under CJL. As shown in Fig 9, CJL males and females are more sensitive to LPS than controls at CT0, and exhibit reduced induction of cytokines at CT12. This supports our hypothesis that the CJL induced by an 8-h phase advance of the lung circadian clock would reverse the times of lowest and highest sensitivity to LPS. Interestingly, CT18 appears to be a time of lesser sensitivity to LPS regardless of the experience of the host: CJL or normal lighting conditions (Fig 9).
In general, the extent of sequelae experienced by male and female rats varied across the circadian day. Females had a more disrupted inflammatory response closer to CT12. Fig 9D shows that CJL females were not able to recover the second peak in IL-10 at any of the times tested. This means that CJL females did not produce as much pro-inflammatory cytokines (e.g. CT9, CT12) as controls. Compared to CJL males, CJL females produce less cytokines overall during acute inflammation. Males, however, lost their circadian gating of cytokines closer to CT0 (see Fig 9: CT21, CT0) and produced greater amounts of pro-inflammatory cytokines, making them more susceptible to sepsis at that time [91, 92].
Discussion
The circadian clock is responsible for the daily rhythms in immune functions [93]. A growing body of research supports the role of clock genes in regulating cytokines before and during infection [94]. In a reciprocal fashion, immune agents can impact the clock [95]. To investigate the interplay between the immune system and the circadian clock, we developed a mathematical model incorporating the bidirectional coupling between the lung circadian clock and the acute inflammatory response. We adapted this model to study the sexual-dimorphic effects of shift work (a.k.a. CJL) on both the clock mechanism and inflammation. It has been recognized that shift work has a negative impact on health [96] and a better understanding of the mechanisms by which disruption of circadian rhythms affects immunity, and how that effect differs between males and females, may help the development of chronotherapies for treating shift work-related disorders such as shift work sleep disorder (SWSD) and its related health-risks.
Given that sensitivity to LPS is highest at CT12 in rodents [15, 56], we showed circadian disruption induced by an 8-h phase advance reduces cytokine production at this time while exacerbating the response at CT0. Remarkably, our models predict a second peak in the production of the anti-inflammatory cytokine IL-10 when the immune system is poised for attack (e.g. CT12). At times when the immune system is undergoing regeneration and repair (e.g. CT18-CT6) [15], the model predicts a single peak in IL-10 because the inflammatory response is weaker. The recurrence of this pattern at different doses of LPS implies the existence of qualitative differences at CT0 compared to CT12.
Overall, our results show that the extent of sequelae experienced by male and female rats depends on the time of infection. Females suffered more severe sequelae than males when infected during the late rest or early active periods. Specifically, IL-6 and TNF-α production at CT12 was greatly lowered in females. This response is not potent enough to maintain long term control of the infection. Female rats produce less cytokines overall during acute inflammation when compared to males. Nonetheless, males also suffer from circadian-induced immune disruption. Their higher levels of IL-6 and TNFα and damage could increase their susceptibility to sepsis.
The modulation of circadian activity by cytokines has been reported over the last years. For instance, TNFα-incubation has been shown to suppress Per gene expression in vitro and in vivo in mice [62] as well as Cry1 [97]. Some recent work by [98] and [99] reveals that TNFα modulates the transcription of Bmal1 through the up-regulation of Rorα. The present model does not include the direct links from cytokines to clock genes and proteins, but those links can be incorporated into future extensions of the model. It should be noted that different lengths of phase advances and phase delays in expression of clock genes could lead to different immune responses in males and females. Our current model focuses on 8h advance of the circadian phase, but if more data is available in the future, it could lead to an extension of this investigation to different lengths of phase shifts. Testing different shifts will help determine 1) if specific changes are better than others, 2) if the male/female difference is as crucial as the polymorphisms that alter circadian timing in specific individuals. These questions will be considered in future extensions of this model. The development of mathematical models that investigate the role of circadian rhythms in immunity and vice versa help our understanding of the dynamics involved in the interplay between these two systems. Extending the model to investigate the circadian control of other organ systems such as the liver [100] and kidney [101] would also be worthwhile.
