Abstract
Health decision models are the only available tools designed to consider the lifetime natural history of human papillomavirus (HPV) infection and pathogenesis of cervical cancer, and the estimated long-term impact of preventive interventions. Yet health decision modeling results are often considered a lesser form of scientific evidence due to the inherent needs to rely on imperfect data and make numerous assumptions and extrapolations regarding complex processes. We propose a new health decision modeling framework that de-emphasizes cytologic-colposcopic-histologic diagnoses due to their subjectivity and lack of reproducibility, relying instead on HPV type and duration of infection as the major determinants of subsequent transition probabilities. We posit that the new model health states (normal, carcinogenic HPV infection, precancer, cancer) and corollary transitions are universal, but that the probabilities of transitioning between states may vary by population. Evidence for this variability in host response to HPV infections can be inferred from HPV prevalence patterns in different regions across the lifespan, and might be linked to different average population levels of immunologic control of HPV infections. By prioritizing direct estimation of model transition probabilities from longitudinal data (and limiting reliance on model-fitting techniques that may propagate error when applied to multiple transitions), we aim to reduce the number of assumptions for greater transparency and reliability. We propose this new microsimulation model for critique and discussion, hoping to contribute to models that maximally inform efficient strategies toward global cervical cancer elimination.
Keywords: Cancer screening, Human papillomavirus (HPV), HPV DNA tests, uterine cervical neoplasms, decision analysis, mathematical model
1. Introduction
Understanding of human papillomavirus (HPV) and the necessary steps in cervical carcinogenesis has led to effective prevention methods. Yet the absolute number of cases of cervical cancer is rising worldwide due to lack of resources and aging of lower-resource populations. More than a half-million cases and quarter-million deaths still occur each year— almost 90% in low- and middle-income countries (LMIC).1 Prophylactic HPV vaccination can protect against infection with the carcinogenic HPV types that cause between 70% and 90% of cervical cancers,2 but only ~10% of girls in LMIC have been vaccinated.3 Women past the target age of vaccination can be protected against cancer through detection and treatment of cervical cancer precursor lesions (“precancer”), but less than 20% in LMIC have ever been screened in effective programs.4
Health decision models have been used extensively to inform decision-making related to cervical cancer control policies globally.5 In May 2018, the Director-General of the World Health Organization (WHO) announced a global call to action towards the elimination of cervical cancer.6 Health decision modeling based on highly optimistic benchmarks for vaccine uptake and screening program coverage was presented in support of this call to action, setting interim prevention implementation targets to be achieved by 2030 in order to reach the elimination goal over the coming century.7 However, with the current COVID-19 pandemic, the 2030 targets of the call to action are very unlikely to be realized. Cervical cancer is likely to continue to disproportionately kill women in LMIC. We might already need to adjust approaches and expectations.
Health decision analyses that guide choices between cervical cancer prevention strategic alternatives estimate the costs and benefits to women over the long-term, extending past the limits of empirical studies that cannot fully compare all relevant strategies.8 Randomized clinical trials and rigorous longitudinal cohort studies are ideal to evaluate preventive methods over the short-term. However, given the typically long interval between acquisition of HPV infection and cancer, health decision models are the only available tools designed to consider the lifetime natural history of HPV and pathogenesis of cervical cancer, and the estimated long-term impact of prevention strategies. Particularly in LMIC, policy makers increasingly rely on health decision model projections of health impact and cost-effectiveness for decision making.
Given the essential role of cost-effectiveness analyses on global cervical cancer prevention policy, it is imperative that the health decision models reflect advancing knowledge of HPV natural history and prove to be trustworthy.9 Due to inherent complexity and requisite assumptions, models are often perceived as “black boxes” that lack transparency; findings are not easily reproduced independently.10 To the degree that there are unknowns and we must estimate (with possible error) the model inputs for a substantial proportion of the details, the final answers are prone to change. For example, the modeling efforts that underlie the current WHO call to action7 project trends over nearly a century and do not consider novel prevention strategies. Different models may yield qualitatively different results, leaving decision makers in a quandary regarding which (if any) are accurate.11-13 Comparative modeling exercises must be undertaken not only with the goal of understanding modeling differences, but with an openness to revisiting fundamental model assumptions when inconsistencies are revealed.11,12
We acknowledge the enormity of effort involved in revising health decision models. Faced with evolving natural history data, modelers must decide when incremental improvements will be sufficient and when a more substantive revision is necessary. Existing models of HPV and cervical pathogenesis are in different stages of evolution. However, at this critical juncture, we have advanced scientific understanding of cervical cancer development, necessary precursor states, the performance of leading prevention methods, and the effectiveness of combining prevention methods into implementable strategies.14 To evaluate these strategies reliably and accurately, the models need greater fidelity to the natural history than they currently have.
In this manuscript, we propose an HPV type-based framework for a new set of microsimulation models that we are developing for evaluation of novel prevention strategies. We posit that the proposed model health states are universal, but that the probabilities of transitioning between states may vary by population as a result of differences host behavior and immunologic response; we present evidence in support of this hypothesis and describe ongoing work to further evaluate it. By explicitly showing how existing models differ from the proposed framework, we aim to foster discussion and further refinement of cervical cancer microsimulation models, as well as scientific consensus in health decisions related to cervical cancer prevention and control.
2. Overview of state-transition modeling
The steps for building and applying health decision models for cervical cancer control are presented (Table 1). Of these, the first— building and testing a model— is the most fundamental step to projecting accurate results. Below we present our methodologic approach to building a new state-transition model, in which we identify necessary model health states; define corollary transitions between health states; define variables that modify transition probabilities; directly estimate transition probabilities; and identify highly uncertain transition probabilities.
Table 1.
Step-by-step health decision analysis for cervical cancer control.
| Step | Components of a state-transition model |
|---|---|
| 1. Build and test a model: | a.Understand the etiology of cervical cancer. b.Identify the necessary intermediate states leading from a normal cervix to cancer. c.Define the corollary transitions between the causal states. d.Define population- and individual-level variables that meaningfully modify the transition. e.Directly estimate transition probabilities from longitudinal data in a representative population and reckon how confident we are of each transition probability. f.Identify uncertain transition probabilities that cannot be directly estimated. g.Calibrate uncertain transition probabilities (when data are lacking) using epidemiologic data targets from a population of interest (e.g., to produce realistic matches to empirical type- and age-specific prevalence of HPV and precancer; cervical cancer incidence). h.Validate the state-transition model to determine adequacy of model fit to data from different, independent populations that were not used to derive transition probabilities. |
| 2. Estimate intervention impact (costs and health outcomes): | a.Identify the available and soon-to-be-available prevention methods. b.Determine population- and individual-level variables that meaningfully modify performance of the prevention methods. c.Directly estimate the performance of prevention methods (i.e., HPV vaccination; screening; treatment of precancer) based on where each interrupts the causal pathway. d.Anticipate likely combinations of the prevention methods into alternative strategies. e.Measure effective coverage and costs of strategies specific to different regions. |
| 3. Perform the health decision modeling analysis and compare alternative strategies. | a.Run the natural history model to project cost and health outcomes in the absence of any intervention. b.Simulate each prevention strategy to project cost and health outcomes. c.Compare strategies incrementally, eliminating strategies that are more costly and less effective than other strategies (i.e., strong dominance) or less costly and less cost-effective than more effective strategies (i.e., extended dominance). d.Perform extensive scenario and sensitivity analysis on uncertain factors. |
The objective for the proposed state-transition model is to project costs, clinical events, and health outcomes over an extended time period (e.g., lifetime) of a large theoretical cohort, which can be done (for example) through a technical process called microsimulation (Figure 1).15
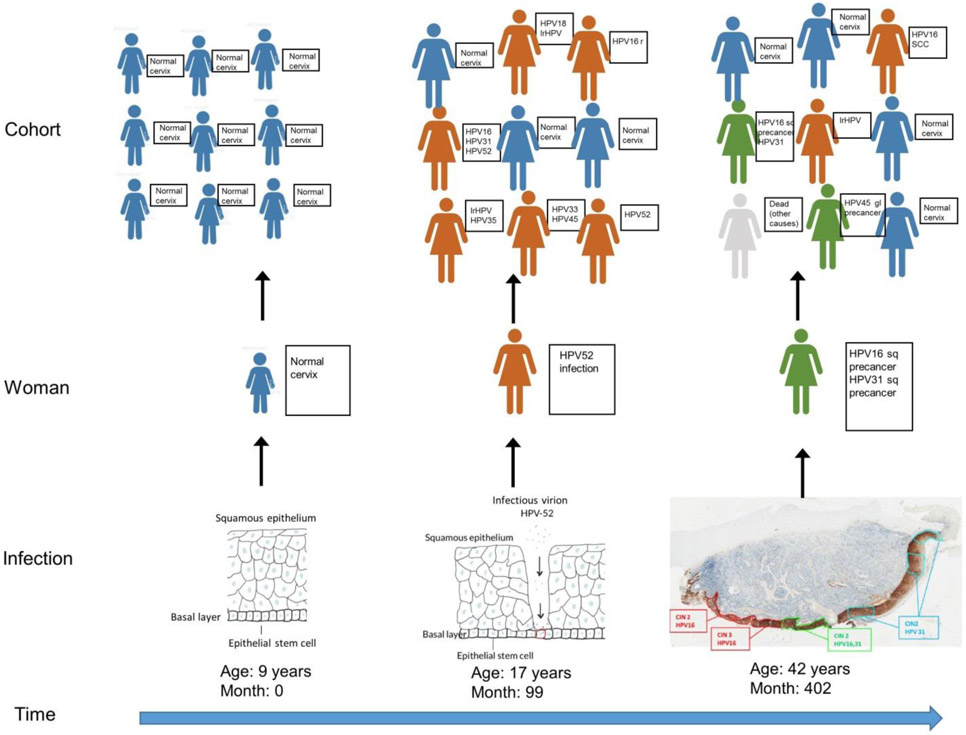
Figure 1. Microsimulation of HPV infection and cervical carcinogenesis: Translating the molecular pathogenesis of HPV to health decision modeling.
