Abstract
Introduction Psychiatric disease after traumatic limb loss impacts rehabilitation, prosthesis use, and quality of life. The purpose of this study was to evaluate the prevalence of psychiatric disease in civilians after isolated, traumatic upper extremity amputation and determine if any risk factors are associated with developing psychiatric disease.
Materials and Methods Demographics, time since injury, mechanism of injury, amputation level, hand affected (dominant vs. nondominant), Bureau of Workers’ Compensation (BWC) status, and prosthesis use were retrospectively reviewed for all patients treated from 2012 to 2017. For patients with an International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) diagnosed psychiatric disease, the diagnosis and length of treatment were recorded. Patients were grouped by presence or absence of psychiatric diagnosis and data analysis was performed using descriptive statistics, Fisher’s exact test, and relative risk.
Results Forty-six patients met the inclusion criteria. Thirty-one patients (67.4%) had at least one diagnosed psychiatric condition. Major depressive disorder was the most common ( n = 14), followed by posttraumatic stress disorder ( n = 11), adjustment disorder ( n = 11), anxiety ( n = 6), and panic disorder ( n = 2). No statistically significant correlation was seen between psychiatric illness and gender, age at the time of injury, time since injury, current employment status, BWC status, hand injured (dominant vs. nondominant), prosthetic use, or level of amputation.
Conclusion The rates of depression and anxiety after traumatic upper limb loss in the civilian population are similar to reported rates after combat injury. While we were unable to identify a statistically significant association with any of the studied variables, upper extremity surgeons should be aware of the high prevalence of psychiatric disease after traumatic upper extremity amputation.
Keywords: amputation, farm, prevalence, psychiatric, traumatic
Introduction
Approximately 2 million people are currently living with an amputation in the United States, and up to 150,000 new amputations occur every year. 1 Limb loss can negatively impact patients’ social life, occupational status, activities of daily living, and overall life satisfaction. 2 Previous epidemiological studies have shown that 14 to 50% of all amputations involve the upper extremity and that trauma is the most common etiology (68%). 1 3
After amputation, the importance of a multidisciplinary approach to treatment involving surgeons, physical medicine and rehabilitation, occupational therapy, prosthetists, and pain management has been well established. 4 5 6 7 8 9 However, a focus on functional outcomes after amputation, without properly addressing associated psychological sequelae, can result in maladaptive behaviors, poor psychosocial adjustment, and ultimately, the development of psychiatric illness, which can impact return to work, interpersonal relationships, and prosthetic use. 10 11 12
Traumatic amputation as a result of combat injury and the subsequent psychological effects have been well established. 3 13 14 15 16 However, previous studies of the prevalence of psychiatric disease after traumatic upper extremity amputation in the civilian population are limited by the inclusion of upper and lower extremities limb loss and include both traumatic and medical etiologies. 17 18 19 20 None has focused on psychiatric disease after traumatic, isolated, upper extremity amputation in the civilian population. The purpose of this study was to determine the frequency of psychiatric disease in patients treated at our upper extremity limb loss clinic and determine whether there was any correlation between development of psychiatric disease and several studied patient variables. We hypothesized that the prevalence of psychiatric disease in our patient group is similar to previously reported rates after upper limb loss from a combat-associated injury.
Materials and Methods
After Institutional Review Board approval, all patients who have been seen at our upper extremity limb loss clinic from 2012 to 2017 were identified through the electronic medical record (EMR) for possible inclusion in the study. Inclusion criteria used were: age older than 18 years, isolated traumatic upper extremity limb loss, and no known preexisting psychiatric diagnosis. Patient demographics were collected for all patients including: age, gender, and current employment status. The risk factors studied for development of psychiatric disease were time since amputation, mechanism of injury, amputation level (transhumeral, transradial, transmetacarpal, and transphalangeal), hand affected (dominant vs. nondominant), Bureau of Workers’ Compensation (BWC) status, and current prosthetic use.
If an ICD-10–coded psychiatric diagnosis was documented in the EMR, the specific diagnosis, psychiatric medication(s) used, and length of follow-up with psychiatry or psychology were recorded. All psychiatric diagnoses were made by an independent psychiatrist or clinical rehabilitation psychologist according to the diagnostic criteria found in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition. Patients were divided into two groups for data analysis: those diagnosed with at least one psychiatric illness versus those without psychiatric diagnoses. Odds ratios for the presence of at least one psychiatric diagnosis were calculated for each of the above-mentioned potential risk factors. Fisher’s exact test was used to assess significance for categorical values, while Student’s t -test was used for continuous variables. Statistical significance was set at p< 0.05.
