Abstract
Ligamentous wrist injuries are common occurrences that require complex anatomical mastery and extensive understanding of diagnostic and treatment modalities. The purpose of this educational review article is to delve into the most clinically relevant wrist ligaments in an organized manner to provide the reader with an overview of relevant anatomy, function, clinical examination findings, imaging modalities, and options for management. Emphasis is placed on elucidating reported diagnostic accuracies and treatment outcomes to encourage evidence-based practice.
Keywords: wrist ligaments, wrist injuries, wrist ligament anatomy, diagnostic modalities
Introduction
Injuries to wrist ligaments are common occurrences, with causes ranging from acute occupational or sports accidents to chronic injury due to joint overuse or repetitive trauma. However, the anatomical complexity of ligamentous structures of the wrist can complicate the diagnosis and treatment of these injuries. The wrist is not a single joint, but a complex of 20 joints with different levels of mobility, which are held together by a complex of ligaments. Although existing articles provide in-depth reviews of injury patterns, diagnosis, and treatment for specific ligaments or groups of like ligaments, 1 2 progress is being made and new data are accrued. Additionally, there is a paucity of literature providing a concise yet thorough review that addresses the scope of clinically relevant wrist ligament injuries with evidence-based discussion of current diagnostic and treatment modalities. Thus, the authors present this review detailing anatomical considerations, functional implications, common injuries, evidence-based diagnostic modalities, and surgical management of the most clinically relevant wrist ligament injuries.
Extrinsic Carpal Ligaments
The extrinsic carpal ligaments connect the forearm to the carpus and are contained inside the joint. They can be divided into palmar, dorsal, radiocarpal, and ulnocarpal. The primary palmar radiocarpal extrinsic ligaments are: radioscaphocapitate (RSC), long radiolunate (LRL), and short radiolunate (SRL) ligaments. The palmar ulnocarpal ligaments are the superficial ulnocapitate and the deeper ulnolunate and ulnotriquetral ligaments. There is one primary dorsal extrinsic ligament—the dorsal radiocarpal (DRC) ligament. No dorsal ligaments connect the ulna and carpus ( Figs. 1 2 ).
Fig. 1.
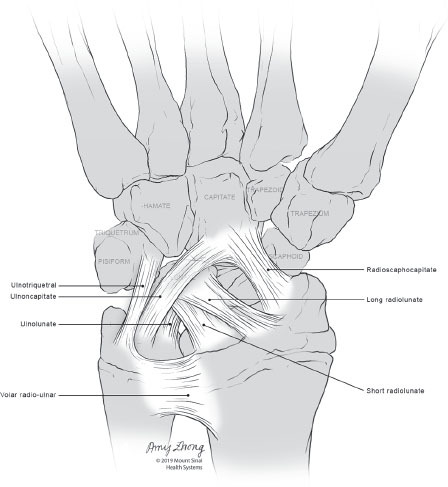
Volar wrist ligaments.
Fig. 2.
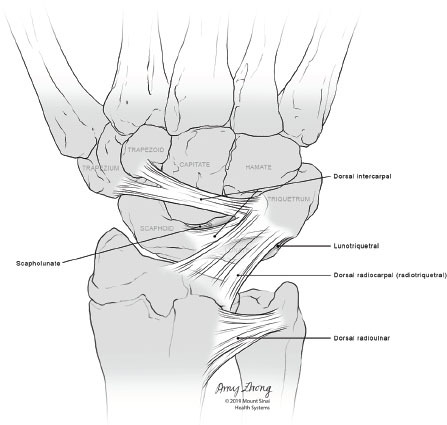
Dorsal wrist ligaments.
Palmar Extrinsic Ligaments
The RSC ligament is the most superficial and radial of the extrinsic palmar ligaments. It is an oblique ligament that originates from the anterolateral margin of radius and runs across the waist of the scaphoid to insert onto the palmar aspect of the capitate, forming a sling over which the scaphoid rotates. 3 4 5 6 Avulsion fractures of the radial styloid contain the origin of the RSC ligament, which are treated with anatomical reduction and fixation. Pure isolated midsubstance rupture of the RSC ligament is exceedingly rare. 4 Following proximal row carpectomy (PRC), the RSC ligament serves as the primary stabilizer of the wrist and must be preserved to prevent ulnar translation. 7
The LRL ligament originates ulnar to the RSC ligament at the radial styloid process and runs obliquely, attaching to the palmar aspect of the lunate to serve as the primary support of the lunate. 8 Separating the RSC and LRL ligaments is the interligamentous sulcus (“space of Poirier”), representing a weak spot through which perilunate dislocations occur. Injury to the LRL often occurs concurrently with other ligamentous injuries in severe, high-energy radiocarpal dislocations. 9
The SRL ligament is a flat thickening of the volar capsule which arises ulnar to the radioscapholunate (RSL) ligament from the anteromedial surface of the distal radius and attaches vertically to the palmar surface of the lunate. The SRL ligament plays a key role in perilunate instability, as it holds the lunate and resists extension forces. 10 11 Furthermore, rupture or attenuation of the LRL and SRL ligaments may occur with scapholunate injury. Any reconstructive effort to restore scapholunate stability must reestablish radiolunate stability (“the foundation”) or else it will fail.
Imaging of wrist injuries should first include four routine X-rays: neutral-rotation PA, lateral with arm adducted to the patient’s side, scaphoid view, and oblique in 45 degrees of pronation. MRI is generally effective for identifying extrinsic ligament trauma due to its superior soft-tissue contrast, particularly using thin slices and 3D MRI imaging techniques ( Fig. 3 ). 12 13 MR arthrography has been shown to have a low sensitivity for detection of RSC and LRL ligaments’ injuries. Ultrasonography is a promising imaging modality for injury detection in these ligaments, with the exception of the RSL ligament. 14 15 16
Fig. 3.
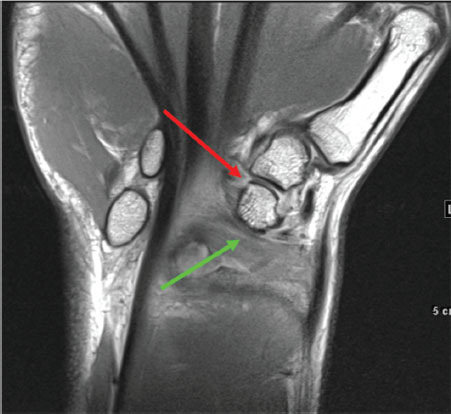
Coronal proton density MRI showing partial tear of the radioscaphocapitate (red) and long radiolunate ligaments (green) on the volar side of the wrist, as evidenced by the bright signal intensity.
