Abstract
Objectives
Mental health problems significantly increased worldwide during the coronavirus (COVID-19) pandemic. At the early stage of the outbreak, the government of Bangladesh imposed lockdown and quarantine approaches to prevent the spread of the virus, which impacted people’s daily life and health. The COVID-19 pandemic has also affected people’s economic status, healthcare facilities and other lifestyle factors in Bangladesh. We aimed to assess the impact of the COVID-19 pandemic on mental health among the Bangladeshi population.
Methods
We conducted an online cross-sectional survey among 672 Bangladeshi people aged between 15 and 65 years all over the country from 15 April to 10 May 2020. After obtaining electronic consent, we conducted a survey assessing people’s sociodemographic profiles and psychometric measures. We used The University of California, Los Angeles (UCLA) Loneliness Scale-8, Patient Health Questionnaire-9, Generalized Anxiety Disorder 7-Item Scale and Pittsburgh Sleep Quality Index to assess loneliness, depression, anxiety and sleep disturbance, respectively.
Results
The prevalence of loneliness, depression, anxiety and sleep disturbance was estimated at 71% (mild: 32%, moderate: 29%, severe: 10%), 38% (mild: 24%, moderate: 11%, severe: 3%), 64% (mild: 30%, moderate: 17%, severe: 17%) and 73% (mild: 50%, moderate: 18%, severe: 5%), respectively. In Bangladesh, the key factors associated with poor mental health during COVID-19 were female sex, unemployment, being a student, obesity and living without a family. The present study also identified statistically significant interrelationships among the measured mental health issues.
Conclusions
A large portion of respondents reported mental health problems during the COVID-19 pandemic in Bangladesh. The present study suggests longitudinal assessments of mental health among Bangladeshi people to determine the gravity of this issue during and after the pandemic. Appropriate supportive programmes and interventional approaches would address mental health problems in Bangladesh during the COVID-19 pandemic.
Keywords: COVID-19, depression & mood disorders, anxiety disorders, adult psychiatry, public health
Strengths and limitations of this study.
The study assessed the four major mental health issues among the general Bangladeshi population during the COVID-19 pandemic.
The study ensured rapid data collection during public health emergencies and suitability to developing context-specific mental health programmes.
Online self-reporting surveys might have multiple biases and are not representative of those without internet facilities.
This cross-sectional study was not able to measure the impact of these mental illnesses over time.
Introduction
The novel coronavirus strain SARS-CoV-2 which causes COVID-19 originated from Wuhan, China. COVID-19 was declared a pandemic on 11 March 2020 due to the uncontrolled spread worldwide.1 As of 29 December 2020, over 79.2 million COVID-19 cases and over 1.7 million deaths have been reported worldwide since the start of the pandemic.2 In December 2020, we observed the highest weekly average of 4.3 million confirmed new cases than any previous time.3 This devastating condition has not yet improved due to lack of proper treatment and medications, although more than a hundred vaccine candidates are in different stages of development.4 Most countries imposed lockdown to limit the spread of the virus, which eventually affected people’s socioeconomic conditions and mental health regardless of age, sex, profession and so on.5 COVID-19 is usually transmitted through breathing droplets or contact with infected individuals. This fear of coronavirus infection impacted the lifestyle, psychological health and relationship status of people.6 About 52.1% of people felt worried during the COVID-19 pandemic, and among them 57.8%–77.9% needed mental support from their family and friends.7
Major epidemic and pandemic outbursts have several negative impacts on individual and collective mental health in the society.5 The previous Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS) severely impacted the local people’s mental health.8 9 Healthcare providers experienced long-term occupational and psychological effects during the SARS outbreak.10 In the USA, a study was conducted among Capitol Hill staff workers to determine how they successfully responded to disaster-related mental health after the anthrax attacks in 2001. The study reported prevalence rates of post-traumatic stress disorder and postanthrax psychiatric disorder among respondents of 55% and 27%, respectively.11
The mental health of many individuals is potentially affected by COVID-19 in many ways. Family members and friends of patients with COVID-19, their close contacts, isolated or suspected population, healthcare providers, and the general population experience extra mental health burden during the COVID-19 pandemic.12 Therefore, understanding the impact of the COVID-19 pandemic on an individual’s mental health might reduce many current and future mental health issues.
Bangladesh is a densely populated country with a population size of about 164 million people. The population density is five times higher than any other mega country.13 Several factors that affect mental health are population density, housing, economic status, employment, life experience, disease burden and so on.14 The financial condition of the general population was affected after the implementation of lockdown from 26 March 2020. The Institute of Epidemiology, Disease Control and Research of Bangladesh reported the first COVID-19 cases on 8 March 2020.15 Between 8 March and 27 December 2020, there were 509 148 confirmed cases with 7452 fatalities reported in Bangladesh. It ranks 27th among countries affected by COVID-19, contributing 0.64% COVID-19-related disease burden to the world.16 At the initial stage of the pandemic, many hospitals were not ready to treat COVID-19 and testing facilities were limited. This situation impacted the mental health of many Bangladeshi people. A few people had suicidal ideations after failing to cope with this extra mental burden.17–19 The infection has reached every corner of the country. The number of confirmed cases significantly increased, and as a result mental health-related disorders may increase, particularly among susceptible people. Therefore, more attention needs to be paid to mental health burden during and after the COVID-19 pandemic.20–22 It is equally applicable to other low-income and middle-income countries, where resources are limited to tackle any pandemic situation and its associated mental health issues.23–25 The present study aimed to assess the prevalence rates of loneliness, depression, anxiety and sleep disturbance among the general Bangladeshi population during the COVID-19 pandemic. We also expected to identify factors associated with mental health problems during the COVID-19 pandemic.