Cervical cancer incidence and mortality in a theoretical cohort is the summation of individual women's lifetime experiences with each of the carcinogenic or “high-risk” (hr) HPV types. Over time, a woman's cervix is exposed (or not) to each of the hrHPV types. She reacts to each type independently. The worst viral outcome measured at a given moment defines the woman's health state. She might have cleared 10 types previously but if one is present at the time of measurement, she is "infected". If any type persists and a precancer develops, she has "precancer". If any precancer invades, the woman has incident cancer. Outcomes are aggregated over the entire cohort (a “bottom-up” approach) over time to estimate the long-term population impact and cost-effectiveness of different scenarios. The proposed microsimulation model represents the summation of an individual woman’s experience with each HPV type (or group of types) in the cervix at any given month. The model begins tracking a theoretical cohort of girls prior to sexual initiation (e.g., age 9 years) on a monthly basis. Upon entering the model, all females in the cohort have a normal cervix (blue) (left). While HPV exposures do not necessarily happen concurrently, they are likely to happen soon after the woman becomes sexually active. Women who are infected with HPV are depicted in orange. Outcomes for individual women are then aggregated over the entire theoretical cohort to project population-level outcomes. With time, most infections clear but some persist, increasing the risk of progression to precancer (green) which, if untreated, may invade. The health decision modeling framework categorizes a woman by the status of her worst clone or lesion associated with each HPV type at a given time. In the example at right, the woman would be classified as having HPV-16 associated squamous precancer and an HPV-31 associated squamous precancer, but the model would not keep track of the multiple clones associated with each type. By tracking the worst clone or lesion for a given HPV type, the model aggregates information at the level of the infection, then the level of the woman, and then the level of the population. Women in the theoretical cohort can die of cervical cancer or of other causes (gray). Photograph from van der Marel MD, Quint WGV, Schiffman M, et al. Molecular mapping of high-grade cervical intraepithelial neoplasia shows etiological dominance of HPV16. International Journal of Cancer 2012;131:E946-E953. Used with permission from John Wiley & Sons, Inc.
3. Identify necessary model health states: The multi-stage causal pathway to cervical cancer
The fundamental natural history pathway includes the following necessary and reliably measured stages/states in the development of cervical cancer: 1) infection with a specific type of carcinogenic or “high-risk” (hr) HPV; 2) precancer, which we define as a persistent, transforming HPV infection associated with lesions at a high likelihood of invasion if left untreated; and 3) invasive cervical cancer. Both "precancer" and "cancer" are divided into predominant squamous versus less common glandular pathways (Figure 2).16 These health states are thought to apply to all settings, and will be stratified by HPV type.
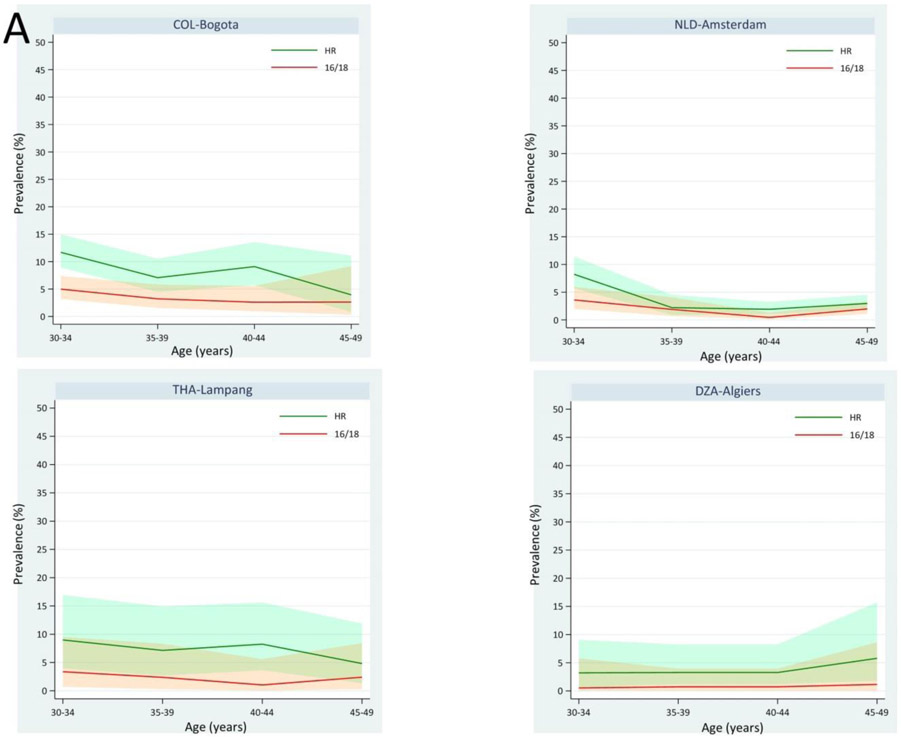
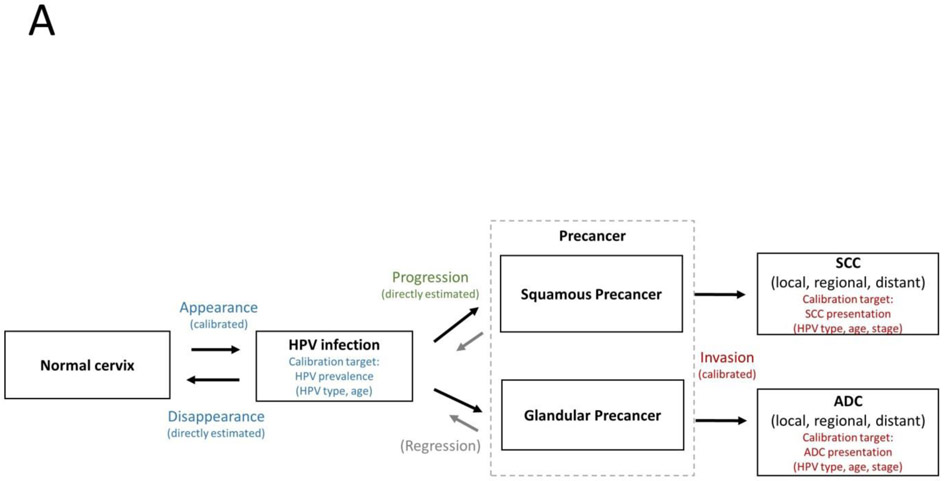
Figure 2. New health decision model schematic: Universal natural history of cervical carcinogenesis.
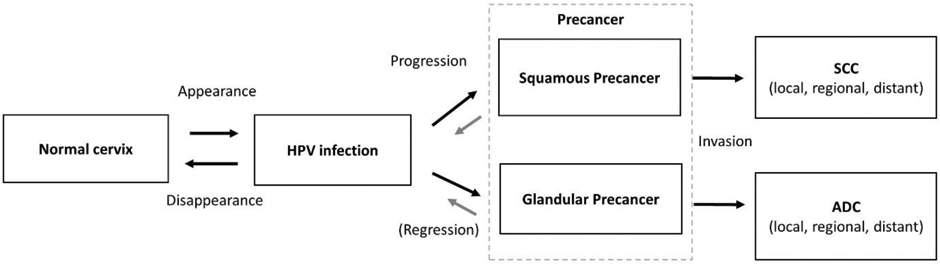
Each box represents a necessary stage, or health state, on the path to cervical cancer, including acquisition of a carcinogenic, “high-risk” HPV infection; progression of a persistent hrHPV infection to precancer (defined as persistent lesions with a high likelihood of invasion if left untreated); and invasion to cervical cancer. Each arrow represents the risk of transitioning between stages. Appearance— the risk of transitioning from No HPV infection to HPV infection— may include new acquisition of a particular genotype, re-infection with the same genotype, or reactivation of a latent infection. Disappearance— the risk of transitioning from HPV infection to No HPV infection— refers to the shift from a would-be detectable infection to non-detectable by a clinical HPV DNA assay, whether attributable to complete viral clearance or viral latency. The model distinguishes progression to squamous precancer (which may transition to squamous cell carcinoma) from progression to glandular precancer (which may transition to adenocarcinoma). Precancer occurs when a hrHPV infection that is primarily a productive infection (i.e., producing more viral particles) becomes instead an abortive transforming infection (i.e., associated clone of cells with severe disruption of cellular growth and differentiation controls, decreased programmed cell death [apoptosis] and increased genetic mutability). Regression of precancer through immune recognition and cell-mediated immune control is still possible, but much less likely than the control of earlier productive infections. The probability of invasion of a precancer is a function of time and the accumulation of genetic changes needed to overcome the coded cellular safeguards against growth inward into the cervical stroma across the epithelial basement membrane. Although invasion can occur quickly in unfortunate, but rare occurrences, precancers typically grow circumferentially within the epithelial layer for years if not decades before acquiring an invasive phenotype. Multiple precancers can occur on a cervix. If any invades, cancer results.