Few studies report on the outcome of operative reconstruction of the volar extrinsic ligaments extending from the radius, with most reports describing reconstruction in the context of extensive carpal injury. Use of a free flexor carpi radialis tendon autograft and mini suture anchors have been described in a cadaveric model of static scapholunate dissociation involving RSC and LRL ligaments’ repair. 17 Further studies are needed to elucidate best practice in the operative management of these ligamentous injuries.
The palmar extrinsic ligaments extending from the ulna exist as an ulnocarpal ligamentous complex (UCLC), containing the ulnocapitate, ulnotriquetral, and ulnolunate ligaments ( Fig. 1 ). 18 The ulnocapitate ligament is the most superficial, 19 and it extends from the palmar portion of the ulnar fovea to the capitate to join with fibers from the RSC ligament on the radial side to create the arcuate ligament, which is shaped like an inverted V. 18 20 The ulnolunate ligament originates from the volar radioulnar ligament at its distal ulnar attachment and inserts onto the volar aspect of the lunate. 4 The ulnotriquetral ligament originates from the radioulnar ligament and attaches to the proximal and ulnar aspects of the triquetrum. 4 21 Together with the interosseous membrane, the volar and dorsal radioulnar ligaments are the primary stabilizers of the distal radioulnar joint (DRUJ), and they are important for conferring stability in the palmar and dorsal directions. 22
The ligaments contained in the UCLC play a controversial role in the stability of the ulnocarpal joint. 23 24 Since both the ulnolunate and ulnotriquetral ligaments originate from a ligament, injury or disease affecting the palmar radioulnar ligament will also result in ulnocarpal instability. This is classically seen with rheumatoid arthritis, affecting the foveal insertion, and resulting in DRUJ subluxation and ulnocarpal supination deformity.
Although rarely reported in the literature, ulnolunate injury can cause chronic wrist pain, locking and pain with grip, and be difficult to diagnose, requiring arthroscopic examination for confirmation. 25 26 The ulnotriquetral ligament is often injured through a single traumatic event, causing longitudinal splitting in the ligament due to weakness in the ligament’s longitudinal direction from vascular perforations, as well as differing vectors of force transmission due to its split origins in the triangular fibrocartilage complex (TFCC) and the ulnar styloid. 27 28 Clinical examination includes assessing the ulnar fovea sign: pain on palpation of the ulnar foveal region (in between the ulnar styloid process and flexor carpi ulnaris tendon proximal to the pisiform and distal to the ulnar head), which has a sensitivity of 95.2% and a specificity of 86.5%. 29 The diagnosis of ulnotriquetral ligament tears requires confirmation by arthroscopy, as MRI has poor sensitivity and specificity. 30 Following arthroscopic assessment of the TFCC, operative management, using an “outside-to-inside” repair, has been shown to yield significant improvement in pain and grip strength. 27 31
Dorsal Extrinsic Ligaments and the Dorsal Radioulnar Ligament
The only dorsal extrinsic ligament is the DRC ligament, otherwise known as the radiotriquetral ligament. The DRC ligament originates from the dorsal aspect of the distal radius and extends to the lunate and lunotriquetral interosseous ligament before inserting on the dorsal tubercle of the triquetrum ( Fig. 2 ). It forms a “V” configuration with the dorsal intercarpal ligament (described below) to maintain midcarpal stability, which is particularly important in scaphoid stabilization. 32 DRC ligament injuries are commonly seen concurrently with scapholunate ligament, lunotriquetral ligament, and TFCC injuries (described below), but can exist as isolated incidents. 33 34 34 35 DRC ligament injuries are challenging to identify with standard arthrography and are best viewed on coronal T1- or T2-weighted MRI images. Arthroscopic repair has yielded good results in DRC ligament injuries. 34 36 37
The dorsal radioulnar ligament (DRUL), like its volar counterpart, spans the distal radius and ulna, stabilizing the DRUJ together with the distal interosseous membrane. However, unlike the volar radioulnar ligament, the dorsal radioulnar ligament has been found to have a role in stabilizing the wrist during pronation as well as restraining against palmar displacement in supination. 22 The DRUL is further described as part of the TFCC below.
Triangular Fibrocartilage Complex
Since its description in 1981, the TFCC has been frequently imaged and treated in the context of wrist injury. This ligamentous and cartilaginous connection between the distal radius and ulna comprises multiple structures including the triangular fibrocartilage (also known as the articular disc), the DRUL and volar radioulnar ligament, and the sheath of extensor carpi ulnaris, which has questionable contribution to the TFCC. The TFCC originates from the ulnar aspect of the distal radius and inserts proximally into the base of the ulnar styloid and distally onto the hamate, triquetrum, and base of the fifth metacarpal ( Fig. 4 ). 38 Together with the interosseous membrane, the TFCC is most important for DRUJ stability as well as transmission and absorption of compressive loads.
Fig. 4.
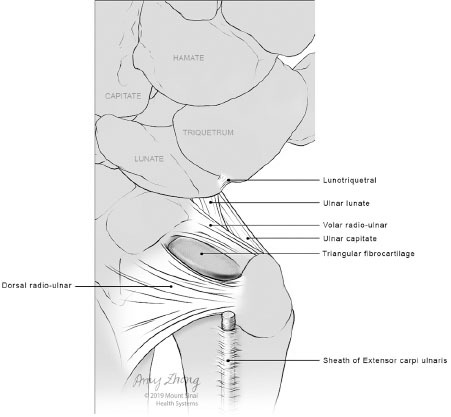
Triangular fibrocartilage complex (TFCC).
Injury to the TFCC is most commonly degenerative, with an increasing incidence with age due to repetitive pronation and supination as well as chronic stress to the ulnar aspect of the wrist. 39 40 Patients with positive ulnar variance have an increased likelihood of developing TFCC lesions as demonstrated by increased numbers of apoptotic cells as compared with ulna neutral. 41 Injury to the TFCC can also be traumatic due to excessive axial loading, forearm rotation, and ulnar deviation, commonly manifesting as ulnar-sided wrist pain with focal tenderness. 39 42 Patients commonly present with ulnar-sided wrist pain after a fall on an outstretched hand, and physical examination should include various provocative tests to reproduce the symptoms. These include ulnocarpal stress test (involving axial stress with ulnar deviation during passive supination-pronation), the ulnar foveal sign (with tenderness at the soft depression between flexor carpi ulnaris [FCU] and ulnar styloid), and clinical evaluation of DRUJ instability. 29 42 43 The ulnar grind test, which involves axial load applied with the wrist dorsiflexed and ulnar deviated, can also aid in diagnosis. 44
Several imaging modalities have been used to evaluate TFCC injuries with varying degrees of success. The sensitivity and specificity of using MRI for detecting TFCC injuries has varied widely in the literature, and its efficacy may be subject to radiologist experience and location of injury, with peripheral tears prone to underdetection ( Figs. 4 5 6 ). 45 46 47 MR arthrogram is widely supported as the test of choice for detecting TFCC tears, as it has an accuracy of 79 to 100% in detecting TFCC tears with improved localization of the site of injury; however, prior investigation has found 3.0 T MRI with dedicated coils to be only slightly less accurate than MR arthrogram. 48 49 50 51 Furthermore, axial traction may increase the rate of detection of a TFCC tear. 52 CT arthrogram has been explored as an alternative diagnostic modality, with a recent meta-analysis suggesting that its sensitivity and specificity are statistically equivalent to that of MR arthrogram. 53 Wrist arthroscopy is sensitive for diagnosis of TFCC injuries and central degenerative tears. It was found to be more sensitive for peripheral tears, which are hard to visualize through noninvasive means. 46 While arthroscopy allows for the use of a variety of diagnostic tests, such as the hook test with a 90% sensitivity and specificity for TFCC foveal detachment, the interobserver reliability of arthroscopic examination has recently been questioned. 54 55
Fig. 5.