In conclusion, our results suggest that circadian disruption due to shift work is primarily mediated by the circadian disruption of REV-ERB and CRY. REV-ERB in particular acts as an equilibrist by negatively affecting the expression of pro-inflammatory cytokine IL-6 and anti-inflammatory cytokine IL-10. We also showed the importance of sexual dimorphism in the magnitude of the inflammatory response during CJL. A functional and rhythmic clock confers immunoprotection and improves organismal fitness [102]. Thus, it is important to understand the molecular mechanisms that link the clock to immune functions, particularly during unrest caused by behavioral changes such as shift work.
Supporting information
(Table A) List of variables, (Table B) list of the differential equations defining the mathematical model; relates to Fig 1. (Tables C-J) Nominal parameter set of the mathematical model. (Tables K-M) Parameter values in CJL models. Supplemental experimental procedure: Sobol’ sensitivity analysis.
(PDF)
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
A.T.L. is supported by the Canada 150 Research Chairs Program and the Natural Sciences and Engineering Research Council of Canada (NSERC Discovery award: RGPIN-2019-03916); https://www.canada150.chairs-chaires.gc.ca/home-accueil-eng.aspx, https://www.nserc-crsng.gc.ca. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Dibner C, Schibler U, Albrecht U. The mammalian circadian timing system: organization and coordination of central and peripheral clocks. Annu Rev Physiol. 2010;72:517–549. 10.1146/annurev-physiol-021909-135821 [DOI] [PubMed] [Google Scholar]
- 2. Albrecht U, Eichele G. The mammalian circadian clock. Curr Opin Genet Dev. 2003;13(3):271–277. 10.1016/S0959-437X(03)00055-8 [DOI] [PubMed] [Google Scholar]
- 3. Mohawk JA, Green CB, Takahashi JS. Central and peripheral circadian clocks in mammals. Annu Rev Neurosci. 2012;35:445–462. 10.1146/annurev-neuro-060909-153128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sundar IK, Yao H, Sellix MT, Rahman I. Circadian molecular clock in lung pathophysiology. Am J Physiol Lung Cell Mol Physiol. 2015;309(10):L1056–L1075. 10.1152/ajplung.00152.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pilorz V, Cunningham PS, Jackson A, West AC, Wager TT, Loudon AS, et al. A novel mechanism controlling resetting speed of the circadian clock to environmental stimuli. Curr Biol. 2014;24(7):766–773. 10.1016/j.cub.2014.02.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vasu VT, Cross CE, Gohil K. Nr1d1, an important circadian pathway regulatory gene, is suppressed by cigarette smoke in murine lungs. Integr Cancer Ther. 2009;8(4):321–328. 10.1177/1534735409352027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gebel S, Gerstmayer B, Kuhl P, Borlak J, Meurrens K, Müller T. The kinetics of transcriptomic changes induced by cigarette smoke in rat lungs reveals a specific program of defense, inflammation, and circadian clock gene expression. Toxicol Sci. 2006;93(2):422–431. 10.1093/toxsci/kfl071 [DOI] [PubMed] [Google Scholar]
- 8. Sukumaran S, Jusko WJ, DuBois DC, Almon RR. Light-dark oscillations in the lung transcriptome: implications for lung homeostasis, repair, metabolism, disease, and drug action. J Appl Physiol. 2011;110(6):1732–1747. 10.1152/japplphysiol.00079.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Logan RW, Zhang C, Murugan S, O’Connell S, Levitt D, Rosenwasser AM, et al. Chronic shift-lag alters the circadian clock of NK cells and promotes lung cancer growth in rats. J Neuroimmunol. 2012;188(6):2583–2591. 10.4049/jimmunol.1102715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wolff G, Duncan MJ, Esser KA. Chronic phase advance alters circadian physiological rhythms and peripheral molecular clocks. J Appl Physiol. 2013;115(3):373–382. 10.1152/japplphysiol.01139.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Davidson AJ, Castanon-Cervantes O, Leise TL, Molyneux PC, Harrington ME. Visualizing jet lag in the mouse suprachiasmatic nucleus and peripheral circadian timing system. Eur J Neurosci. 2009;29(1):171–180. 10.1111/j.1460-9568.2008.06534.x [DOI] [PubMed] [Google Scholar]
