Abstract
Background: Phalanx fractures are common, and plate fixation can be used to treat difficult fractures. Major complications have been reported in up to 64% of phalanx fractures treated with plate fixation, with stiffness being the most common. Low-profile anatomic plates (LPAP) have been designed to decrease soft tissue irritation and postoperative stiffness. The objective of this study was to determine whether the use of LPAP has decreased complications in plate fixation of phalanx fractures. Methods: A retrospective chart review was performed of patients with phalanx fractures treated with open reduction and internal fixation (ORIF) using LPAP at a single institution from January 1, 2010, to January 25, 2018. Twenty-three patients with 23 phalanx fractures treated with LPAP were included. The primary outcome was the presence of a complication. Results: Of the 23 patients, 12 patients (52.2%) had a postoperative complication. Nine patients (39.1%) required return to the operating room, with 7 (30.4%) returning for removal of hardware and tenolysis/capsulotomy. Two patients (8.7%) had superficial infections, one requiring irrigation and debridement. The other infection resolved clinically after 2 courses of oral antibiotics, with the fracture going on to nonunion. One patient had delayed wound healing treated prophylactically with cephalexin; although the wound healed, the patient developed a boutonniere deformity requiring surgery. There were 2 malunions (8.7%), one requiring revision surgery and the other electing for nonoperative management. All but one fracture progressed to union. Conclusions: ORIF with LPAP consistently achieves fracture union for phalanx fractures, but it does not appear that LPAP reduce the high complication rate.
Keywords: phalanx, fracture, complications, plate, low-profile, open reduction internal fixation, finger, fracture/dislocation, diagnosis
Introduction
Phalanx fractures are the second most common upper extremity fracture, accounting for approximately 23% of fractures of the upper limb. These injuries are more common in men and have a bimodal age distribution.1 Many phalanx fractures can be successfully treated nonoperatively, but if it is not possible to immobilize the fracture in acceptable alignment, operative fixation may be required. Operative treatment options include closed reduction and percutaneous fixation with pins or screws and open reduction and internal fixation (ORIF) with pins, screws, plates, or a combination. There is controversy regarding optimal treatment for different fracture patterns.2 Due to the theoretical advantage of precise alignment and stable fixation, allowing early postoperative range of motion (ROM), plate fixation is often used to treat unstable or comminuted fractures. However, major complications have been reported in up to 64% of phalanx fractures treated with plate fixation. Complications include stiffness, complex regional pain syndrome (CRPS), infection, delayed union, nonunion, malunion, and plate loosening, with stiffness being the most common.3,4
Low-profile anatomic plates (LPAP) have been designed to require less soft tissue dissection and decrease soft tissue irritation, and have been shown to have similar construct stiffness and strength compared with the more traditional 2.7-mm dynamic compression plate (DCP) plating system in a metacarpal fracture model.5 A biomechanical study by Shanmugam et al6 demonstrated that laterally placed low-profile phalanx plates have similar construct stiffness and load to failure as laterally and dorsally placed traditional phalanx plates; however, they did not test dorsally placed LPAP. The LPAP should allow anatomic reduction and stable fixation, allowing early ROM, while decreasing soft tissue dissection and postoperative irritation. Theoretically, this should decrease complications such as stiffness, infection, and CRPS. However, there are no studies to date demonstrating a decreased incidence of complications with LPAP compared with traditional plates in the treatment of phalanx fractures.7 The objective of this study was to determine whether the use of LPAP has decreased complications in plate fixation of phalanx fractures as compared with historical data of earlier generation plates.
Materials and Methods
A retrospective chart review was performed, after institutional review board approval, on patients who had undergone ORIF with LPAP by 3 fellowship-trained hand surgeons at a single academic institution (S.K.M., D.S.R., M.J.R., Duke University Health System) over an 8-year period. All patients with Current Procedural Terminology codes 26765 (open treatment of distal phalangeal fracture, finger or thumb, with or without internal or external fixation, each) or 26735 (open treatment of phalangeal shaft fracture, proximal or middle phalanx, finger or thumb, with or without internal or external fixation, each) were searched using an institutional query tool, and their charts were reviewed for use of LPAP using operative reports and radiographs.