4. Define corollary transitions between health states on the causal pathway
Just as the causal states are the same across settings, so are the corollary transitions (i.e., the forward and backward “steps” between health states): appearance of hrHPV types; viral disappearance versus persistence; progression to precancer; and invasion.16 Women initially transition from a normal cervix to an HPV-infected state (with one or more infections) based on sexual behavior patterns, which change with age; peak incidence for all HPV types typically follows soon after age at sexual initiation.17 Women then face probabilities of viral clearance, or, given viral persistence (i.e., the absence of clearance), progression to the precancer state. Clearance is thought to represent cell-mediated immune suppression of the type-specific infection, which is either eliminated or kept in an undetectable 'latent' state that may reappear later due to temporary weakening of immune surveillance or age-related “immune senescence”;18 we thus refer to viral “appearance” (instead of “acquisition”) and “disappearance” (instead of “clearance”) to acknowledge the limitations of existing measurement assays and the potential for reactivation of latent infections. Precancer occurs when a hrHPV infection that is primarily a productive infection (i.e., producing more viral particles) becomes instead a transforming infection (i.e., associated clone of cells with severe disruption of cellular growth and differentiation controls).19 Regression of precancer through cell-mediated immune control is still possible, but much less likely than the control of earlier productive infections. Although invasion can occur quickly in unfortunate, but rare occurrences, precancers typically grow circumferentially for years, if not decades, before acquiring an invasive phenotype.
5. Define variables that modify transition probabilities
5.1. HPV genotype
The transitions to precancer and cancer are influenced mainly by HPV genotype. HPV16 poses a uniquely elevated risk of precancer and cancer. Other hrHPV types fall into 3 distinct risk groups: 1) HPV18 and HPV45 are not particularly elevated in squamous precancer but produce a heightened risk of squamous cancer, as well as rarer glandular precancer and adenocarcinoma;2,20 2) HPV31, HPV33, HPV351, HPV52, and HPV58 are genetically related to HPV16 and can be considered an intermediate risk group; 3) less risky types of HPV have carcinogenic potential but, in fact, rarely cause invasive cancer; these include HPV39, HPV51, HPV56, HPV59, and HPV68.2,21 Health states in the new natural history model will be stratified as follows: HPV16, HPV18, HPV45, HPV31, HPV33, HPV35,22 HPV52, and HPV58 (IARC Group 1, carcinogenic to humans)23 have enough supportive data to estimate type-specific risks of transition between the health states; with rare cancer outcomes, HPV39, HPV51, HPV56, and HPV59 (IARC Group 1), and HPV68 (IARC Group 2A, probably carcinogenic to humans)23 are pooled into a single stratum called 'other hrHPV types'; and the many non-carcinogenic “low-risk” (lr) types are also pooled into two strata including types classified into IARC Group 2B (possibly carcinogenic to humans; includes HPV26, HPV53, HPV56, HPV66, HPV67, HPV70, HPV73, HPV82, HPV30, HPV34, HPV69, HPV85, HPV97) and IARC Group 3 (not classifiable; includes condyloma-associated HPV6 and HPV11 and common lr types like HPV61 and HPV72).23,24 While lrHPV infections only rarely cause true precancer or cancer,25 we will include these in the natural history model because they can cause false positive results on hrHPV assays or contribute to “look-alike” lesions resembling precancer when screening interventions are modeled; misclassifying them as high-risk tends to lead to higher costs and overtreatment.
5.2. Time since Infection
The duration of detectable infection is the main determinant of HPV clearance.21 In the absence of progression to precancer, the different HPV types tend to disappear following the same exponential curve (rapid initial clearance that plateaus by three years).21,26 The longer an infection persists as a detectable infection using clinically validated assays, the greater the likelihood of continued persistence, which is independent of other types present and highly linked to progression to precancer.21,26,27 The probability of invasion of a precancer is a function of time and the accumulation of mutations.19
5.3. Host response to HPV: Hypothesized differences In cell-mediated Immune responses at the population level
The probabilities of transitioning between states show variability not fully acknowledged in current models, as signaled by the differences in HPV prevalence patterns across the lifespan linked to different levels of immunologic control of HPV infections. At least three distinct natural history patterns are observed globally (Figure 3), and may require separate health decision models with different transition probabilities: 1) immunocompetent populations are typically characterized by uniformly low rates of HPV across the lifespan or, more often, declining HPV prevalence with age, low prevalence in mid-adult ages where screening is optimal, and often a minor secondary uptick at older ages (henceforth referred to as the Lower HPV Prevalence Model); 2) partially immunodeficient populations without HIV (e.g., those affected by chronic parasitoses in some lower-resource areas) show stable or even increasing, moderate HPV prevalence at mid-adult ages (Higher HPV Prevalence Model); and 3) HIV-infected populations have pronounced immunodeficiency in controlling HPV infections, leading to continuous high prevalence across ages (HIV Model). While there is robust evidence supporting the need for an HIV model, it is not yet clear whether distinct models will be needed to reflect Lower and Higher HPV prevalence settings.
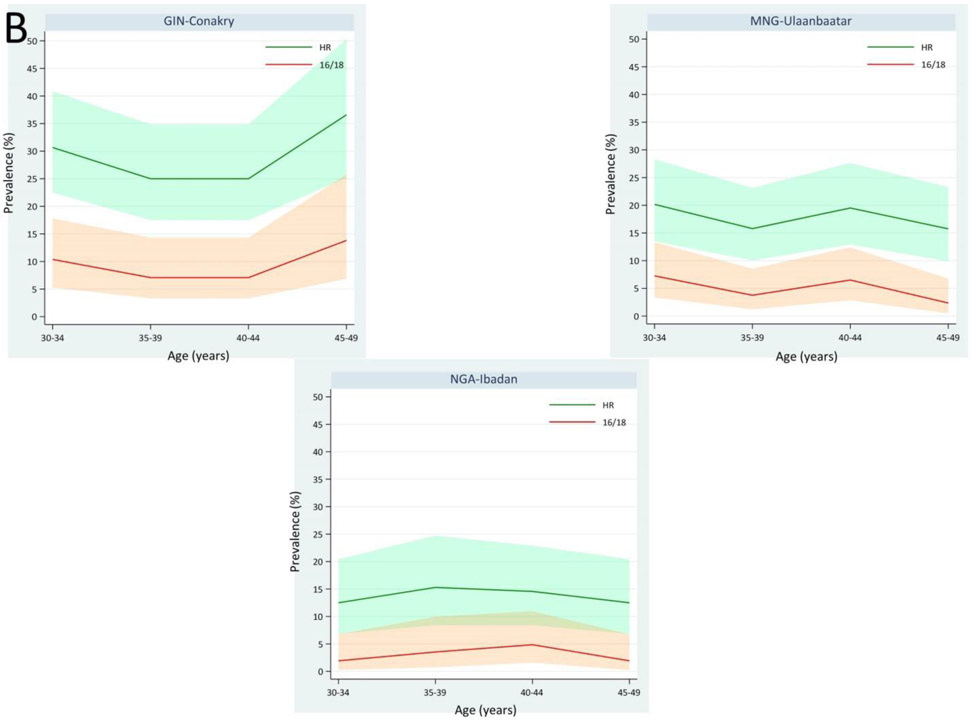
Figure 3. Global HPV prevalence patterns.
There are at least three distinct HPV natural history patterns that are observed globally, likely linked to different levels of immunologic control of HPV infections: a) immunocompetent populations are characterized by lower HPV prevalence in mid-adult women between the ages of 30 and 49 years, when screening is optimal; this pattern is characteristic of the Americas, Europe, and parts of Asia and the Middle East/Northern Africa; b) partially immunodeficient populations that do not have a high burden of HIV but appear to have reduced cell-mediated immunity (for instance, due to chronic parasitoses) show higher HPV prevalence at optimal screening ages; this pattern is characteristic particularly in sub-Saharan Africa; and c) HIV-infected women, with pronounced immunodeficiency in controlling HPV infections, leading to continuous high prevalence across screening ages. The graphs display the prevalence of any hrHPV (green lines) and HPV16/18 (red lines).
6. Directly estimate transition probabilities from representative populations
We hypothesize that each of the observed HPV prevalence patterns (i.e., Lower HPV Prevalence, Higher HPV Prevalence, and HIV) requires its own natural history model with different underlying transition risks. We reason that population differences in rates of HPV appearance and/or disappearance drive the differences between these prevalence curves, and may be attributable to viral-host interactions—particularly cell-mediated immunity, which may vary by setting.
6.1. The Lower HPV Prevalence Model.
The Lower HPV Prevalence Model characterizes most higher-resource populations in the Americas, Europe, and Oceania,28 with HPV prevalence that peaks soon after sexual initiation and declines with age (or, in some countries in Asia, the Middle East, and North Africa, remains low throughout the lifespan, likely as a result of reduced sexual transmission).17 A slight rebound around menopause may be attributed to immune senescence (i.e., weakening of the HPV-suppressive cell-mediated immune response due to age).29 Based on data from screened populations with this HPV prevalence pattern, precancer prevalence requires a period of lesional growth in order to be diagnosed, and therefore peaks several years after the initial rise in HPV prevalence, although the exact moment of progression on the molecular level to a clone of transformed cells is earlier and not observable. Cancer incidence typically peaks or plateaus many years later.30
Of the three models, data are most abundant to inform transitions in the Lower HPV Prevalence Model, as most longitudinal studies of HPV infection occur in populations characterized by this pattern. Large NCI-funded data sources allowing for direct estimation of appearance, disappearance, and progression in Lower HPV Prevalence settings include the National Cancer Institute/Kaiser Permanente Northern California Persistence and Progression (NCI/KPNC PaP) study, the Guanacaste Natural History Study,31 the control arm of the Costa Rica Vaccine Trial and Long-Term Follow-Up Study,32 and the ASCUS-LSIL Triage Study (ALTS).33 We would welcome additional collaborations to confirm portability of our estimates.