Methods
Participants and procedures
We carried out a nationwide cross-sectional online survey between 15 April and 10 May 2020 using the Google survey tool (Google Forms). Here we used the purposive sampling technique to collect primary data from the participants. We assumed the CI, margin of error and expected prevalence at 95%, 5% and 30%, respectively. According to our assumption, the required sample size was 323. We initially thought the response rate might be 20% and invited 1615 people to participate in the survey. However, the actual response rate was 46%, with 736 responses received. After screening, we excluded 64 responses due to partial or incomplete information. Finally, we included 672 respondents (381 men, 291 women) aged between 15 and 65 years in the analysis. Before participation in the survey, the participants reviewed and acknowledged a brief description of the survey, eligibility requirements, procedures and electronic consent form. We obtained electronic consent from all participants. All the respondents of this survey were of Bangladeshi ethnicity and living in Bangladesh at that time. People aged between 15 and 65 years who understood the questions were included in this survey. Exclusion criteria included history of other psychiatric disorders such as delusions, mental retardation, bipolar disorder, schizophrenia, personality disorder, mood-congruent or mood-incongruent psychotic features, comorbid psychiatric illness, neurological disease, or clinical evidence of dementia. Additional exclusion criteria were acute medical conditions, chronic diseases and history of addiction. We did not pay for participation.
Estimations
We used two sets of questionnaires for this survey. The first one was a structured questionnaire designed by the researchers which contained the informed consent and sociodemographic information. The second set was a self-reported structured questionnaire from different psychometric assessment scales. We prepared both sets of questionnaire in English and then translated them to Bangla. First, all questionnaires were translated to Bangla by a medical graduate and a general person who were native speakers of Bangla and were fluent in English. An independent researcher compiled and addressed discrepancies to make a single Bangla forward version. A professional translator with expertise in medical translation and a medical graduate who was not involved in forward translation translated this Bangla version back to English. Again, an independent researcher compiled these back-translated versions in the same way.26 We piloted the questionnaire in a randomly selected small group to confirm clarity and understanding. We circulated the questionnaire in both English and Bengali versions for proper understanding of the questions. We sent the link of the designed Google Forms to participants through emails and social networking sites. The educated family members of illiterate or older respondents helped to collect their responses.
Sociodemographic and biophysical measures
We collected the most relevant sociodemographic information of the respondents. Collected data were regarding age, sex, body mass index (BMI), marital status, education level, occupation, economic status, residence, living status (with or without family) and smoking habit.
Loneliness Scale
The University of California, Los Angeles Loneliness Scale-8 (UCLA-8) is a short form of the UCLA Loneliness Scale which contains eight questions.27 Each question is scored from 1 to 4, depending on the respondent’s answer: 1 (never), 2 (rarely), 3 (sometimes) and 4 (often). We followed reverse scoring for two positive questions from other negative questions (‘I am an outgoing person’ and ‘I can find companionship when I want it’). The total score ranges from 8 to 32. Higher score indicates higher degree of loneliness. We divided the cumulative score into four groups: 8–16, no loneliness; 7–21, mild loneliness; 22–16, moderate loneliness; and 27 or above, severe loneliness.
Patient Health Questionnaire
The Patient Health Questionnaire-9 (PHQ-9) has nine different questions that assess respondents’ depressive symptoms. The total score ranges from 0 to 27 points, where each question is scored from 0 to 3 depending on the answer: 0 (not at all), 1 (several days), 2 (half of the days), and 3 (nearly every day). A score below 10 indicates no depressive symptoms, while a score of 10 or higher indicates the presence of depressive symptoms.28 To determine the gravity of depression, we divided the total score into four levels: cumulative scores <10, 10–15, 16–21 and 22–27 for no depression, mild depression, moderate depression and severe depression, respectively.
Generalized Anxiety Disorder Scale
The Generalised Anxiety Disorder 7-Item Scale (GAD-7) consists of seven basic questions that evaluate respondents’ anxiety disorder. The total score ranges from 0 to 21. Each question has four different scores depending on the response: 0 (not at all), 1 (several days), 2 (more than half the days) and 3 (nearly every day). Higher score indicates high degree of anxiety, divided into four different segments, where <5, 5–9, 10–14 and 15–21 indicate no, mild, moderate and severe anxiety, respectively.29
Pittsburgh Sleep Quality Index
We used the Pittsburgh Sleep Quality Index (PSQI) to determine the sleep quality of respondents over 1 month. This questionnaire consists of 19 specific questions in 7 different domains: (1) sleep quality (one question), (2) sleep latency (two questions), (3) sleep duration (one question), (4) sleep efficiency (three questions), (5) sleep disturbance (nine questions), (6) sleep medication (one question) and (7) daily dysfunction (two questions). Each domain score ranges from 0 to 3. The cumulative score of the seven domains ranges from 0 to 21. A higher total score indicates poor sleep quality, which determines severity. A total PSQI score below 5 indicates no sleep disturbance. A cumulative score of 5 or more indicates poor sleep. Respondents with PSQI scores greater than 10 are considered bad sleepers.30
Statistical analysis
We performed statistical analysis using Microsoft Excel 2016 and Statistical Packages for Social Sciences V.25.0. We used Microsoft Excel for data editing, sorting, coding, classification and tabulation. We then imported the Excel file into IBM SPSS software. We used descriptive statistics to analyse the characteristics of the respondents. We applied χ2 test to observe the differences in loneliness status (yes or no) with or without depression, anxiety or sleep disturbance among the respondents. We assessed the correlations between risk factors and psychometric measures (loneliness, depression, anxiety and sleep quality) using binary logistic regression analysis with a 95% CI. Statistically significant results were considered at p<0.05.
Patient and public involvement
Patients and the public were not involved in this study.
Results
The descriptive statistics for all variables of the respondents are presented in table 1. Of the 672 respondents, 57% and 43% were men and women, respectively. Half of the respondents were above 30 years of age. Of the respondents, 65% had normal BMI and about two-thirds completed higher secondary education. Of the respondents, 57%, 74% and 46% were married, non-smokers and of middle economic class, respectively. We observed two-thirds of the total respondents were living with their family (64%) in a rural area (62%).
Table 1.
