Abstract
Background
Limited health literacy is a driver of cancer disparities and associated with less participation in medical decisions. Mammography screening decisions are an exemplar of where health literacy may impact decision-making and outcomes.
Objective
To describe informational needs and shared decision-making (SDM) experiences among women ages 40–54 who have limited health literacy and primary care providers (PCPs).
Design
Qualitative, in-depth interviews explored experiences with mammography counseling and SDM.
Participants
Women ages 40–54 with limited health literacy and no history of breast cancer or mammogram in the prior 9 months were approached before a primary care visit at a Boston academic, safety-net hospital. PCPs practicing at this site were eligible for PCP interviews.
Approach
Interviews were audio-recorded and transcribed verbatim. A set of deductive codes for each stakeholder group was developed based on literature and the interview guide. Inductive codes were generated during codebook development. Codes were compared within and across patient and PCP interviews to create themes relevant to mammography decision-making.
Key Results
The average age of 25 interviewed patients was 46.5; 18 identified as black, 3 as Hispanic, 2 as non-Hispanic white, and 2 had no recorded race or ethnicity. Of 20 PCPs, 15 were female; 12 had practiced for >5 years. Patients described a lack of technical (appropriate tests and what they do) and process (what happens during a mammogram visit) knowledge, viewing these as necessary for decision-making. PCPs were reluctant to engage patients with limited health literacy in SDM due to time constraints and feared that increased information might confuse patients or deter them from having mammograms. Both groups felt pre-visit education would facilitate mammography-related SDM during clinical visits.
Conclusion
Both patients and PCPs perceived a need for tools to relay technical and process knowledge about mammography prior to clinical encounters to address the scope of information that patients with limited health literacy desired.
Electronic supplementary material
The online version of this article (10.1007/s11606-020-06213-2) contains supplementary material, which is available to authorized users.
Key Words: breast cancer, mammography, shared decision-making, health literacy
INTRODUCTION
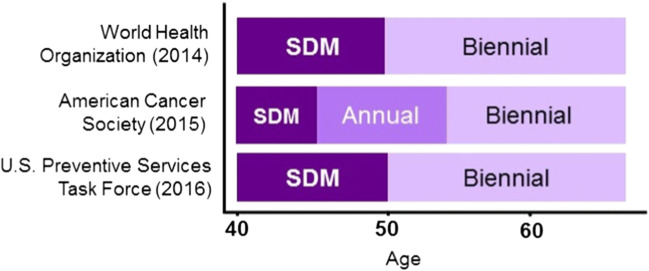
Professional guidelines recommend that women under 50 years old make breast cancer screening decisions based on personal risk and values, via shared decision-making (SDM) with their clinicians.1, 2 While these guidelines have gained acceptance in moving away from routine mammography screening at age 40 (Fig. 1), implementation of SDM that has been mandated to replace routine mammography has been suboptimal.3 A scoping review by DuBenske and colleagues identified three key aspects of mammography decision-making: information delivery/patient education (focused on benefits and risks), clinician-patient communication, and having a framework for decision-making.4 Primary care providers (PCPs) have cited limitations in carrying out these activities, including insufficient time available in a visit,5–7 physician beliefs or bias,8, 9 and lack of knowledge about mammography and/or confidence in conducting shared decision-making.6, 7 In a survey that directly evaluated physician knowledge of mammography harms and benefits, harms, including rates of additional imaging and breast biopsy, were underestimated by 90% and 82% of physicians, respectively.6 Research from the patient perspective has likewise documented barriers to SDM, including patients having different expectations about what information they should receive relative to what they do receive,10, 11 uncertainty about personal risk,12–15 and lack of self-efficacy in making mammography decisions.7 While these barriers are well-documented in the literature, other issues, including how health literacy affects mammography decision-making, are less known.16
Figure 1.
Shared decision-making in guidelines for breast cancer screening.
Clinicians may feel that introducing SDM to populations with limited health literacy is overly burdensome, which may create a disparity in achieving SDM in screening decisions for women.17 Women of color and those with limited health literacy are less likely to have sufficient knowledge about mammography,18, 19 to know about their own risk factors for breast cancer,19–21 to receive a personal risk assessment,22 or to be asked about their personal values and preferences.23 If women with limited health literacy are at a disadvantage in receiving each of these, the cumulative result may be less engagement in SDM24–26 and less engagement in mammography screening overall.27
While there have been calls to develop more patient-centered decision-support tools for mammography,28, 29 the perspectives of women with limited health literacy are required to develop tools that address their preferences and needs effectively,30–33 while balancing these needs with provider knowledge, skill, and structural constraints.34 Historically, women with limited health literacy and minority populations have been underrepresented in research on both mammography and SDM.35 The exclusion of these perspectives may both overestimate the effectiveness of tools that are designed by and for populations with higher health literacy, and may exacerbate informational access disparities, which influence subsequent participation in mammography decision-making.36
This study sought to understand the informational needs and experiences with mammography-related SDM among women ages 40–54 who have limited health literacy, and to describe SDM practices among PCPs at a safety-net hospital who counsel women on mammography. The goal of this work is to identify opportunities to address both stakeholders’ needs in developing interventions to improve mammography SDM among women with limited health literacy.
