Abstract
Emerging evidence suggests substantial overlap between the symptoms of Meniere’s disease (MD) and migraine-related cochlear/vestibular disorders. We report a 5-year-old girl with a 6-month history of left-sided hearing loss followed by daily episodes of vertigo, headache, and vomiting who met the criteria for definite MD. The patient became symptom-free and gained near normal hearing levels after starting on a 6-week migraine diet/lifestyle regimen with riboflavin and magnesium. We believe that the symptoms of MD may be primarily due to a vestibular migraine phenomenon. Pediatric MD patients may benefit from migraine lifestyle/dietary changes with control of both cochlear and vestibular symptoms.
Keywords: Meniere’s disease, vestibular migraine, cochlear migraine, pediatric, lifestyle change
1. Introduction
Meniere’s disease (MD) is a disorder of middle-aged individuals with a mean onset age of 40-50 years and rarely affects the pediatric age group, accounting for 1.5-3% of cases [1-4]. Emerging evidence suggests substantial overlap between the symptoms of vestibular migraine (VM) and those of MD [5, 6]. The presence of sensorineural hearing loss (SNHL) has notably been suggested to be the distinguishing factor between MD and VM, highlighting the previously held and popular notion that migraine will seldom have a negative impact on the auditory pathways and generate cochlear symptoms, such as hearing loss and tinnitus [7]. This notion has been questioned recently, with population-based evidences showing that migraine not only can contribute to the generation of auditory symptoms but also is a risk factor for sudden SNHL [8, 9]. Here, we describe a child with definite MD according to the American Academy of Otolaryngology – Head and Neck Surgery (AAO-HNS) criteria whose complaints including SNHL disappeared with migraine lifestyle/dietary changes.
2. Case Report
A 5-year-old girl was referred to our tertiary neurotology clinic for evaluation of a 6-month left-sided hearing loss followed by recurrent attacks of vertigo, headache, and vomiting. During her course of illness, she mostly had 3-hour episodes of vertigo but also had some short-lasting episodes (20 minutes) with increased frequency and duration over time along with hearing loss (Figure 1) and tinnitus in her left ear. Her parents noticed that several of her worst episodes occurred after birthday parties or overstimulation at Disneyland. Microscopic ear examination was normal on all occasions and retrocochlear or cochleovestibular abnormalities were ruled out using MRI and CT scans of the temporal bone. She had a normal past medical and developmental history and her mother had a history of migraine headaches.
Figure 1.
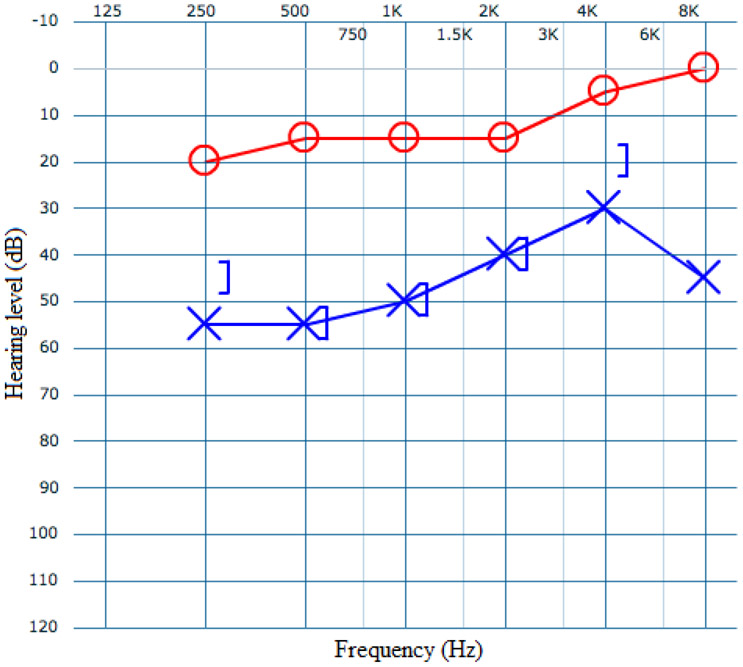
Pre-treatment audiogram of left (X) and right (O) ears showing left-sided hearing loss which was a consistent finding for 6 months.