Distribution of variables and their association with different mental health problems among the respondents
| Total N=672 |
Loneliness n=478 |
Depression n=256 |
Generalised anxiety n=429 |
Sleep disturbance n=494 |
||||||||||||||||||
| n | % | Yes | χ2 | df | P value | Yes | χ2 | df | P value | Yes | χ2 | df | P value | Yes | χ2 | df | P value | |||||
| n | % | n | % | n | % | n | % | |||||||||||||||
| Age (years) | ||||||||||||||||||||||
| 15–30 | 344 | 51 | 236 | 69 | 2.19 | 1 | 0.139 | 119 | 35 | 3.67 | 1 | 0.056 | 213 | 62 | 1.12 | 1 | 0.289 | 242 | 70 | 3.62 | 1 | 0.051 |
| Above 30 | 328 | 49 | 242 | 74 | 137 | 42 | 216 | 66 | 252 | 77 | ||||||||||||
| Sex | ||||||||||||||||||||||
| Male | 381 | 57 | 278 | 73 | 1.44 | 1 | 0.23 | 117 | 31 | 20.35 | 1 | <0.001 | 223 | 59 | 10.74 | 1 | 0.001 | 271 | 71 | 2.57 | 1 | 0.109 |
| Female | 291 | 43 | 200 | 69 | 139 | 48 | 206 | 71 | 233 | 80 | ||||||||||||
| Body mass index (kg/m2) | ||||||||||||||||||||||
| Below 18.5 | 32 | 5 | 24 | 75 | 0.25 | 2 | 0.88 | 18 | 56 | 4.74 | 2 | 0.093 | 28 | 88 | 8.16 | 2 | 0.017 | 26 | 81 | 1.08 | 2 | 0.584 |
| 18.5–25 | 435 | 65 | 308 | 71 | 163 | 37 | 272 | 63 | 317 | 73 | ||||||||||||
| Above 25 | 205 | 31 | 146 | 71 | 75 | 37 | 129 | 63 | 151 | 74 | ||||||||||||
| Marital status | ||||||||||||||||||||||
| Unmarried | 289 | 43 | 210 | 73 | 0.58 | 1 | 0.446 | 107 | 37 | 0.25 | 1 | 0.619 | 187 | 65 | 0.16 | 1 | 0.685 | 207 | 72 | 0.93 | 1 | 0.336 |
| Married | 383 | 57 | 268 | 70 | 149 | 39 | 242 | 63 | 287 | 75 | ||||||||||||
| Education | ||||||||||||||||||||||
| Illiterate | 26 | 4 | 21 | 81 | 7.53 | 4 | 0.11 | 15 | 58 | 6 | 4 | 0.199 | 18 | 69 | 7.39 | 4 | 0.117 | 19 | 73 | 0.71 | 4 | 0.849 |
| Primary | 85 | 13 | 59 | 69 | 35 | 41 | 61 | 72 | 65 | 76 | ||||||||||||
| Secondary | 61 | 9 | 48 | 79 | 23 | 38 | 44 | 72 | 44 | 72 | ||||||||||||
| Higher secondary | 410 | 61 | 279 | 68 | 146 | 36 | 246 | 60 | 302 | 74 | ||||||||||||
| Graduate/above | 90 | 13 | 71 | 79 | 37 | 41 | 60 | 67 | 64 | 71 | ||||||||||||
| Occupation | ||||||||||||||||||||||
| Service | 219 | 33 | 153 | 70 | 3.75 | 3 | 0.29 | 66 | 30 | 12.45 | 3 | 0.006 | 125 | 57 | 9.28 | 3 | 0.026 | 158 | 72 | 0.56 | 3 | 0.906 |
| Business | 28 | 4 | 20 | 71 | 7 | 25 | 17 | 61 | 20 | 71 | ||||||||||||
| Student | 208 | 31 | 158 | 76 | 88 | 42 | 148 | 71 | 153 | 74 | ||||||||||||
| Unemployed | 217 | 32 | 147 | 68 | 95 | 44 | 139 | 64 | 163 | 75 | ||||||||||||
| Economic status | ||||||||||||||||||||||
| Low | 245 | 36 | 179 | 73 | 0.75 | 2 | 0.688 | 106 | 43 | 6.11 | 2 | 0.047 | 163 | 67 | 1.39 | 2 | 0.499 | 177 | 72 | 2.6 | 2 | 0.273 |
| Middle | 310 | 46 | 218 | 70 | 103 | 33 | 195 | 63 | 224 | 72 | ||||||||||||
| High | 117 | 17 | 81 | 69 | 47 | 40 | 71 | 61 | 93 | 79 | ||||||||||||
| Residence | ||||||||||||||||||||||
| Urban | 255 | 38 | 184 | 72 | 0.21 | 1 | 0.646 | 109 | 43 | 3.79 | 1 | 0.052 | 164 | 64 | 0.04 | 1 | 0.841 | 192 | 75 | 0.67 | 1 | 0.413 |
| Rural | 417 | 62 | 194 | 47 | 147 | 35 | 265 | 64 | 302 | 72 | ||||||||||||
| Living status | ||||||||||||||||||||||
| With family | 430 | 64 | 291 | 68 | 11.62 | 3 | 0.009 | 179 | 42 | 9.86 | 3 | 0.02 | 274 | 64 | 1.56 | 3 | 0.665 | 323 | 75 | 4.82 | 3 | 0.185 |
| Without family | 242 | 36 | 187 | 77 | 77 | 32 | 155 | 64 | 171 | 71 | ||||||||||||
| Smoking habit | ||||||||||||||||||||||
| Smoker | 177 | 26 | 135 | 76 | 3.09 | 1 | 0.079 | 50 | 28 | 9.88 | 1 | 0.002 | 105 | 59 | 2.12 | 1 | 0.145 | 129 | 73 | 0.05 | 1 | 0.825 |
| Non-smoker | 495 | 74 | 343 | 69 | 206 | 42 | 324 | 65 | 365 | 74 | ||||||||||||
| Loneliness | ||||||||||||||||||||||
| Yes | 478 | 71 | 478 | 100 | – | – | – | 228 | 48 | 64.75 | 1 | <0.001 | 366 | 77 | 116.23 | 1 | <0.001 | 391 | 82 | 58.4 | 1 | <0.001 |
| No | 194 | 29 | 0 | 0 | 28 | 14 | 63 | 32 | 103 | 53 | ||||||||||||
| Depression | ||||||||||||||||||||||
| Yes | 256 | 38 | 228 | 89 | 64.75 | 1 | <0.001 | 256 | 100 | – | – | – | 244 | 95 | 177.45 | 1 | <0.001 | 222 | 87 | 37.04 | 1 | <0.001 |
| No | 416 | 62 | 250 | 60 | 0 | 0 | 185 | 44 | 272 | 65 | ||||||||||||
| Generalised anxiety | ||||||||||||||||||||||
| Yes | 429 | 64 | 366 | 85 | 116.23 | 1 | <0.001 | 244 | 57 | 177.45 | 1 | <0.001 | 429 | 100 | – | – | – | 366 | 85 | 84.86 | 1 | <0.001 |
| No | 243 | 36 | 112 | 46 | 12 | 5 | 0 | 0 | 128 | 53 | ||||||||||||
| Sleep disturbance | ||||||||||||||||||||||
| Yes | 494 | 75 | 391 | 79 | 58.4 | 1 | <0.001 | 222 | 45 | 37.04 | 1 | <0.001 | 366 | 75 | 84.88 | 1 | <0.001 | 494 | 100 | – | – | – |
| No | 178 | 25 | 87 | 49 | 34 | 19 | 63 | 35 | 0 | 0 | ||||||||||||
P values are significant at 95% CI (p<0.05). Significant p values are shown in bold.