METHODS
We conducted a qualitative study from November 2018 to May 2019 using in-person interviews to learn about patient and PCP approaches to, challenges with, and desired conditions for mammography-related SDM. Interview guides for both groups were based on prior literature and a framework for how health literacy, through access to care, interactions with providers, and self-care, produces health outcomes.37 All activities and materials were approved by the Boston University Medical Center Institutional Review Board.
Patient Interviews
We sought women ages 40–54 with no mammogram in the prior 9 months and no history of breast cancer. The age range for eligibility was chosen based on professional guidelines, which vary in mammography initiation and spacing up to age 55, where they generally converge around recommending routine screening with biennial mammography for all women. For these women, SDM is the recommended activity to determine mammography use (Fig. 1), yet this process is relatively unexplored in those with limited health literacy. Women who were identified as having upcoming primary care visits at a Boston-based academic, safety-net primary care practice who met the above criteria were then approached for screening in the waiting room. If interested, women completed the Health Literacy Skills Instrument-10, a 10-item validated measure of health literacy focused on decision-making skills.38 If a woman scored less than 7, the validated cutoff that suggests limited health literacy, she was invited to participate in a qualitative interview. Interviews took place immediately following the primary care visit, where possible, or were scheduled at the participants’ convenience. Because we sought to interview women with a range of prior mammogram experiences, we purposively sampled at least 10 participants with and without any prior mammograms.
Interview guides were pilot tested in 5 women with LHL prior to study start. Topics included prior knowledge and experience learning about and receiving counseling about mammography, familiarity with breast cancer risk, knowledge of other screening tests, and preferences for and experiences with SDM. Interviews were conducted by a trained research assistant and designed to last 45–60 min, using a flexible, conversational approach to elicit responses to topical questions. Post-interview memos were created by the interviewer and included key themes and contextual factors about the interview from the interviewer’s perspective. These memos assisted in establishing when theoretical saturation39 had been reached. Patients received $40 as an incentive.
Primary Care Provider (PCP) Interviews
PCPs (physicians and nurse practitioners) were eligible if they practiced in one of the outpatient general internal medicine or family medicine clinics within the hospital. All 150 PCPs seeing patients in the general internal medicine and family medicine outpatient clinics were invited via email and through in-person invitations during practice-wide meetings. Interviews were scheduled and took place in a private office. PCPs who participated were entered into a raffle to receive $100, which was allotted at the conclusion of recruitment.
PCP interview guides were pilot tested with clinician study team members before study start. Topics covered in the PCP interviews included eliciting counseling practices generally and through use of a scenario-based question, experiences with eliciting patient preferences, assessing understanding, and use of risk estimates for decision-making. PCPs were also asked about their challenges and successes in implementing mammography-related SDM, their perceived role in SDM, and ideas for facilitating mammography SDM in clinical encounters. Interviews were conducted by an investigator (CG) and lasted 30 min. Sampling continued until theoretical saturation was achieved.
Data Analysis
All interviews were audio recorded and professionally transcribed verbatim. Transcripts were verified against the audio files to ensure fidelity and then uploaded into NVivo 12.1.0 qualitative data management software. We conducted a content analysis,40, 41 combining deductive and inductive thematic development approaches. Deductive codes were developed based on the literature and our guiding conceptual framework,37 both of which informed the interview guide. Inductive codes were also generated during codebook development. Three patient and three PCP interviews were independently coded by two investigators (CG, AM). Codes and their application were compared and consensus was achieved in defining and clarifying deductive and inductive codes. All of the remaining interviews were coded by AM with six reviewed by another investigator (CG) to ensure quality.
Codes were compared within and across patient and PCP interview groups to create themes relevant to mammography decision-making. To facilitate comparisons, CG and AM created summaries that represented content from key themes for each participant.42 Final themes and chosen representative quotes were refined using a constant comparison technique.43 Each theme is represented below, with pseudonyms replacing patient names to preserve confidentiality.
RESULTS
We identified 213 potentially eligible patients with upcoming appointments; 126 showed up for their appointments, 74 were approached for participation, and 65 completed screening questions. Three declined participation and 26 were ineligible due to a recent mammogram (n = 13), scoring >7 on the HLSI-10 (n = 10), or not speaking English (n = 3). Interviews were conducted until saturation was achieved, at 23 interviews. Two previously scheduled interviews were completed, resulting in a sample of 25 patients. Of the 150 invited PCPs, 26 expressed interest. Using post-interview summaries as a guide, we established saturation had been achieved by 20 interviews, and concluded enrollment. Table 1 displays the demographics of the enrolled participants. Below, we present four themes characterizing both groups’ approaches to, challenges with, and desired conditions for SDM, with additional quotes in Table 2.