- 12. Hadden H, Soldin SJ, Massaro D. Circadian disruption alters mouse lung clock gene expression and lung mechanics. J Appl Physiol. 2012;113(3):385–392. 10.1152/japplphysiol.00244.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gibbs J, Ince L, Matthews L, Mei J, Bell T, Yang N, et al. An epithelial circadian clock controls pulmonary inflammation and glucocorticoid action. Nat Med. 2014;20(8):919–926. 10.1038/nm.3599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sundar IK, Ahmad T, Yao H, Hwang Jw, Gerloff J, Lawrence BP, et al. Influenza A virus-dependent remodeling of pulmonary clock function in a mouse model of COPD. Sci Rep. 2015;5(1):1–14. 10.1038/srep09927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Curtis AM, Bellet MM, Sassone-Corsi P, O’Neill LA. Circadian clock proteins and immunity. Immunity. 2014;40(2):178–186. 10.1016/j.immuni.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 16. Haus EL, Smolensky MH. Shift work and cancer risk: potential mechanistic roles of circadian disruption, light at night, and sleep deprivation. Sleep Med Rev. 2013;17(4):273–284. 10.1016/j.smrv.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 17. Khan S, Duan P, Yao L, Hou H. Shiftwork-mediated disruptions of circadian rhythms and sleep homeostasis cause serious health problems. Int J Genomics. 2018;2018. 10.1155/2018/8576890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Meyer-Hermann M, Figge MT, Straub RH. Mathematical modeling of the circadian rhythm of key neuroendocrine–immune system players in rheumatoid arthritis: A systems biology approach. Arthritis Rheum. 2009;60(9):2585–2594. 10.1002/art.24797 [DOI] [PubMed] [Google Scholar]
- 19. Scheff JD, Calvano SE, Lowry SF, Androulakis IP. Modeling the influence of circadian rhythms on the acute inflammatory response. J Theor Biol. 2010;264(3):1068–1076. 10.1016/j.jtbi.2010.03.026 [DOI] [PubMed] [Google Scholar]
- 20.Bangsgaard EO. Mathematical Modelling of the Dynamic Role of the HPA Axis in the Immune System [mthesis]. Technical University of Denmark, Department of Applied Mathematics and Computer Science. Richard Petersens Plads, Building 324, DK-2800 Kgs. Lyngby, Denmark, computecompute.dtu.dk; 2016.
- 21. Wang X, Yu W, Zheng L. The dynamics of NF-κB pathway regulated by circadian clock. Math Biosci. 2015;260:47–53. 10.1016/j.mbs.2014.07.012 [DOI] [PubMed] [Google Scholar]
- 22. Hergenhan S, Holtkamp S, Scheiermann C. Molecular Interactions Between Components of the Circadian Clock and the Immune System. J Mol Biol. 2020; p. 3700–3713. 10.1016/j.jmb.2019.12.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reppert SM, Weaver DR. Coordination of circadian timing in mammals. Nature. 2002;418(6901):935–941. 10.1038/nature00965 [DOI] [PubMed] [Google Scholar]
- 24. Ko CH, Takahashi JS. Molecular components of the mammalian circadian clock. Hum Mol Genet. 2006;15(suppl_2):R271–R277. 10.1093/hmg/ddl207 [DOI] [PubMed] [Google Scholar]