The parents were given instructions on migraine lifestyle changes (preventing dehydration, eating three meals per day, and sleeping on the same schedule on weekends and weekdays) including a detailed diet list. The diet included avoiding certain foods such as certain preservatives, frozen, canned, or pre-packaged foods such as chips (high monosodium glutamate), fermented products (e.g., cheese, etc.), chocolate, nuts, egg white, fresh breads/yeast products, aged/processed meats, certain beans, certain fruits (high histamine/tyramine), and pickled or preserved fruits/vegetables. We did not restrict sodium intake as long as the patient stayed well-hydrated. We also recommended vitamin B2 (riboflavin) 100 mg bid and magnesium 200 mg bid to help with migraine prevention. We did not start migraine prophylactic medication at that time. We asked the parents to have the child avoid activities that provide excessive stimulation for six weeks, such as birthday parties and amusement parks.
On her follow-up visit after 6 weeks, she had a near normal audiogram (Figure 2) without experiencing any of her previous symptoms. She was asymptomatic after 3 months of follow up with no vertigo episodes since starting the migraine dietary and lifestyle changes as well as the supplements. The patient was weaned off the supplements and maintained her hearing and was free of vertigo at 4 months. The parents were asked to follow the migraine diet and lifestyle changes.
Figure 2.
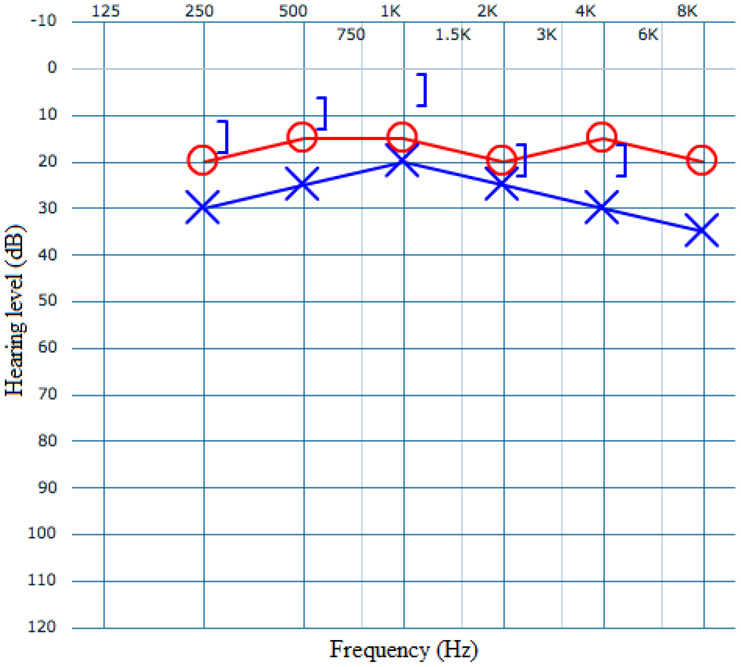
Audiogram of left (X) and right (O) ears after 6 weeks of being on the migraine regimen.
3. Discussion
MD is diagnosed based on the presence of vertigo, tinnitus, and hearing loss according to the AAO-HNS criteria [10]. However, these criteria do not include a fourth symptom described in Meniere’s original writing, migraine headaches [11]. Meniere proposed a common etiology between migraine headaches and the symptomatic triad of MD. His observations allowed him to deduce that migraine headaches were a unique symptom present in parallel with, but not consequential to, the triad of MD symptoms [11]. It has been shown that migraine occurs more often in patients with MD than in the general population and that the classical symptoms of MD and migraine might be related [12, 13].
Despite the clear distinction between MD and VM according to their different diagnostic criteria, much overlap exists between these two diseases. For example, similar to MD, some cases of VM can also present with reduced cochlear function and fluctuating vertigo that can last from minutes to hours [14, 15]. However, this diagnostic overlap can vary over different patient demographics. For instance, sensitivity to noise and light is commonly associated with both VM and MD in adults. In children, however, sensitivity to noise and light forms a diagnostic criterion for VM, but not MD [5, 14, 16]. Additionally, while VM has been found to be more common than MD among the pediatric population [17], the presence of low-frequency hearing loss, as found in the patient, serves as a reliable differentiating feature of MD [14].