Table 1.
Interview Participant Characteristics
| Women with limited health literacy (N = 25) | |
|---|---|
| Age (μ = 46) | n (%) |
| 40–45 | 10 (40) |
| 46–50 | 9 (36) |
| 51–54 | 6 (24) |
| HLSI-10 score | |
| 0 | 1 (4) |
| 1 | 2 (8) |
| 2 | 1 (4) |
| 3 | 6 (24) |
| 4 | 3 (12) |
| 5 | 6 (24) |
| 6 | 6 (24) |
| Mammography history | |
| Prior mammogram | 12 (48) |
| No prior mammogram | 13 (52) |
| Race | |
| Black/African American | 18 (72) |
| White | 2 (8) |
| Not available | 5 (20) |
| Ethnicity | |
| Hispanic/Latina | 3 (12) |
| Non-Hispanic/Latina | 22 (88) |
| Primary care providers (N = 20) | |
| Gender | n (%) |
| Female | 15 (75) |
| Male | 5 (25) |
| Number of years in practice | |
| ≤ 5 years | 8 (40) |
| 6–10 years | 6 (30) |
| 11–20 years | 2 (10) |
| > 20 years | 4 (20) |
| Mammography educational materials provided to patients | |
| None | 17 (85) |
| In office handouts | 2 (10) |
| Out of office referrals | 1 (5) |
Table 2.
Theme Summaries with Supporting Quotes from Patients and Primary Care Providers
| Theme | Sub-theme | Patient exemplar | PCP exemplar |
|---|---|---|---|
| While desiring SDM, patients and PCPs expressed knowledge barriers to implementing it. | A perceived lack of technical and process knowledge gave PCPs greater decision-making power, but could threaten trust. | “I mean I do not even know what [mammograms] are, so I would not say it would be on a patient, because they are not knowledgeable to medical stuff as much as a doctor would be.” | “So if I tell them, ‘You need a mammogram,’ they are going to do it– even if they do not know what it is, even if they do not think it’s valuable...So I try to give them more information, so that they will not just be doing it because I say so.” |
| Concerns about patient capacity to understand comprehensive information curtailed SDM. | “Sometimes they use a word you are not familiar with, and you hear it again and you are like, ‘Okay I remember what that means’... So I actually kind of do like the terms that they use, because at least I know how to actually say something right if I do remember.” | “I think we get away from it should be a shared decision-making conversation... We should be doing appropriate counseling on the risks and benefits of it. And I think for the majority of the visits we are like, ‘Oh, you are due for a mammogram. I’m just going to put that order in.’” | |
| Most patients sought technical and process knowledge; PCPs acknowledged that these elements were undercommunicated. | There was a desire for providing patients with process and technical knowledge. | “I think if people talked about the steps, that’s important … I do not think anybody explains that. It’s just go get your mammogram, make the appointment.” | “What is it they are actually doing? We do that for everything else that we do procedurally for patients, but mammograms we are just like, ‘Here’s your order for your mammogram. Go get a mammogram’… nobody really prepares them.” |
| There were misperceptions about the accuracy of mammograms. | “They’re going to tell you what you have. It’s not bad. I mean something that hurts… But [it will] tell you what you have, what you can do, they tell you everything.” | “I feel like I spend a lot of time allaying anxiety because I think the scientificness of the process gives this idea that I somehow have a crystal ball.” | |
| Mammograms were perceived to be a well-known test, which was a barrier to addressing patients’ informational needs during visits. | Mammograms are in the public discourse and well-understood. | “Even if there is nothing there they should go into it more, I mean like on the basics... because I kind of feel dumb right now. Like I know, but I do not.” | “I would say 100% literally, regardless of the language that they speak or their education level, understand what a mammogram is… It’s really kind of permeated cultures so that people understand that.” |
| Assessing understanding was curtailed due to the perception that mammography was understood. | “If somebody just saying, ‘Yeah,’ but they really do not understand, they [doctors] will not say, ‘Do you understand what I’m saying?’ Make sure to ask them. Do not wait until the end and get upset when they are asking and they say, ‘I just told you.’ I did not know what that was.” | “Especially when there’s the interpreter line. That’s like a huge barrier in all routine health … There’s been times when I’m like I do not know if they truly understood what I was trying to say…Occasionally, I’ll try teach back … but other times, just kind of move along with the visit because there’s a lot of other things to tackle.” | |
| Systems-level issues across healthcare settings discouraged PCPs from tailoring mammography recommendations and confused patients. | Conflicting information led to confusion. | “When the nurse practitioner asked me again… it was kind of—not a shock, but I wasn’t aware that she’s going to ask me to get a mammogram. Because in my head, we have to do it at age 50.” | “I would say that would be one of the biggest things is the diversity of how much the guidelines change, and the fact that they are all kind of conflicting, it makes it easy for patients to doubt providers.” |
| Information provided ahead of the visit would better support SDM. | “They should give classes on it to patients so they’ll know what to expect. That way their doctors will not have to explain it to them. They could show a movie of mammogram… or explain to the class about what a mammogram is and how to go about getting a mammogram, what to expect.” | “It would be nice if the patient comes in having some [information] … So then you can start a discussion at a different time… If you have somebody that has read something… you can have a different conversation.” | |