Results
Of the 63 patients who were evaluated at our upper limb loss clinic, 46 patients met the inclusion criteria for our study. The average age was 45.3 years (23–71), and there were 37 males (80.4%) and 9 females (19.5%). The average time since injury was 43 months (range: 2–252 months). The most common mechanisms of injury included industrial accidents ( n = 28), motor vehicle collisions ( n = 10), saw injuries ( n = 4), farm accidents ( n = 2), and other ( n = 2). The level of amputation was: transhumeral (7 patients), transradial (16 patients), transmetacarpal (11 patients), and transphalangeal or partial hand (12 patients). The dominant hand was involved in 23 patients (50%) and nondominant hand in 19 patients (41.3%). Four patients had bilateral amputations (8.7%). Thirty patients (65.2%) were involved in a BWC injury and 26 patients (56.5%) were currently using a prosthesis.
Thirty-one patients (67.4%) had at least one diagnosed psychiatric condition. Demographics of patients with and without psychiatric diagnoses are listed in Table 1 . The average length of follow-up with psychiatry and/or psychology for these patients was 30 months. No statistically significant correlation was seen between gender ( p = 0.70), age at the time of injury ( p = 0.37), time since injury ( p = 0.25), current employment status ( p = 0.20), BWC status ( p = 0.10), or prosthetic use ( p = 0.53). Level and laterality of injuries are shown in Table 2 . Note that a psychiatric diagnosis was present in all four patients with bilateral injuries; however, this was not statistically significant when compared with unilateral amputation ( p = 0.29). Level of injury also did not correlate with presence of psychiatric diagnoses ( Table 3 ).
Table 1. Demographic factors.
| Psychiatric diagnoses | No psychiatric diagnoses | p -Value | OR (95% CI) | |
|---|---|---|---|---|
| Abbreviations: BWC, Bureau of Workers’ Compensation; CI, confidence interval; OR, odds ratio. Note: When applicable, values are reported as mean ± standard deviation. Percentages and ranges appear in parenthesis. | ||||
| Total | 31 | 15 | ||
| Age | 45.2 ± 11.9 (23–62) | 41.8 ± 12.6 (30–71) | 0.37 | |
| Time since injury (y) | 6.21 ± 5.5 (1.1–27.0) | 4.45 ± 2.7 (1.5–12.7) | 0.25 | |
| Male | 24 (77.4%) | 13 (86.7%) | 0.70 | 0.53 (0.10–2.91) |
| Unemployed | 20 (64.5%) | 6 (40.0%) | 0.20 | 2.73 (0.77–9.69) |
| BWC status | 23 (74.2%) | 7 (46.7%) | 0.10 | 3.29 (0.90–11.99) |
| Prosthetic use | 19 (61.3%) | 7 (46.7%) | 0.53 | 1.81 (0.52–6.29) |
Table 2. Details of amputation.
| Total | Psychiatric diagnoses | No psychiatric diagnoses | |
|---|---|---|---|
| Number | 46 | 31 | 15 |
| Highest level of amputation | |||
| Transphalangeal | 12 | 6 | 6 |
| Transmetacarpal | 11 | 9 | 2 |
| Transradial | 16 | 10 | 6 |
| Transhumeral | 7 | 6 | 1 |
| Injured hand | |||
| Nondominant | 19 | 11 | 8 |
| Dominant | 23 | 16 | 7 |
| Bilateral | 4 | 4 | 0 |
Table 3. Level of amputation as a risk factor for psychiatric disease.
| Psychiatric diagnoses | No psychiatric diagnoses | p -Value | OR (95% CI) | |
|---|---|---|---|---|
| Abbreviations: CI, confidence interval; OR, odds ratio. Note: Percentages appear in parenthesis. | ||||
| All amputees | 31 | 15 | ||
| Transhumeral | 6 | 1 | 0.40 | 3.36 (0.37–30.80) |
| Transradial and prox | 16 | 7 | 1.00 | 1.22 (0.35–4.19) |
| Transmetacarpal and prox | 25 | 9 | 0.16 | 2.78 (0.71–10.87) |
Of the 31 patients with a diagnosed psychiatric condition, major depressive disorder (MDD) was the most common ( n = 14), followed by posttraumatic stress disorder (PTSD) ( n = 11), adjustment disorder ( n = 11), anxiety ( n = 6), and panic disorder ( n = 2) ( Fig. 1 ). While 20 patients had only one psychiatric diagnosis, two diagnoses were present in 9 patients and three diagnoses in 2 patients ( Fig. 2 ).
