Abstract
People living with HIV (PLWH) have a higher risk of experiencing sexual assault. Prior studies have shown independent associations between sexual assault, depression and ART adherence. However, research analyzing the potential mediating effects of depressive symptoms between sexual assault and ART adherence, and the associated age and sex disparities, especially among PLWH in the Southern United States, is lacking. Therefore, the current study sought to determine whether depressive symptoms mediate the association between sexual assault and ART adherence and to evaluate the associated age and sex disparities among PLWH in South Carolina. Data were collected from 337 individuals who received HIV care from an immunology center in South Carolina. Crude and adjusted path analysis models stratified by age and sex were used to determine the association between sexual assault, depressive symptoms and ART adherence. Depressive symptoms were associated with ART adherence among adults aged 18–34 (β=−0.281, p=0.018) and 35–49 (β=−0.185, p=0.005), and men (β=−0.205, p=0.011). Sexual assault was associated with depressive symptoms (β=0.211, p=0.001) and with ART adherence (β=−0.172, p=0.010) among adults 35–49. Among men (β=−0.238; p=0.029) and women (β=−0.344, p=0.001), sexual assault was associated with ART adherence; and among women, sexual assault with depressive symptoms (β=0.280, p=0.006). Depressive symptoms mediated the association between sexual assault and ART adherence among adults 35–49 (β=−0.039, p=0.035). Interventions addressing depressive symptoms may improve ART adherence among adults aged 18–34, 35–49 and men. Programs also addressing depressive symptoms and using trauma-informed approaches may improve ART adherence especially among middle-aged populations, men, and women.
Keywords: sexual assault, ART adherence, depression, men, women
Introduction
HIV continues to be a public health challenge globally and in the United States (US) (World Health Organization, 2019; Centers for Control Disease and Prevention, 2018b). The World Health Organization (WHO) estimates that approximately 37.9 million people were living with HIV in 2018 globally (World Health Organization, 2020). According to the Centers for Disease Control and Prevention (CDC), there were 1.7 million new cases of HIV worldwide in 2018, with 37,832 of these occurring in the US (Centers for Disease Control and Prevention, 2020). However, the number of new HIV diagnoses in the US decreased 9% from 2010 to 2016 in the US (Centers for Disease Control and Prevention, 2020).
The distribution of HIV incidence varies by region through the US. The CDC indicates that the new HIV diagnosis rates (per 100,000 population) were 10.6, 9.4, and 7.4 in the Northeast, the West, and the Midwest in 2017, respectively, while the rate remained highest in the South at 16.1 (Centers for Control Disease and Prevention, 2018b). South Carolina, like other rural Southern states, bears a disproportionate HIV burden (Department of Health and Environmental Control, 2019). In 2017, there were 19,749 people living with HIV (PLWH), and the incidence rate was 15.8 per 100,000 residents (Department of Health and Environmental Control, 2019). HIV also affects various demographic groups disproportionately. In 2017, disparities by age and sex existed among PLWH in South Carolina (Department of Health and Environmental Control, 2019). Men and middle-aged adults have higher HIV prevalence and incidence rates compared to women and other age groups, respectively (Department of Health and Environmental Control, 2019). For example, in 2017, it was estimated that 14,066 men and 5,683 women were living with HIV in South Carolina, and there were 1,239 and 346 new diagnoses among men and women, respectively (Department of Health and Environmental Control, 2019). With regards to age differences, approximately one in five PLWH were between 30 and 39 years old, and an additional 50% were 50 years of age and older (Department of Health and Environmental Control, 2019).
Antiretroviral Therapy Adherence
Antiretroviral therapy (ART) adherence is critical for PLWH to achieve and maintain viral suppression. Despite universal recommendations for ART initiation immediately after diagnosis or as soon as possible (Office of AIDS Research Advisory Council, 2018), only 59% of PLWH across the globe were receiving ART in 2017 (World Health Organization, 2019). Strong evidence exists that high ART adherence (at least 90%−95%) can improve the immunologic, virologic, and clinical conditions of PLWH (Mugavero et al., 2006). In the US, HIV treatment cascade outcomes continue to be subpar, with only 63% of PLWH receiving HIV medical care, 49% remaining engaged in HIV care, and 51% of PLWH achieving viral suppression in 2015 (Centers for Disease Control and Prevention, 2019). Age and sex disparities are also observed in ART adherence in the US (Beer & Skarbinski, 2014; Simoni et al., 2012). People aged 18–39 years and women have been found to be less likely to be adherent to ART compared to people aged 50 years and older, and men, respectively (Beer & Skarbinski, 2014). The Southern US also experiences low rates of ART adherence. In 2017, only 53% of PLWH in South Carolina were retained in continuous HIV care, and 57% of PLWH achieved viral suppression (Department of Health and Environmental Control, 2019). The proportion of those who remained engaged in care and were virally suppressed were similar for men and women (52% vs. 56% and 56% vs. 58%, respectively) (Department of Health and Environmental Control, 2019). Understanding the potential mediating role of depression between sexual assault and ART adherence and the relationship among relevant subgroups can aid in designing effective interventions to improve ART adherence among key populations living with HIV in the US.
Sexual Assault, Depression and ART Adherence
While some studies have studied sexual assault among people living with HIV (Brown et al., 2017; Draughon, 2012; Pyra et al., 2014), to our knowledge, few studies have examined the relationship between sexual assault and ART adherence among PLWH. Cohen et al. (2004) reported that women living with HIV across six clinical sites in New York, Illinois, Washington, DC, and California who had physical or sexual abuse histories were less likely to be on ART (Cohen et al., 2004). While the reasons behind this association were not examined, authors speculated that an inability to trust medical providers may have led women to decline ART. Another study found no significant association between childhood sexual abuse and ART adherence among Latino men who have sex with men (MSM) living with HIV in Texas (Sauceda, Wiebe, & Simoni, 2016).
Sexual assault has also been shown to be associated with depression among PLWH. Sauceda et al. (2016) found that childhood sexual abuse is associated with greater self-reported depressive symptoms in Latino MSM (Sauceda et al., 2016). Indeed, a systematic review and meta-analysis found a statistically significant association between sexual abuse and a lifetime diagnosis of depression where those with a sexual abuse history were almost three times as likely to have depression (Chen et al., 2010). Depression, in turn, may be associated with lower ART adherence (Reisner et al., 2009; DiMatteo, Lepper, & Croghan, 2000; Sauceda et al., 2016; Yu et al., 2018). A systematic review and meta-analysis found that PLWH with depressive symptoms were 42% less likely to have good adherence compared to PLWH without depressive symptoms (Uthman, Magidson, Safren, & Nachega, 2014). Among people living with HIV with histories of childhood sexual abuse, lower ART adherence was associated with trauma symptoms and lower social support (Meade, Hansen, Kochman, & Sikkema, 2009). Number of lifetime traumatic events was also a risk factor for lower ART adherence among people living with HIV from five southern states: AL, GA, LA, NC and SC (Mugavero et al., 2009). Depression was found to lower prevention benefits of ART among populations living with HIV in Uganda (Wagner, Slaughter, & Ghosh-Dastidar, 2017).