Inclusion criteria consisted of all patients with a preoperative diagnosis of a phalanx fracture in which acceptable reduction could not be maintained with closed treatment and who had undergone ORIF of the phalanx fracture with LPAP. Exclusion criteria included concomitant same finger metacarpal or phalanx fracture, previous fracture to the same phalanx, or prior surgery on the operative digit. Patients with concomitant tendon injury, rheumatoid arthritis, or similar condition compromising soft tissue integrity were also excluded. Patients with follow-up less than 1 month were excluded.
Electronic medical records were reviewed, and data were collected on patient demographics, comorbidities, hand dominance, mechanism, prior injuries, and concomitant injuries. Radiographs and operative reports were reviewed extracting injury characteristics, surgical technique, and implants used. Postoperative clinical and radiographic data were reviewed, including ROM, radiographic union, infection, return to the operating room, and other complications. The presence of a complication was the primary outcome, including superficial or deep infection, delayed wound healing, delayed union (no evidence of fracture consolidation at 3 months), nonunion (no bony union at 6 months), malunion, total active flexion (TAF) <180° or extensor lag >35° at 3-month or final follow-up, or return to the operating room.
Several different brands of plate were used. Plates from the Synthes modular hand set (DePuy Synthes, West Chester, Pennsylvania) were used in 11 patients, with 1.3-mm plates used in 8 patients, 1.5-mm plates in 2 patients, and a 2-mm plate in 1 patient. Six patients received 0.8-mm plates from the Acumed Hand Fracture System (Acumed, Hillsboro, Oregon). Three patients received plates from the Medartis Aptus 1.2/1.5 plate system (Medartis, Basel, Switzerland). Two patients received 1.7-mm plates from the Stryker Hand Plating System (Stryker, Kalamazoo, Michigan). One patient received a 0.8-mm plate from the KLS Martin Hand Fracture System (KLS Martin Tuttlingen, Germany). Allograft bone was used in 11 of the 23 fractures.
Results
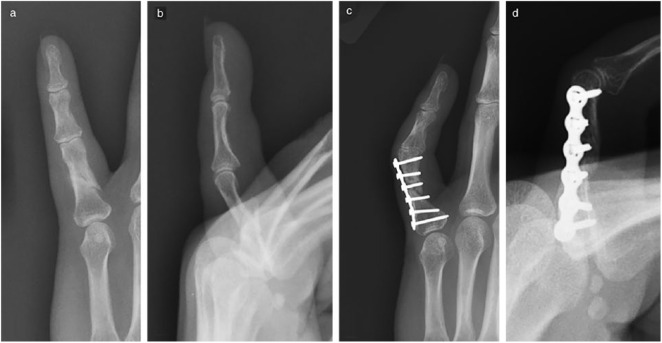
Twenty-three patients with 23 phalanx fractures treated with ORIF using LPAP were included for analysis. One patient had an additional phalanx fracture on another digit of the ipsilateral hand, which was considered stable and treated nonoperatively. Sixteen men and 7 women were included, with a mean age of 42.1 (range = 20-71) years. There were 7 fractures of the small finger, 10 ring, 2 long, 3 index, and 1 of the thumb. Eight proximal phalanx and 15 middle phalanx fractures were included. Twenty-two of the fractures were considered low-energy mechanism, and 1 fracture sustained in a motor vehicle collision was considered high energy. Eighteen of the 23 fractures were comminuted, 4 spiral or oblique, and 1 volar shear; 18 of the 23 fractures were intra-articular (Figure 1). Eleven fractures were plated on the volar surface, 6 lateral (radial or ulnar), and 6 dorsal.
Figure 1.
Preoperative (a) posteroanterior (PA) and (b) lateral, and 2-month postoperative (c) PA and (d) lateral radiographs of a comminuted intra-articular small finger proximal phalanx fracture treated with a low-profile anatomic plate.
Twelve (52.2%) of the 23 patients had a postoperative complication. There were no intraoperative complications. Nine patients (39.1%) required return to the operating room, with 7 (30.4%) returning for removal of hardware and tenolysis/capsulotomy to improve ROM. Two patients had superficial infections, with one requiring operative irrigation and debridement; the other infection resolved clinically after 2 courses of oral antibiotics, but the fracture progressed to nonunion, for which the patient elected for nonoperative management (Figure 2). There was one patient with delayed wound healing treated prophylactically with cephalexin; although the wound healed, the patient later developed a boutonniere deformity requiring surgery. There were 2 malunions, one requiring revision to hemi-hamate arthroplasty and the other electing for nonoperative management. All but one fracture showed signs of bony union at final follow-up.