df, degrees of freedom; n, Number.
The prevalence of loneliness, depression, anxiety and sleep disturbance was estimated at 71%, 38%, 64% and 73%, respectively (figure 1). The proportion of respondents experiencing loneliness was higher in (1) people living without family members versus with family members (77% vs 68%, p=0.009) and (2) people with versus without much depression (89% vs 60%, p<0.001), anxiety (85% vs 46%, p<0.001) and sleep disturbance (79% vs 49%, p<0.001), respectively. The proportion of respondents with depression was higher in (1) women versus men (48% vs 31%, p<0.001), (2) unemployed versus service (44% vs 30%, p=0.006), (3) non-smoker versus smoker (42% vs 28%, p=0.002), (4) people of lower economic status versus middle (43% vs 33%, p=0.047), (5) respondents living with family members versus without family members (42% vs 33%, p=0.020), and (6) people with versus without much loneliness (48% vs 14%, p<0.001), anxiety (57% vs 5%, p<0.001) and sleep disturbance (45% vs 19%, p<0.001), respectively. The proportion of respondents with anxiety was higher in (1) women versus men (71% vs 69%, p=0.001), (2) students versus service (71% vs 57%, p=0.026), (3) people with BMI below 18.5 kg/m2 versus above 25 kg/m2 (88% vs 63%, p=0.017), and (4) people with versus without much loneliness (77% vs 32%, p<0.001), depression (95% vs 44%, p<0.001) and sleep disturbance (75% vs 35%, p<0.001), respectively. Finally the proportion of respondents with sleep disturbance was higher in people with versus without much loneliness (82% vs 53%, p<0.001), depression (87% vs 65%, p<0.001) and anxiety (85% vs 53%, p<0.001), respectively.
Figure 1.
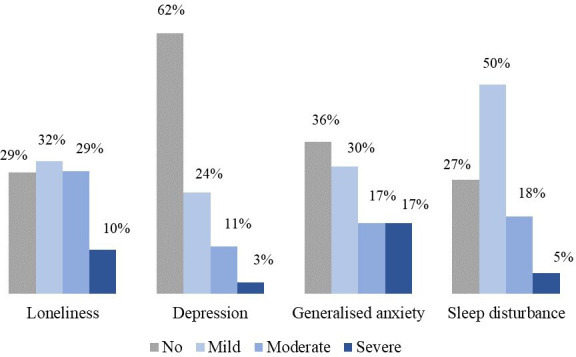
Mental health problems among the respondents based on their distribution and gravity.
We performed binary logistic regression analysis to measure the correlations between dependent and independent variables (table 2). Respondents living with family members were 0.46 times less likely than respondents living away from family members to suffer from loneliness (OR=0.46, 95% CI 0.28 to 0.75, p=0.002). Respondents on business occupations were 1.76 times more likely than the unemployed group to have depression (OR=1.76, 95% CI 1.04 to 2.99, p=0.036). Respondents from the middle economic class were 1.62 times more likely than those from high economic class to have depression (OR=1.62, 95% CI 1.04 to 2.25, p=0.033). Urban respondents were 0.66 times less likely to have depression than rural respondents (OR=0.66, 95% CI 0.43 to 0.99, p=0.044). Respondents living with family members were 1.80 times more likely to have depression than respondents living away from family members (OR=1.80, 95% CI 1.13 to 2.87, p=0.014). The probability of suffering from loneliness was 2.96 times higher in respondents who already have depression (OR=2.96, 95% CI 1.73 to 5.05, p<0.001), 3.95 times higher in respondents with anxiety (OR=3.95, 95% CI 2.51 to 6.21, p<0.001) and 2.64 times higher in respondents suffering from sleep disturbance (OR=2.64, 95% CI 1.72 to 4.05, p<0.001), respectively. The probability of having depression was 18.51 times higher in respondents with anxiety (OR=18.51, 95% CI 9.52 to 35.71, p<0.001) and 1.36 times higher in respondents suffering from sleep disturbance (OR=1.36, 95% CI 0.81 to 2.35, p<0.001), respectively. The likelihood of having anxiety was 3.60 times higher in respondents suffering from sleep disturbance (OR=3.60, 95% CI 2.24 to 5.65, p<0.001).
Table 2.