Theoretical Model
Schnurr and Green (2004) established a theoretical model examining the association between trauma and health. This model suggested that traumatic exposure may be linked to mental health disorders, including PTSD, as well as poor psychosocial functioning. As such, this model may help to explain a depressive mediation pathway between sexual assault and ART adherence. As a form of trauma, sexual assault may lead to greater depressive symptoms (e.g., persistent sadness, hopelessness, fatigue, sleep problems) that increase the risk for poor adherence to ART.
Potential Confounders
Data from a large, nationally representative sample of US adults indicated that individuals from racial and ethnic minority groups, including Black, Asian and Hispanic populations, were less likely to have experienced sexual assault than White populations (Roberts, Gilman, Breslau, Breslau, & Koenen, 2011). However, Cohen et al. did not find this association to be statistically significant (M. Cohen et al., 2000). Studies have also found that race is associated with ART adherence among PLWH in the US (Pence, 2008; Simoni et al., 2012). One study found that PLWH from minority racial and ethnic groups were quicker to discontinue ART and experience virologic failure than non-minority PLWH in the Southeastern US (Pence, 2008). Low educational attainment (i.e., <12 years of formal schooling) was also associated with higher non-adherence to ART among African-American adults (Kalichman, 1999). Similarly, income has also been shown to be positively associated with ART adherence in multiple US studies (Atukunda et al., 2017; McCoy, Waldrop-Valverde, Balderson, Mahoney, & Catz, 2016). However, Mugavero et al., did not find a statistically significant association between income, education and nonadherence among PLWH in the Southern US (Mugavero et al., 2006). Based on these findings, potential confounders of the relationship between sexual assault, depressive symptoms, and ART adherence may include race, ethnicity, education, and income.
Potential Differences by Sex and Age
Depression’s potential mediating effect on the relationship between sexual assault and ART adherence may vary by sex and age. Turner et al. found that women had lower ART adherence than men and were more likely to be diagnosed with depression (Turner, 2003). However, Remien et al., did not find any statistically significant differences in ART adherence among women and men from urban populations in the US, despite differences in sexual orientation (Remien et al., 2014). Wilson et al. found that psychological distress was associated with lower ART adherence, and this relationship was stronger among women compared to men (Wilson, Sikkema, & Ranby, 2014). To our knowledge, no previous study has examined the associations between sexual assault, depressive symptoms, and ART adherence by age. However, research has consistently shown an association between age and adherence, with younger individuals more likely to be non-adherent to ART than older individuals (Gordillo, del Amo, Soriano, & Gonzalez-Lahoz, 1999; Hinkin et al., 2004). Due to these differences, it is possible that there may be age and sex disparities in the mediation pathway between sexual assault, depressive symptoms and ART adherence among PLWH.
Rationale and Study Aims
To date, no study could be identified that has examined the potential mediating role of depression in the association between sexual assault and ART adherence among PLWH in the Southern US where the burden of HIV-related mortality and morbidity is highest (Centers for Control Disease and Prevention, 2018a) and ART adherence is lowest (Department of Health and Environmental Control, 2019). In addition, it is important to determine if sex and/or age differences exist in these associations. Therefore, the current study fills these gaps in the literature. The aims of this study were to: 1) Examine the potential mediating role of depressive symptoms in the association between sexual assault and ART adherence among PLWH in South Carolina; and 2) Assess age and sex differences in the potential mediating role of depressive symptoms between sexual assault and ART adherence. We hypothesized that depressive symptoms would mediate the association between sexual assault and ART adherence among women and men, and among individuals aged 18 to 34, 35 to 49, and 50 and older. The findings will help to determine focal points and specific groups that will benefit from ART adherence interventions.
Methods
Data Source and Study Population
Data were collected from 402 PLWH receiving care from a large immunology center in South Carolina with a cross-sectional survey that was administered from May to September 2018. To be eligible, participants had to be over 18 years old, living with HIV, and willing to participate in the 30–40 minute survey. Participants provided data on psychosocial and behavioral factors and self-reported clinical outcomes (held for review).
The research team and the clinic staff coordinated with each other in the data collection process. Patients living with HIV and receiving care in the clinic were introduced to the study by clinic staff. Those who were willing to participate in the study were directly led to members of the research team, who invited them to take part in the survey. Participation was high with over 80% of patients who were initially approached agreeing to participate. Participants who engaged in the study provided informed consent and received a $20 gift card for their participation. Since the main outcome of the current study was ART adherence, 65 participants who reported not being on ART were excluded from the analysis. Therefore, the final sample size was 337 (215 men and 115 women). The (held for review) Institutional Review Board approved the study protocol.
Measures
Sexual Assault
Sexual assault was measured by two items in the Life Events Checklist (LEC) (Blake et al., 1995). Participants were instructed to indicate whether they had ever experienced “sexual assault (e.g., rape, attempted rape, made to perform any type of sexual act through force or threat of harm)” and any “other unwanted or uncomfortable sexual experience”. Participants were provided six response options: Happened to me, Witnessed it, Learned about it, Part of my job, Not Sure, and Doesn’t Apply. Participants’ responses to both questions were dichotomized to operationalize the direct experience of sexual assault (i.e., Happened to me or Part of my job vs. all other responses).
Depressive Symptoms
Depressive symptoms were measured by the Patient Health Questionnaire–9 (PHQ-9) (Kroenke, Spitzer, & Williams., 2001). The PHQ-9 is a 9-item module from the full Patient Health Questionnaire (PHQ), which assesses eight diagnoses including depressive disorder, panic disorder, binge eating disorder among others (Kroenke, Spitzer, & Williams., 2001). An example of the PHQ-9 items is “How often have you been bothered by feeling down, depressed, or hopeless?” Response options in the PHQ-9 were based on a four-point Likert-type scale response option ranging from Not at all (1) to Nearly every day (4). Sum scores were obtained by summing responses to the nine items with higher scores indicated greater depressive symptoms. The standardized Cronbach’s alpha values for the PHQ-9 were 0.91 overall, 0.90 for men, and 0.93 for women, 0.91 for participants aged 18–34, 0.92 for those aged 35–49, and 0.91 for those aged 50 and older.
ART Adherence
ART adherence was measured by the question: “How often do you miss a dose of ART medication over a typical month?” with response options ranging from Never miss (1) to At least 6 days (5). ART adherence was operationalized as a binary variable reporting 100% adherence (i.e., Never miss) vs. <100% adherence to account for the tendency of individuals to overestimate their ART adherence (Biello et al., 2016). Nevertheless, self-reported ART adherence has been shown to reflect antiretroviral concentration in biomarkers (Zhang et al., 2020).
Subgroups
Sex was operationalized by the question “What sex were you assigned at birth” with response options: male, female, other. Age was calculated using the participant’s date of birth.
