Abstract
Background
Nationally representative data of cannabis-tobacco co-use have shown these substances are closely entwined and have significant adverse health consequences, though population-level harms of co-use are largely unknown. Current epidemiological research does not assess co-use in a manner that has yielded the necessary data to draw conclusions regarding health effects. This has given rise to a hidden population of co-users who go under-served. Therefore, this paper has two aims: 1) to review new challenges in the collection of co-use data due to rapidly changing regulations of cannabis and nicotine products, and 2) to provide recommendations for the terminology and assessment of co-use.
Argument
We argue that: 1) the prevalence of co-use is not being assessed accurately at a population level and 2) changes in legalisation have created novel challenges, but without proper monitoring, the impact on co-use will go undetected. We propose a three-level tiered set of recommendations for co-use assessments, which includes assessments of cannabis, tobacco, and co-use metrics ranging from least burdensome (self-report of co-administered products) to most burdensome (assays, event-level data).
Conclusions
We propose that clinical studies begin to incorporate cannabis-tobacco co-use assessments to justify better their inclusion in clinical trials and national surveillance surveys. Integration of co-use assessments will aid in understanding the true impact on co-use of the changing cannabis and tobacco/nicotine regulatory environments. Co-use is prevalent and problematic and the ability to make conclusions about its health outcomes is hindered by lack of nuance in data collection. If you don’t measure it, you can’t manage it.
Keywords: Cannabis, Tobacco, Co-use, Legalisation, Vaping, Epidemiology, Population-level Harm, Measurement
Section I: SIGNIFICANCE
Prevalence of cannabis and tobacco use globally
Cannabis and nicotine (mostly consumed through tobacco cigarettes) are two of the world’s most commonly used drugs. There are an estimated 1.3 billion tobacco cigarette smokers and 219 million people who used cannabis in the past year (1, 2). The landscape of cannabis and tobacco/nicotine use has dramatically changed in the past decade because of the growing legalisation of cannabis and changes in availability, safety and acceptability of nicotine through electronic nicotine delivery systems (ENDS; also referred to as vaping). Cannabis is legal for medical use in 33 states within the Unites States (US) and many countries globally. Recreational use is legal in 11 states and 1 district in the US, Canada and Uruguay. Youth in North America live in countries with some of the highest cannabis use rates globally and therefore can be seen as a population-level experiment in action (3). From this experiment, it has become clear that legalisation comes with advancements in product diversity that has increased the ways cannabis can be consumed (4, 5). This is paralleled with the reduction in tobacco use globally (6) although cigarette smoking remains the leading preventable cause of death and disease worldwide (6).
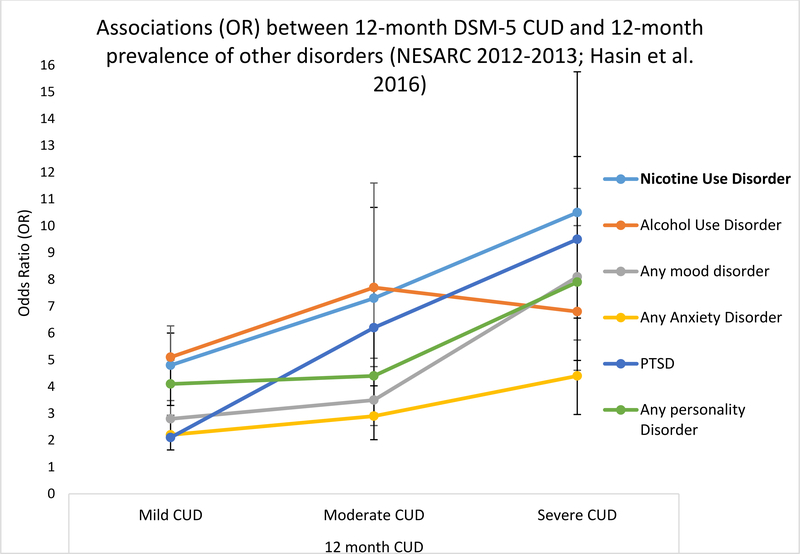
Nationally representative surveillance data used to assess population-level prevalence of cannabis and tobacco/nicotine co-use over time are increasingly important tools as these global changes in legislation and product availability occur. These data have been essential in demonstrating use of cannabis and tobacco is entangled, common and frequent across the lifespan. Cannabis use (and cannabis use disorder [CUD]) is more common amongst tobacco users (7–11) and tobacco use (tobacco/nicotine use disorder [TUD/NUD] is common in cannabis users (12–14). Figure 1 illustrates how the relationship between CUD and NUD becomes stronger with increasing severity of CUD, in comparison to other mood/substance use disorders. In the year preceding recreational cannabis legalisation in Canada, current cigarette smoking was three times more prevalent in cannabis users (38%) than non-users (11%) (15). In the US, 1 in 14 cigarette smokers aged 26+ were daily cannabis users, while 1 in 5 cigarette smokers aged 18–25 were daily cannabis users. In comparison, 1 in 100 never cigarette smokers were daily cannabis users (16). Importantly, co-use is associated with psychiatric, psychosocial and medical harms to its users which have previously been reviewed (17–19).