| Post-visit supports are needed. | “I mean, even if they just put in information for patients [on the patient portal] - materials to read on what you should be doing, next step, preventive care, you should be on time for this maybe six months or a year…so that they are not always trying to get the doctor on the phone.” | “There’s no good summary of this is what you decided for your routine health maintenance after this visit. So if there was an easy way to click and say, ‘we decided you are going to,’…and just to say this is actually the result outcome of our shared decision making around cancer.” | |
| Non-clinical staff can support information-sharing. | “You do not have to be a doctor. It could somebody like a nurse practitioner or just a counselor who works in that area all about that for women with mammograms.” | “I’m not using any sort of specialized clinical knowledge... “I’m just using a model, an algorithm to say like, ‘You fall into this category you do this…’ And really like a lot of people could do that... You do not have to have an MD next to your name to be able to do that.” |
Theme 1: Patients with Limited Health Literacy and PCPs Desired Shared Decisions, but Implementation Was Impeded by Knowledge Barriers
Patients in our sample sought SDM, which was often described as where the doctor provides input, but the decision rests with the patient: “I’m the one that is supposed to decide, not the doctor, me. And maybe she gives me advice.” Patients further described three knowledge types germane to their participation in mammography decision-making—technical, embodied, and process. Technical knowledge referred to an understanding of health learned via medical training or patient education and included familiarity with breast cancer screening definitions and the purpose of mammography or other screening tests: “You [the PCP] should tell me when I need it.” Embodied knowledge was a woman’s intrinsic experience of her body and awareness of changes: “You know your body first.” Process knowledge encompassed knowledge about procedural elements of obtaining care (e.g., what happens at the visit) as well as associated tasks that facilitate test completion: “If people talked about the steps… that’s important.” Patients ascribed embodied knowledge primarily to themselves, while technical and process knowledge were more often associated with PCPs.
Patients, like Grace below, who described comprehensive technical and process knowledge as having greatest legitimacy associated primary decision-making power with PCPs:
When I come to the hospital and they do all these tests the doctor knows more than I know, right? So, I would like the doctor to do what the doctor does and tell me when I should be able to come in, when I should not be able to come in. – Grace
PCPs acknowledged that when patients deferred decisions to them, they worried that negative experiences could undermine the patient-provider relationship. One provider said, “[Patients] defer to me, so I would assume that if something happened, I’d be blamed. And that would impact the relationship.” While all patients in this study viewed technical and process knowledge as powerful, when this was combined with their own embodied knowledge, they viewed such knowledge as enhancing their decision-making power (Table 2).
Technical and process knowledge were highly valued by patients, but many PCPs described struggling with the types and amount of information to share with patients. They feared that increased information might confuse patients with limited health literacy or, for PCPs encouraging mammograms, deter patients from completing them.
I don’t tend to go into [potential harms] because I feel like it gets us off track and then people are less likely to be willing to do it, right? … I tend to gloss over those more, because … I know that doing it is better than not doing it and that we can deal with anxiety and whatever that comes from any sort of potential harms. – PCP 6
Concerns about what information to share and whether patients appreciate the risks and benefits of mammography deterred PCPs from fully engaging in SDM. PCPs described that visit time constraints meant robust tools like teach backs were replaced with shorter and less comprehensive evaluations. Such evaluations included assessing patients’ body language, asking if the patient understood information, or relying on the patients to ask “good” questions. Overall, both groups wanted to engage in shared decisions, but patients identified knowledge gaps that were described to be the basis of relying on PCPs, and PCPs relayed concerns about what information to share that inhibited full engagement in SDM.
Theme 2: Most Patients Sought Specific Technical and Process Knowledge, while PCPs Perceived that Patients’ Limitations of Technical Knowledge Heightened Anxiety for Patients
In line with knowledge gaps described above, patients had strong desires for information about “what is a mammogram?,” “why is it important?,” and “how does it happen?”: “Somebody in that field [should] tell you these are the steps. And I’m going to put you to sleep so you won’t feel a thing, but afterwards this is how it’s done, this is how we detect if there is this, or if there is that… However the process goes. We’ll give you a call.” (see Table 2). Even among patients with prior mammogram experience, some articulated questions indicating continued knowledge gaps: “I have an appointment for [my second] mammogram. But I don’t know the real meaning of it. I don’t know what it is about.”