Confounders
Prior research has shown that a number of sociodemographic characteristics are associated with sexual assault and ART adherence (Atukunda et al., 2017; Cohen et al., 2000; Kalichman, 1999; McCoy et al., 2016; Mugavero et al., 2006; Pence, 2008; Roberts et al., 2011; Simoni et al., 2012). However, these characteristics are not in the direct pathway between sexual assault and ART adherence. Therefore, the potential confounders considered in the current study for subgroup analyses included race, ethnicity, education, and income. The overall model adjusted for age, sex, race, ethnicity, education, and income. Confounders were modeled as direct predictors of depression and ART adherence (Figure 1).
Figure 1.
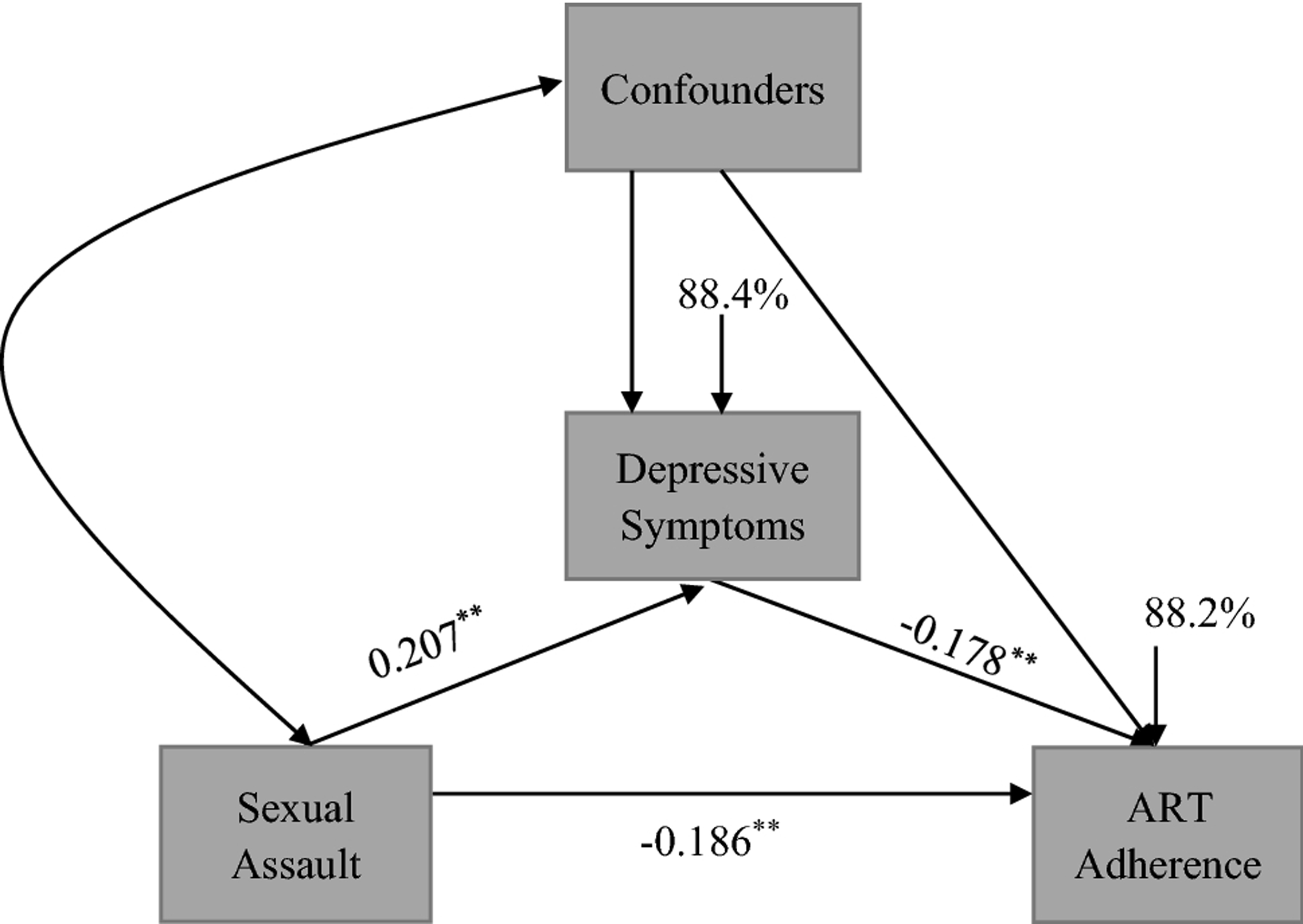
Mediation Diagram between Sexual Assault, Depressive Symptoms and ART Adherence among Overall Sample.
Note: **p<0.01, *p<0.05
Values for proportion of variance explained are shown in percentages.
Analytic Approach
Descriptive statistics were used to assess the distribution of sociodemographic characteristics of the participants and prevalence of sexual assault. Chi-square tests were used to examine group differences. Path analyses were conducted to determine the direct and indirect effects between sexual assault, depressive symptoms, and ART adherence in the overall study population. Crude and adjusted models were stratified by age (18–34, 35–49, 50+) and sex (men and women). Adjusted models controlled for race, ethnicity, education and income. Models stratified by age additionally adjusted for sex, and models stratified by sex additionally adjusted for age. In path analysis, ten observations are needed for each variable in a regression model (excluding the outcome) (Wilson van Voorhis & Morgan, 2007). Adjustment for five variables suggest that 60 observations will be needed for each group. There were 111 women, 215 men, 95 people aged 18 to 34, 114 aged 35 to 49, and 119 aged 50 and older. (Based on doing 5 subgroup analyses, the number of false positives would be 0.25.) Descriptive analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC) and path analyses were conducted in Mplus version 8 (Muthén & Muthén, Los Angeles, CA). Fit indices were examined to determine model fit: comparative fit index (CFI); Tucker Lewis index (TLI); standardized root mean square residual (SRMR); root mean square error of approximation (RMSEA); and χ2 test of model fit. The estimation method used in Mplus was the WLSMV estimator.
Results
Distribution of Sociodemographic Characteristics, Depressive Symptoms and ART Adherence
Table 1 shows the distribution of sociodemographic characteristics and experience of sexual assault among PLWH. Statistically significant differences by sex were found with a higher percent of women reporting sexual assault vs. no sexual assault (46% vs. 30%) and a higher percent of men reporting no sexual assault vs. sexual assault (70% vs. 54%). There were no statistically significant differences in reporting sexual assault by other sociodemographic characteristics. However, the mean [SD] value of depressive symptoms was higher among participants who reported sexual assault compared to those who did not report sexual assault (7.3 [6.9] vs. 4.5 [5.5]) with a range from 0 to 27. One in five (19.6%) participants met screening criteria for being moderately, moderately severe, or severely depressed (PHQ-9 ≥ 10) (data not shown). ART adherence also differed by reports of sexual assault where a lower percent of participants who reported sexual assault were 100% adherent compared to participants who did not report sexual assault (39% vs. 53%).