Regression analysis of variables by mental health problems among the respondents
| Loneliness n=478 |
Depression n=256 |
Generalised anxiety n=429 |
Sleep disturbance n=494 |
|||||||||
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Age (years) | ||||||||||||
| 15–30 | 0.606 | 0.359 to 1.023 | 0.061 | 0.653 | 0.386 to 1.105 | 0.112 | 0.857 | 0.490 to 1.501 | 0.59 | 0.834 | 0.499 to 1.394 | 0.489 |
| Above 30 | 1 | 1 | 1 | 1 | ||||||||
| Sex | ||||||||||||
| Male | 0.666 | 0.411 to 1.080 | 0.099 | 1.624 | 1.000 to 2.637 | 0.05 | 1.453 | 0.869 to 2.431 | 0.154 | 1.036 | 0.648 to 1.658 | 0.882 |
| Female | 1 | 1 | 1 | 1 | ||||||||
| Body mass index (kg/m2) | ||||||||||||
| Below 18.5 | 1.574 | 0.557 to 4.443 | 0.392 | 0.889 | 0.346 to 2.282 | 0.806 | 0.27 | 0.072 to 1.011 | 0.052 | 0.818 | 0.289 to 2.319 | 0.706 |
| 18.5–25 | 1.244 | 0.399 to 3.877 | 0.706 | 0.832 | 0.287 to 2.410 | 0.735 | 0.347 | 0.085 to 1.411 | 0.139 | 0.877 | 0.281 to 2.737 | 0.821 |
| Above 25 | 1 | 1 | 1 | 1 | ||||||||
| Marital status | ||||||||||||
| Unmarried | 0.902 | 0.508 to 1.600 | 0.723 | 0.845 | 0.463 to 1.542 | 0.584 | 1.097 | 0.599 to 2.011 | 0.763 | 1.009 | 0.578 to 1.764 | 0.974 |
| Married | 1 | 1 | 1 | 1 | ||||||||
| Education | ||||||||||||
| Illiterate | 0.498 | 0.211 to 1.172 | 0.111 | 1.076 | 0.476 to 2.430 | 0.861 | 0.511 | 0.215 to 1.211 | 0.127 | 1.346 | 0.617 to 2.935 | 0.455 |
| Primary | 1.365 | 0.491 to 3.794 | 0.551 | 1.545 | 0.620 to 3.851 | 0.351 | 0.566 | 0.210 to 1.525 | 0.26 | 0.855 | 0.350 to 2.090 | 0.732 |
| Secondary | 1.123 | 0.293 to 4.309 | 0.866 | 1.813 | 0.507 to 6.485 | 0.36 | 0.244 | 0.059 to 1.006 | 0.051 | 0.829 | 0.249 to 2.763 | 0.761 |
| Higher secondary | 0.518 | 0.204 to 1.314 | 0.166 | 1.006 | 0.430 to 2.351 | 0.989 | 0.788 | 0.311 to 2.000 | 0.616 | 1.396 | 0.589 to 3.310 | 0.449 |
| Graduate/above | 1 | 1 | 1 | 1 | ||||||||
| Occupation | ||||||||||||
| Service | 0.889 | 0.292 to 2.711 | 0.836 | 0.315 | 0.099 to 1.009 | 0.052 | 0.855 | 0.296 to 2.481 | 0.774 | 0.894 | 0.318 to 2.515 | 0.831 |
| Business | 1.476 | 0.895 to 2.434 | 0.127 | 1.76 | 1.037 to 2.994 | 0.036 | 1.3 | 0.754 to 2.237 | 0.344 | 1.161 | 0.702 to 1.923 | 0.559 |
| Student | 0.628 | 0.264 to 1.962 | 0.253 | 0.752 | 0.363 to 1.052 | 0.093 | 0.548 | 0.362 to 0.952 | 0.452 | 0.524 | 0.241 to 1.183 | 0.263 |
| Unemployed | 1 | 1 | 1 | |||||||||
| Economic status | ||||||||||||
| Low | 1.111 | 0.636 to 1.941 | 0.712 | 1.478 | 0.832 to 2.624 | 0.183 | 0.562 | 0.312 to 1.011 | 0.054 | 1.588 | 0.893 to 2.824 | 0.115 |
| Middle | 1.133 | 0.725 to 1.771 | 0.583 | 1.618 | 1.038 to 2.252 | 0.033 | 0.981 | 0.613 to 1.572 | 0.938 | 0.852 | 0.558 to 1.300 | 0.458 |
| High | 1 | 1 | 1 | 1 | ||||||||
| Residence | ||||||||||||
| Urban | 1.06 | 0.697 to 1.611 | 0.785 | 0.655 | 0.434 to 0.988 | 0.044 | 1.146 | 0.737 to 1.781 | 0.545 | 0.929 | 0.618 to 1.397 | 0.724 |
| Rural | 1 | 1 | 1 | 1 | ||||||||
| Living status | ||||||||||||
| With family | 0.457 | 0.278 to 0.751 | 0.002 | 1.797 | 1.126 to 2.867 | 0.014 | 0.842 | 0.511 to 1.388 | 0.501 | 1.344 | 0.844 to 2.140 | 0.213 |
| Without family | 1 | 1 | 1 | 1 | ||||||||
| Smoking habit | ||||||||||||
| Smoker | 0.637 | 0.376 to 1.078 | 0.093 | 1.441 | 0.849 to 2.447 | 0.176 | 1.032 | 0.611 to 1.743 | 0.906 | 0.925 | 0.567 to 1.509 | 0.755 |
| Non-smoker | 1 | 1 | 1 | 1 | ||||||||
| Loneliness | ||||||||||||
| Yes | – | – | – | 2.89 | 1.669 to 5.000 | <0.001 | 3.952 | 2.500 to 6.211 | <0.001 | 2.525 | 1.647 to 3.875 | <0.001 |
| No | – | 1 | 1 | 1 | ||||||||
| Depression | ||||||||||||
| Yes | 2.958 | 1.733 to 5.050 | <0.001 | – | – | – | 18.518 | 9.615 to 35.714 | <0.001 | 1.344 | 0.800 to 2.257 | 0.263 |
| No | 1 | – | 1 | 1 | ||||||||
| Generalised anxiety | ||||||||||||
| Yes | 3.952 | 2.506 to 6.211 | <0.001 | 18.518 | 9.523 to 35.714 | <0.001 | – | – | – | 3.367 | 2.127 to 3.519 | <0.001 |
| No | 1 | 1 | – | 1 | ||||||||
| Sleep disturbance | ||||||||||||
| Yes | 2.638 | 1.718 to 4.048 | <0.001 | 1.385 | 0.814 to 2.352 | 0.229 | 3.558 | 2.237 to 5.649 | <0.001 | – | – | – |
| No | 1 | 1 | 1 | – | ||||||||
P values are significant at 95% CI (p<0.05). Significant p values are shown in bold.
n, Number.