Coronal proton density fat-saturated MRI showing a tear of the triangular fibrocartilage disc, foveal attachment (arrow pointing to tear of foveal attachment), as evidenced by the bright signal intensity.
Fig. 6.

Coronal proton density fat-saturated MRI showing tear of the triangular fibrocartilage disc, radial attachment (arrow pointing to radial attachment), as evidenced by the bright signal intensity.
TFCC injury can be classified using the Palmer classification ( Table 1 ), which differentiates injuries based on their traumatic or degenerative nature, and further delineates based on anatomic location in the former class and anatomic location along with extent of degenerative changes in the latter class. 39 However, since patients usually present several months after an injury, it is not clear how to distinguish traumatic and degenerative lesions on physical examination. Additionally, the reliability and accuracy of this classification has never been adequately tested. Treatment can initially involve conservative measures, including observation along with strengthening of the secondary stabilizers and radioulnar straps. Time can be both therapeutic and diagnostic for many patients with ulnar-sided wrist pain and no DRUJ instability, as symptoms gradually resolve. The surgical approach (open or arthroscopic) and type of intervention will depend on location and extent of injury. Arthroscopic debridement to treat Palmer type 1A injuries has been found to be widely successful, except in the setting of positive ulnar variance, where the failure rate has been found to be as high as 30%. 56 57 Palmer 1B lesions can be repaired through open or arthroscopic means, with the latter approach having a variety of reported techniques including inside-out, outside-in, and all-inside. Likewise, repair of Palmer 1C and 1D lesions have been reported through arthroscopic and open approaches. 58 Although a recent systematic review found arthroscopic and open approaches to result in comparable outcomes, the study emphasized the need for further prospective studies comparing surgical approaches. 59
Table 1. Palmer classification for TFCC injury.
| Class 1: Traumatic injury | Class 2: Degenerative injury |
|---|---|
| Abbreviations: LT, lunotriquetral; TFCC, triangular fibrocartilage. Source: Reproduced with permission from Palmer, AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989; 14(4): 594–606. | |
| A) Central perforation | A) TFCC wear |
| B) Ulnar avulsion with or without distal ulnar fracture | B) TFCC wear + lunate and/or ulnar chondromalacia |
| C) Distal avulsion | C) TFCC perforation + lunate and/or ulnar chondromalacia |
| D) Radial avulsion with or without sigmoid notch fracture |
D) TFCC perforation + lunate and/or ulnar chondromalacia + LT ligament perforation |
| E) TFCC perforation + lunate and/or ulnar chondromalacia + LT ligament perforation + ulnocarpal arthritis | |
Intrinsic Carpal Ligaments
Dorsal Intrinsic Ligaments
The dorsal intercarpal (DIC) ligament originates from the dorsal tubercle of the triquetrum and attaches distally on the lunate with insertions into the dorsal aspect of the lunate and groove of the scaphoid and onto the scapholunate and lunotriquetral ligaments as well as to the dorsal rim of the trapezium and trapezoid ( Fig. 2 ). 32 The DIC, which acts as a primary dorsal stabilizer of the scaphoid during wrist motion, works with the DRC to provide scaphoid and lunate stability. Both ligaments were found to have a high concentration of mechanoreceptors and nerve endings providing proprioceptive feedback. The ligaments serve as the first line of defense against instability, and provide the nervous system with the necessary information, to activate the muscles, which are the ultimate wrist stabilizers.
The DIC can be visualized using thin-section coronal MRI images ( Fig. 7 ), with particularly high detection rates using 3D Fourier transform MR imaging. 22 60 Chronic DIC avulsion, most commonly accompanied by scapholunate instability, repaired through arthroscopy-assisted dorsal capsuloplasty was found to improve the scapholunate angle, pain, wrist range of motion, and grip strength. 61 Similarly, in chronic scapholunate dissociation with irreparable scapholunate ligament, a ligamentoplasty with a free palmaris longus graft was used to reconstruct scapholunate and DIC, resulting in improvement in pain and decrease in scapholunate angle. 62
Fig. 7.
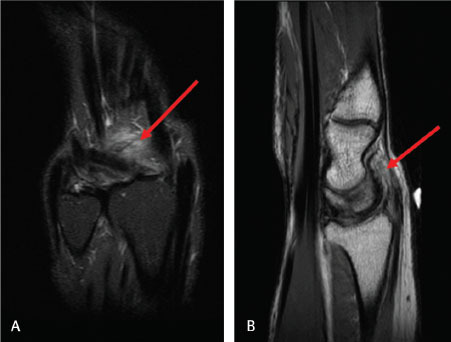
Heterogeneity and periligamentous edema involving the dorsal intercarpal ligament consistent with a sprain as evidenced by diffuse bright signal. ( A ) Coronal short tau inversion recovery (STIR) image. ( B ) Sagittal proton density (PD)-weighted image.
Interosseous Ligaments
The most clinically relevant interosseous ligaments are the scapholunate ligament (SLL) and lunotriquetral ligament (LTL). Both serve as important wrist stabilizers, and injury to either one can lead to potential carpal instability. The SLL is a C-shaped ligament connecting all but the distal articular surfaces of the scaphoid and lunate ( Fig. 2 ). It is comprised of dorsal, palmar, and proximal components, with the dorsal component being the thickest of the three and the most important stabilizer. 63 64 The SLL is most commonly injured through a fall on an extended wrist with ulnar deviation and intercarpal supination, which has been associated with up to 64% of distal radius fractures. 65 66 Typically, flexion of the scaphoid causes palmar flexion of the lunate via the SLL connection. However, with rupture of the SLL, scaphoid palmar flexion occurs without the lunate, which then dorsiflexes through its intact connection with the triquetrum via the LTL ( Fig. 8A ). 67 It is important to note that isolated SLL injury does not generally lead to dorsal intercalated segment instability (DISI), which requires an additional injury of scaphotrapeziotrapezoid or dorsal intercarpal ligaments. 68
Fig. 8.