PCPs’ expressed awareness that patients believe that mammograms are a test with perfect predictive power, which some PCPs felt led to poor patient experience:
The idea that a medical test is not like a crystal ball I think is news to a lot of people, and not just low health literacy people… That a test would have questionable efficacy at different times is just not something that’s necessarily part of most people’s health speak. – PCP 13
Support for this uncertainty was sought by PCPs to better address the range of possible outcomes of mammography.
Theme 3: PCP Perceptions that Mammograms Were a Well-Known Test Were a Barrier to Addressing Patients’ Informational Needs during Time-Crunched Visits
One factor related to PCPs’ inconsistent counseling about the what, why, and how of mammography was their perception that mammograms are well-understood because mammography is in general public health discourse. Describing why she uses teach backs less in mammography than in other areas, PCP 9 said: “Compared to other disease processes and screening tests, I believe there is more information about breast cancer. There’s pink ribbons on yogurt. I think it’s just something that is more talked about.” This assumption that informational prevalence engenders individual understanding curbed their active assessment of patient understanding for some PCPs (Table 2). In turn, PCPs felt that limiting mammography descriptions was a way to save time in visits with patients who had complex medical, social, language, and literacy needs. For example:
The woman I saw who asked me about the mammogram, she also has poorly controlled diabetes, severe depression, she disclosed to me that her daughter was hospitalized for anorexia, her father is sick; there was so much else going on at that visit, and that’s really a typical visit. So there’s just not a lot of space for a mammography conversation. – PCP 18
Providers perceived greater barriers to SDM among those with limited language or literacy skills, which hindered their addressing mammography where they might have otherwise done so.
Theme 4: Systems-Level Informational Inputs across Healthcare Settings Discouraged PCPs from Tailoring Mammography Recommendations and Confused Patients
Discordant information between guidelines and among other healthcare providers (e.g., radiologists, OB/GYNs) contributed to patient confusion that was difficult for PCPs to address during visits. PCPs felt that they did not have the bandwidth to address such system-level issues, saying they were “way too much of a boulder to lift up a hill” (PCP 15), but expressed interest in finding a way to unify messages. PCPs thought that addressing structural barriers, including time pressure in the setting of medical complexity and mixed messages from different groups, would enhance the prevalence and quality of SDM conversations.
Patients and PCPs described preferences for mammography information supports that responded to patient informational needs and structural barriers that inhibited SDM:
We all have questions, especially on this topic. No one is really quite on it. And if we have that dialogue and using graphics, and the computer is just amazing, you know... I think the more data that we receive the better… Even though that we might be fearful of whatever the outcome might be… we feel more confident in knowing these were our choices, we were included in the conversation. – Celeste
As Celeste notes, visual aids were perceived to be helpful, but only 2 PCPs reported supporting discussions with visual aids (Table 1).
Pre-visit time was identified as a key educational opportunity for decision-making primers. Addressing didactic information, ideally in the waiting room via print handouts, videos, or interactive tablets, was suggested to enhance visit time such that PCPs could engage in more robust decision-making conversations that clinic time pressures typically impede (Table 2). PCPs and patients also sought post-visit information opportunities like take-home handouts or patient portal notifications. Such tools could reinforce educational content; summarize which healthcare decisions were made; and support ongoing information retention. Both groups encouraged support staff (e.g., medical assistant, health educator) involvement in mammography, explaining the mammography process pre- or post-PCP visit. Many PCPs preferred this distribution of responsibilities because this could alleviate provider pressure so they could then invest time in a narrower role—facilitating SDM and ordering mammograms. PCPs acknowledged that support staff implementing patient education, as well as mammography care coordination, aligned well with the broader medical transition to team-based care.
DISCUSSION
This study elicited the needs of women with limited health literacy and PCPs to facilitate SDM in mammography for patients under 55, where guideline recommendations for mammography screening diverge, making SDM particularly important. We found that patients and PCPs identified gaps in knowledge across several dimensions that facilitated or impeded their participation in SDM. Several pathways to improving SDM were identified, including improving the provision of technical and process knowledge about mammography for patients outside of the PCP visit. Both perspectives underscored the need to improve both stakeholders’ capacity to engage in SDM for mammography.
The types of knowledge identified—embodied, process, and technical—provide insight into the relevant domains of information that are sought by patients. Women expressed ideas about their own embodied knowledge, most of which reflected how that knowledge should be used in decision-making about their health. PCPs might consider eliciting women’s perceptions of their own embodied knowledge as one entry point to discussions about personal values and preferences, both for decision-making and mammography participation. As has been found by others, the process knowledge dimension (i.e., where do I go? What happens to me when I go there?) is less often addressed de novo by PCPs relative to technical descriptions (i.e., the purpose of mammography, risk of finding cancer).19 Effectively, the practical process knowledge that is a fundamental priority for patients is not addressed by some physicians.
