Abstract
Objectives
To comprehensively map the existing evidence assessing the impact of travel-related control measures for containment of the SARS-CoV-2/COVID-19 pandemic.
Design
Rapid evidence map.
Data sources
MEDLINE, Embase and Web of Science, and COVID-19 specific databases offered by the US Centers for Disease Control and Prevention and the WHO.
Eligibility criteria
We included studies in human populations susceptible to SARS-CoV-2/COVID-19, SARS-CoV-1/severe acute respiratory syndrome, Middle East respiratory syndrome coronavirus/Middle East respiratory syndrome or influenza. Interventions of interest were travel-related control measures affecting travel across national or subnational borders. Outcomes of interest included infectious disease, screening, other health, economic and social outcomes. We considered all empirical studies that quantitatively evaluate impact available in Armenian, English, French, German, Italian and Russian based on the team’s language capacities.
Data extraction and synthesis
We extracted data from included studies in a standardised manner and mapped them to a priori and (one) post hoc defined categories.
Results
We included 122 studies assessing travel-related control measures. These studies were undertaken across the globe, most in the Western Pacific region (n=71). A large proportion of studies focused on COVID-19 (n=59), but a number of studies also examined SARS, MERS and influenza. We identified studies on border closures (n=3), entry/exit screening (n=31), travel-related quarantine (n=6), travel bans (n=8) and travel restrictions (n=25). Many addressed a bundle of travel-related control measures (n=49). Most studies assessed infectious disease (n=98) and/or screening-related (n=25) outcomes; we found only limited evidence on economic and social outcomes. Studies applied numerous methods, both inferential and descriptive in nature, ranging from simple observational methods to complex modelling techniques.
Conclusions
We identified a heterogeneous and complex evidence base on travel-related control measures. While this map is not sufficient to assess the effectiveness of different measures, it outlines aspects regarding interventions and outcomes, as well as study methodology and reporting that could inform future research and evidence synthesis.
Keywords: public health, infectious diseases, diabetic foot
Strengths and limitations of this study.
We applied systematic and standardised methods at all stages and have produced a comprehensive evidence map of travel-related control measures for containment of the SARS-CoV-2/COVID-19 pandemic.
For title/abstract and full-text screening, we developed guidance documents and conducted piloting exercises to ensure consistency among review authors; we additionally collected and clarified all uncertainties on a rolling basis through daily team calls.
We conducted searches in three major health-related databases and two COVID-specific databases; however, it is likely that most studies assessing economic and social outcomes are found in other databases.
The unspecific and inconsistent reporting of primary studies with regard to interventions, especially when a package of control measures was investigated, meant that determining eligibility, as well as summarising and mapping these studies, was challenging.
We did not include travel warning or travel advice in the evidence map, which limits the scope of this map.
Introduction
In December 2019, the occurrence of the SARS-CoV-2 was reported in Wuhan, China. Over the next weeks, the virus and the associated respiratory disease referred to as COVID-19 spread further into China and other parts of Asia including Japan, South Korea and Thailand.1 By mid-March 2020, when the WHO declared COVID-19 a global pandemic, cases had been observed in over 100 countries and territories across the globe.2
According to WHO, various travel-related control measures, such as entry/exit screening, travel bans to and/or from specific areas within or between countries, and quarantine of travellers have since been implemented by most countries around the world to contain and mitigate the spread of SARS-CoV-2 and COVID-19.3 Following the early-stage responses in Asian countries, strict measures, such as border closures and drastic reductions in airline travel, have been put into place in most countries around the world, starting in February 2020 and continuing into May 2020. While in the context of a rapidly evolving pandemic decisions often need to be made even in the absence of high quality evidence, efforts to identify and synthesise the best available evidence will help inform whether the currently implemented measures should be sustained, adapted or lifted. Where possible, decisions need to be based on evidence regarding the effectiveness of these measures in contributing to the control of the pandemic, as well as regarding the associated economic and social impacts. They will also need to take into account short-term and longer term costs, acceptability and feasibility of such measures.
Travel-related control measures have been assessed through systematic or narrative reviews in the context of previous epidemics and pandemics, such as influenza, severe acute respiratory syndrome (SARS-CoV-1/SARS) and Middle East respiratory syndrome (MERS-CoV/MERS). Regarding the containment of influenza, these reviews have examined the effectiveness of a broad set of measures,4–6 as well as the effectiveness of specific measures, such as entry/exit screening6 7; they have also assessed the economic implications of various pharmaceutical and non-pharmaceutical interventions during influenza pandemics.8 9 Effectiveness of measures, such as international travel bans and entry/exit screening, have also been examined in reviews of SARS and MERS.7 10 To date and to the best of our knowledge, the evidence on travel-related control measures for the control of the current pandemic has not been systematically assessed.
In this paper, we aim to systematically identify and map the existing evidence assessing the impact of travel-related control measures (ie, border closures, travel restrictions and bans, entry and exit screening, quarantine/isolation of travellers crossing borders and multiple interventions combined) for containment of the SARS-CoV-2/COVID-19 pandemic, drawing on evidence from the current pandemic, as well as on evidence in relation to SARS, MERS and influenza. This evidence map was commissioned by the WHO to serve as an important resource for researchers and policymakers in providing an overview of the currently available evidence in relation to various travel-related control measures to contain the COVID-19 pandemic. In itself, the evidence map is not sufficient to assess the effectiveness of different measures. Instead, it provides an important basis for decisions regarding the need for and possibility to conduct primary research as well as more specific evidence synthesis (eg, regarding a specific category of control measures or a specific type of studies).
Methods
Search strategy
We designed the evidence map in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) reporting guideline, and implemented the entire project within ten days (see online supplemental file S1) for the completed PRISMA-ScR checklist). We searched the following databases: (1) Ovid MEDLINE ALL (1946–present); (2) Embase.com (Elsevier); (3) Science Citation Index Expanded (1900–present), Social Sciences Citation Index (1900–present) and Emerging Sources Citation Index (2015–present) (Web of Science); (4) the US Centers for Disease Control and Prevention’s COVID-19 Research Articles Downloadable Database (includes published articles, as well as grey literature, such as preprints) and (5) WHO COVID-19 Database (includes published articles only).
bmjopen-2020-041619supp001.pdf (1.6MB, pdf)
The initial search strategy was developed for MEDLINE (see online supplemental file S2) and further adapted for the other databases. All database searches were conducted up to 3 May 2020. The search strategies were designed and conducted by an experienced information specialist. The searches were conducted in English. Where database functionality allowed for it, we limited the search results to Armenian, English, French, German, Italian and Russian, based on the language capacity of the research team and considered studies for inclusion published in all of these languages. We also conducted forward and backward citation searches of all relevant (systematic) reviews identified through the database searches (see online supplemental file S3) up to 6 May 2020 in Scopus (Elsevier).
Eligibility criteria
We determined eligibility of studies based on the investigated population/context, intervention, outcome and study type.
Regarding the population/context, this evidence map draws on direct evidence from human populations susceptible to the current SARS-CoV-2/COVID-19, as well as indirect evidence from a set of other relevant respiratory infectious diseases. To help define a set of diseases that is most similar and relevant to COVID-19, we used the following criteria: (1) diseases of viral origin; (2) mode of transmission primarily airborne via droplets/aerosols (as well as person to person); (3) acute disease with the potential to cause an epidemic/pandemic; (4) similar clinical features (ie, non-specific febrile illness with the potential to develop into pneumonia and acute respiratory distress syndrome; difficult diagnosis based on clinical features during transmission-relevant phase, including the period prior to symptom development and during early-stage symptoms); and (5) unavailability of a vaccine and/or difficulty to contain an outbreak through vaccination. As a result, we considered:
SARS-CoV-2/COVID-19.
SARS-CoV-1/SARS.
MERS-CoV/MERS.
Influenza.
Studies in all other populations/contexts, including evidence on infectious diseases less relevant to the current SARS-CoV-2/COVID-19 pandemic (eg, avian influenza, Ebola, meningitis, HIV/AIDS, tuberculosis, dengue, plague, cholera, fever, smallpox, measles or Zika virus) were excluded.
Regarding the intervention, we considered travel-related control measures affecting human travel across national or subnational borders, specifically:
Closure of borders (borders closed to entry and/or exit).
Travel bans (suspension of flights, ground crossing, ship itineraries, refusal of entry or travel and visa suspension/denial) between countries and between regions and large cities within countries.
Travel restrictions (ie, varying levels of travel reductions) between countries and between regions and large cities within countries).
Entry/exit screening (eg, temperature measurement, health questionnaire, thermography, physical examination, laboratory tests, passive observation and/or follow-up quarantine) at airports, ports, land borders and train stations.
Quarantine/isolation of travellers from affected regions (at borders, at designated institutions or at home).
Any combination of the above measures and/or with other control measures (eg, combination of border closure and school closure).
All other interventions were excluded. This comprised those not directly related to travel (eg, community-based quarantine, hygiene measures and bans on mass gatherings), those related to the movement of animals or goods, travel warnings or travel advice issued by the WHO or national governments, situations affecting travel but not representing travel-related control measures (eg, school holidays) and those solely concerned with the effectiveness of laboratory tests rather than their implementation as part of an entry/exit screening procedure.
Regarding outcomes, we considered those assessing the quantitative impacts of the interventions on:
Infectious disease outcomes (eg, number/proportion of cases, number/proportion of deaths, time to/delay in epidemic arrival or peak, reproduction number, healthcare demand and utilisation).
Screening outcomes (eg, number/proportion of persons screened and number/proportion of those screened identified as cases).
Other health outcomes (eg, psychosocial impact).
Economic outcomes (eg, travel volumes, costs of measures implemented and losses to different economic sectors).
Social outcomes (eg, stigmatisation/discrimination of foreigners, xenophobia and migration volumes).
All other outcomes, such as those on the human rights and legal implications of interventions, were excluded.
Regarding study types, we considered all types of empirical studies that quantitatively evaluate impact (eg, epidemiological, modelling, simulations and econometric studies). All other study types, including qualitative studies, diagnostic studies focused on test performance and non-empirical studies (eg, commentaries, narrative and systematic reviews) were excluded.