VM has been shown to present without any headache symptoms in 30% of cases [18]. Moreover, it has recently been shown that 51% of MD patients also suffered from migraine headaches [5]. To solve this discrepancy between these two terms, Lai and Liu have recently introduced the new concept of cochlear migraine [19]. Further, Hwang et al. [8] supported this concept in a large-scale cohort study. They showed that the cumulative incidence of cochlear symptoms, defined as tinnitus, SNHL, and/or sudden deafness was significantly higher in patients with history of migraine headaches than those without a migraine history [8]. This provides further evidence suggesting that there is a link between migraine and peripheral/central auditory dysfunction [20, 21].
Migraine and cochlear disorders might share common pathophysiologic characteristics. A proposed possible mechanism for migraine-related cochlear (i.e., episodic hearing loss) and vestibular (balance) symptoms is compromised blood flow to the inner ear and to the brain as a result of vasospasm of the branches of the posterior cerebral circulation as well as possibly trigeminal neurogenic inflammation [6]. There is clearly a significant overlap between VM, MD, and cochlear migraine which may suggest that the three conditions may be variants of each other. As such, the therapeutic effects of lifestyle and dietary changes for VM [14, 22] could be similarly beneficial for MD. Different treatment modalities have been used so far for pediatric MD [1] but to our knowledge migraine lifestyle/dietary change have never been used as the main and first option to treat this condition.
We have already theorized that MD is most likely a variant of VM and the symptoms are a consequence of a migraine etiology and not an intrinsic inner ear disorder [5]. We hypothesize that involvement of a combination of the anterior vestibular artery, vestibulocochlear artery, its individual branches, and the spiral modiolar arteries are affected. We recommend all patients including pediatric ones with MD with or without migraine headaches or VM based on International Headache Society criteria should be treated with migraine lifestyle/dietary and migraine prophylactic agents prior to surgical or destructive intratympanic therapy. This report sheds new light on the intriguing linkage between MD and vestibular/cochlear migraine and the way we can approach to treat these entities.
This paper is limited due to the single case report and the relatively short follow-up. It could be stated that the disease may have naturally gone into remission. However, the patient was having daily symptoms prior to seeing us and had been treated with a low-sodium diet as well without success. There was an immediate improvement in symptoms upon starting the supplements and the migraine diet and lifestyle regimen with complete disappearance of the vertigo and restoration of hearing. We have seen this type of dramatic improvement in 92% of our adult MD patients treated with the migraine regimen and prophylactic therapy [23] and believe that these results are far more likely than spontaneous remission. Larger prospective studies would help further characterize the existing link between MD and migraine-related cochlear/vestibular disorders but awareness of the blurred line between these conditions might be helpful in clinical diagnosis and treatment.
4. Conclusion
We found that a pediatric patient with definite MD responded completely to migraine dietary and lifestyle changes as well as magnesium and riboflavin supplementation. Definite MD patients may benefit from migraine lifestyle/dietary changes with control of both cochlear and vestibular symptoms.
Footnotes
Financial Disclosure: None
Conflict of Interest: None
References
- 1.Wang C, Wu CH, Cheng PW, Young YH. Pediatric Meniere’s disease. Int J Pediatr Otolaryngol 2018; 105: 16–9. [DOI] [PubMed] [Google Scholar]