In reference to technical knowledge, we also add to the existing literature documenting that harms discussions were curtailed,36, 44 with the explanation that describing harms like false positives would be confusing to those with limited health literacy. Yet, research shows that younger patients who do not communicate with physicians about mammography are 3.2 times more likely to forgo mammograms after a false positive, and false positives are associated with delays in subsequent mammography.35 Communication about false positives with patients might promote adherence among women who begin mammography. If true, this would enhance the overall effectiveness of mammography at the population level by ensuring those who need screening continue to engage in it over time, where mortality benefits accrue.
Our findings support others’ calls for creating decision support tools that are patient-centered and improve patient–physician communication,29 as only two of twenty participating PCPs reported using educational supports. While several decision aids for mammography exist,45, 46 a vast majority have not explicitly been tested or designed for populations with limited health literacy. A meta-analysis shows that SDM interventions decrease outcome disparities for those with limited health literacy, with greater effects when information is tailored to those with limited health literacy.47 However, the quality of evidence and sample sizes for literacy subgroup comparisons warrants caution in interpreting these effects. More robust testing of interventions designed to increase SDM among populations with limited health literacy is needed to optimize the design of materials.
As a qualitative study conducted at a single institution, some findings may be context-specific and have limited generalizability. While we created and tested our interview guides with input from both the literature and stakeholders, some other relevant topics may not be well-represented in these data. Finally, this was an observational study conducted at a single point in time and relied solely on reports of interactions from either the patient or PCP. We were also unable to explore the interaction between PCP gender and the conduct of mammography-related SDM with these data, which may shed further light on the provision of process-related knowledge. Further studies should more firmly establish predictors of engagement in both SDM and mammography behaviors, including the interplay between cognitive, social, and health literacy–related contributors to behaviors. A strength of this study is that our findings do suggest specific areas for improving understanding about mammography and SDM in a population that has previously been underrepresented in studies on this topic. Future studies could, for example, explore how enhancing PCP engagement with the patient experience of mammography at their practice location could facilitate more patient-centered mammography counseling that includes process-focused information. Finally, although this study focused solely on women with limited health literacy, findings reflect the broader literature on mammography-related SDM and informational needs. This suggests there may be shared uncertainties about successfully conducting mammography-related SDM across the literacy spectrum.19
CONCLUSIONS
This study suggests that mammography counseling continues to be less robust than guidelines for SDM envision. Particular attention to the different types of knowledge (technical, process, embodied) is one way to enhance current practices. Our interviews suggest that a team-based approach to mammography counseling may be a practical solution that supports information sharing by a lay health educator and focused decision-making with clinicians. This study highlights strategies that might support patients with limited health literacy in better engaging in mammography discussions, including avoiding the assumption that mammography is common knowledge and sharing the process-focused information about breast cancer screening that patients desire.
Electronic supplementary material
(DOCX 19.2 kb)
Acknowledgments
Funding for this work was provided by the National Cancer Institute (1K07CA221899).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Oeffinger KC, Fontham ET, Etzioni R, et al. Breast Cancer Screening for Women at Average Risk: 2015 Guideline Update From the American Cancer Society. Jama. 2015;314(15):1599-1614. [DOI] [PMC free article] [PubMed]
- 2.Siu AL. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2016;164(4):279–296. doi: 10.7326/M15-2886. [DOI] [PubMed] [Google Scholar]
- 3.Couët N, Desroches S, Robitaille H, et al. Assessments of the extent to which health-care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expectations. 2015;18(4):542-561. [DOI] [PMC free article] [PubMed]
- 4.DuBenske LL, Schrager SB, Hitchcock ME, et al. Key Elements of Mammography Shared Decision-Making: a Scoping Review of the Literature. Journal of General Internal Medicine. 2018;33(10):1805-1814. [DOI] [PMC free article] [PubMed]
- 5.Haas JS, Sprague BL, Klabunde CN, et al. Provider Attitudes and Screening Practices Following Changes in Breast and Cervical Cancer Screening Guidelines. Journal of General Internal Medicine. 2016;31(1):52-59. [DOI] [PMC free article] [PubMed]