Study selection
After deduplication, all titles and abstracts were screened by one reviewer (shared among several team members), excluding only those studies that were clearly irrelevant. For all studies deemed potentially relevant or unclear at the title/abstract screening stage, one reviewer screened the full text. At this stage, a final decision regarding eligibility was made. We adopted a very inclusive approach: any unclear cases were discussed with a second reviewer, and remaining uncertainties were resolved with involvement of a third reviewer and/or the whole review team. In addition, all studies excluded at the full-text screening stage based on the intervention (ie, not addressing travel-related control measures) were double-checked by a second reviewer to make sure that no relevant studies were excluded.
We used Endnote to manage collection and deduplication of records. For title and abstract screening, we used Rayyan, a web-based application designed for citation screening for systematic reviews.11 We documented reasons for the exclusion of full texts and reported those using Microsoft Excel.
For both the title/abstract and full-text screening stages, we developed screening guidance forms to ensure that all reviewers screen similarly and consistently. We discussed inconsistencies and challenges encountered within the review team, after having screened approximately 300 titles/abstracts and 50 full texts and subsequently refined the screening guidance. We additionally collected and clarified all uncertainties in screening on a rolling basis. These were discussed in daily online meetings to ensure consistency in screening across multiple reviewers and that any questions and comments were addressed.
Data extraction
One reviewer extracted study characteristics and data into the predefined categories of the data extraction form in Microsoft Excel (see online supplemental file S4). The extraction form was pilot-tested in the review team. The following categories were covered by the extraction form: population, setting and context; characterisation of the respiratory pathogen/disease (ie, SARS-CoV-2/COVID-19, SARS CoV-1/SARS, MERS CoV/MERS and influenza), types of interventions (eg, entry/exit screening, border closure, quarantine of travellers and travel bans), comparisons (where available), outcomes of interest (eg, health, economic and social impact) and study designs (eg, epidemiological study and modelling study).
Mapping
We charted the extracted data based on categories and present findings in a tabular, narrative or graphical manner. Most of these categories were defined a priori, while one category, namely, geographical setting, was adapted post hoc. Specifically, we sought to define, summarise and present clusters of studies based on the pathogen/disease (ie, SARS-CoV-2/COVID-19, SARS-CoV-1/SARS, MERS-CoV/MERS and influenza), type of intervention (border closure, entry/exist screening including follow-up measures, such as isolation of positive cases, travel ban, travel-related quarantine in the absence of entry/exit screening, travel restrictions and multiple travel-related control measures combined), timing of the intervention (ie, early phase, local transmission phase, postpeak phase and unclear phase), outcomes of interest (ie, infectious disease outcomes, screening outcomes, other health outcomes, economic and social outcomes) and study designs (eg, epidemiologic study and modelling study). All data presented in the tables, text and graphics were double-checked by a second reviewer with an emphasis on accuracy in reporting on populations, interventions and outcomes and in relation to consistency of presentation.
Patient and public involvement
Considering the time constraints and the nature of this research (ie, a rapid systematic evidence map), it was conducted without patient and public involvement.
Results
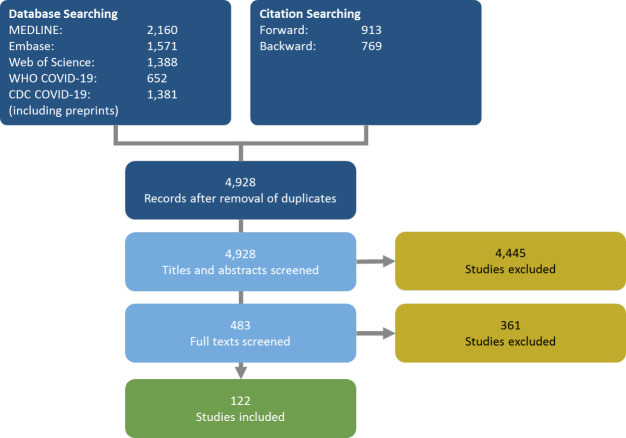
Database searches yielded a total of 4928 unique records. Through snowballing of reviews identified through the database searches, we identified an additional 1700 studies. During the title/abstract screening stage, we excluded 4445 records as clearly irrelevant. We subsequently assessed the full texts of 483 records and excluded another 361 records. Overall, we included 122 studies in this evidence map (see online supplemental file S5 for the full list). Of these, 80 were journal articles, 41 were preprints and 1 was a report. Figure 1 provides an overview of our searching and screening procedures.
Figure 1.
Flow chart of studies identified and included during different stages of searching and screening.
Characteristics of included studies
The 122 included studies were characterised by substantial heterogeneity in relation to the countries and populations targeted, the diseases addressed, the types of travel-related control measures examined (sometimes assessed against a range of other interventions to contain an epidemic/pandemic) and the numerous outcomes assessed. They comprise both studies that are inferential in nature and studies that are descriptive in nature, varying greatly in the specific methods applied; notably, many of the studies addressing COVID-19 were preprints. We summarise these aspects below and provide a description of each study in table 1.
Table 1.
Characteristics of included studies
| Study | Study type | WHO region | Geographical setting | Region protected by travel-related measure | Region restricted by travel-related measure | Disease | Intervention category | Outcome type |
| Adekunle 202014 (preprint) | Inferential | WPR | Island state | Australia | China, Iran, South Korea and Italy | COVID-19 | Travel ban | Number or proportion of cases |
| Aleta 202015 (preprint) | Inferential | WPR | Non-island state | Regions within China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Anonymous 200316 | Descriptive | AMR | Non-island state | Vancouver, Toronto, other parts of Canada | All other countries | SARS | Entry/exit screening | Detection of high risk persons or cases |
| Anzai 202017 | Inferential | WPR | Non-island state | Multiple countries | China | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; temporal development of epidemic |
| Arima 202018 | Descriptive | WPR | Island state | Japan | China | COVID-19 | Entry/exit screening; travel-related quarantine |
Detection of high risk persons or cases |
| Arino 200719 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Hypothetical infectious disease | Travel restriction | Number or proportion of cases |
| Bajardi 201120 | Inferential | All | Non-island state | All countries | Mexico | Influenza (H1N1 2009 pandemic) | Travel ban; travel restriction: land |
Temporal development of epidemic |
| Banholzer 202021 (preprint) | Inferential | EUR, WPR and AMR | Non-island state | Austria, Australia, Belgium, Canada Denmark, France, Finland, Italy, Norway, Switzerland, Sweden, Spain and USA | All other countries | COVID-19 | Border closure | Number or proportion of cases |
| Bolton 201222 | Inferential | WPR | Non-island state | Mongolia | Neighbouring countries | Influenza (H1N1 2009 pandemic) | Travel restriction | Number or proportion of cases |
| Boyd 201723 | Inferential | WPR | Island state | New Zealand | All other countries | Hypothetical infectious disease | Border closure | Costs |
| Boyd 201824 | Inferential | WPR | Island state | New Zealand | All other countries | Hypothetical infectious disease | Border closure | Costs |
| Caley 200725 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza | Entry/exit screening; travel restriction: air |
Detection of high risk persons or cases; temporal development of epidemic |
| Chang 202026 (preprint) | Inferential | WPR | Island state | Taiwan | Different cities in Taiwan | COVID-19 | Travel restriction | Number or proportion of cases; temporal development of epidemic |
| Cheng 202027 | Descriptive | WPR | Island state | Taiwan | China | COVID-19 | Exit/entry screening; travel-related quarantine |
Number or proportion of cases |
| Chinazzi 202028 | Inferential | WPR | Non-island state | Other regions of China, all other countries | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Chiyomaru 202029 (preprint) | Inferential | Non-island state | Multiple countries | Multiple countries | COVID-19 | Travel ban | Number or proportion of cases | |
| Chong 201230 | Inferential | WPR | Quasi-island state | Hong Kong | All other countries | Influenza (H1N1 2009 pandemic) | Travel restriction: land, air and maritime | Number or proportion of cases; temporal development of epidemic |
| Chung 201531 | Inferential | Non-island state | Multiple countries | Multiple countries | SARS; 2006 Avian influenza; 2009 Swine influenza H1N1 | Travel restriction: air | Industry impact | |
| Ciofi 200832 | Inferential | EUR | Non-island state | Italy | Italy and all other countries | Influenza | Travel restriction: air | Number or proportion of cases; temporal development of epidemic |
| Clifford 202033
(preprint) |
Inferential | n.a. | Hypothetical | Hypothetical | All other countries | COVID-19 | Entry/exit screening | Detection of high risk persons or cases; temporal development of epidemic |
| Colizza 200734 | Inferential | All | Non-island state | All countries | All countries | Influenza | Travel restriction: air | Number or proportion of cases; temporal development of epidemic |
| Cooper 200635 | Inferential | All | Non-island state | All countries | All countries | Influenza | Travel restriction: air | Temporal development of epidemic |
| Costantino 202036 (preprint) | Inferential | WPR | Island state | Australia | All other countries | COVID-19 | Travel ban | Number or proportion of cases; number or proportion of deaths; temporal development of epidemic |
| Cowling 202037 | Inferential | WPR | Quasi-island state | Hong Kong | China, South Korea, Iran, Italy and affected regions in France, Germany, Japan, and Spain, Schengen Area, Macau and Taiwan. | COVID-19 | Travel restriction: air and land; travel ban; travel-related quarantine; border closure |
Reproduction number; number or proportion of cases; acceptability |
| Dandekar 202038 (preprint) | Inferential | WPR, EUR and AMR | Island state; quasi-island state |
China, Italy, South Korea and USA | All other countries | COVID-19 | Multiple travel-related control measures | Reproduction number |
| de Vlas 200939 | Descriptive | WPR | Non-island state | Regions of China | Regions of China | SARS | Travel-related quarantine | Reproduction number |
| Ediriweera 202040 (preprint) | Inferential | SEAR | Island state | Sri Lanka | All other countries | COVID-19 | Multiple travel-related control measures; travel-related quarantine |
Number or proportion of cases; healthcare resources |
| Eichner 200941 | Inferential | WPR | Hypothetical | Hypothetical | All other countries | Influenza (pandemic) | Travel restriction: air | Probability of epidemic |
| Epstein 200742 | Inferential | All | Non-island state | All countries (focus on USA) | All countries | Influenza | Travel restriction: air | Number or proportion of cases; temporal development of epidemic |
| Fang 202043 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Ferguson 200644 | Inferential | AMR | Island state; quasi-island state |
USA and UK | Countries connected by air traffic | Influenza (pandemic) | Border controls; travel restrictios | Number or proportion of cases; temporal development of epidemic |
| Flahault 200645 | Inferential | n.a. | Quasi-island state | 52 international cities and surrounding regions | Cities connected via air traffic | Influenza (pandemic) | Travel restriction: air | Number or proportion of cases |
| Fujita 201146 | Inferential | WPR | Island state | Regions in Japan | USA, Canada and Mexico | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Detection of high risk persons or cases |
| Germann 200647 | Inferential | AMR | Non-island state | USA | Influenza (pandemic) | Travel restriction: air | Number or proportion of cases | |
| Glass 200648 | Inferential | n.a. | Non-island state | Non-infected region | Non-infected region | SARS | Entry/exit screening | Probability of epidemic |
| Gostic 202049 | Inferential | All | Island state | All countries | All countries | COVID-19 | Entry/exit screening | Detection of high risk persons or cases |
| Gostic 201550 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | SARS; MERS; influenza (H1N1 2009 pandemic) | Entry/exit screening | Detection of high-risk persons or cases |
| Goubar 200951 | Inferential | EUR | Island state; quasi-island state |
Germany and UK | China and Hong Kong | SARS | Entry/exit screening | Number or proportion of cases |
| Gunaratnam 201452 | Descriptive | WPR | Island state | Australia | All other countries | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Detection of high-risk persons or cases |
| Hale 201253 | Descriptive | WPR | Island state | New Zealand | Initially USA, Canada, Mexico, then all other countries | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Detection of high-risk persons or cases |
| Hamidouche 202054 (preprint) |
Inferential | AFR | Non-island state | Algeria | All neighbouring and connected (via air) countries | COVID-19 | Border closure; travel ban; travel-related quarantine |
Number or proportion of cases; reproduction number |