Figure 2.
Preoperative (a) posteroanterior (PA) and (b) lateral, and 11-month postoperative (c) PA and (d) lateral radiographs of a small finger proximal phalanx fracture treated with a low-profile anatomic plate resulting in a nonunion.
Seven (63.6%) of the 11 patients with a volar plate experienced a complication, compared with 3 (50%) of the 6 patients with a lateral plate and 2 (33.3%) of the 6 patients with a dorsal plate (P = .523). Nine (50%) of the 18 patients with intra-articular fractures experienced complications, compared with 3 (60%) of the 5 patients with extra-articular fractures experiencing complications (P = .708). Nine (50%) of the 18 patients with comminuted fractures experienced complications, compared with 3 (60%) of the 5 patients with simple fracture patterns experiencing complications (P = .708). Eight (72.7%) of the 11 patients with Synthes plates experienced complications; the patient with a 2.0-mm plate and each of the 2 patients with 1.5-mm plates experienced complications, compared with 5 (62.5%) of the 8 patients with 1.3-mm Synthes plates experiencing complications. Two (33.3%) of the 6 patients treated with Acumed 0.8-mm plates experienced complications. One (33.3%) of the 3 patients treated with plates from the Medartis 1.2/1.5 system experienced complications. One (50%) of the 2 patients treated with Stryker 1.7-mm plates experienced complications. The one patient treated with a 0.8-mm KLS Martin plate did not experience a complication. The 72.7% complication rate in the Synthes group compared with the 33.3% complication rate in the remaining patients combined (Acumed, Medartis, Stryker, and KLS Martin) did not meet significance (P = .063).
The 11 patients treated with volar plates had sustained intra-articular fractures of the base of P2 with subluxation or dislocation of the proximal interphalangeal (PIP) joint, a fracture pattern traditionally associated with poor clinical results. These patients were treated with a volar transverse plate or T plate. Those patients treated with a volar transverse plate, termed the seatbelt procedure, have been reported upon in a previous study.8
At a mean final follow-up of 7.6 months (range = 1-28), the mean TAF was 187°. The mean extensor lag was 27.4°. Of the 20 patients with extensor lag measured at final follow-up, 5 (25%) had extensor lag greater than 35°. Of the 18 patients with final TAF measurement, 6 (33.3%) had TAF less than 180°.
Discussion
The high postoperative complication rate demonstrated in this study is similar to previous complication rates reported in the literature after ORIF of phalanx fractures using a plate and screws.3,4,7,9-12 Previous studies present data for different fracture types, and each defines complications differently, making results difficult to compare directly.
In the only study directly comparing LPAP with traditional plates, Agarwal and Pickford7 found no significant differences in ROM or complications in a combined group of metacarpal and phalanx fractures from 2002 to 2004. Kurzen et al reviewed 64 unstable or comminuted phalanx fractures treated with ORIF using plates between 1991 and 2002, and they reported that 31 (57%) of the 54 patients and 33 (52%) of the 64 fractures experienced a complication.4 Brei-Thoma et al reviewed 32 patients with 36 extra-articular proximal phalanx fractures treated with mini-fragment plate systems from 2006 to 2012. Despite treating only extra-articular proximal phalanx fractures, 14 (43.8%) of the 32 patients required additional surgery.9 Ouellette et al reviewed 53 patients with 68 hand fractures, including metacarpal and phalanx fractures, treated with minicondylar plates from 1986 to 1989. Complication data were available for 51 patients, with 65 fractures, and they reported that 29 patients (56.9%) experienced a complication.10 Page and Stern reviewed 82 patients with 105 metacarpal and/or phalanx fractures stabilized with plates from 1988 to 1996; they reported at least one complication in 36 (92%) of the 39 phalanx fractures and a major complication in 25 (64%) of the 39 phalanx fractures.3 Berman et al reviewed 16 phalanx fractures treated with titanium miniplates from 1991 to 1998; they reported complications in 4 (25%) of the 16 fractures. Of note, all patients were taken to the operating room within 8 hours of arrival to the emergency department, and complications were not clearly defined.11