- 6.Martinez KA, Deshpande A, Ruff AL, Bolen SD, Teng K, Rothberg MB. Are Providers Prepared to Engage Younger Women in Shared Decision-Making for Mammography? Journal of Women's Health. 2018;27(1):24–31. doi: 10.1089/jwh.2016.6047. [DOI] [PubMed] [Google Scholar]
- 7.DuBenske LL, Schrager S, McDowell H, Wilke LG, Trentham-Dietz A, Burnside ES. Mammography Screening: Gaps in Patient's and Physician's Needs for Shared Decision-Making. The Breast Journal. 2017;23(2):210–214. doi: 10.1111/tbj.12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siedlikowski S, Ells C, Bartlett G. Scrutinizing screening: a critical interpretive review of primary care provider perspectives on mammography decision-making with average-risk women. Public Health Rev. 2018;39:15–15. doi: 10.1186/s40985-018-0092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Radhakrishnan A, Nowak SA, Parker AM, Visvanathan K, Pollack CE. Physician Breast Cancer Screening Recommendations Following Guideline Changes: Results of a National Survey. JAMA Intern Med. 2017;177(6):877–878. doi: 10.1001/jamainternmed.2017.0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davey C, White V, Gattellari M, Ward JE. Reconciling population benefits and women's individual autonomy in mammographic screening: in-depth interviews to explore women's views about 'informed choice'. Australian and New Zealand Journal of Public Health. 2005;29(1):69–77. doi: 10.1111/j.1467-842X.2005.tb00752.x. [DOI] [PubMed] [Google Scholar]
- 11.Davey HM, Barratt AL, Butow PN, Houssami N. The impact of different criteria for selecting information to be provided to women undergoing diagnostic breast tests. Patient Education and Counseling. 2008;71(1):86–94. doi: 10.1016/j.pec.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Davis S, Stewart S, Bloom J. Increasing the accuracy of perceived breast cancer risk: results from a randomized trial with Cancer Information Service callers. Preventive Medicine. 2004;39(1):64–73. doi: 10.1016/j.ypmed.2004.02.043. [DOI] [PubMed] [Google Scholar]
- 13.Edwards A, Unigwe S, Elwyn G, Hood K. Effects of communicating individual risks in screening programmes: Cochrane systematic review. BMJ. 2003;327(7417):703–709. doi: 10.1136/bmj.327.7417.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gillespie C. The experience of risk as ‘measured vulnerability’: health screening and lay uses of numerical risk. Sociology of Health & Illness. 2012;34(2):194–207. doi: 10.1111/j.1467-9566.2011.01381.x. [DOI] [PubMed] [Google Scholar]
- 15.Gunn C, Bokhour B, Parker V, Parker P, Bandos H, Holmberg C. Exploring Explanatory Models of Risk in Breast Cancer Risk Counseling Discussions. International Academy for Communication in Healthcare; 2014; Amsterdam, Netherlands.
- 16.Stacey D, Hill S, McCaffery K, Boland L, Lewis KB, Horvat L. Shared Decision Making Interventions: Theoretical and Empirical Evidence with Implications for Health Literacy. Stud Health Technol Inform. 2017;240:263–283. [PubMed] [Google Scholar]
- 17.Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: Evidence, models and interventions. Patient Education and Counseling. 2006;61(3):319–341. doi: 10.1016/j.pec.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Shi W, Nagler R, Fowler E, Gollust S. Predictors of Women's Awareness of the Benefits and Harms of Mammography Screening and Associations with Confusion, Ambivalence, and Information Seeking. Health communication. 2019. [DOI] [PubMed]
- 19.Mazor KM, Rubin DL, Roblin DW, et al. Health literacy-listening skill and patient questions following cancer prevention and screening discussions. Health expectations : an international journal of public participation in health care and health policy. 2016;19(4):920-934. [DOI] [PMC free article] [PubMed]
- 20.Manning M, Albrecht TL, Yilmaz-Saab Z, Penner L, Norman A, Purrington K. Explaining between-race differences in African-American and European-American women's responses to breast density notification. Social Science & Medicine. 2017;195:149–158. doi: 10.1016/j.socscimed.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manning M, Purrington K, Penner L, Duric N, Albrecht TL. Between-race differences in the effects of breast density information and information about new imaging technology on breast-health decision-making. Patient Education and Counseling. 2016;99(6):1002–1010. doi: 10.1016/j.pec.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson EE, Hoskins KJ. Individual Breast Cancer Risk Assessment in Underserved Populations: Integrating Empirical Bioethics and Health Disparities Research. Journal of Health Care for the Poor and Underserved. 2012;23(4):34–46. doi: 10.1353/hpu.2012.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spring LM, Marshall MR, Warner ET. Mammography decision making: Trends and predictors of provider communication in the Health Information National Trends Survey, 2011 to 2014. Cancer. 2017;123(3):401–409. doi: 10.1002/cncr.30378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chang H-L, Li F-S, Lin C-F. Factors Influencing Implementation Of Shared Medical Decision Making In Patients With Cancer. Patient preference and adherence. 2019;13:1995–2005. doi: 10.2147/PPA.S217561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muscat DM, Shepherd HL, Morony S, et al. Can adults with low literacy understand shared decision making questions? A qualitative investigation. Patient education and counseling. 2016;99(11):1796-1802. [DOI] [PubMed]