| He 202055 (preprint) |
Inferential | WPR | Island state; quasi-island state |
China, South Korea, Italy and Iran | Italy (Lombardy, Veneto, Emilia-Romagna, Piedmont and Marche) and China (Zhejiang). | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; temporal development of epidemic |
| Hien 201056 | Inferential | WPR | Non-island state | Vietnam | Countries with confirmed cases of 2009 H1N1 | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Detection of high-risk persons or cases |
| Hollingsworth 200657 | Inferential | n.a. | Hypothetical | Hypothetical | Countries connected via air traffic | SARS and influenza | Travel restriction: air | Number or proportion of cases; temporal development of epidemic |
| Hossain 202058 (preprint) | Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Temporal development of epidemic |
| Hou 202059 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; reproduction number |
| Hsieh 200760 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza (endemic) | Travel ban | Reproduction number |
| Hsieh 200661 | Inferential | WPR | Island state | Taiwan | Countries with SARS cases | SARS | Travel-related quarantine | Number or proportion of cases |
| Jia 202062 | Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; other |
| Jiang 202063 (preprint) |
Inferential | WPR | Non-island state | Regions of China | Regions of China | COVID-19 | Multiple travel-related control measures | Other |
| Kerneis 200864 | Inferential | n.a. | Non-island state | 52 international cities and surrounding regions | 52 international cities and surrounding regions | Influenza (pandemic) | Travel restriction: air | Number or proportion of cases; temporal development of epidemic |
| Khan 201365 | Inferential | AMR | Non-island state | Other countries | Mexico | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Detection of high-risk persons or cases; other |
| Kim 201766 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Hypothetical infectious disease | Entry/exit screening | Reproduction number |
| Kong 202067 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 and influenza | Multiple travel-related control measures | Number or proportion of cases |
| Kraemer 202068 | Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Kuo 200969 | Descriptive | WPR | Island state | Taiwan | All affected countries (eg, Mexico, USA and Canada) | Influenza (H1N2 2009 pandemic) | Entry/exit screening | Detection of high-risk persons or cases |
| Lai 202070 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Lam 201171 | Inferential | WPR | Quasi-island state | Hong Kong | All other countries | Influenza (H1N1 2009 pandemic) | Travel restriction | Probability of epidemic; temporal development of epidemic |
| Lau 202072 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; temporal development of epidemic |
| Lee 201273 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza (H1N1 2009 pandemic) | Travel restriction | Temporal development of epidemic |
| Li 202074 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Lin 202075 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Reproduction number; other |
| Linka 202076 (preprint) |
Inferential | EUR | Non-island state | All European countries | All European countries | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Liu 200677 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Hypothetical infectious disease | Entry/exit screening | Reproduction number |
| Liu 202078 | Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Liu 2020a79 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Cities outside of Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Malmberg 202080 (preprint) | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Hypothetical infectious disease | Travel restriction; travel-related quarantine | Probability of epidemic |
| Malone 200981 | Inferential | AMR | Non-island state | USA | Asia | Influenza (pandemic) | Entry/exit screening | Detection of high-risk persons or cases; number or proportion of cases; number of deaths |
| Mandal 202082 | Inferential | SEAR | Non-island state | India | China, Hong Kong, Singapore, Thailand, Japan, South Korea, Iran and Italy | COVID-19 | Entry/exit screening | Temporal development of epidemic; number or proportion of cases |
| Marcelino 201283 | Inferential | All | Non-island state | All countries | Mexico city | Influenza (pandemic) | Travel restriction: air | Number or proportion of cases |
| Mbuvha 202084 (preprint) | Inferential | AFR | Non-island state | South Africa | South Africa and the all other countries | COVID-19 | Travel ban | Number or proportion of cases; temporal development of epidemic |
| Mondal 202085 (preprint) |
Inferential | SEAR | Non-island state | India | India | COVID-19 | Travel ban | Number or proportion of cases |
| Moriarty 202086 | Inferential | WPR and AMR | Non-island state | Japan, USA, home countries of cruise ship passengers | Home countries of cruise ships | COVID-19 | Travel-related quarantine | Detection of high risk persons or cases |
| Mummert 201387 | Inferential | AMR | Non-island state | USA | Mexico | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Number or proportion of cases |
| Muraduzzaman 201888 |
Descriptive | SEAR | Non-island state | Bangladesh | Saudi Arabia | MERS | Entry/exit screening | Detection of high-risk persons or cases |
| Nakata 201589 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Hypothetical infectious disease | Travel restriction | Reproduction number |
| Nigmatulina 200990 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza | Travel restriction | Number or proportion of cases |
| Nishiura 200991 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza (pandemic) | Travel-related quarantine | Detection of high-risk persons or cases |
| Odendaal 202092 (preprint) |
Inferential | AMR | Non-island state | USA | China and other affected countries | COVID-19 | Travel restriction | Number or proportion of cases |
| Pan 202093 (preprint) | Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Pan 2020a94 | Inferential | WPR | Non-island state | China | China | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; reproduction number |
| Pang 200395 | Descriptive | WPR | Non-island state | Beijing | All other countries | SARS | Entry/exit screening | Number or proportion of cases |
| Pinkas 200396 | Descriptive | EUR | Non-island state | Poland | All other countries | COVID-19 | Entry/exit screening; border closure; travel ban; travel-related quarantine |
Number or proportion of cases |
| Pitman 200597 | Descriptive | EUR | Quasi-island state | UK | Any of the top 100 sources of international airline passengers | SARS and influenza | Entry/exit screening | Detection of high-risk persons or cases |
| Priest 201398 | Descriptive | WPR | Island state | New Zealand | Australia | Influenza (type A and B) | Entry/exit screening | Detection of high-risk persons or cases |
| Pullano 202099 | Inferential | WPR | Non-island state | Other regions of China and European countries | Wuhan | COVID-19 | Travel ban | Probability of epidemic |
| Qiu 2020100 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Quilty 2020101 (preprint) |
Inferential | WPR | Non-island state | Beijing, Chongqing, Hangzhou and Shenzhen | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; probability of epidemic |
| Ray 2020102 |
Inferential | SEAR | Non-island state | India | All other countries | COVID-19 | Travel ban | Number or proportion of cases |
| Sakaguchi 2012103 | Descriptive | WPR | Island state | Japan | Mexico, USA and Canada | Influenza (A H1N1 2009 pandemic) | Entry/exit screening | Detection of high-risk persons or cases |
| Samaan 2004104 | Descriptive | WPR | Island state | Australia | All countries affected by SARS | SARS | Entry/exit screening | Detection of high-risk persons or cases |
| Sang 2012105 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | SARS | Entry/exit screening | Reproduction number; temporal development of epidemic; number or proportion of cases; number or proportion of deaths |
| Scala 2020106 (preprint) |
Inferential | EUR | Non-island state | Individual regions of Italy | Individual regions of Italy | COVID-19 | Travel restriction | Temporal development of epidemic |
| Scalia Tomba 2008107 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza (pandemic) | Travel restriction/border control | Temporal development of epidemic |
| Shi 2020108 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Song 2020109Wang 2020110 | Inferential | WPR | Non-island state | Other regions of China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; reproduction number |
| St. John 2005111 | Descriptive | AMR | Non-island state | Canada | All other countries | SARS | Entry/exit screening | Detection of high-risk persons or cases |
| Su 2020112 (preprint) |
Inferential | WPR | Non-island state | Beijng, Shanghai, Guangzhou and Shenzhen | Beijng, Shanghai, Guangzhou and Shenzhen | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; temporal development of epidemic |
| Tang 2020113T | Inferential | WPR | Non-island state | Beijing | Wuhan and other cities in China | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Tian 2020114 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in China | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; temporal development of epidemic |
| Tsuboi 2020115 | Descriptive | WPR | Island state | Japan | Diamond Princess | COVID-19 | Travel-related quarantine | Number or proportion of quarantined diagnosed |
| Wang 2015116 | Inferential | n.a. | Hypothetical | Hypothetical (low-risk patches) | Hypothetical (high-risk patch) | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Reproduction number |
| Wang 2020110 | Inferential | WPR | Non-island state | China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; number or proportion of deaths |
| Wang 2007117 | Descriptive | WPR | Island state | Taiwan | All SARS-affected regions | SARS | Travel-related quarantine | Detection of high-risk persons or cases diagnosed |
| Wang 2012118 | Inferential | WPR | Non-island state | Different regions in China | Different regions in China | Influenza (pandemic) | Travel restriction | Temporal development of epidemic |
| Wells 2020119 | Inferential | WPR | Non-island state | All other countries | China | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; probability of epidemic |
| Weng 2015120 | Inferential | WPR | Hypothetical | Hypothetical | Hypothetical | Influenza (H1N1 2009 pandemic) | Travel restriction | Number or proportion of cases |
| Wilder-Smith 2003121 | Descriptive | WPR | Non-island state | Singapore | All SARS-affected regions | SARS | Entry/exit screening | Detection of high-risk persons or cases |
| Wood 2007122 | Inferential | WPR | Non-island state | Melbourne and Sydney | Sydney and Darwin | Influenza | Travel restriction: air | Temporal development of epidemic |
| Yang 2020123 | Inferential | WPR | Non-island state | Other regions of China, particularly Guangdong and Zhjiang provinces | Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; temporal development of epidemic |
| Ying 2020124 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Yu 2012125 | Inferential | WPR | Non-island state | China | All other countries | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Number or proportion of cases |
| Yuan 2020126 (preprint) |
Inferential | WPR | Non-island state | Other regions of China and countries | Wuhan | COVID-19 | Multiple travel-related control measures | Temporal development of epidemic |
| Yuan 2020a127 (preprint) |
Inferential | WPR | Non-island state | China | Wuhan | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Zhang 2012128 |
Descriptive | WPR | Non-island state | Beijing | All other countries | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Number or proportion of screened identified as cases |
| Zhang 2014129 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza (pandemic) | Entry/exit screening | Number or proportion of cases; temporal development of epidemic |
| Zhang 2019130 | Inferential | n.a. | Hypothetical | Hypothetical | Hypothetical | Influenza (H1N1 2009 pandemic) | Entry/exit screening; reductions in human mobility |
Temporal development of epidemic |
| Zhang 2020131 |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases |
| Zhang 2020a132 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; reproduction number |
| Zhao 2020133 | Inferential | WPR | Non-island state | Regions of China | Regions of China | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; reproduction number; temporal development of epidemic |
| Zhou 2020134 (preprint) |
Inferential | WPR | Non-island state | Other regions of China | Wuhan and other cities in Hubei | COVID-19 | Multiple travel-related control measures | Number or proportion of cases; number or proportion of deaths |
| Zlojutro 2019135 | Inferential | AMR | Non-island state | USA | All other countries | Influenza (H1N1 2009 pandemic) | Entry/exit screening | Number or proportion of cases; cost; other |
AFR, African region; AMR, region of the Americas; EUR, European region; MERS, Middle East respiratory syndrome; SARS, severe acute respiratory syndrome; SEAR, Southeast Asia region; WPR, Western Pacific Region.