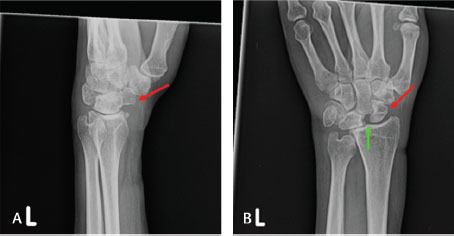
Radiographic signs of scapholunate injury. ( A ) Left hand lateral radiograph of wrist with scapholunate advanced collapse (SLAC) showing volar-flexed scaphoid (red arrow). ( B ) Left hand frontal radiograph of wrist with SLAC showing Terry Thomas sign (green arrow) and signet-ring sign (red arrow).
Depending on the severity and chronicity of the SLL injury, the patient can present with radial and dorsal wrist pain accompanied by wrist instability. Physical examination can reveal swelling and tenderness to palpation in the anatomical snuffbox and around the dorsal radiocarpal joint. 1 The scaphoid shift or Watson’s test can be used to assess for scaphoid instability: the examiner’s thumb pressed against the scaphoid tubercle, while the patient’s wrist is moved from ulnar deviation and slight extension to radial deviation and slight flexion. Pain with asymmetric hypermobility or decreased motion along with a palpable “clunk,” as thumb pressure is released is suggestive of SLL injury. Given that the sensitivity and specificity are reported as 69% and 66%, respectively, additional diagnostic modalities should be employed. 69 70
Radiographs are an important first radiologic test in the evaluation of any suspected ligamentous injury, particularly to assess SLL injury severity ranging from dynamic to static instability. The latter is apparent with the presence of the Terry Thomas sign, disruption of carpal Gilula arcs (normal carpal alignment as viewed on PA radiographs), and the scaphoid ring sign (cortical ring appearance due to abnormal scaphoid volar flexion) with the wrist at rest ( Fig. 8B ). Dynamic instability is apparent on radiographs, with these signs only visualized upon stress of the wrist with a closed fist or clenched pencil, and a normal appearance of radiographs at rest. 1 71
Detection of SLL tears using MRI was found to be variable on systematic review with sensitivities ranging from 11% to 89% and specificities ranging from 55% to 100% ( Fig. 9 ). 72 Although use of higher resolution machines and axial wrist views have been shown to improve the diagnosis, 73 74 MRA has been found on systematic review to be superior to MRI for SLL tear detection, with a sensitivity of 82.1% and specificity of 92.8%, although 3.0 T MRI still has a higher specificity. 75 While arthroscopy remains the gold standard for SLL detection, particularly due to its utility in enabling visualization of SLL dynamic instability and application of the Geissler Arthroscopic Grading System ( Table 2 ), recent advances in dynamic noninvasive imaging modalities (i.e., 4-D CT) could create a future paradigm shift in diagnostic methods. 76 77
Fig. 9.
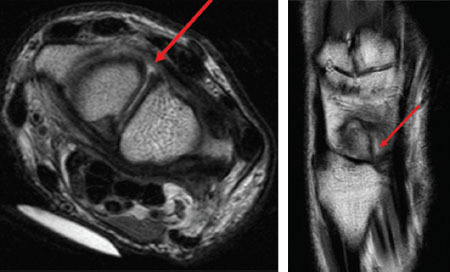
Incomplete tear involving the dorsal band of the scapholunate ligament with fluid in the gap as evidenced by increase signal intensity. Arrow in all images pointing to tear in scapholunate ligament. ( A ) Axial proton density (PD)-weighted image. ( B ) Coronal PD-weighted image.
Table 2. Geissler arthroscopic classification of intracarpal ligament tears.
| Grade | Description |
|---|---|
| Source: Reproduced with permission from Geissler et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996; 78(3): 357–65. | |
| I | Attenuation or hemorrhage of interosseous ligament as seen from radiocarpal space. No incongruency of carpal alignment in midcarpal space. |
| II | Attenuation or hemorrhage of interosseous ligament as seen from radiocarpal space. Incongruency or step-off of carpal space. There may be slight gap (less than width of probe) between carpal bones. |
| III | Incongruency or step-off of carpal alignment as seen from both radiocarpal and midcarpal space. Probe may be passed through gap between carpal bones. |
| IV | Incongruency or step-off of carpal alignment, as seen from both radiocarpal and midcarpal space. There is gross instability with manipulation. 2.7 mm arthroscope may be passed through gap between carpal bones. |
Treatment of SLL tears, according to the widely cited algorithm by Garcia-Elias et al, can be guided based on six parameters including whether the dorsal SLL is intact, if there is sufficient tissue to repair a dorsal SLL, if there is normal scaphoid alignment, if carpal malalignment is reducible, the lunate position, and if cartilage at radiocarpal and midcarpal joints are normal. Using these parameters, the severity of injury can then be translated into an appropriate operative approach that ranges from K-wire fixation with or without dorsal capsulodesis for a partial SLL injury to a motion-preserving procedure that relieves pain, such as a proximal row carpectomy or limited wrist arthrodesis, in cases of SLAC. 78 While there is still much debate about indications for proximal carpectomy versus four-corner fusion in cases of SLAC, the latter has been associated with greater improvement in postoperative radial deviation and grip strength, and proximal row carpectomy has been associated with greater improvement in wrist flexion and extension with a lower complication rate. 79
The LTL is a horseshoe-shaped ligament that connects the proximal lunate and triquetrum ( Fig. 2 ). 8 Like the SLL, the LTL also comprises dorsal, palmar, and proximal components; however, unlike the SLL, the palmar component is the thickest of the three and the most important to stabilization of the lunotriquetral joint. 80 Acute and isolated LTL injury is uncommon, but can occur through a fall on an outstretched, pronated, and extended hand that is in radial deviation. 81 In most cases, isolated LTL injury alone is insufficient to cause volar intercalated segmental instability (VISI), defined as volar flexion of the longitudinal axis of the lunate in relation to the capitate and radius with the wrist at neutral position ( Fig. 10A ). This condition typically requires concurrent injury of secondary supporting ligaments including dorsal radiocarpal, dorsal intercarpal, or ulnar arcuate ligaments; however, it can result from sprain of the LTL. 82 83 Similar to DISI, the severity of VISI ranges from dynamic to static instability, where the former has the abnormal radiographic appearance described below only with stress positions, and the latter has an abnormal radiographic appearance even with the wrist at rest. 81 84 85
Fig. 10.
