INTRODUCTION
Bell’s palsy is an idiopathic peripheral palsy of the facial nerve that commonly presents as unilateral facial muscle weakness.1 The facial nerve is responsible for the muscles of facial expression, taste to anterior 2/3 of the tongue, and parasympathetic supply to salivary and lacrimal glands.2 Bell’s palsy accounts for 60–75% of unilateral facial paralysis cases with an annual incidence of 15 to 30 cases per 100,000 people.3, 4 Although rare, malignant tumors can also affect the facial nerve with similar presentation as Bell’s palsy. Malignant peripheral nerve sheath tumor (MPNST) is an aggressive tumor with an annual incidence of 0.8 cases per 100,000 people.5 MPNST arises sporadically from a peripheral nerve either from a pre-existing benign peripheral nerve sheath tumor as a consequence of radiation treatment or associated with neurofibromatosis type 1 (NF1) syndrome.6 More than 50% of MPNST are associated with NF1 syndrome, and patients with NF1 syndrome have an 8 to 13% lifetime incidence of developing of MPNST.5 Hence, a diagnosis of MPNST warrants a thorough examination for skin lesions such as café au lait macules, axillary freckling, and lisch nodules consistent with NF1 syndrome.7 MPNST has variable presentations depending on tumor location, commonly affecting the extremities and, more rarely, the head and neck (H&N).8 We report a case of a middle-aged woman with a gradual onset of facial palsy slowly progressing over an 18-month period that ultimately was found to be caused by a MPNST of the facial nerve with temporal bone involvement. We discuss the approach on how to differentiate benign versus malignant causes of unilateral peripheral facial palsy, and review the diagnosis and management of MPNST.
CASE DESCRIPTION
A 54-year-old woman with history of stage IB1 squamous cell carcinoma of the cervix treated with chemotherapy and radiation therapy and left facial nerve palsy presented to a primary care clinic for an initial routine visit. When reviewing her medical history of left facial nerve palsy, she reported that her left jaw and facial pain started about 18 months ago. Over the next 6 months, she developed slowly progressive left upper and lower facial weakness, numbness, and eventual inability to close her left eye. She was initially evaluated in an urgent care and was diagnosed with Bell’s palsy. Despite her symptoms gradually progressing with worsening weakness, the patient did not seek medical attention again until this routine primary care visit, 12 months after her urgent care visit. She denied eye dryness or pain, visual changes, hearing changes, dizziness, or any involvement of the right side of the face. There was no prior history of stroke, radiation treatment, or trauma. Her physical exam was significant for left-sided upper and lower partial facial paralysis and decreased sensation to light touch involving the forehead. She was unable to close her left eyelid with maximum effort (Fig. 1). No other focal neurological deficits were noted. There was no palpable cervical lymphadenopathy.
Figure 1.
Left-sided facial droop with loss of left nasolabial fold (left). Impaired left eye closure (right).
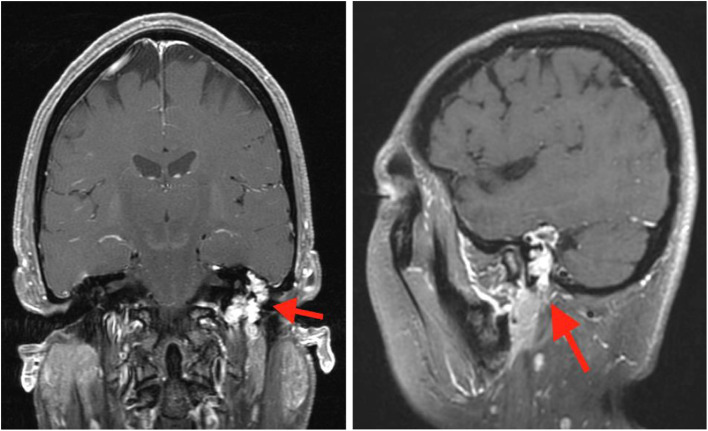
Complete blood count was within normal limits. Due to the slow onset and progression of her symptoms, which was atypical for Bell’s palsy, a magnetic resonance imaging (MRI) of the orbit, face, and neck was performed, revealing a diffuse enhancement of the middle ear and mastoid cavities that was confluent with a 1.7 × 1.3 × 2.0 cm globular enhancing mass (Fig. 2). A computed tomography (CT) of the temporal bone was performed to further evaluate the middle ear and mastoid enhancement. It showed a mass with aggressive features centered in the left mastoid cavity with associated osseous erosion, local extension to the left external auditory canal, middle ear cavity, and involvement of the left facial nerve. Otoscope exam performed after imaging results revealed a soft tissue mass along the posterior wall of her left external auditory canal partially obstructing the tympanic membrane. A review of her previous visits revealed that an otoscope exam had not been performed. A biopsy of the left ear mass showed a low-grade MPNST which was not consistent with a metastasis, given the patient’s known gynecological malignancy.