Figure 1:
The relationship between 12m DSM-5 Nicotine Use Disorder and 12m DSM-5 Cannabis Use Disorder. Data derived from 36,309 participants ≥18 years old who were interviewed in the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC) representative survey 2012–2013. Adjusted for sex, age, race/ethnicity, marital status, education, family income, urban/rural, and region (Midwest, Northeast, South, West). All Odds Ratios are significant p<0.05).
Current definitions of co-use and why they are insufficient
Cannabis-tobacco co-use is an umbrella term, broadly used in the literature to define use of these two substances, within the same person, in a given time frame (see Table 1 for a glossary of terms). This has traditionally been separated into two sub-definitions of:
Concurrent use: Use of both products within a pre-defined time period, but not necessarily simultaneous administration. This definition encompasses all forms of co-use, but without specification e.g. sequential use. Concurrent use is a crude measurement of co-use that does not specify the relationship between substances.
Co-administration: Use of both drugs at the same time, in the same delivery method e.g. blunts or spliffs. This category of co-use appears to be critical to capture as co-administered products are associated with greater risk for consumption to hazardous levels, dependence, and poor cessation outcomes for each substance (20, 21).
Table 1:
Glossary of terms
| Term | Definition |
|---|---|
| Co-use | An umbrella term for the use of cannabis and tobacco within the same individual. |
| Concurrent co-use | The use of both cannabis and tobacco within a pre-specified timeframe (/ever/past year/past month) e.g. Past month cannabis users and past month tobacco users. |
| Sequential co-use | A specific form of concurrent use. When one substance is used shortly after another, suggesting a relationship on subjective drug effects or impact on craving (also referred to as chasing). |
| Co-administration | Use of cannabis and tobacco at the same time, and specifically within the same delivery method e.g. in a blunt or a spliff (see below). Also referred to as simultaneous use/combined use/mixing. |
| Blunt | Hollowed out cigar wrappers, made of tobacco and therefore containing nicotine, filled with cannabis (and sometimes some of the tobacco from inside the cigar). Can also be rolled using little cigars or cigarillos. Brands include ‘Swisher sweets’ or ‘Backwoods’ |
| Spliff | Cannabis and loose leaf tobacco rolled together in a rolling paper. Also known as mulled cigarettes. |
| Joint | A culturally-specific term. In the US, this terms refers to cannabis rolled in a rolling paper and smoked. However, in the UK, this term is synonymous with “spliff”. |
| Dry-herb Vaporiser | Cannabis flowers are heated (i.e. not combusted) to aerosolize the active compounds either via direct contact (conduction) or by heating the air around the cannabis (convection). These can also come with drip pads so liquids/oils/concentrates can also be vaporized. Brands include ‘Pax’ (portable) and ‘Volcano’ (non-portable). |
| Electronic Nicotine Delivery System (ENDS) | Non-combusted nicotine delivered via an e-liquid that is aerosolized and directly inhaled via a hand-held portable device. ENDS are also known as e-cigarettes or vape pens. Brands for nicotine include JUUL, NJOY, Blu, SMOK, Vype. Product visual dictionary available (42). ENDS can also be used to deliver cannabis (THC, CBD), flavorings, chemicals, and other substances such as cannabis concentrates (i.e. potent and refined forms of cannabis e.g. shatter, butane hash oil) and these are called “dab” pens. |
| Vaping | Using a battery-powered heating component that converts e-liquid into aerosol. The term “vaping” conflates cannabis vaping and nicotine vaping (53, 54). No clear definition of the term “vaping” exists. |
Making the distinction between concurrent and co-administering user groups is important because it affects prevalence rates in epidemiological studies in several ways. Firstly, co-administration significantly contributes to the prevalence and negative health effects of co-use. Nationally representative data from the US suggest that co-administration conflates the basic co-use statistic (e.g. number of past month cannabis users who were past-month tobacco users) by 10% when accounting for blunts, without also considering other co-administration methods (12, 22–24). Secondly, there are also cross-cultural differences in co-administration. Tobacco-based routes of cannabis administration are popular in Europe (77–91%) and Australasia (21–52%) but uncommon in the Americas (4–16%). (13). Thirdly, question structure has a significant effect on prevalence because cannabis users (not reporting tobacco use) and tobacco users (not reporting cannabis use) are often not questioned further about co-administered methods (such as blunts), leading to misclassification (25, 26). However, not all users may be aware that blunts/spliffs contain nicotine (27, 28). Fourthly, many individuals fall into both concurrent and co-administration user groups (e.g. using spliffs and cigarettes). This potentially represents a new level of risk that is not represented and is often unaccounted. Finally, they do not properly account for non-daily, intermittent smokers, a group of smokers increasingly becoming daily cannabis users. The number of intermittent smokers who were daily cannabis users increased by 23%, whilst decreasing 18.5% among non-cannabis users, and 19% among non-daily cannabis users between 2002–2015 (14). Notably, it is highly unusual to see an increase in smoking in any population given globally declining rates of smoking. Increased cannabis use among tobacco users, needs to specifically be considered because it can easily be hidden amongst the greater declining statistic (29).