Fig. 1.
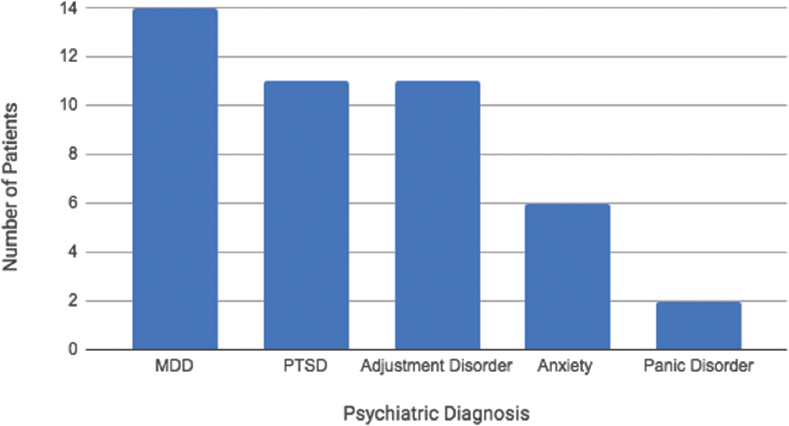
Number of patient with each psychiatric diagnosis. MDD, major depressive disorder, PTST, post traumatic stress disorder.
Fig. 2.
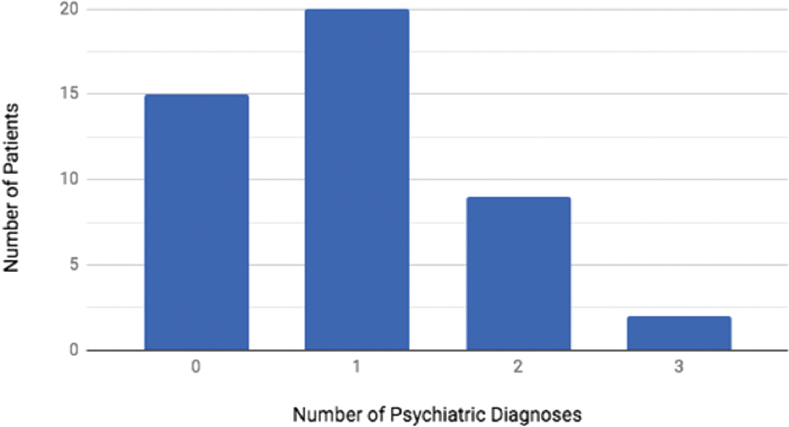
Number of psychiatric diagnoses per patient.
Discussion
The World Health Organization states that a person’s well-being is influenced by physical, psychological, social, emotional, and spiritual factors. All of these factors are negatively impacted by traumatic amputation. After amputation, patients have reported unemployment, socioeconomic difficulties, social avoidance, substance abuse, and change in marital status as a result of their injury or surgery. 10 The early identification of the psychiatric disease after traumatic upper extremity amputation is a critical part of properly treating these patients as it has been shown to impact clinical rehabilitation, prosthesis use, and quality of life. 21 22 Early, short-term psychiatric treatment has also been shown to reduce the incidence of psychiatric morbidity after mixed limb loss from 72.5 to 50%. 23
While previous studies have investigated the prevalence of psychiatric disease after amputation, interpretation of the results is difficult because of the multiple types of screening or diagnostic tools used, the varying time since amputation, variable causes of amputation, and inclusion of both upper and lower extremities amputation. 13 17 18 24 · In the largest study of civilian amputees, Darnall et al screened 913 patients who had undergone upper and lower limb amputations for vascular, oncologic, or traumatic indications and documented severe depressive symptoms in 28.7% of respondents. 15 In a systematic literature review of anxiety and depression after traumatic limb amputation, Mckechnie and John found that meta-analysis was inappropriate because of study heterogeneity due to the various scoring systems used and methods used for diagnosis. 18 However, they reported depression rates of 20.6 to 63% and anxiety in 25.4 to 57%. 18 Another systematic review reported a prevalence of psychiatric disorders in 32 to 84% of amputees, with depression in 10.4 to 63%, PTSD in 3.3 to 56.3%, anxiety in 3.4 to 10%, and phantom limb phenomenon in 14 to 92%. 25
Differentiating the psychological effects after upper or lower limb loss is critical because upper limb loss has been shown to be more devastating to patients than lower limb loss. 3 26 Traumatic upper extremity limb loss patients have worse anxiety and depression scores measured by the Hospital Anxiety and Depression Scale and worse body image disturbance and social discomfort assessed using the Amputation Body Image Scale-Revised and Social Discomfort Score when compared with lower limb loss. 27 Furthermore, patients with upper extremity loss report greater activity restriction and worse prosthetic adjustment. 25 Clinician diagnosed psychiatric conditions are also higher after upper limb loss compared with lower limb loss (53 vs. 47%, respectively) in the immediate postamputation period, and PTSD is significantly more likely after upper extremity limb loss in the military population. 3 28
Although limited, the prevalence of psychiatric disease after isolated traumatic, upper extremity limb loss has been studied in military combatants. In a long-term follow-up of 25 soldiers with isolated unilateral upper extremity limb loss, Ebrahimzadeh et al reported a 32% incidence of PTSD, depression, or difficultly with impulse control. 14 Another study, which used a mailed screening tool, found possible signs of clinical depression in 28.3% and anxiety in 35.5%. 21