- 2.Hausler R, Toupet M, Guidetti G, Basseres F, Montandon P. Menière's disease in children. Am J Otolaryngol 1987; 8(4): 187–93. [DOI] [PubMed] [Google Scholar]
- 3.Akagi H, Yuen K, Maeda Y, Fukushima K, Kariya S, Orita Y, et al. Ménière's disease in childhood. Int J Pediatr Otorhinolaryngol 2001; 61(3): 259–64. [DOI] [PubMed] [Google Scholar]
- 4.Meyerhoff WL, Paparella MM, Shea D. Ménière’s disease in children. Laryngoscope 1978; 88(9 Pt 1): 1504–11. [DOI] [PubMed] [Google Scholar]
- 5.Ghavami Y, Mahboubi H, Yau AY, Maducdoc M, Djalilian HR. Migraine features in patients with Meniere’s disease. Laryngoscope 2016; 126(1): 163–8. [DOI] [PubMed] [Google Scholar]
- 6.Lin HW, Djalilian HR. The role of migraine in hearing and balance symptoms. JAMA Otolaryngol Head Neck Surg 2018; 144(8): 717–8. [DOI] [PubMed] [Google Scholar]
- 7.Battista RA. Audiometric findings of patients with migraine-associated dizziness. Otol Neurotol 2004; 25(6): 987–92. [DOI] [PubMed] [Google Scholar]
- 8.Hwang JH, Tsai SJ, Liu TC, Chen YC, Lai JT. Association of tinnitus and other cochlear disorders with a history of migraines. JAMA Otolaryngol Head Neck Surg 2018; 144(8): 712–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chu CH, Liu CJ, Fuh JL, Shiao AS, Chen TJ, Wang SJ. Migraine is a risk factor for sudden sensorineural hearing loss: a nationwide population-based study. Cephalagia 2013; 33(2): 80–6. [DOI] [PubMed] [Google Scholar]
- 10.Committee on Hearing, Equilibrium Guidelines for the Diagnosis, Evaluation of Therapy in Meniere’s Disease. American Academy of Otolaryngology-Head and Neck Foundation, Inc. Otolaryngol Head Neck Surg 1995; 113(3): 181–5. [DOI] [PubMed] [Google Scholar]
- 11.Moshtaghi O, Sahyouni R, Lin HW, Ghavami Y, Djalilian HR. A Historical Recount: Discovering Meniere’s Disease and Its Association with Migraine Headaches. Otol Neurotol 2016; 37(8): 1199–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker W Meniere’s disease. Etiologic considerations. Arch Otolaryngol Head Neck Surg 1995; 121(4): 377–82. [DOI] [PubMed] [Google Scholar]
- 13.Minor LB, Schessel DA, Carey JP. Meniere’s disease. Curr Opin Neurol 2004; 17(1): 9–16. [DOI] [PubMed] [Google Scholar]
- 14.Dieterich M, Obermann M, Celebisoy N. Vestibular migraine: the most frequent entity of episodic vertigo. J Neurol 2016; 263(Suppl 1): S82–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radtke A, von Brevern M, Neuhauser H, Hottenrott T, Lempert T. Vestibular migraine: long-term follow-up of clinical symptoms and vestibulo-cochlear findings. Neurology 2012; 79(15): 1607–14. [DOI] [PubMed] [Google Scholar]
- 16.Jahn K, Langhagen T, Schroeder AS, Heinen F. Vertigo and dizziness in childhood - update on diagnosis and treatment. Neuropediatrics 2011; 42(4): 129–34. [DOI] [PubMed] [Google Scholar]
- 17.Weisleder P, Fife TD. Dizziness and headache: a common association in children and adolescents. J Child Neurol 2001; 16(10): 727–30. [DOI] [PubMed] [Google Scholar]
- 18.Strupp M, Versino M, Brandt T. Vestibular migraine. Handb Clin Neurol 2010; 97: 755–71. [DOI] [PubMed] [Google Scholar]
- 19.Lai JT, Liu TC. Proposal for a new diagnosis for cochlear migraine. JAMA Otolaryngol Head Neck Surg 2018; 144(3): 185–6. [DOI] [PubMed] [Google Scholar]
- 20.Joffily L, de Melo Tavares de Lima MA, Vincent MB, Frota SM. Assessment of otoacoustic emission suppression in women with migraine and phonophobia. Neurol Sci 2016; 37(5): 703–9. [DOI] [PubMed] [Google Scholar]
- 21.Agessi LM, Villa TR, Carvalho DS, Pereira LD. Auditory processing in children with migraine: a controlled study. Neuropediatrics 2017; 48(2): 123–6. [DOI] [PubMed] [Google Scholar]
- 22.Devaraja K Vertigo in children; a narrative review of the various causes and their management. Int J Pediatr Otorhinolaryngol 2018; 111: 32–8. [DOI] [PubMed] [Google Scholar]
- 23.Ghavami Y, Haidar YM, Moshtaghi O, Lin HW, Djalilian HR. Evaluating Quality of Life in Patients with Meniere’s Disease Treated as Migraine. Ann Otol Rhinol Laryngol 2018; 127(12): 877–87. [DOI] [PubMed] [Google Scholar]