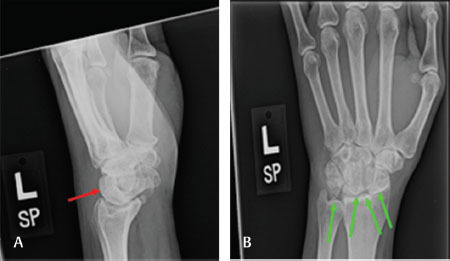
Radiographic signs of lunotriquetral injury. ( A ) Left hand lateral radiograph of volar intercalated segmental instability (VISI) deformity secondary to chronic lunotriquetral insufficiency showing volar rotation of the lunate (red arrow). ( B ) Left hand frontal radiograph of VISI deformity secondary to chronic lunotriquetral insufficiency showing severe disruption of the carpal Gilula arcs (green arrows).
Depending on the severity of the injury, the patient will present with intermittent ulnar-sided wrist pain, which may be reproduced using several clinical tests: the ballottement test (pisiform and triquetrum are compressed against the secured lunate), the Regan “shuck” test (lunate is displaced in dorsal or volar direction while the rest of the wrist is displaced in the opposite direction), and the Kleinman “shear” test (lunate and radial wrist are secured with stress placed on the LT joint through pisiform and triquetrum displacement). 86 However, these tests have variable efficacies, with the ballottement test having only a 64% sensitivity and 44% specificity, thus additional diagnostic modalities should be employed. 70
Similar to suspected SLL injuries, the first step in radiologic evaluation of LTL injuries should be simple radiographs, as disruption of carpal Gilula arcs may be visualized ( Fig. 10B ); however, radiographs are often normal even in the setting of injury. Additionally, triquetrum-lunate malalignment and alteration of the scapholunate angle may also be visualized in the event of LT dissociation with VISI deformity ( Fig. 10A ). 81 Similar to SLL, detection of LTL tears using MRI was variable on systematic review with sensitivities ranging from 0% to 82% and specificities ranging from 76% to 100% ( Fig. 11 ). 72 Arthrography has been found to be valuable in detecting LTL tears, with CT arthrography having a higher sensitivity and specificity than MRI and a particular diagnostic utility in detecting dorsal segment tears. 87 Arthroscopy remains the gold standard due to the ability to directly observe LTL tears and apply the Geissler Arthroscopic Grading System ( Table 2 ) as well as assess LT joint integrity. 81
Fig. 11.

Nondistracted full thickness tear through the volar fibers of the lunotriquetral ligament as seen in coronal short tau inversion recovery (STIR) image and as evidenced by bright signal intensity. Findings are apparent in the background of severe inflammatory arthropathy, noting multicompartmental synovitis/pannus, diffuse cartilage loss, and erosive change.
Like other ligamentous injuries, the course of intervention varies based on severity, chronicity, and associated degenerative changes, with nonoperative management often indicated for initial treatment of mild injuries. 88 The range of operative interventions includes LT arthrodesis, ligament reconstruction using a distal extensor carpi ulnaris tendon graft, and ligament repair. Study of operative approaches in a largely subacute or chronic patient population revealed that the probability of remaining complication free after 5 years was 68.6% for reconstruction, 13.5% for repair, and less than 1% for arthrodesis with significantly higher subjective indicators of pain relief and satisfaction in those receiving reconstruction or repair. 89
Conclusion
Wrist ligament injuries are common and complex injuries that require anatomical mastery, extensive understanding of injury patterns, and evidence-based diagnostic modalities to devise the best course of action for each patient. If an operative approach is indicated, a variety of options are available and the best one should be chosen based on injury severity and chronicity, with the goal of optimizing functional outcomes.
Acknowledgments
The authors wish to thank Amy Zhong, MA for her illustrations.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Chim H, Moran S L. Wrist essentials: the diagnosis and management of scapholunate ligament injuries. Plast Reconstr Surg. 2014;134(02):312e–322e. doi: 10.1097/PRS.0000000000000423. [DOI] [PubMed] [Google Scholar]
- 2.Sammer D M, Shin A Y. Wrist surgery: management of chronic scapholunate and lunotriquetral ligament injuries. Plast Reconstr Surg. 2012;130(01):138e–156e. doi: 10.1097/PRS.0b013e318254b5de. [DOI] [PubMed] [Google Scholar]
- 3.Ozçelik A, Günal I, Köse N, Seber S, Omeroğlu H. Wrist ligaments: their significance in carpal instability. Ulus Travma Acil Cerrahi Derg. 2005;11(02):115–120. [PubMed] [Google Scholar]
- 4.Connell D, Page P, Wright W, Hoy G. Magnetic resonance imaging of the wrist ligaments. Australas Radiol. 2001;45(04):411–422. doi: 10.1046/j.1440-1673.2001.00948.x. [DOI] [PubMed] [Google Scholar]
- 5.Smith D K. Volar carpal ligaments of the wrist: normal appearance on multiplanar reconstructions of three-dimensional Fourier transform MR imaging. Am J Roentgenol. 1993;161(02):353–357. doi: 10.2214/ajr.161.2.8333377. [DOI] [PubMed] [Google Scholar]
- 6.Bencardino J T, Rosenberg Z S. Sports-related injuries of the wrist: an approach to MRI interpretation. Clin Sports Med. 2006;25(03):409–432. doi: 10.1016/j.csm.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 7.van Kooten EO, Coster E, Segers M J, Ritt M J. Early proximal row carpectomy after severe carpal trauma. Injury. 2005;36(10):1226–1232. doi: 10.1016/j.injury.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Timins M E, Jahnke J P, Krah S F, Erickson S J, Carrera G F. MR imaging of the major carpal stabilizing ligaments: normal anatomy and clinical examples. Radiographics. 1995;15(03):575–587. doi: 10.1148/radiographics.15.3.7624564. [DOI] [PubMed] [Google Scholar]
- 9.Yuan B J, Dennison D G, Elhassan B T, Kakar S. Outcomes after radiocarpal dislocation: a retrospective review. Hand (N Y) 2015;10(03):367–373. doi: 10.1007/s11552-014-9736-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rominger M B, Bernreuter W K, Kenney P J, Lee D H. MR imaging of anatomy and tears of wrist ligaments. Radiographics. 1993;13(06):1233–1246. doi: 10.1148/radiographics.13.6.8290721. [DOI] [PubMed] [Google Scholar]