Discussion
This study examines the impact of the COVID-19 pandemic on the mental health of the general Bangladeshi population. We observed the prevalence rates of loneliness, depression, anxiety and sleep disturbance among the general population were 71%, 38%, 64% and 73%, respectively (figure 1). We observed the associated factors behind the mental health issues are female sex, low economic status, being a student or unemployed, and living without a family. The findings showed a much higher rate of loneliness, depression, anxiety and sleep disturbance among Bangladeshi people during the COVID-19 pandemic. Consistent with our study findings, a cross-sectional epidemiological study reported a higher prevalence of stress (73.4%), depression (50.7%), anxiety (44.7%) and sleep disturbance (36.1%) among Chinese people at the early stage of the outbreak.31 The higher rates of mental health problems in the present study are consistent with the previous SARS and MERS outbreaks.8 9 During the early stage of the pandemic, people had little knowledge about the virus, preventive measures and treatment procedures, fatality rate, and so on. The little information and uncertainty about COVID-19 might contribute to the higher rate of mental health problems.
The present study found that about three in every four people in Bangladesh suffered from loneliness at any level of gravity during the lockdown period. Among them, 39% were suffering from moderate to severe loneliness. People living without family during lockdown are more prone to developing loneliness than people living with family. A previous report suggested that social isolation during the COVID-19 pandemic was a risk factor for loneliness.32 People with considerable loneliness are prone to developing other mental health problems, low well-being and suicidal behaviours.33 34 Following the current findings, one study conducted in the UK observed 36% of the respondents felt lonely during the COVID-19 pandemic, which is higher than any previous time.35 Another two studies also reported higher loneliness scores among the general population during COVID-19 than the past times.36 37 We observed a high prevalence of loneliness among people living without their family members. In agreement with the present findings, a recent study reported increased levels of loneliness among women, young people, single, unemployed and those who have other psychiatric illnesses.38 Public communication regarding social distancing and mental well-being involving psychologists, social scientists and mental health specialists can reduce the burden of loneliness.39
Among the respondents, 38% experienced depressive symptoms, including mild (24%), moderate (11%) and severe (3%) symptoms. We also observed a higher prevalence of depressive symptoms among women, people of low economic class, unemployed people, students and people living without a family. Several previous studies also reported a higher rate of depressive symptoms among women than men during the COVID-19 pandemic.40–43 Similar to the results of the present study, an increased rate of depression was reported in several recent studies in Spain, China and Hong Kong due to the COVID-19 pandemic.44–46 However, some previous studies reported depression symptoms among the general Chinese population were 16.5% and among Japanese people 11.4%.47 48 These inconsistencies might be the result of developed socioeconomic status and healthcare facilities. Among the study participants, 64% reported anxiety symptoms, where 30%, 17% and 17% were mild, moderate and severe cases, respectively. Similar to our findings, a study reported the prevalence rate of anxiety disorder in China was 28.8%, ranging from moderate to severe symptoms.49 Also, a high prevalence of anxiety disorder was observed among respondents from many countries during the COVID-19 pandemic compared with previous times.4 40 The prevalence rate of anxiety among Bangladeshi students was 71% in the present study. Final-year students of different education levels might contribute to this high rate due to uncertainty in examinations and the job market. We observed 73% of the general population were suffering from sleep disturbance during the COVID-19 pandemic. Among them, 50%, 18% and 5% reported mild, moderate and severe sleep disturbance. The present study also demonstrated that respondents suffering from loneliness, depression or anxiety are more likely to have sleep disturbance than healthy individuals. Many recent studies reported similar findings. A previous study in China observed that among the general population 29.2% had insomnia, 27.9% had depressive symptoms and 31.6% had anxiety disorder during the COVID-19 pandemic.50 Similarly, another study among Italian people observed 42.2% sleep disturbance, 17.4% moderate or severe insomnia, 24.7% depressive symptoms and 23.2% anxiety symptoms.51
To prevent the rapid spread of COVID-19 infection, the Bangladesh government has closed all educational institutions since 18 March 2020. A country-wide lockdown has been imposed to limit public movement since 26 March 2020 and ordered people to stay at home.17 The country-wide movement restrictions and stay at home orders greatly impacted the market economy, offices, business organisations and transport systems.52 53 Most of the Bangladeshi population depend on regular income, and due to the indefinite lockdown they were uncertain about returning to their workplace. This situation created a confounding impact on their mental health status.54 In Bangladesh, we observed several reported suicide cases during the COVID-19 pandemic as a result of getting infected, economic loss, social security, job security and emotional breakdown among marginalised wage earners.55 56 An Indian case study suggested that COVID-19 may significantly impact the mental health status and influence suicidal ideation and suicide attempts among the affected people; other comorbid diseases may aggravate the situation.57 We found that 44% of unemployed and 30% of service holders were suffering from depression. About 43% of people belonging to the lower economic class faced depression during the lockdown period.