Given tobacco is a strong contributor to global morbidity, mortality and healthcare costs, even small increases in tobacco consumption can increase its population-level harms. As suggested by Caulkins, et al. (30), a 1% increase/decrease in tobacco smoking could lead to nearly 500 more/fewer tobacco-related deaths per year.
A hidden population of co-users
When co-use is accurately assessed, longitudinal representative data show important trends in young people. Firstly, it suggests that young people (12–17 years old) in the US are more likely to be co-users (5.4%) than exclusive cannabis (3.9%), or tobacco (2.2%), users with 9 in 10 young people using blunts within the past month (25). Amongst 18–24 year olds, only 1% reported exclusive cannabis use without alcohol or tobacco between 2011–2015 (31). Moreover, between 2005–2014, there was no significant change in co-use prevalence, whilst cannabis use doubled and tobacco use halved in the same ten year period (25), suggesting tobacco use is not decreasing amongst co-users. This implies co-users are a difficult-to-reach population who may not consider themselves tobacco users. This absence of reduction suggests interventions to reduce tobacco smoking in young people appear to only be impacting tobacco-only users and may not be reaching youth at risk for, or who are already engaging in, co-use.
Additionally, there is hidden tobacco exposure amongst non-smokers who use cannabis (8, 9). Nationally representative data from Europe show that smoking spliffs is common among non-cigarette smokers (76.5%). Sixty-seven percent of these spliff users classified themselves as non-smokers even though they always reported co-administering cannabis and tobacco, exposing themselves to nicotine. This suggests that self-identified “non-smokers” are being exposed to the negative effects of tobacco.
Improved assessment of co-use
Co-use is a term frequently used to encompass a broad range of drug use behaviours that exist on an (undefined) continuum of harm. We argue the prevalence of co-use is not being assessed accurately at a population level, meaning the population-level harm associated with co-use is currently unknown. Further, the ability to draw conclusions about the health outcomes of co-use is hindered by variation in terminology. This Addiction Debate has two aims; 1) to review new challenges in the collection and study of co-use that have emerged due to rapidly changing legislation of cannabis and tobacco/nicotine product diversity, and 2) to provide recommendations for the terminology and assessment of co-use to inform the literature and better capture a hidden population of co-users.
Section II: NEW CHALLENGES FOR CO-USE
Effects of medical and recreational cannabis laws on co-use
The issue of how macro-level cannabis laws influence population-level use of cannabis and other drugs is important because legalisation has already been associated with increases in cannabis use, CUD (3, 32, 33), the development of new products, reductions in price and increases in potency (33). However, some suggest the overall health effects of cannabis legalisation will be shaped by what happens to the consumption of tobacco and other substances (34). If a primary public health goal is to reduce tobacco use in the population, it is essential to determine how legalising cannabis affects the prevalence of drugs commonly used with cannabis. It is unclear whether legalisation will lead to an increase or decrease in co-use and associated disease burden of these two drugs and whether this will be via substitution or complimentary effects.