- 11.Berger R A, Landsmeer J M. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg Am. 1990;15(06):847–854. doi: 10.1016/0363-5023(90)90002-9. [DOI] [PubMed] [Google Scholar]
- 12.Adler B D, Logan P M, Janzen D L et al. Extrinsic radiocarpal ligaments: magnetic resonance imaging of normal wrists and scapholunate dissociation. Can Assoc Radiol J. 1996;47(06):417–422. [PubMed] [Google Scholar]
- 13.Shahabpour M, De Maeseneer M, Pouders C et al. MR imaging of normal extrinsic wrist ligaments using thin slices with clinical and surgical correlation. Eur J Radiol. 2011;77(02):196–201. doi: 10.1016/j.ejrad.2010.05.043. [DOI] [PubMed] [Google Scholar]
- 14.Mak W H, Szabo R M, Myo G K. Assessment of volar radiocarpal ligaments: MR arthrographic and arthroscopic correlation. Am J Roentgenol. 2012;198(02):423–427. doi: 10.2214/AJR.11.6919. [DOI] [PubMed] [Google Scholar]
- 15.Lacelli F, Muda A, Sconfienza L M, Schettini D, Garlaschi G, Silvestri E. High-resolution ultrasound anatomy of extrinsic carpal ligaments. Radiol Med (Torino) 2008;113(04):504–516. doi: 10.1007/s11547-008-0269-2. [DOI] [PubMed] [Google Scholar]
- 16.Boutry N, Lapegue F, Masi L, Claret A, Demondion X, Cotten A. Ultrasonographic evaluation of normal extrinsic and intrinsic carpal ligaments: preliminary experience. Skeletal Radiol. 2005;34(09):513–521. doi: 10.1007/s00256-005-0929-4. [DOI] [PubMed] [Google Scholar]
- 17.Dunn M J, Johnson C. Static scapholunate dissociation: a new reconstruction technique using a volar and dorsal approach in a cadaver model. J Hand Surg Am. 2001;26(04):749–754. doi: 10.1053/jhsu.2001.26025. [DOI] [PubMed] [Google Scholar]
- 18.Moritomo H. Anatomy and clinical relevance of the ulnocarpal ligament. J Wrist Surg. 2013;2(02):186–189. doi: 10.1055/s-0033-1345023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berger R A. The ligaments of the wrist. A current overview of anatomy with considerations of their potential functions. Hand Clin. 1997;13(01):63–82. [PubMed] [Google Scholar]
- 20.Taljanovic M S, Goldberg M R, Sheppard J E, Rogers L F. US of the intrinsic and extrinsic wrist ligaments and triangular fibrocartilage complex–normal anatomy and imaging technique. Radiographics. 2011;31(01):e44. doi: 10.1148/rg.e44. [DOI] [PubMed] [Google Scholar]
- 21.Berger R A. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;(383):32–40. doi: 10.1097/00003086-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Bateni C P, Bartolotta R J, Richardson M L, Mulcahy H, Allan C H. Imaging key wrist ligaments: what the surgeon needs the radiologist to know. Am J Roentgenol. 2013;200(05):1089–1095. doi: 10.2214/AJR.12.9738. [DOI] [PubMed] [Google Scholar]
- 23.Allieu Y, Garcia-Elias M. Dynamic radial translation instability of the carpus. J Hand Surg [Br] 2000;25(01):33–37. doi: 10.1054/jhsb.1999.0285. [DOI] [PubMed] [Google Scholar]
- 24.Moritomo H, Murase T, Arimitsu S, Oka K, Yoshikawa H, Sugamoto K. Change in the length of the ulnocarpal ligaments during radiocarpal motion: possible impact on triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2008;33(08):1278–1286. doi: 10.1016/j.jhsa.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 25.Mooney J F, Poehling G G. Disruption of the ulnolunate ligament as a cause of chronic ulnar wrist pain. J Hand Surg Am. 1991;16(02):347–349. doi: 10.1016/s0363-5023(10)80124-8. [DOI] [PubMed] [Google Scholar]
- 26.Sato R, Hibino N, Hamada Y, Sairyo K. Ulnolunate Ligament Avulsion Fracture of the Lunate: A Case Report. J Wrist Surg. 2017;6(02):148–151. doi: 10.1055/s-0036-1593359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tay S C, Berger R A, Parker W L. Longitudinal split tears of the ulnotriquetral ligament. Hand Clin. 2010;26(04):495–501. doi: 10.1016/j.hcl.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Hyatt B T, Rhee P C. Longitudinal split tears of the ulnotriquetral ligament. Oper Tech Sports Med. 2016;24(02):126–130. [Google Scholar]
- 29.Tay S C, Tomita K, Berger R A. The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg Am. 2007;32(04):438–444. doi: 10.1016/j.jhsa.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 30.Ringler M D, Howe B M, Amrami K K, Hagen C E, Berger R A. Utility of magnetic resonance imaging for detection of longitudinal split tear of the ulnotriquetral ligament. J Hand Surg Am. 2013;38(09):1723–1727. doi: 10.1016/j.jhsa.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 31.Tang C QY, Lai S WH, Leow G, Tay S C. Patient-reported outcome following ulnotriquetral ligament split tear repair. J Hand Surg Asian Pac Vol. 2017;22(04):445–451. doi: 10.1142/S0218810417500484. [DOI] [PubMed] [Google Scholar]
- 32.Viegas S F, Yamaguchi S, Boyd N L, Patterson R M. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg Am. 1999;24(03):456–468. doi: 10.1053/jhsu.1999.0456. [DOI] [PubMed] [Google Scholar]
- 33.Slutsky D J. Incidence of dorsal radiocarpal ligament tears in the presence of other intercarpal derangements. Arthroscopy. 2008;24(05):526–533. doi: 10.1016/j.arthro.2007.12.014. [DOI] [PubMed] [Google Scholar]
- 34.Slutsky D J. The management of dorsal radiocarpal ligament tears. J Hand Surg Am. 2005;5(03):167–174. doi: 10.1016/j.jhsa.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 35.Slutsky D J. The incidence of dorsal radiocarpal ligament tears in patients having diagnostic wrist arthroscopy for wrist pain. J Hand Surg Am. 2008;33(03):332–334. doi: 10.1016/j.jhsa.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 36.Slutsky D J. Arthroscopic repair of dorsal radiocarpal ligament tears. Arthroscopy. 2002;18(09):E49. doi: 10.1053/jars.2002.36471. [DOI] [PubMed] [Google Scholar]
- 37.Slutsky D J. Arthroscopic dorsal radiocarpal ligament repair. Arthroscopy. 2005;21(12):1486. doi: 10.1016/j.arthro.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Palmer A K, Werner F W. The triangular fibrocartilage complex of the wrist–anatomy and function. J Hand Surg Am. 1981;6(02):153–162. doi: 10.1016/s0363-5023(81)80170-0. [DOI] [PubMed] [Google Scholar]
- 39.Palmer A K. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14(04):594–606. doi: 10.1016/0363-5023(89)90174-3. [DOI] [PubMed] [Google Scholar]