- 25. Duong HA, Robles MS, Knutti D, Weitz CJ. A molecular mechanism for circadian clock negative feedback. Science. 2011;332(6036):1436–1439. 10.1126/science.1196766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Takahashi JS. Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet. 2017;18(3):164. 10.1038/nrg.2016.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu AC, Tran HG, Zhang EE, Priest AA, Welsh DK, Kay SA. Redundant function of REV-ERBα and β and non-essential role for Bmal1 cycling in transcriptional regulation of intracellular circadian rhythms. PLoS Genet. 2008;4(2):e1000023. 10.1371/journal.pgen.1000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Relógio A, Westermark PO, Wallach T, Schellenberg K, Kramer A, Herzel H. Tuning the mammalian circadian clock: robust synergy of two loops. PLoS Comput Biol. 2011;7(12):e1002309. 10.1371/journal.pcbi.1002309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cho H, Zhao X, Hatori M, Ruth TY, Barish GD, Lam MT, et al. Regulation of circadian behaviour and metabolism by REV-ERB-α and REV-ERB-β. Nature. 2012;485(7396):123–127. 10.1038/nature11048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bugge A, Feng D, Everett LJ, Briggs ER, Mullican SE, Wang F, et al. Rev-erbα and Rev-erbβ coordinately protect the circadian clock and normal metabolic function. Genes Dev. 2012;26(7):657–667. 10.1101/gad.186858.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wei N, Gumz ML, Layton AT. Predicted effect of circadian clock modulation of NHE3 of a proximal tubule cell on sodium transport. Am J Physiol Renal Physiol. 2018;315(3):F665–F676. 10.1152/ajprenal.00008.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li Q, McDonough AA, Layton HE, Layton AT. Functional implications of sexual dimorphism of transporter patterns along the rat proximal tubule: modeling and analysis. Am J Physiol Renal Physiol. 2018:315(3): F692–F700. 10.1152/ajprenal.00171.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee E, Kim EY. A role for timely nuclear translocation of clock repressor proteins in setting circadian clock speed. Exp neurobiol. 2014;23(3):191–199. 10.5607/en.2014.23.3.191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roy A, Clermont G, Daun S, Parker RS. A mathematical model of acute inflammatory response to endotoxin challenge. In: AIChE Annual Meeting, Salt Lake City, UT, 538g; 2007.
- 35. Daun S, Rubin J, Vodovotz Y, Roy A, Parker R, Clermont G. An ensemble of models of the acute inflammatory response to bacterial lipopolysaccharide in rats: results from parameter space reduction. J Theor Biol. 2008;253(4):843–853. 10.1016/j.jtbi.2008.04.033 [DOI] [PubMed] [Google Scholar]
- 36. Nash AA, Dalziel RG, Fitzgerald JR. Mechanisms of Cell and Tissue Damage. Mims’ Pathogenesis of Infectious Disease. 2015; p. 171. 10.1016/B978-0-12-397188-3.00008-1 [DOI] [Google Scholar]
- 37. Freeman BD, Natanson C. Anti-inflammatory therapies in sepsis and septic shock. Expert Opin Investig Drugs. 2000;9(7):1651–1663. 10.1517/13543784.9.7.1651 [DOI] [PubMed] [Google Scholar]
- 38. Bellingan G. Inflammatory cell activation in sepsis. Br Med Bull. 1999;55(1):12–29. 10.1258/0007142991902277 [DOI] [PubMed] [Google Scholar]
- 39. Pretolani M. Interleukin-10: an anti-inflammatory cytokine with therapeutic potential. Clin Exp Allergy. 1999;29(9):1164–1171. 10.1046/j.1365-2222.1999.00456.x [DOI] [PubMed] [Google Scholar]
- 40. Pinsky MR. Sepsis: a pro-and anti-inflammatory disequilibrium syndrome. Contrib Nephrol. 2001;132:354–366. 10.1159/000060100 [DOI] [PubMed] [Google Scholar]
- 41. Matzinger P. The danger model: a renewed sense of self. Science. 2002;296(5566):301–305. 10.1126/science.1071059 [DOI] [PubMed] [Google Scholar]
- 42. Giannoudis PV, Smith RM, Perry SL, Windsor AJ, Dickson RA, Bellamy MC. Immediate IL-10 expression following major orthopaedic trauma: relationship to anti-inflammatory response and subsequent development of sepsis. Intensive Care Med. 2000;26(8):1076–1081. 10.1007/s001340051320 [DOI] [PubMed] [Google Scholar]