In Table S1, we review the recent literature evaluating the effects of cannabis legalisation on cannabis and tobacco use and co-use with nationally representative data (n=6). Apart from in adolescents (35), cannabis use appears to be increasing concurrent with cannabis legalisation (36–39); whilst tobacco use rates do not show a consistent pattern. Tobacco use rates were either not collected or evaluated, though two studies found a decrease in tobacco use resulting from cannabis legalisation (36, 37). In the three studies that assessed concurrent co-use (37–39), tobacco use rates appear to be greater in legal vs. illegal cannabis states, whilst only one study has assessed co-administration but only amongst cigarette smokers (39), where no consistent pattern emerges. This preliminary literature on the impact of cannabis legalisation on cannabis and tobacco use patterns does not allow for definitive conclusions to be drawn regarding any harmful or beneficial impact of legalisation and may be a function of policy transition effects (32). The conclusion from this literature is that even in studies interested in co-use patterns, the data available to answer those questions may not be sufficient or granular enough.
Growing popularity of vaporizers for the administration of cannabis and tobacco
The products available for the consumption of cannabis and nicotine are moving away from traditional combustible formats and data suggests they are starting to overlap at a potentially larger rate than smoked cannabis and tobacco. Independently, both cannabis and nicotine vaping (Table 1) have been increasing among young adults (40, 41). Whilst nicotine vaping is more common, devices are now available that can be used for either drug (42).
There is confusion about different terminology used in this area, which leads to conflation of statistics capturing vaping. Cannabis vaping can occur via several forms and products are constantly evolving (42). Currently, the level of cannabis vaping may be under-represented in national surveys as those who vape cannabis are being mischaracterised as nicotine only users (43), with some research finding misclassification was more likely in the US data, followed by Canada and the UK (43). Efforts are being made towards building an ontology of vaping which will aid the delineation of cannabis versus nicotine vaping (44).
Misclassification and unregulated cannabis vaping products has serious implications; 68 deaths have been attributed to the e-cigarette or vaping product use associated lung injury (EVALI) outbreak in the US in 2019 (45). EVALI cases were initially thought to be a result of nicotine vaping, as it coincided with large increases in youth vaping. However, it was then identified to be a result of vitamin e-acetate (an additive) in cannabinoid fluids sold in the illicit, unregulated market (46, 47).
The nationally representative literature is growing on the topic of co-use with respect to the use of ENDS and cannabis vaping (Table S2). Here, we summarize recent studies (n=10) in the categories of; 1) the prevalence of co-using ENDS and cannabis, 2) the associations and predictors of the initiation of co-use and severity, and 3) the patterns of co-use specific to vaping nicotine and/or cannabis. Previous meta-analyses (not included in our review of the literature here) have shown the odds of cannabis use were higher in youth who had used ENDS versus those who did not (AOR, 3.4 [95%CI, 2.6–4.6]) and this was greater in those in the 12–17 age category than the 18–24 category (48).
Table S2 suggests the odds of ENDS and cannabis vaping co-use seem to be greater amongst those who are male, live in a household where cigarette smoking or ENDS were common or living in a state with medical/recreational cannabis policies. The literature suggests co-use of ENDS and cannabis is common in the US, whilst studies have minimally reported extent of use and dependence, it is known from the combustible literature that using cannabis and tobacco together increases risk of dependence to both substances and can cause harm (21, 49). All studies summarized in Table S2 presented data on co-use, though only two presented data on co-administration, and a third presented data on blunts, but not other forms of co-administration (spliffs). This preliminary literature demonstrates the high rate of use of multiple vaping products for cannabis and nicotine, and its association with combustible cannabis and tobacco leading to both poly-tobacco and poly-cannabis methods. Survey data should aim to provide precise and clear terminology to gain accurate assessments of vaporiser co-use.
Section III: TOWARDS THE ACCURATE COLLECTION OF CO-USE DATA
Co-use assessment recommendations
While we acknowledge there is added burden to implementing assessments of co-use, we argue some modification must be made to pay greater attention to a hidden population of co-users, particularly given the challenges highlighted above regarding the rapidly changing cannabis and tobacco/nicotine environment and potential downstream effects on co-use. As such, we propose a tiered set of recommendations for domains of co-use, which includes recommendations for cannabis and tobacco exclusively. Some separate cannabis and tobacco use metrics can be used to inform co-use metrics, but this is not sufficient to adequately capture the nuance of co-use patterns. Importantly, validated measures for the assessment of co-use do not currently exist with most research groups using their own methods. Whilst we do not endorse any particular measure as part of these recommendations, we support harmonisation of assessments and measures as much as possible (e.g. by using common assessment batteries, such as the PhenX toolkit (https://www.phenxtoolkit.org/)), though several others are widely available. The authors are also involved in developing ‘The International Cannabis Toolkit’, a standardized, internationally-relevant tool for measuring cannabis use (https://canntoolkit.com/). We provide three levels of domains to assess (Table 2), ranging from the least amount of data required (Level 1) to the most intensive, burdensome, and costly assessment of cannabis, tobacco, and co-use metrics (Level 3).