Figure 2.
Coronal (left) and sagittal (right) T1 weighted contrast-enhanced MR image showing enhancing mass.
Otolaryngology and neurosurgery were consulted. 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) did not reveal metastatic disease. Given localized disease, the patient underwent a left mastoidectomy, left facial nerve resection, and radical left parotidectomy. A fascia lata sling was performed to correct her facial asymmetry as a result of the tumor resection, and a gold weight was placed in her left eyelid to correct her lagophthalmos. Unfortunately, post-surgical biopsy returned with positive margins. The patient was referred to radiation and medical oncology and completed a course of adjuvant radiotherapy. Follow-up MRIs over the next year showed no disease progression. Her left eye still does not fully close despite the gold weight placement, and the patient is being followed by oculoplastic surgery.
DISCUSSION
The etiology of Bell’s palsy is still unknown, with the general mechanism involving inflammation and edema of the facial nerve leading to compression, and thus, it is a diagnosis of exclusion based on a thorough history and physical examination.9 Approximately 70% of peripheral facial nerve palsies are benign Bell’s palsy, suggesting that 30% may have an underlying etiology.10 Causes of unilateral facial nerve palsy include stroke; trauma; neoplasms of the brain, parotid gland, or infratemporal fossa; infections (e.g., herpes zoster, Lyme disease, and human immunodeficiency virus); sarcoidosis; and diabetes mellitus.2, 10 A complete medical history should include recent rashes, arthralgias, fevers, or viral prodromes; history of peripheral nerve palsy, trauma, stroke, or neoplasms; and exposure to vaccines, new medications, or ticks. Signs and symptoms that are atypical with Bell’s palsy are dysphagia, dizziness, diplopia, fever, malaise, headache, stiff neck, rash, arthralgias, forehead sparing, or other neurologic abnormalities. A thorough physical examination should include careful inspection of the ear canal and tympanic membrane with an otoscope, so as not to miss an inner ear mass, as in our patient.2 Clinicians should also examine the oropharynx, parotid gland, skin of the head, face, and cheek, cranial nerves, and peripheral nerve function in the extremities.2
The presentation and onset of symptoms are key distinguishing features to differentiate Bell’s palsy from other causes. Bell’s palsy symptoms typically peak within 3 days and most always within 1 week, and usually self-resolve within 3 months.11 Thus, clinicians should reconsider the diagnosis of Bell’s palsy in patients with insidious onset, recurrent or bilateral symptoms, progression after 2 weeks from symptom onset, or incomplete facial recovery after 3 months from symptom onset.1, 2, 10, 11 It is imperative to recognize malignant mimickers of Bell’s palsy because these conditions could be fatal if diagnosis and intervention are delayed. Occult malignant causes of facial nerve palsy include infratemporal, extratemporal, and skull base malignancies, cutaneous squamous cell carcinoma with perineural invasion, and metastasis of the facial nerve from lung cancer.12–14 In addition to the gradual onset and progression of the symptoms, facial pain in the absence of herpes zoster infection may suggest malignancy as the underlying etiology. For example, a neoplasm of the temporal bone could cause painful chronic otorrhea with facial paralysis. The American Academy of Otolaryngology-Head and Neck Surgery Foundation’s guideline development group does not recommend routine laboratory testing or diagnostic imaging for new onset Bell’s palsy, unless when indicated by history, risk factors, or an atypical presentation as mentioned above.10 In these cases, the literature strongly supports the use of imaging, and MRI with and without contrast of the complete anatomical path of the facial nerve is the modality of choice.10 However, there have been published reports of facial paralysis caused by occult malignancy with normal imaging.12, 13 With these findings, patients with facial paralysis with no improvement after 6 months warrant surgical exploration and biopsy of the facial nerve, even in the setting of normal imagings.12, 13
MPNST has previously been referred to as neurofibrosarcoma, malignant schwannoma, and malignant neurofibroma. MPNST is rare, with an incidence of 0.001% in the general population, and only 10% of those are located in the H&N.8, 15 A review of the literature shows H&N MPNST more commonly involves the neck, mandible, maxilla, and, rarely, the temporal bone with only a few reported cases. To our knowledge, there has not been a published case of a MPNST presenting solely as facial paralysis mimicking Bell’s palsy.8, 15, 16 MPNST with involvement of the temporal bone commonly presents as enlarging, painful masses with intact facial nerve function, rather than facial palsy.17, 18 Biopsy is required for diagnosis, and imaging is needed for staging and treatment planning.19 CT of the chest is usually used for staging given the high potential of metastatic spread to the lungs. MRI is the most useful imaging technique to define the borders of the tumor for surgical planning.6 18F-fluorodeoxyglucose positron emission tomography is increasingly being used for staging, treatment planning, and follow-up. Prompt referral to subspecialists, such as otolaryngology and neurosurgery, is crucial to further guide and expedite diagnosis and treatment planning.