Countries and settings
Included studies assessed interventions across the globe, including, according to WHO world regions, from the Western Pacific Region (WPR) (n=71), the Southeast Asia region (n=5), the region of the Americas (n=12), the European region (EUR) (n=8), and the African region (AFR) (n=2). None of the studies included in this evidence map was conducted in a country of the Eastern Mediterranean Region (EMR). The specific countries in which interventions were implemented are listed in table 1 (under ‘regions protected by travel related measure’). Several modelling studies looked at hypothetical regions (n=16).
Of the identified interventions, some were implemented in island states (n=24) or in what we define quasi-island states (n=9), such as the UK or Hong Kong, which have limited land borders connected through, for example, a tunnel. Most interventions were implemented in non-island states (n=74). The remaining interventions assessed hypothetical regions, some of which were framed as comparable to island states, while others were more general in their framing and assumptions.
COVID-19 and other relevant respiratory infectious diseases
Included studies assessed the impact of interventions aiming to prevent or slow the transmission of COVID-19 and other infectious respiratory diseases. We identified a large number of studies focusing on COVID-19 (n=59); we also found studies focusing on SARS (n=11), MERS (n=1) and various strains of influenza (n=39). Other studies looked at multiple infectious respiratory diseases (n=5) or a hypothetical infectious disease with COVID-19 relevant properties (n=7).
Figure 2 illustrates how the number of publications concerned with each disease has developed over time and explores where interventions have been implemented. As expected, there has been a rapid burst of research related to COVID-19 travel restrictions in 2020 (panel A), currently consisting mostly of non-peer-reviewed preprints. Research on SARS, MERS and influenza travel restrictions is more spread over time and also clusters around specific outbreaks (eg, SARS 2003; H1N1 influenza 2009) (panel B).
Figure 2.
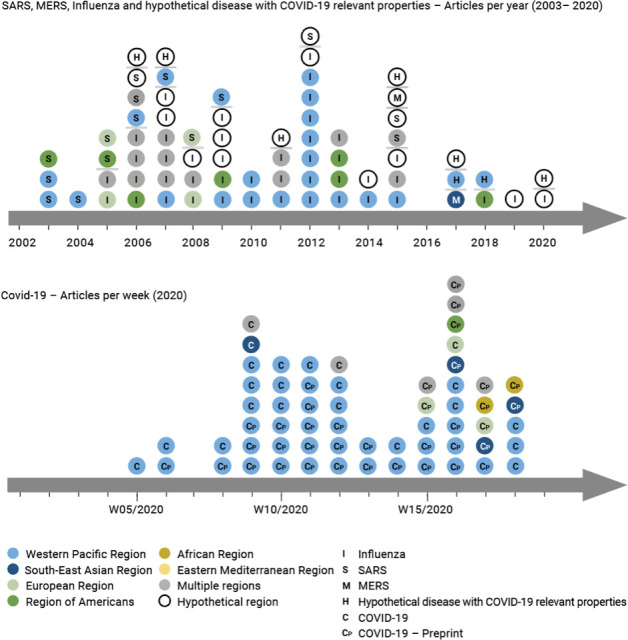
Illustration of the number of studies published over time; the top panel (2002–2020) shows studies focused on SARS, MERS, influenza and hypothetical disease with COVID-19 relevant properties, while the bottom panel (2020) shows studies focused on COVID-19. The specific disease is indicated by the single letter within the circle. Additionally, the colour represents the WHO world region. MERS, Middle East respiratory syndrome; SARS, severe acute respiratory syndrome.
Intervention categories and interventions
The 122 included studies assessed the impact of a wide range of travel-related control measures. We classified these according to broad intervention categories, including border closures (n=3), entry/exit screening (n=31), travel-related quarantine (n=6), travel bans, such as suspension of international flights (n=8), and travel restrictions (n=25).
For travel restrictions, a few studies described imposing restrictions in relation to the mode of travel (eg, restricting air, land or maritime travel); most used the term ‘travel restrictions’ without providing any specification. However, most of the studies in this category were modelling studies, which commonly simulated ‘travel restrictions’ as different percentage reductions in the travel volume (eg, 50% and 90%).
We identified a relatively large number of studies assessing the impact of a bundle of different travel-related control measures (eg, entry/exit screening and quarantining all arriving passengers) (n=49). More than half of these (n=29) assessed the impact of the lockdown of Wuhan (n=29), combining several travel-related measures. We classified all of these studies as assessing multiple travel-related control measures (see online supplemental file S6), as it was impossible to identify the specific measures assessed due to lack of reporting.
Figure 3 visualises the body of evidence according to the respective disease, intervention implemented, as well as region in which an intervention was implemented. It becomes clear that the majority of the evidence assesses multiple travel-related control measures to delay or limit the progression of COVID-19. The second largest block of evidence emerges from studies focusing on various influenza strains and the impact of travel restrictions and entry/exit screening.
Figure 3.
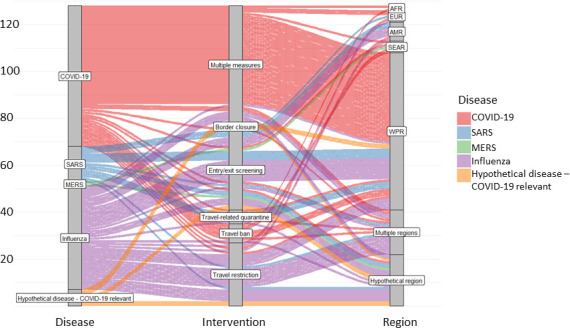
Overview of the body of evidence showing the frequency of studies investigating the specific diseases (left column), interventions (middle column) and the WHO world regions (right column). MERS, Middle East respiratory syndrome; SARS, severe acute respiratory syndrome.
A critical aspect in relation to the likely impact of travel-related control measures is the timing of implementation. Figure 4 (panel A) visualises during which phase of an epidemic or pandemic different types of interventions addressed by included studies were implemented. With respect to the timing of implementation we distinguish the following:
Figure 4.
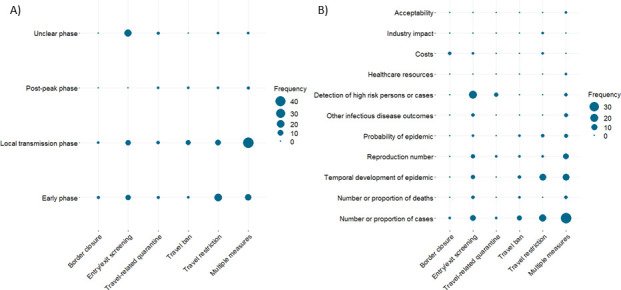
Bubble plots illustrating in included studies (A) during which phase of an epidemic or pandemic different types of interventions were implemented and (B) which intervention categories were assessed against different types of outcomes.
Early phase: interventions are implemented at a time when there are either no or only singular detected/notified cases (ie, all cases are detected and quarantined). During this phase, imported cases represent the main source of infections.
Local transmission phase: interventions are implemented during more or less widespread human-to-human transmission of the disease. During this phase, local transmission and imported cases represent sources of infections.