Table 1.
Distribution of Sociodemographic Characteristics and Experiencing Sexual Assault among People Living with HIV
| Characteristic | Overall N (%) | Sexual Assault N (%) | No Sexual Assault N (%) | P-valuea |
|---|---|---|---|---|
| Sex | 0.006 | |||
| Female | 111 (34.0) | 40 (46.0) | 71 (29.7) | |
| Male | 215 (66.0) | 47 (54.0) | 168 (70.3) | |
| Age (Mean, [SD]) | 44.3 [13.8] | 42.7 [14.7] | 44.9 [13.4] | 0.230b |
| 18–34 | 95 (29.0) | 31 (34.1) | 64 (27.0) | 0.402 |
| 35–49 | 114 (34.7) | 31 (34.1) | 83 (35.0) | |
| 50+ | 119 (36.3) | 29 (31.8) | 90 (38.0) | |
| Race | 0.556 | |||
| Black | 258 (76.8) | 72 (78.3) | 186 (76.2) | |
| White | 61 (18.1) | 14 (15.2) | 47 (19.3) | |
| Other | 17 (5.1) | 6 (6.5) | 11 (4.5) | |
| Ethnicity | 0.762 | |||
| Hispanic | 12 (4.3) | 4 (4.8) | 8 (4.0) | |
| Non-Hispanic | 270 (95.7) | 76 (95.2) | 191 (96.0) | |
| Education | 0.761 | |||
| Less than high school | 34 (12.2) | 9 (12.3) | 25 (12.1) | |
| High school | 83 (29.7) | 20 (27.4) | 63 (30.6) | |
| Some college | 101 (36.2) | 30 (41.1) | 71 (34.4) | |
| Bachelor’s/post graduate | 61 (21.9) | 14 (19.2) | 47 (22.8) | |
| Employment | 0.550 | |||
| Employed | 149 (53.8) | 42 (56.8) | 107 (52.7) | |
| Unemployed | 128 (46.2) | 32 (43.2) | 96 (47.3) | |
| Income | 0.209 | |||
| <$10,000 | 108 (33.6) | 37 (41.1) | 71 (30.7) | |
| $10,000 to $49,000 | 172 (53.6) | 43 (47.8) | 129 (55.8) | |
| $50,000+ | 41 (12.8) | 10 (11.1) | 31 (13.4) | |
| Time since diagnosis | 0.796 | |||
| ≤ 5 years | 92 (28.4) | 23 (26.1) | 69 (29.2) | |
| < 5 years to ≤ 10 years | 81 (25.0) | 21 (23.9) | 60 (25.4) | |
| >10 years to ≤ 20 years | 83 (25.6) | 26 (29.5) | 57 (24.2) | |
| >20 years | 68 (21.0) | 18 (20.5) | 50 (21.2) | |
| Depressive symptoms (Mean, [SD]) | 5.3 [6.0] | 7.3 [6.9] | 4.5 [5.5] | < 0.001b |
| ART Adherence | 0.027 | |||
| 100% Adherent | 165 (49.0) | 36 (39.1) | 129 (52.7) | |
| <100% Adherent | 172 (51.0) | 56 (60.9) | 116 (47.4) |
Bolded p-values are statistically significant at p<0.05.
P-values are based on the Chi-square statistic.
P-value is based on the Welch’s Anova.
Standardized Direct Estimates between Sexual Assault, Depressive Symptoms, and ART Adherence
Table 2 shows the direct standardized estimates between sexual assault, depressive symptoms and ART adherence among PLWH for the overall sample, by age, and by sex. After adjusting for age, sex, race, education and income, sexual assault was positively associated with depressive symptoms (β=0.207, p=0.002) and negatively associated with ART adherence (β=−0.186, p=0.006). Depressive symptoms were also negatively associated with ART adherence (β=−0.178, p=0.009).
Table 2.
Direct Standardized Estimates between Sexual Assault, Depressive Symptoms and ART Adherence among People Living with HIV
| Sexual Assault → Depressive Symptoms | Depressive Symptoms → ART Adherence | Sexual Assault → ART Adherence | ||||
|---|---|---|---|---|---|---|
| Crude β | p-value | Crude β | p-value | Crude β | p-value | |
| Overall | 0.209 | <0.001 | −0.167 | 0.002 | −0.086 | 0.116 |
| 18–34 | 0.137 | 0.155 | −0.215 | 0.023 | −0.045 | 0.644 |
| 35–49 | 0.209 | <0.001 | −0.167 | 0.002 | −0.086 | 0.116 |
| 50+ | 0.230 | 0.008 | −0.048 | 0.605 | −0.111 | 0.234 |
| Men | 0.140 | 0.032 | −0.190 | 0.003 | −0.026 | 0.698 |
| Women | 0.209 | <0.001 | −0.167 | 0.002 | −0.086 | 0.116 |
| Adjusted βa | p-value | Adjusted βa | p-value | Adjusted β | p-value | |
| Overall | 0.207 | 0.002 | −0.178 | 0.009 | −0.186 | 0.006 |
| 18–34 | 0.113 | 0.310 | −0.281 | 0.018 | −0.180 | 0.110 |
| 35–49 | 0.211 | 0.001 | −0.185 | 0.005 | −0.172 | 0.010 |
| 50+ | 0.181 | 0.116 | −0.126 | 0.248 | −0.238 | 0.029 |
| Men | 0.085 | 0.284 | −0.205 | 0.011 | −0.139 | 0.076 |
| Women | 0.280 | 0.006 | −0.056 | 0.621 | −0.344 | 0.001 |
Bolded coefficients and p-values are statistically significant at p<0.05
Overall adjusted estimates controlled for age, sex, race, ethnicity, education and income; Models stratified by age controlled for sex, race, ethnicity, education and income; Models stratified by sex controlled for age, race, ethnicity, education and income
After adjusting for sex, race, education and income, sexual assault was positively associated with depressive symptoms (β=0.211, p=0.001) and negatively associated with ART adherence (β=−0.172, p=0.010) among adults aged 35 to 49. Depressive symptoms were significantly and negatively associated with ART adherence among adults ages 18 to 34 (β=−0.281, p=0.018) and 35 to 49 (β=−0.185, p=0.005). Among older adults, sexual assault was negatively associated with ART adherence (β=−0.238, p=0.029).
After adjusting for age, race, education and income, depressive symptoms were significantly and negatively associated with ART adherence among men (β=−0.205, p=0.011). This association was not statistically significant among women. However, sexual assault was positively associated with depressive symptoms (β=0.280, p=0.006) and negatively associated among ART adherence (β=−0.344, p=0.001) among women.
Standardized Indirect Estimates and Mediation Pathways between Sexual Assault, Depressive Symptoms and ART Adherence
With regards to standardized indirect estimates, the mediation pathway between sexual assault, depressive symptoms and ART adherence was statistically significant among the overall study population (β=−0.037, p=0.044). This statistically significant association was mainly driven by adults aged 35 to 49 (β=−0.039, p=0.035). This pathway did not attain statistical significance among men, women, or other age groups.