6.2. The Higher HPV Prevalence Model.
Compared to the Lower HPV Prevalence Model, the Higher HPV Prevalence Model is characterized by a lesser decline in HPV prevalence as women age.28 Meta-analytic data suggest that this HPV prevalence curve is observed in some equatorial populations in Africa and Central and South America, and does not appear to be solely attributable to HIV burden as it occurs even in populations with a low burden of HIV.34,35 This continuously high burden of HPV prior to menopause may be due to environmental conditions that lead to a compromised immune response, including chronic parasitosis or helminth infestation.36
An alternative explanation of the HPV prevalence patterns might be that the presence (absence) of screening and treatment programs— not altered natural history transitions— lead to lower (higher) hrHPV prevalence in mid-adult women. Data from the NCI/Kaiser Permanente Northern California cohort suggest that among women under age 25 years, the cumulative risk of CIN2+ over 16 years of follow-up is approximately 10% (unpublished data); if treatment also results in resolution of the hrHPV infection, this could partially explain the very low prevalence in mid-adult women in Lower HPV Prevalence settings with organized programs. The KPNC population is very well-screened (the cumulative risk of colposcopy in the same age group reaches approximately 35% over 16 years), and it is unclear how many of the lesions in young women would regress spontaneously within a short timespan. In Higher HPV Prevalence settings, hrHPV prevalence remains high among mid-adult women with normal cytology (Supplemental Figure 1). It is unclear whether this is due to different patterns of sexual behavior (male and/or female) across settings.
We hypothesize that impairment of cell-mediated immunity may lead to reduced HPV clearance, thus contributing to sustained HPV prevalence. The only way to test whether there are, in fact, different transition probabilities by population is through analysis of prospective data; we and others are in the process of analyzing data fromthe ACCME cohort (Nigeria)35 and the CONCEPT cohort (Tanzania). More longitudinal data from high-prevalence settings would be welcome (particularly from studies in which multiple biopsies are routinely collected), and will inform decisions about whether distinct Lower and Higher HPV Prevalence models are necessary.
6.3. The HIV Model
The HIV Model represents populations of women living with HIV (WLHIV), who experience a profound and sustained loss of effective HPV control. HPV prevalence remains very high across all ages, due to the increased risk of acquiring HPV and reduced HPV disappearance associated with HIV and declining CD4+ cell count.37-39 Relative to immunocompetent women, WLHIV appear to have an increased risk of HPV persistence, precancer, and cancer that is associated with low CD4+ count,39-41 but it is unclear how much of the increase in cancer is primarily attributable to their higher burden of persistent HPV and associated precancers, versus the extent to which WLHIV with precancer may also be at greater risk of invasion (on a per precancerous lesion level). HIV infection is thought to have less of an impact on the transition to cancer, as invasion depends upon accumulation of mutations rather than immune control. Antiretroviral therapy (ART) has led to significant life expectancy gains, but it does not appear to correct fully the deficient HPV control and viral persistence over time.39,42 Further data are needed on HPV type-and duration-dependent disappearance and progression risks in order to clarify how natural history transitions are modified by HIV and ART status. Because the natural history of HPV is so altered in WLHIV, the HIV model deserves separate consideration beyond the scope of this paper.
7. Identify uncertain transitions that cannot be directly estimated
Natural history transitions that remain uncertain across all three natural history models include 1) the risk of HPV type-specific reappearance; 2) the risk of progression to precancer following HPV type-specific reappearance; and 3) the risk of invasion. Resolution of these uncertainties based on direct observation is unlikely, due to limitations of current measurement tools, the inability to follow individual women over the lifespan, and the obvious ethical reasons against observing the transition from precancer to cancer without intervention. Below we summarize the limited evidence regarding these uncertain transitions, and the assumptions we make within the proposed modeling framework.
7.1. The risk of HPV type-specific reappearance and subsequent progression to precancer
We cannot discern the underlying cause for a woman’s shift from HPV-negative to HPV-positive (i.e., appearance versus reappearance) in the absence of genetic analysis of HPV variants from samples obtained from the time of first infection— which can determine whether an infection is genetically identical to a woman’s initial type-specific infection, or a distinct infection. Evidence for viral latency and subsequent reactivation has been provided by epidemiologic studies in which newly detected HPV infections were found in older women who reported no new sexual partners during the interval between negative and positive HPV tests.43,44 The hypothesized mechanism for viral latency involves maintenance of the viral genome in basal epithelial cells without viral shedding or evidence of clinical disease.18,45 Age-related immune senescence may trigger reactivation and subsequently, redetection. Counteracting this potential for type-specific reappearance following an initial infection, some women develop systemic, type-specific antibodies that may protect against acquisition of future infections with the same type.46-48 However, it is not clear what proportion of women experience a protective level or how long protection may last following seroconversion, and measurement is further complicated by the differential sensitivity of type-specific serology assays.
From a modeling perspective, the underlying cause of type-specific reappearance— whether acquisition of a new infection or reactivation of a prior one— only needs to be specified if 1) there is a difference in subsequent risk of progression to precancer; or 2) for evaluations of vaccination, the vaccine has differential effectiveness against new acquisition versus reactivation. We hypothesize that reactivated infections in older women behave similarly to newly acquired infections— that is, only active (as opposed to latent) infections confer a risk of progression to precancer, and the critical determinant of progression is whether the infection persists at a detectable level or whether a woman’s immune system is able to regain control of it.49 This hypothesis is supported by evidence from the KPNC/PaP study cohort (in which the incidence of CIN2+ or CIN3+ following a newly detected HPV infection was similar or lower in older women compared to younger women)50 and from the Guanacaste Natural History Study (which demonstrated that women with re-appearance of type-specific infections following two or more negative HPV tests had a very low risk of CIN2+).51 By assuming (consistent with the evidence) that reactivated infections in older women behave no worse than newly acquired infections, we avoid the need to model differential progression risks for newly acquired versus reactivated infections when screening is being evaluated. Instead we model HPV appearance, which includes both newly acquired and reactivated infections, and can be measured when a woman shifts from a negative to a positive HPV result on a validated assay; the time clock determining the risks of disappearance and progression starts at the time of appearance, whether or not a woman has been infected with this type before. Given that vaccine trials in women over age 25 years have been underpowered to examine vaccine effectiveness in older women with evidence of past HPV exposure,52,53 health decision models may not be able to reliably evaluate vaccination in older women unless new data become available.
7.2. The risk of invasion
The risk of invasion remains the most uncertain transition in cervical carcinogenesis, and it cannot be directly estimated. Modeling the risk of invasion requires estimating the duration of precancer in the absence of intervention— the so-called “dwell time”. As modern clinical studies censor women upon the development of CIN2/3, the transition risk from precancer to cancer cannot be observed for ethical reasons. A retrospective study from New Zealand analyzed historical data of women with typically large, long-standing cases of CIN3 (average age of 39) that were followed unethically many years ago,54 but the implied dwell time is underestimated because it is not clear how long lesions were present prior to the beginning of follow-up. Below we address methods for indirect estimation of this and other uncertain transition risks in the proposed models.
8. Calibrate uncertain transitions
In the absence of direct estimates, we rely on model fitting techniques known as calibration to infer values for uncertain transitions. As described above, the risk of invasion remains uncertain; additionally, HPV appearance risks may vary considerably between populations, as sexual behavior patterns differ. Once natural history model transitions have been directly estimated to the extent that available data allow (e.g., risks of HPV disappearance and progression to precancer, which we assume as a necessary simplification are consistent within each of the Lower HPV Prevalence, Higher HPV Prevalence, and HIV Models), statistical methods can be used to explore values for uncertain transitions (e.g., risks of appearance, invasion) (Figure 4A, 4B). The goal of calibration is to hone in on values for the uncertain transitions that are consistent with both the data-driven transition risks and empirical data on, for example, type-specific HPV prevalence in a population (considering age and cohort effects); distribution of HPV types in precancer and cancer; and incidence of invasive cancer (considering age and period effects). A strength of the proposed framework is that it focuses on direct estimation (rather than calibration) for most transitions. With fewer unknown transitions, the model is less vulnerable to non-identifiability (i.e., different combinations of transition values can fit the same empirical data), which can weaken the utility of health decision analysis.