- 43. Kamm K, VanderKolk W, Lawrence C, Jonker M, Davis AT. The effect of traumatic brain injury upon the concentration and expression of interleukin-1β and interleukin-10 in the rat. J. Trauma Acute Care Surg. 2006;60(1):152–157. 10.1097/01.ta.0000196345.81169.a1 [DOI] [PubMed] [Google Scholar]
- 44. Gouel-Chéron A, Allaouchiche B, Guignant C, Davin F, Floccard B, Monneret G, et al. Early interleukin-6 and slope of monocyte human leukocyte antigen-DR: a powerful association to predict the development of sepsis after major trauma. PloS one. 2012;7(3):e33095. 10.1371/journal.pone.0033095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mera S, Tatulescu D, Cismaru C, Bondor C, Slavcovici A, Zanc V, et al. Multiplex cytokine profiling in patients with sepsis. Apmis. 2011;119(2):155–163. 10.1111/j.1600-0463.2010.02705.x [DOI] [PubMed] [Google Scholar]
- 46. Chaudhry H, Zhou J, Zhong Y, Ali MM, McGuire F, Nagarkatti PS, et al. Role of cytokines as a double-edged sword in sepsis. In Vivo. 2013;27(6):669–684. [PMC free article] [PubMed] [Google Scholar]
- 47. Nguyen KD, Fentress SJ, Qiu Y, Yun K, Cox JS, Chawla A. Circadian gene Bmal1 regulates diurnal oscillations of Ly6Chi inflammatory monocytes. Science. 2013;341(6153):1483–1488. 10.1126/science.1240636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Curtis AM, Fagundes CT, Yang G, Palsson-McDermott EM, Wochal P, McGettrick AF, et al. Circadian control of innate immunity in macrophages by miR-155 targeting Bmal1. PNAS. 2015;112(23):7231–7236. 10.1073/pnas.1501327112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hashiramoto A, Yamane T, Tsumiyama K, Yoshida K, Komai K, Yamada H, et al. Mammalian clock gene Cryptochrome regulates arthritis via proinflammatory cytokine TNF-α. J Neuroimmunol. 2010;184(3):1560–1565. [DOI] [PubMed] [Google Scholar]
- 50. Narasimamurthy R, Hatori M, Nayak SK, Liu F, Panda S, Verma IM. Circadian clock protein cryptochrome regulates the expression of proinflammatory cytokines. PNAS. 2012;109(31):12662–12667. 10.1073/pnas.1209965109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cao Q, Zhao X, Bai J, Gery S, Sun H, Lin DC, et al. Circadian clock cryptochrome proteins regulate autoimmunity. PNAS. 2017;114(47):12548–12553. 10.1073/pnas.1619119114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Stapleton CM, Jaradat M, Dixon D, Kang HS, Kim SC, Liao G, et al. Enhanced susceptibility of staggerer (RORαsg/sg) mice to lipopolysaccharide-induced lung inflammation. Am J Physiol Lung Cell Mol Physiol. 2005;289(1):L144–L152. 10.1152/ajplung.00348.2004 [DOI] [PubMed] [Google Scholar]
- 53. Dzhagalov I, Giguère V, He YW. Lymphocyte development and function in the absence of retinoic acid-related orphan receptor α. J Neuroimmunol. 2004;173(5):2952–2959. [DOI] [PubMed] [Google Scholar]
- 54. Nejati Moharrami N, Bjørkøy Tande E, Ryan L, Espevik T, Boyartchuk V. RORα controls inflammatory state of human macrophages. PloS one. 2018;13(11):e0207374. 10.1371/journal.pone.0207374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Delerive P, Monté D, Dubois G, Trottein F, Fruchart-Najib J, Mariani J, et al. The orphan nuclear receptor RORα is a negative regulator of the inflammatory response. EMBO reports. 2001;2(1):42–48. 10.1093/embo-reports/kve007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Gibbs JE, Blaikley J, Beesley S, Matthews L, Simpson KD, Boyce SH, et al. The nuclear receptor REV-ERBα mediates circadian regulation of innate immunity through selective regulation of inflammatory cytokines. PNAS. 2012;109(2):582–587. 10.1073/pnas.1106750109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sato S, Sakurai T, Ogasawara J, Shirato K, Ishibashi Y, Oh-ishi S, et al. Direct and indirect suppression of interleukin-6 gene expression in murine macrophages by nuclear orphan receptor REV-ERBα. ScientificWorldJournal. 