Figures 1 to 3 show the adjusted mediation pathways between sexual assault, depressive symptoms and ART adherence among the overall sample, those aged 18 to 34, 35 to 49, 50 and older, and men and women, respectively. Examination of the absolute fit indices for each mediation model showed good model fit: CFI > 0.98; TLI > 0.98; SRMR < 0.05; RMSEA < 0.06; and χ2 test of model fit p-value <0.05.
Figure 3.
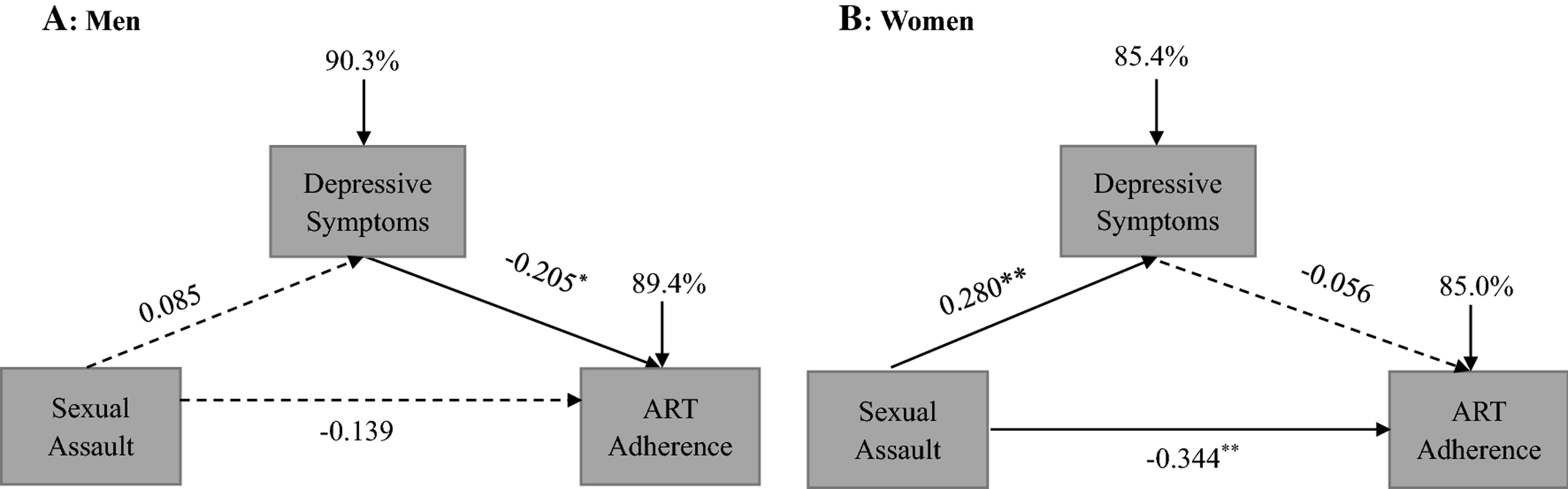
Mediation diagram between sexual assault, depressive symptoms and art adherence among men and women. Note: *p < .05. Solid arrows ( ) indicate statistical significance at p < .05. Dashed arrows ( ) indicate non-statistical significance at p < .05. Values for proportion of variance explained are shown in percentages.
Discussion
To the best of our knowledge, this is the first study to examine the mediation pathways between sexual assault, depressive symptoms, and ART adherence, as well as associated disparities by age and sex among PLWH. The main findings were that PLWH aged 35–49 years, 50 and older, and women living with HIV who experienced sexual assault were less likely to report ART adherence. Depressive symptoms acted as a mediator between sexual assault and ART adherence among PLWH aged 35 to 49 years.
Depressive Symptoms among the Study Population
The mean values of depressive symptoms among participants who reported sexual assault were higher compared to participants who did not report sexual assault. However, the mean scores were in the mild range (5–9) of depression severity based on the PHQ-9 (Kroenke & Spitzer, 2002). However, 20% of the population reported symptoms of at least moderate depression severity. This prevalence is similar to other estimates of depression among other populations living with HIV ranging from 20–28% among populations in London, UK and urban populations in the US (Bengtson et al., 2017; McGowan et al., 2018), but lower than that seen among midwestern US clinic populations (81%) (Lopez, Shacham, & Brown, 2018). These findings suggest that depression should be screened for in HIV care and depression treatment should be a priority component in HIV care so as to improve physical, physiological and mental well-being among populations living with HIV.
Sexual Assault and Depressive Symptoms
The current study found a statistically significant association between sexual assault and depressive symptoms among middle-aged participants. Prior research has shown that there were associations between sexual assault and depressive symptoms among middle-aged adults (i.e., median ages between 30–49 years), though there were age nuances (Levine et al., 2018; Sauceda et al., 2016; Tsai et al., 2016). This age group slightly differs from the operationalization of middle age used in the current study (i.e., ages 35–49). However, we did not find a statistically significant association between sexual assault and depressive symptoms among older adults (aged 50 years or older) living with HIV. Nevertheless, one previous study (Kamiya, Timonen, & Kenny, 2016) revealed a statistically significant association between childhood sexual assault and depression among older adults. The potential reason for these differences in findings may be due to differences in primary variables and study populations. The current study was conducted among PLWH in South Carolina while the study by Kamiya et al. was among Irish adults aged 50 and older with no specification about HIV serostatus. The current study did not differentiate between sexual assault experienced as a minor versus that experienced as an adult while Kamiya et al. assessed childhood abuse. The methods used to operationalize depressive symptoms were also different. Kamiya et al., used the 20-item Center for Epidemiological Studies Depression scale (CES-D), while the current study assessed used the PHQ-9 to assess depressive symptoms.
The current study found statistical significance and a lack thereof in the association between sexual assault and depressive symptoms among women and men living with HIV, respectively. Previous research has also shown a stronger association between history of childhood sexual abuse and depressive symptoms among men compared to women (Brown et al., 2017). Two prior studies also showed a statistically significant association between childhood sexual abuse and depression among Latino MSM (Levine et al., 2018; Sauceda et al., 2016). However, Tsai et al. (Tsai et al., 2016) found that sexual victimization was associated with greater depression among women living with HIV in rural Uganda. Nevertheless, the differences in study populations and the assessment of childhood sexual abuse by Brown et al., Sauceda et al., and Levine et al., rather than lifetime sexual assault may have explained the differences in findings.