- 40.Chan J J, Teunis T, Ring D. Prevalence of triangular fibrocartilage complex abnormalities regardless of symptoms rise with age: systematic review and pooled analysis. Clin Orthop Relat Res. 2014;472(12):3987–3994. doi: 10.1007/s11999-014-3825-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Unglaub F, Wolf M B, Thome M A, Germann G, Sauerbier M, Reiter A. Correlation of ulnar length and apoptotic cell death in degenerative lesions of the triangular fibrocartilage. Arthroscopy. 2008;24(03):299–304. doi: 10.1016/j.arthro.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 42.Henry M H. Management of acute triangular fibrocartilage complex injury of the wrist. J Am Acad Orthop Surg. 2008;16(06):320–329. doi: 10.5435/00124635-200806000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Nakamura R, Horii E, Imaeda T, Nakao E, Kato H, Watanabe K. The ulnocarpal stress test in the diagnosis of ulnar-sided wrist pain. J Hand Surg [Br] 1997;22(06):719–723. doi: 10.1016/s0266-7681(97)80432-9. [DOI] [PubMed] [Google Scholar]
- 44.Ahn A K, Chang D, Plate A M.Triangular fibrocartilage complex tears: a review Bull NYU Hosp Jt Dis 200664(3-4)114–118. [PubMed] [Google Scholar]
- 45.Blazar P E, Chan P S, Kneeland J B, Leatherwood D, Bozentka D J, Kowalchick R. The effect of observer experience on magnetic resonance imaging interpretation and localization of triangular fibrocartilage complex lesions. J Hand Surg Am. 2001;26(04):742–748. doi: 10.1053/jhsu.2001.24966. [DOI] [PubMed] [Google Scholar]
- 46.Haims A H, Schweitzer M E, Morrison W B et al. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol. 2002;178(02):419–422. doi: 10.2214/ajr.178.2.1780419. [DOI] [PubMed] [Google Scholar]
- 47.Potter H G, Asnis-Ernberg L, Weiland A J. Hotchkiss RN, Peterson MG, McCormack RR Jr. The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J Bone Joint Surg Am. 1997;79(11):1675–1684. doi: 10.2106/00004623-199711000-00009. [DOI] [PubMed] [Google Scholar]
- 48.Joshy S, Ghosh S, Lee K, Deshmukh S C. Accuracy of direct magnetic resonance arthrography in the diagnosis of triangular fibrocartilage complex tears of the wrist. Int Orthop. 2008;32(02):251–253. doi: 10.1007/s00264-006-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee R K, Ng A W, Tong C S et al. Intrinsic ligament and triangular fibrocartilage complex tears of the wrist: comparison of MDCT arthrography, conventional 3-T MRI, and MR arthrography. Skeletal Radiol. 2013;42(09):1277–1285. doi: 10.1007/s00256-013-1666-8. [DOI] [PubMed] [Google Scholar]
- 50.Pederzini L, Luchetti R, Soragni O et al. Evaluation of the triangular fibrocartilage complex tears by arthroscopy, arthrography, and magnetic resonance imaging. Arthroscopy. 1992;8(02):191–197. doi: 10.1016/0749-8063(92)90036-b. [DOI] [PubMed] [Google Scholar]
- 51.Boer B C, Vestering M, van Raak S M, van Kooten E O, Huis In ’t Veld R, Vochteloo A JH. MR arthrography is slightly more accurate than conventional MRI in detecting TFCC lesions of the wrist. Eur J Orthop Surg Traumatol. 2018;28(08):1549–1553. doi: 10.1007/s00590-018-2215-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee R K, Griffith J F, Ng A W, Nung R C, Yeung D K. Wrist traction during MR arthrography improves detection of triangular fibrocartilage complex and intrinsic ligament tears and visibility of articular cartilage. AJR Am J Roentgenol. 2016;206(01):155–161. doi: 10.2214/AJR.15.14948. [DOI] [PubMed] [Google Scholar]
- 53.Treiser M D, Crawford K, Iorio M L. TFCC injuries: meta-analysis and comparison of diagnostic imaging modalities. J Wrist Surg. 2018;7(03):267–272. doi: 10.1055/s-0038-1629911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Trehan S K, Wall L B, Calfee R P et al. Arthroscopic diagnosis of the triangular fibrocartilage complex foveal tear: a cadaver assessment. J Hand Surg Am. 2018;43(07):6800–6.8E7. doi: 10.1016/j.jhsa.2017.12.017. [DOI] [PubMed] [Google Scholar]
- 55.Park A, Lutsky K, Matzon J, Leinberry C, Chapman T, Beredjiklian P K. An evaluation of the reliability of wrist arthroscopy in the assessment of tears of the triangular fibrocartilage complex. J Hand Surg Am. 2018;43(06):545–549. doi: 10.1016/j.jhsa.2018.02.031. [DOI] [PubMed] [Google Scholar]
- 56.Bernstein M A, Nagle D J, Martinez A. Stogin JM Jr, Wiedrich TA. A comparison of combined arthroscopic triangular fibrocartilage complex debridement and arthroscopic wafer distal ulna resection versus arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnocarpal abutment syndrome. Arthroscopy. 2004;20(04):392–401. doi: 10.1016/j.arthro.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 57.Minami A, Ishikawa J, Suenaga N, Kasashima T. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg Am. 1996;21(03):406–411. doi: 10.1016/s0363-5023(96)80353-4. [DOI] [PubMed] [Google Scholar]
- 58.Kovachevich R, Elhassan B T. Arthroscopic and open repair of the TFCC. Hand Clin. 2010;26(04):485–494. doi: 10.1016/j.hcl.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 59.Andersson J K, Åhlén M, Andernord D. Open versus arthroscopic repair of the triangular fibrocartilage complex: a systematic review. J Exp Orthop. 2018;5(01):6. doi: 10.1186/s40634-018-0120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smith D K. Dorsal carpal ligaments of the wrist: normal appearance on multiplanar reconstructions of three-dimensional Fourier transform MR imaging. AJR Am J Roentgenol. 1993;161(01):119–125. doi: 10.2214/ajr.161.1.8517289. [DOI] [PubMed] [Google Scholar]
- 61.Binder A C, Kerfant N, Wahegaonkar A L, Tandara A A, Mathoulin C L. Dorsal wrist capsular tears in association with scapholunate instability: results of an arthroscopic dorsal capsuloplasty. J Wrist Surg. 2013;2(02):160–167. doi: 10.1055/s-0032-1333426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Athlani L, Pauchard N, Dautel G. Outcomes of scapholunate intercarpal ligamentoplasty for chronic scapholunate dissociation: a prospective study in 26 patients. J Hand Surg Eur Vol. 2018;43(07):700–707. doi: 10.1177/1753193418772801. [DOI] [PubMed] [Google Scholar]