There are multiple studies comparing plate and screw fixation with other forms of fixation with mixed results. Basar et al compared treatment of spiral oblique metacarpal and proximal phalanx fractures treated with screw only or mini plate and screw. They found significantly quicker return to work in patients treated with mini plate plus screw in both groups. For proximal phalanx fractures, they found significantly greater total ROM and the shortened version of the Disabilities of the Arm, Shoulder and Hand Questionnaire (QuickDASH) scores in the screw-only group.13 However, regarding the QuickDASH score, the previously established minimally important difference of 11 points was not met.14 Pun et al reviewed 53 proximal or middle phalanx fractures treated with ORIF with screw or plate and screw fixation; they saw a trend toward improved results using screw fixation compared with plate and screws, but it did not meet statistical significance. They also compared results of ORIF from this study with the previously reported group of patients with the same indications treated with K-wire fixation and found no significant difference in results, although it is unclear whether this comparison is adequately controlled or powered.15,16
Placement of phalanx plate dorsally versus laterally has been studied with conflicting results. Onishi et al17 reviewed 70 patients with 75 proximal phalanx fractures treated with ORIF with titanium plates and/or screws, and they found plate fixation and dorsal placement of the plate to be independent risk factors for finger stiffness. However, Robinson et al12 did not find a significant difference in outcomes, complication, or revision rate when comparing dorsal versus lateral plating in 42 proximal phalanx fractures. In our study, 7 (63.6%) of the 11 patients with a volar plate experienced a complication, compared with 3 (50.0%) of the 6 patients with a lateral plate and 2 (33.3%) of the 6 patients with a dorsal plate. The 11 patients treated with volar plates had sustained intra-articular fractures of the base of P2 with subluxation or dislocation of the PIP joint, a fracture pattern traditionally associated with poor clinical results. If we were to exclude this group, the complication rate was 42%, which still falls within the previously reported range of complications in both traditional and low-profile plates.
The argument could be made that return to the operating room for removal of hardware and tenolysis/capsulotomy is expected in ORIF of phalanx fractures with plate fixation and should not be considered a complication. If this was not considered a complication, 9 (39%) of the 23 patients had other complications, which still falls within the previously reported range of complications. Of the dorsally and laterally placed plates, 3 (25%) of the 12 patients experienced complications if excluding return to the operating room as a complication.
A systematic review of the literature on treatment of extra-articular proximal and middle phalanx fractures of the hand was performed by Verver et al. They concluded that when ORIF is required for extra-articular spiral or oblique fractures, lag screw fixation is preferable to plate and screw fixation, and transverse K-wires provide similar recovery and function as lag screws in that situation.2
There are limitations to this study. It is a retrospective review of patients and is subject to the inherent limitations of this study format. This study compares patients with historical controls, which is limited in that indications may have changed over time, that is, comparing with different patient populations and surgeons. Given the short-term follow-up, assumptions cannot be made regarding medium- or long-term complication rates.