Postpeak phase: interventions are implemented during/after successful containment of an initial outbreak/epidemic/pandemic with the possibility of recurrence. During this phase, imported cases may again represent a major source of infections.
Unclear phase: the phase of the outbreak/epidemic/pandemic is not reported or is not directly relevant for implementation of the intervention.
Figure 4 (panel A) shows, for example, that many interventions, especially those comprising multiple measures, are implemented when local transmission of the disease has already been established. Travel restrictions are often employed in the early phase of an epidemic or pandemic while entry/exit screening measures tend to be implemented both in the early stages, as well as throughout the phases of an epidemic or pandemic. Further details on the specific travel-related control measures reported in each included study and their phase of implementation is presented in the online supplemental file S6.
Outcome categories and outcomes
We considered studies assessing five broad categories of outcomes: infectious disease outcomes, screening outcomes, other health outcomes, economic outcomes and social outcomes. Identified studies, however, largely assessed infectious disease (n=98) and/or screening outcomes (n=25). We identified no studies concerned with other health outcomes and very few studies assessing economic (n=5) or social outcomes (n=1).
Infectious disease outcomes included several types of outcomes related to disease timing and transmission, including the number or proportion of cases, the number or proportion of deaths, the reproduction number, the probability of an epidemic, demand for healthcare resources and the temporal development of the epidemic. Studies assessed various specific outcomes under these broader types, for example, ‘time to epidemic peak’ and ‘delay of epidemic’ both belong to the outcome type ‘temporal development of the epidemic’. Screening outcomes all comprised some form of measuring the number and/or proportion of high-risk persons and/or cases detected. Economic outcomes covered costs and industry impact, and social outcomes examined the acceptability of travel-related control measures. These outcome types as assessed in each study are listed in table 1. A comprehensive list of the specific outcomes reported for each category and type of outcome and how often these were used across the evidence map can be found in online supplemental file S7.
Figure 4 (panel B) illustrates which intervention categories were assessed by different outcome categories. Infectious disease outcomes such as the number or proportion of cases, the temporal development of an epidemic and the reproduction number were well represented across all intervention types. Conversely, screening outcomes were assessed primarily with respect to entry/exit screening. The lack of studies assessing economic and social outcomes is also clearly visible.
Study types
We included all studies assessing the quantitative impact of travel-related control measures on infectious disease, screening, economic and social outcomes. As a consequence of this broad scope, included studies employed a range of vastly different approaches drawing from the fields of infectious disease research, epidemiology, economics, biology and mathematics, among others. We categorised each study as being either inferential or descriptive. Most of the studies we found were inferential in nature (n=103), aiming to retrospectively calculate or prospectively forecast the impact of one or multiple travel-related control measures on outcomes. The remaining studies were descriptive in nature (n=19), aiming to describe the impact of control measures through summary statistics and/or graphics.
Within these broad categories, however, included studies varied greatly with regard to the specific approach taken. Inferential studies applied numerous modelling and epidemiological techniques; compartmental models, such as SIR models (S: susceptible, I: infectious, R: recovered) or SIR model derivatives, were common. Several studies also applied spatial models to explore how disease transmission moves geographically. Epidemiological time series models, as well as other epidemiological modelling and testing strategies, were also common. Descriptive studies comprised primarily observational studies and graphical summary studies, both of which measured and reported descriptive summary statistics related to intervention impact. The types of studies illustrated here are not exhaustive, and the methodological boundaries between the approaches employed are sometimes blurry. In fact, several studies apply multiple techniques, combining, for example, compartmental and spatial models or compartmental and time series models. online supplemental file S8 provides a more detailed overview of the study types included, along with examples from the included studies.
Discussion
Summary of findings
This evidence map provides a comprehensive overview of travel-related control measures available for the control of SARS-CoV-2/COVID-19.
Most of the included studies used infectious disease or epidemiological modelling methods to examine the impact of travel-related control measures on the current COVID-19 pandemic. We also identified studies on SARS-CoV-1/SARS and influenza, mostly undertaken in the context of previous epidemics/pandemics. We found very few studies addressing MERS-CoV/MERS. The identified studies assessing travel-related control measures in the context of SARS-CoV-2/COVID-19, were mostly preprint publications that have not yet undergone peer review and are often characterised by poor reporting and conduct.12
Studies were undertaken across the globe. The geographical region most represented was WPR, driven in part by a number of studies focusing on the Hubei region of China and in part by studies across the region during the previous SARS-CoV-1/SARS outbreak. AFR and EUR were the least represented; we did not identify any studies from EMR. Most studies operated at the level of countries and reported little about specific settings of interest (eg, a named airport and a specific country border) or the broader implementation context (eg, usual border arrangements when control measures are not in place).
Travel-related control measures can be classified as (1) border closure, (2) travel bans, (3) travel restrictions, (4) entry/exit screening, (5) travel-related quarantine and (6) multiple travel-related control measures. Studies were identified and mapped for all of these categories. We identified a relatively large body of evidence on entry/exit screening, as well as on travel restrictions. The latter also included subnational measures, for example, city-to-city travel restrictions across broader regions, making a clear distinction from general social distancing measures challenging. We also found many studies examining the impact of bundles of travel-related control measures. Interventions are often poorly described, both in relation to the measure itself (eg, border closure) and in relation to how the measure is implemented or enforced (eg, border patrols, fines and exceptions). Moreover, travel-related control measures rarely happen in a vacuum: the closer to real-life the intervention (and the study), the more cointerventions tend to be involved. This makes it very difficult to assess the unique impact of a specific measure.
The impact of travel-related control measures in controlling geographical spread and overall disease transmission likely varies between early, local transmission and postpeak phases of an outbreak/epidemic/pandemic, yet reporting of the timing of implementation tends to be poor. Most studies focused on the early and local transmission phases; few studies were concerned with the postpeak phase.
The identified studies almost exclusively examined infectious disease and screening outcomes. Surprisingly, we did not identify any study reporting on other health outcomes, such as implications for the physical and psychosocial health of stranded travellers, of those unable to visit family members, of regular commuters unable to reach their workplace, of individuals quarantined, of people unable to obtain medical treatment and other collateral damage (eg, suspended immunisation programmes and impacts on food supply due to limited air, maritime and land travel of either people or goods). Only three included studies were concerned with economic and social outcomes.
The bulk of the evidence derives from modelling studies. In an acute outbreak situation, the time and resources that can be dedicated to conducting timely, empirical research are limited. Modelling studies vary greatly in type (eg, SIR-like models vs time series models) and in the underlying assumptions regarding the disease, interventions or regions/settings. Additionally, many studies do not fall into clean categories, and a single study may combine compartmental infectious disease models with epidemiological spatial models. They also vary with respect to whether and how they have been validated through real-life applications.
Gaps in the current evidence base
The evidence map identified several gaps in the evidence base related to travel-related control measures that could inform future research as well as evidence synthesis. First, some regions were under-represented, specifically studies conducted or simulated for the countries in the AFR, EMR and EUR were lacking. Second, the most commonly reported travel-related control measures were entry/exit screening and restrictions, which in the context of modelling studies were simulated as different levels of travel reductions. Thus, the evidence base regarding more stringent measures, such as travel bans and complete border closures, remains sparse. Third, our evidence map identified lack of consideration of the impact of these measures on broader health outcomes, such as physical and mental health, as well as social and economic outcomes, such as cost and burden on communities and socioeconomic inequalities. Finally, the key gap relates to the lack of empirical studies assessing the impact of travel-related control measures, including experimental and quasiexperimental approaches.
Methodological limitations of this study
This evidence map was put together over 10 days, and the process is thus characterised by several limitations.
While we conducted searches in three major databases and two COVID-specific databases, these were mostly health centric. We only searched Web of Science—comprising Science Citation Index Expanded (1900–present), Social Sciences Citation Index (1900–present) and Emerging Sources Citation Index (2015–present)—to identify social and economic studies. As we identified very few economic and social outcomes, it is likely that there is another body of evidence to be located with more focused searches in specific economic and social science databases. In addition, we did not search for grey literature sources. Furthermore, since COVID-19 initially started in Wuhan, China, many studies are published on the topic in Chinese journals and databases. Because of the language barrier, we did not consider these sources.
The unspecific and inconsistent reporting of primary studies with regard to interventions, especially when a package of control measures was investigated, sometimes made inclusion/exclusion decisions difficult. While we developed and calibrated screening guidance to ensure consistency among reviewers, it is nevertheless possible that we excluded some travel-related control measures that were not explicitly described as such. Also, we did not undertake double-screening of all studies but only reassessed a subset of studies excluded at the full-text screening stage. In general, however, we applied a very conservative approach to title/abstract, as well as full-text screening, where any uncertainties associated with a study were marked for further checking by a second reviewer and/or for discussion among the whole review team.
We developed and calibrated data extraction guidance to be used consistently by reviewers. Nevertheless, we had to refine some categories post hoc. We also had a large number of reviewers extracting data, which created heterogeneity in the dataset. To address this, a second reviewer double-checked all extracted information for each of the main domains, that is, all information regarding interventions, outcomes and study design. Overall, high-quality data extraction was limited by poor reporting of the travel-related control measures and the specific contexts in which they are implemented in primary studies.13
Finally, we did not include travel warning or travel advice in the evidence map, which limits the scope of this map. While these may be classified as travel-related control measures,13 their inclusion would have likely broadened our search strategy and prolonged the timeline of its development. In general, lack of intervention specification in the included studies makes it challenging to draw clear categories of interventions without potential overlap (eg, drawing clear distinction between a travel ban vs a travel restriction and when these are used only as descriptors in the studies without further specification).
Implications for moving forward
An evidence map is not designed to assess the effectiveness of interventions, in this case the effectiveness of travel-related control measures in controlling infectious disease spread. The present evidence map sheds light on the variety of evidence available with regards to the quantifiable impacts of travel-related control measures, the outcomes used, as well as the study types employed. It thus represents a stepping stone towards a systematic review on the effectiveness of all or a subset of travel-related control measures.