In our patient population, we found that the overall rate of psychiatric disease after isolated traumatic upper limb loss is 67.4%. This is in stark contrast to a previously reported prevalence of 17.6% for common mental disorders in the general population. 29 The rate of specific psychiatric diagnoses after injury in our study was: MDD (30.4%), PTSD (23.9%), adjustment disorder (23.9%), anxiety disorder (13.3%), and panic disorder (4.3%). The rate of depression and PTSD seen in this study is similar to that after combat-associated upper extremity amputation. While anxiety was less common in our population, this may be due to the differentiation between “anxiety” and “adjustment disorder with anxiety features.” Direct comparison is also difficult because unlike several previous studies, we did not include phantom limb pain as a psychiatric diagnosis. While previous studies have reported an incidence as high as 86%, phantom limb pain was excluded from our analysis because of debate in the literature whether this represents a normal physiological or abnormal psychological response to limb loss and its impact on depression and anxiety levels is unclear. 6 15 24 30 31 32 33 34
While we did not find a statistically significant association between psychiatric disease and the variables studied, it is important to note that no significant association between psychiatric disease and time from amputation exists. A previous study by Grunert et al evaluated psychological response to work-related hand injury in 170 patients with mixed injuries consisting of amputation, crush injury, and nerve lacerations. 19 Depression was seen in 62.4% of patients within 5 days of injury but improved to 14.1% at 18-month follow-up. Similar findings were seen for anxiety which improved from 48.2 to 5.9%. 19 The improvement in psychiatric symptoms found by Grunert et al’s study may be confounded by the mixed injury pattern of the patients and is not supported by our study or previous studies. 13 17 24 31
There are several limitations to the current study. It is a retrospective study, which limits data interpretation and prevents further patient evaluation utilizing quality of life questionnaires or other patient-reported outcome measures. Despite the relatively large number of patients included in our study, it may lack adequate power to identify statistically significant associated risk factors such as BWC status or bilateral amputations. A strength of our study was that all diagnoses were made by an independent treating psychiatrist or psychologist rather than screening tool or questionnaire. However, not all patients accepted referral for evaluation and treatment. Thus, our findings may actually underreport the true rate of psychiatric conditions in our patient population. Twenty-six of our patients also report prosthetic use which may confound results, as it has previously been shown to reduce symptoms of depression, improve quality of life, and help patients adapt to extremity loss. 35 36 Because of the nature of the study, we are unable to comment on whether patients improved with, or benefited from psychiatric treatment, or whether the rate and/or severity of psychological illness improved over time. We were also unable to examine the timing of development of psychiatric symptoms in relation to the time of injury. Finally, we focused on depression, anxiety, and PTSD as psychiatric diagnoses; other authors have reported additional psychiatric symptoms after amputation including: somatization, anger, interpersonal sensitivity, and sleep disorders that we may have failed to capture based on our study design. 31 Despite these limitations, as a result of our findings, we urge all surgeons to screen all patients with traumatic, upper extremity limb in the civilian population to consider early psychiatric referral.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.Freeland A E, Psonak R. Traumatic below-elbow amputations. Orthopedics. 2007;30(02):120–126. doi: 10.3928/01477447-20070201-16. [DOI] [PubMed] [Google Scholar]