Conclusions
The ORIF of phalanx fractures with plate and screw fixation reliably achieves union, but it carries a high complication and reoperation rate. Low-profile anatomic plates have been designed to decrease soft tissue dissection and irritation, while maintaining construct stiffness, in hopes of decreasing complications. Compared with historical controls, it does not appear that LPAP have significantly decreased the complication rate in plate fixation of phalanx fractures. Given the high complication rate of phalanx plates, the authors reserve plate fixation only for fractures that cannot be fixed with appropriate stability by other methods. If treating a phalanx fracture with a plate, patients should be appropriately counseled on the high complication rate and likelihood of return to the operating room for removal of hardware and tenolysis/capsulotomy.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: No experiments on animals were performed for this study. No experimental procedures were performed on any human subject for this study.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.J.R. declares association or financial involvement as a consultant for Acumed, Depuy Synthes, and Medartis. D.S.R. declares association or financial involvement as a consultant for Acumed.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Evan M. Guerrero  https://orcid.org/0000-0001-7942-2529
https://orcid.org/0000-0001-7942-2529
References
- 1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908-915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2. Verver D, Timmermans L, Klaassen RA, et al. Treatment of extra-articular proximal and middle phalangeal fractures of the hand: a systematic review. Strategies Trauma Limb Reconstr. 2017;12(2):63-76. doi: 10.1007/s11751-017-0279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(5):827-832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 4. Kurzen P, Fusetti C, Bonaccio M, et al. Complications after plate fixation of phalangeal fractures. J Trauma. 2006;60(4):841-843. doi: 10.1097/01.ta.0000214887.31745.c4. [DOI] [PubMed] [Google Scholar]
- 5. Fischer KJ, Bastidas JA, Provenzano DA, et al. Low-profile versus conventional metacarpal plating systems: a comparison of construct stiffness and strength. J Hand Surg Am. 1999;24(5):928-934. doi: 10.1053/jhsu.1999.0928. [DOI] [PubMed] [Google Scholar]
- 6. Shanmugam R, Ernst M, Stoffel K, et al. Angular stable lateral plating is a valid alternative to conventional plate fixation in the proximal phalanx. Clin Biomech (Bristol, Avon). 2015;30(5):405-410. doi: 10.1016/j.clinbiomech.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 7. Agarwal AK, Pickford MA. Experience with a new ultralow-profile osteosynthesis system for fractures of the metacarpals and phalanges. Ann Plast Surg. 2006;57(2):206-212. doi: 10.1097/01.sap.0000215925.58902.bc. [DOI] [PubMed] [Google Scholar]
- 8. Federer A, Guerrero E, Dekker T, et al. Open reduction internal fixation with transverse volar plating for unstable proximal interphalangeal fracture-dislocation: the seatbelt procedure [published online ahead of print July 28, 2018]. Hand (N Y). doi: 10.1177/1558944718790063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brei-Thoma P, Vögelin E, Franz T. Plate fixation of extra-articular fractures of the proximal phalanx: do new implants cause less problems. Arch Orthop Trauma Surg. 2015;135(3):439-445. doi: 10.1007/s00402-015-2155-4. [DOI] [PubMed] [Google Scholar]
- 10. Ouellette EA, Freeland AE. Use of the minicondylar plate in metacarpal and phalangeal fractures. Clin Orthop Relat Res. 1996;327:38-46. doi: 10.1097/00003086-199606000-00007. [DOI] [PubMed] [Google Scholar]
- 11. Berman KS, Rothkopf DM, Shufflebarger JV, et al. Internal fixation of phalangeal fractures using titanium miniplates. Ann Plast Surg. 1999;42(4):408-410. doi: 10.1097/00000637-199904000-00010. [DOI] [PubMed] [Google Scholar]
- 12. Robinson LP, Gaspar MP, Strohl AB, et al. Dorsal versus lateral plate fixation of finger proximal phalangeal fractures: a retrospective study. Arch Orthop Trauma Surg. 2017;137(4):567-572. doi: 10.1007/s00402-017-2650-x. [DOI] [PubMed] [Google Scholar]
- 13. Başar H, Başar B, Başçı O, et al. Comparison of treatment of oblique and spiral metacarpal and phalangeal fractures with mini plate plus screw or screw only. Arch Orthop Trauma Surg. 2015;135(4):499-504. doi: 10.1007/s00402-015-2164-3. [DOI] [PubMed] [Google Scholar]
- 14. Polson K, Reid D, McNair PJ, et al. Responsiveness, minimal importance difference and minimal detectable change scores of the shortened disability arm shoulder hand (QuickDASH) questionnaire. Man Ther. 2010;15(4):404-407. doi: 10.1016/j.math.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 15. Pun W, Chow S, So Y, et al. Unstable phalangeal fractures: treatment by A.O. screw and plate fixation. J Hand Surg Am. 1991;16(1):113-117. [DOI] [PubMed] [Google Scholar]
- 16. Pun W, Chow S, So Y, et al. A prospective study on 284 digital fractures of the hand. J Hand Surg Am. 1989;14(3):474-481. [DOI] [PubMed] [Google Scholar]
- 17. Onishi T, Omokawa S, Shimizu T, et al. Predictors of postoperative finger stiffness in unstable proximal phalangeal fractures. Plast Reconstr Surg Glob Open. 2015;3(6):e431. doi: 10.1097/GOX.0000000000000396. [DOI] [PMC free article] [PubMed] [Google Scholar]