Given our health-centric searches, we feel confident that we have identified most of the available body of evidence regarding the quantifiable impacts of travel-related control measures on health. In terms of conducting a systematic review of effectiveness, it would, however, be advisable to undertake additional forward-backward citation searches and/or similar studies searches with included studies. We identified a number of challenges related to the full analysis of this evidence base. These include: (1) classifying interventions in an appropriate and consistent manner; (2) capturing the details of interventions (eg, components, timing and implementation characteristics) and cointerventions through an analysis of linked sources of evidence; (3) assessing the quality and usefulness of different types of studies ranging from simple observational studies to complex modelling studies; (4) quantitatively synthesising this extremely heterogeneous evidence base; and (5) dealing with the large number of preprint studies and their varying quality. Moving forward with a full analysis, we suggest reviewers plan ahead and develop strategies on how these challenges can be adequately managed. For example, this might entail consideration of external sources of evidence beyond scientific databases, such as governmental websites on the implementation of different travel-related control measures (eg, their timing and duration) and other measures in local contexts. To contain the COVID-19 pandemic, governments have employed a range of public health measures often in a bundle, which challenges assessment of the effectiveness of any single measure, such as a travel ban. It would therefore be important to explicitly document and, where possible, assess various combinations of measures implemented—including those related to travel–in future research.
Importantly, decisions to maintain or stop travel-related control measures are determined by a range of factors beyond effectiveness, including legal and human rights aspects, as well as considerations of broader health, economic and social implications, as well as sociocultural and political acceptability. Gathering evidence about these broader factors in a systematic manner was beyond the scope of the current evidence map; however, such aspects might be important to inform decision making. Future evidence synthesis would therefore require a different scope and a broader search strategy, notably encompassing searches in economics and social science databases, as well as multidisciplinary databases (eg, EconLit, PsycINFO and Scopus).
Supplementary Material
Acknowledgments
We are grateful to Susan L Norris and Carmen Dolea for their guidance in scoping this evidence map.
Footnotes
Twitter: @strahwald
Contributors: JB, AM, ER and OH defined the study scope and developed the study protocol with significant intellectual input from all review authors. JB and AM coordinated the entire study process. IK designed the search strategy and conducted all the searches. JB, AM, RB, MC, KG, LMP, PvP, KS, BS, JMS, SV and ER conducted data screening and extraction. JB, AM, JMS, LMP and PvP did data mapping. JB, AM and ER prepared the first draft of the manuscript, which was further critically examined by all the authors and revised based on their feedback. All review authors reviewed and approved the final draft.
Funding: The conduct of this evidence map was funded by the World Health Organization (WHO; grand/award number: N/A).
Disclaimer: This study was commissioned and paid for by the World Health Organization (WHO). Copyright of the original work, a report submitted to WHO, belongs to WHO. This article was developed based on the WHO report and the authors have been given permission to publish. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the views, decisions or policies of WHO.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. No original data were generated for this study. All studies included in the evidence map are presented in the supplementary file.
References
- 1.WHO . Novel Coronavirus (2019-nCoV) situation report - 1. Geneva: World Health Organization, 2020. [Google Scholar]
- 2.WHO . Novel coronavirus (2019-nCoV) situation report - 51. Geneva: World Health Organization, 2020. [Google Scholar]
- 3.WHO . Weekly update on COVID-19, April 8–15, 2020. health emergencies programme. Geneva: World Health Organization, 2020. [Google Scholar]
- 4.Mateus ALP, Otete HE, Beck CR, et al. Effectiveness of travel restrictions in the rapid containment of human influenza: a systematic review. Bull World Health Organ 2014;92:868–80. 10.2471/BLT.14.135590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ryu S, Gao H, Wong JY, et al. Nonpharmaceutical measures for pandemic influenza in Nonhealthcare Settings-International Travel-Related measures. Emerg Infect Dis 2020;26:961–6. 10.3201/eid2605.190993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO . Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza. Licence: CC BY-NC-SA 3.0 IGO.: Licence: CC BY-NC-SA 3.0 IGO, 2019. Available: https://creativecommons.org/
- 7.Mouchtouri VA, Christoforidou EP, An der Heiden M, et al. Exit and entry screening practices for infectious diseases among travelers at points of entry: looking for evidence on public health impact. Int J Environ Res Public Health 2019;16:4638. 10.3390/ijerph16234638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasquini-Descomps H, Brender N, Maradan D. Value for money in H1N1 influenza: a systematic review of the cost-effectiveness of pandemic interventions. Value Health 2017;20:819–27. 10.1016/j.jval.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 9.Pérez Velasco R, Praditsitthikorn N, Wichmann K, et al. Systematic review of economic evaluations of preparedness strategies and interventions against influenza pandemics. PLoS One 2012;7:e30333. 10.1371/journal.pone.0030333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Errett NA, Sauer LM, Rutkow L. An integrative review of the limited evidence on international travel bans as an emerging infectious disease disaster control measure. J Emerg Manag 2020;18:7–14. 10.5055/jem.2020.0446 [DOI] [PubMed] [Google Scholar]
- 11.Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glasziou PP, Sanders S, Hoffmann T. Waste in covid-19 research. BMJ 2020;369:m1847. 10.1136/bmj.m1847 [DOI] [PubMed] [Google Scholar]
- 13.Lee K, Worsnop CZ, Grépin KA, et al. Global coordination on Cross-border travel and trade measures crucial to COVID-19 response. Lancet 2020;395:1593–5. 10.1016/S0140-6736(20)31032-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adekunle AI, Adekunle AI, Meehan M, et al. Delaying the COVID-19 epidemic in Australia: evaluating the effectiveness of international travel bans.. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aleta A, Aleta A, Hu Q, et al. A data-driven assessment of early travel restrictions related to the spreading of the novel COVID-19 within mainland China.. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anonymous . Thermal image scanners to detect fever in airline passengers, Vancouver and Toronto, 2003. Can Commun Dis Rep 2004;30:165–7. [PubMed] [Google Scholar]
- 17.Anzai A, Kobayashi T, Linton NM, et al. Assessing the impact of reduced travel on exportation dynamics of novel coronavirus infection (COVID-19). J Clin Med 2020;9:601. 10.3390/jcm9020601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arima Y, Kutsuna S, Shimada T. Severe acute respiratory syndrome coronavirus 2 infection among Returnees to Japan from Wuhan, China, 2020. Emerg Infect Dis 2020;26:1596–600. 10.3201/eid2607.200994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arino J, Jordan R, van den Driessche P. Quarantine in a multi-species epidemic model with spatial dynamics. Math Biosci 2007;206:46–60. 10.1016/j.mbs.2005.09.002 [DOI] [PubMed] [Google Scholar]
- 20.Bajardi P, Poletto C, Ramasco JJ, et al. Human mobility networks, travel restrictions, and the global spread of 2009 H1N1 pandemic. PLoS One 2011;6:e16591. 10.1371/journal.pone.0016591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Banholzer N, van Weenen E, Kratzwald B, et al. Estimating the impact of non-pharmaceutical interventions on documented infections with COVID-19: a cross-country analysis.. medRxiv. 2020. [Google Scholar]
- 22.Bolton KJ, McCaw JM, Moss R, et al. Likely effectiveness of pharmaceutical and non-pharmaceutical interventions for mitigating influenza virus transmission in Mongolia. Bull World Health Organ 2012;90:264–71. 10.2471/BLT.11.093419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boyd M, Baker MG, Mansoor OD, et al. Protecting an island nation from extreme pandemic threats: proof-of-concept around border closure as an intervention. PLoS One 2017;12:e0178732. 10.1371/journal.pone.0178732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boyd M, Mansoor OD, Baker MG, et al. Economic evaluation of border closure for a generic severe pandemic threat using new Zealand Treasury methods. Aust N Z J Public Health 2018;42:444–6. 10.1111/1753-6405.12818 [DOI] [PubMed] [Google Scholar]
- 25.Caley P, Becker NG, Philp DJ. The waiting time for inter-country spread of pandemic influenza. PLoS One 2007;2:e143. 10.1371/journal.pone.0000143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang M-C, Kahn R, Li Y-A LC-S, et al. Modeling the impact of human mobility and travel restrictions on the potential spread of SARS-CoV-2 in Taiwan.. medRxiv. 2020. [Google Scholar]
- 27.Cheng H-Y, Li S-Y, Yang C-H. Initial rapid and proactive response for the COVID-19 outbreak - Taiwan's experience. J Formos Med Assoc 2020;119:771–3. 10.1016/j.jfma.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chinazzi M, Davis JT, Ajelli M, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020;368:395–400. 10.1126/science.aba9757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chiyomaru K, Takemoto K. Global COVID-19 transmission rate is influenced by precipitation seasonality and the speed of climate temperature warming.. medRxiv. 2020. [Google Scholar]