Table 2:
Co-Use domain recommendations
| Level 1: Minimal burden to incorporate elements into data sets. Recommend the collection of multiple types of co-use; not just concurrent use, but also co-administration and sequential use. The goal of Level 1 assessments is to sufficiently capture those with varying patterns of co-use, with minimal added burden. | ||
| Cannabis metrics | Tobacco/nicotine metrics | Co-Use metrics |
| • Consumption metrics of cannabis (methods of use) • Frequency (days of use, times used per day, amount used per day) Timeframe: Ever (metrics collected when using) and past 12 months |
• Consumption metrics of tobacco/nicotine use • Frequency (daily, near-daily, weekly, monthly) • Quantity of use (cigs/day, vaping episodes per day) Timeframe: Ever (metrics collected when using) and past 12 months |
• Consumption metrics of co-administered products (blunts, spliffs) • Frequency of co-administered products • Patterns of co-use (sequential use, concurrent use) and temporal relations in use Assessment of concurrent co-use may also be derived from exclusive cannabis and tobacco metrics Timeframe: Ever and past 12 months |
| Level 2: Additional domains recommended to capture patterns of co-use, products used, and levels of dependence, quantity, frequency. This level allows for the assessment of associations between cannabis and tobacco use among co-users and should occur in addition to Level 1. | ||
| Cannabis metrics | Tobacco/nicotine metrics | Co-Use metrics |
| • Cannabis use methods: Combustible (joint/pipe/bong), vaporizer (dry herb/oil), edibles, dabbing/concentrates CBD • Potency: % THC, ratio of THC: CBD, strength of product • Dependence levels Timeframe: Past 12 months and past month |
• Tobacco/nicotine use detailed methods: ENDS, smokeless, hookah • ENDS characteristics: nicotine concentration, flavors, type of device used • Dependence levels Timeframe: Past 12 months and past month |
• Subjective effects of co-use • Substitution of products (during quit attempts, reduction, situations where one product cannot be used) • Changes in craving Timeframe: Past 12 months and past month |
| Level 3: Most comprehensive level and includes all measures from Levels 1 and 2, but also includes biochemical testing to determine levels of use for both tobacco/nicotine and cannabis, as well as toxicant exposure. | ||
| Cannabis metrics | Tobacco/nicotine metrics | Co-Use metrics |
| • Biochemical Assays: Biological samples to indicate use of substances (quantitative, if possible) • THC: 11-OH-THC, THC-COOH • CBD: 11-OH-CBD, CBD-COOH Timeframe: Subject to specific assays and times of detection |
• Biochemical Assays: Biological samples to indicate use of substances (quantitative, if possible) • Cotinine • Total nicotine • Toxicant exposure Timeframe: Subject to specific assays and times of detection |
• Event-level data: Ecologically-valid measures of co-use patterns (temporal relationships, impact on craving, substitution) • Relatedness: Assessment to capture the degree of relatedness (subjective effects, craving, shared triggers). Low relatedness suggests substances are used at different times; do not interfere with craving for the other substance and have few shared triggers. Timeframe: Past month |
Challenges in collecting co-use data
Co-use assessment recommendations are made here with acknowledgement of the challenges associated with additional data collection. Nationally representative surveys and surveillance must undertake the arduous task of piloting question comprehension and relevance, which may take years and incorporating questions must be done carefully and judiciously. Assessments are more easily incorporated into clinical research studies, therefore, we recommend that this step be incorporated immediately and broadly in data collection efforts among studies of tobacco or cannabis users within study data collection. Specific to smoking cessation trials, measures of cannabis use should be included, particularly when using breath carbon monoxide (CO) as a biochemical measure of smoking. Cannabis will confound breath CO readings, even among those who have quit using combustible tobacco products. Co-use data from clinical research can then be used to justify inclusion in population surveys and decide which data to collect in those surveys.
Incorporation of additional assessments can be time-intensive, costly, and not the primary outcome, all of which contribute to the limited capacity to collect these data. However, as we have argued, co-users are an often overlooked population who may experience increased harms, making accurate collection of this information essential.