- 2.Saradjian A, Thompson A R, Datta D. The experience of men using an upper limb prosthesis following amputation: positive coping and minimizing feeling different. Disabil Rehabil. 2008;30(11):871–883. doi: 10.1080/09638280701427386. [DOI] [PubMed] [Google Scholar]
- 3.Tennent D J, Wenke J C, Rivera J C, Krueger C A. Characterisation and outcomes of upper extremity amputations. Injury. 2014;45(06):965–969. doi: 10.1016/j.injury.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Dakpa R, Heger H. Prosthetic management and training of adult upper limb amputees. Curr Orthop. 1997;11:193–202. [Google Scholar]
- 5.Brenner C D, Brenner J K. The use of preparatory/evaluation/training prostheses in developing evidenced-based practice in upper limb prosthetics. J Prosthetics Orthot. 2008;20:70–82. [Google Scholar]
- 6.Solomon G F, Schmidt K M. A burning issue. Phantom limb pain and psychological preparation of the patient for amputation. Arch Surg. 1978;113(02):185–186. doi: 10.1001/archsurg.1978.01370140075015. [DOI] [PubMed] [Google Scholar]
- 7.Esquenazi A.Amputation rehabilitation and prosthetic restoration. From surgery to community reintegration Disabil Rehabil 200426(14-15)831–836. [DOI] [PubMed] [Google Scholar]
- 8.Ennion L, Rhoda A. Roles and challenges of the multidisciplinary team involved in prosthetic rehabilitation, in a rural district in South Africa. J Multidiscip Healthc. 2016;9:565–573. doi: 10.2147/JMDH.S116340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhaskaranand K, Bhat A K, Acharya K N. Prosthetic rehabilitation in traumatic upper limb amputees (an Indian perspective) Arch Orthop Trauma Surg. 2003;123(07):363–366. doi: 10.1007/s00402-003-0546-4. [DOI] [PubMed] [Google Scholar]
- 10.Srivastava S, Trivedi J K, Mall C P et al. Psychosocial aspects of amputation. Indian J Psychiatry. 1997;39(03):247–250. [PMC free article] [PubMed] [Google Scholar]
- 11.Bhutani S, Bhutani J, Chhabra A, Uppal R. Living with amputation: anxiety and depression correlates. J Clin Diagn Res. 2016;10(09):RC09–RC12. doi: 10.7860/JCDR/2016/20316.8417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavanagh S R, Shin L M, Karamouz N, Rauch S L. Psychiatric and emotional sequelae of surgical amputation. Psychosomatics. 2006;47(06):459–464. doi: 10.1176/appi.psy.47.6.459. [DOI] [PubMed] [Google Scholar]
- 13.Melcer T, Walker G J, Galarneau M, Belnap B, Konoske P. Midterm health and personnel outcomes of recent combat amputees. Mil Med. 2010;175(03):147–154. doi: 10.7205/milmed-d-09-00120. [DOI] [PubMed] [Google Scholar]
- 14.Ebrahimzadeh M H, Fattahi A S, Nejad A B. Long-term follow-up of Iranian veteran upper extremity amputees from the Iran-Iraq war (1980-1988) J Trauma. 2006;61(04):886–888. doi: 10.1097/01.ta.0000236014.78230.77. [DOI] [PubMed] [Google Scholar]
- 15.Darnall B D, Ephraim P, Wegener S T et al. Depressive symptoms and mental health service utilization among persons with limb loss: results of a national survey. Arch Phys Med Rehabil. 2005;86(04):650–658. doi: 10.1016/j.apmr.2004.10.028. [DOI] [PubMed] [Google Scholar]
- 16.Abeyasinghe N L, de Zoysa P, Bandara K M, Bartholameuz N A, Bandara J M. The prevalence of symptoms of post-traumatic stress disorder among soldiers with amputation of a limb or spinal injury: a report from a rehabilitation centre in Sri Lanka. Psychol Health Med. 2012;17(03):376–381. doi: 10.1080/13548506.2011.608805. [DOI] [PubMed] [Google Scholar]
- 17.Trivedi J K, Mall C P, Mishra U S et al. Psychiatric sequelae of amputation: ii long term effects. Indian J Psychiatry. 1997;39(04):318–323. [PMC free article] [PubMed] [Google Scholar]