- 30.Chong KC, Ying Zee BC. Modeling the impact of air, sea, and land travel restrictions supplemented by other interventions on the emergence of a new influenza pandemic virus. BMC Infect Dis 2012;12. 10.1186/1471-2334-12-309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung LH. Impact of pandemic control over Airport economics: reconciling public health with Airport business through a streamlined approach in pandemic control. J Air Transp Manag 2015;44:42–53. 10.1016/j.jairtraman.2015.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ciofi degli Atti ML, Merler S, Rizzo C, et al. Mitigation measures for pandemic influenza in Italy: an individual based model considering different scenarios. PLoS One 2008;3:e1790. 10.1371/journal.pone.0001790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klepac P, voort SJ, Quilty SJ. Interventions targeting air travellers early in the pandemic may delay local outbreaks of SARS-CoV-2. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Colizza V, Barrat A, Barthelemy M, et al. Modeling the worldwide spread of pandemic influenza: baseline case and containment interventions. PLoS Med 2007;4:e13–110. 10.1371/journal.pmed.0040013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cooper BS, Pitman RJ, Edmunds WJ, et al. Delaying the International spread of pandemic influenza. PLoS Med 2006;3:e212–55. 10.1371/journal.pmed.0030212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Costantino V, Heslop DJ, MacIntyre C, et al. The effectiveness of full and partial travel bans against COVID-19 spread in Australia for travellers from China. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. The Lancet Public Health 2020;5:279–88. 10.1016/S2468-2667(20)30090-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dandekar R, Barbastathis G. Quantifying the effect of quarantine control in Covid-19 infectious spread using machine learning. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Vlas SJ, Feng D, Cooper BS, et al. The impact of public health control measures during the SARS epidemic in mainland China. Trop Med Int Health 2009;14 Suppl 1:101–4. 10.1111/j.1365-3156.2009.02348.x [DOI] [PubMed] [Google Scholar]
- 40.Ediriweera DS, de Silva NR, Malavige GN, et al. An epidemiological model to aid decision-making for COVID-19 control in Sri Lanka. PLoS One 2020;15:e0238340. 10.1371/journal.pone.0238340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eichner M, Schwehm M, Wilson N, et al. Small islands and pandemic influenza: potential benefits and limitations of travel volume reduction as a border control measure. BMC Infect Dis 2009;9:160. 10.1186/1471-2334-9-160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Epstein JM, Goedecke DM, Yu F, et al. Controlling pandemic flu: the value of international air travel restrictions. PLoS One 2007;2:e401. 10.1371/journal.pone.0000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fang H, Wang L, Yang Y. Human mobility restrictions and the spread of the novel coronavirus (2019-nCoV) in China. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferguson NM, Cummings DAT, Fraser C, et al. Strategies for mitigating an influenza pandemic. Nature 2006;442:448–52. 10.1038/nature04795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Flahault A, Vergu E, Coudeville L, et al. Strategies for containing a global influenza pandemic. Vaccine 2006;24:6751–5. 10.1016/j.vaccine.2006.05.079 [DOI] [PubMed] [Google Scholar]
- 46.Fujita M, Sato H, Kaku K, et al. Airport quarantine inspection, follow-up observation, and the prevention of pandemic influenza. Aviat Space Environ Med 2011;82:782–9. 10.3357/ASEM.3023.2011 [DOI] [PubMed] [Google Scholar]
- 47.Germann TC, Kadau K, Longini IM, et al. Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci U S A 2006;103:5935–40. 10.1073/pnas.0601266103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Glass K, Becker NG. Evaluation of measures to reduce international spread of SARS. Epidemiol Infect 2006;134:1092–101. 10.1017/S0950268806005863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gostic K, Gomez AC, Mummah RO, et al. Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. Elife 2020;9. 10.7554/eLife.55570. [Epub ahead of print: 24 02 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gostic KM, Kucharski AJ, Lloyd-Smith JO. Effectiveness of traveller screening for emerging pathogens is shaped by epidemiology and natural history of infection. eLife. 2015 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goubar A, Bitar D, Cao WC, et al. An approach to estimate the number of SARS cases imported by international air travel. Epidemiol Infect 2009;137:1019–31. 10.1017/S0950268808001635 [DOI] [PubMed] [Google Scholar]
- 52.Gunaratnam PJ, Tobin S, Seale H, et al. Airport arrivals screening during pandemic (H1N1) 2009 influenza in New South Wales, Australia. Med J Aust 2014;200:290–2. 10.5694/mja13.10832 [DOI] [PubMed] [Google Scholar]
- 53.Hale MJ, Hoskins RS, Baker MG. Screening for influenza A(H1N1)pdm09, Auckland International Airport, New Zealand. Emerg Infect Dis 2012;18:866–8. 10.3201/eid1805.111080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hamidouche M. COVID-19 epidemic in Algeria: assessment of the implemented preventive strategy. medRxiv 2020. [Google Scholar]
- 55.He J, Chen G, Jiang Y, et al. Comparative Analysis of COVID-19 Transmission Patterns in Three Chinese Regions vs. South Korea, Italy and Iran. medRxiv 2020. [Google Scholar]
- 56.Hien TT, Boni MF, Bryant JE, et al. Early pandemic influenza (2009 H1N1) in Ho Chi Minh City, Vietnam: a clinical virological and epidemiological analysis.. PLoS Medicine / Public Library of Science 2009;7:e1000277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hollingsworth TD, Ferguson NM, Anderson RM. Will travel restrictions control the International spread of pandemic influenza? Nat Med 2006;12:497–9. 10.1038/nm0506-497 [DOI] [PubMed] [Google Scholar]
- 58.Hossain MP, Junus A, et al. , et al . The effects of border control and quarantine measures on global spread of COVID-19. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hou J, Hong J, et al. Changing transmission dynamics of COVID-19 in China: a nationwide population-based piecewise mathematical modeling study. medRxiv 2020. [Google Scholar]
- 60.Hsieh Y-H, van den Driessche P, Wang L. Impact of travel between patches for spatial spread of disease. Bull Math Biol 2007;69:1355–75. 10.1007/s11538-006-9169-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hsieh Y-H, King C-C, Chen CWS, et al. Impact of quarantine on the 2003 SARS outbreak: a retrospective modeling study. J Theor Biol 2007;244:729–36. 10.1016/j.jtbi.2006.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jia JS, Lu X, Yuan Y, et al. Population flow drives spatio-temporal distribution of COVID-19 in China. Nature 2020;582:389–94. 10.1038/s41586-020-2284-y [DOI] [PubMed] [Google Scholar]
- 63.Jiang X, Chang L, Shi Y. How does the outbreak of 2019-nCoV spread in mainland China? A retrospective analysis of the dynamic transmission routes. medRxiv 2020;92. 10.2139/ssrn.3546741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kernéis S, Grais RF, Boëlle P-Y, et al. Does the effectiveness of control measures depend on the influenza pandemic profile? PLoS One 2008;3:e1478. 10.1371/journal.pone.0001478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khan K, Eckhardt R, Brownstein JS, et al. Entry and exit screening of airline travellers during the A(H1N1) 2009 pandemic: a retrospective evaluation. Bull World Health Organ 2013;91:368–76. 10.2471/BLT.12.114777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kim S, Chang DE, . Border screening vs. community level disease control for infectious diseases: Timing and effectivenes. American Institute of Physics Inc, 2017. [Google Scholar]
- 67.Kong XS, Liu F, Wang HB, et al. Epidemic prevention and control measures in China significantly curbed the epidemic of COVID-19 and influenza. medRxiv 2020. [Google Scholar]
- 68.Kraemer MUG, Yang C-H, Gutierrez B, et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020;368:493–7. 10.1126/science.abb4218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kuo JS, Lee YH, Heish JW, et al. Initial evaluation on screening of novel influenza A (H1N1) at international ports in Taiwan. Taiwan Epidemiol Bull 2009;25:254–67. [Google Scholar]
- 70.Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions for containing the COVID-19 outbreak in China. medRxiv 2020. [Google Scholar]
- 71.Lam EHY, Cowling BJ, Cook AR, et al. The feasibility of age-specific travel restrictions during influenza pandemics. Theor Biol Med Model 2011;8:44. 10.1186/1742-4682-8-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lau H, Khosrawipour V, Kocbach P, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med 2020;27. 10.1093/jtm/taaa037. [Epub ahead of print: 18 05 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lee JM, Choi D, Cho G, et al. The effect of public health interventions on the spread of influenza among cities. J Theor Biol 2012;293:131–42. 10.1016/j.jtbi.2011.10.008 [DOI] [PubMed] [Google Scholar]
- 74.Li D, Liu Z, Liu Q, et al. Estimating the efficacy of traffic blockage and quarantine for the epidemic caused by 2019-nCoV (COVID-19). medRxiv 2020. [Google Scholar]
- 75.Lin H, Liu W, Gao H, et al. Trends in transmissibility of 2019 novel coronavirus-infected pneumonia in Wuhan and 29 provinces in China. medRxiv 2020. 10.2139/ssrn.3544821 [DOI] [Google Scholar]
- 76.Linka K, Peirlinck M, Sahli Costabal F, et al. Outbreak dynamics of COVID-19 in Europe and the effect of travel restrictions. Comput Methods Biomech Biomed Engin 2020;23:710–7. 10.1080/10255842.2020.1759560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu X, Takeuchi Y. Spread of disease with transport-related infection and entry screening. J Theor Biol 2006;242:517–28. 10.1016/j.jtbi.2006.03.018 [DOI] [PubMed] [Google Scholar]
- 78.Liu K, Ai S, Song S, et al. Population movement, City closure in Wuhan and geographical expansion of the 2019-nCoV pneumonia infection in China in January. Clinical infectious diseases 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liu H, Bai X, Shen H, et al. Synchronized travel restrictions across cities can be effective in COVID-19 control. medRxiv 2020. a. [Google Scholar]
- 80.Malmberg H, Britton T. Inflow restrictions can prevent epidemics when contact tracing efforts are effective but have limited capacity. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Malone JD, Brigantic R, Muller GA, et al. U.S. Airport entry screening in response to pandemic influenza: modeling and analysis. Travel Med Infect Dis 2009;7:181–91. 10.1016/j.tmaid.2009.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mandal S, Bhatnagar T, Arinaminpathy N, et al. Prudent public health intervention strategies to control the coronavirus disease 2019 transmission in India: a mathematical model-based approach. Indian J Med Res 2020;151:23. 10.4103/ijmr.IJMR_504_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Marcelino J, Kaiser M. Critical paths in a metapopulation model of H1N1: efficiently delaying influenza spreading through flight cancellation. PLoS Curr 2012;4:e4f8c9a2e1fca8. 10.1371/4f8c9a2e1fca8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mbuvha R, Marwala T. Bayesian inference of COVID-19 spreading rates in South Africa. PLoS One 2020;15:e0237126. 10.1371/journal.pone.0237126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mondal S, Ghosh S. Searching the Sigmoid-type trend in lock down period covid19 data of India and its different states. medRxiv 2020. [Google Scholar]