Depressive Symptoms and ART Adherence
Depressive symptoms were negatively associated with ART adherence in the overall sample, and specifically for people aged 18 to 34 and 35 to 49, and among men. Our findings support previous research, which found that PLWH who were nonadherent to ART were three times more depressed compared to PLWH who were adherent to their ART (Gebrezgabher et al., 2017). However, this association was not statistically significant among older adults and women in the current study. This finding both contradicts and supports previous research (Lipira et al., 2018; Turan et al., 2019). Prior studies have shown conflicting findings showing an association between depression and ART adherence (Turan et al., 2019), and a lack thereof (Lipira et al., 2018) among women living with HIV. The differences in findings with the Turan et al. study could have been due to differences in study design (cross-sectional vs. longitudinal), or the ways the primary measures were operationalized. In the current study, we examined adherence as 100% vs. less than 100% to account for overreporting of adherence while Turan et al. dichotomized adherence at 95% vs. less than 95%. Depression was measured by the PHQ-9 in the current study while measured by the CES-D Scale in the Turan et al. study. Lipira et al., did not find a statistically significant association between depression and ART adherence among Black women living with HIV. They measured depressive symptoms with the PHQ-8, an abridged version of the PHQ-9, and operationalized ART adherence as the number of days in the past 30 days in which women missed at least one dose of their ART. One explanation for the similar findings between the current study and Lipira et al. could be the similarity in study populations as majority of women (80.2%) in our study were Black women.
Sexual Assault and ART Adherence
The current study also found that sexual assault was negatively associated with ART adherence, especially among adults aged 35–49, 50 and older, and women. Our findings support results from Cohen et al. who found that women living with HIV who had experienced any physical or sexual abuse were less likely to be on ART compared to women who had no history of abuse (Cohen et al., 2004). The finding that sexual assault was not associated with ART adherence among men corresponded with Sauceda’s findings (Sauceda et al., 2016). However, according to our knowledge, no previous research has assessed the association between sexual assault and ART adherence by age among PLWH. One important implication of our findings is that even though older adults are more likely to adhere to ART compared to younger adults (Beer & Skarbinski, 2014), middle aged and older adults who have experienced sexual trauma are less likely to adhere to treatment compared to their counterparts who have not been exposed to sexual assault. Therefore, trauma-informed approaches geared toward improving ART adherence are also warranted for middle-aged and older adults living with HIV.
Mediation of Depressive Symptoms between Sexual Assault and ART Adherence
The mediation pathway between sexual assault, depressive symptoms and ART adherence was statistically significant among middle-aged PLWH, 35 to 49 years of age. This pathway was not statistically significant for other groups but was marginally statistically significant for young PLWH. The model by Schnurr and Green (2004) implies that exposure to traumatic events can lead to mental health challenges, which affect psychosocial functioning. Based on the findings from the current study, additional research is needed to determine if this model applies specifically to middle-aged PLWH with regards to these primary variables. These findings also suggest that intervention programs aimed at improving ART adherence may benefit middle-aged PLWH who are in care, if they simultaneously address depressive symptoms and a history of sexual assault.
Limitations and Strengths
There are some limitations to be considered when interpreting the findings from the current study. The study design was cross-sectional so causality cannot be determined from the results. Within the causal framework, the temporal order, which is assumed in path models, is a critical limitation. Adherence was measured through self-report and so adherence may be overreported. Nevertheless, ART adherence was operationalized in an attempt to account for overreporting of ART adherence. However, the effect estimates of pathways including ART adherence that were obtained may be underestimates of the “true” association. Depressive symptoms were also based on self-report and were not confirmed through clinical interviews. Nevertheless, we were able to use clinical cut-off values to estimate the prevalence of depression in the study population. Subgroup analyses are also a limitation (Wang & Ware, 2013). Nevertheless, we had sufficient power for each subgroup analysis conducted.
Strengths of the current study were that adjusted analyses controlled for sociodemographic characteristics, which may alter the associations in the mediation pathway. Depressive symptoms were measured as a continuous variable, which helps to prevent loss of power in analyses.
Conclusions
PLWH are at higher risk than the general population for experiencing sexual assault, and sexual violence is increasingly recognized as an important driver of the HIV epidemic. This study represents an important step in examining the disparities in age and sex in examining psychosocial pathways and relationships involving sexual trauma, depressive symptoms and adherence to ART. The findings also highlight the importance of integrating trauma-informed care approaches in HIV care and also that the design of these approaches must consider age and sex differences. Future studies should examine the qualitative nuances of these age and sex differences in the effects of sexual trauma and the way they may affect HIV treatment outcomes. Alternative mediation pathways should also be considered in future research. For example, sexual assault was associated with lower ART adherence among people 50 and older, and women, but depressive symptoms did not statistically significantly mediate this association among these populations. Future studies may look at the role of PTSD and substance use as potential mediators in the association between sexual assault and ART adherence. Future research should also assess these relationships specifically among other populations that are disproportionately affected by HIV and sexual trauma such as MSM and transgender women.
Supplementary Material
Figure 2.
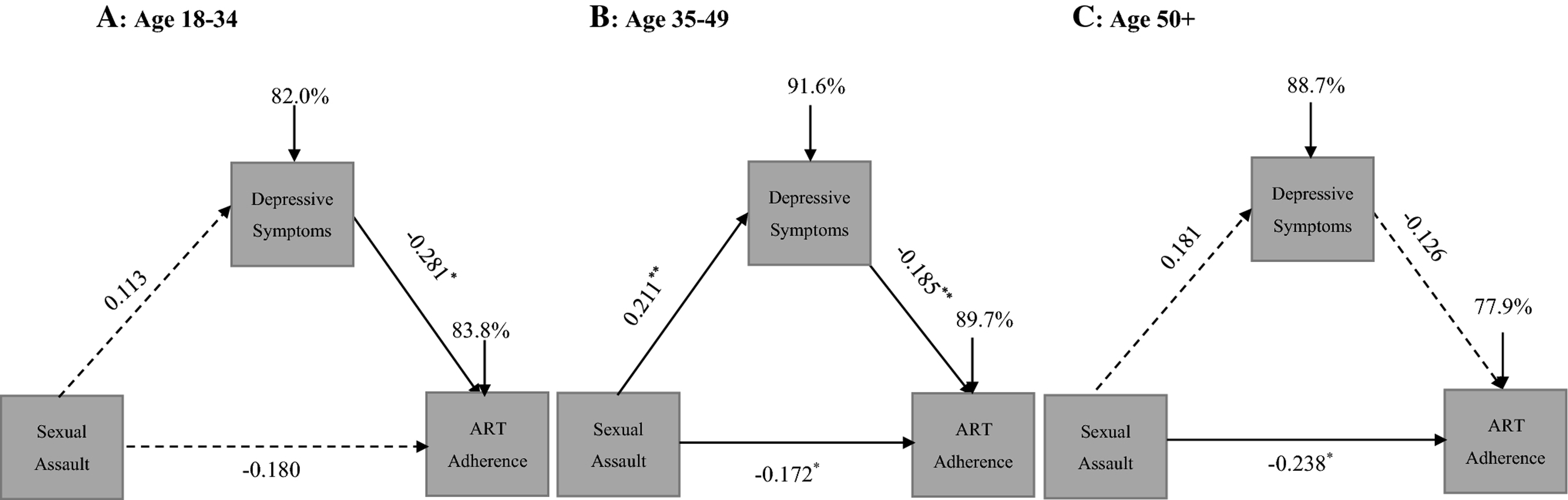
Mediation Diagram between Sexual Assault, Depressive Symptoms and ART Adherence among Adults by Age Group
Note: **p<0.01, *p<0.05
Solid arrows ( ) indicate statistical significance at p<0.05.