2014;2014. 10.1155/2014/685854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Pariollaud M, Gibbs JE, Hopwood TW, Brown S, Begley N, Vonslow R, et al. Circadian clock component REV-ERBα controls homeostatic regulation of pulmonary inflammation. J Clin Invest. 2018;128(6):2281–2296. 10.1172/JCI93910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Chandra V, Mahajan S, Saini A, Dkhar HK, Nanduri R, Raj EB, et al. Human IL10 gene repression by Rev-erbα ameliorates Mycobacterium tuberculosis clearance. J Biol Chem. 2013;288(15):10692–10702. 10.1074/jbc.M113.455915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lundkvist G, Hill R, Kristensson K. Disruption of circadian rhythms in synaptic activity of the suprachiasmatic nuclei by African trypanosomes and cytokines. Neurobiol Dis. 2002;11(1):20–27. 10.1006/nbdi.2002.0536 [DOI] [PubMed] [Google Scholar]
- 61. Marpegán L, Bekinschtein TA, Costas MA, Golombek DA. Circadian responses to endotoxin treatment in mice. J Neuroimmunol. 2005;160(1-2):102–109. 10.1016/j.jneuroim.2004.11.003 [DOI] [PubMed] [Google Scholar]
- 62. Cavadini G, Petrzilka S, Kohler P, Jud C, Tobler I, Birchler T, et al. TNF-α suppresses the expression of clock genes by interfering with E-box-mediated transcription. PNAS. 2007;104(31):12843–12848. 10.1073/pnas.0701466104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kwak Y, Lundkvist GB, Brask J, Davidson A, Menaker M, Kristensson K, et al. Interferon-γ alters electrical activity and clock gene expression in suprachiasmatic nucleus neurons. J Biol Rhythms. 2008;23(2):150–159. 10.1177/0748730407313355 [DOI] [PubMed] [Google Scholar]
- 64. Okada K, Yano M, Doki Y, Azama T, Iwanaga H, Miki H, et al. Injection of LPS causes transient suppression of biological clock genes in rats. J Surg Res. 2008;145(1):5–12. 10.1016/j.jss.2007.01.010 [DOI] [PubMed] [Google Scholar]
- 65. Bellet MM, Deriu E, Liu JZ, Grimaldi B, Blaschitz C, Zeller M, et al. Circadian clock regulates the host response to Salmonella. PNAS. 2013;110(24):9897–9902. 10.1073/pnas.1120636110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Shimizu T, Watanabe K, Anayama N, Miyazaki K. Effect of lipopolysaccharide on circadian clock genes Per2 and Bmal1 in mouse ovary. J Physiol Sci. 2017;67(5):623–628. 10.1007/s12576-017-0532-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Haimovich B, Calvano J, Haimovich AD, Calvano SE, Coyle SM, Lowry SF. In vivo endotoxin synchronizes and suppresses clock gene expression in human peripheral blood leukocytes. J Crit Care Med. 2010;38(3):751. 10.1097/CCM.0b013e3181cd131c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wang Y, Pati P, Xu Y, Chen F, Stepp DW, Huo Y, et al. Endotoxin disrupts circadian rhythms in macrophages via reactive oxygen species. PloS one. 2016;11(5):e0155075. 10.1371/journal.pone.0155075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB. A circadian gene expression atlas in mammals: implications for biology and medicine. PNAS. 2014;111(45):16219–16224. 10.1073/pnas.1408886111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Mavroudis PD, DuBois DC, Almon RR, Jusko WJ. Daily variation of gene expression in diverse rat tissues. PloS one. 2018;13(5):e0197258. 10.1371/journal.pone.0197258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Iversen MH, Hahn RG. Acute effects of vitamin A on the kinetics of endotoxin in conscious rabbits. Intensive Care Med. 1999;25(10):1160–1164. 10.1007/s001340051029 [DOI] [PubMed] [Google Scholar]
- 72. Warner AE, DeCamp MM Jr, Molina RM, Brain JD. Pulmonary removal of circulating endotoxin results in acute lung injury in sheep. Lab. Invest. 1988;59(2):219–230. [PubMed] [Google Scholar]