Section IV: DISCUSSION AND CONCLUSIONS
In this Addiction Debate we have outlined the complicated nature of cannabis tobacco co-use with the aim of highlighting population-level prevalence and harms which are suspected to be greater than use of either substance alone, though current epidemiological research and surveillance does not account for this sufficiently. Thus, to date, co-use has not been assessed in a way that has yielded the necessary data to draw conclusions regarding adverse health effects, so population-level harms are therefore unknown. Further, data will be insufficient to fully capture the impact of a rapidly changing regulatory environment for cannabis and product diversity for tobacco/nicotine on co-use prevalence and patterns. Future studies should consider the potential that cannabis users are being exposed to tobacco/nicotine through joints/blunts and via vaping but might not identify as nicotine users in a national, household survey. Those who are co-administering are potentially at the greatest risk for dependence but are a hidden population. We argue that national survey methodology should allow for tobacco users not reporting cannabis use, and cannabis users not reporting tobacco use, to respond to questions about co-administration. In order to improve the accurate collection of co-use data, we recommend a minimum set of data elements (Table 2) be included in clinical research studies, national surveys, and more broadly as part of health screeners administered in clinical care settings. Moreover, screening, treatment services, physicians and healthcare providers should remain vigilant in identifying co-users and attempt to provide treatment for both substances.
Both legalisation of cannabis and the changing product landscape used for consuming both drugs indicate that there is an urgent need to understand how these products are being used to support the co-use of both substances. Whilst previously it was thought vaping cannabis might be an effective harm reduction strategy to move away from combustible tobacco use (13, 50, 51), current epidemiology suggests use of cannabis and tobacco/nicotine overlap, and this will likely have negative addiction-related outcomes, especially in young people (52). Current measures in nationally representative population-data are inadequate to monitor these changes given insufficient capture and a lack of nuance in the data collection of co-administration and concurrent co-use. How will we be able to detect public health impacts on co-use if the measures are insufficient? If you don’t measure it, you can’t manage it.
Supplementary Material
Acknowledgements:
The authors would like to thank Tom Freeman for his helpful review on a previous version of this manuscript. C.H is supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre. E.A.M is supported by funding from the National Institutes of Health (NCI R37 CA237245, PI). The authors received no specific funding for the development of this article.
Footnotes
Declaration of interests: None.
References
- 1.UNODC. World Drug Report 2019, United Nations publication, Sales No. E.19.XI.8; 2019. [Google Scholar]
- 2.WHO. Tobacco, https://www.who.int/news-room/fact-sheets/detail/tobacco: World Health Organization; 2020. [Google Scholar]
- 3.Hasin DS , Shmulewitz D , Sarvet AL Time trends in US cannabis use and cannabis use disorders overall and by sociodemographic subgroups: a narrative review and new findings, The American Journal of Drug and Alcohol Abuse 2019: 45: 623–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smart R , Caulkins JP , Kilmer B , Davenport S , Midgette G Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state, Addiction (Abingdon, England) 2017: 112: 2167–2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borodovsky JT , Budney AJ Legal cannabis laws, home cultivation, and use of edible cannabis products: A growing relationship?, Int J Drug Policy 2017: 50: 102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015, Lancet 2017: 389: 1885–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodwin RD , Pacek LR , Copeland J , Moeller SJ , Dierker L , Weinberger A et al. Trends in Daily Cannabis Use Among Cigarette Smokers: United States, 2002–2014, American Journal of Public Health 2017: e1–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fix BV , Smith D , O’Connor R , Heckman BW , Willemsen MC , Cummings M et al. Cannabis use among a nationally representative cross-sectional sample of smokers and non-smokers in the Netherlands: results from the 2015 ITC Netherlands Gold Magic Survey, BMJ Open 2019: 9: E024497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith DM , Miller C , O’Connor RJ , Kozlowski LT , Wadsworth E , Fix BV et al. Modes of delivery in concurrent nicotine and cannabis use (“co-use”) among youth: Findings from the International Tobacco Control (ITC) Survey, Substance Abuse 2020: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh T , Kennedy SM , Sharapova SS , Schauer GL , Rolle I V . Modes of ever marijuana use among adult tobacco users and non-tobacco users—Styles2014, Journal of Substance Use 2016: 21: 631–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinberger AH , Pacek LR , Wall MM , Zvolensky MJ , Copeland J , Galea S et al. Trends in cannabis use disorder by cigarette smoking status in the United States, 2002–2016, Drug and Alcohol Dependence 2018: 191: 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schauer GL , Berg CJ , Kegler MC , Donovan DM , Windle M Differences in tobacco product use among past month adult marijuana users and nonusers: findings from the 2003–2012 National Survey on Drug Use and Health, Nicotine & Tobacco Research 2016: 18: 281–288. [DOI] [PubMed] [Google Scholar]