- 86.Moriarty LF, Plucinski MM, Marston BJ, et al. Public Health Responses to COVID-19 Outbreaks on Cruise Ships - Worldwide, February-March 2020. MMWR Morb Mortal Wkly Rep 2020;69:347–52. 10.15585/mmwr.mm6912e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mummert A, Weiss H, Long L-P, et al. A perspective on multiple waves of influenza pandemics. PLoS One 2013;8:e60343. 10.1371/journal.pone.0060343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Muraduzzaman AKM, Khan MH, Parveen R, et al. Event based surveillance of middle East respiratory syndrome coronavirus (MERS- CoV) in Bangladesh among pilgrims and travelers from the middle East: an update for the period 2013–2016. PLoS One 2018;13:e0189914. 10.1371/journal.pone.0189914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nakata Y, Röst G. Global analysis for spread of infectious diseases via transportation networks. J Math Biol 2015;70:1411–56. 10.1007/s00285-014-0801-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nigmatulina KR, Larson RC. Living with influenza: impacts of government imposed and voluntarily selected interventions. Eur J Oper Res 2009;195:613–27. 10.1016/j.ejor.2008.02.016 [DOI] [Google Scholar]
- 91.Nishiura H, Wilson N, Baker MG. Quarantine for pandemic influenza control at the borders of small island nations. BMC Infect Dis 2009;9. 10.1186/1471-2334-9-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Odendaal WG. A method to model outbreaks of new infectious diseases with pandemic potential such as COVID-19. medRxiv 2020. [Google Scholar]
- 93.Pan J, Yao Y, Liu Z, et al. Effectiveness of control strategies for coronavirus disease 2019: a SEIR dynamic modeling study. medRxiv 2020. 10.1101/2020.02.19.20025387 [DOI] [Google Scholar]
- 94.Pan X, Ojcius DM, Gao T, et al. Lessons learned from the 2019-nCoV epidemic on prevention of future infectious diseases. Microbes Infect 2020. a;22:86–91. 10.1016/j.micinf.2020.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pang X, Zhu Z. Evaluation of control measures implemented in the severe acute respiratory syndrome outbreak in Beijing, 2003. JAMA 2003;290:3215–21. 10.1001/jama.290.24.3215 [DOI] [PubMed] [Google Scholar]
- 96.Pinkas J, Jankowski M, Szumowski Łukasz, et al. Public health interventions to mitigate early spread of SARS-CoV-2 in Poland. Med Sci Monit 2020;26:e924730. 10.12659/MSM.924730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pitman RJ, Cooper BS, Trotter CL, et al. Entry screening for severe acute respiratory syndrome (SARS) or influenza: policy evaluation. BMJ 2005;331:1242.2–3. 10.1136/bmj.38573.696100.3A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Priest PC, Jennings LC, Duncan AR, et al. Effectiveness of border screening for detecting influenza in arriving airline travelers. Am J Public Health 2013;103:1412–8. 10.2105/AJPH.2012.300761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pullano G, Pinotti F, Valdano E, et al. Novel coronavirus (2019-nCoV) early-stage importation risk to Europe, January 2020. Eurosurveillance 2020;25. 10.2807/1560-7917.ES.2020.25.4.2000057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Qiu Y, Chen X, Shi W. Impacts of social and economic factors on the transmission of coronavirus disease (COVID-19) in China. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Quilty BJ, Diamond C, Liu Y, et al. The effect of inter-city travel restrictions on geographical spread of COVID-19: evidence from Wuhan, China. medRxiv 2020. [Google Scholar]
- 102.Ray D, Salvatore M, Bhattacharyya R, et al. Predictions, role of interventions and effects of a historic national lockdown in India's response to the COVID-19 pandemic: data science call to arms. Harv Data Sci Rev 2020;2020. 10.1162/99608f92.60e08ed5. [Epub ahead of print: 09 06 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sakaguchi H, Tsunoda M, Wada K, et al. Assessment of border control measures and community containment measures used in Japan during the early stages of pandemic (H1N1) 2009. PLoS One 2012;7:e31289. 10.1371/journal.pone.0031289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Samaan G, Patel M, Spencer J, et al. Border screening for SARS in Australia: what has been learnt? Med J Aust 2004;180:220–3. 10.5694/j.1326-5377.2004.tb05889.x [DOI] [PubMed] [Google Scholar]
- 105.Sang Z, Qiu Z, Yan X, et al. Assessing the effect of non-pharmaceutical interventions on containing an emerging disease. Math Biosci Eng 2012;9:147–64. 10.3934/mbe.2012.9.147 [DOI] [PubMed] [Google Scholar]
- 106.Scala A, Flori A, Spelta A, et al. Between geography and demography: key interdependencies and exit mechanisms for Covid-19. medRxiv 2020. [Google Scholar]
- 107.Scalia Tomba G, Wallinga J. A simple explanation for the low impact of border control as a countermeasure to the spread of an infectious disease. Math Biosci 2008;214:70–2. 10.1016/j.mbs.2008.02.009 [DOI] [PubMed] [Google Scholar]
- 108.Shi Z, Fang Y. Temporal relationship between outbound traffic from Wuhan and the 2019 coronavirus disease (COVID-19) incidence in China. medRxiv 2020. 10.1101/2020.03.15.20034199 [DOI] [Google Scholar]
- 109.Song PX, Wang L, Zhou Y, et al. An epidemiological forecast model and software assessing interventions on COVID-19 epidemic in China. medRxiv 2020. [Google Scholar]
- 110.Wang F, Li Y, Tang D, et al. Trend of the coronavirus Disease-2019 epidemic in China after the Lockdown of Wuhan City on January 23. SSRN 2020. [Google Scholar]
- 111.St John RK, King A, de Jong D, et al. Border screening for SARS. Emerg Infect Dis 2005;11:6–10. 10.3201/eid1101.040835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Su L, Hong N, Zhou X, et al. Evaluation of the secondary transmission pattern and epidemic prediction of COVID-19 in the four metropolitan areas of China. Front Med 2020;7:171. 10.3389/fmed.2020.00171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tang B, et al. , et al, et al . Estimation of the transmission risk of the 2019-nCoV and its implication for public health interventions. Journal of Clinical Medicine 2020;9:07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Tian H, Liu Y, Li Y, et al. The impact of transmission control measures during the first 50 days of the COVID-19 epidemic in China. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tsuboi M, Hachiya M, Noda S, et al. Epidemiology and quarantine measures during COVID-19 outbreak on the cruise SHIP diamond Princess docked at Yokohama, Japan in 2020: a descriptive analysis. Glob Health Med 2020;2:102–6. 10.35772/ghm.2020.01037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang X, Liu S, Wang L, et al. An epidemic patchy model with Entry-Exit screening. Bull Math Biol 2015;77:1237–55. 10.1007/s11538-015-0084-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang T-H, Wei K-C, Hsiung CA, et al. Optimizing severe acute respiratory syndrome response strategies: lessons learned from quarantine. Am J Public Health 2007;97 Suppl 1:S98–100. 10.2105/AJPH.2005.082115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang L, Zhang Y, Huang T, et al. Estimating the value of containment strategies in delaying the arrival time of an influenza pandemic: a case study of travel restriction and patient isolation. Phys Rev E Stat Nonlin Soft Matter Phys 2012;86:032901. 10.1103/PhysRevE.86.032901 [DOI] [PubMed] [Google Scholar]
- 119.Wells CR, Sah P, Moghadas SM, et al. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci U S A 2020;117:7504–9. 10.1073/pnas.2002616117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Weng W, Ni S. Evaluation of containment and mitigation strategies for an influenza A pandemic in China. Simulation 2015;91:407–16. 10.1177/0037549715581637 [DOI] [Google Scholar]
- 121.Wilder-Smith A, Paton NI, Goh KT. Experience of severe acute respiratory syndrome in Singapore: importation of cases, and defense strategies at the Airport. J Travel Med 2003;10:259–62. 10.2310/7060.2003.2676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wood JG, Zamani N, MacIntyre CR, Raina MacIntyre C, et al. Effects of internal border control on spread of pandemic influenza. Emerg Infect Dis 2007;13:1038–45. 10.3201/eid1307.060740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yang Z, Zeng Z, Wang K, et al. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J Thorac Dis 2020;12:165–74. 10.21037/jtd.2020.02.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ying S, Li F, et al. , et al . Spread and control of COVID-19 in China and their associations with population movement, public health emergency measures, and medical resources. medRxiv 2020. [Google Scholar]
- 125.Yu H, Cauchemez S, Donnelly CA, et al. Transmission dynamics, border entry screening, and school holidays during the 2009 influenza A (H1N1) pandemic, China. Emerg Infect Dis 2012;18:758–66. 10.3201/eid1805.110356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yuan H-Y, Hossain MP, et al. , et al . Estimating the risk on outbreak spreading of 2019-nCoV in China using transportation data. medRxiv 2020. [Google Scholar]
- 127.Yuan Z, Xiao Y, Dai Z, et al. A simple model to assess Wuhan lock-down effect and region efforts during COVID-19 epidemic in China mainland. medRxiv 2020. a. [Google Scholar]
- 128.Zhang Y, Yang P, Liyanage S, et al. The characteristics of imported cases and the effectiveness of outbreak control strategies of pandemic influenza A (H1N1) in China. Asia Pac J Public Health 2012;24:932–9. 10.1177/1010539511408285 [DOI] [PubMed] [Google Scholar]
- 129.Zhang W-D, Zu Z-H, Xu Q, et al. Optimized strategy for the control and prevention of newly emerging influenza revealed by the spread dynamics model. PLoS One 2014;9:11. 10.1371/journal.pone.0084694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhang N, Zhao P, Li Y. Increased infection severity in downstream cities in infectious disease transmission and tourists surveillance analysis. J Theor Biol 2019;470:20–9. 10.1016/j.jtbi.2019.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zhang C, Chen C, Shen W, et al. Impact of population movement on the spread of 2019-nCoV in China. Emerg Microbes Infect 2020;9:988-990. 10.1080/22221751.2020.1760143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhang B, Zhou H, Zhou F. Study on SARS-COV-2 transmission and the effects of control measures in China. medRxiv 2020. a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhao S, Chen H. Modeling the epidemic dynamics and control of COVID-19 outbreak in China. Quant Biol 2020:11–19. 10.1007/s40484-020-0199-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhou X, Wu Z, Yu R, et al. Modeling-Based evaluation of the effect of quarantine control by the Chinese government in the coronavirus disease 2019 outbreak. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zlojutro A, Rey D, Gardner L. A decision-support framework to optimize border control for global outbreak mitigation. Sci Rep 2019;9:2216. 10.1038/s41598-019-38665-w [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-041619supp001.pdf (1.6MB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. No original data were generated for this study. All studies included in the evidence map are presented in the supplementary file.