- 18.Mckechnie P S, John A. Anxiety and depression following traumatic limb amputation: a systematic review. Injury. 2014;45(12):1859–1866. doi: 10.1016/j.injury.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 19.Grunert B K, Devine C A, Matloub H S et al. Psychological adjustment following work-related hand injury: 18-month follow-up. Ann Plast Surg. 1992;29(06):537–542. doi: 10.1097/00000637-199212000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Gaine W J, Smart C, Bransby-Zachary M. Upper limb traumatic amputees. Review of prosthetic use. J Hand Surg [Br] 1997;22(01):73–76. doi: 10.1016/s0266-7681(97)80023-x. [DOI] [PubMed] [Google Scholar]
- 21.Desmond D M. Coping, affective distress, and psychosocial adjustment among people with traumatic upper limb amputations. J Psychosom Res. 2007;62(01):15–21. doi: 10.1016/j.jpsychores.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 22.Asano M, Rushton P, Miller W C, Deathe B A. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int. 2008;32(02):231–243. doi: 10.1080/03093640802024955. [DOI] [PubMed] [Google Scholar]
- 23.Kashif A W, Walia T S, Salujha S K et al. Effect of short-term psychiatric intervention in amputees. Med J Armed Forces India. 2004;60(03):231–234. doi: 10.1016/S0377-1237(04)80052-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shukla G D, Sahu S C, Tripathi R P, Gupta D K. A psychiatric study of amputees. Br J Psychiatry. 1982;141:50–53. doi: 10.1192/bjp.141.1.50. [DOI] [PubMed] [Google Scholar]
- 25.Sahu A, Sagar R, Sarkar S, Sagar S. Psychological effects of amputation: a review of studies from India. Ind Psychiatry J. 2016;25(01):4–10. doi: 10.4103/0972-6748.196041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beasley R W. General considerations in managing upper limb amputations. Orthop Clin North Am. 1981;12(04):743–749. [PubMed] [Google Scholar]
- 27.Desteli E E, İmren Y, Erdoğan M, Sarısoy G, Coşgun S. Comparison of upper limb amputees and lower limb amputees: a psychosocial perspective. Eur J Trauma Emerg Surg. 2014;40(06):735–739. doi: 10.1007/s00068-014-0418-3. [DOI] [PubMed] [Google Scholar]
- 28.Shukla G D, Sahu S C, Tripathi R P, Gupta D K. Phantom limb: a phenomenological study. Br J Psychiatry. 1982;141:54–58. doi: 10.1192/bjp.141.1.54. [DOI] [PubMed] [Google Scholar]
- 29.Steel Z, Marnane C, Iranpour C et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43(02):476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Desmond D M, MacLachlan M. Affective distress and amputation-related pain among older men with long-term, traumatic limb amputations. J Pain Symptom Manage. 2006;31(04):362–368. doi: 10.1016/j.jpainsymman.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 31.Durmus D, Safaz I, Adıgüzel E et al. The relationship between prosthesis use, phantom pain and psychiatric symptoms in male traumatic limb amputees. Compr Psychiatry. 2015;59:45–53. doi: 10.1016/j.comppsych.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 32.Frazier S H, Kolb L C. Psychiatric aspects of pain and the phantom limb. Orthop Clin North Am. 1970;1(02):481–495. [PubMed] [Google Scholar]
- 33.Katz J, Melzack R. Pain ‘memories’ in phantom limbs: review and clinical observations. Pain. 1990;43(03):319–336. doi: 10.1016/0304-3959(90)90029-D. [DOI] [PubMed] [Google Scholar]
- 34.Parkes C M. Factors determining the persistence of phantom pain in the amputee. J Psychosom Res. 1973;17(02):97–108. doi: 10.1016/0022-3999(73)90010-x. [DOI] [PubMed] [Google Scholar]
- 35.Horgan O, MacLachlan M.Psychosocial adjustment to lower-limb amputation: a review Disabil Rehabil 200426(14-15)837–850. [DOI] [PubMed] [Google Scholar]
- 36.Akarsu S, Tekin L, Safaz I, Göktepe A S, Yazicioğlu K. Quality of life and functionality after lower limb amputations: comparison between uni- vs. bilateral amputee patients. Prosthet Orthot Int. 2013;37(01):9–13. doi: 10.1177/0309364612438795. [DOI] [PubMed] [Google Scholar]