- 13.Hindocha C , Freeman TP , Ferris JA , Lynskey MT , Winstock AR No Smoke without Tobacco: A Global Overview of Cannabis and Tobacco Routes of Administration and Their Association with Intention to Quit, Frontiers in Psychiatry 2016: 7: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pacek LR , Copeland J , Dierker L , Cunningham CO , Martins SS , Goodwin RD Among whom is cigarette smoking declining in the United States? The impact of cannabis use status, 2002–2015, Drug and Alcohol Dependence 2018: 191: 355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Statistics Canada. Canadian Tobacco, Alcohol and Drugs Survey, 2017. In: StanCan, editor. The Daily, https://www150.statcan.gc.ca/n1/daily-quotidien/181030/dq181030b-eng.htm; 2018. [Google Scholar]
- 16.Goodwin RD , Pacek LR , Copeland J , Moeller SJ , Dierker L , Weinberger A et al. Trends in Daily Cannabis Use Among Cigarette Smokers: United States, 2002–2014, American Journal of Public Health 2018: 108: 137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McClure EA , Rabin RA , Lee DC , Hindocha C Treatment Implications Associated with Cannabis and Tobacco Co-Use, Current Addiction Reports; In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peters EN , Schwartz RP , Wang S , O’Grady KE , Blanco C Psychiatric, psychosocial, and physical health correlates of co-occurring cannabis use disorders and nicotine dependence, Drug Alcohol Depend 2014: 134: 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meier E , Hatsukami DK A review of the additive health risk of cannabis and tobacco co-use, Drug Alcohol Depend 2016: 166: 6–12. [DOI] [PubMed] [Google Scholar]
- 20.Agrawal A , Lynskey MT , Madden PA , Pergadia ML , Bucholz KK , Heath AC Simultaneous cannabis and tobacco use and cannabis-related outcomes in young women, Drug and alcohol dependence 2009: 101: 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agrawal A , Budney AJ , Lynskey MT The co‐occurring use and misuse of cannabis and tobacco: a review, Addiction 2012: 107: 1221–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schauer GL , Rosenberry ZR , Peters EN Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review, Addictive Behaviors 2017: 64: 200–211. [DOI] [PubMed] [Google Scholar]
- 23.Schauer GL , King BA , McAfee TA Prevalence, correlates, and trends in tobacco use and cessation among current, former, and never adult marijuana users with a history of tobacco use, 2005–2014, Addict Behav 2017: 73: 165–171. [DOI] [PubMed] [Google Scholar]
- 24.Schauer GL , Berg CJ , Kegler MC , Donovan DM , Windle M Assessing the overlap between tobacco and marijuana: Trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012, Addict Behav 2015: 49: 26–32. [DOI] [PubMed] [Google Scholar]
- 25.Schauer GL , Peters EN Correlates and trends in youth co-use of marijuana and tobacco in the United States, 2005–2014, Drug and Alcohol Dependence 2018: 185: 238–244. [DOI] [PubMed] [Google Scholar]
- 26.Delnevo CD , Bover-Manderski MT , Hrywna M Cigar, marijuana, and blunt use among US adolescents: Are we accurately estimating the prevalence of cigar smoking among youth?, Preventive medicine 2011: 52: 475–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peters EN , Schauer GL , Rosenberry ZR , Pickworth WB Does marijuana “blunt” smoking contribute to nicotine exposure?: Preliminary product testing of nicotine content in wrappers of cigars commonly used for blunt smoking, Drug Alcohol Depend 2016: 168: 119–122. [DOI] [PubMed] [Google Scholar]
- 28.Timberlake DS , Haberstick BC , Hopfer CJ , Bricker J , Sakai JT , Lessem JM et al. Progression from marijuana use to daily smoking and nicotine dependence in a national sample of US adolescents, 2007: 88: 272–281. [DOI] [PubMed] [Google Scholar]
- 29.Smart R , Pacula RL Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: Findings from state policy evaluations, The American journal of drug and alcohol abuse 2019: 45: 644–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caulkins JP , Kilmer B , Kleimann AR Marijuana Legalization: What Everyone Needs to Know: Oxford: University Press; 2001. [Google Scholar]
- 31.Cohn AM , Johnson AL , Rath JM , Villanti AC Patterns of the co-use of alcohol, marijuana, and emerging tobacco products in a national sample of young adults, The American Journal on Addictions 2016: 25: 634–640. [DOI] [PubMed] [Google Scholar]