- 63.Berger R A, Imeada T, Berglund L, An K N. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg Am. 1999;24(05):953–962. doi: 10.1053/jhsu.1999.0953. [DOI] [PubMed] [Google Scholar]
- 64.Berger R A. The gross and histologic anatomy of the scapholunate interosseous ligament. J Hand Surg Am. 1996;21(02):170–178. doi: 10.1016/S0363-5023(96)80096-7. [DOI] [PubMed] [Google Scholar]
- 65.Mayfield J K, Johnson R P, Kilcoyne R K. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5(03):226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 66.Lans J, Lasa A, Chen N C, Jupiter J B. Incidence and functional outcomes of scapholunate diastases associated distal radius fractures: a 2-year follow-up scapholunate dissociation. Open Orthop J. 2018;12:33–40. doi: 10.2174/1874325001812010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee D J, Elfar J C. Carpal ligament injuries, pathomechanics, and classification. Hand Clin. 2015;31(03):389–398. doi: 10.1016/j.hcl.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pérez A J, Jethanandani R G, Vutescu E S, Meyers K N, Lee S K, Wolfe S W. Role of ligament stabilizers of the proximal carpal row in preventing dorsal intercalated segment instability: a cadaveric study. J Bone Joint Surg Am. 2019;101(15):1388–1396. doi: 10.2106/JBJS.18.01419. [DOI] [PubMed] [Google Scholar]
- 69.Watson H K, Ashmead D, IV, Makhlouf M V. Examination of the scaphoid. J Hand Surg Am. 1988;13(05):657–660. doi: 10.1016/s0363-5023(88)80118-7. [DOI] [PubMed] [Google Scholar]
- 70.LaStayo P, Howell J. Clinical provocative tests used in evaluating wrist pain: a descriptive study. J Hand Ther. 1995;8(01):10–17. doi: 10.1016/s0894-1130(12)80150-5. [DOI] [PubMed] [Google Scholar]
- 71.Lee S K, Desai H, Silver B, Dhaliwal G, Paksima N. Comparison of radiographic stress views for scapholunate dynamic instability in a cadaver model. J Hand Surg Am. 2011;36(07):1149–1157. doi: 10.1016/j.jhsa.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 72.Andersson J K, Andernord D, Karlsson J, Fridén J. Efficacy of magnetic resonance imaging and clinical tests in diagnostics of wrist ligament injuries: a systematic review. Arthroscopy. 2015;31(10):2014–2000. doi: 10.1016/j.arthro.2015.04.090. [DOI] [PubMed] [Google Scholar]
- 73.Spaans A J, Minnen P v, Prins H J, Korteweg M A, Schuurman A H. The value of 3.0-tesla MRI in diagnosing scapholunate ligament injury. J Wrist Surg. 2013;2(01):69–72. doi: 10.1055/s-0032-1333425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Greditzer HGT I V, Zeidenberg J, Kam C C et al. Optimal detection of scapholunate ligament tears with MRI. Acta Radiol. 2016;57(12):1508–1514. doi: 10.1177/0284185115626468. [DOI] [PubMed] [Google Scholar]
- 75.Hafezi-Nejad N, Carrino J A, Eng J et al. Scapholunate interosseous ligament tears: diagnostic performance of 1.5 T, 3 T MRI, and MR arthrography-A systematic review and Meta-analysis. Acad Radiol. 2016;23(09):1091–1103. doi: 10.1016/j.acra.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 76.Kakar S, Breighner R E, Leng S et al. The role of dynamic (4D) CT in the detection of scapholunate ligament injury. J Wrist Surg. 2016;5(04):306–310. doi: 10.1055/s-0035-1570463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Geissler W B, Freeland A E, Savoie F H, McIntyre L W, Whipple T L. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78(03):357–365. doi: 10.2106/00004623-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 78.Garcia-Elias M, Lluch A L, Stanley J K. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(01):125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 79.Saltzman B M, Frank J M, Slikker W, Fernandez J J, Cohen M S, Wysocki R W. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015;40(05):450–457. doi: 10.1177/1753193414554359. [DOI] [PubMed] [Google Scholar]
- 80.Ritt M J, Bishop A T, Berger R A, Linscheid R L, Berglund L J, An K N. Lunotriquetral ligament properties: a comparison of three anatomic subregions. J Hand Surg Am. 1998;23(03):425–431. doi: 10.1016/S0363-5023(05)80460-5. [DOI] [PubMed] [Google Scholar]
- 81.Shin A Y, Battaglia M J, Bishop A T. Lunotriquetral instability: diagnosis and treatment. J Am Acad Orthop Surg. 2000;8(03):170–179. doi: 10.5435/00124635-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 82.Reagan D S, Linscheid R L, Dobyns J H. Lunotriquetral sprains. J Hand Surg Am. 1984;9(04):502–514. doi: 10.1016/s0363-5023(84)80101-x. [DOI] [PubMed] [Google Scholar]
- 83.Van O verstraeten, L, Camus E J. The role of extrinsic ligaments in maintaining carpal stability - A prospective statistical analysis of 85 arthroscopic cases. Hand Surg Rehabil. 2016;35(01):10–15. doi: 10.1016/j.hansur.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 84.Horii E, Garcia-Elias M, An K N et al. A kinematic study of luno-triquetral dissociations. J Hand Surg Am. 1991;16(02):355–362. doi: 10.1016/s0363-5023(10)80126-1. [DOI] [PubMed] [Google Scholar]
- 85.Trumble T E, Bour C J, Smith R J, Glisson R R. Kinematics of the ulnar carpus related to the volar intercalated segment instability pattern. J Hand Surg Am. 1990;15(03):384–392. doi: 10.1016/0363-5023(90)90048-v. [DOI] [PubMed] [Google Scholar]
- 86.Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2012;37(07):1489–1500. doi: 10.1016/j.jhsa.2012.04.036. [DOI] [PubMed] [Google Scholar]
- 87.Schmid M R, Schertler T, Pfirrmann C W et al. Interosseous ligament tears of the wrist: comparison of multi-detector row CT arthrography and MR imaging. Radiology. 2005;237(03):1008–1013. doi: 10.1148/radiol.2373041450. [DOI] [PubMed] [Google Scholar]
- 88.Nicoson M C, Moran S L. Diagnosis and treatment of acute lunotriquetral ligament injuries. Hand Clin. 2015;31(03):467–476. doi: 10.1016/j.hcl.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 89.Shin A Y, Weinstein L P, Berger R A, Bishop A T. Treatment of isolated injuries of the lunotriquetral ligament. A comparison of arthrodesis, ligament reconstruction and ligament repair. J Bone Joint Surg Br. 2001;83(07):1023–1028. doi: 10.1302/0301-620x.83b7.11413. [DOI] [PubMed] [Google Scholar]