- 26.Seo J, Goodman MS, Politi M, Blanchard M, Kaphingst KA. Effect of Health Literacy on Decision-Making Preferences among Medically Underserved Patients. Medical decision making : an international journal of the Society for Medical Decision Making. 2016;36(4):550–556. doi: 10.1177/0272989X16632197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Komenaka I, Nodora J, Hsu C, et al. Association of Health Literacy with Adherence to Screening Mammography Guidelines. Obstetrics and Gynecology. 2015;125(4):852-859. [DOI] [PubMed]
- 28.Keating NL, Pace LE. Breast cancer screening in 2018: Time for shared decision making. JAMA. 2018;319(17):1814–1815. doi: 10.1001/jama.2018.3388. [DOI] [PubMed] [Google Scholar]
- 29.Schrager S, Burnside ES. Breast Cancer Screening in Primary Care: A Call for Development and Validation of Patient-Oriented Shared Decision-Making Tools. Journal of Women's Health. 2019;28(2):114–116. doi: 10.1089/jwh.2017.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borrayo EA. Where's Maria? A video to increase awareness about breast cancer and mammography screening among low-literacy Latinas. Preventive Medicine. 2004;39(1):99–110. doi: 10.1016/j.ypmed.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 31.Brown SM, Culver JO, Osann KE, et al. Health literacy, numeracy, and interpretation of graphical breast cancer risk estimates. Patient Education and Counseling. 2011;83(1):92-98. [DOI] [PMC free article] [PubMed]
- 32.Garcia-Retamero R, Cokely ET. Designing Visual Aids That Promote Risk Literacy: A Systematic Review of Health Research and Evidence-Based Design Heuristics. Hum Factors. 2017;59(4):582–627. doi: 10.1177/0018720817690634. [DOI] [PubMed] [Google Scholar]
- 33.Marcus EN, Koru-Sengul T, Miao F, Yepes M, Sanders L. How do Breast Imaging Centers Communicate Results to Women with Limited English Proficiency and Other Barriers to Care? Journal of Immigrant and Minority Health. 2014;16(3):401–408. doi: 10.1007/s10903-012-9771-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schapira MM, Sprague BL, Klabunde CN, et al. Inadequate Systems to Support Breast and Cervical Cancer Screening in Primary Care Practice. Journal of General Internal Medicine. 2016;31(10):1148-1155. [DOI] [PMC free article] [PubMed]
- 35.DeFrank JT, Rimer BK, Bowling JM, Earp JA, Breslau ES, Brewer NT. Influence of false-positive mammography results on subsequent screening: do physician recommendations buffer negative effects? Journal of Medical Screening. 2012;19(1):35–41. doi: 10.1258/jms.2012.011123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoffman RM, Lewis CL, Pignone MP, et al. Decision-Making Processes for Breast, Colorectal, and Prostate Cancer Screening: The DECISIONS Survey. Medical Decision Making. 2010;30(5 suppl):53S–64S. doi: 10.1177/0272989X10378701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paasche-Orlow MK, Wolf MS. The Causal Pathways Linking Health Literacy to Health Outcomes. American journal of health behavior. 2007;31(1):S19–S26. doi: 10.5993/AJHB.31.s1.4. [DOI] [PubMed] [Google Scholar]
- 38.Bann CM, McCormack LA, Berkman ND, Squiers LB. The Health Literacy Skills Instrument: a 10-item short form. Journal of health communication. 2012;17(Suppl 3):191–202. doi: 10.1080/10810730.2012.718042. [DOI] [PubMed] [Google Scholar]
- 39.Ando H, Cousins R, Young C. Achieving saturation in thematic analysis: development and refinement of a codebook. Comprehensive Psychology. 2014;3(4):1–7. [Google Scholar]
- 40.Schreier M. Qualitative content analysis in practice. Thousand Oaks, CA: Sage; 2012. [Google Scholar]
- 41.Cho JY, Lee E-H. Reducing Confusion about Grounded Theory and Qualitative Content Analysis: Similarities and Differences. The Qualitative Report. 2014;19(64):1–20. [Google Scholar]
- 42.Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis: A Methods Sourcebook. 4. Thousand Oaks, CA: Sage Publications; 2020. [Google Scholar]
- 43.Charmaz K. Constructing Grounded Theory: A practical guide through qualitative analysis. Thousand Oaks, CA: SAGE Publications, Inc.; 2006. [Google Scholar]
- 44.Hoffmann TC, Del Mar C. Patients’ expectations of the benefits and harms of treatments, screening, and tests: A systematic review. JAMA Internal Medicine. 2015;175(2):274–286. doi: 10.1001/jamainternmed.2014.6016. [DOI] [PubMed] [Google Scholar]
- 45.Breast Screening Decisions (2014) http://breastscreeningdecisions.com/#/. Accessed May 15, 2016.
- 46.Scariati P, Nelson L, Watson L, Bedrick S, Eden KB. Impact of a decision aid on reducing uncertainty: pilot study of women in their 40s and screening mammography. BMC Medical Informatics and Decision Making. 2015;15:89. doi: 10.1186/s12911-015-0210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Durand M-A, Carpenter L, Dolan H, et al. Do Interventions Designed to Support Shared Decision-Making Reduce Health Inequalities? A Systematic Review and Meta-Analysis. PLoS ONE. 2014;9(4):e94670. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 19.2 kb)