The prevalence rates of mental health problems before the COVID-19 period varied from 6.5% to 31.0% among adults in Bangladesh.58 The significant increase in prevalence rates of mental health issues during the COVID-19 pandemic (ranging from 38% to 73%) in the present study is a concern. Therefore, the National Institute of Mental Health of Bangladesh has announced some recommendations. Recommendations regarding the management of mental health during the COVID-19 pandemic include using psychotropics, avoiding COVID-19 news or scrolling the news several times a day, authenticating sources of information, less use of social media, employing simple relaxation techniques such as breathing exercises, and so on.59 In agreement with these suggestions, several studies also recommended online responses, counselling, social support, and training on mental health for patients, healthcare professionals, public service holders, youth, students and elderly populations to manage mental health problems.24 60 61 Worldwide, the COVID-19 pandemic has revealed how unprepared the healthcare systems are, as well as the scarcity of resources (personal protective equipment, testing kits and so on) to combat the situation.62
Strengths and limitations of this study
The present study has some limitations. First, online self-reporting surveys might have multiple biases and are not representative of those without internet facilities. Second, this cross-sectional study was not able to measure the impact of these mental illnesses over time. Third, we did not assess the altered lifestyle of the respondents during the COVID-19 pandemic. The present study also has some advantages. First, this is the first ever study in Bangladesh to assess the four major mental health issues during the COVID-19 pandemic. This study provides an idea about the mental health of the Bangladeshi population during the COVID-19 pandemic.
Future research
This study highlights the need for mental health assessment and proper management of these issues during the COVID-19 pandemic and future research among healthcare professionals to explore their actual mental health status in this pandemic situation.
Conclusion
In summary, our findings reflect the gravity of mental health problems during the COVID-19 pandemic. A large portion of the general population in Bangladesh were affected mentally with different levels of severity. We suggest intensive mental healthcare services for the Bangladeshi people. Therefore, integrated government, non-government and community activities can ensure individual and collective mental health. Mental health support, social security and economic stability should also be top priorities to grow confidence among the general population.
Supplementary Material
Acknowledgments
All the authors are thankful to the participants for their cooperation to conduct this study.
Footnotes
Contributors: RD conceived the idea, designed the study, collected the data and prepared the initial draft of the manuscript. MRH and SD contributed to the development of the study design, collected the data and edited the manuscript. MRI conceived and designed the study, analysed and interpreted the data, reviewed the manuscript for important intellectual content and supervised the whole work. All authors approved the final version of the manuscript for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All relevant data and information can be obtained from the corresponding author upon reasonable request.
References
- 1.Talevi D, Socci V, Carai M, et al. Mental health outcomes of the CoViD-19 pandemic. Riv Psichiatr 2020;55:137–44. 10.1708/3382.33569 [DOI] [PubMed] [Google Scholar]
- 2.WHO . COVID-19 Weekly Epidemiological Update - 29 December, 2020. Available: https://www.who.int/publications/m/item/weekly-epidemiological-update-29-december-2020 [Accessed 06 Feb 2021].
- 3.WHO . Who coronavirus disease (COVID-19) Dashboard. Available: https://covid19.who.int/?gclid=Cj0KCQiAmfmABhCHARIsACwPRADLrk2VaTyZeSFy6kf8pjyrLYNDLGHR0c8z4nYnqSyLggvDD63O9eAaAiK0EALw_wcB [Accessed 06 Feb 2021].
- 4.Chen Y, Zhou H, Zhou Y, et al. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res 2020;288:113005. 10.1016/j.psychres.2020.113005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry 2020;7:300–2. 10.1016/S2215-0366(20)30073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madabhavi I, Sarkar M, Kadakol N. COVID-19: a review. Monaldi Arch Chest Dis 2020;90. 10.4081/monaldi.2020.1298. [Epub ahead of print: 14 May 2020]. [DOI] [PubMed] [Google Scholar]
- 7.Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Public Health 2020;17:2381. 10.3390/ijerph17072381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lau JTF, Griffiths S, Choi KC, et al. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect Dis 2010;10:139. 10.1186/1471-2334-10-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeong H, Yim HW, Song Y-J, et al. Mental health status of people isolated due to middle East respiratory syndrome. Epidemiol Health 2016;38:e2016048. 10.4178/epih.e2016048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maunder RG, Lancee WJ, Balderson KE, et al. Long-Term psychological and occupational effects of providing Hospital healthcare during SARS outbreak. Emerg Infect Dis 2006;12:1924–32. 10.3201/eid1212.060584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.North CS, Pfefferbaum B, Vythilingam M, et al. Exposure to bioterrorism and mental health response among staff on capitol Hill. Biosecur Bioterror 2009;7:379–88. 10.1089/bsp.2009.0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020;7:228–9. 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Central Intelligence Agency . The world factbook, 2020. Available: https://www.cia.gov/library/publications/resources/the-world-factbook/geos/print_bg.html [Accessed 01 Sep 2020].
- 14.Streatfield PK, Karar ZA. Population challenges for Bangladesh in the coming decades. J Health Popul Nutr 2008;26:261–72. [PMC free article] [PubMed] [Google Scholar]
- 15.Paul R. Bangladesh confirms its first three cases of coronavirus, 2020. Available: https://www.reuters.com/article/us-healthcoronavirus-bangladesh-idUSKBN20V0FS [Accessed 14 Apr 2020].
- 16.WHO . WHO Bangladesh COVID-19 Morbidity and Mortality Weekly Update - 27 - December 2020 (MMWU). Available: https://cdn.who.int/media/docs/default-source/searo/bangladesh/covid-19-who-bangladesh-situation-reports/who_covid-19-update_44_20201227.pdf?sfvrsn=bffee8db_7 [Accessed 06 Feb 2021].
- 17.The Daily Star . Man left out of relief net dies by suicide in Chattogram, 2020. Available: https://www.thedailystar.net/coronavirus-deadly-new-threat/news/man-left-out-relief-net-dies-suicide-chattogram-1893409 [Accessed 16 Apr 2020].
- 18.The Kaler Kantho . Day labourer commits suicide in Naldanga (in Bangla), 2020. Available: https://www.kalerkantho.com/home/printnews/898402/2020-04-13 [Accessed 13 Apr 2020].
- 19.The Jugantor . The young woman committed suicide after losing her job in corona left Posting on Facebook (in Bangla), 2020. Available: https://rb.gy/pmssav [Accessed 11 Jul 2020].