Dashed arrows (→ indicate non-statistical significance at p<0.05.
Proportions of variance explained are shown in percentages.
Table 3.
Indirect Standardized Estimates Between Sexual Assault, Depressive Symptoms and ART Adherence among People Living with HIV
| Crude β | p-value | |
|---|---|---|
| Overall | −0.035 | 0.015 |
| 18–34 | −0.029 | 0.230 |
| 35–49 | −0.035 | 0.015 |
| 50+ | −0.011 | 0.612 |
| Men | −0.027 | 0.085 |
| Women | −0.035 | 0.015 |
| Adjusted βa | p-value | |
| Overall | −0.037 | 0.044 |
| 18–34 | −0.032 | 0.351 |
| 35–49 | −0.039 | 0.035 |
| 50+ | −0.023 | 0.353 |
| Men | −0.017 | 0.324 |
| Women | −0.016 | 0.627 |
Bolded p-values are statistically significant at p<0.05
Overall adjusted estimates controlled for age, sex, race, ethnicity, education and income; Age-moderated models controlled for sex, race, ethnicity, education and income; Sex-moderated models controlled for age, race, ethnicity, education and income
Acknowledgements:
We would like to thank the following individuals who coordinated and participated in survey instrument development and data collection: Joi Anderson, Amir Bhochhibhoya, Akeen Hamilton, LaDrea Ingram, and Crystal Stafford as well as the administrative staff of the immunology clinic where this study was conducted. Finally, we are deeply grateful for the willingness of study participants to share their time and experiences with us. We take seriously our commitment to use study findings to improve outcomes for people living with HIV in South Carolina and recognize that this work could not be done without their participation and contributions.
Funding: This study was funded by the South Carolina SmartState Program®. M. J. Brown is supported by grant K01MH115794 from the National Institute of Mental Health. S. Harrison is supported by grant K01MH118073. The sponsors had no role in the design, analysis or decision to publish these findings. The content is solely the responsibility of the authors and does not necessarily represent the official views of the South Carolina SmartState Program® or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Atukunda EC, Musiimenta A, Musinguzi N, Wyatt MA, Ashaba J, Ware NC, & Haberer JE (2017). Understanding patterns of social support and their relationship to an art adherence intervention among adults in rural southwestern Uganda. AIDS and Behavior, 21(2), 428–440. doi: 10.1007/s10461-016-1559-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beer L, & Skarbinski J. (2014). Adherence to antiretroviral therapy among HIV-infected adults in the United States. AIDS Education and Prevention, 26(6), 521–537. doi: 10.1521/aeap.2014.26.6.521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtson AM, Pence BW, Moore R, Mimiaga MJ, Mathews WC, Heine A, . . . Mugavero MJ (2017). Relationship between ever reporting depressive symptoms and all-cause mortality in a cohort of HIV-infected adults in routine care. AIDS, 31(7), 1009–1016. doi: 10.1097/qad.0000000000001431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biello KB, Oldenburg CE, Safren SA, Rosenberger JG, Novak DS, Mayer KH, & Mimiaga MJ (2016). Multiple syndemic psychosocial factors are associated with reduced engagement in HIV care among a multinational, online sample of HIV-infected MSM in Latin America. AIDS Care, 28Suppl 1, 84–91. doi: 10.1080/09540121.2016.1146205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8, 75–90. [DOI] [PubMed] [Google Scholar]
- Brown MJ, Harrison SE, & Li X. (2019). Gender disparities in traumatic life experiences and antiretroviral therapy adherence among people living with HIV in South Carolina. AIDS and Behavior, 23, 2904–2915. doi: 10.1007/s10461-019-02440-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown MJ, Masho SW, Perera RA, Mezuk B, Pugsley RA, & Cohen SA (2017). Sex disparities in adverse childhood experiences and HIV/STIs: Mediation of psychopathology and sexual behaviors. AIDS and Behavior, 21(6), 1550–1566. doi: 10.1007/s10461-016-1553-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, (2018a). HIV in the Southern United States. CDC Issue Brief. Retrieved from https://www.cdc.gov/hiv/pdf/policies/cdc-hiv-in-the-south-issue-brief.pdf
- Centers for Disease Control and Prevention, (2018b). HIV/AIDS: HIV in the United States by Region. Retrieved from https://www.cdc.gov/hiv/statistics/overview/geographicdistribution.html
- Centers for Disease Control and Prevention, (2020). HIV/AIDS: Statistics Overview. Retrieved from https://www.cdc.gov/hiv/statistics/overview/index.html
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, . . . Zirakzadeh A. (2010). Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clinic Proceedings, 85(7), 618–629. doi: 10.4065/mcp.2009.0583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen M, Deamant C, Barkan S, Richardson J, Young M, Holman S, . . . Melnick S. (2000). Domestic violence and childhood sexual abuse in HIV-infected women and women at risk for HIV. American Journal of Public Health, 90, 560–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MH, Cook JA, Grey D, Young M, Hanau LH, Tien P, . . . Wilson TE (2004). Medically eligible women who do not use HAART: the importance of abuse, drug use, and race. American Journal of Public Health , 94(7), 1147–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR, Lepper HS, & Croghan TW (2000). Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Archives of Internal Medicine, 160, 2101–2107. [DOI] [PubMed] [Google Scholar]
- Draughon JE (2012). Sexual assault injuries and increased risk of HIV transmission. Advanced Emergency Nursing Journal, 34(1), 82–87. doi: 10.1097/TME.0b013e3182439e1a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebrezgabher BB, Kebede Y, Kindie M, Tetemke D, Abay M, & Gelaw YA (2017). Determinants to antiretroviral treatment non-adherence among adult HIV/AIDS patients in northern Ethiopia. AIDS Research and Therapy, 14(1). doi: 10.1186/s12981-017-0143-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordillo V, del Amo J, Soriano V, & Gonzalez-Lahoz J. (1999). Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS, 13(13), 1763–1769. [DOI] [PubMed] [Google Scholar]
- Hinkin CH, Hardy DJ, Mason KI, Castellon SA, Durvasula RS, Lam MN, & Stefaniak M. (2004). Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS, 18 Suppl 1, S19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Catz S, & Ramachandran B. . (1999). Barriers to HIV/AIDS treatment and treatment adherence among African-American adults with disadvantaged education. Journal of the National Medical Association, 91, 439–446. [PMC free article] [PubMed] [Google Scholar]