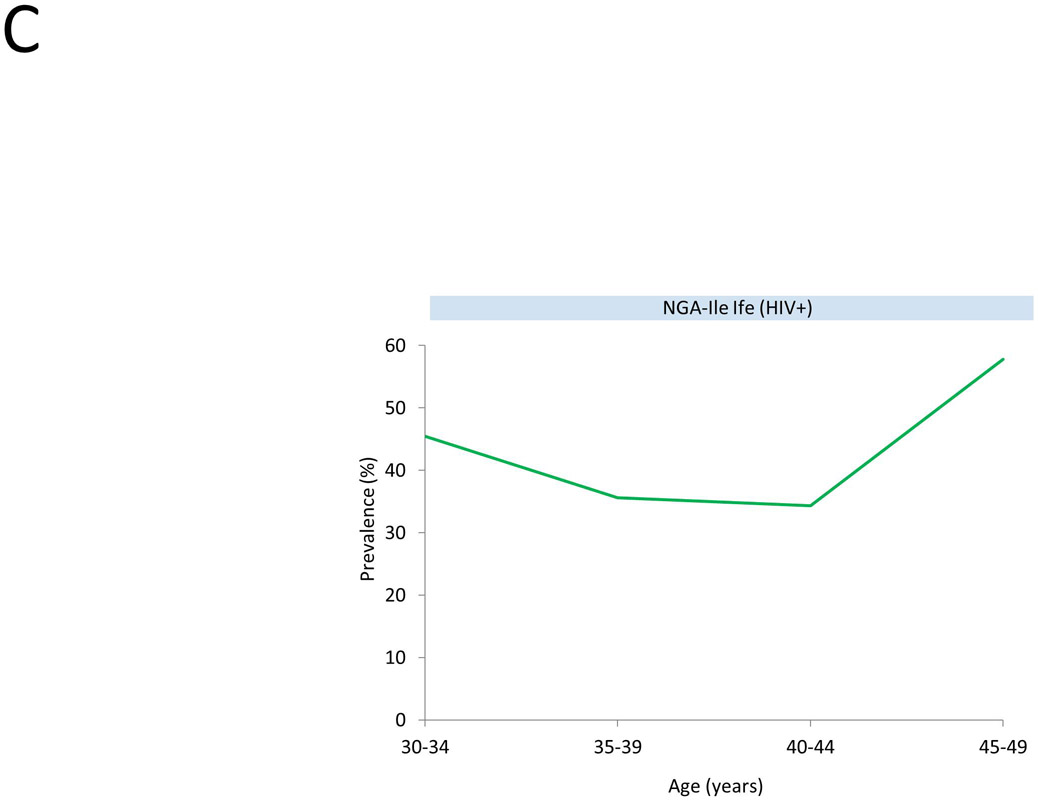
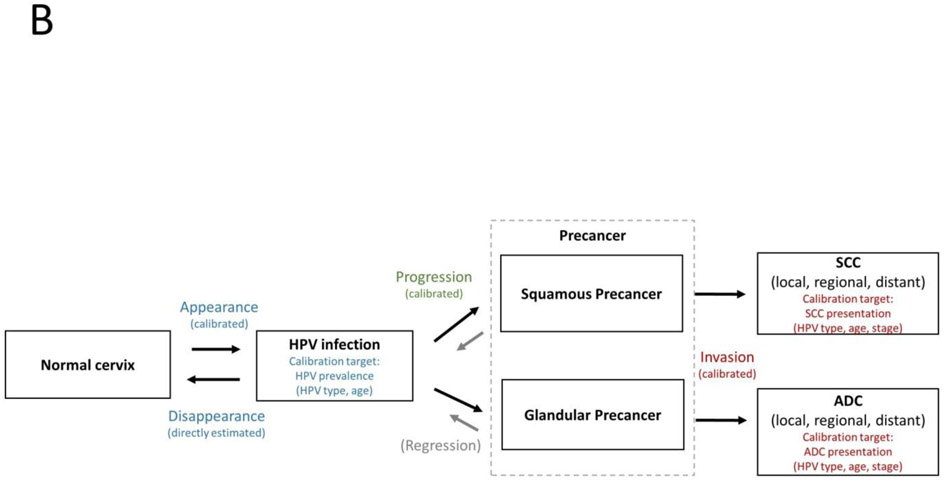
Figure 4. Direct estimation versus calibration of transition probabilities.
In the Lower HPV Prevalence Model (A), data are available to directly estimate transition risks for disappearance and progression from longitudinal studies. We assume these risks are consistent across Lower HPV Prevalence populations. The transition risks for appearance vary according to sexual behavior in a population, and can only be directly estimated when population-based longitudinal data are available. Thus, in most cases, the risk of appearance is calibrated to fit HPV prevalence (by genotype and age) while using direct estimates for disappearance. We will explore the impact of individual-level frailty and how it may impact clustering of infections appearing within a woman (due to sexual behavior or immune factors). We assume the risk of disappearance is the same whether an infection was newly acquired or reactivated.
In the Higher HPV Prevalence Model (B), data will soon be available from longitudinal studies to directly estimate transition risks for disappearance. We assume these risks are consistent across Higher HPV Prevalence populations with a low burden of HIV. As in Lower HPV Prevalence settings, direct estimates for the risk of appearance are rarely available, so this transition risk will be calibrated to fit HPV prevalence while using direct estimates for disappearance. Due to limited data, direct estimates for progression risks in Higher HPV Prevalence settings are not available. We are exploring the relationship between the prevalence of precancer among women with hrHPV in Lower and Higher HPV prevalence settings to determine whether progression risks (conditional on hrHPV infection) are similar to Lower HPV Prevalence settings or would need to be calibrated.
In both the Lower and Higher HPV Prevalence models, the risk of invasion is unobserved for ethical reasons, and must be calibrated to fit cancer presentation data for squamous cell carcinoma and adenocarcinoma (by HPV genotype, age and stage at presentation prior to widespread screening). Whether the risk of invasion is initially calibrated in a Higher HPV Prevalence setting (where screening may be less widespread and HPV prevalence patterns may better reflect sexual behavior patterns among more recent cohorts) or a Lower HPV Prevalence setting (where more data are available to directly estimate progression risk and prevalence of precancer), we anticipate holding the risk of invasion constant between models, as we hypothesize that this transition does not change as a function of cell-mediated immunity.
The HIV Model is not shown, as it is not yet clear which transition risks can be directly estimated versus calibrated.
9. Summary of main differences between the proposed and current natural history models
Existing health decision models of HPV infection and cervical carcinogenesis have been instrumental in evaluating the shift from cytology-based screening to HPV testing— starting with HPV triage of ASC-US (or equivocal cytology) rather than repeat cytology,55 and now moving to primary screening.56,57 The earliest models defined precancerous health states using cytologic classifications (e.g., LSIL, HSIL);58-60 later models shifted towards histologic classifications (i.e., CIN1, CIN2, CIN3).13,56,61,62 One published model (developed by several authors of this paper) initiated the removal of CIN1 as a health state on the causal pathway and also implemented time-dependent transition risks.63 The proposed framework relies on these fundamental changes, as well as others described in Table 2. In order to project the performance of new technologies that can identify a transforming infection with increasing accuracy, microsimulation models will need to define precancer more rigorously than at present; to evaluate prevention strategies (i.e., age, screening interval, screening test), transitions must reflect time-in-state.
Table 2.
Summary of main differences between the proposed and current natural history models of HPV infection and cervical carcinogenesis.a
| Model feature | Existing models | Proposed modeling framework |
|---|---|---|
| Health states | Normal cervix HPV infection Immuneb CIN1, CIN2, CIN3 Cervical cancer Pros:
Cons:
|
Normal cervix HPV infection Precancer Cervical cancer Pros:
Cons:
|
| Corollary transitions | HPV acquisition HPV clearance (with or without immunityb) HPV progression/regression to/from CIN1, CIN2, CIN3 Invasion Pros:
Cons:
|
HPV appearance HPV disappearance HPV progression Invasion Pros:
Cons:
|
| Variables that modify transitions | HPV acquisition: Age, HPV type, history of prior type-specific infectionb HPV clearance: Age, HPV type HPV progression/regression: Age, HPV type Invasion: Age, HPV type Stratified models for: WLHIV Pros:
Cons:
|
HPV appearance: Age, HPV type HPV disappearance: time since infection HPV progression: HPV type, time since infection Invasion: HPV type, time since infection/duration of precancer Stratified models for: Lower HPV prevalence setting Higher HPV prevalence setting WLHIV Pros:
Cons:
|
| Direct estimation of transition Probabilities c | Varies by model Pros:
Cons:
|
HPV appearance (when data available) HPV disappearance HPV progression (Lower HPV prevalence setting) Data sources: Guanacaste Natural History Study, Costa Rica Vaccine Trial and Long-Term Follow-Up Study, ALTS (Lower HPV Prevalence Model) ACCME Cohort, Project Itoju (Higher HPV Prevalence Model) Pros:
Cons:
|
| Uncertain parameters requiring calibration or model-fitting Techniques c | Estimation of most transitions requires some use of model-fitting techniques Pros:
Cons:
|
HPV appearance (when data unavailable) HPV progression (Higher HPV prevalence settings) Invasion Pros:
Cons:
|
HPV: human papillomavirus; CIN: cervical intraepithelial neoplasia (grade 1, 2, or 3); WLHIV: women living with HIV.
“Immune” refers to a reduced risk of HPV type-specific re-infection. Existing models typically include either a separate immune health state or a reduced likelihood of repeat acquisition with the same type.
Data on HPV transition risks for WLHIV, as a function of immune and antiretroviral therapy status, are very limited. The HIV Model deserves thorough consideration that is beyond the scope of this paper.