MPNST overall has a poor prognosis and high rates of recurrence despite aggressive therapy. Treatment depends on the stage of the disease at the time of diagnosis. Similar to other soft-tissue sarcomas, localized MPNST is best managed with surgical excision. Surgical margin status is the most predictive prognostic factor with failure to attain negative free margins significantly reducing survival. 15, 20–22 Radiotherapy is recommended in tumor size > 5 cm prior to resection.23 Systemic chemotherapy is used in patients who have metastatic disease on presentation. To detect local recurrence, MRI is recommended yearly for the first 5 years after resection.16, 24
Our patient fortunately did not have any distant metastasis based on 18F-FDG PET at the time of diagnosis, 18 months after the onset of her symptoms, but any further delay in diagnosis and management most likely would have affected her morbidity and mortality significantly.
CONCLUSION
We describe a rare case of MPNST of the facial nerve involving the temporal bone in a woman presenting with a progressive and chronic facial paralysis initially misdiagnosed as Bell’s palsy. To our knowledge, this is the first case presentation of MPNST reported with isolated unilateral facial paralysis. Clinicians should be vigilant for atypical presentations of Bell’s palsy with a thorough history and physical examination and be especially cognizant of the course of the onset and duration of the symptoms. Gradual progression after 2 weeks and lack of symptomatic improvement after 3 months from onset of symptoms should prompt clinicians to pursue further evaluation with imaging and potentially surgical exploration. This case demonstrates a unique presentation mimicking Bell’s palsy of an already rare disease, MPNST involving the facial nerve. Recognizing atypical presentations of facial nerve palsies is imperative to allow for appropriate workup and prompt diagnosis, as malignant causes of facial nerve palsies, such as MPNST, are associated with poor prognosis when treatment is delayed.
Acknowledgments
Contributors: Insun Chong, MD, the radiology resident who helped us obtain the imagings. Dr. Aparna Jotwani, MD, the oncologist who reviewed the discussion section of MPNST of our manuscript.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior presentation
Poster clinical vignette presentation at the National Society of General Internal Medicine Meeting, May 10, 2019.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gilden DH. Bell’s palsy. N Engl J Med. 2004;351(13):1323–31. doi: 10.1056/NEJMcp041120. [DOI] [PubMed] [Google Scholar]
- 2.Tiemstra JD, Khatkhate N. Bell’s palsy: diagnosis and management. Am Fam Physician. 2007;76(7):997–1002. [PubMed] [Google Scholar]
- 3.Adour KK, Byl FM, Hilsinger RL, Jr, Kahn ZM, Sheldon MI. The true nature of Bell’s palsy: analysis of 1,000 consecutive patients. Laryngoscope. 1978;88:787–801. doi: 10.1002/lary.1978.88.5.787. [DOI] [PubMed] [Google Scholar]
- 4.Morris AM, Deeks SL, Hill MD, et al. Annualized incidence and spectrum of illness from an outbreak investigation of Bell’s palsy. Neuroepidemiology. 2002;21:255–61. doi: 10.1159/000065645. [DOI] [PubMed] [Google Scholar]
- 5.Ng VY, Scharschmidt TJ, Mayerson JL, Fisher JL. Incidence and survival in sarcoma in the United States: a focus on musculoskeletal lesions. Anticancer Res. 2013;33:2597–2604. [PubMed] [Google Scholar]
- 6.Farid M, Demicco EG, Garcia R, et al. Malignant peripheral nerve sheath tumors. Oncologist. 2014;19(2):193–201. doi: 10.1634/theoncologist.2013-0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Widemann BC. Current status of sporadic and neurofibromatosis type 1-associated malignant peripheral nerve sheath tumors. Curr Oncol Rep. 2009;11(4):322–8. doi: 10.1007/s11912-009-0045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mullins BT, Hackman T. Malignant peripheral nerve sheath tumors of the head and neck: a case series and literature review. Case Rep Otolaryngol. 2014;2014:368920. doi: 10.1155/2014/368920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang W, Xu L, Luo T, Wu F, Zhao B, Li X. The etiology of Bell’s palsy: a review. J Neurol. 2020;267(7):1896–1905. doi: 10.1007/s00415-019-09282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baugh RF, Basura GJ, Ishii LE, et al. Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg. 2013;149(3 Suppl):S1–27. doi: 10.1177/0194599813505967. [DOI] [PubMed] [Google Scholar]