- Kamiya Y, Timonen V, & Kenny RA (2016). The impact of childhood sexual abuse on the mental and physical health, and healthcare utilization of older adults. International Psychogeriatrics, 28(3), 415–422. doi: 10.1017/S1041610215001672 [DOI] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals., 32(9), 509–515. [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of general internal medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine EC, Martinez O, Mattera B, Wu E, Arreola S, Rutledge SE, . . . Carballo-Dieguez A. (2018). Child sexual abuse and adult mental health, sexual risk behaviors, and drinking patterns among Latino men who have sex with men. Journal of Child Sexual Abuse, 27(3), 237–253. doi: 10.1080/10538712.2017.1343885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipira L, Williams EC, Huh D, Kemp CG, Nevin PE, Greene P, . . . Rao D. (2018). HIV-related stigma and viral suppression among African-American women: exploring the mediating roles of depression and ART nonadherence. AIDS and Behavior, 23, 2025–2036. doi: 10.1007/s10461-018-2301-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez JD, Shacham E, & Brown T. (2018). Suicidal ideation persists among individuals engaged in HIV care in the era of antiretroviral therapy. AIDS and Behavior, 22(3), 800–805. doi: 10.1007/s10461-016-1666-5 [DOI] [PubMed] [Google Scholar]
- McCoy K, Waldrop-Valverde D, Balderson BH, Mahoney C, & Catz S. (2016). Correlates of antiretroviral therapy adherence among HIV-infected older adults. Journal of the International Association of Providers of AIDS Care, 15(3), 248–255. doi: 10.1177/2325957416642019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan JA, Brown J, Lampe FC, Lipman M, Smith C, & Rodger A. (2018). Resilience and physical and mental well-being in adults with and without HIV. AIDS and Behavior, 22(5), 1688–1698. doi: 10.1007/s10461-017-1980-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CS, Hansen NB, Kochman A, & Sikkema KJ (2009). Utilization of medical treatments and adherence to antiretroviral therapy among HIV-positive adults with histories of childhood sexual abuse. AIDS Patient Care STDS, 23(4), 259–266. doi: 10.1089/apc.2008.0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugavero M, Ostermann J, Whetten K, Leserman J, Swartz M, Stangl D, & Thielman N. (2006). Barriers to antiretroviral adherence: The importance of depression, abuse, and other traumatic events. AIDS Patient Care and STDs, 20, 418–428. [DOI] [PubMed] [Google Scholar]
- Office of AIDS Research Advisory Council (2018). Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Retrieved from https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf
- Pence BW, Ostermann J, Kumar V, Whetten K, Thielman N, & Mugavero MJ (2008). The influence of psychosocial characteristics and race/ethnicity on the use, duration, and success of antiretroviral therapy. Journal of Acquired Immune Deficiency Syndromes, 47, 194–201. [DOI] [PubMed] [Google Scholar]
- Pyra M, Weber K, Wilson TE, Cohen J, Murchison L, Goparaju L, & Cohen MH (2014). Sexual minority status and violence among HIV infected and at-risk women. Journal of General Internal Medicine, 29(8), 1131–1138. doi: 10.1007/s11606-014-2832-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Skeer M, Perkovich B, Johnson CV, & Safren SA (2009). A review of HIV antiretroviral adherence and intervention studies among HIV-infected youth. Topics in HIV Medicine, 17, 14–25. [PMC free article] [PubMed] [Google Scholar]
- Remien RH, Dolezal C, Wagner GJ, Goggin K, Wilson IB, Gross R, . . . Liu H. (2014). The association between poor antiretroviral adherence and unsafe sex: differences by gender and sexual orientation and implications for scale-up of treatment as prevention. AIDS and Behavior, 18(8), 1541–1547. doi: 10.1007/s10461-013-0656-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(1), 71–83. doi: 10.1017/s0033291710000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sauceda JA, Wiebe JS, & Simoni JM (2016). Childhood sexual abuse and depression in Latino men who have sex with men: Does resilience protect against nonadherence to antiretroviral therapy? Journal of Health Psychology, 21(6), 1096–1106. doi: 10.1177/1359105314546341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, & Green BL (2004). Understanding relationships among trauma, posttraumatic stress disorder, and health outcomes. Advances in Mind-Body Medicine, 20, 18–29. [PubMed] [Google Scholar]
- Simoni JM, Huh D, Wilson IB, Shen J, Goggin K, Reynolds NR, . . . Liu H. (2012). Racial/Ethnic disparities in ART adherence in the United States: findings from the MACH14 study. Journal of Acquired Immune Deficiency Syndromes, 60(5), 466–472. doi: 10.1097/QAI.0b013e31825db0bd [DOI] [PMC free article] [PubMed] [Google Scholar]
- South Carolina Department of Health and Environmental Control (2019). An Epidemiologic Profile of HIV and AIDS in South Carolina 2018. Retrieved from https://www.scdhec.gov/sites/default/files/media/document/2018%20Epi%20Profile.pdf
- Tsai AC, Wolfe WR, Kumbakumba E, Kawuma A, Hunt PW, Martin JN, . . . Weiser SD (2016). Prospective study of the mental health consequences of sexual violence among women living with HIV in rural Uganda. Journal of Interpersonal Violence, 31(8), 1531–1553. doi: 10.1177/0886260514567966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B, Rice WS, Crockett KB, Johnson M, Neilands TB, Ross SN, . . . Turan JM (2019). Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: the mediating role of depression. AIDS, 33(3), 571–576. doi: 10.1097/QAD.0000000000002071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner BJ, Laine C, Cosler L, & Hauck WW . (2003). Relationship of gender, depression, and health care delivery with antiretroviral adherence in HIV-infected drug users. Journal of General Internal Medicine, 18, 248–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uthman OA, Magidson JF, Safren SA, & Nachega JB (2014). Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep, 11(3), 291–307. doi: 10.1007/s11904-014-0220-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner GJ, Slaughter M, & Ghosh-Dastidar B. (2017). Depression at Treatment Initiation Predicts HIV Antiretroviral Adherence in Uganda. Journal of the International Association of Providers of AIDS Care, 16(1), 91–97. doi: 10.1177/2325957416677121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang R, & Ware JH (2013). Detecting moderator effects using subgroup analyses. Prevention Science, 14(2), 111–120. doi: 10.1007/s11121-011-0221-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson SM, Sikkema KJ, & Ranby KW (2014). Gender moderates the influence of psychosocial factors and drug use on HAART adherence in the context of HIV and childhood sexual abuse. AIDS Care, 26(8), 959–967. doi: 10.1080/09540121.2013.873765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson Van Voorhis CR, Morgan BL. Understanding power and rules of thumb for determining sample sizes. Tutorials in Quantitative Methods for Psychology 2007;3:43–50. [Google Scholar]
- World Health Organization, (2020). HIV/AIDS: Data and statistics. Retrieved from https://www.who.int/hiv/data/en/
- Yu Y, Luo D, Chen X, Huang Z, Wang M, & Xiao S. (2018). Medication adherence to antiretroviral therapy among newly treated people living with HIV. BMC Public Health, 18(1), 825. doi: 10.1186/s12889-018-5731-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