9.1. Shifting away from health states defined by histopathology
The move away from the CIN scale might be seen as controversial but it is important. Most health decision models still require sequential progression through separate health states for CIN1 (mild dysplasia), CIN2 (moderate dysplasia), and CIN3 (severe dysplasia and carcinoma in situ) prior to cervical cancer. However, there is strong evidence against the reproducibility and biologic meaning of this three-part diagnostic scoring and its inventor long ago abandoned it.64 While considered a reference standard of diagnosis, histopathology results depend on the placement of colposcopically-directed biopsy, and typically only the most visible lesion(s) are sampled. The categories are not reproducible.65 CIN1 is merely an inaccurate indication of HPV infection, rather than a necessary and measurable stage on the causal pathway to cervical cancer.66 CIN2 is a heterogeneous classification— while some will eventually invade, many will regress over time.67 Efforts to divide CIN2 into low-grade and high-grade lesions based on immunohistochemical staining of p16, a progression-related biomarker (i.e., the Lower Anogenital Squamous Terminology [LAST] classification system), have proved inadequate, with many lesions staining positive without evidence of precancer.68 Even reliance on the stricter histologic classification of CIN3/AIS as a surrogate for precancer may lead to some misspecification of invasive potential, because several hrHPV types (e.g., HPV51) are commonly found in CIN3/AIS but very rarely in invasive cancers.21,69
In short, we argue that while histopathologic CIN2 or CIN3 or histologic HSIL or AIS taken alone are potential markers of precancer, these are neither sufficiently reproducible nor specific to represent discrete and necessary health states on the causal pathway. Acknowledging that precancer cannot be perfectly discriminated, we aim to rely on composite measures, including both molecular and morphological endpoints, to estimate this health state in the proposed natural history model. The ideal would be to avoid identifying precancer too narrowly (missing some lesions at high risk of invasion) or too broadly (including lesions that are not likely to invade). Important predictors of lesion severity, to be used in combination as available with histology, include restriction to lesions associated with definitely carcinogenic HPV types and known duration of infection. At present, we will define precancer as a reference pathology diagnosis of CIN2 or CIN3 or a LAST system HSIL that is accompanied by at least one of the 13 hrHPV types. Requiring reference pathology standards and genotyping to define precancer restricts the primary data sources that can be used to develop the natural history model, but allows the model to more accurately assess the enhanced predictive value of forthcoming biomarker assays, some of which will eventually be better at identifying precancer than the current CIN scale. As novel biomarkers with improved predictive value are validated and available from longitudinal data sets, these could be incorporated into the modeling framework’s definition of precancer (e.g., the size of the lesion as a measure of duration of precancer, detection of over-expression of HPV E6 and E7 oncoproteins, viral/host DNA methylation and integration).
9.2. Transitions based on time-in-state
Another difference in the proposed model (relative to most earlier generations of health decision models) is the assumption that transitions from the HPV-infected state rely profoundly on duration—that is, the longer an infection actively persists, the less likely it is to clear and the more likely it is to have progressed. Invasion also relies on duration but with a more linear transition probability. Other health decision models have typically based these transitions on age— assuming that as women age, the risks of viral persistence and progression tend to increase. We suggest that these age-based HPV risks are combining two different groups of infection in older women: 1) persistent infections that have been present for years (often these infections are prevalently detected at baseline in long-term follow-up studies); and 2) newer appearing infections (either newly acquired or 'reactivated' due to loss of immune control). Newly appearing infections at any age of a woman are associated with lower risk than persistent ones.49 By averaging transition risks for these two different groups, models using age-based clearance and progression risks will likely underestimate the risk of longstanding prevalent infections and overestimate the risk of newly appearing infections in older women. Thus, these models likely overestimate the median age at which cancer-causing HPV infections are acquired, thus overestimating the benefits of vaccination at older ages. To compensate for later age at acquiring the causal infection these models must speed the risks of progression and invasion to achieve model fit to cancer incidence targets, thus yielding potentially erroneous policy conclusions regarding the length of screening intervals for primary HPV testing.13 By estimating transition risks by duration of infection and rigorously defining precancer, the proposed model can reflect the differential risk of precancer among women with persistent versus newly appearing infections.
10. Conclusions
We present a new health decision modeling framework that is aligned with the multi-stage causal pathway to cervical cancer. We argue that the model health states (i.e., normal cervix, HPV infection, precancer, and cancer) and corollary transitions (i.e., appearance, disappearance, progression, and invasion) apply universally across all populations. However, the risks of transitioning between health states likely differ, as evidenced by variation in HPV prevalence patterns attributable to cell-mediated immunity. We argue that direct estimates of HPV-type specific transition probabilities are available to inform more natural history transitions than existing models currently use. It will be critical to determine whether HPV transition risks vary by population based on cell-mediated immunity, necessitating at least two natural history models for HIV-negative women.
The proposed microsimulation modeling framework will be well-suited to address complex cervical screening and triage algorithms, including novel biomarker tests. It will also be able to estimate the direct benefits associated with HPV vaccination strategies. However, we acknowledge that a variety of modeling approaches are useful. Further work will be needed to develop companion dynamic models of HPV transmission consistent with the proposed framework to estimate the indirect benefits (i.e., herd immunity) of vaccination strategies; these models will likely rely on calibration to a greater extent than the microsimulation model we propose here. Disadvantages of the proposed microsimulation framework are the resource requirements for development— both time and data needs are intensive. However, once microsimulation models evolve to have greater fidelity to the natural history, we expect they will be better able to inform simpler and more accessible modeling approaches with fewer data needs.
We are working actively with colleagues who work in lower-prevalence settings to validate this model; in higher-prevalence populations to fill in remaining data gaps among populations with the greatest burden of cervical cancer; and among WLHIV to gather data on the fundamental effectiveness of prevention strategies. We invite discussion and challenges to our approach. Our goal is to elevate the perceived quality of evidence from microsimulation models so that these tools can be used with maximum achievable confidence to inform efficient use of resources and achieve global cervical cancer control.
Supplementary Material
Highlights:
Health decision models project HPV natural history and impact of cervical cancer prevention methods over women's lifetimes.
Such models are often considered a lesser form of scientific evidence due to uncertain input data and base assumptions.
We propose a new modeling framework aligned with type-specific HPV natural history and necessary, measurable causal steps.
Acknowledgments
Conflict of interest statement
Dr. Campos reports other salary support from the National Cancer Institute, and personal fees from Basic Health International, outside the submitted work. Dr. Demarco, Dr. Desai, Dr. Gage, and Dr. Schiffman have received cervical cancer screening equipment, supplies, and masked HPV and cytology test results at no cost for independent evaluations of technologies from Roche Molecular Systems, BD Diagnostics, Qiagen, and MobileODT. Dr. Bruni has received HPV test kits at no cost from Roche for research purposes; the Cancer Epidemiology Research Programme with which Dr. Bruni is affiliated has received sponsorship for grants from Merck and Co., Inc. Dr. Adebamowo reports grants from the National Institutes of Health and the American Cancer Society during the conduct of the study. Dr. Kim reports grants from the National Cancer Institute during the conduct of the study. Dr. de Sanjose reports no competing interest.
Funding
The study was funded by the NCI Intramural Research Program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
HPV35 appears to be more prevalent in cancers among women of African descent. The differential natural history of HPV35 across racial groups is still being explored.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2.Guan P, Howell-Jones R, Li N, Bruni L, de Sanjose S, Franceschi S, Clifford GM. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer 2012;131:2349–59. [DOI] [PubMed] [Google Scholar]
- 3.Bruni L, Saura A, Montoliu A, Brotons M, Alemany L, Diallo MS, Afsar OZ, LaMontagne DS, Mosina L, Contreras M, Velandia-Gonzalez M, Pastore R, Gacic-Dobo M, Bloem P HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Preventive Medicine 2020;106399. [DOI] [PubMed] [Google Scholar]
- 4.Gakidou E, Nordhagen S, Obermeyer Z. Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PLoS Med 2008;5:e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canfell K, Chesson H, Kulasingam SL, Berkhof J, Diaz M, Kim JJ. Modeling preventative strategies against human papillomavirus-related disease in developed countries. Vaccine 2012;30 Suppl 5:F157–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Organization WH. WHO Director-General calls for all countries to take action to help end the suffering caused by cervical cancer. 2018.