- 20.Silva Junior FJGda, Sales JCES, Monteiro CFdeS, et al. Impact of COVID-19 pandemic on mental health of young people and adults: a systematic review protocol of observational studies. BMJ Open 2020;10:e039426. 10.1136/bmjopen-2020-039426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lopes-Júnior LC, Bomfim E, Silveira DSCda, et al. Effectiveness of mass testing for control of COVID-19: a systematic review protocol. BMJ Open 2020;10:e040413. 10.1136/bmjopen-2020-040413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Every-Palmer S, Jenkins M, Gendall P, et al. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: a cross-sectional study. PLoS One 2020;15:e0241658. 10.1371/journal.pone.0241658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e15–16. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang Y, Li W, Zhang Q, et al. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e19. 10.1016/S2215-0366(20)30079-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beaton DE, Bombardier C, Guillemin F, et al. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000;25:3186–91. 10.1097/00007632-200012150-00014 [DOI] [PubMed] [Google Scholar]
- 27.Hays RD, DiMatteo MR. A short-form measure of loneliness. J Pers Assess 1987;51:69–81. 10.1207/s15327752jpa5101_6 [DOI] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 30.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 31.Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e17–18. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dahlberg L. Loneliness during the COVID-19 pandemic. Aging Ment Health 2021;25:1–4. [DOI] [PubMed] [Google Scholar]
- 33.Leigh-Hunt N, Bagguley D, Bash K, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017;152:157–71. 10.1016/j.puhe.2017.07.035 [DOI] [PubMed] [Google Scholar]
- 34.Rico-Uribe LA, Caballero FF, Martín-María N, et al. Association of loneliness with all-cause mortality: a meta-analysis. PLoS One 2018;13:e0190033. 10.1371/journal.pone.0190033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res 2020;291:113267. 10.1016/j.psychres.2020.113267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luchetti M, Lee JH, Aschwanden D, et al. The trajectory of loneliness in response to COVID-19. Am Psychol 2020;75:897–908. 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Killgore WDS, Cloonan SA, Taylor EC, et al. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res 2020;290:113117. 10.1016/j.psychres.2020.113117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoffart A, Johnson SU, Ebrahimi OV. Loneliness and social distancing during the COVID-19 pandemic: risk factors and associations with psychopathology. Front Psychiatry 2020;11:589127. 10.3389/fpsyt.2020.589127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Popa E. Loneliness and negative effects on mental health as trade-offs of the policy response to COVID-19. Hist Philos Life Sci 2021;43:15. 10.1007/s40656-021-00372-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhou S-J, Zhang L-G, Wang L-L, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry 2020;29:749–58. 10.1007/s00787-020-01541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Islam MR, Ali S, Karmoker JR, et al. Evaluation of serum amino acids and non-enzymatic antioxidants in drug-naïve first-episode major depressive disorder. BMC Psychiatry 2020;20:333. 10.1186/s12888-020-02738-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li G, Miao J, Wang H, et al. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J Neurol Neurosurg Psychiatry 2020;91:895–7. 10.1136/jnnp-2020-323134 [DOI] [PubMed] [Google Scholar]
- 43.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun 2020;87:11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.González-Sanguino C, Ausín B, Castellanos Miguel Ángel, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 2020;87:172–6. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020;288:112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 2020;17:3740. 10.3390/ijerph17103740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 2020;87:40–8. 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ueda M, Stickley A, Sue H, et al. Mental health status of the general population during the COVID-19 pandemic: a cross-sectional national survey in Japan. medRxiv 2020. 10.1101/2020.04.28.20082453 [DOI] [Google Scholar]
- 49.Liu X, Luo W-T, Li Y, et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect Dis Poverty 2020;9:58. 10.1186/s40249-020-00678-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shi L, Lu Z-A, Que J-Y, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open 2020;3:e2014053. 10.1001/jamanetworkopen.2020.14053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gualano MR, Lo Moro G, Voglino G, et al. Effects of Covid-19 Lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health 2020;17:4779. 10.3390/ijerph17134779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.The Bangla Tribune . The patient committed suicide by jumping from the roof as He was infected with corona (in Bangla), 2020. Available: https://rb.gy/jfogjx [Accessed 11 Jun 2020].
- 53.The Somoy News . Patient commits suicide without getting treatment in hospital (in Bangla), 2020. Available: https://www.somoynews.tv/pages/details/214750 [Accessed 20 May 2020].
- 54.Hossain KA, Roy S, Ullah MM. COVID-19 and mental health challenges in Bangladesh. AMDHS 2020;2:31–3. 10.5530/amdhs.2020.2.8 [DOI] [Google Scholar]
- 55.The BBC News . Corona virus: COVID-19 patient committed suicide after escaping from the hospital (in Bangla), 2020. Available: https://www.bbc.com/bengali/news-53125017 [Accessed 21 Jun 2020].
- 56.The Desh Rupantor . Corona-infected businessman commits suicide (in Bangla), 2020. Available: https://www.deshrupantor.com/mofossol/2020/07/07/230368 [Accessed 07 Jul 2020].
- 57.Hossain MM, Tasnim S, Sultana A. COVID-19 and suicide of an army soldier in India: perspectives on psychosocial epidemiology of suicidal behavior. SocArXiv 2020. [Google Scholar]
- 58.Hossain MD, Ahmed HU, Chowdhury WA, et al. Mental disorders in Bangladesh: a systematic review. BMC Psychiatry 2014;14:216. 10.1186/s12888-014-0216-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.National Institute of Mental Health (MIMH) . Recommendations from sub Committee for mental health, 2020. Available: https://mofa.portal.gov.bd/sites/default/files/files/mofa.portal.gov.bd/page/ad1f289c_47cf_4f6c_8dee_887957be3176/Guideline%20for%20Mental%20Health%20Issue-COVID-19-%20DGHS.pdf [Accessed 01 Sep 2020].
- 60.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Armitage R, Nellums LB. The COVID-19 response must be disability inclusive. Lancet Public Health 2020;5:e257. 10.1016/S2468-2667(20)30076-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020;383:510–2. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data and information can be obtained from the corresponding author upon reasonable request.