- 73. Banks HT, Tran HT. Mathematical and Experimental Modeling of Physical and Biological Processes. Chapman & Hall/CRC PRESS. 2009. [Google Scholar]
- 74. Thun E, Le Hellard S, Osland T, Bjorvatn B, Moen B, Magerøy N, et al. Circadian clock gene variants and insomnia, sleepiness, and shift work disorder. Sleep Biol Rhythms. 2016;14(1):55–62. 10.1007/s41105-015-0023-9 [DOI] [Google Scholar]
- 75. Landgraf D, Wang LL, Diemer T, Welsh DK. NPAS2 compensates for loss of CLOCK in peripheral circadian oscillators. PLoS genetics. 2016;12(2):e1005882. 10.1371/journal.pgen.1005882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. DeBruyne JP, Weaver DR, Reppert SM. CLOCK and NPAS2 have overlapping roles in the suprachiasmatic circadian clock. Nat Neurosci. 2007;10(5):543–545. 10.1038/nn1884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Wu M, Zeng J, Chen Y, Zeng Z, Zhang J, Cai Y, Ye Y, Fu L, Xian L, Chen Z. Experimental chronic jet lag promotes growth and lung metastasis of Lewis lung carcinoma in C57BL/6 mice. Oncol Rep. 2012;27(5):1417–1428. [DOI] [PubMed] [Google Scholar]
- 78. Iwamoto A, Kawai M, Furuse M, Yasuo S. Effects of chronic jet lag on the central and peripheral circadian clocks in CBA/N mice. Chronobiol Int. 2014;31(2):189–98. 10.3109/07420528.2013.837478 [DOI] [PubMed] [Google Scholar]
- 79. Karatsoreos I, Silver R. Body clocks in health and disease. In: Conn’s Translational Neuroscience. Elsevier; 2017. p. 599–615. [Google Scholar]
- 80. Halberg F. Temporal coordination of physiologic function. In: Cold Spring Harbor symposia on quantitative biology. vol. 25. Cold Spring Harbor Laboratory Press; 1960. p. 289–310. [DOI] [PubMed] [Google Scholar]
- 81. Shackelford PG, Feigin RD. Periodicity of susceptibility to pneumococcal infection: influence of light and adrenocortical secretions. Science. 1973;182(4109):285–287. 10.1126/science.182.4109.285 [DOI] [PubMed] [Google Scholar]
- 82. Chow CC, Clermont G, Kumar R, Lagoa C, Tawadrous Z, Gallo D, et al. The acute inflammatory response in diverse shock states. Shock. 2005;24(1):74–84. 10.1097/01.shk.0000168526.97716.f3 [DOI] [PubMed] [Google Scholar]
- 83. Marpegan L, Leone MJ, Katz ME, Sobrero PM, Bekinstein TA, Golombek DA. Diurnal variation in endotoxin-induced mortality in mice: correlation with proinflammatory factors. Chronobiol Int. 2009;26(7):1430–1442. 10.3109/07420520903408358 [DOI] [PubMed] [Google Scholar]
- 84. Castanon-Cervantes O, Wu M, Ehlen JC, Paul K, Gamble KL, Johnson RL, et al. Dysregulation of inflammatory responses by chronic circadian disruption. J Neuroimmunol. 2010;185(10):5796–5805. 10.4049/jimmunol.1001026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Adams KL, Castanon-Cervantes O, Evans JA, Davidson AJ. Environmental circadian disruption elevates the IL-6 response to lipopolysaccharide in blood. J Biol Rhythms. 2013;28(4):272–277. 10.1177/0748730413494561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Guerrero-Vargas NN, Guzmán-Ruiz M, Fuentes R, García J, Salgado-Delgado R, Basualdo MdC, et al. Shift work in rats results in increased inflammatory response after lipopolysaccharide administration: a role for food consumption. J Biol Rhythms. 2015;30(4):318–330. 10.1177/0748730415586482 [DOI] [PubMed] [Google Scholar]
- 87. Phillips DJ, Savenkova MI, Karatsoreos IN. Environmental disruption of the circadian clock leads to altered sleep and immune responses in mouse. Brain Behav Immun. 2015;47:14–23. 10.1016/j.bbi.2014.12.008 [DOI] [PubMed] [Google Scholar]