- 7.Brisson M, Kim JJ, Canfell K, Drolet M, Gingras G, Burger EA, Martin D, Simms KT, Benard E, Boily MC, Sy S, Regan C, Keane A, Caruana M, Nguyen DTN, Smith MA, Laprise JF, Jit M, Alary M, Bray F, Fidarova E, Elsheikh F, Bloem PJN, Broutet N, Hutubessy R. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet 2020;395:575–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldie SJ, Kim JJ, Myers E. Chapter 19: Cost-effectiveness of cervical cancer screening. Vaccine 2006;24 Suppl 3:S3/164–70. [DOI] [PubMed] [Google Scholar]
- 9.Egger M, Johnson L, Althaus C, Schoni A, Salanti G, Low N, Norris SL. Developing WHO guidelines: Time to formally include evidence from mathematical modelling studies. F1000Res 2017;6:1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frommert D Spot on or way off? Validating results of the AVID microsimulation model retrospectively. International Journal of Microsimulation 2015;8:3–32. [Google Scholar]
- 11.Kuntz KM, Lansdorp-Vogelaar I, Rutter CM, Knudsen AB, van Ballegooijen M, Savarino JE, Feuer EJ, Zauber AG. A systematic comparison of microsimulation models of colorectal cancer: the role of assumptions about adenoma progression. Med Decis Making 2011;31:530–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pignone M, Ransohoff DF. Cross-model comparisons to improve the value of modeling: the case of colorectal cancer screening. Med Decis Making 2011;31:524–6. [DOI] [PubMed] [Google Scholar]
- 13.Burger EA, de Kok I, Groene E, Killen J, Canfell K, Kulasingam S, Kuntz KM, Matthijsse S, Regan C, Simms KT, Smith MA, Sy S, Alarid-Escudero F, Vaidyanathan V, van Ballegooijen M, Kim JJ. Estimating the Natural History of Cervical Carcinogenesis Using Simulation Models: A CISNET Comparative Analysis. J Natl Cancer Inst 2020;112:955–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schiffman M, Doorbar J, Wentzensen N, de Sanjose S, Fakhry C, Monk BJ, Stanley MA, Franceschi S. Carcinogenic human papillomavirus infection. Nat Rev Dis Primers 2016;2:16086. [DOI] [PubMed] [Google Scholar]
- 15.Rutter CM, Zaslavsky AM, Feuer EJ. Dynamic microsimulation models for health outcomes: a review. Med Decis Making 2011;31:10–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schiffman M, Wentzensen N. Human papillomavirus infection and the multistage carcinogenesis of cervical cancer. Cancer Epidemiol Biomarkers Prev 2013;22:553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, Bajos N. Sexual behaviour in context: a global perspective. Lancet 2006;368:1706–28. [DOI] [PubMed] [Google Scholar]
- 18.Hammer A, de Koning MN, Blaakaer J, Steiniche T, Doorbar J, Griffin H, Mejlgaard E, Svanholm H, Quint WG, Gravitt PE. Whole tissue cervical mapping of HPV infection: Molecular evidence for focal latent HPV infection in humans. Papillomavirus Res 2019;7:82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Doorbar J, Quint W, Banks L, Bravo IG, Stoler M, Broker TR, Stanley MA. The biology and life-cycle of human papillomaviruses. Vaccine 2012;30 Suppl 5:F55–70. [DOI] [PubMed] [Google Scholar]
- 20.Stoler MH, Wright TC, Parvu V, Yanson K, Eckert K, Kodsi S, Cooper C. HPV Testing With 16, 18, and 45 Genotyping Stratifies Cancer Risk for Women With Normal Cytology. Am J Clin Pathol 2019;151:433–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demarco M, Hyun N, Carter-Pokras O, Raine-Bennett TR, Cheung L, Chen X, Hammer A, Campos N, Kinney W, Gage JC, Befano B, Perkins RB, He X, Dallal C, Chen J, Poitras N, Mayrand MH, Coutlee F, Burk RD, Lorey T, Castle PE, Wentzensen N, Schiffman M. A study of type-specific HPV natural history and implications for contemporary cervical cancer screening programs. EClinicalMedicine 2020;22:100293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinheiro M, Gage JC, Clifford GM, Demarco M, Cheung LC, Chen Z, Yeager M, Cullen M, Boland JF, Chen X, Raine-Bennett T, Steinberg M, Bass S, Befano B, Xiao Y, Tenet V, Walker J, Zuna R, Poitras NE, Gold MA, Dunn T, Yu K, Zhu B, Burdett L, Turan S, Lorey T, Castle PE, Wentzensen N, Burk RD, Schiffman M, Mirabello L. Association of HPV35 with cervical carcinogenesis among women of African ancestry: Evidence of viral-host interaction with implications for disease intervention. Int J Cancer 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.International Agency for Research on Cancer. A review of human carcinogens. Part B: Biological agents. In. 2009 ed. Lyon: International Agency for Research on Cancer; 2009. [Google Scholar]
- 24.Clifford GM, Smith JS, Plummer M, Munoz N, Franceschi S. Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br J Cancer 2003;88:63–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guimera N, Lloveras B, Alemany L, Iljazovic E, Shin HR, Jung-Il S, de Sanjose S, Jenkins D, Bosch FX, Quint W. Laser capture microdissection shows HPV11 as both a causal and a coincidental infection in cervical cancer specimens with multiple HPV types. Histopathology 2013;63:287–92. [DOI] [PubMed] [Google Scholar]
- 26.Plummer M, Schiffman M, Castle PE, Maucort-Boulch D, Wheeler CM, Group A. A 2-year prospective study of human papillomavirus persistence among women with a cytological diagnosis of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion. J Infect Dis 2007;195:1582–9. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez AC, Schiffman M, Herrero R, Hildesheim A, Bratti C, Sherman ME, Solomon D, Guillen D, Alfaro M, Morales J, Hutchinson M, Katki H, Cheung L, Wacholder S, Burk RD. Longitudinal study of human papillomavirus persistence and cervical intraepithelial neoplasia grade 2/3: critical role of duration of infection. J Natl Cancer Inst 2010;102:315–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bruni L, Diaz M, Castellsague X, Ferrer E, Bosch FX, de Sanjose S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis 2010;202:1789–99. [DOI] [PubMed] [Google Scholar]
- 29.Gravitt PE. The known unknowns of HPV natural history. J Clin Invest 2011;121:4593–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Plummer M, Peto J, Franceschi S, International Collaboration of Epidemiological Studies of Cervical C. Time since first sexual intercourse and the risk of cervical cancer. Int J Cancer 2012;130:2638–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bratti MC, Rodriguez AC, Schiffman M, Hildesheim A, Morales J, Alfaro M, Guillen D, Hutchinson M, Sherman ME, Eklund C, Schussler J, Buckland J, Morera LA, Cardenas F, Barrantes M, Perez E, Cox TJ, Burk RD, Herrero R. Description of a seven-year prospective study of human papillomavirus infection and cervical neoplasia among 10000 women in Guanacaste, Costa Rica. Rev Panam Salud Publica 2004;15:75–89. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez P, Hildesheim A, Herrero R, Katki H, Wacholder S, Porras C, Safaeian M, Jimenez S, Darragh TM, Cortes B, Befano B, Schiffman M, Carvajal L, Palefsky J, Schiller J, Ocampo R, Schussler J, Lowy D, Guillen D, Stoler MH, Quint W, Morales J, Avila C, Rodriguez AC, Kreimer AR. Rationale and design of a long term follow-up study of women who did and did not receive HPV 16/18 vaccination in Guanacaste, Costa Rica. Vaccine 2015;33:2141–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schiffman M, Solomon D. Findings to date from the ASCUS-LSIL Triage Study (ALTS). Arch Pathol Lab Med 2003;127:946–9. [DOI] [PubMed] [Google Scholar]
- 34.Gage JC, Ajenifuja KO, Wentzensen N, Adepiti AC, Stoler M, Eder PS, Bell L, Shrestha N, Eklund C, Reilly M, Hutchinson M, Wacholder S, Castle PE, Burk RD, Schiffman M. Effectiveness of a simple rapid human papillomavirus DNA test in rural Nigeria. Int J Cancer 2012;131:2903–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adebamowo SN, Dareng EO, Famooto AO, Offiong R, Olaniyan O, Obende K, Adebayo A, Ologun S, Alabi B, Achara P, Bakare RA, Odutola M, Olawande O, Okuma J, Odonye G, Adebiyi R, Dakum P, Adebamowo CA. Cohort Profile: African Collaborative Center for Microbiome and Genomics Research's (ACCME's) Human Papillomavirus (HPV) and Cervical Cancer Study. Int J Epidemiol 2017;46:1745–1745j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gravitt PE, Marks M, Kosek M, Huang C, Cabrera L, Olortegui MP, Medrano AM, Trigoso DR, Qureshi S, Bardales GS, Manrique-Hinojosa J, Cardenas AZ, Larraondo MA, Cok J, Qeadan F, Siracusa M, Gilman RH. Soil-Transmitted Helminth Infections Are Associated With an Increase in Human Papillomavirus Prevalence and a T-Helper Type 2 Cytokine Signature in Cervical Fluids. J Infect Dis 2016;213:723–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strickler HD, Burk RD, Fazzari M, Anastos K, Minkoff H, Massad LS, Hall C, Bacon M, Levine AM, Watts DH, Silverberg MJ, Xue X, Schlecht NF, Melnick S, Palefsky JM. Natural history and possible reactivation of human papillomavirus in human immunodeficiency virus-positive women. J Natl Cancer Inst 2005;97:577–86. [DOI] [PubMed] [Google Scholar]