- 32.Fischer B , Lee A , O’Keefe-Markman C , Hall W Initial indicators of the public health impacts of non-medical cannabis legalization in Canada, EClinicalMedicine 2020: 20: 100294–100294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hall W , Lynskey M Assessing the public health impacts of legalizing recreational cannabis use: the US experience, World Psychiatry 2020: 19: 179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caulkins JP , Kilmer B , Kleiman MA Marijuana legalization: what everyone needs to know. New York: Oxford University Press; 2016. [Google Scholar]
- 35.Cerdá M , Sarvet AL , Wall M , Feng T , Keyes KM , Galea S et al. Medical marijuana laws and adolescent use of marijuana and other substances: Alcohol, cigarettes, prescription drugs, and other illicit drugs, Drug Alcohol Depend 2018: 183: 62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi A , Dave D , Sabia JJ Smoke gets in your eyes: medical marijuana laws and tobacco cigarette use, American Journal of Health Economics 2019: 5: 303–333. [Google Scholar]
- 37.Wang JB , Ramo DE , Lisha NE , Cataldo JK Medical marijuana legalization and cigarette and marijuana co-use in adolescents and adults, Drug Alcohol Depend 2016: 166: 32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang JB , Cataldo JK Medical Marijuana Legalization and Co-use in Adult Cigarette Smokers, Am J Health Behav 2016: 40: 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gravely S , Driezen P , Smith DM , Borland R , Lindblom EN , Hammond D et al. International differences in patterns of cannabis use among adult cigarette smokers: Findings from the 2018 ITC Four Country Smoking and Vaping Survey, Int J Drug Policy 2020: 79: 102754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miech RA , Patrick ME , O’Malley PM , Johnston LD , Bachman JG Trends in Reported Marijuana Vaping Among US Adolescents, 2017–2019, Jama 2020: 323: 475–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cullen KA , Gentzke AS , Sawdey MD , Chang JT , Anic GM , Wang TW et al. e-Cigarette Use Among Youth in the United States, 2019, Jama 2019: 322: 2095–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.CDC. E-Cigarette, or Vaping, products visual dictionary, https://www.cdc.gov/tobacco/basic_information/e-cigarettes/pdfs/ecigarette-or-vaping-products-visual-dictionary-508.pdf; 2020.
- 43.Fataar F , Hammond D The Prevalence of Vaping and Smoking as Modes of Delivery for Nicotine and Cannabis among Youth in Canada, England and the United States, International Journal of Environmental Research and Public Health 2019: 16: 4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cox S , Hastings J , West R , Notley C The case for development of an E-cigarette Ontology (E-CigO) to improve quality, efficiency and clarity in the conduct and interpretation of research, Qeios 2020: [pre-print]. [Google Scholar]
- 45.CDC. Outbreak of Lung Injury Associated with the Use of E-Cigarette, or Vaping, Products, https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html: Centers for Disease Control and Prevention; 2020.
- 46.Duffy B , Li L , Lu S , Durocher L , Dittmar M , Delaney-Baldwin E et al. Analysis of Cannabinoid-Containing Fluids in Illicit Vaping Cartridges Recovered from Pulmonary Injury Patients: Identification of Vitamin E Acetate as a Major Diluent, Toxics 2020: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hall W , Gartner C , Bonevski B Lessons from the public health responses to the US outbreak of vaping-related lung injury, Addiction: n/a. [DOI] [PubMed] [Google Scholar]
- 48.Chadi N , Schroeder R , Jensen JW , Levy S Association Between Electronic Cigarette Use and Marijuana Use Among Adolescents and Young Adults: A Systematic Review and Meta-analysis, JAMA Pediatrics 2019: 173: e192574–e192574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peters EN , Budney AJ , Carroll KM Clinical correlates of co‐occurring cannabis and tobacco use: A systematic review, Addiction 2012: 107: 1404–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lynskey MT , Hindocha C , Freeman TP Legal regulated markets have the potential to reduce population levels of harm associated with cannabis use, Addiction 2016: 111: 2091–2092. [DOI] [PubMed] [Google Scholar]
- 51.Hindocha C , Freeman TP , Winstock AR , Lynskey MT Vaping cannabis (marijuana) has the potential to reduce tobacco smoking in cannabis users, Addiction 2016: 111: 375–375. [DOI] [PubMed] [Google Scholar]
- 52.Budney AJ , Sargent JD , Lee DC Vaping cannabis (marijuana): parallel concerns to e-cigs?, Addiction 2015: 110: 1699–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pearson JL , Reed DM , Villanti AC Vapes, E-cigs, and Mods: What Do Young Adults Call E-cigarettes?, Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco 2020: 22: 848–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pearson JL , Villanti AC It Is Past Time to Consider Cannabis in Vaping Research, Nicotine & Tobacco Research 2020: 22: 597–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.