- 88. Pearson GL, Savenkova M, Barnwell JJ, Karatsoreos IN. Circadian desynchronization alters metabolic and immune responses following lipopolysaccharide inoculation in male mice. Brain Behav Immun. 2020; p. 220–229. 10.1016/j.bbi.2020.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Stowie A, Ellis I, Adams K, Castanon-Cervantes O, Davidson AJ. A reductionist, in vitro model of environmental circadian disruption demonstrates SCN-independent and tissue-specific dysregulation of inflammatory responses. Plos one. 2019;14(5):e0217368. 10.1371/journal.pone.0217368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Tiwari T, Basu P, Singaravel M. Differences in post-chronic jet lag parameters in male and female mice. Biol Rhythm Res. 2019; p. 1–11. [Google Scholar]
- 91. Angele MK, Pratschke S, Hubbard WJ, Chaudry IH. Gender differences in sepsis: cardiovascular and immunological aspects. Virulence. 2014;5(1):12–19. 10.4161/viru.26982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Nasir N, Jamil B, Siddiqui S, Talat N, Khan FA, Hussain R. Mortality in sepsis and its relationship with gender. Pak J Med Sci. 2015;31(5):1201. 10.12669/pjms.315.6925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Orozco-Solis R, Aguilar-Arnal L. Circadian regulation of immunity through epigenetic mechanisms. Front Cell Infect Microbiol. 2020;10:96. 10.3389/fcimb.2020.00096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Haspel JA, Anafi R, Brown MK, Cermakian N, Depner C, Desplats P, et al. Perfect timing: circadian rhythms, sleep, and immunity—an NIH workshop summary. JCI insight. 2020;5(1). 10.1172/jci.insight.131487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Barik S. Molecular Interactions between Pathogens and the Circadian Clock. Int J Mol Sci. 2019;20(23):5824. 10.3390/ijms20235824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. James SM, Honn KA, Gaddameedhi S, Van Dongen HP. Shift work: disrupted circadian rhythms and sleep—implications for health and well-being. Curr Sleep Med Rep. 2017;3(2):104–112. 10.1007/s40675-017-0071-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Perez-Aso M, Feig JL, Aránzazu M, Cronstein BN. Adenosine A 2A receptor and TNF-α regulate the circadian machinery of the human monocytic THP-1 cells. Inflammation. 2013;36(1):152–162. 10.1007/s10753-012-9553-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Yoshida K, Nakai A, Kaneshiro K, Hashimoto N, Suzuki K, Uchida K, et al. TNF-a induces expression of the circadian clock gene Bmal1 via dual calcium-dependent pathways in rheumatoid synovial cells. Biochem Biophys Res Commun. 2017;30:1e6. [DOI] [PubMed] [Google Scholar]
- 99. Ertosun MG, Kocak G, Ozes ON. The regulation of circadian clock by tumor necrosis factor alpha. Cytokine Growth Factor Rev. 2019; p. 10–16. 10.1016/j.cytogfr.2019.04.001 [DOI] [PubMed] [Google Scholar]
- 100.Sadria M, Layton AT. Interactions among mTORC, AMPK, and SIRT: A Computational Model for Cell Energy Balance and Metabolism. Cell Communication and Signaling, in press, 2021. [DOI] [PMC free article] [PubMed]
- 101. Layton AT, Laghmani K, Vallon V, Edwards A. Solute transport and oxygen consumption along the nephrons: effects of Na+ transport inhibitors American Journal of Physiology-Renal Physiology. 311(6): F1217–F1229, 2016. 10.1152/ajprenal.00294.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Man K, Loudon A, Chawla A. Immunity around the clock. Science. 2016;354(6315):999–1003. 10.1126/science.aah4966 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(Table A) List of variables, (Table B) list of the differential equations defining the mathematical model; relates to Fig 1. (Tables C-J) Nominal parameter set of the mathematical model. (Tables K-M) Parameter values in CJL models. Supplemental experimental procedure: Sobol’ sensitivity analysis.
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting information files.