- 38.Safaeian M, Kiddugavu M, Gravitt PE, Gange SJ, Ssekasanvu J, Murokora D, Sklar M, Serwadda D, Wawer MJ, Shah KV, Gray R. Determinants of incidence and clearance of high-risk human papillomavirus infections in rural Rakai, Uganda. Cancer Epidemiol Biomarkers Prev 2008;17:1300–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu G, Sharma M, Tan N, Barnabas RV. HIV-positive women have higher risk of human papilloma virus infection, precancerous lesions, and cervical cancer. AIDS 2018;32:795–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dhokotera T, Bohlius J, Spoerri A, Egger M, Ncayiyana J, Olago V, Singh E, Sengayi M. The burden of cancers associated with HIV in the South African public health sector, 2004-2014: a record linkage study. Infect Agent Cancer 2019;14:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abraham AG, D'Souza G, Jing Y, Gange SJ, Sterling TR, Silverberg MJ, Saag MS, Rourke SB, Rachlis A, Napravnik S, Moore RD, Klein MB, Kitahata MM, Kirk GD, Hogg RS, Hessol NA, Goedert JJ, Gill MJ, Gebo KA, Eron JJ, Engels EA, Dubrow R, Crane HM, Brooks JT, Bosch RJ, Strickler HD, North American ACCoR, Design of Ie DEA. Invasive cervical cancer risk among HIV-infected women: a North American multicohort collaboration prospective study. J Acquir Immune Defic Syndr 2013;62:405–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Minkoff H, Ahdieh L, Massad LS, Anastos K, Watts DH, Melnick S, Muderspach L, Burk R, Palefsky J. The effect of highly active antiretroviral therapy on cervical cytologic changes associated with oncogenic HPV among HIV-infected women. AIDS 2001;15:2157–64. [DOI] [PubMed] [Google Scholar]
- 43.Gonzalez P, Hildesheim A, Rodriguez AC, Schiffman M, Porras C, Wacholder S, Pineres AG, Pinto LA, Burk RD, Herrero R. Behavioral/lifestyle and immunologic factors associated with HPV infection among women older than 45 years. Cancer Epidemiol Biomarkers Prev 2010;19:3044–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paul P, Hammer A, Rositch AF, Burke AE, Viscidi RP, Silver MI, Campos N, Youk AO, Gravitt PE. Rates of new human papillomavirus detection and loss of detection in middle-aged women by recent and past sexual behavior. J Infect Dis 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Doorbar J Host control of human papillomavirus infection and disease. Best Pract Res Clin Obstet Gynaecol 2018;47:27–41. [DOI] [PubMed] [Google Scholar]
- 46.Beachler DC, Kreimer AR, Schiffman M, Herrero R, Wacholder S, Rodriguez AC, Lowy DR, Porras C, Schiller JT, Quint W, Jimenez S, Safaeian M, Struijk L, Schussler J, Hildesheim A, Gonzalez P. Multisite HPV16/18 Vaccine Efficacy Against Cervical, Anal, and Oral HPV Infection. J Natl Cancer Inst 2016;108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Safaeian M, Castellsague X, Hildesheim A, Wacholder S, Schiffman MH, Bozonnat MC, Baril L, Rosillon D. Risk of HPV-16/18 Infections and Associated Cervical Abnormalities in Women Seropositive for Naturally Acquired Antibodies: Pooled Analysis Based on Control Arms of Two Large Clinical Trials. J Infect Dis 2018;218:84–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rosillon D, Baril L, Del Rosario-Raymundo MR, Wheeler CM, Skinner SR, Garland SM, Salmeron J, Lazcano-Ponce E, Vallejos CS, Stoney T, Ter Harmsel B, Lim TYK, Quek SC, Minkina G, McNeil SA, Bouchard C, Fong KL, Money D, Ilancheran A, Savicheva A, Cruickshank M, Chatterjee A, Fiander A, Martens M, Bozonnat MC, Struyf F, Dubin G, Castellsague X. Risk of newly detected infections and cervical abnormalities in adult women seropositive or seronegative for naturally acquired HPV-16/18 antibodies. Cancer Med 2019;8:4938–4953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hammer A, Demarco M, Campos N, Befano B, Gravitt PE, Cheung L, Lorey TS, Poitras N, Kinney W, Wentzensen N, Castle PE, Schiffman M. A study of the risks of CIN3+ detection after multiple rounds of HPV testing: Results of the 15-year cervical cancer screening experience at Kaiser Permanente Northern California. Int J Cancer 2020;147:1612–1620. [DOI] [PubMed] [Google Scholar]
- 50.Gage JC, Katki HA, Schiffman M, Fetterman B, Poitras NE, Lorey T, Cheung LC, Castle PE, Kinney WK. Age-stratified 5-year risks of cervical precancer among women with enrollment and newly detected HPV infection. Int J Cancer 2015;136:1665–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rodriguez AC, Schiffman M, Herrero R, Hildesheim A, Bratti C, Sherman ME, Solomon D, Guillen D, Alfaro M, Morales J, Hutchinson M, Cheung L, Wacholder S, Burk RD. Low risk of type-specific carcinogenic HPV re-appearance with subsequent cervical intraepithelial neoplasia grade 2/3. Int J Cancer 2012;131:1874–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Castellsague X, Munoz N, Pitisuttithum P, Ferris D, Monsonego J, Ault K, Luna J, Myers E, Mallary S, Bautista OM, Bryan J, Vuocolo S, Haupt RM, Saah A. End-of-study safety, immunogenicity, and efficacy of quadrivalent HPV (types 6, 11, 16, 18) recombinant vaccine in adult women 24-45 years of age. Br J Cancer 2011;105:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wheeler CM, Skinner SR, Del Rosario-Raymundo MR, Garland SM, Chatterjee A, Lazcano-Ponce E, Salmeron J, McNeil S, Stapleton JT, Bouchard C, Martens MG, Money DM, Quek SC, Romanowski B, Vallejos CS, Ter Harmsel B, Prilepskaya V, Fong KL, Kitchener H, Minkina G, Lim YK, Stoney T, Chakhtoura N, Cruickshank ME, Savicheva A, da Silva DP, Ferguson M, Molijn AC, Quint WG, Hardt K, Descamps D, Suryakiran PV, Karkada N, Geeraerts B, Dubin G, Struyf F. Efficacy, safety, and immunogenicity of the human papillomavirus 16/18 AS04-adjuvanted vaccine in women older than 25 years: 7-year follow-up of the phase 3, double-blind, randomised controlled VIVIANE study. Lancet Infect Dis 2016;16:1154–68. [DOI] [PubMed] [Google Scholar]
- 54.McCredie MR, Sharples KJ, Paul C, Baranyai J, Medley G, Jones RW, Skegg DC. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol 2008;9:425–34. [DOI] [PubMed] [Google Scholar]
- 55.Kim JJ, Wright TC, Goldie SJ. Cost-effectiveness of alternative triage strategies for atypical squamous cells of undetermined significance. JAMA 2002;287:2382–90. [DOI] [PubMed] [Google Scholar]
- 56.Jansen E, Naber SK, Aitken CA, de Koning HJ, van Ballegooijen M, de Kok I. Cost-effectiveness of HPV-based cervical screening based on first year results in the Netherlands: a modelling study. BJOG 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim JJ, Burger EA, Regan C, Sy S. Screening for Cervical Cancer in Primary Care: A Decision Analysis for the US Preventive Services Task Force. JAMA 2018;320:706–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goldie SJ, Weinstein MC, Kuntz KM, Freedberg KA. The costs, clinical benefits, and cost-effectiveness of screening for cervical cancer in HIV-infected women. Ann Intern Med 1999;130:97–107. [DOI] [PubMed] [Google Scholar]
- 59.Myers ER, McCrory DC, Nanda K, Bastian L, Matchar DB. Mathematical model for the natural history of human papillomavirus infection and cervical carcinogenesis. Am J Epidemiol 2000;151:1158–71. [DOI] [PubMed] [Google Scholar]
- 60.Kulasingam SL, Myers ER, Lawson HW, McConnell KJ, Kerlikowske K, Melnikow J, Washington AE, Sawaya GF. Cost-effectiveness of extending cervical cancer screening intervals among women with prior normal pap tests. Obstet Gynecol 2006;107:321–8. [DOI] [PubMed] [Google Scholar]
- 61.Messoudi W, Elmahi T, Nejjari C, Tachfouti N, Zidouh A, Saadani G, Morina D, Diaz M. Cervical cancer prevention in Morocco: a model-based cost-effectiveness analysis. J Med Econ 2019;22:1153–1159. [DOI] [PubMed] [Google Scholar]
- 62.Vanni T, Legood R, Franco EL, Villa LL, Luz PM, Schwartsmann G. Economic evaluation of strategies for managing women with equivocal cytological results in Brazil. Int J Cancer 2011;129:671–9. [DOI] [PubMed] [Google Scholar]
- 63.Campos NG, Burger EA, Sy S, Sharma M, Schiffman M, Rodriguez AC, Hildesheim A, Herrero R, Kim JJ. An updated natural history model of cervical cancer: derivation of model parameters. Am J Epidemiol 2014;180:545–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Richart RM. A modified terminology for cervical intraepithelial neoplasia. Obstet Gynecol 1990;75:131–3. [PubMed] [Google Scholar]
- 65.Stoler MH, Schiffman M. Interobserver reproducibility of cervical cytologic and histologic interpretations: realistic estimates from the ASCUS-LSIL Triage Study. JAMA 2001;285:1500–5. [DOI] [PubMed] [Google Scholar]
- 66.Cox JT, Schiffman M, Solomon D. Prospective follow-up suggests similar risk of subsequent cervical intraepithelial neoplasia grade 2 or 3 among women with cervical intraepithelial neoplasia grade 1 or negative colposcopy and directed biopsy. Am J Obstet Gynecol 2003;188:1406–12. [DOI] [PubMed] [Google Scholar]
- 67.Tainio K, Athanasiou A, Tikkinen KAO, Aaltonen R, Cardenas J, Hernandes, Glazer-Livson S, Jakobsson M, Joronen K, Kiviharju M, Louvanto K, Oksjoki S, Tahtinen R, Virtanen S, Nieminen P, Kyrgiou M, Kalliala I. Clinical course of untreated cervical intraepithelial neoplasia grade 2 under active surveillance: systematic review and meta-analysis. BMJ 2018;360:k499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Castle PE, Adcock R, Cuzick J, Wentzensen N, Torrez-Martinez NE, Torres SM, Stoler MH, Ronnett BM, Joste NE, Darragh TM, Gravitt PE, Schiffman M, Hunt WC, Kinney WK, Wheeler CM. Relationships of p16 Immunohistochemistry and Other Biomarkers With Diagnoses of Cervical Abnormalities: Implications for LAST Terminology. Arch Pathol Lab Med 2020;144:725–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith JS, Lindsay L, Hoots B, Keys J, Franceschi S, Winer R, Clifford GM. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer 2007;121:621–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.