- 11.Pietersen E. Bell’s palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol Suppl. 2002;549:4–30. doi: 10.1080/000164802760370736. [DOI] [PubMed] [Google Scholar]
- 12.Alghamdi M, Strenger T, Thoelken R, Schaller T, Zenk J. Facial Nerve Palsy, When should we be alarmed: a case report of facial nerve paralysis caused by occult malignancy and review of the literature. Clin Med Rev Case Rep. 2019;6:283. [Google Scholar]
- 13.Marzo SJ, Leonetti JP, Petruzzelli G. Facial paralysis caused by malignant skull base neoplasms. Neurosurg Focus. 2002;12(5):e2. doi: 10.3171/foc.2002.12.5.3. [DOI] [PubMed] [Google Scholar]
- 14.Yildiz O, Buyuktas D, Ekiz E, Selcukbiricik F, Papila I, Papila C. Facial nerve palsy: an unusual presenting feature of small cell lung cancer. Case Rep Oncol. 2011;4(1):35–8. doi: 10.1159/000324182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Minovi A, Basten O, Hunter B, Draf W, Bockmühl U. Malignant peripheral nerve sheath tumors of the head and neck: management of 10 cases and literature review. Head Neck. 2007;29(5):439–445. doi: 10.1002/hed.20537. [DOI] [PubMed] [Google Scholar]
- 16.Ziadi A, Saliba I. Malignant peripheral nerve sheath tumor of intracranial nerve: a case series review. Auris Nasus Larynx. 2010;37(5):539–545. doi: 10.1016/j.anl.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 17.Gogate BP, Anand M, Deshmukh SD, Purandare SN. Malignant peripheral nerve sheath tumor of facial nerve: presenting as parotid mass. J Oral Maxillofac Pathol. 2013;17(1):129–131. doi: 10.4103/0973-029X.110708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daga G, Paul R, Mandal G, Kumar R. Malignant peripheral nerve sheath tumor of the parotid gland. Indian J Surg Oncol. 2018;9(4):629–632. doi: 10.1007/s13193-018-0779-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim HY, Hwang JY, Kim HJ, et al. CT, MRI, and 18F-FDG PET/CT findings of malignant peripheral nerve sheath tumor of the head and neck. Acta Radiol. 2017;58(10):1222–1230. doi: 10.1177/0284185116684674. [DOI] [PubMed] [Google Scholar]
- 20.Martin E, Muskens IS, Coert JH, Smith TR, Broekman ML. Treatment and survival differences across tumor sites in malignant peripheral nerve sheath tumors: a SEER database analysis and review of the literature. Neurooncol Pract. 2019;6(2):134–143. doi: 10.1093/nop/npy025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zou CY, Smith KD, Zhu QS, et al. Dual targeting of AKT and mammalian target of rapamycin: a potential therapeutic approach for malignant peripheral nerve sheath tumor. Mol Cancer Ther. 2009;8(5):1157–68. doi: 10.1158/1535-7163.MCT-08-1008. [DOI] [PubMed] [Google Scholar]
- 22.Patel TD, Shaigany K, Fang CH, Park RC, Baredes S, Eloy JA. Comparative analysis of head and neck and non–head and neck malignant peripheral nerve sheath tumors. Otolaryngol Head Neck Surg. 2016;154(1):113–20. doi: 10.1177/0194599815606700. [DOI] [PubMed] [Google Scholar]
- 23.Prudner BC, Ball T, Rathore R, Hirbe AC. Diagnosis and management of malignant peripheral nerve sheath tumors: current practice and future perspectives. Neurooncol Adv. 2019;2(Suppl 1):i40–9. doi: 10.1093/noajnl/vdz047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.L’heureux-Lebeau B, Saliba I. Updates on the diagnosis and treatment of intracranial nerve malignant peripheral nerve sheath tumors. Onco Targets Ther. 2013;6:459–470. doi: 10.2147/OTT.S41397. [DOI] [PMC free article] [PubMed] [Google Scholar]